Patents
Literature
Hiro is an intelligent assistant for R&D personnel, combined with Patent DNA, to facilitate innovative research.
296 results about "Vascular structure" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
Vascular structure - a structure composed of or provided with blood vessels. anatomical structure, bodily structure, body structure, complex body part, structure - a particular complex anatomical part of a living thing; "he has good bone structure". pulp - the soft inner part of a tooth.
Devices and methods for selective surgical removal of tissue
ActiveUS7738969B2Improve securityAvoid injuryCannulasAnti-incontinence devicesSurgical removalVascular structure
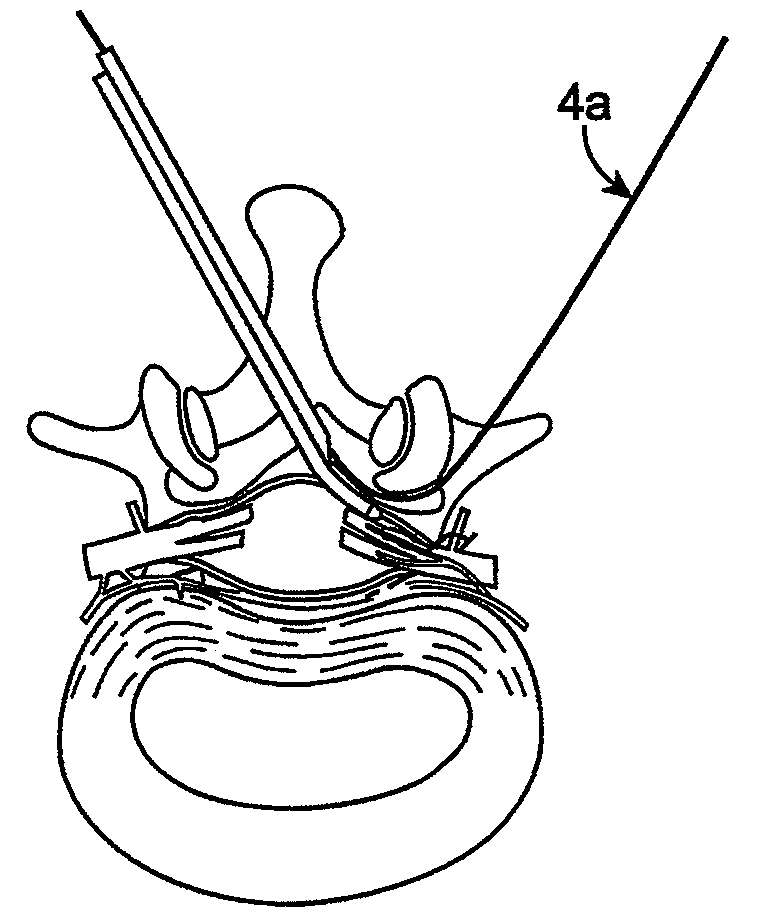
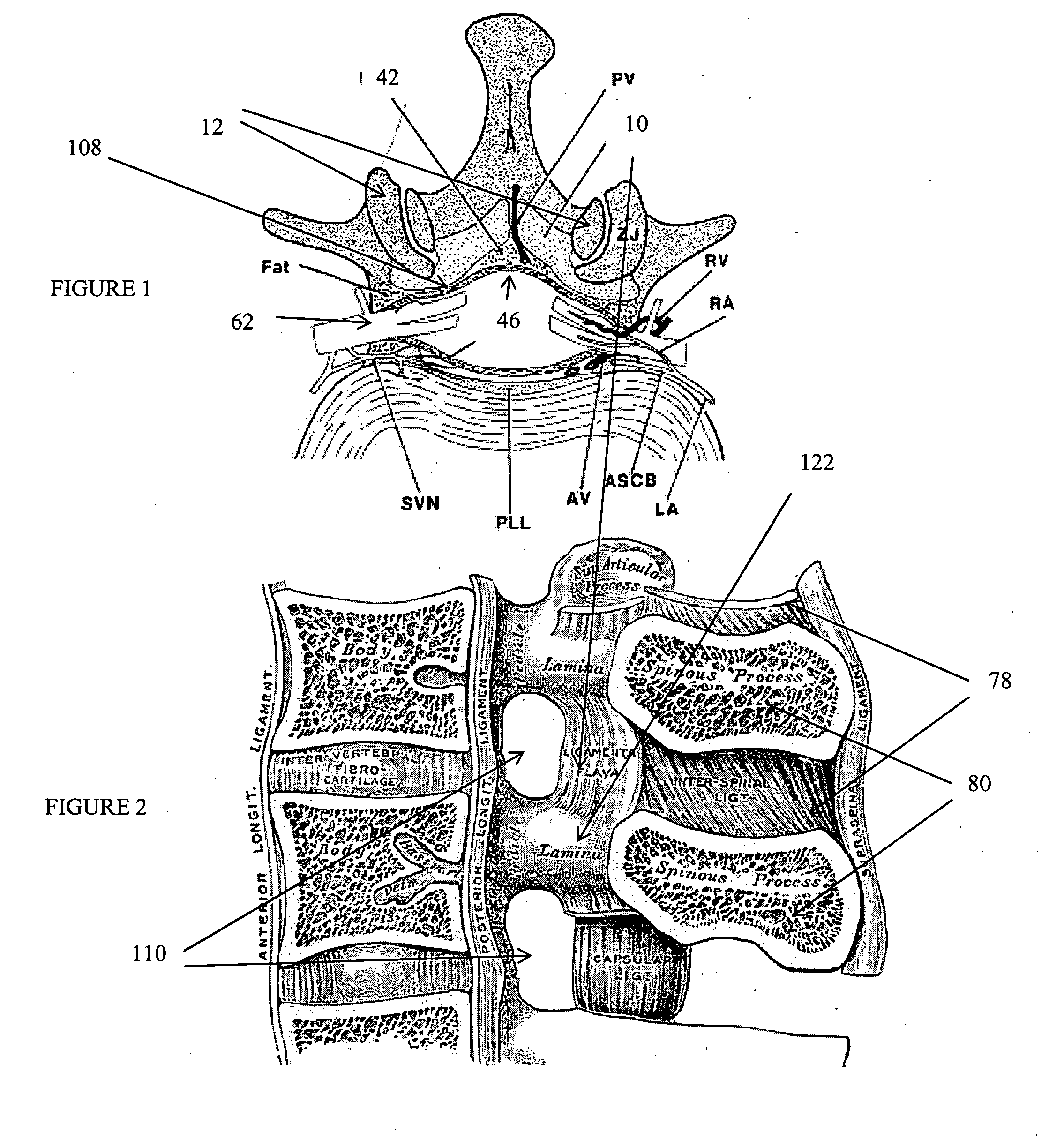
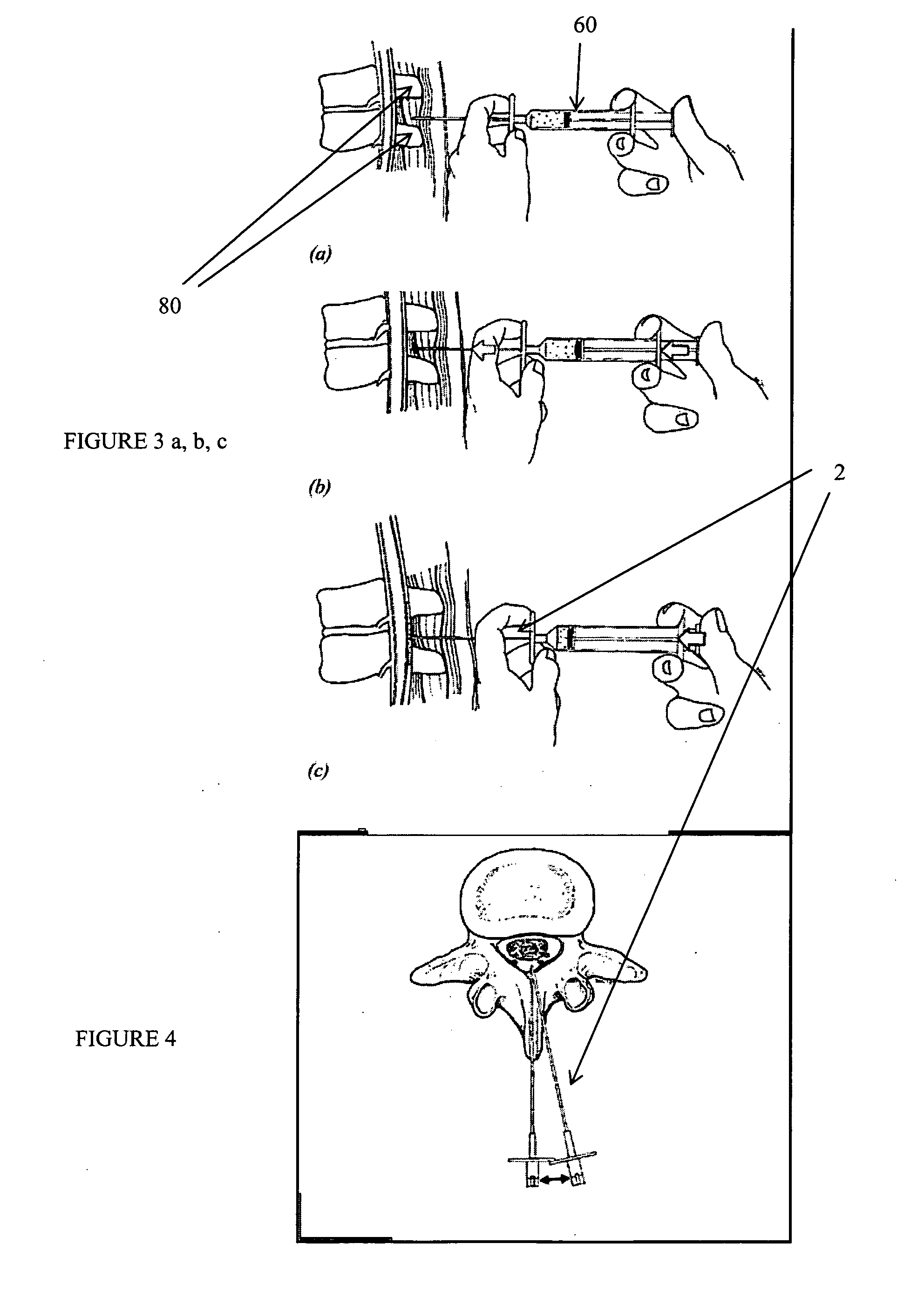
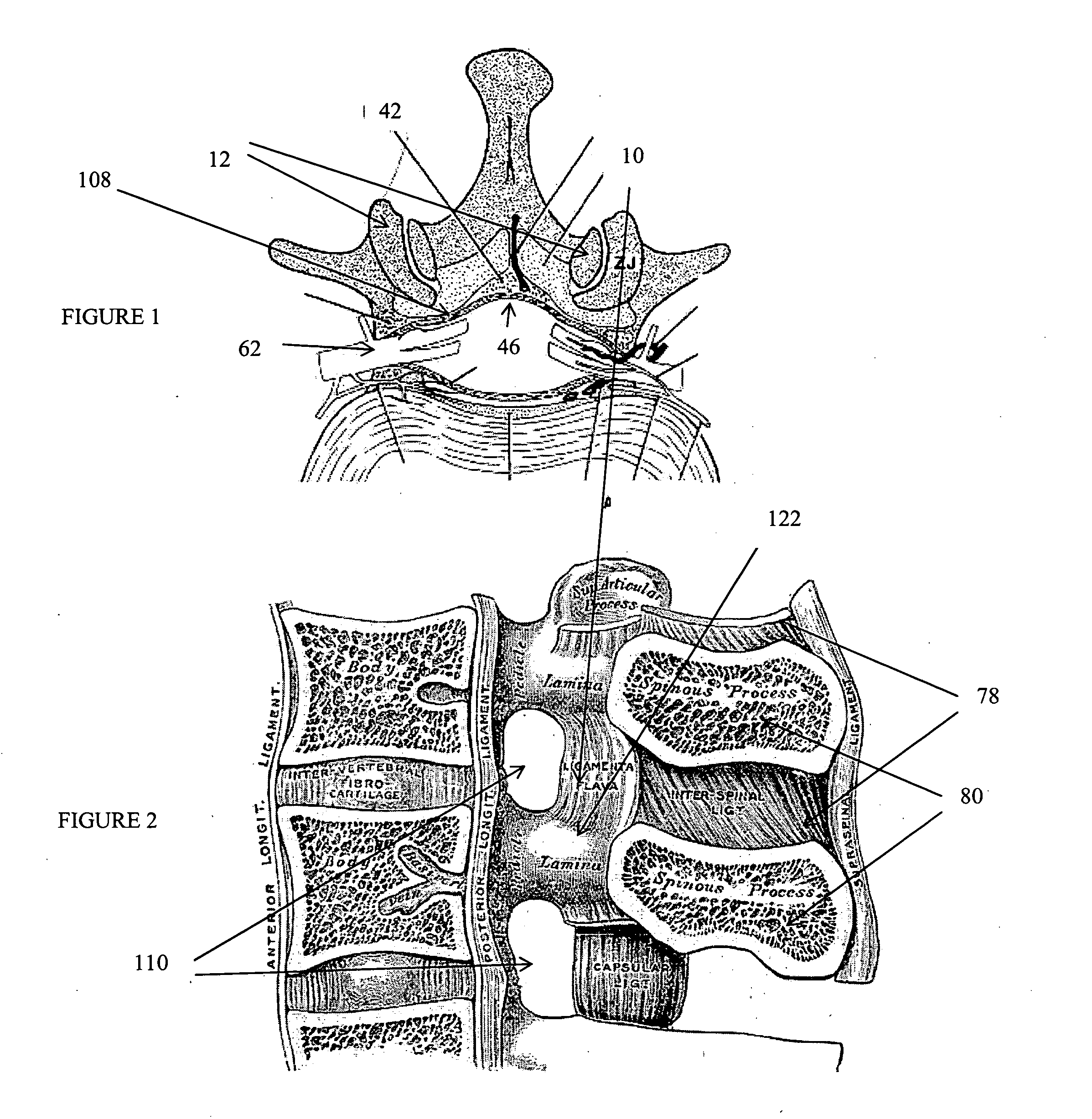
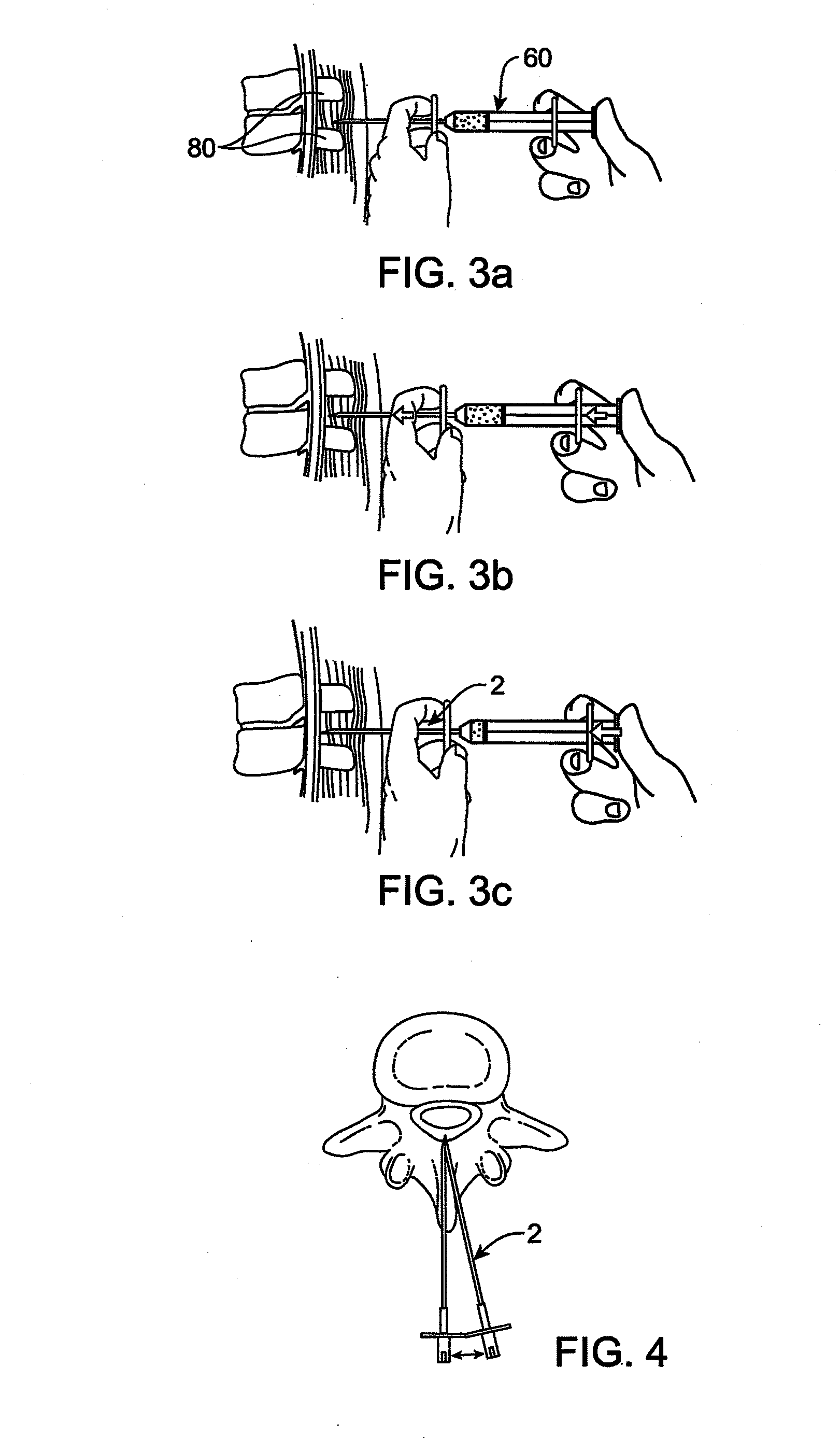
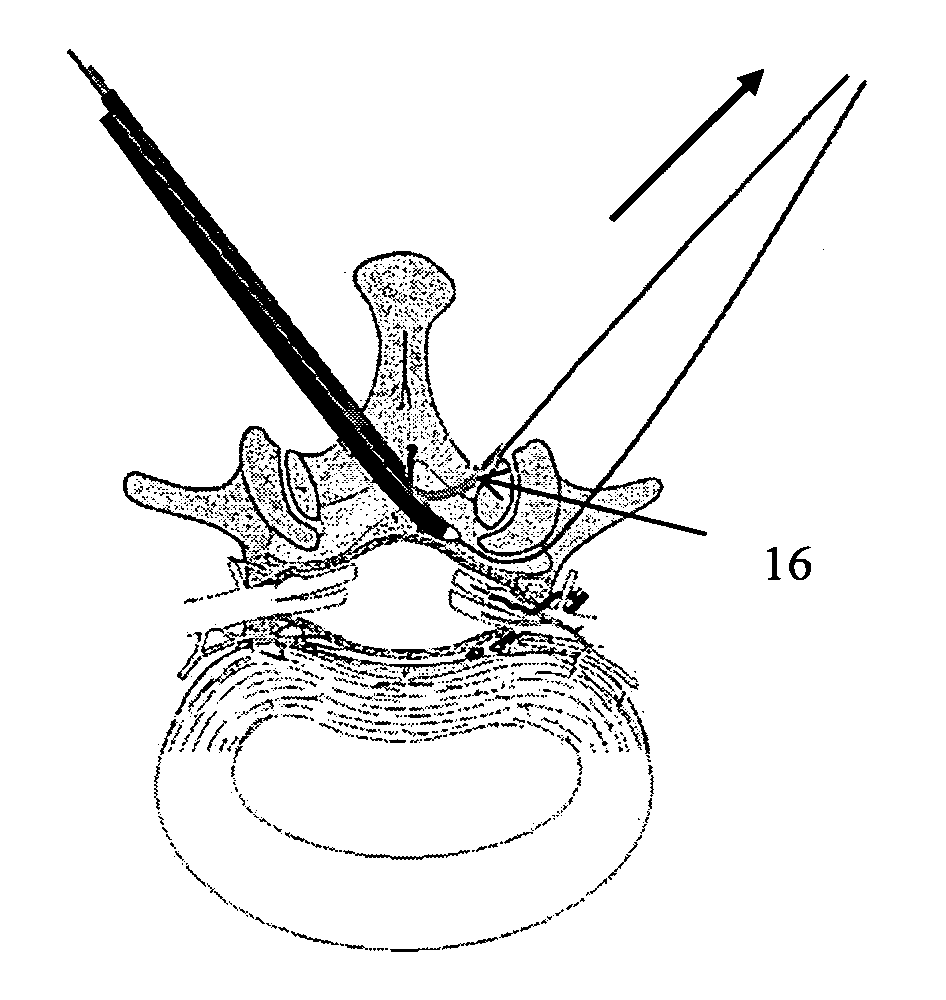
Methods and apparatus are provided for selective surgical removal of tissue. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. The sharp tip of the needle in the epidural space, can be converted to a blunt tipped instrument for further safe advancement. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. A nerve stimulator may be provided to reduce a risk of inadvertent neural abrasion.
Owner:MIS IP HLDG LLC +1
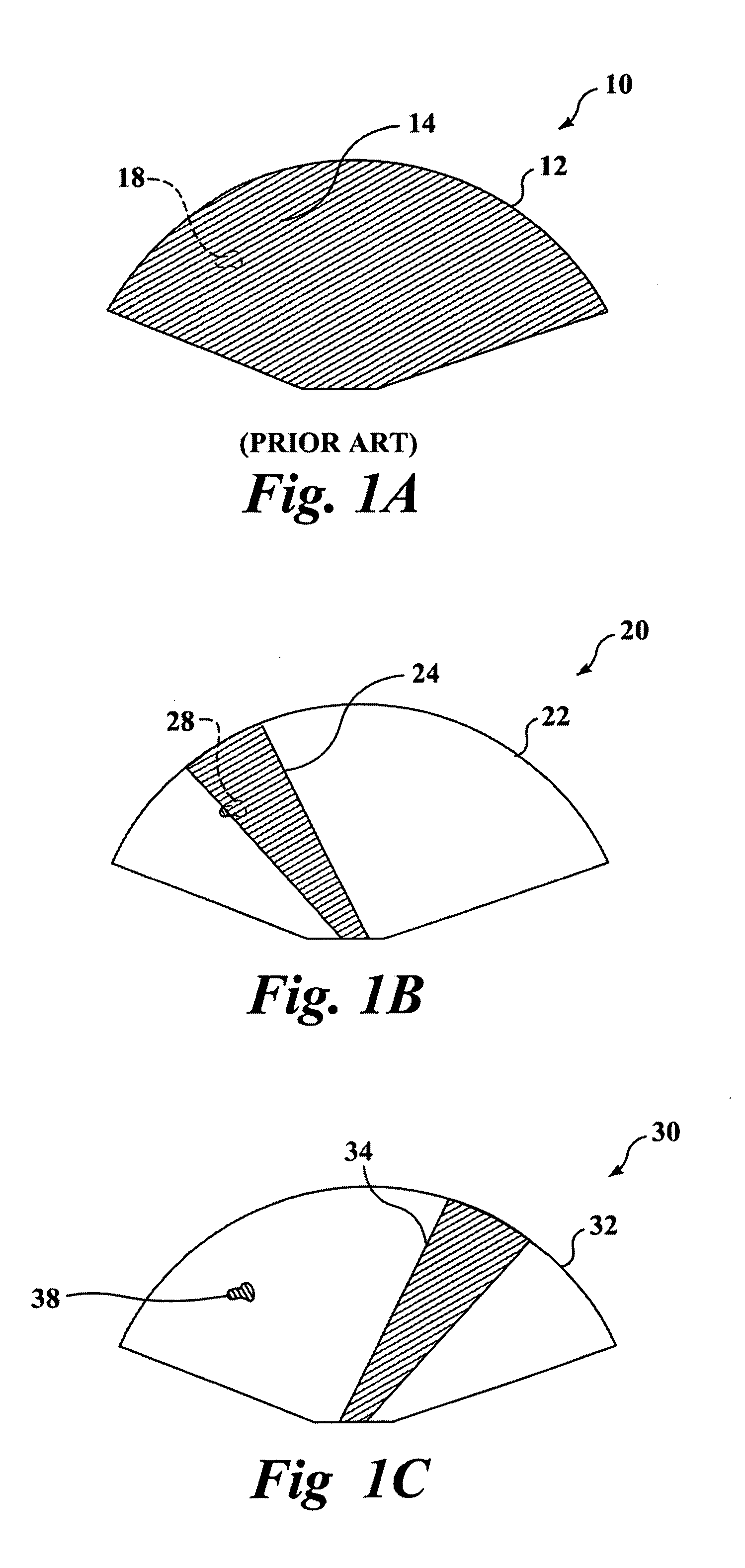
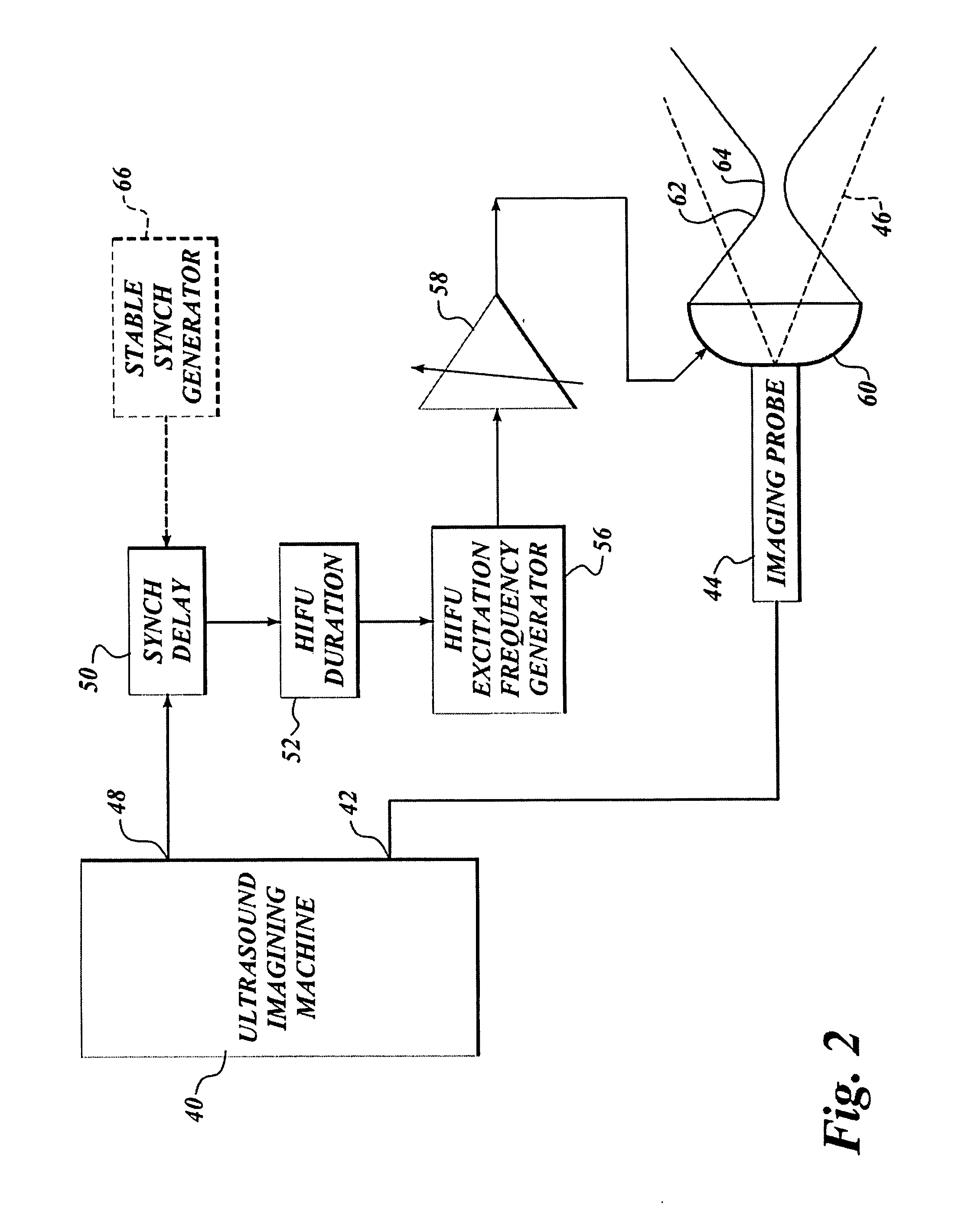
Use of contrast agents to increase the effectiveness of high intensity focused ultrasound therapy
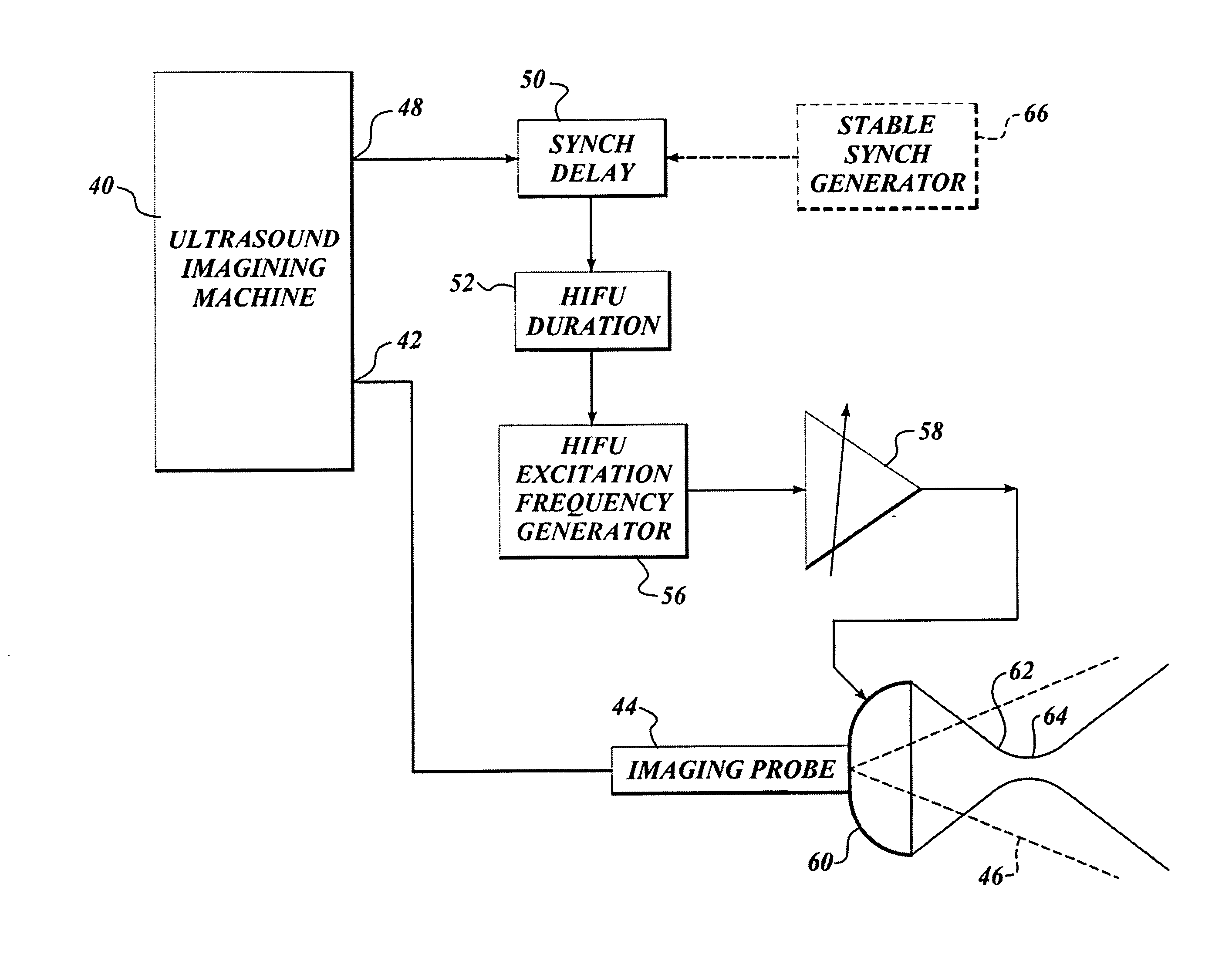
InactiveUS20050038340A1Easy to useGood choiceUltrasound therapyBlood flow measurement devicesCavitationUltrasound contrast media
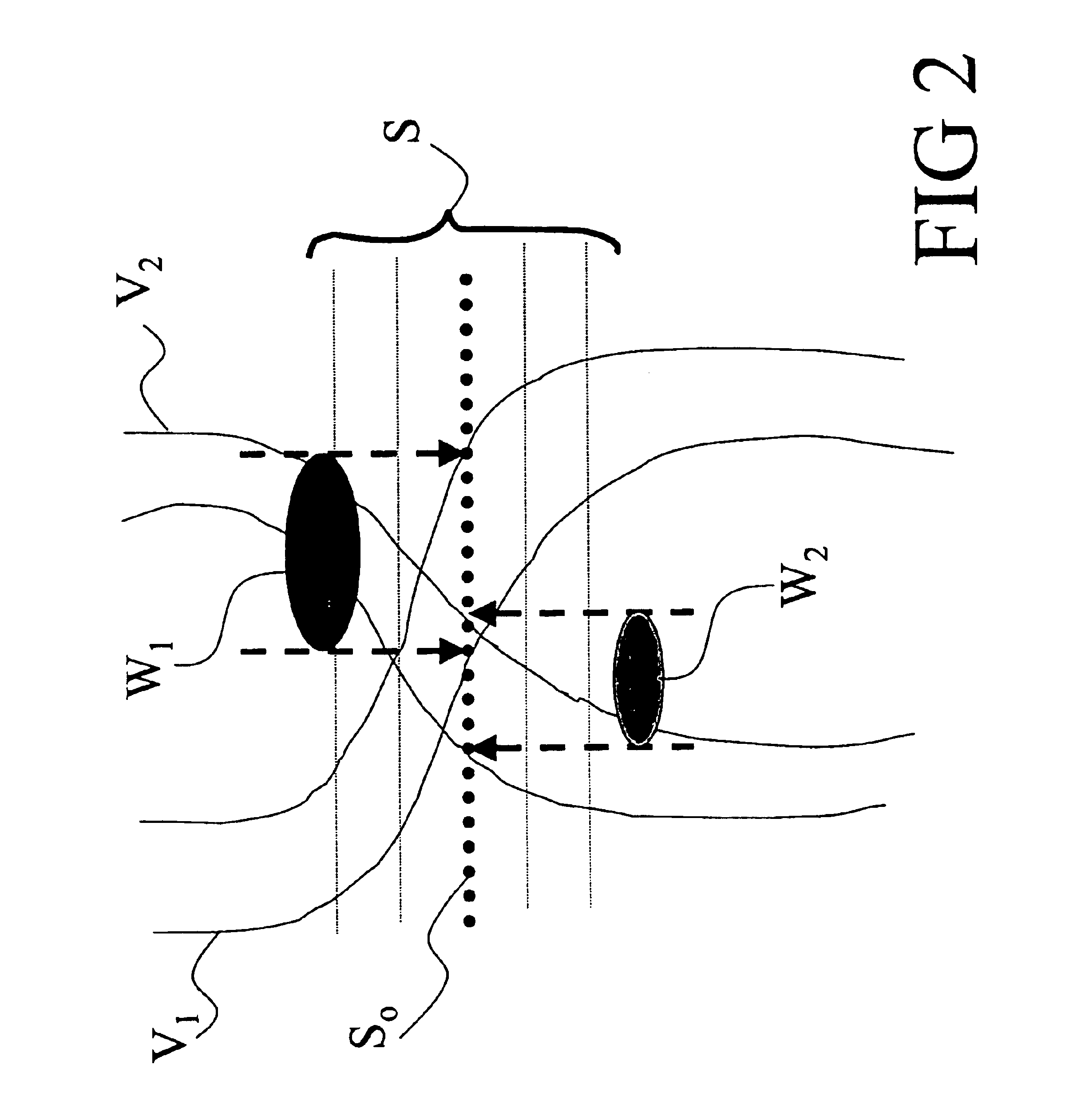
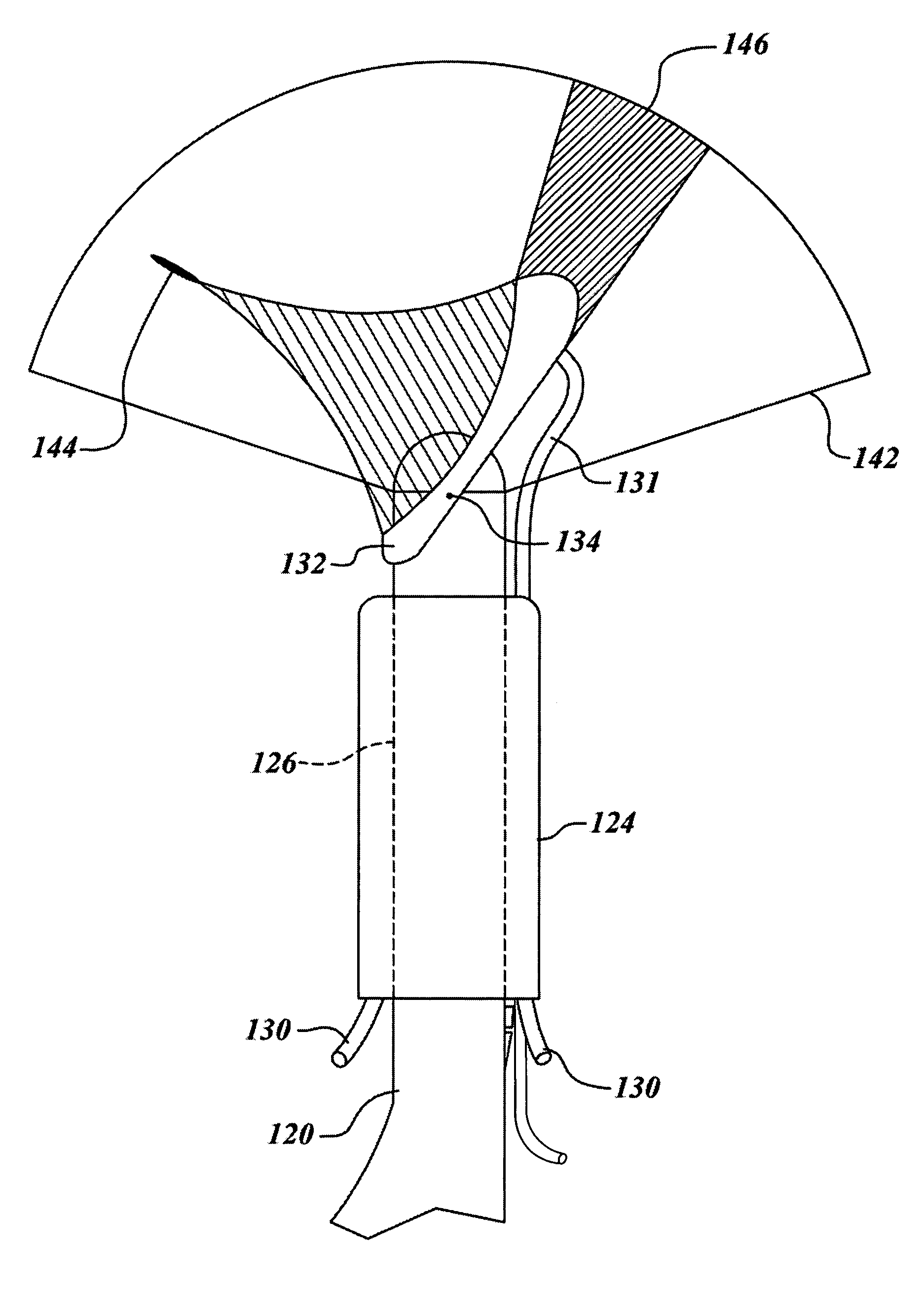
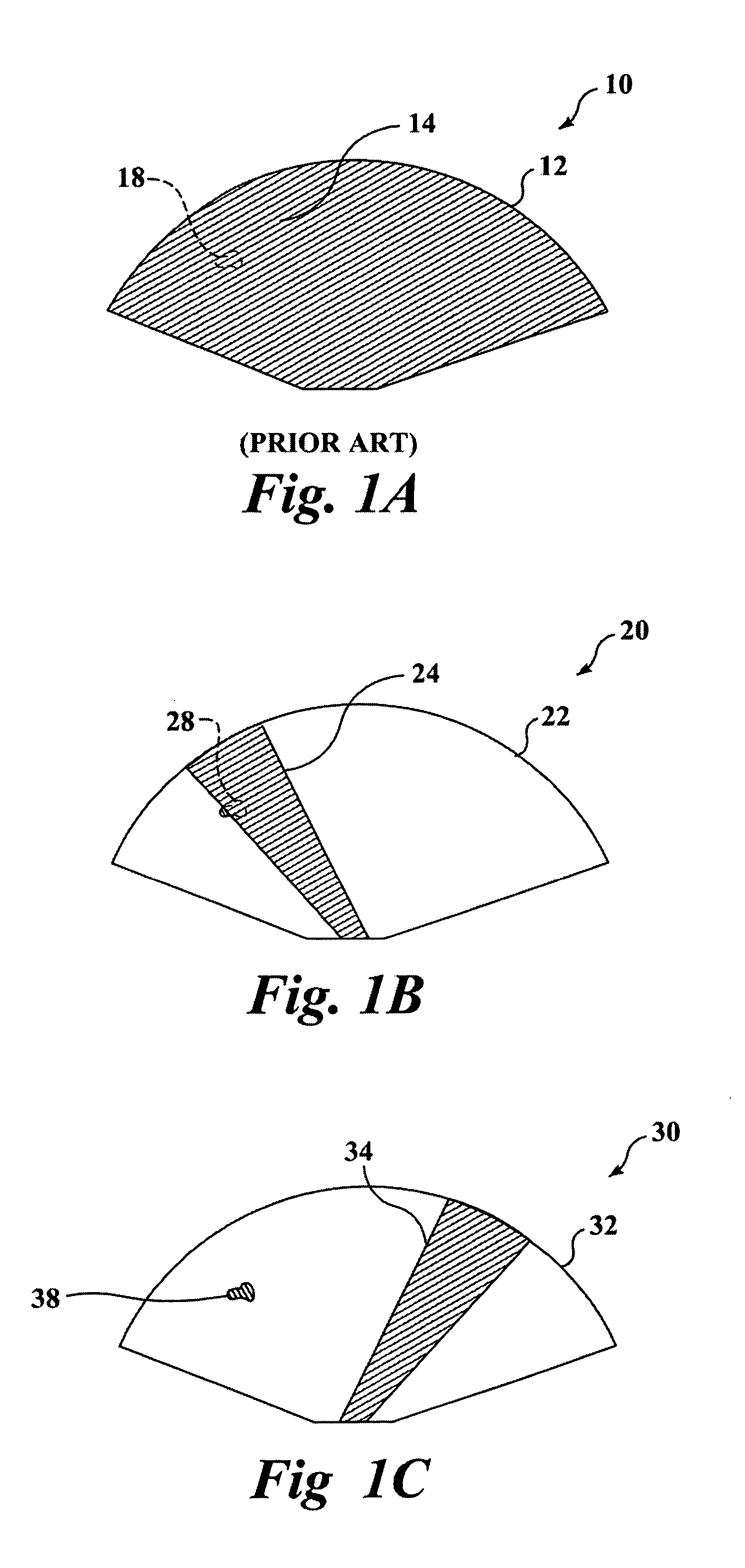
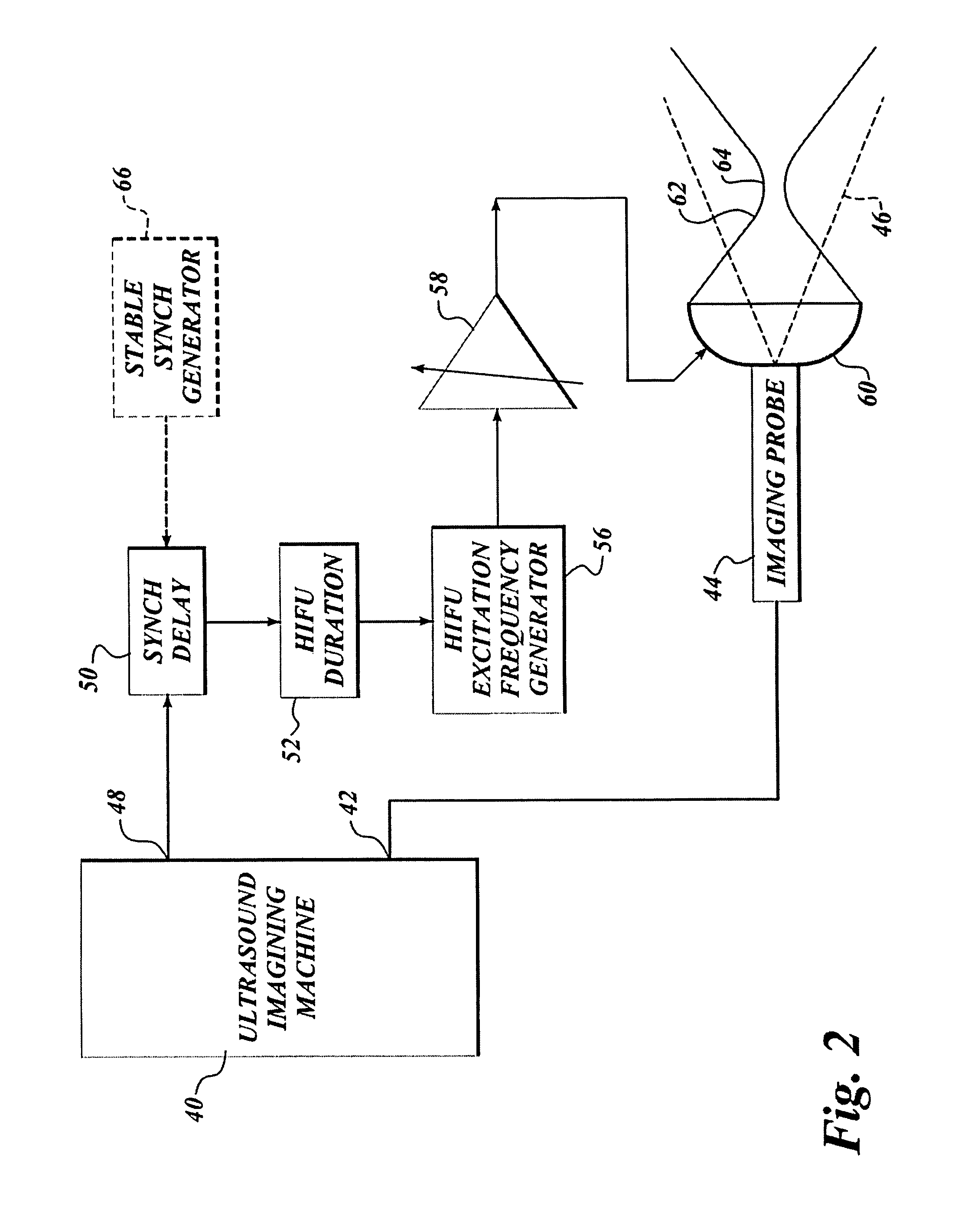
Ultrasound contrast agents are used to enhance imaging and facilitate HIFU therapy in four different ways. A contrast agent is used: (1) before therapy to locate specific vascular structures for treatment; (2) to determine the focal point of a HIFU therapy transducer while the HIFU therapy transducer is operated at a relatively low power level, so that non-target tissue is not damaged as the HIFU is transducer is properly focused at the target location; (3) to provide a positive feedback mechanism by causing cavitation that generates heat, reducing the level of HIFU energy administered for therapy compared to that required when a contrast agent is not used; and, (4) to shield non-target tissue from damage, by blocking the HIFU energy. Various combinations of these techniques can also be employed in a single therapeutic implementation.
Owner:UNIV OF WASHINGTON
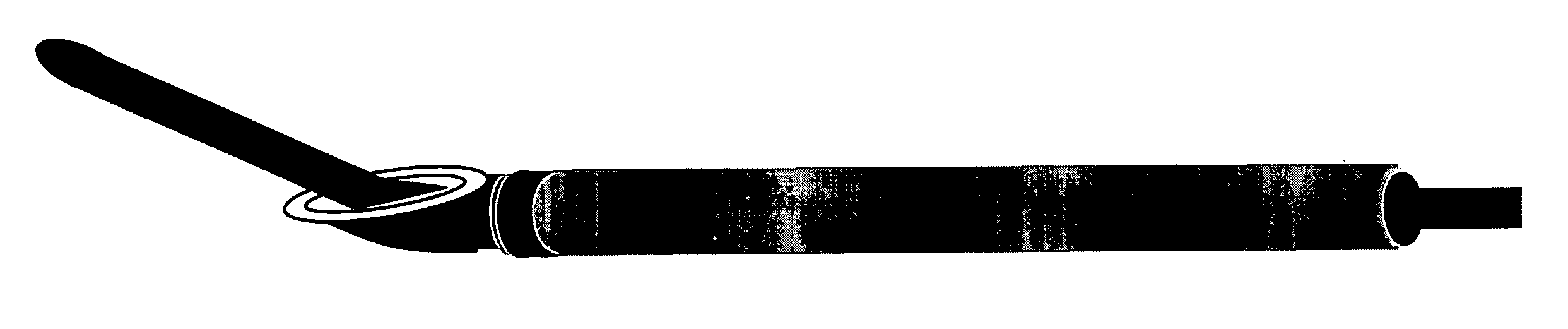
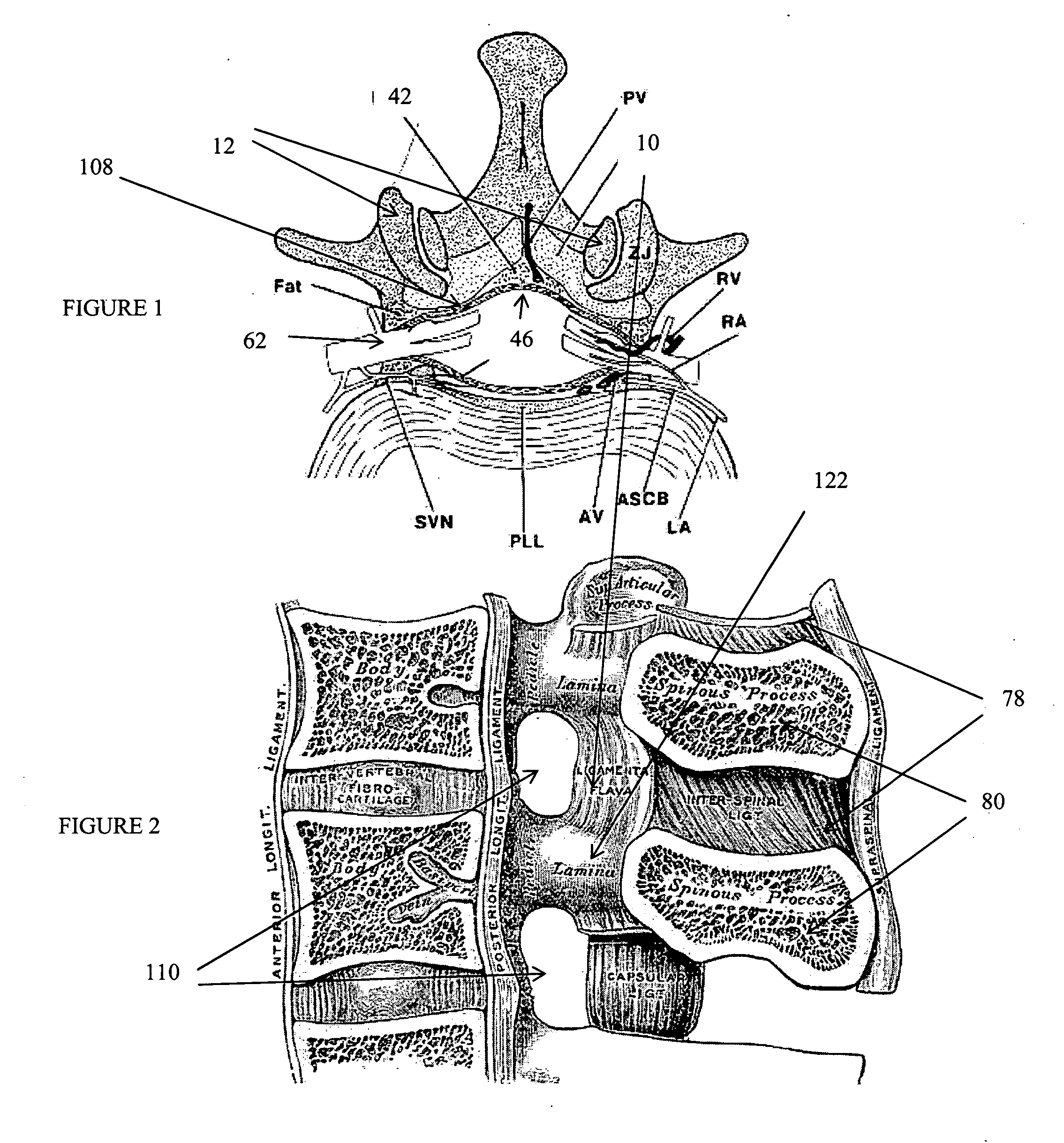
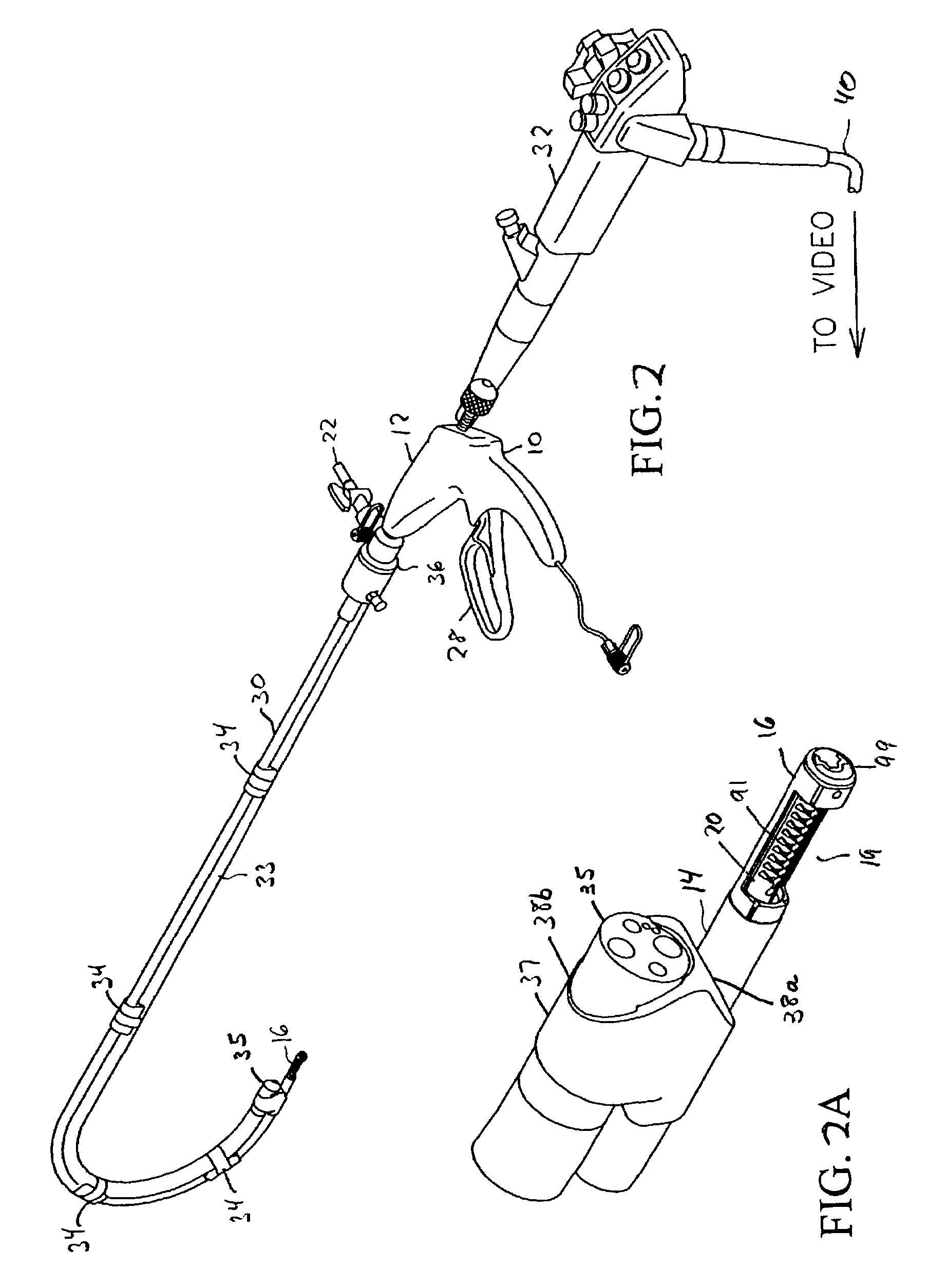
Devices and methods for tissue access
ActiveUS20060089633A1Easy to disassembleEliminate needCannulasAnti-incontinence devicesSurgical departmentNerve stimulation
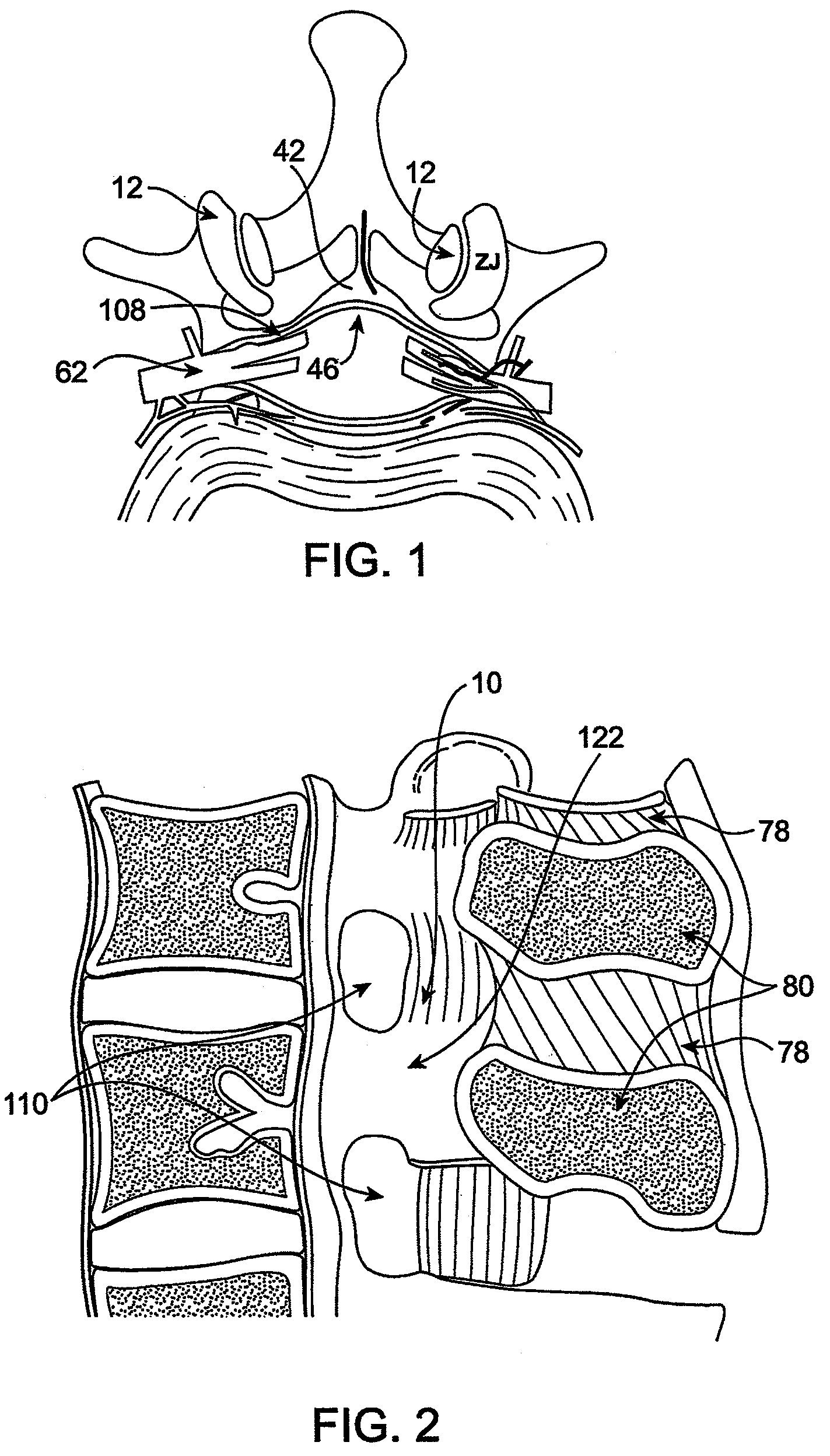
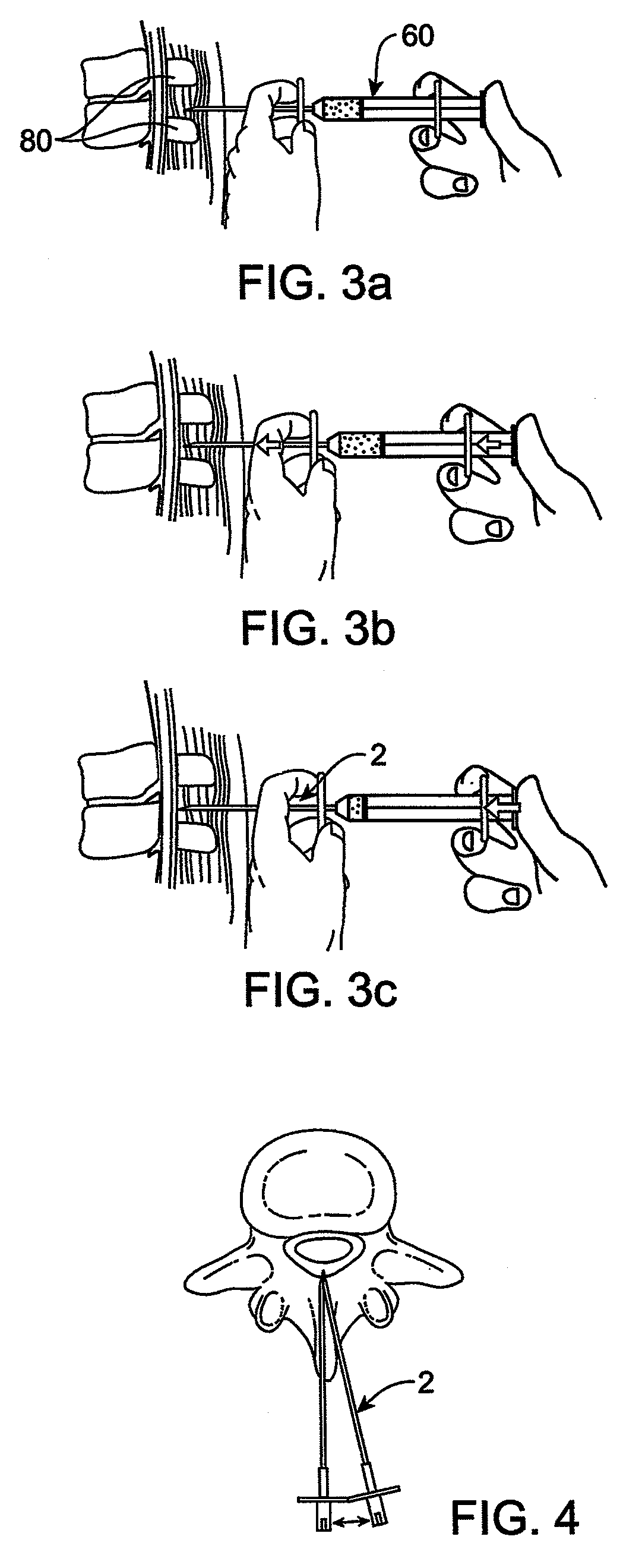
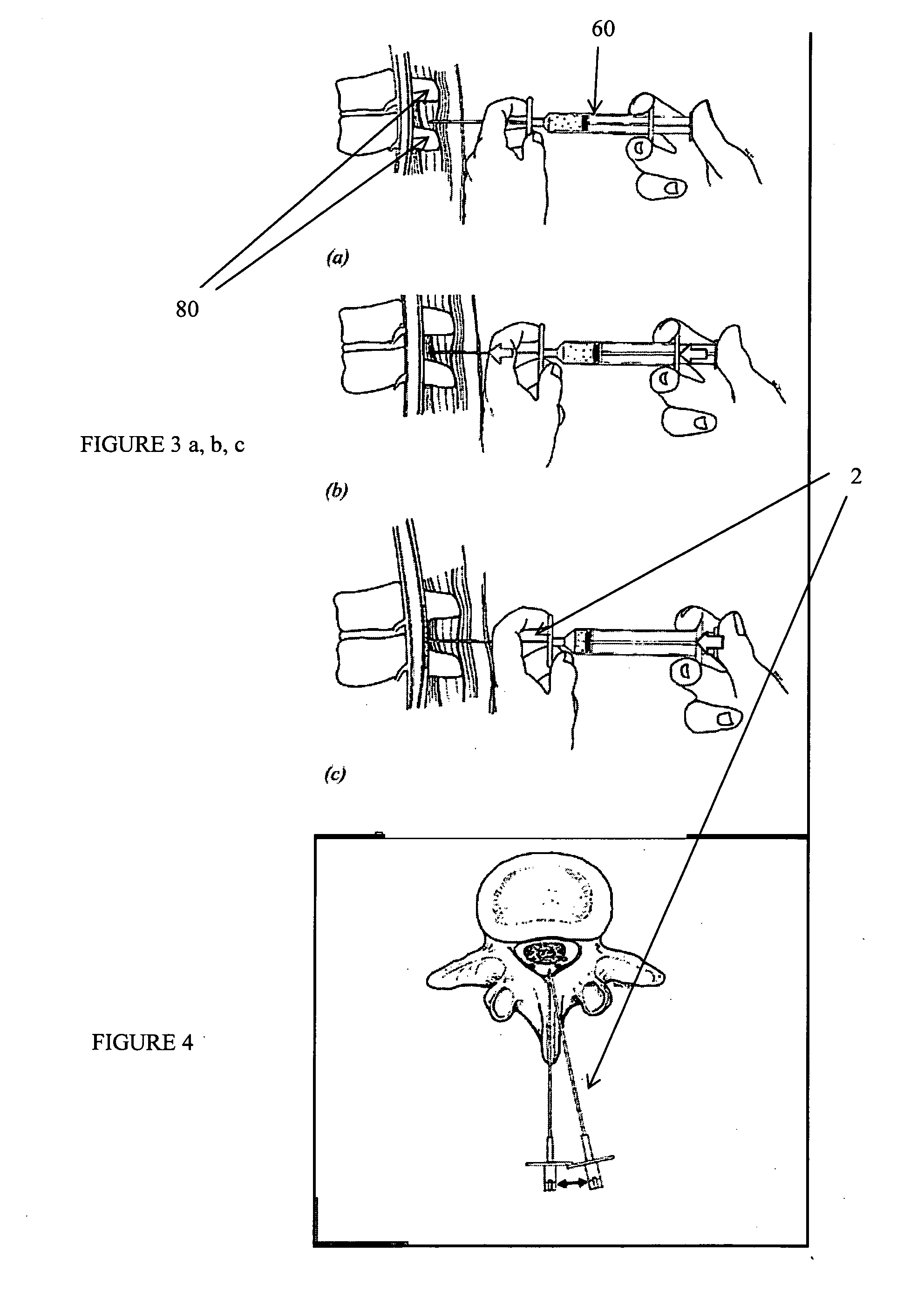
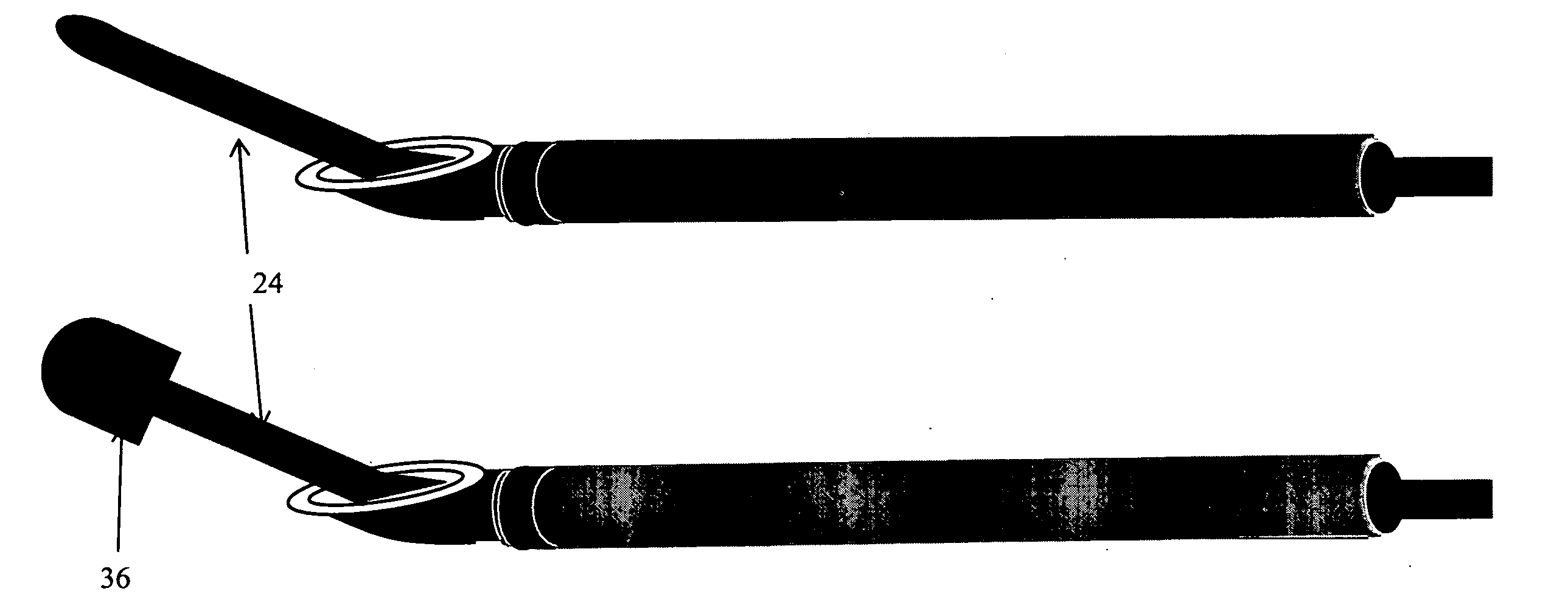
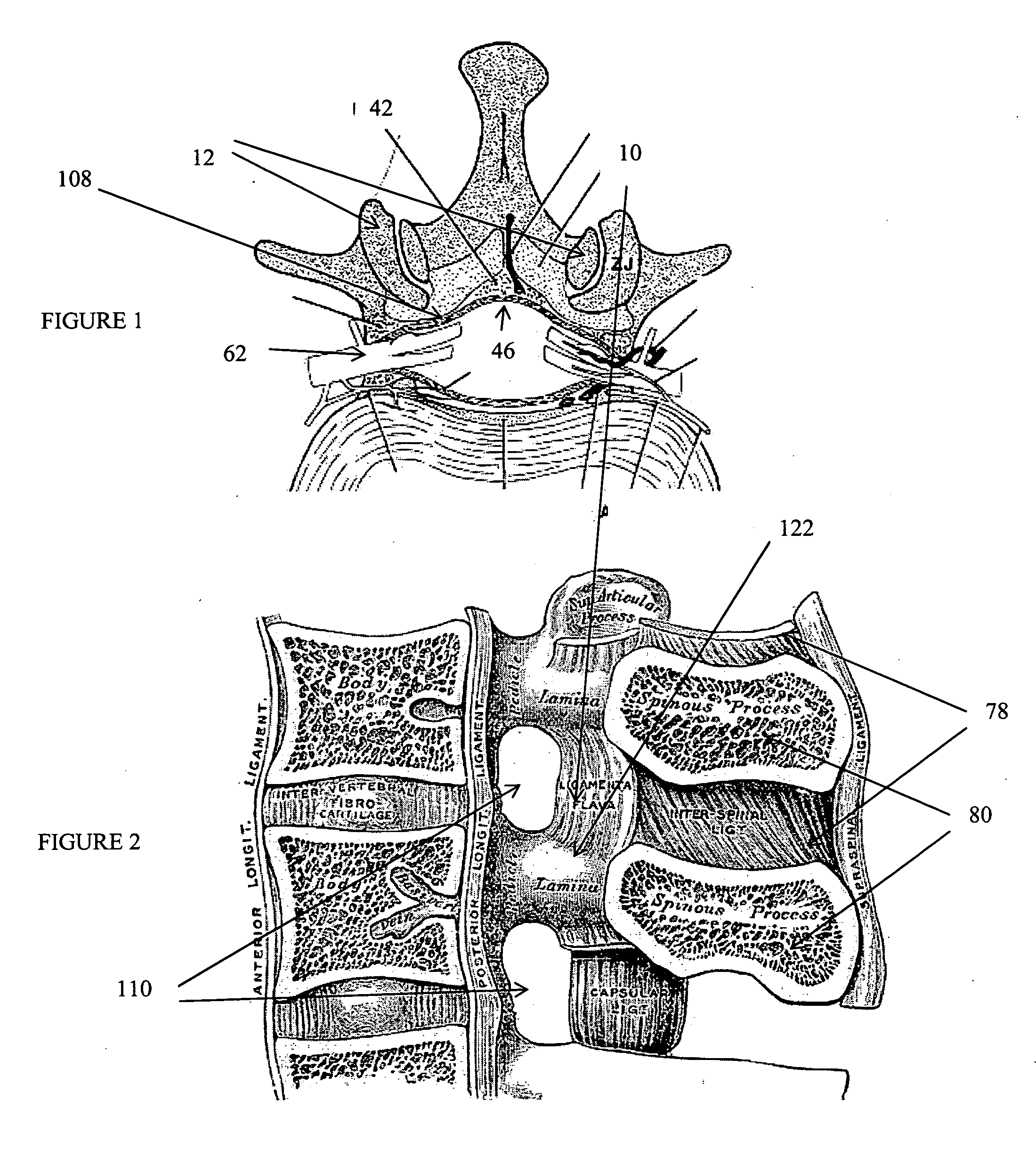
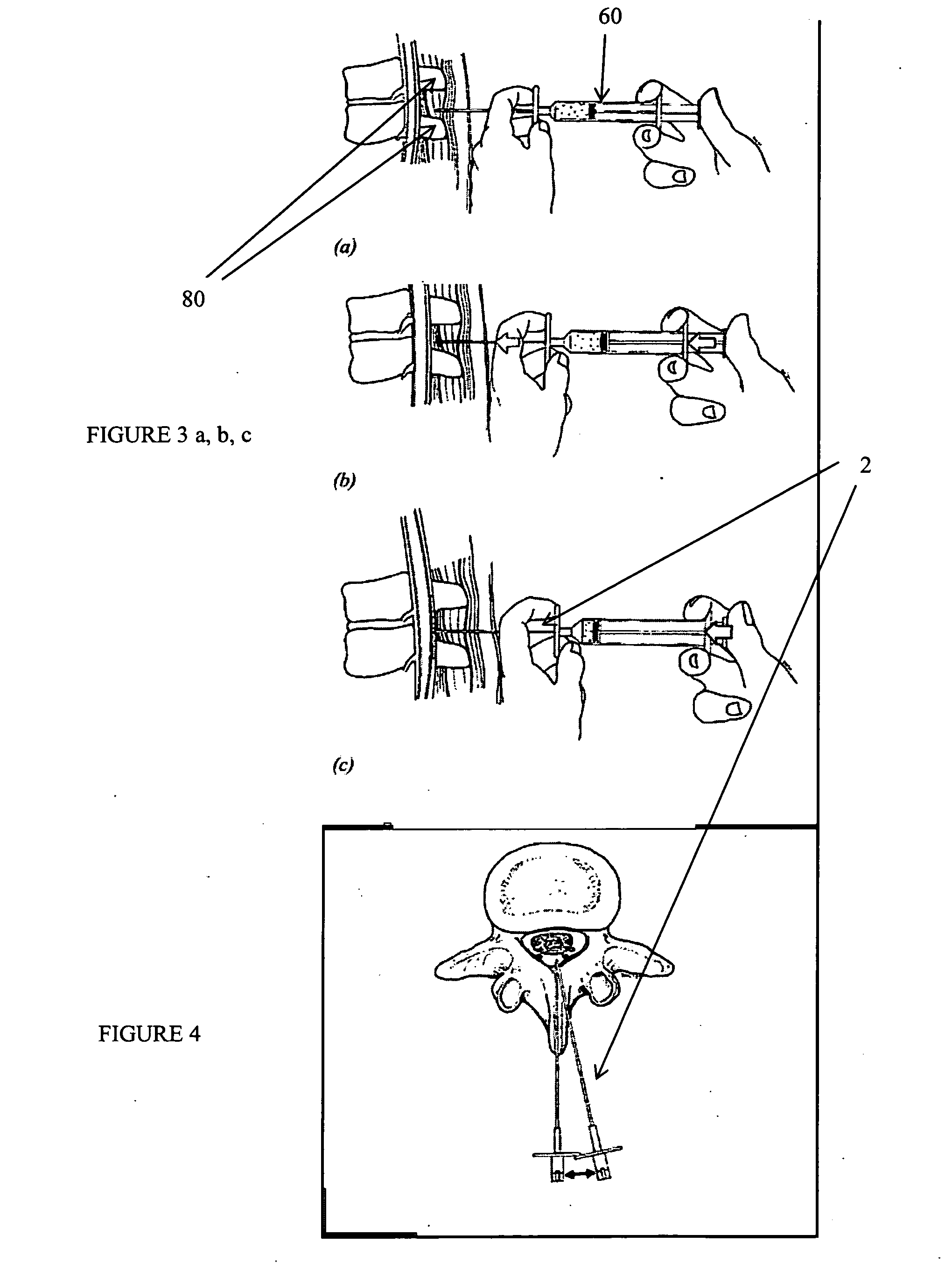
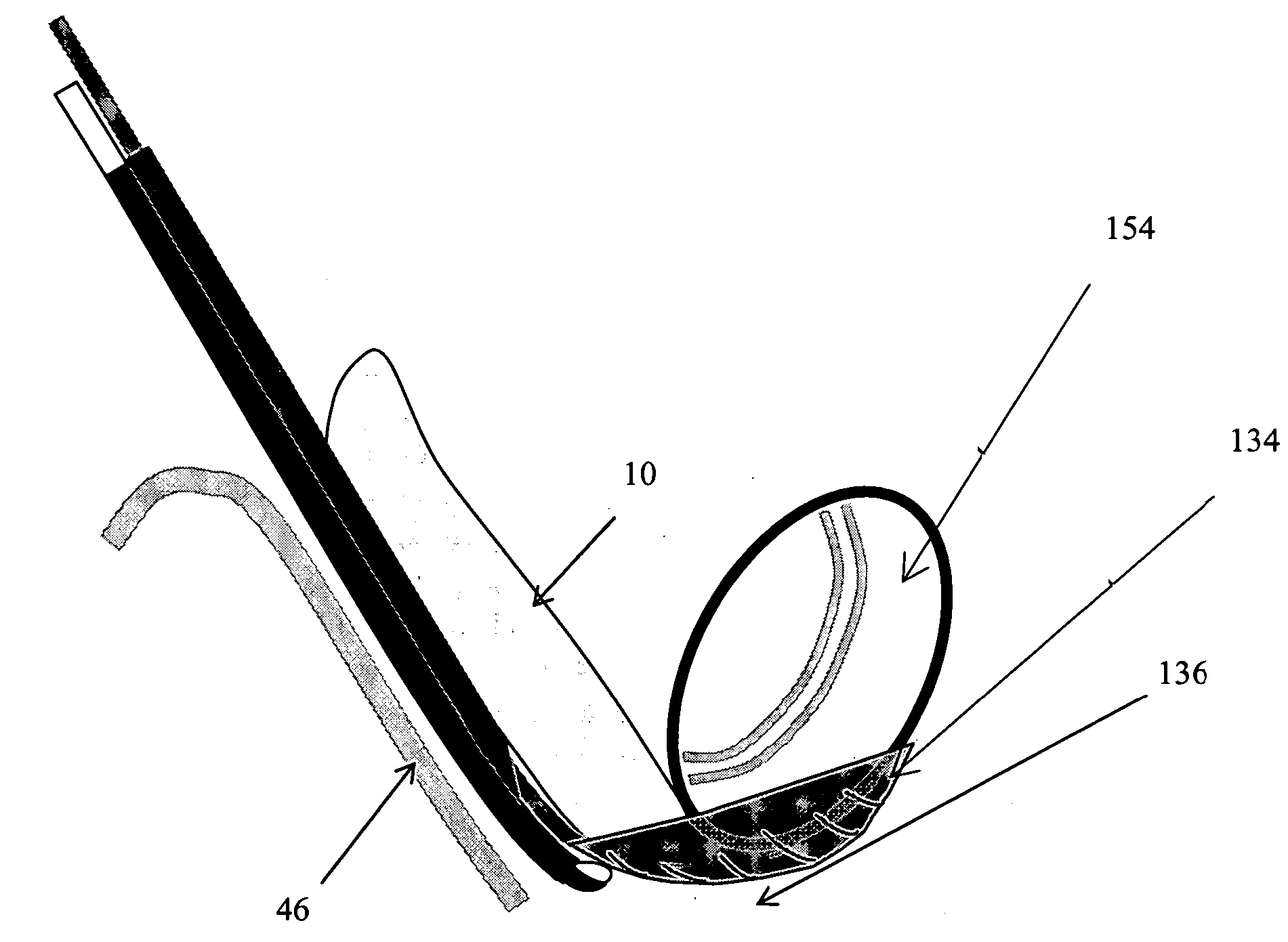
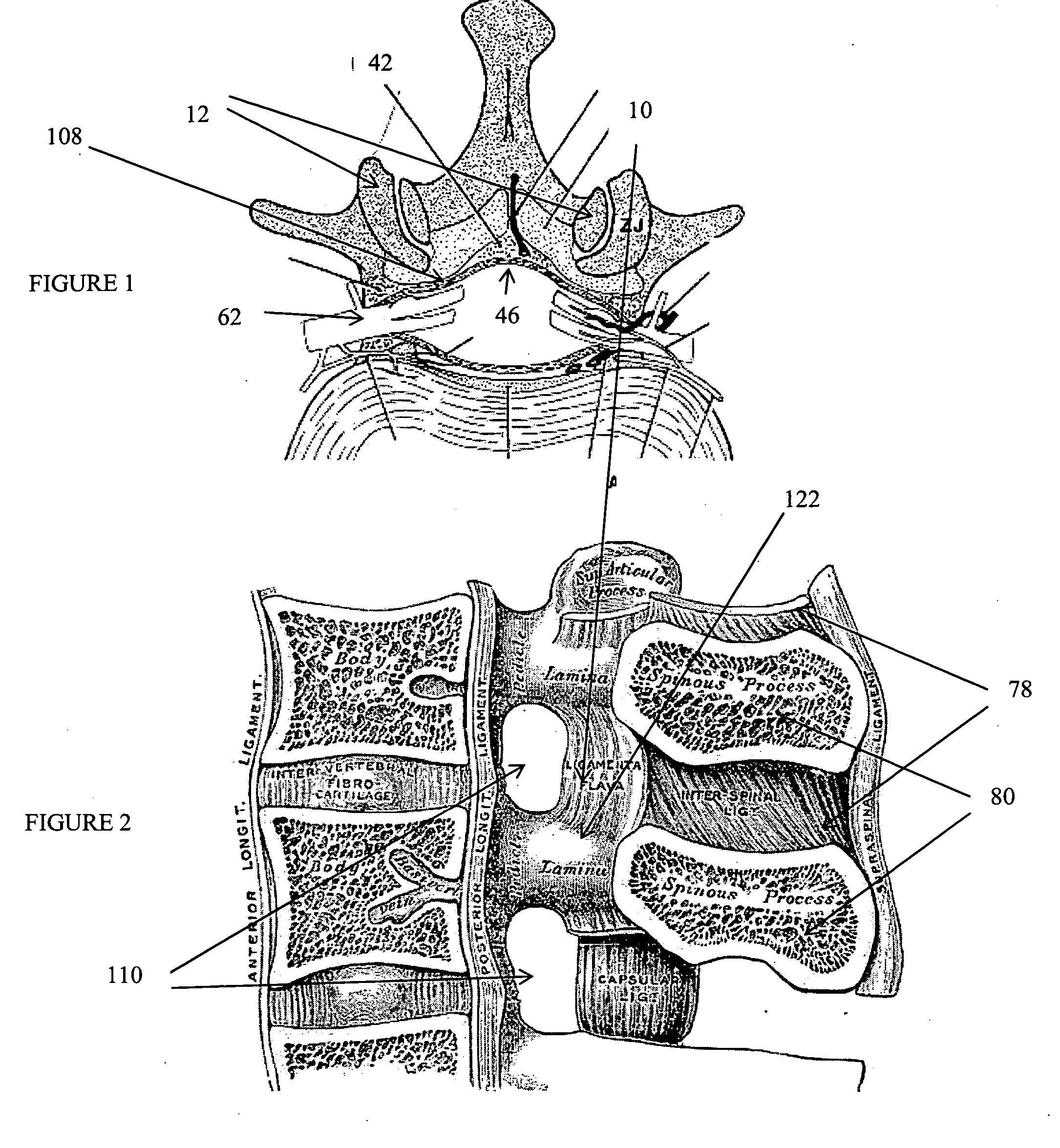
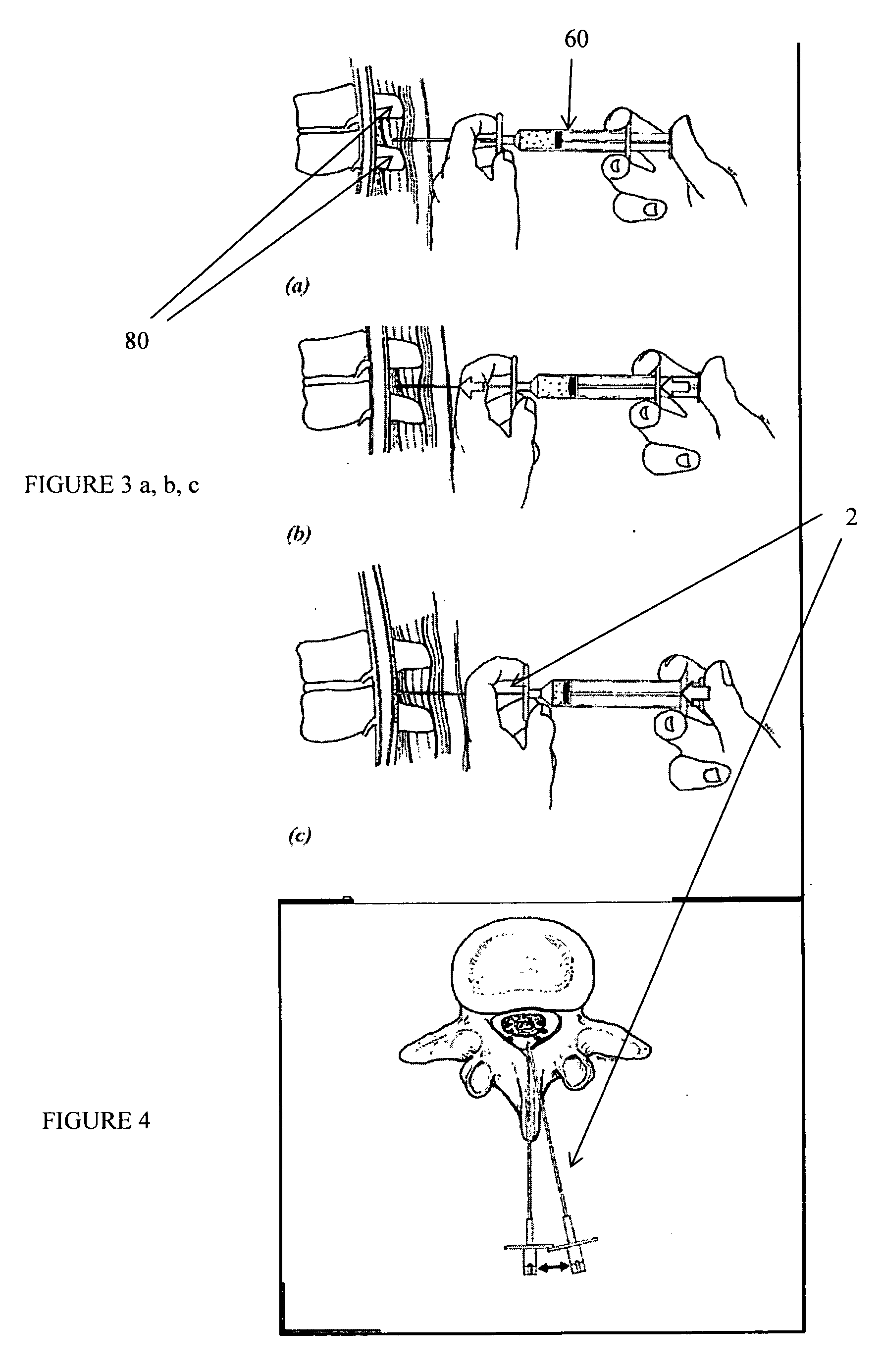
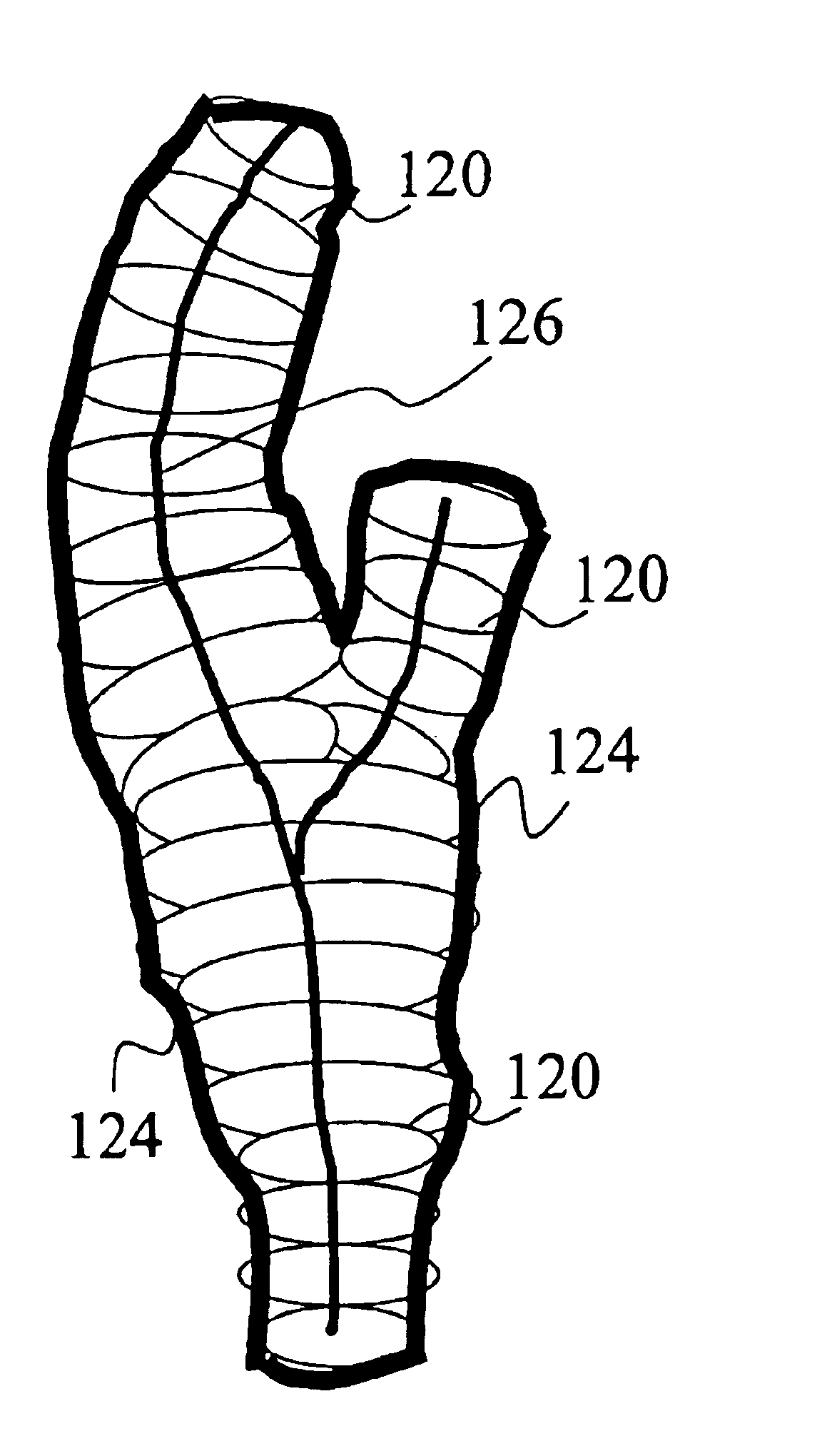
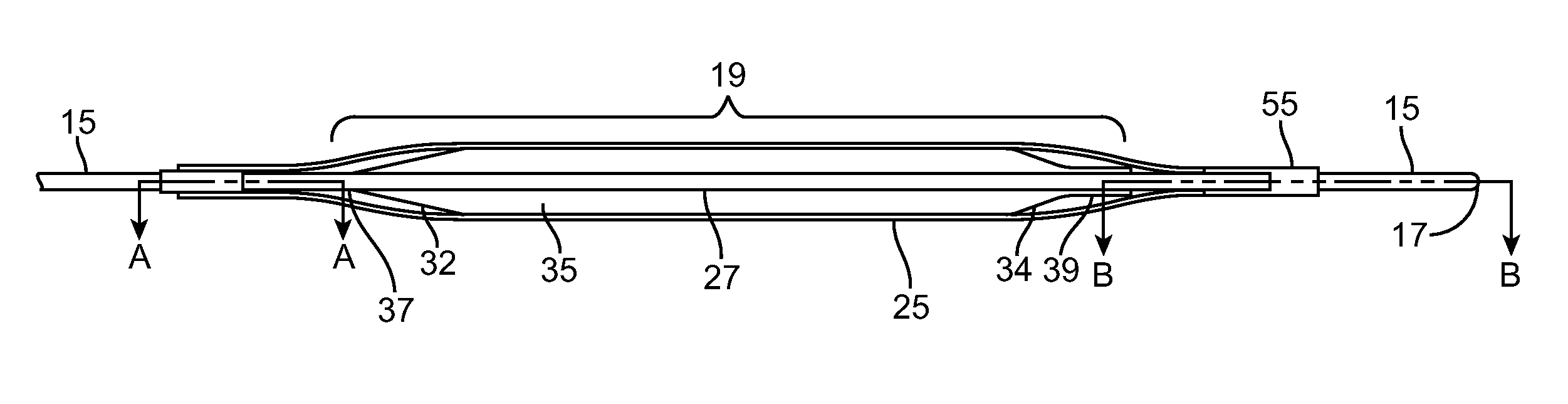
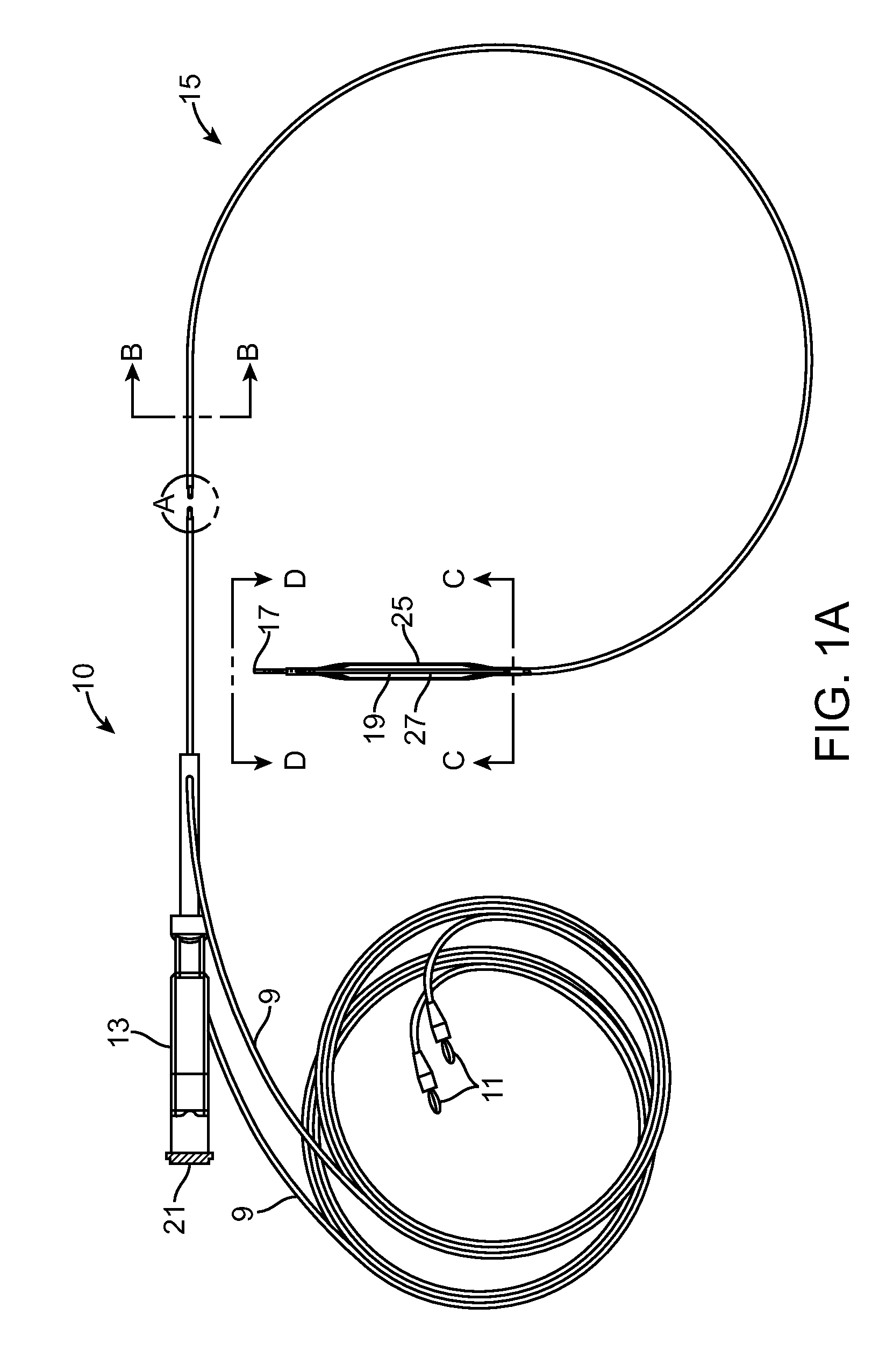
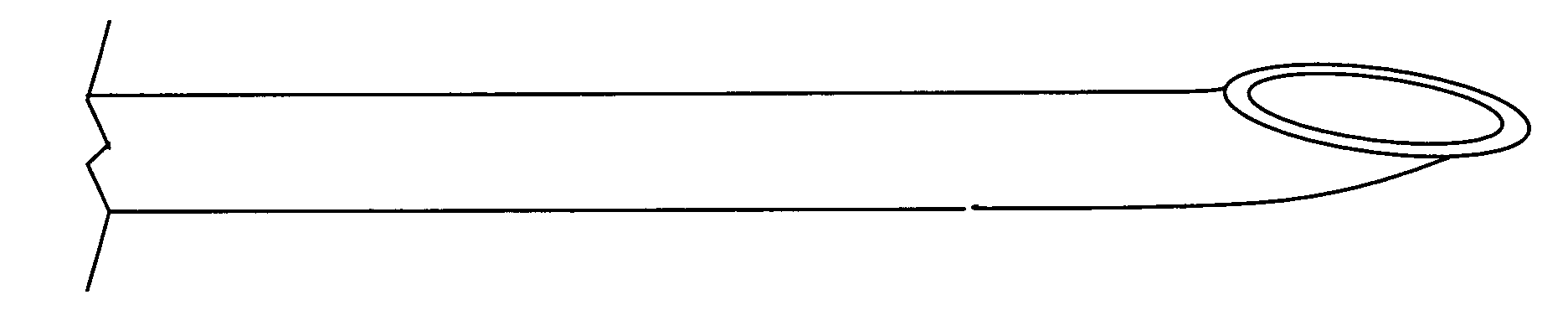
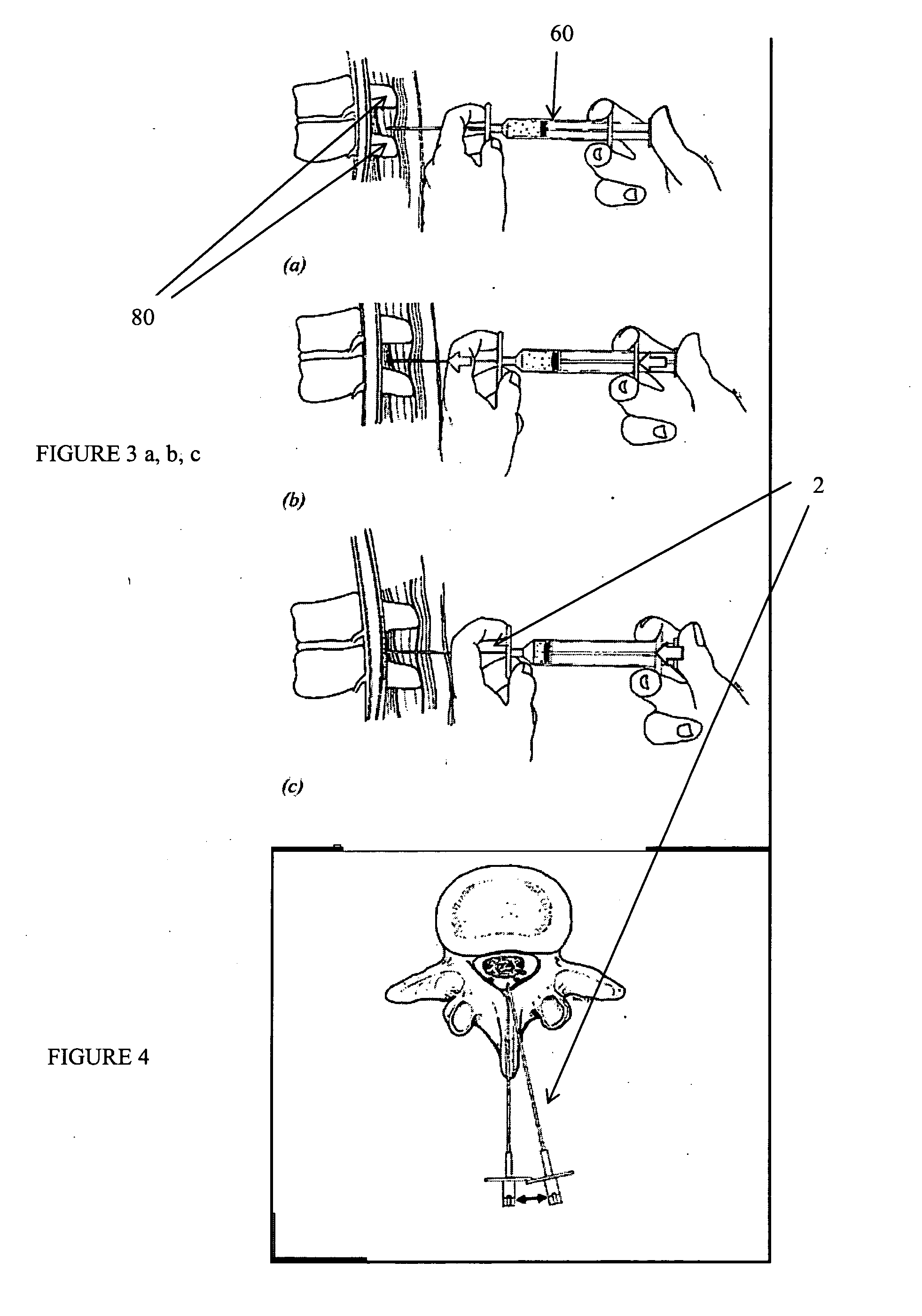
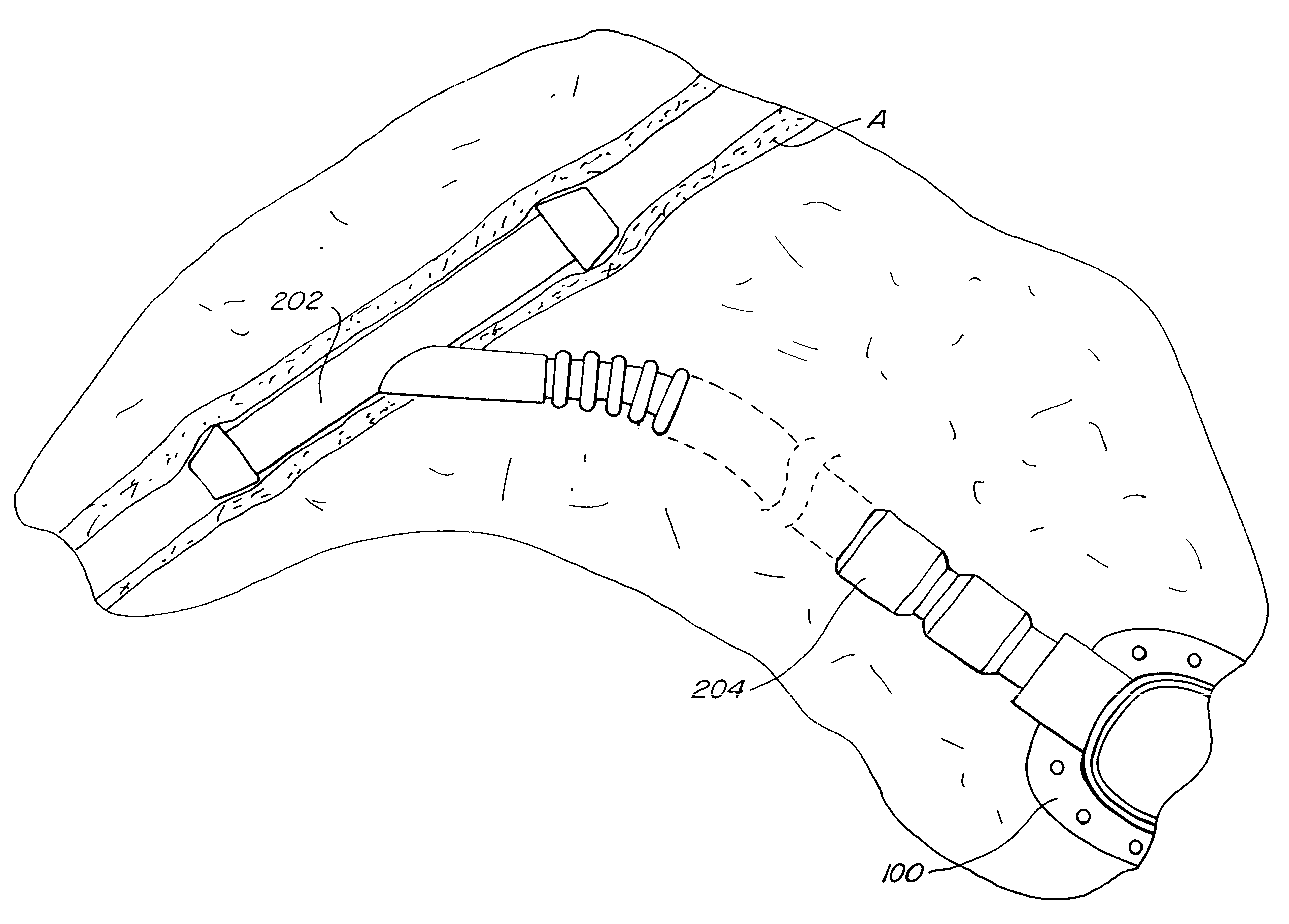
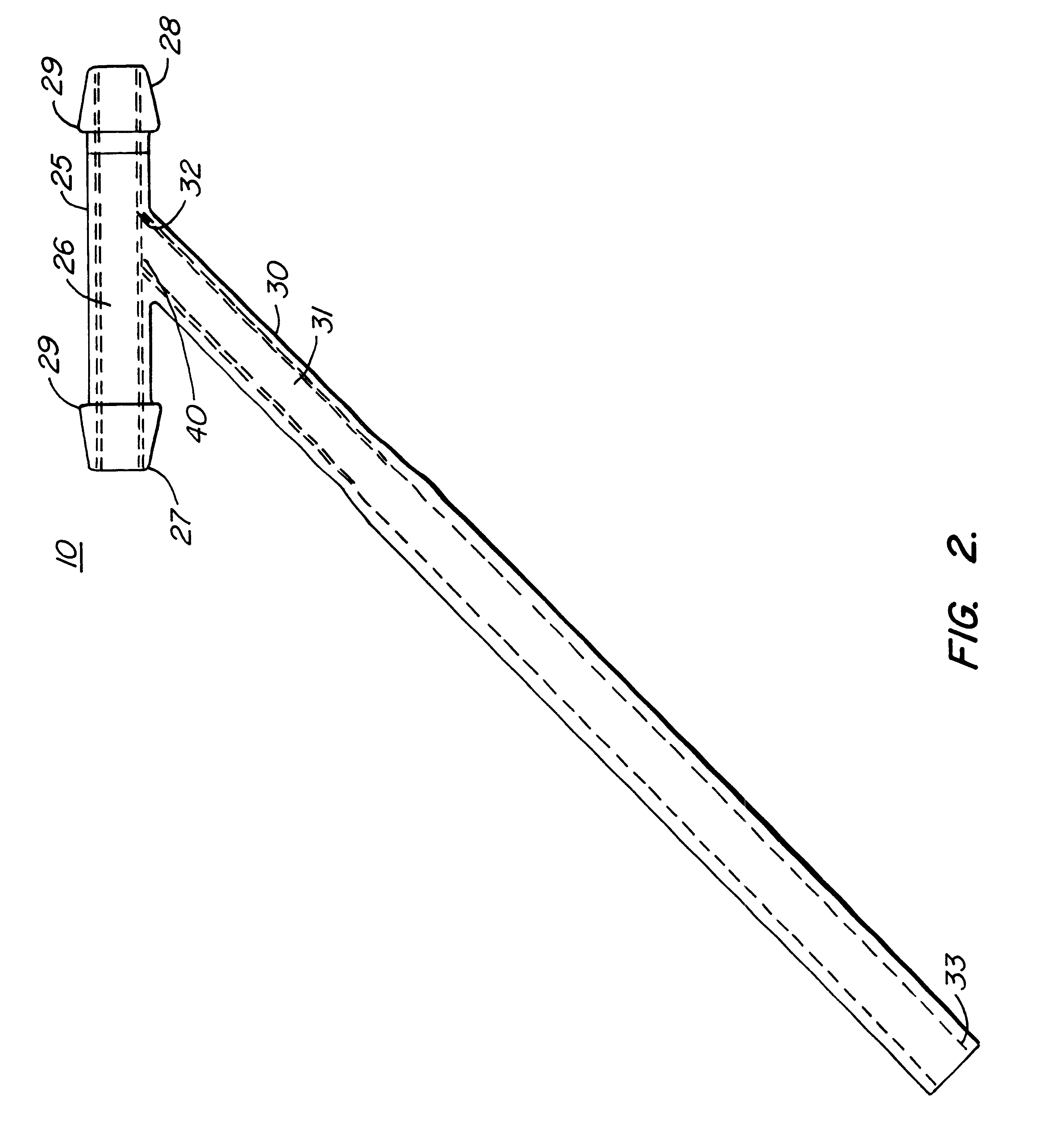
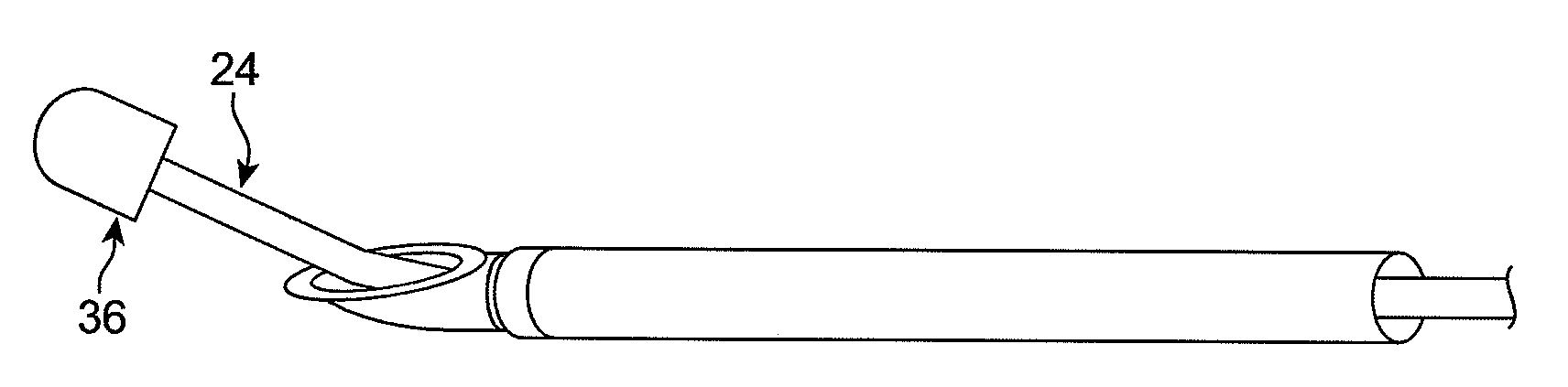
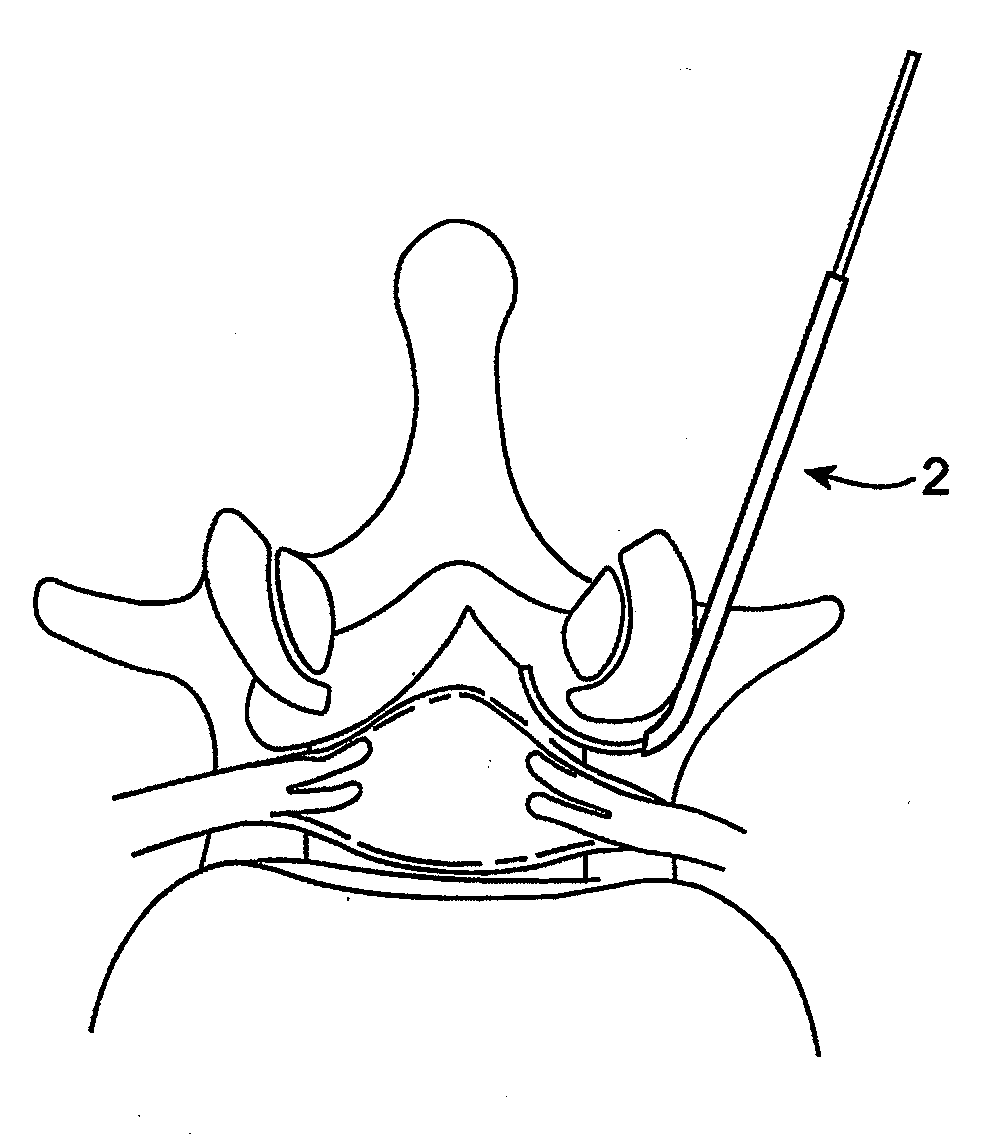
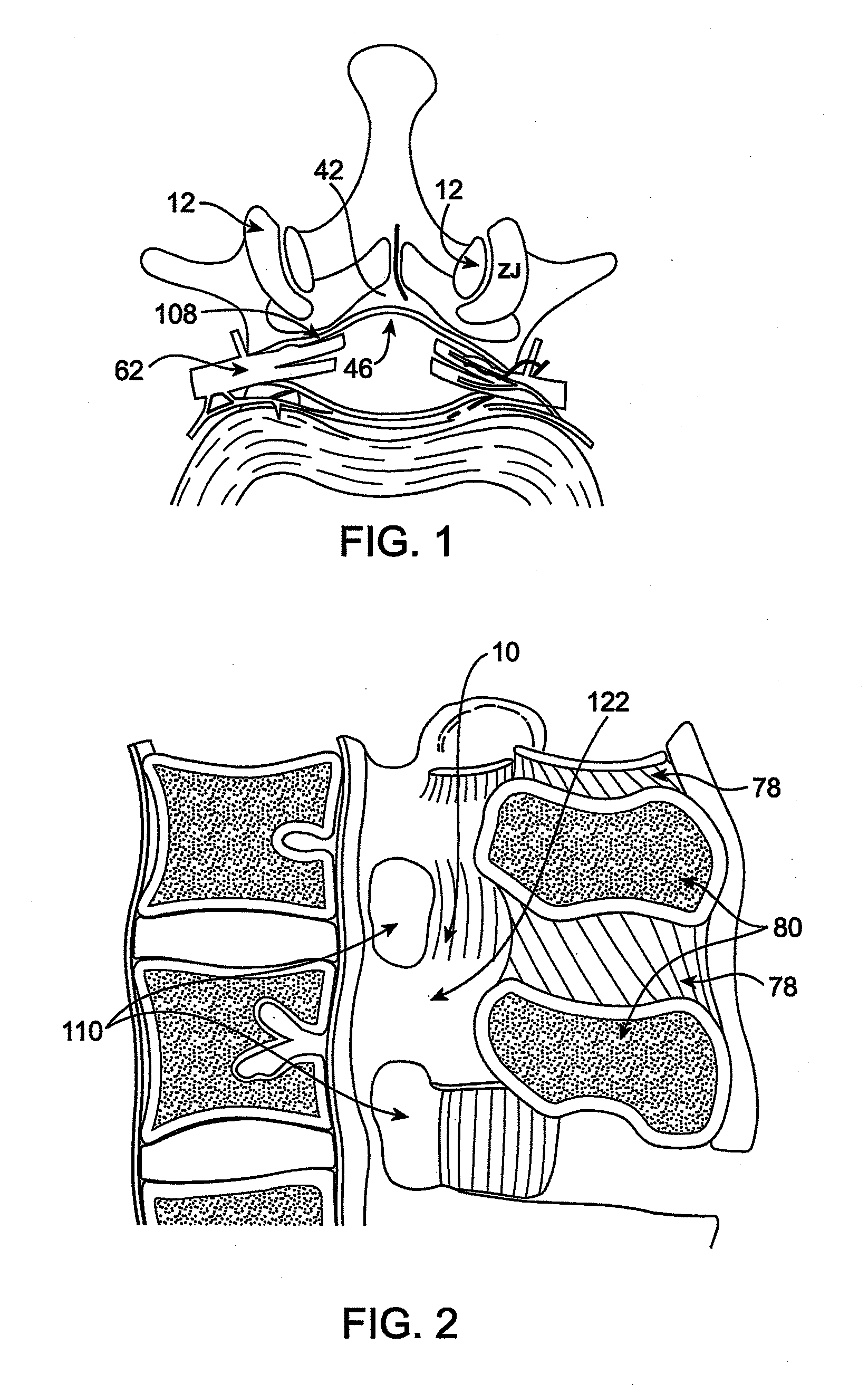
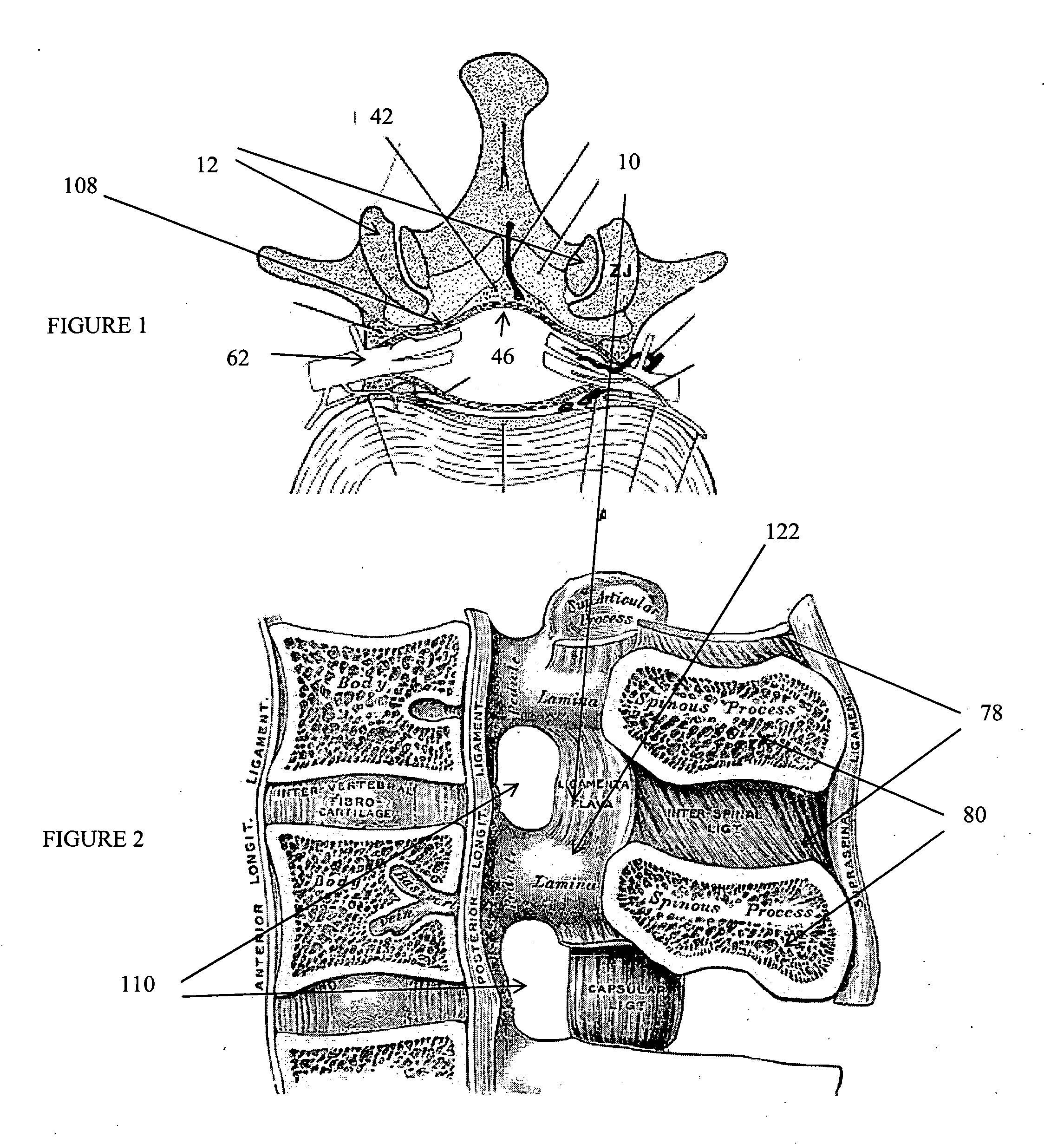
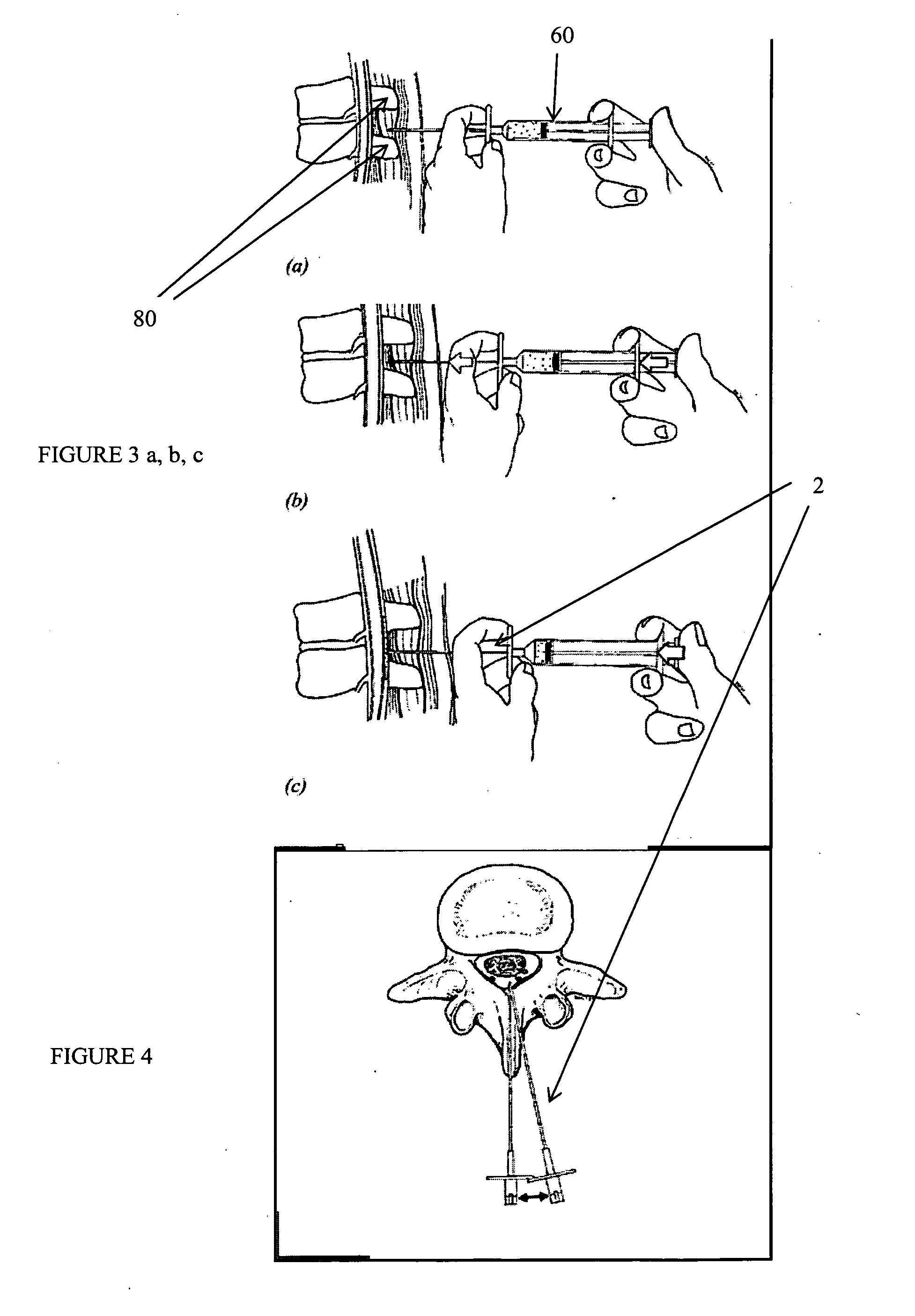
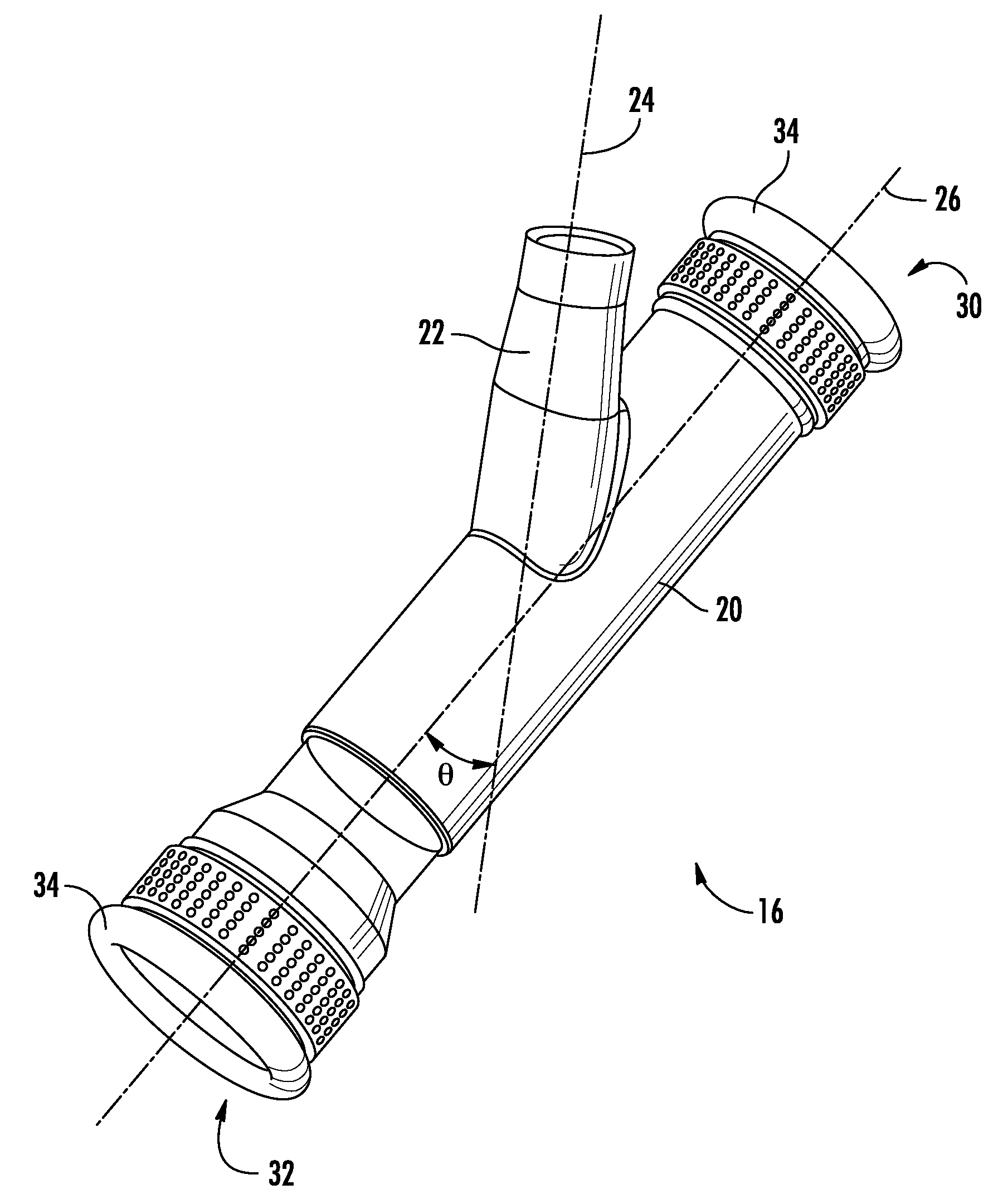
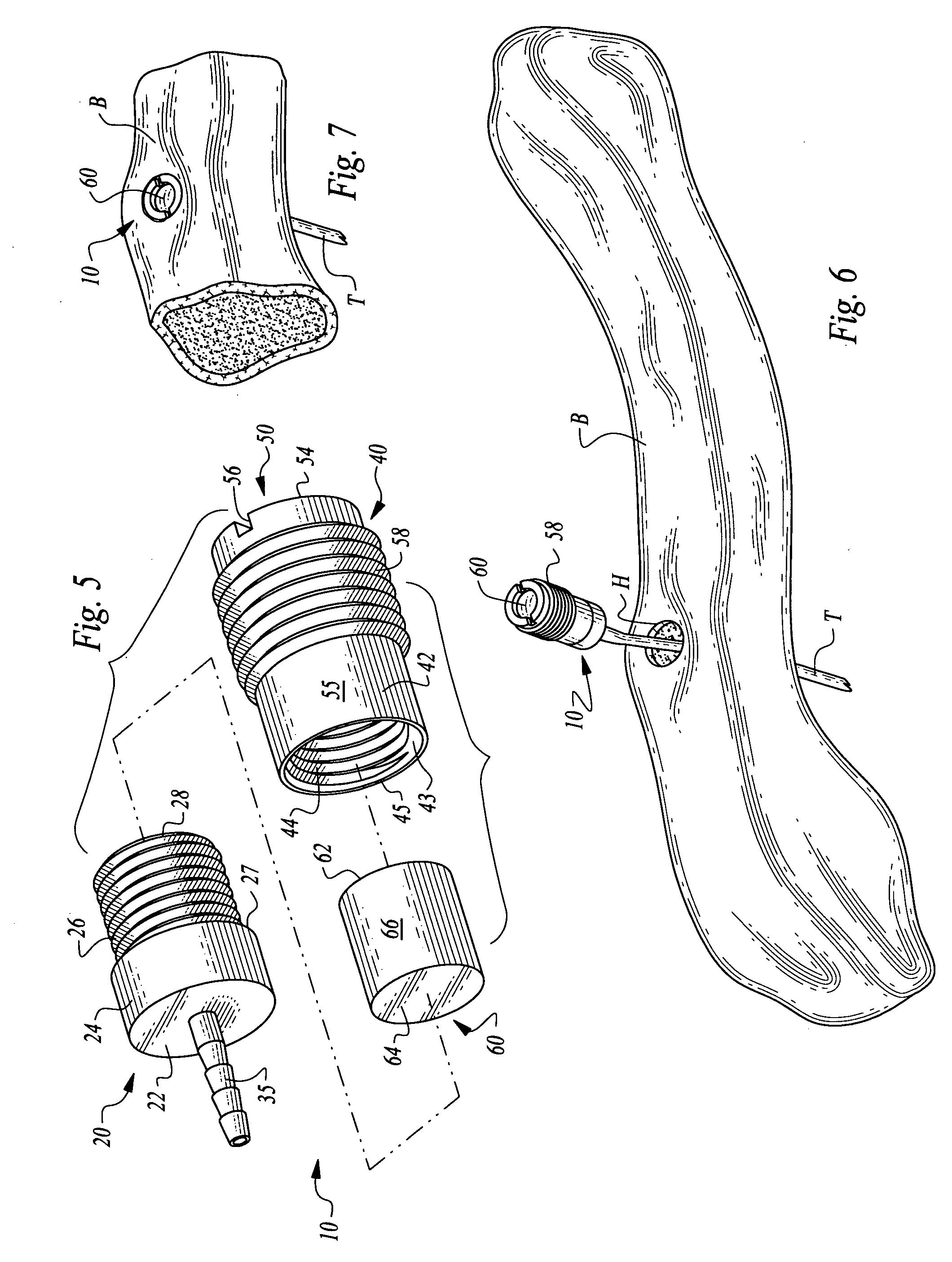
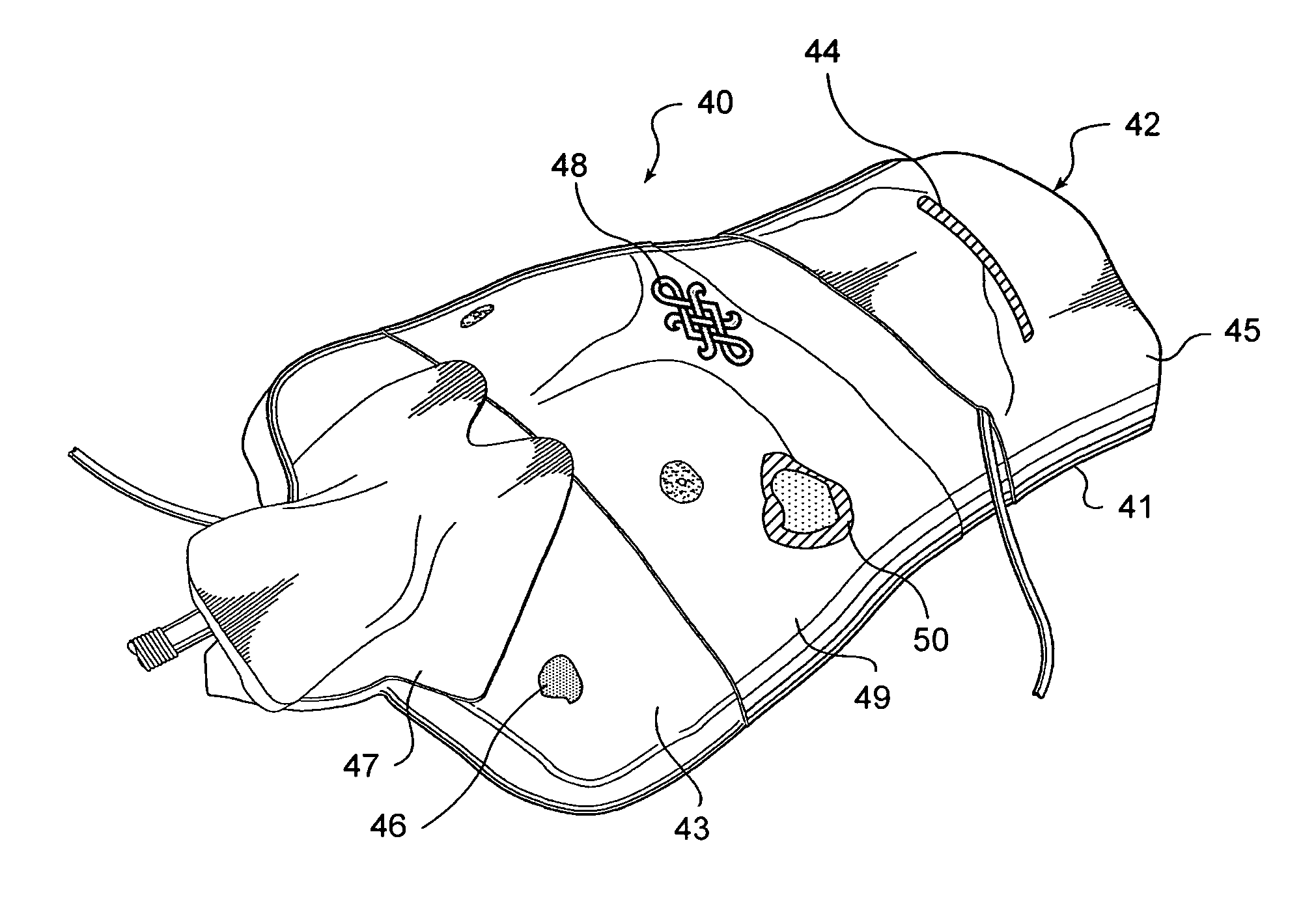
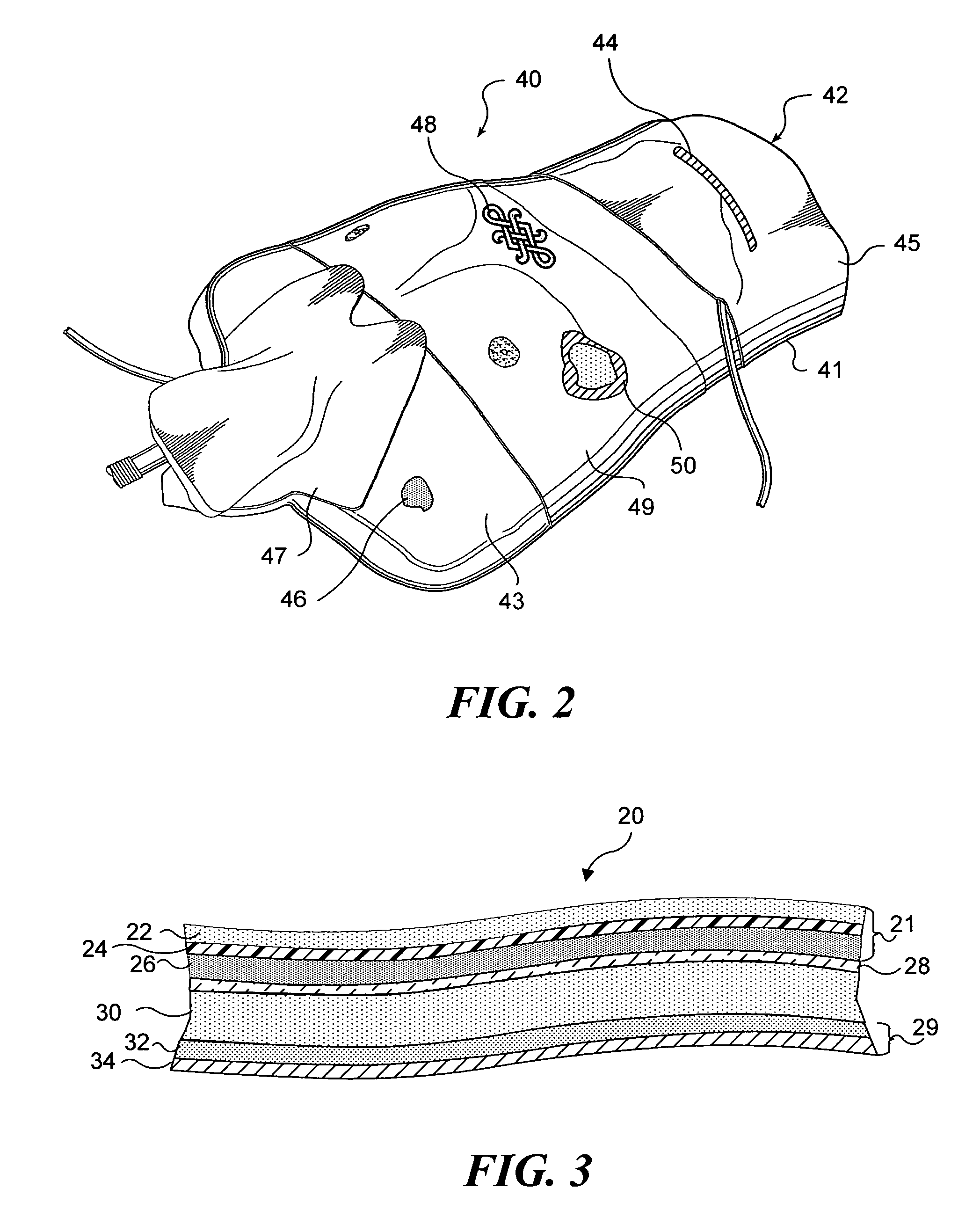
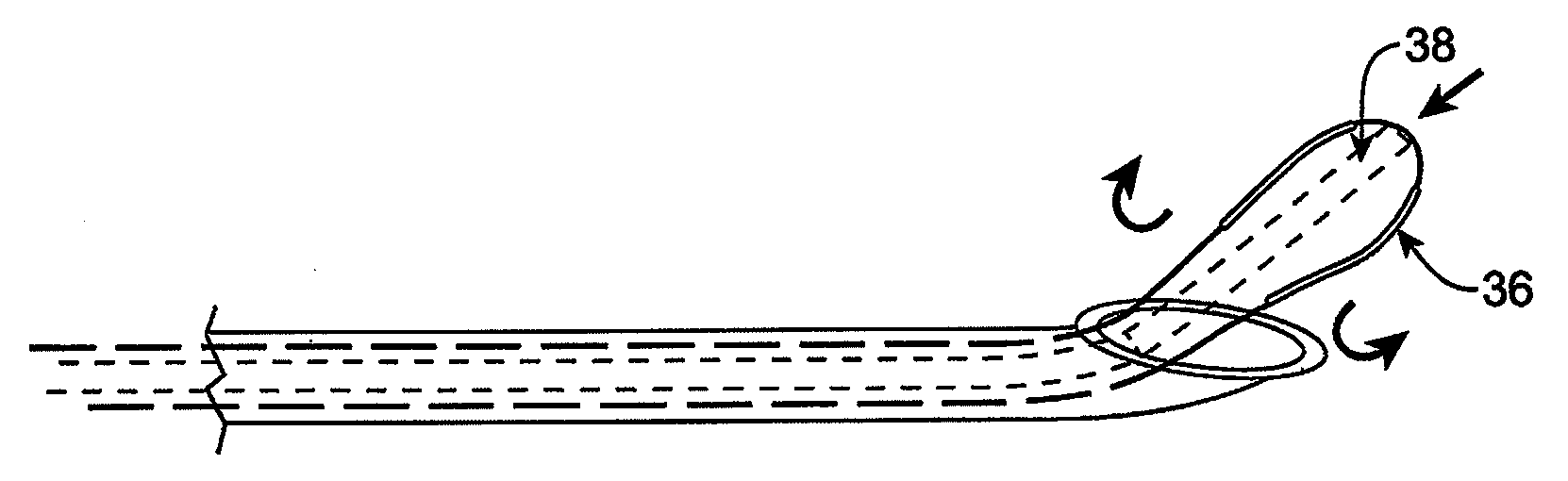
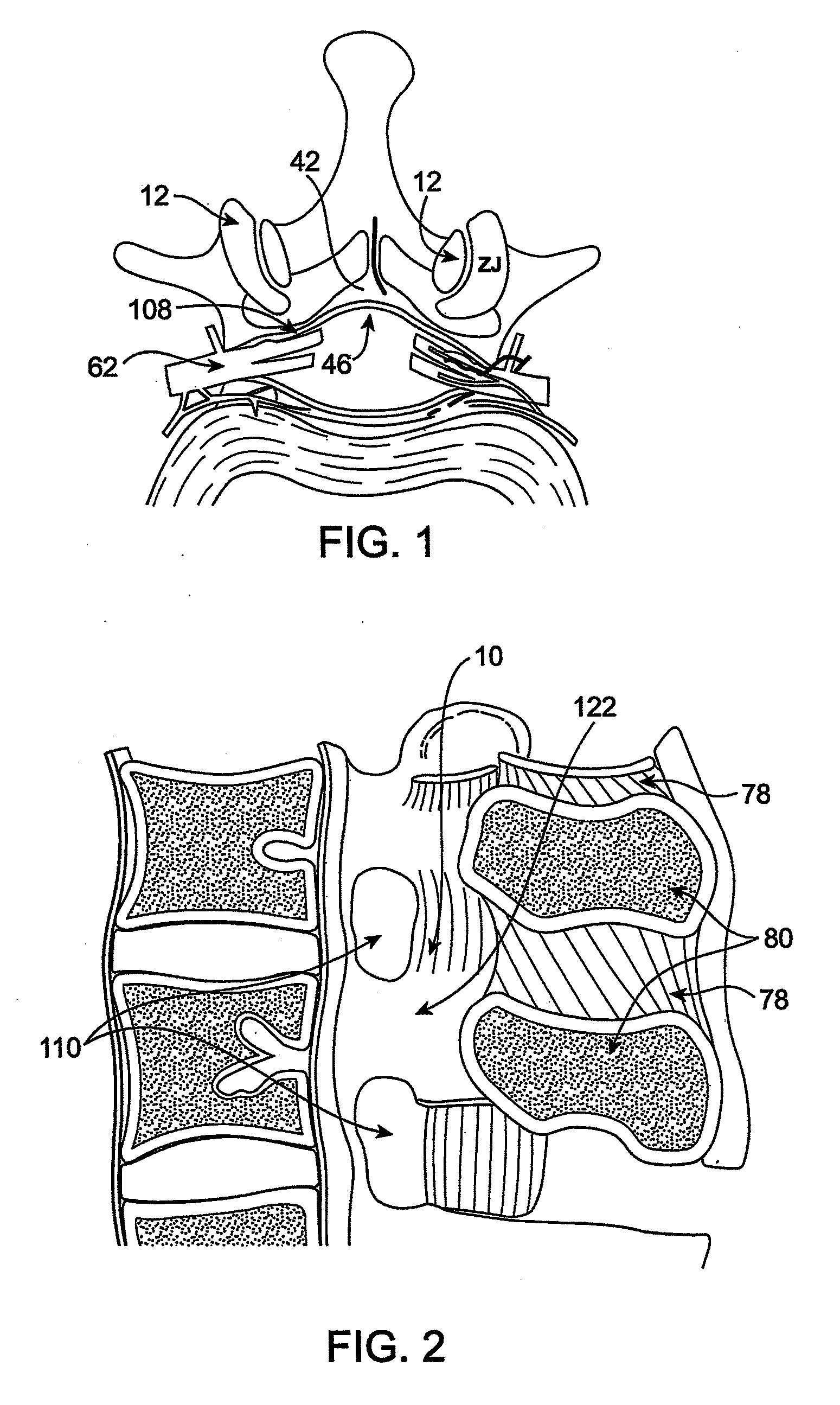
Methods and apparatus are provided for selective surgical removal of tissue, e.g., for enlargement of diseased spinal structures, such as impinged lateral recesses and pathologically narrowed neural foramen. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. Once the sharp tip of the needle is in the epidural space, it is converted to a blunt tipped instrument for further safe advancement. A specially designed epidural catheter that is used to cover the previously sharp needle tip may also contain a fiberoptic cable. Further embodiments of the current invention include a double barreled epidural needle or other means for placement of a working channel for the placement of tools within the epidural space, beside the epidural instrument. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. In one variation, a tissue abrasion device is provided including a thin belt or ribbon with an abrasive cutting surface. The device may be placed through the neural foramina of the spine and around the anterior border of a facet joint. Once properly positioned, a medical practitioner may enlarge the lateral recess and neural foramina via frictional abrasion, i.e., by sliding the abrasive surface of the ribbon across impinging tissues. A nerve stimulator optionally may be provided to reduce a risk of inadvertent neural abrasion. Additionally, safe epidural placement of the working barrier and epidural tissue modification tools may be further improved with the use of electrical nerve stimulation capabilities within the invention that, when combined with neural stimulation monitors, provide neural localization capabilities to the surgeon. The device optionally may be placed within a protective sheath that exposes the abrasive surface of the ribbon only in the area where tissue removal is desired. Furthermore, an endoscope may be incorporated into the device in order to monitor safe tissue removal. Finally, tissue remodeling within the epidural space may be ensured through the placement of compression dressings against remodeled tissue surfaces, or through the placement of tissue retention straps, belts or cables that are wrapped around and pull under tension aspects of the impinging soft tissue and bone in the posterior spinal canal.
Owner:SPINAL ELEMENTS INC +1
Devices and methods for tissue access
InactiveUS20060095028A1Improve securityAvoid injuryEar treatmentCannulasAccess methodSurgical removal
Methods and apparatus are provided for selective surgical removal of tissue. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. The sharp tip of the needle in the epidural space, can be converted to a blunt tipped instrument for further safe advancement. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. A nerve stimulator may be provided to reduce a risk of inadvertent neural abrasion.
Owner:BAXANO
Devices and methods for tissue access
InactiveUS20060122458A1Enabling symptomatic reliefApproach can be quite invasiveCannulasDiagnosticsSurgical departmentNerve stimulation
Methods and apparatus are provided for selective surgical removal of tissue, e.g., for enlargement of diseased spinal structures, such as impinged lateral recesses and pathologically narrowed neural foramen. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. Once the sharp tip of the needle is in the epidural space, it is converted to a blunt tipped instrument for further safe advancement. A specially designed epidural catheter that is used to cover the previously sharp needle tip may also contain a fiberoptic cable. Further embodiments of the current invention include a double barreled epidural needle or other means for placement of a working channel for the placement of tools within the epidural space, beside the epidural instrument. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. In one variation, a tissue removal device is provided including a thin belt or ribbon with an abrasive cutting surface. The device may be placed through the neural foramina of the spine and around the anterior border of a facet joint. Once properly positioned, a medical practitioner may enlarge the lateral recess and neural foramina via frictional abrasion, i.e., by sliding the tissue removal surface of the ribbon across impinging tissues. A nerve stimulator optionally may be provided to reduce a risk of inadvertent neural abrasion. Additionally, safe epidural placement of the working barrier and epidural tissue modification tools may be further improved with the use of electrical nerve stimulation capabilities within the invention that, when combined with neural stimulation monitors, provide neural localization capabilities to the surgeon. The device optionally may be placed within a protective sheath that exposes the abrasive surface of the ribbon only in the area where tissue removal is desired. Furthermore, an endoscope may be incorporated into the device in order to monitor safe tissue removal. Finally, tissue remodeling within the epidural space may be ensured through the placement of compression dressings against remodeled tissue surfaces, or through the placement of tissue retention straps, belts or cables that are wrapped around and pull under tension aspects of the impinging soft tissue and bone in the posterior spinal canal.
Owner:BAXANO
Angiography method and apparatus
InactiveUS6842638B1Overcome failureRapid and accurate vessel boundary estimationImage enhancementImage analysisEngineeringVascular structure
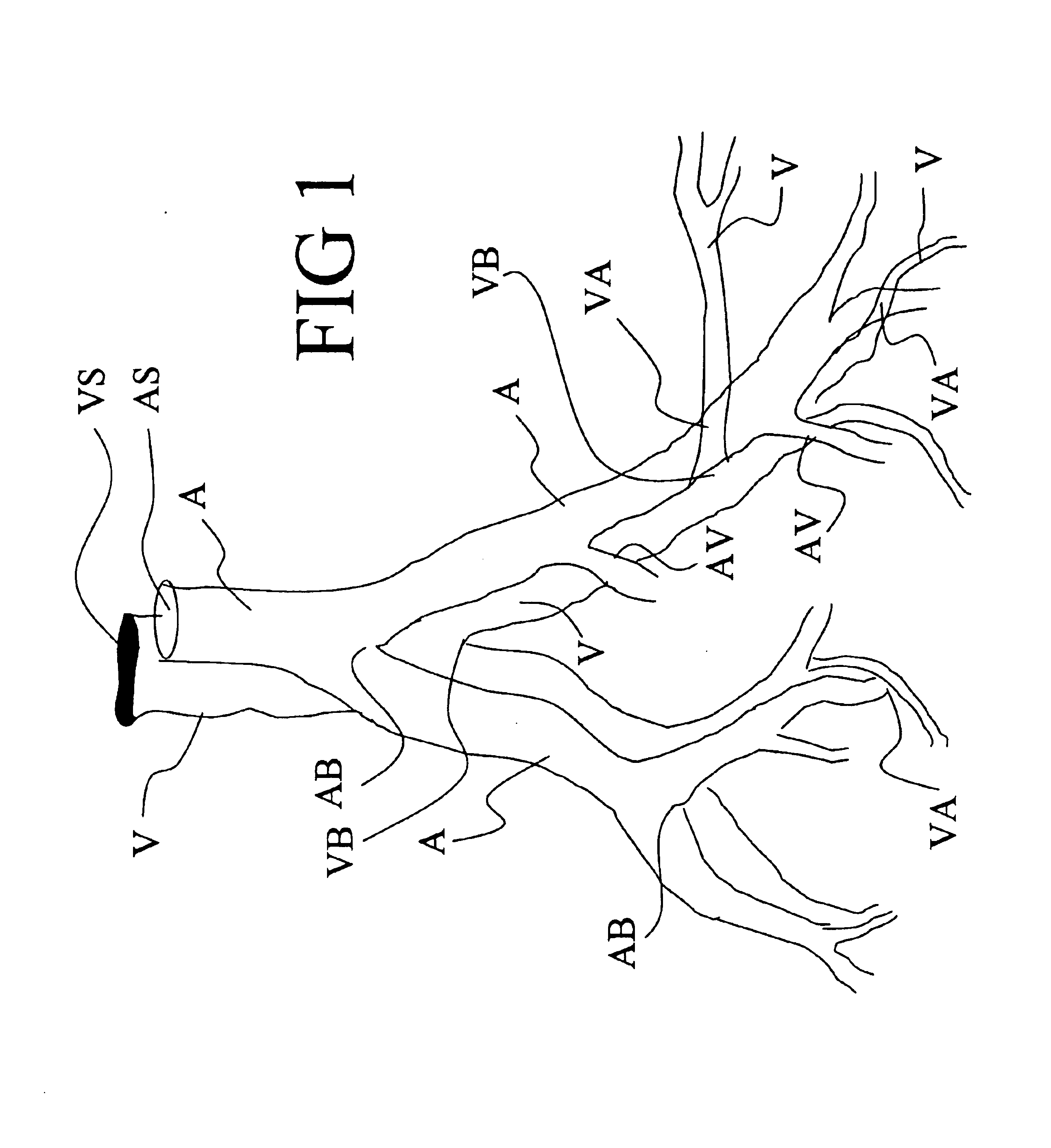
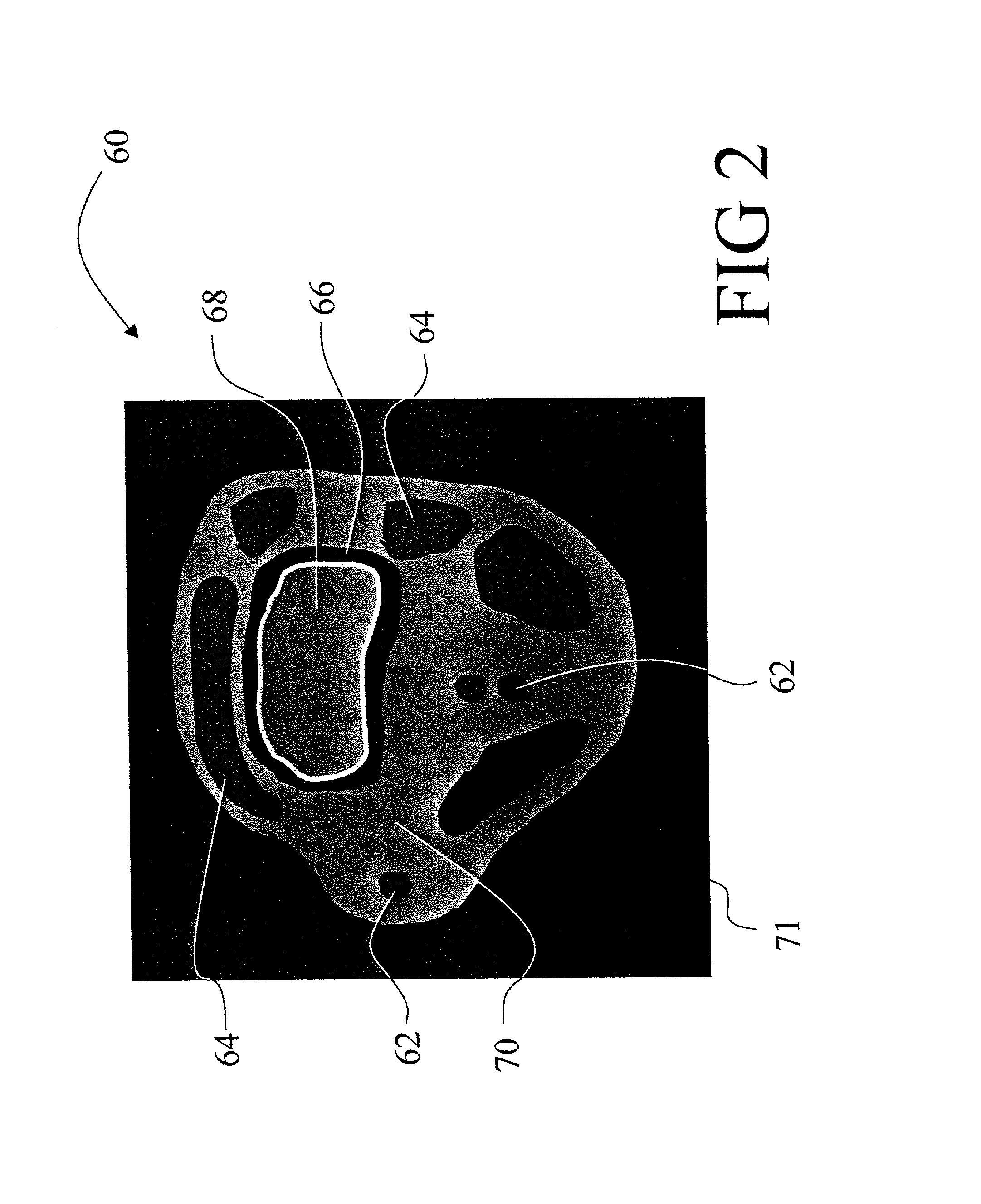
A two-dimensional slice formed of pixels (376) is extracted from the angiographic image (76) after enhancing the vessel edges by second order spatial differentiation (78). Imaged vascular structures in the slice are located (388) and flood-filled (384). The edges of the filled regions are iteratively eroded to identify vessel centers (402). The extracting, locating, flood-filling, and eroding is repeated (408) for a plurality of slices to generate a plurality of vessel centers (84) that are representative of the vascular system. A vessel center (88) is selected, and a corresponding vessel direction (92) and orthogonal plane (94) are found. The vessel boundaries (710) in the orthogonal plane (94) are identified by iteratively propagating (704) a closed geometric contour arranged about the vessel center (88). The selecting, finding, and estimating are repeated for the plurality of vessel centers (84). The estimated vessel boundaries (710) are interpolated (770) to form a vascular tree (780).
Owner:MARCONI MEDICAL SYST +1
Irreversible electroporation device and method for attenuating neointimal
InactiveUS20090248012A1Promote resultsPrevent excessive cell lysingElectrotherapyInfusion devicesPercent Diameter StenosisTunica intima
Restenosis or neointimal formation may occur following angioplasty or other trauma to an artery such as by-pass surgery. This presents a major clinical problem which narrows the artery. The invention provides a device and a method whereby vascular cells in the area of the artery subjected to the trauma are subjected to irreversible electroporation which is a non-thermal, non-pharmaceutical method of applying electrical pulses to the cells so that substantially all of the cells in the area are ablated while leaving the structure of the vessel in place and substantially unharmed due to the non-thermal nature of the procedure.
Owner:RGT UNIV OF CALIFORNIA
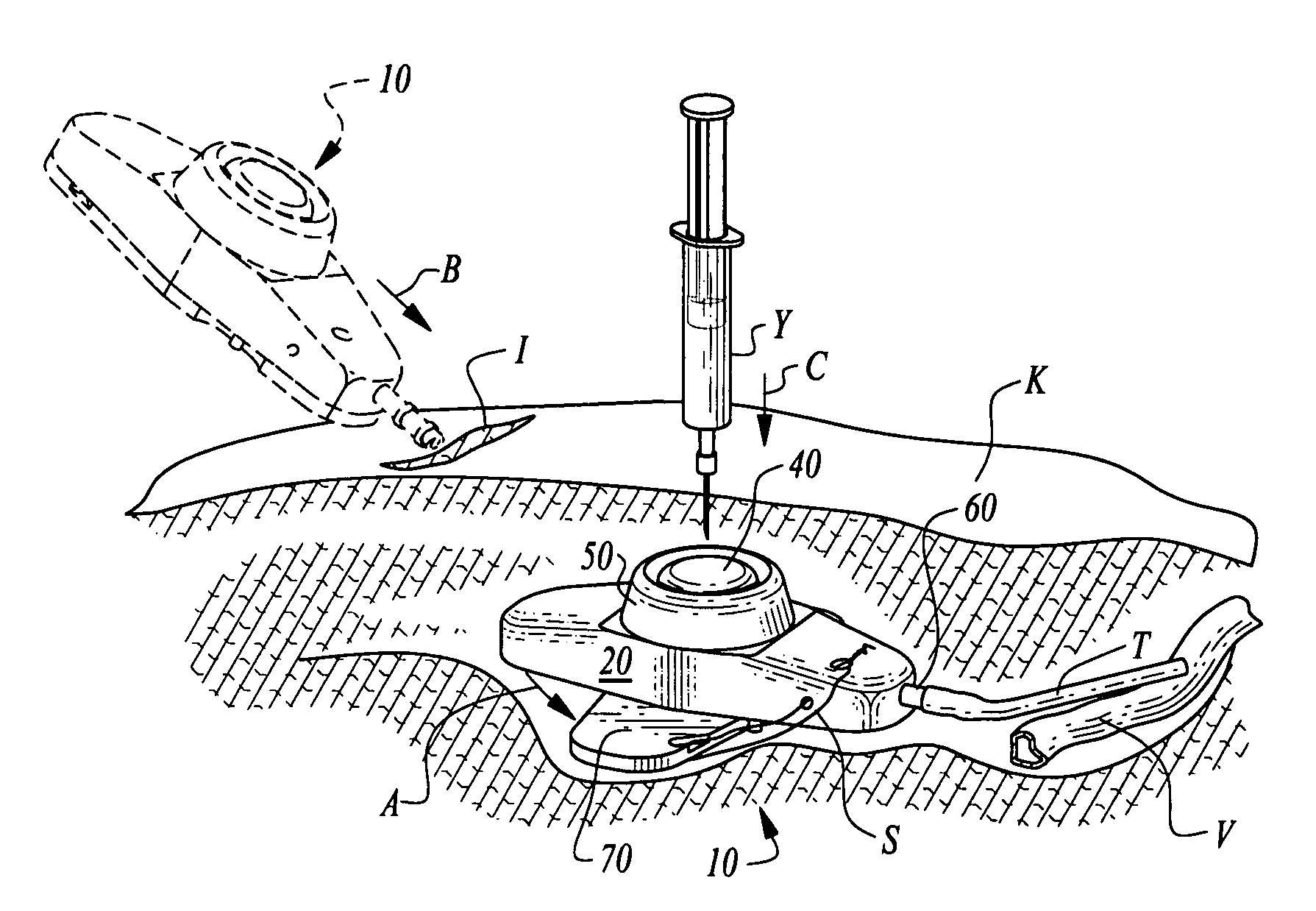
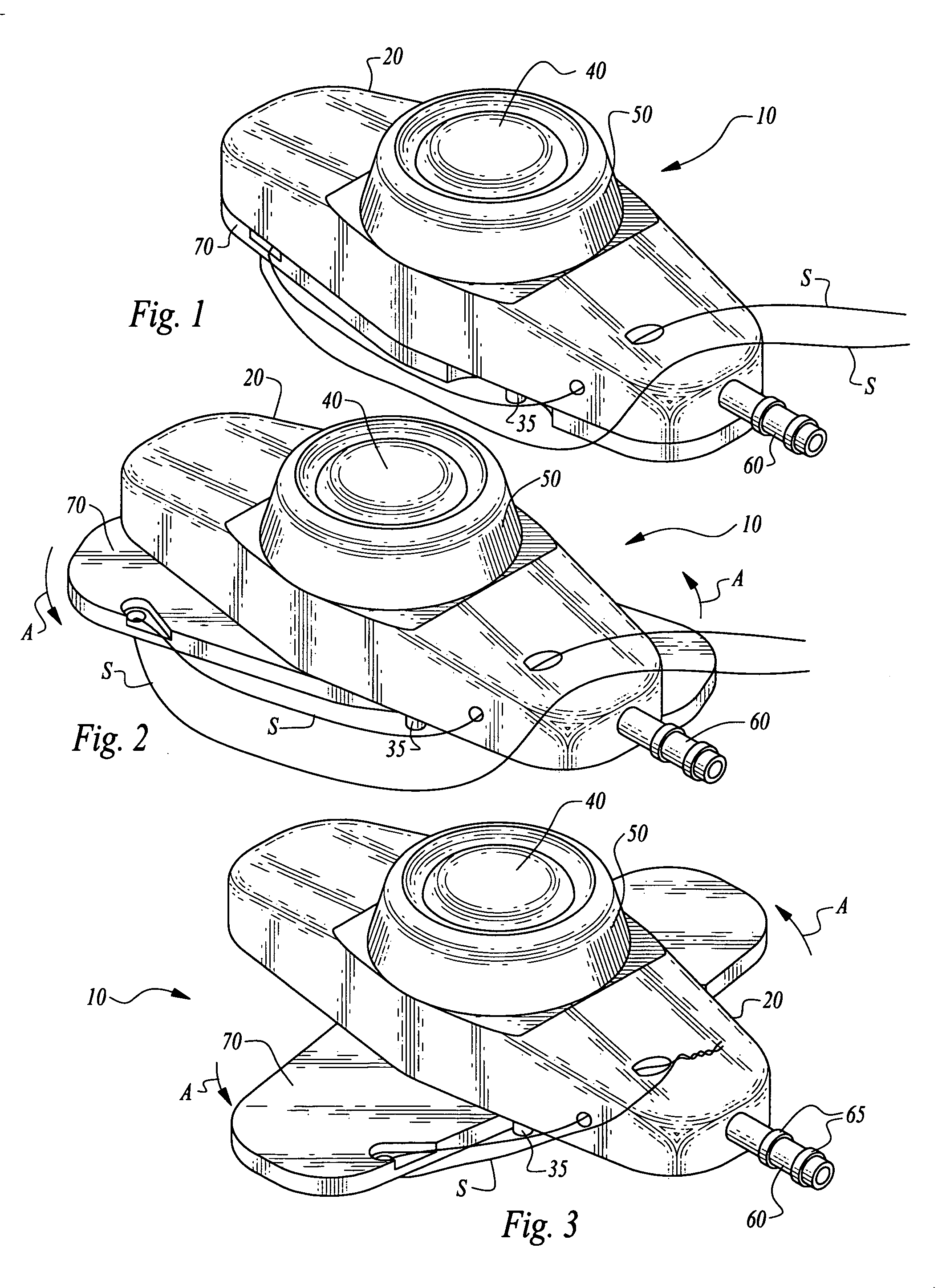
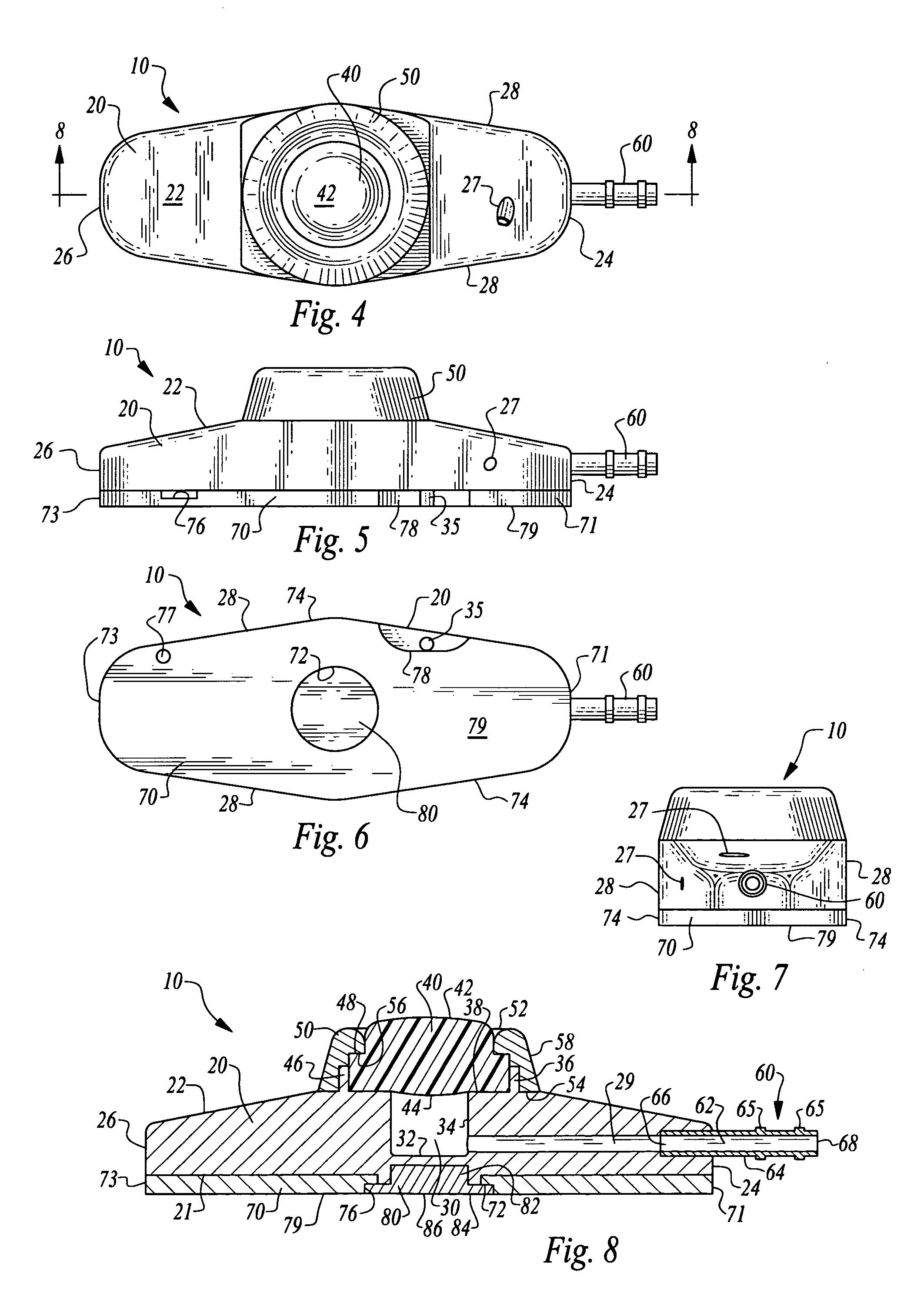
Stabilized implantable vascular access port
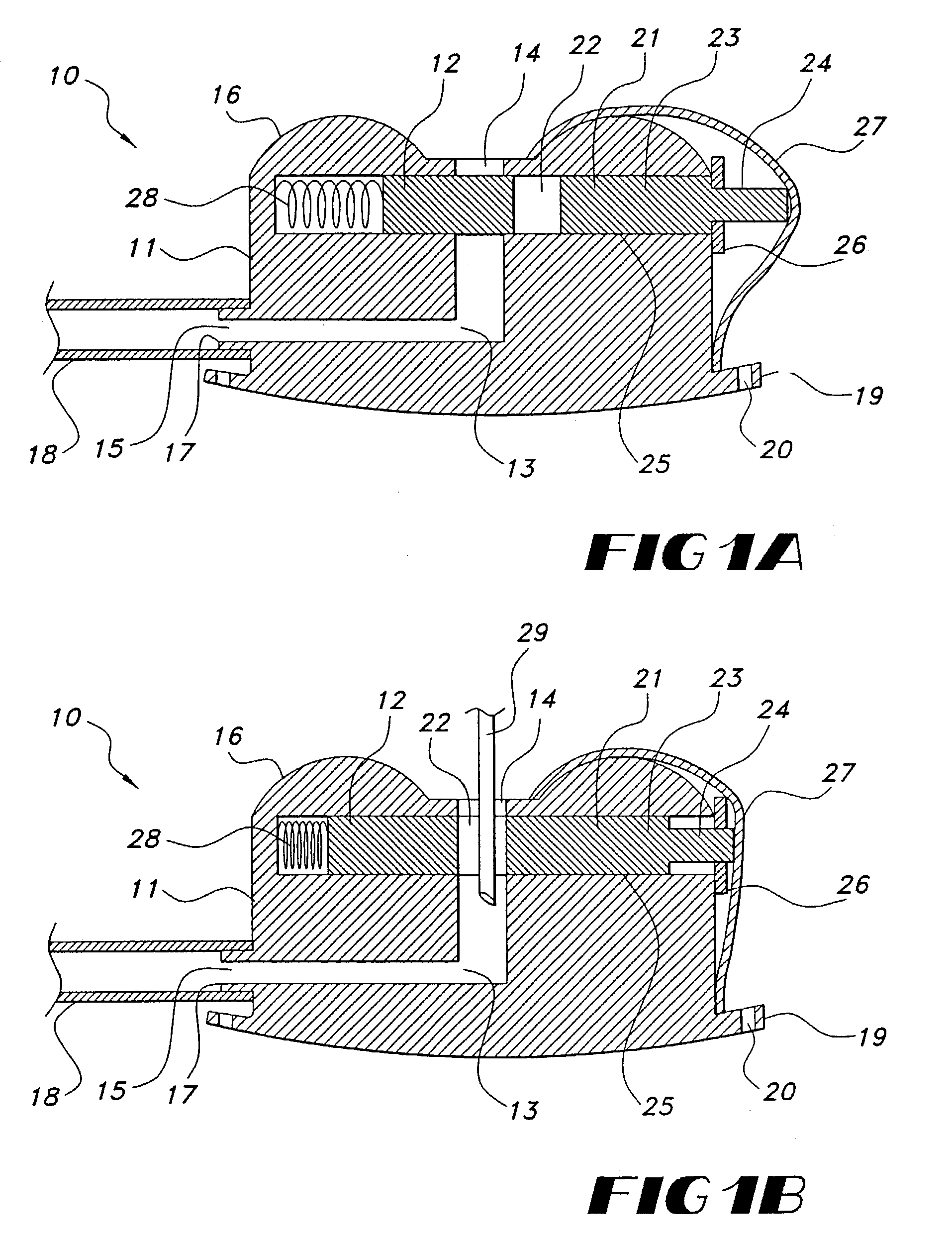
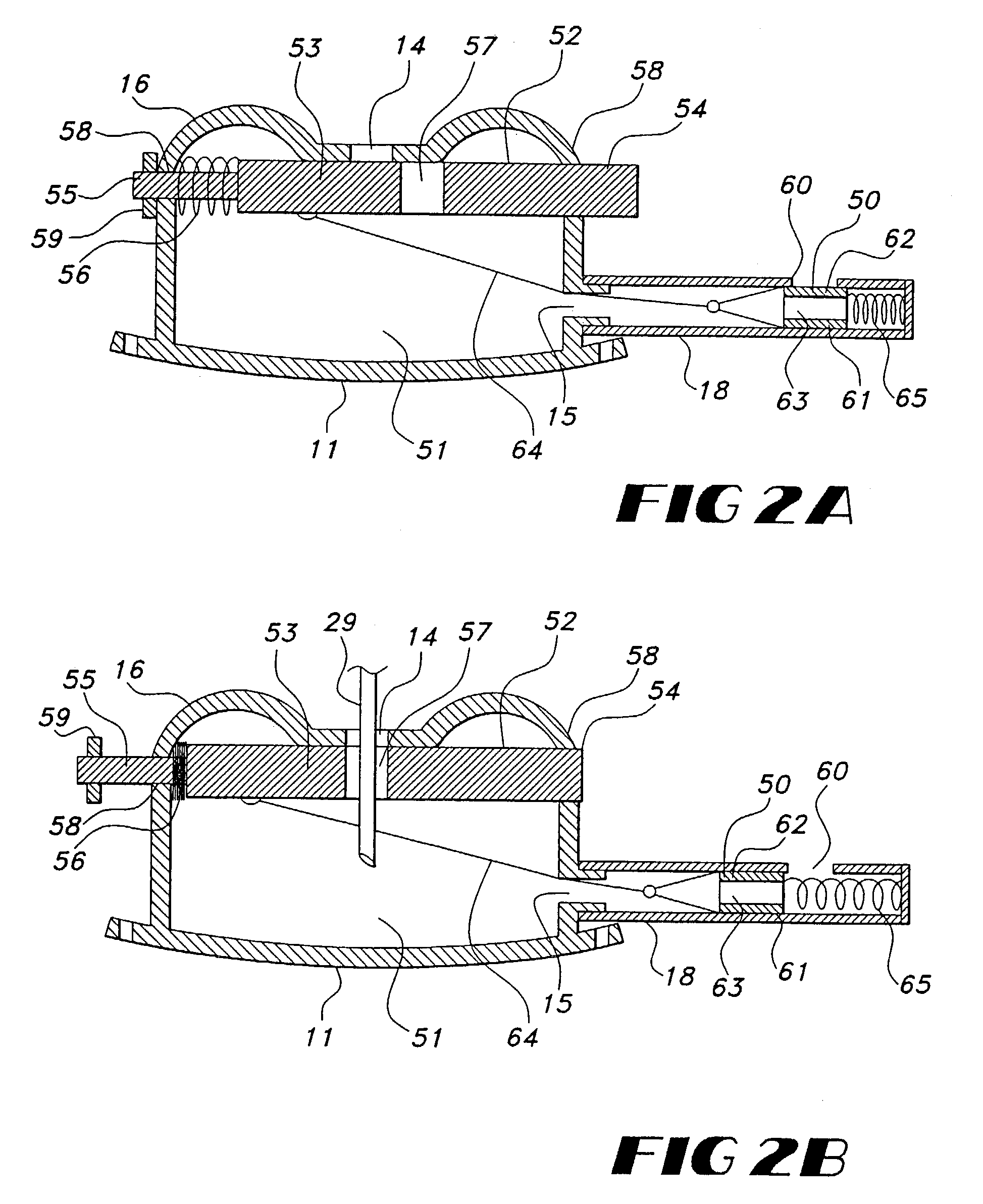
InactiveUS20070161958A1Easy to useSmall sizeSurgeryMedical devicesVascular structureAerospace engineering
The subcutaneously implantable vascular access port has two parts including a body and a wing. The body supports a chamber covered by a septum, with a septum held in place over the chamber by a collar. The chamber is coupleable to a vascular structure, such as through tubing extending from the body, for delivery of medical preparations. The body is preferably elongate in form. The wing is configured to be adjustable in width. In one embodiment the wing rotates relative to the body and has an elongate form similar to that of the body. When the wing is rotated it extends laterally from the body and enhances a stability of the body. In another embodiment, the wing is provided as a deformable wing which can expand laterally out of side openings of a cavern in the body into which the deformable wing is inserted.
Owner:STEALTH THERAPEUTICS
Devices and methods for tissue modification
ActiveUS20060095059A1Easy to disassembleEliminate needCannulasAnti-incontinence devicesSurgical departmentNerve stimulation
Owner:MIS IP HLDG LLC +1
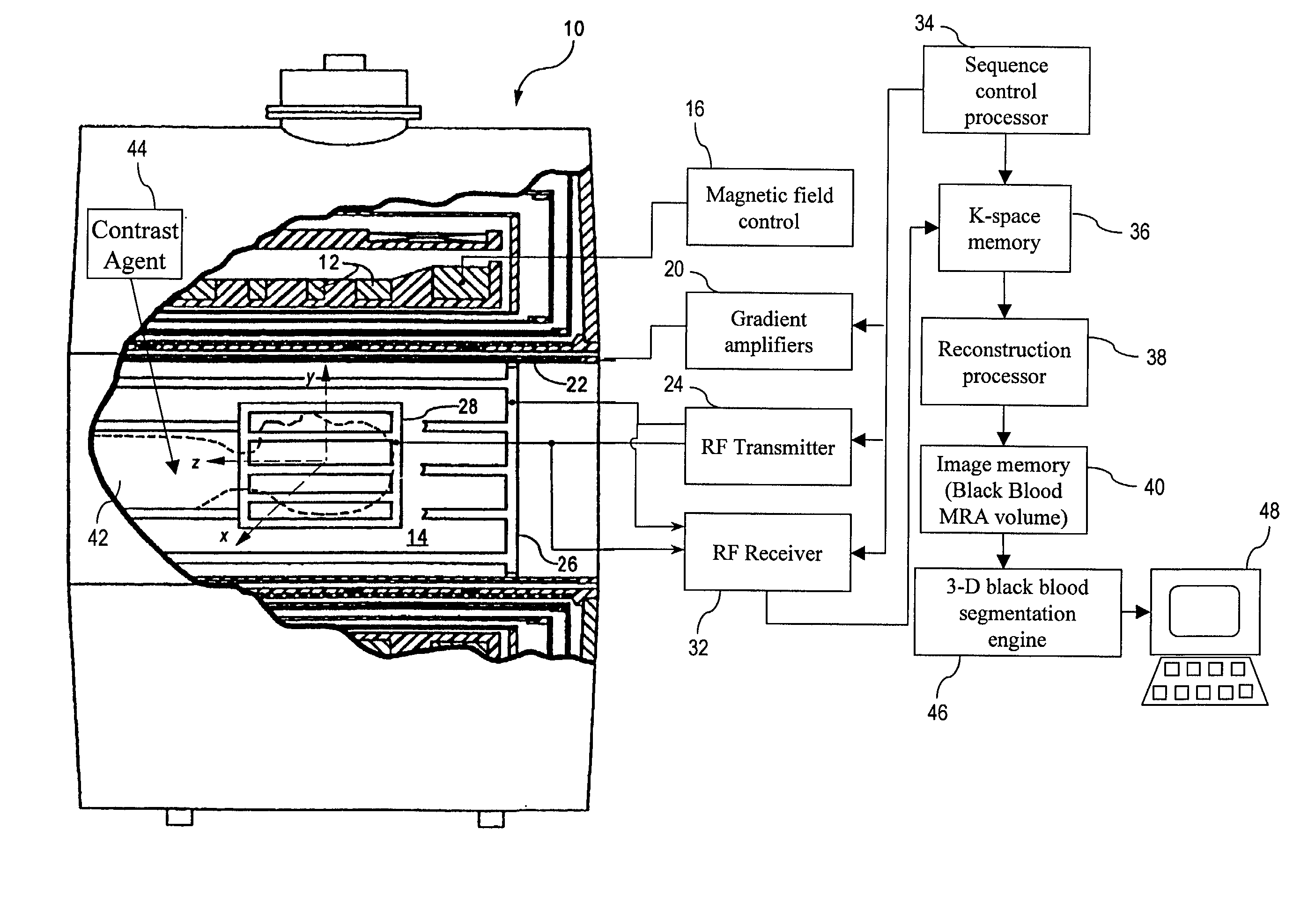
Black blood angiography method and apparatus
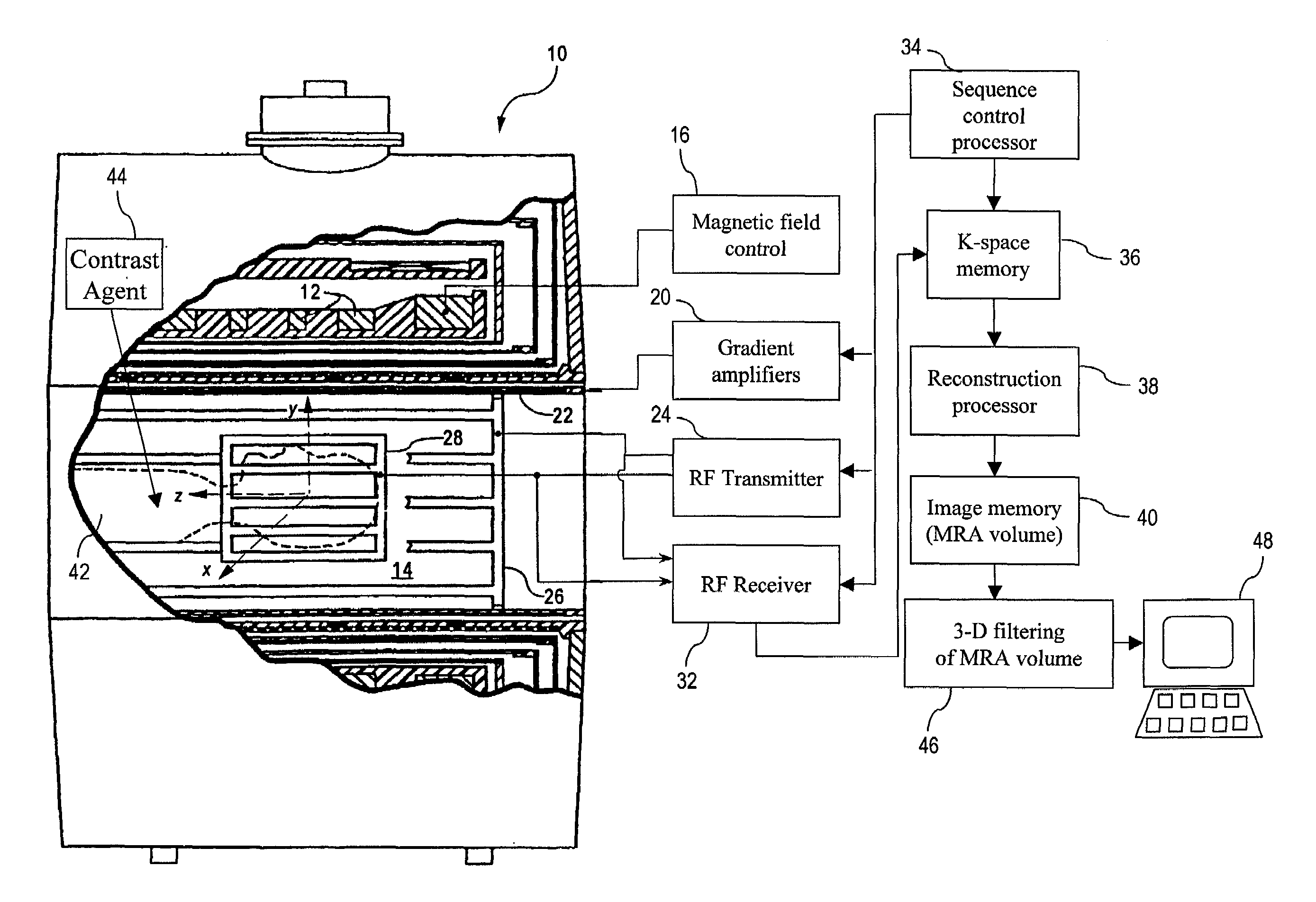
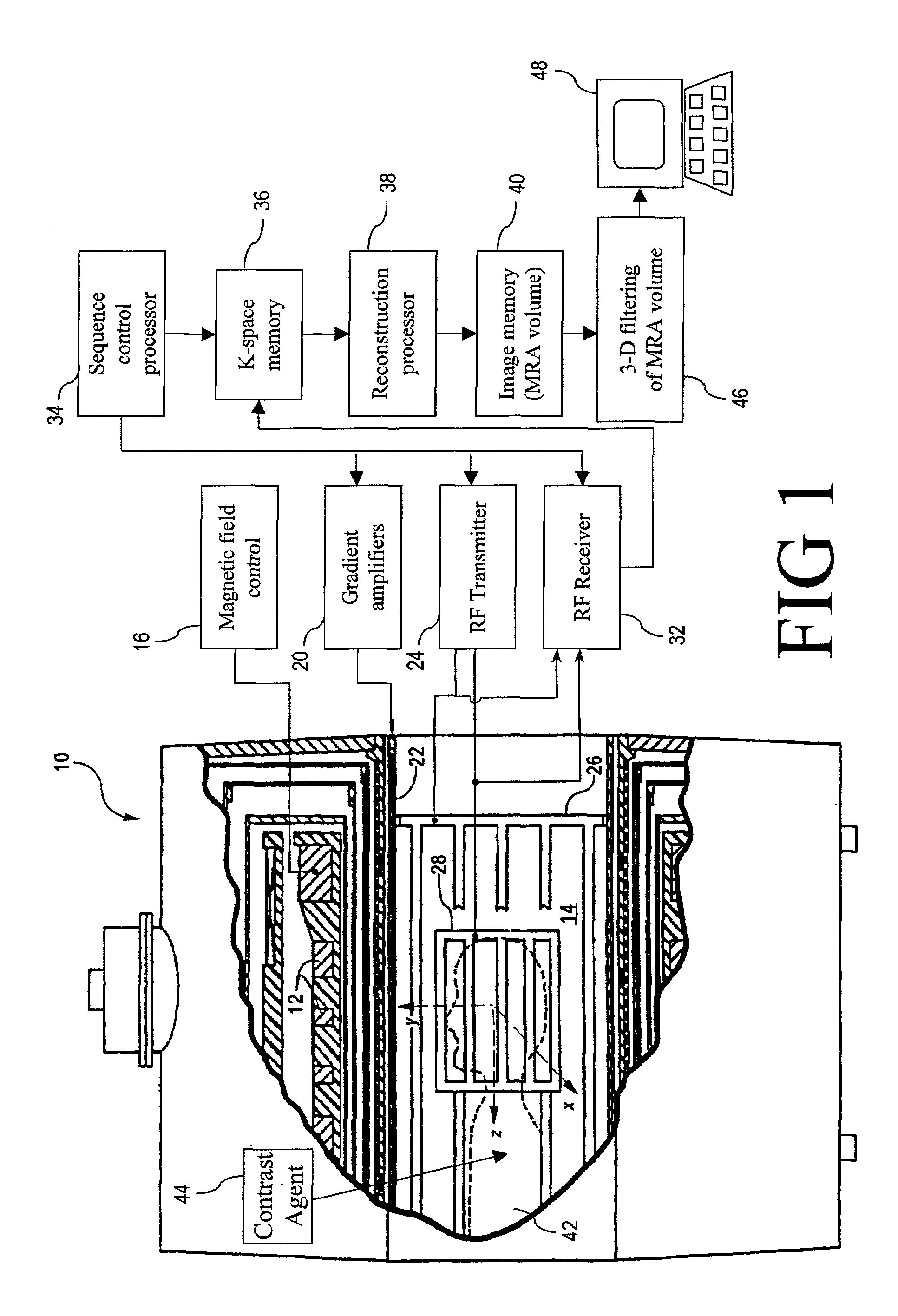
InactiveUS7020314B1Structural interferenceRemove non-vascular contrastImage enhancementCharacter and pattern recognitionBlack bloodBlood Vessel Tissue
To produce a black body angiographic image representation of a subject (42), an imaging scanner (10) acquires imaging data that includes black blood vascular contrast. A reconstruction processor (38) reconstructs a gray scale image representation (100) from the imaging data. A post-acquisition processor (46) transforms (130) the image representation (100) into a pre-processed image representation (132). The processor (46) assigns (134) each image element into one of a plurality of classes including a black class corresponding to imaged vascular structures, bone, and air, and a gray class corresponding to other non-vascular tissues. The processor (46) averages (320) intensities of the image elements of the gray class to obtain a mean gray intensity value (322), and replaces (328) the values of image elements comprising non-vascular structures of the black class with the mean gray intensity value.
Owner:KONINKLIJKE PHILIPS ELECTRONICS NV +1
Use of contrast agents to increase the effectiveness of high intensity focused ultrasound therapy
InactiveUS7686763B2Easy to useGood choiceUltrasound therapyBlood flow measurement devicesCavitationUltrasound contrast media
Ultrasound contrast agents are used to enhance imaging and facilitate HIFU therapy in four different ways. A contrast agent is used: (1) before therapy to locate specific vascular structures for treatment; (2) to determine the focal point of a HIFU therapy transducer while the HIFU therapy transducer is operated at a relatively low power level, so that non-target tissue is not damaged as the HIFU is transducer is properly focused at the target location; (3) to provide a positive feedback mechanism by causing cavitation that generates heat, reducing the level of HIFU energy administered for therapy compared to that required when a contrast agent is not used; and, (4) to shield non-target tissue from damage, by blocking the HIFU energy. Various combinations of these techniques can also be employed in a single therapeutic implementation.
Owner:UNIV OF WASHINGTON
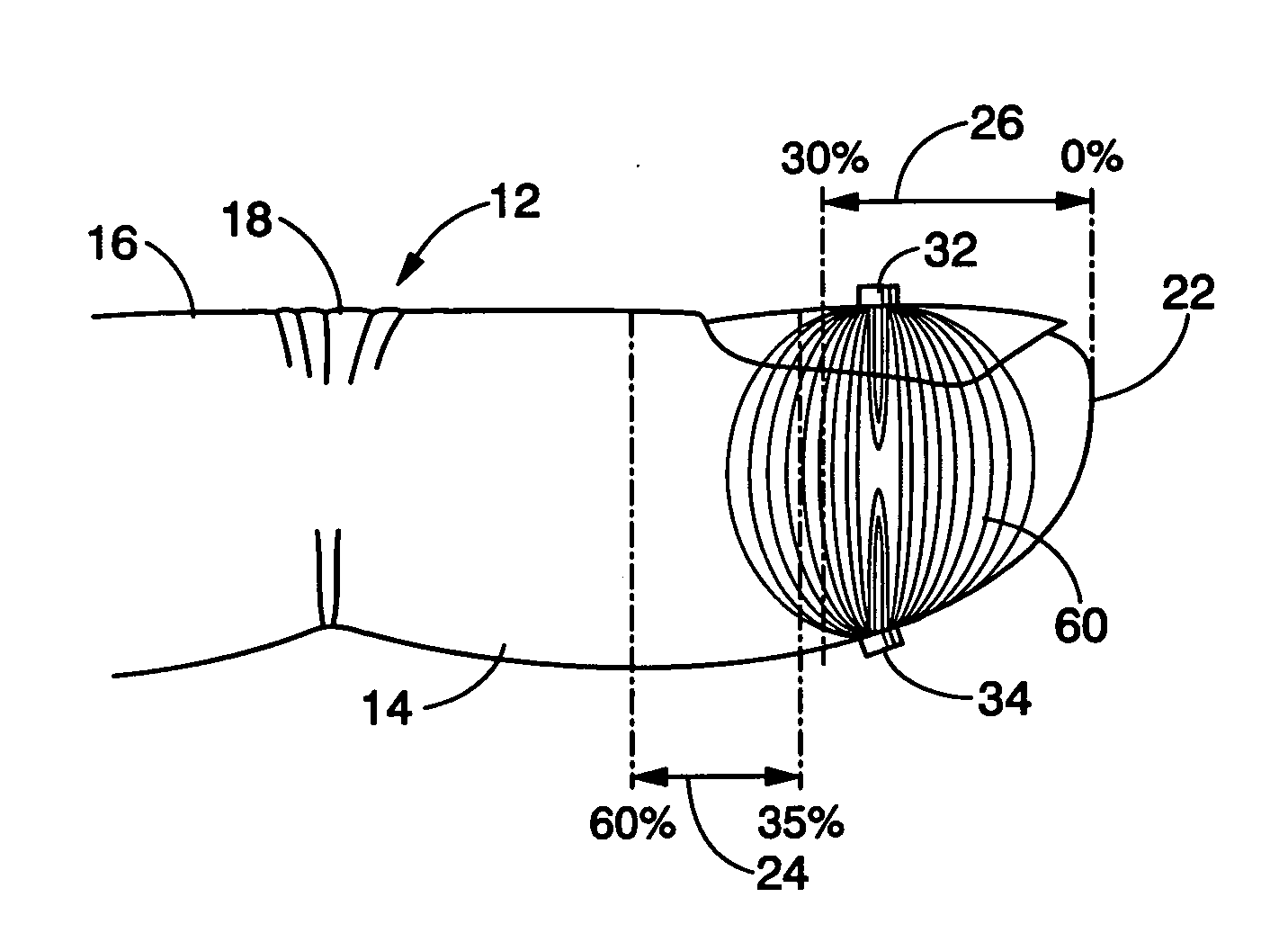
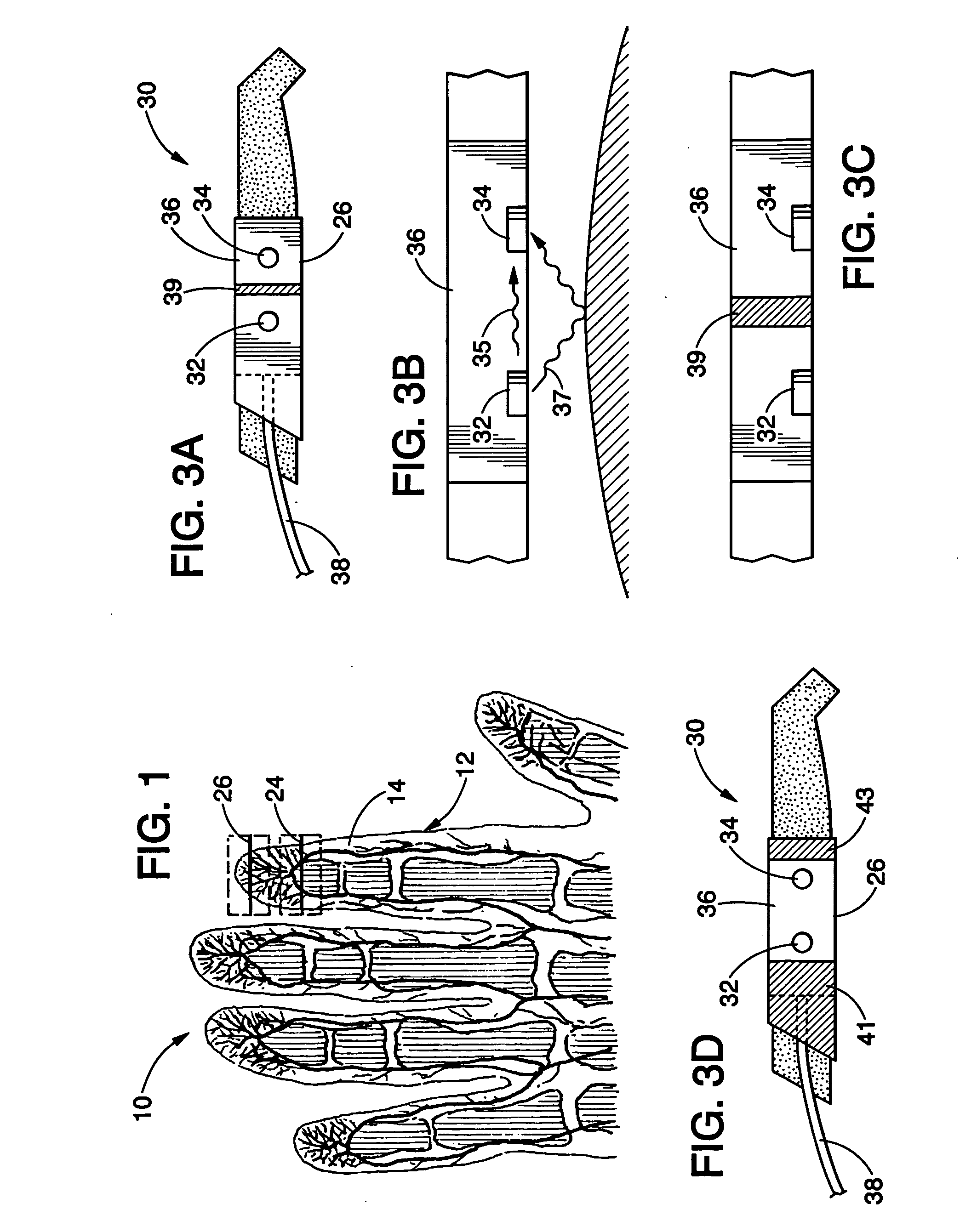
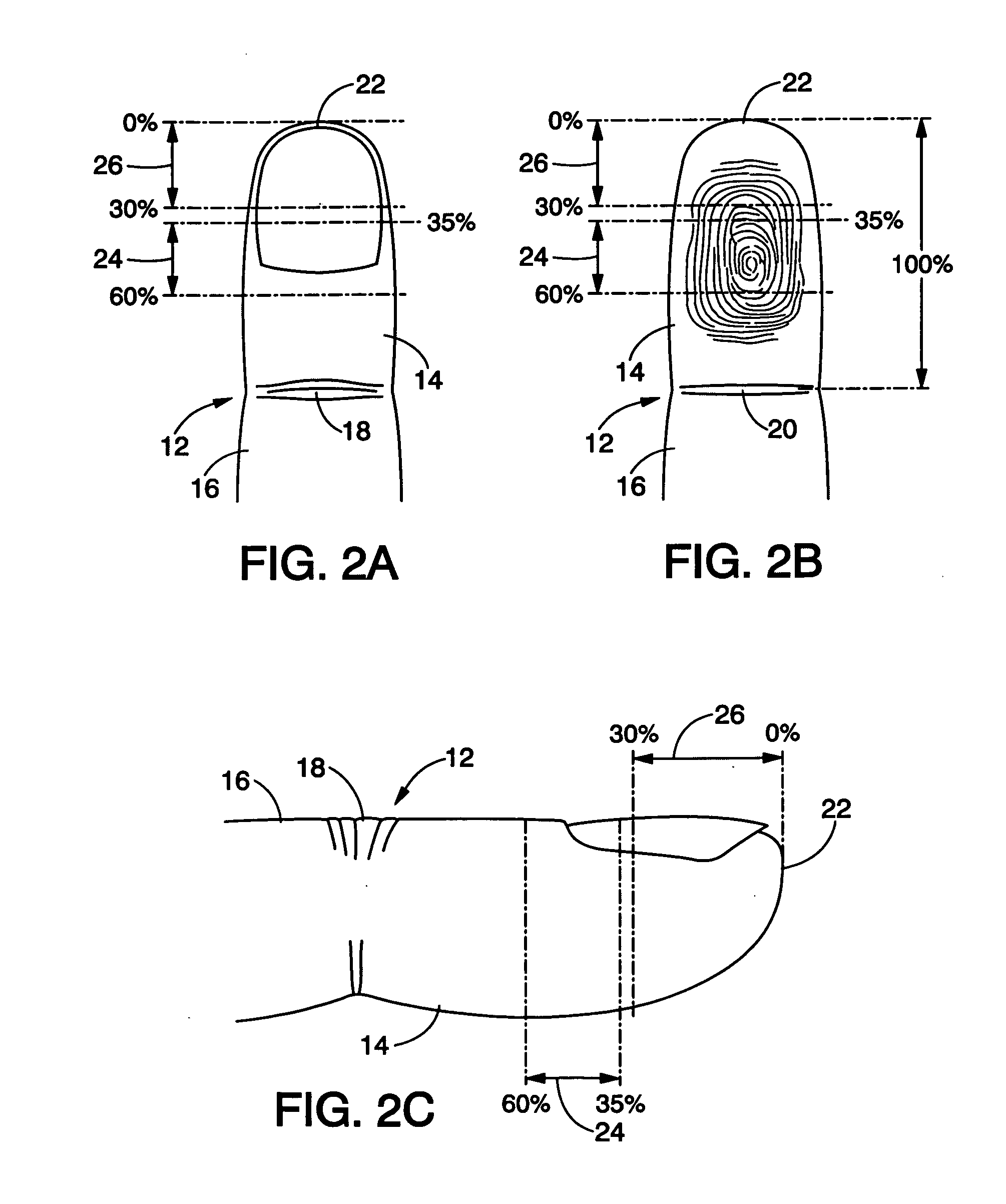
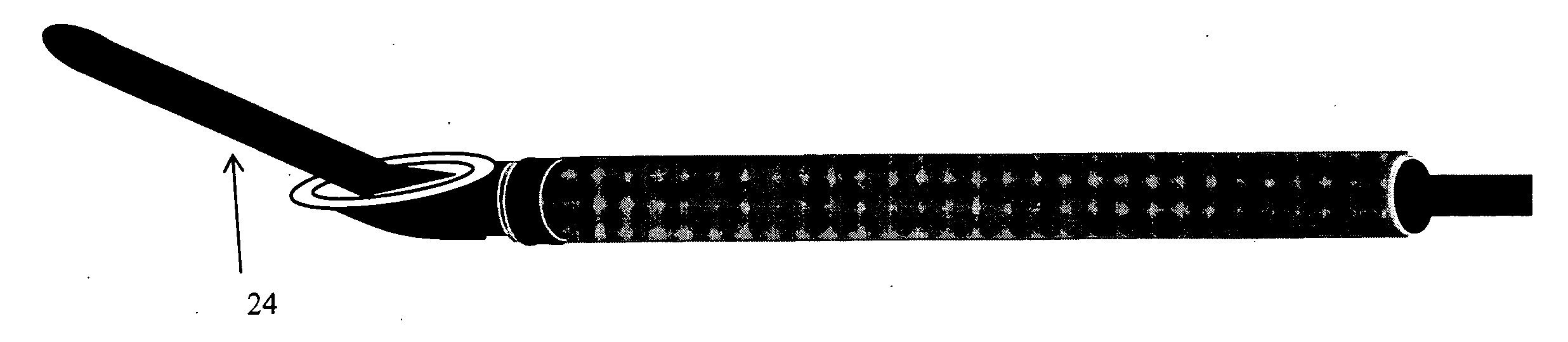
Pulse oximetry sensor and technique for using the same on a distal region of a patient's digit
ActiveUS20060224058A1Diagnostic recording/measuringSensorsOxygen Saturation MeasurementDistal portion
A sensor may be placed on a distal portion of a patient's finger or toe to obtain pulse oximetry measurements. The distal portion of a digit contains few if any large vascular structures that could adversely affect pulse oximetry measurements, but the distal portion does contain microvasculature that carries arterial blood that facilitates pulse oximetry measurements. The sensor may include an emitter and a detector that are spaced apart by an appropriate distance so that they may be located on the distal portion of a patient's digit during pulse oximetry measurements.
Owner:TYCO HEALTHCARE GRP LP
Devices and methods for tissue modification
ActiveUS20060089609A1Enabling symptomatic reliefApproach can be quite invasiveCannulasAnti-incontinence devicesSurgical removalEpidural needles
Methods and apparatus are provided for selective surgical removal of tissue. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. The sharp tip of the needle in the epidural space, can be converted to a blunt tipped instrument for further safe advancement. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. A nerve stimulator may be provided to reduce a risk of inadvertent neural abrasion.
Owner:MIS IP HLDG LLC +1
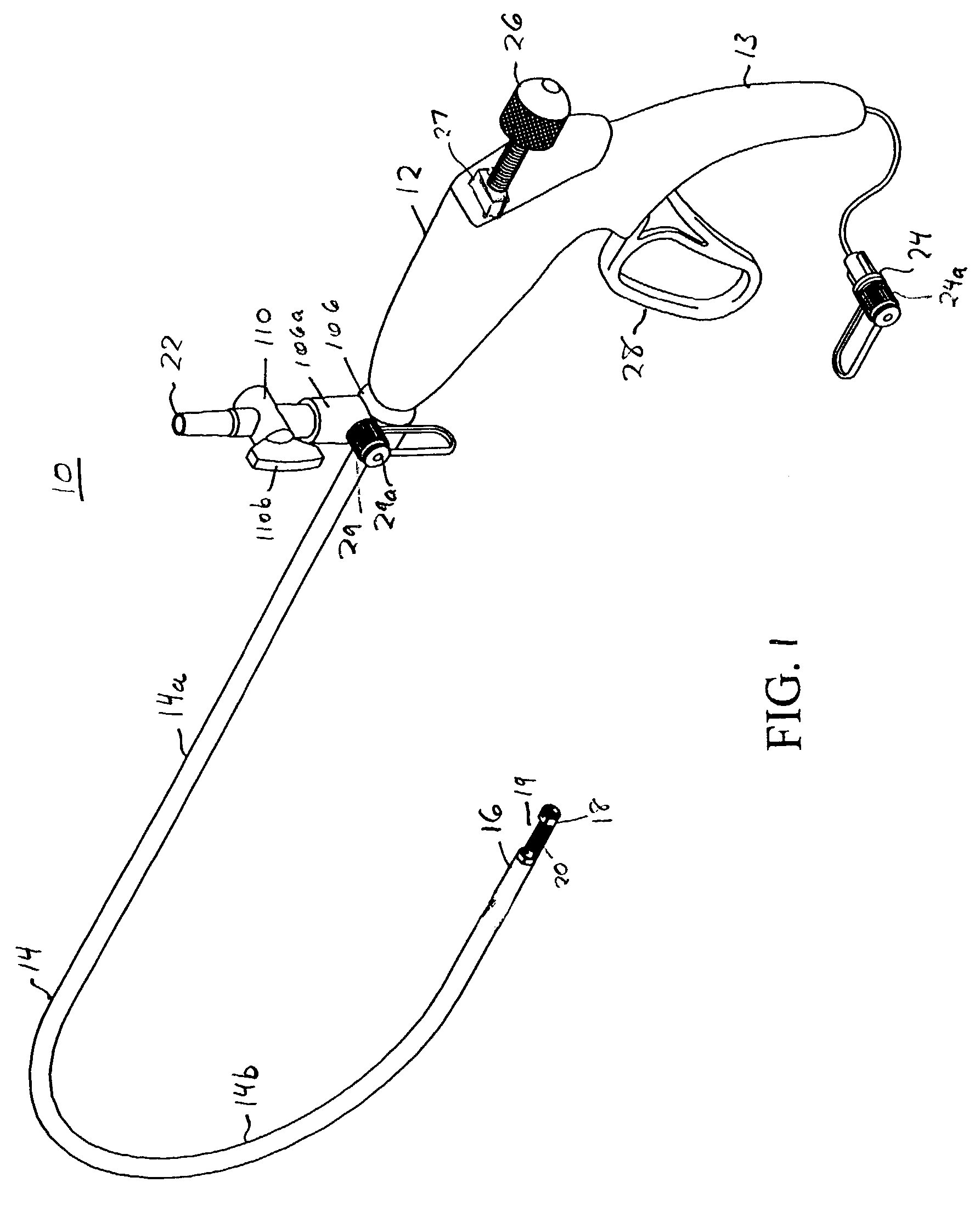
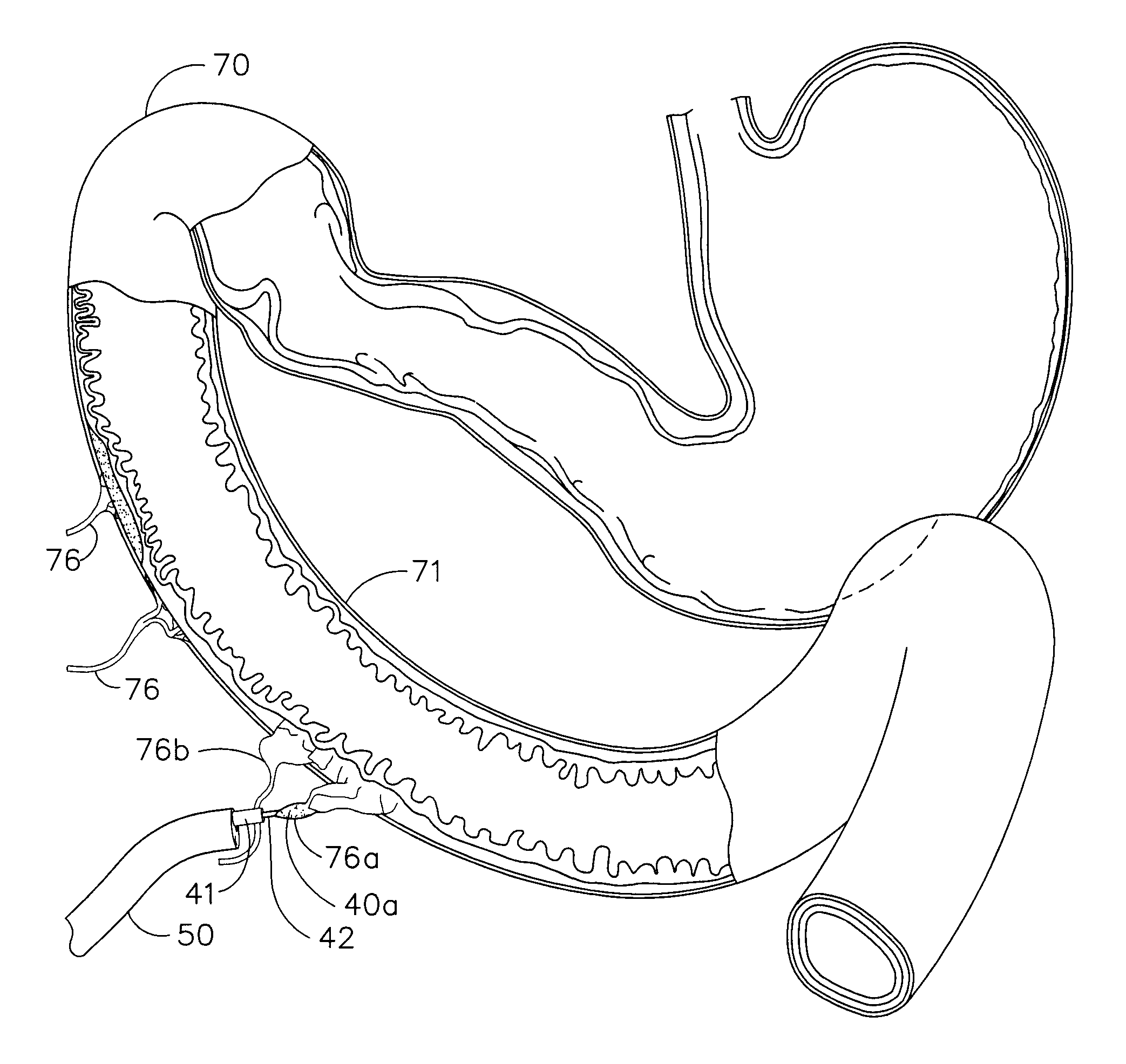
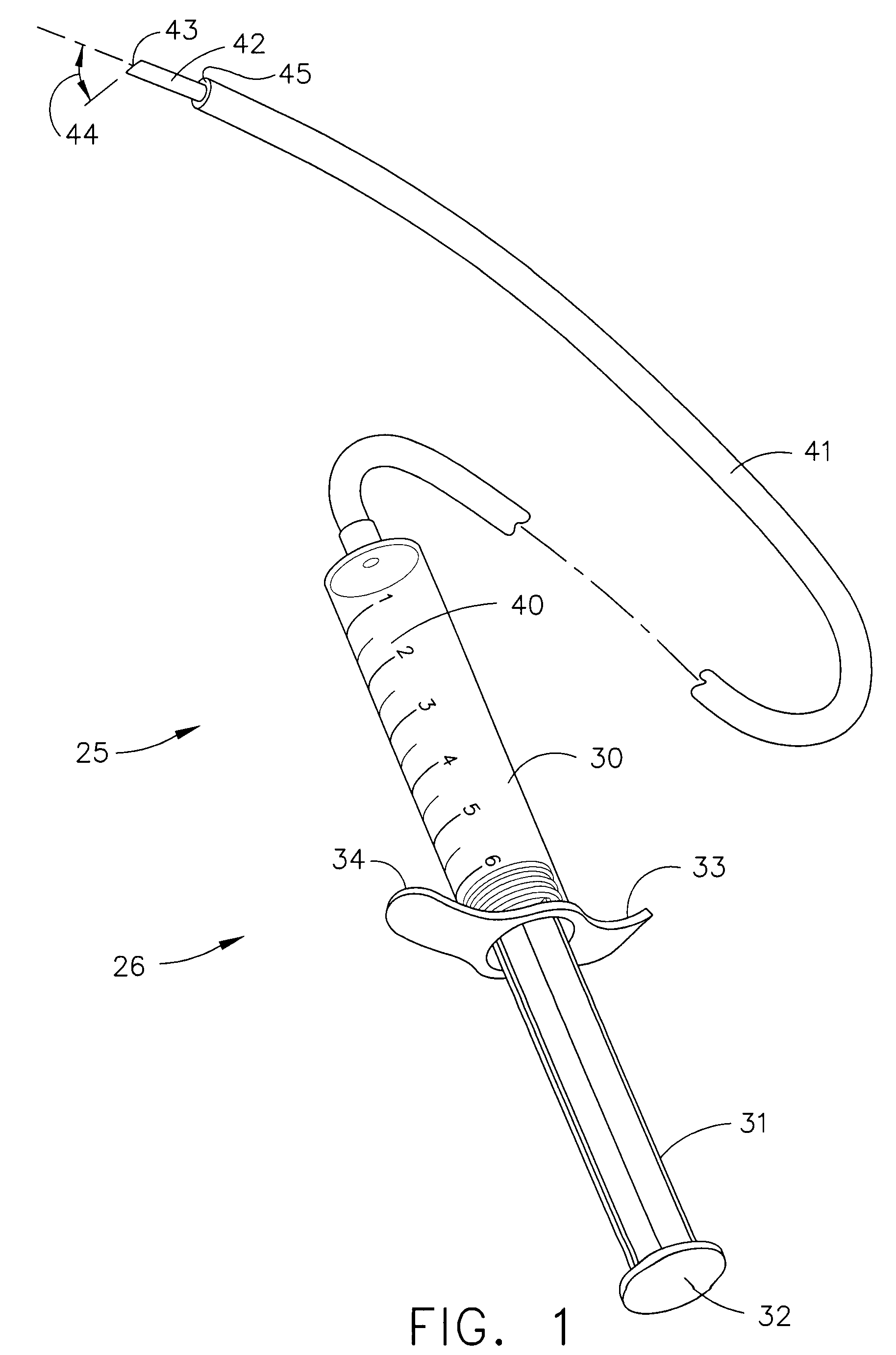
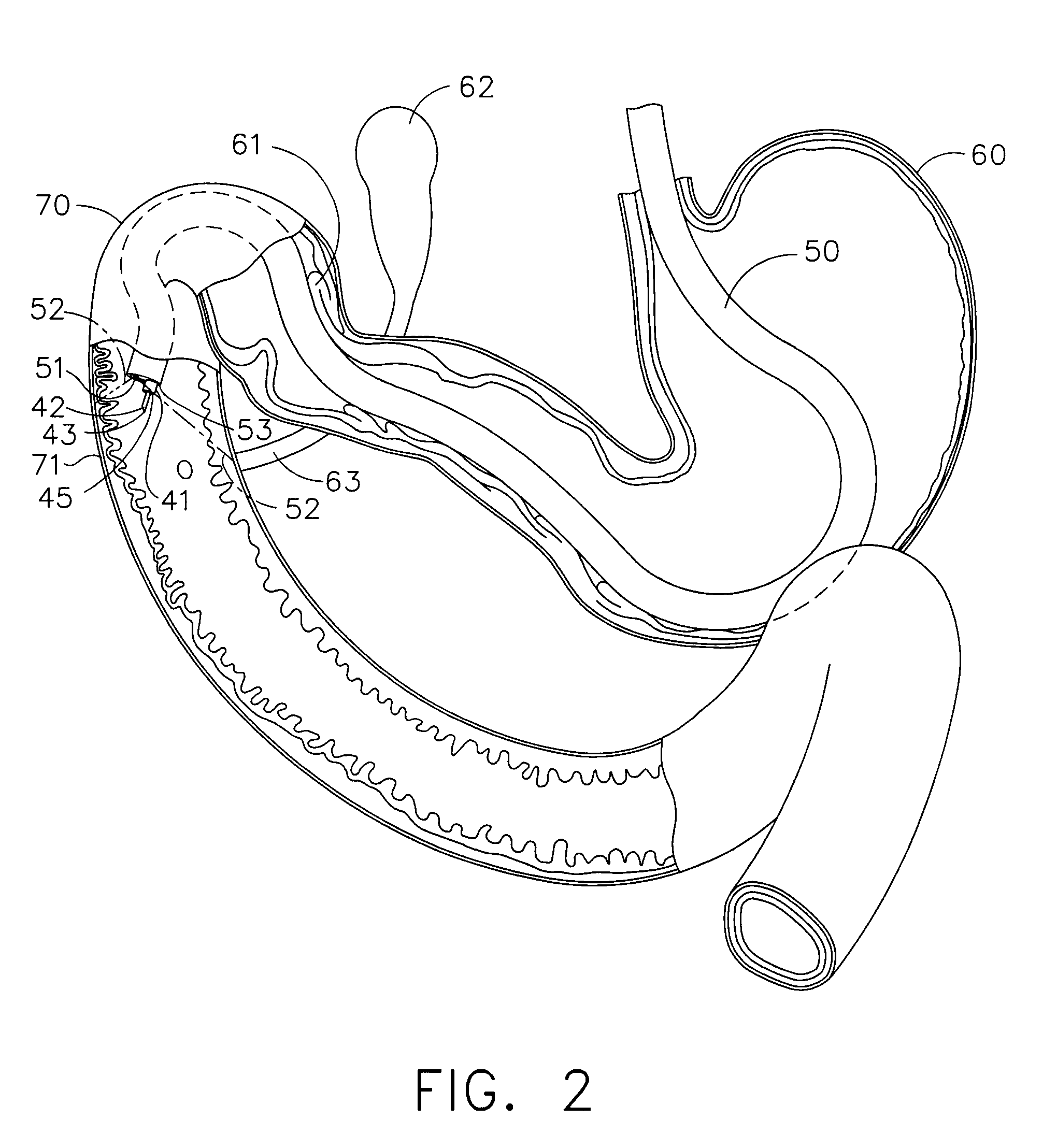
Subcutaneously implanted cannula and method for arterial access
InactiveUS6398764B1Avoid blood lossReduce exerciseMedical devicesCatheterDifferential pressureSubcutaneous implantation
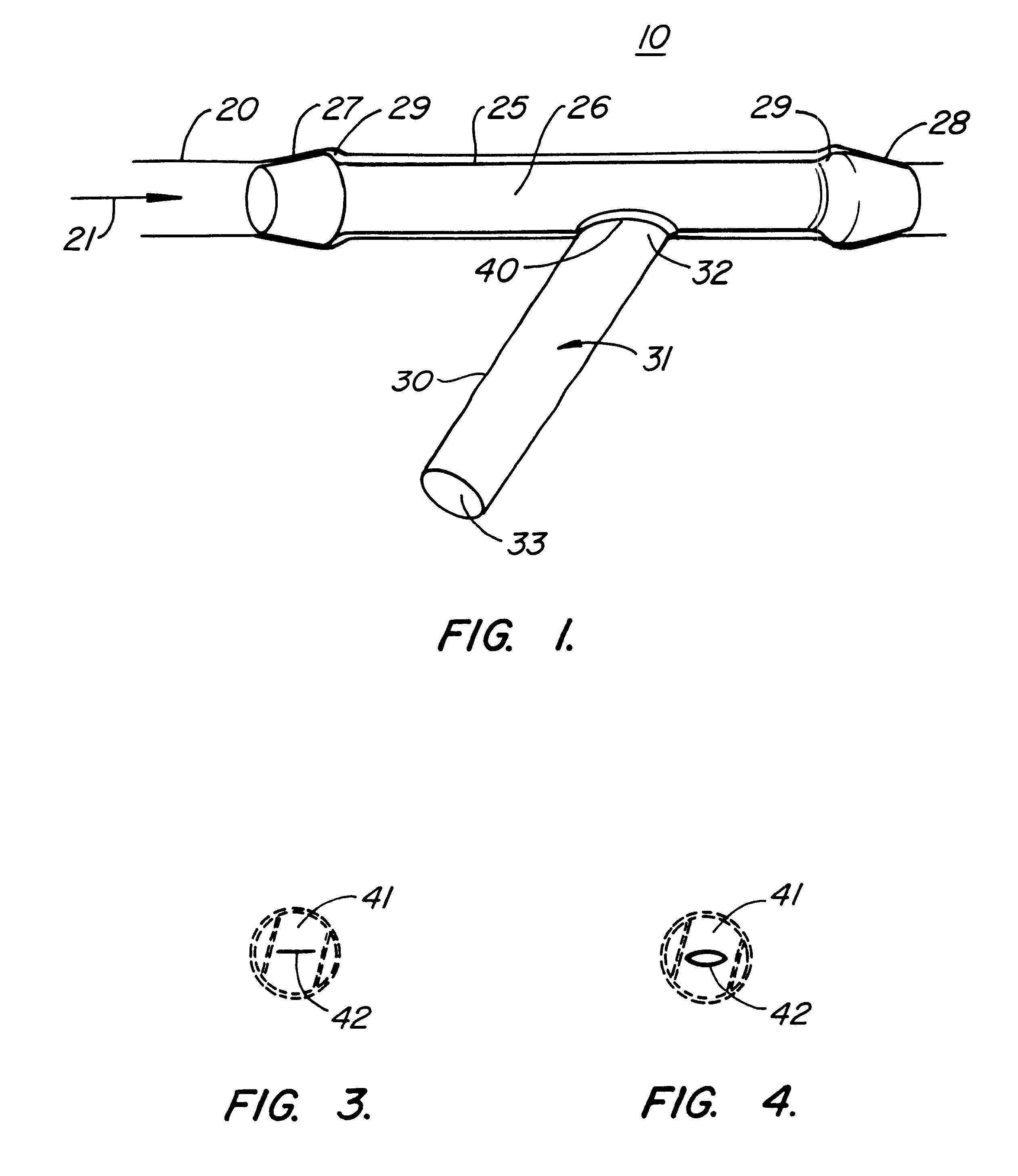
A catheter with valve for implantation in a vascular structure of a living being. The catheter is in the general shape of a "T" with the top of the "T" implanted within the lumen of a vascular structure, and the leg of the "T" extending out of the vascular structure through an incision in the vascular structure. The lumen of the implanted portion of the catheter completely occupies the lumen of the vascular structure, causing all blood flow through the vascular structure to be directed through the implanted portion of the catheter. A valve is placed in the wall of the implanted portion of the catheter which opens into the lumen of the leg of the "T" of the catheter upon application of sufficient differential pressure between the lumens of the two portions of the catheter. The leg of the "T" is connected to the side wall of the implant portion of the catheter at an angle, such that the axis of the lumen of the leg of the "T" intersects the axis of the lumen of the implanted portion of the catheter at approximately a 45 degree angle.
Owner:VASCA
Devices and methods for tissue modification
InactiveUS20100094231A1Improve securityAvoid injuryCannulasDiagnosticsSurgical removalEpidural needles
Owner:BAXANO
Devices and methods for tissue modification
ActiveUS20090204119A1Enabling symptomatic reliefApproach can be quite invasiveSpinal electrodesCannulasSurgical removalVascular structure
Methods and apparatus are provided for selective surgical removal of tissue. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. The sharp tip of the needle in the epidural space, can be converted to a blunt tipped instrument for further safe advancement. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. A nerve stimulator may be provided to reduce a risk of inadvertent neural abrasion.
Owner:MIS IP HLDG LLC +1
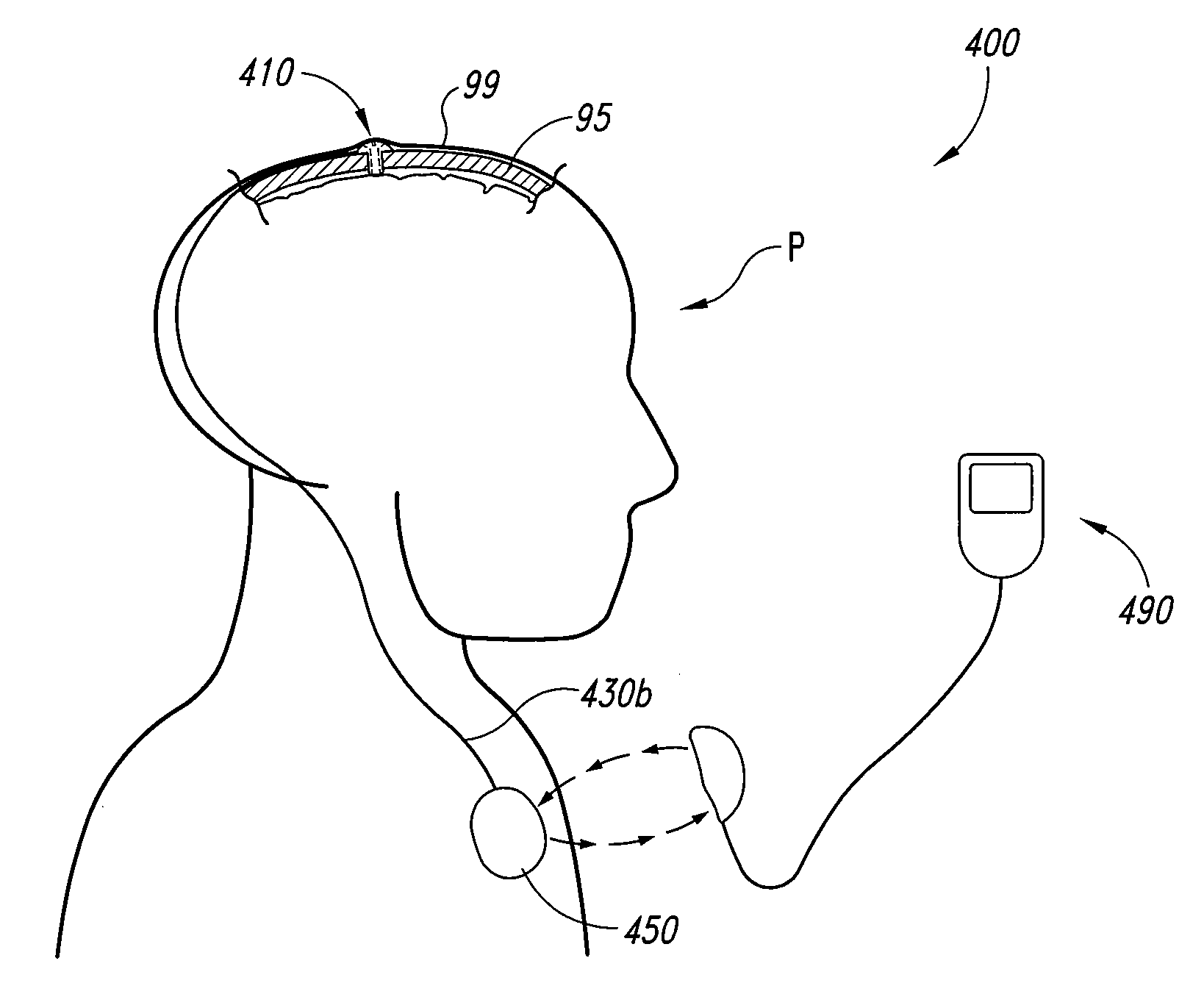
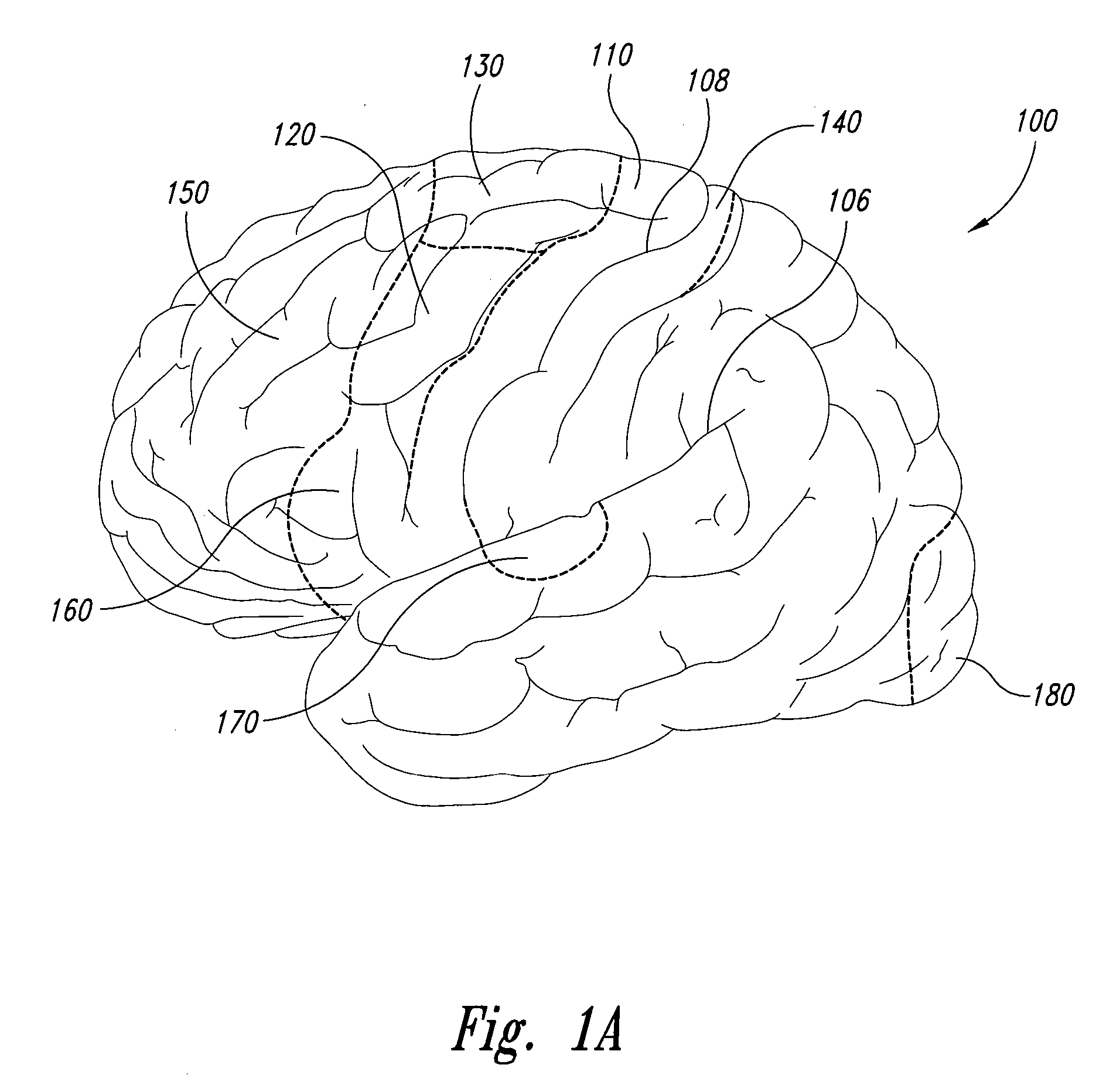
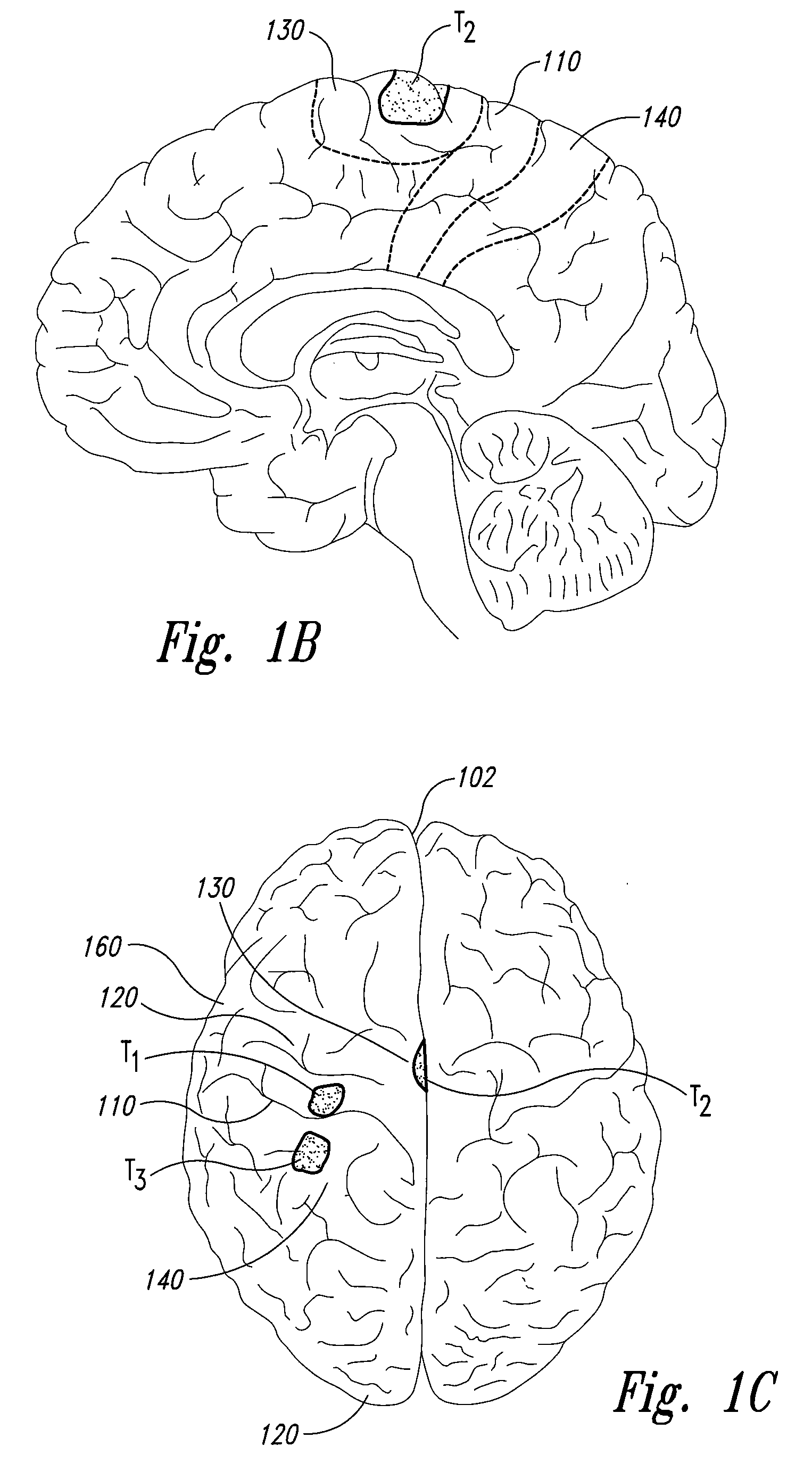
Electrode configurations for reducing invasiveness and/or enhancing neural stimulation efficacy, and associated methods
Owner:ADVANCED NEUROMODULATION SYST INC
Electrode configurations for reducing invasiveness and/or enhancing neural stimulation efficacy, and associated methods
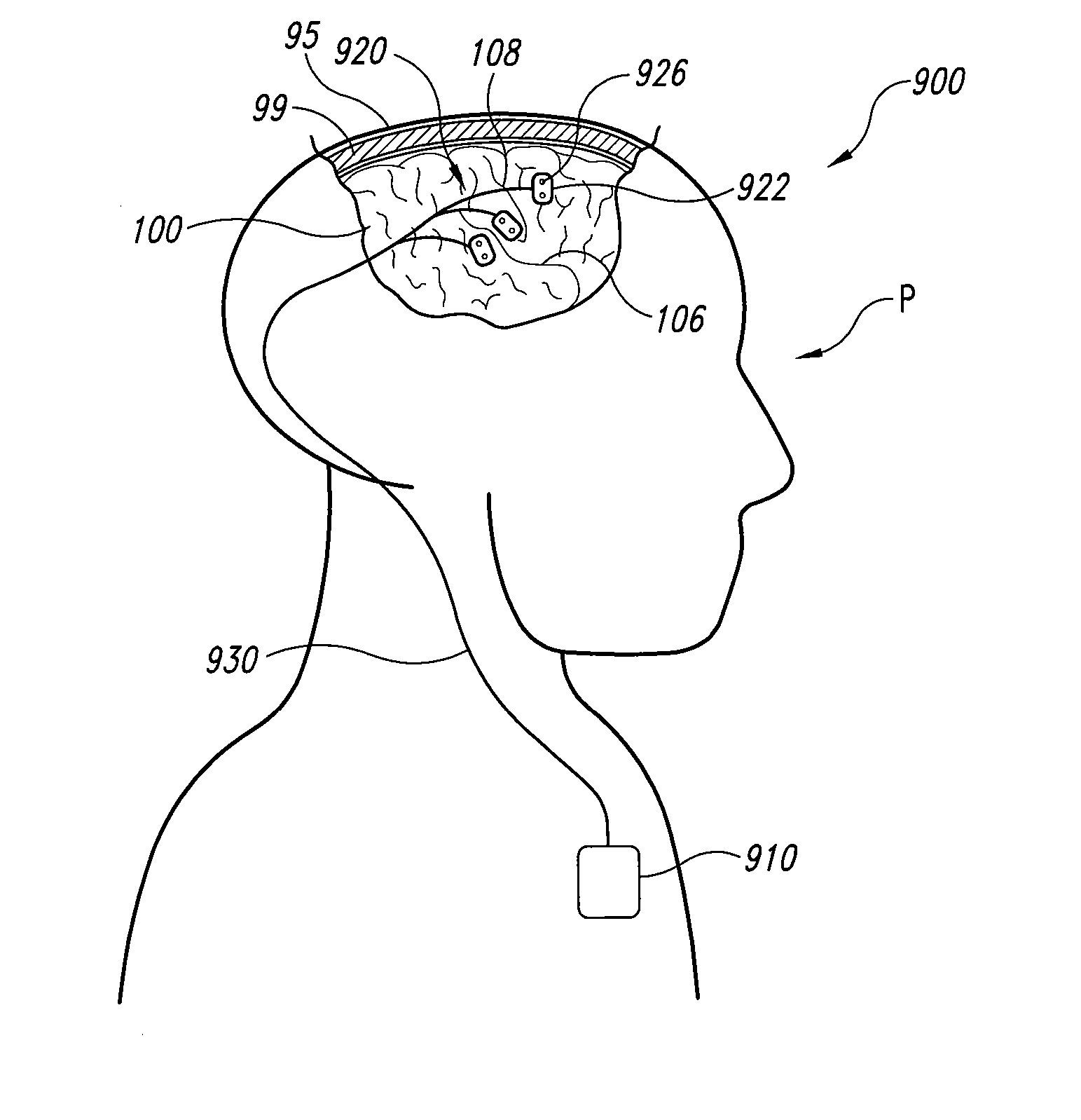
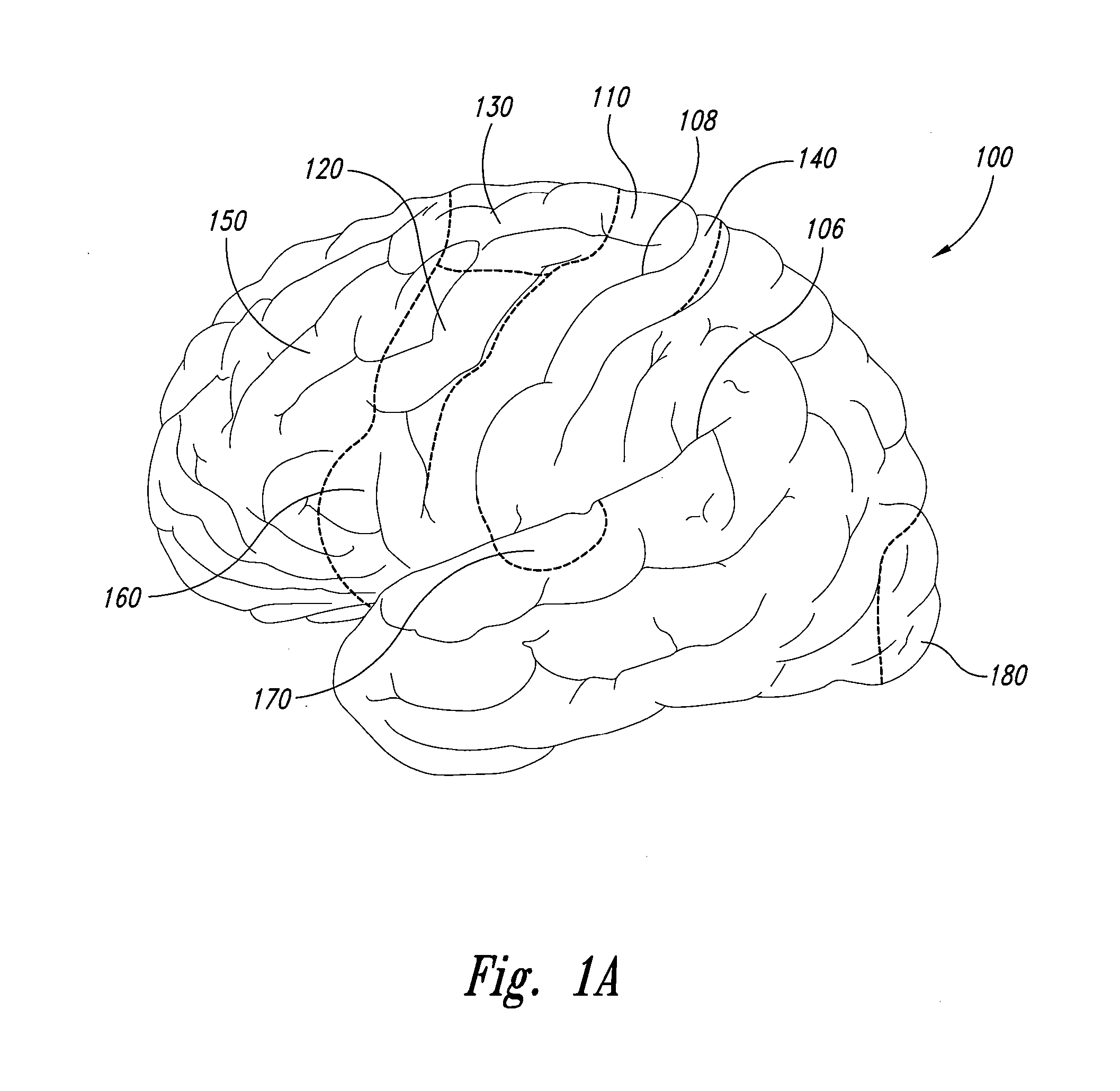
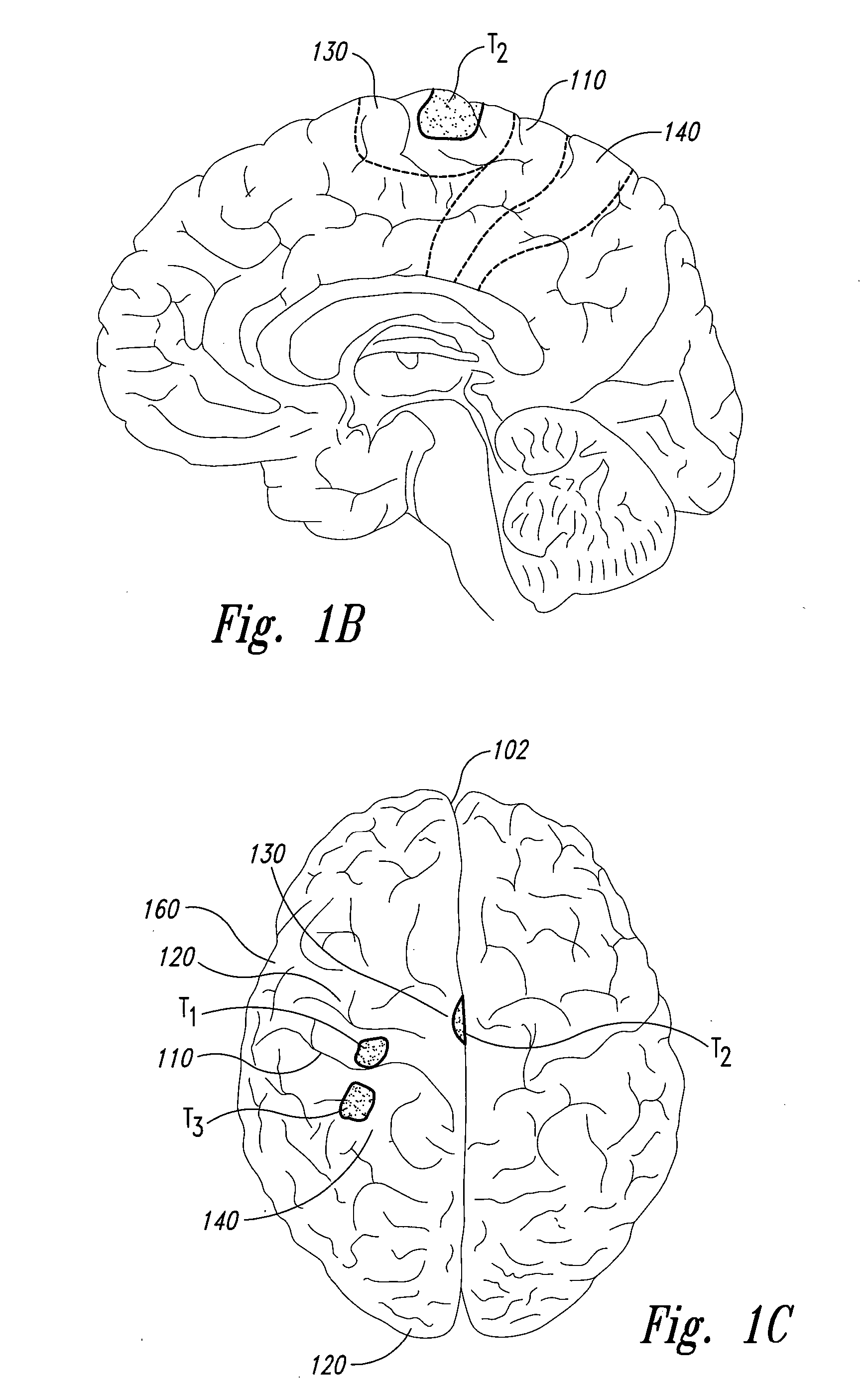
Electrode configurations for reducing invasiveness and / or enhancing neural stimulation efficacy, and associated methods, are disclosed. A method in accordance with one embodiment of the invention for treating a brain disorder includes identifying a target neural structure within a patient's skull and implanting an electrode device within the patient's skull so that an axis that is generally normal to the skull proximate to the electrode device and that passes through at least one electrical contact of the electrode device is offset from the target neural structure. The method further includes stimulating the target neural structure by applying an electrical signal to the at least one electrical contact. In particular embodiments, the electrode device can be positioned between, along, across, or adjacent to a fissure, recess, groove, and / or vascular structure of the patient's brain.
Owner:ADVANCED NEUROMODULATION SYST INC
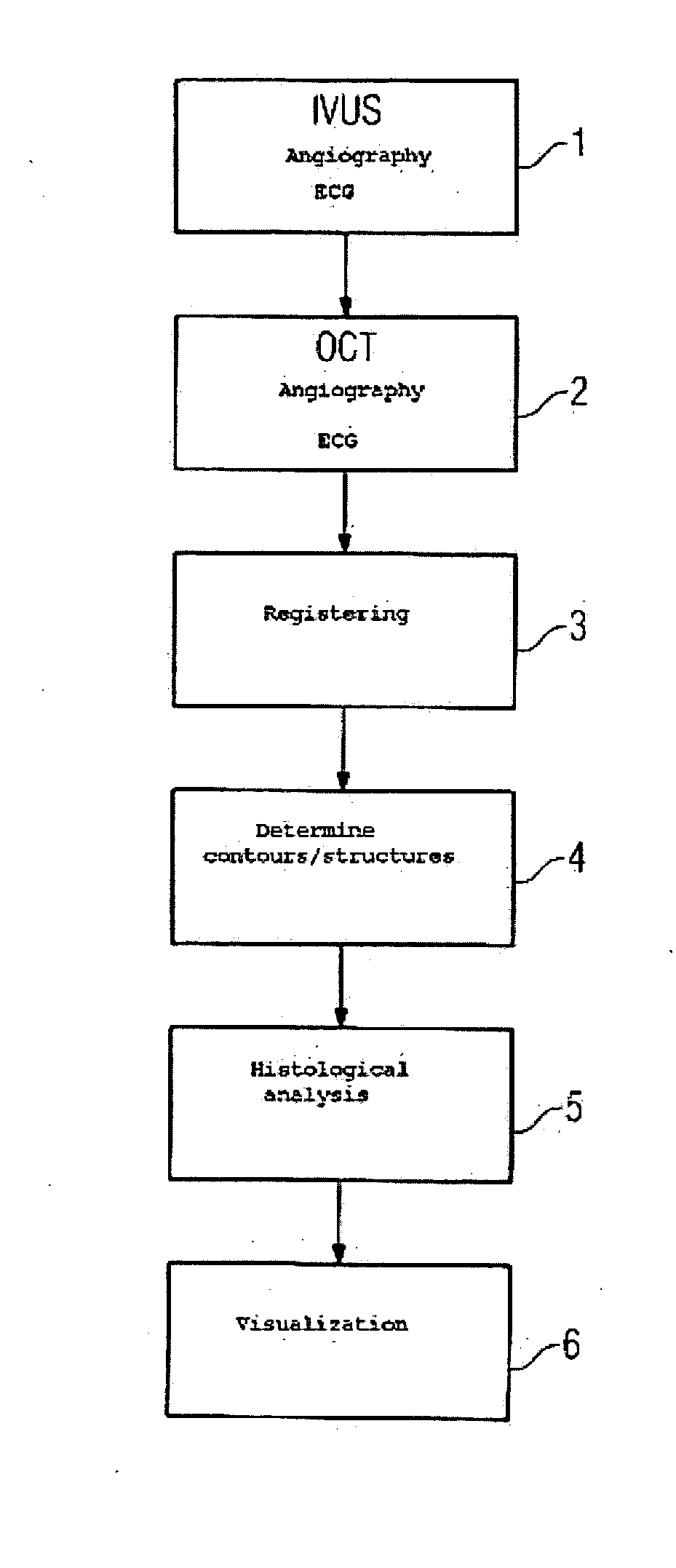
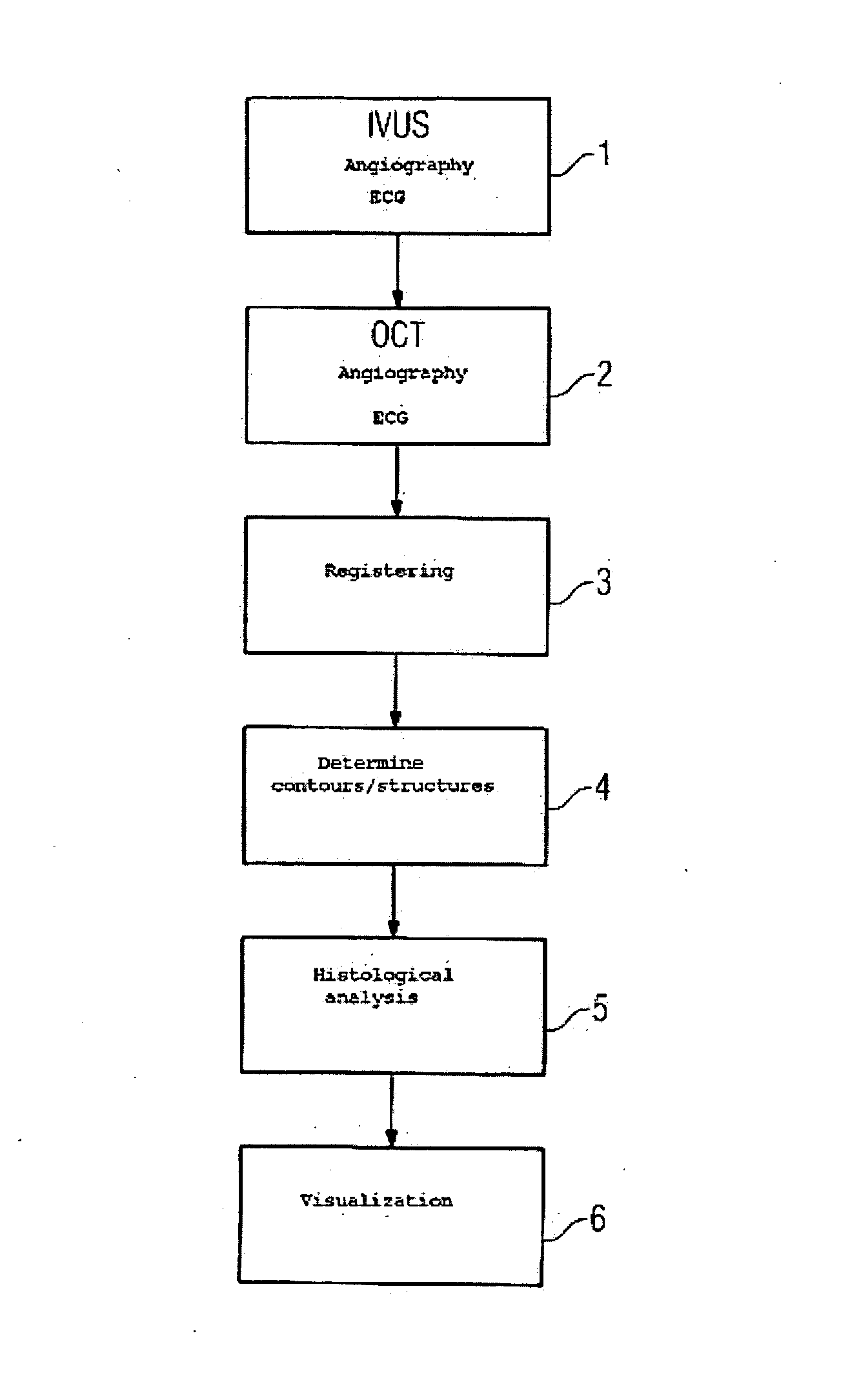
Method for acquiring and evaluating vascular examination data
InactiveUS20070043292A1Reliable and automatic analysisImprove accuracyUltrasonic/sonic/infrasonic diagnosticsSurgeryVascular structureBlood vessel
The invention relates to a method for acquiring and evaluating vascular examination data, comprising: acquisition of IVUS images of a vessel to be examined using an IVUS catheter; simultaneous acquisition of angiography data of the IVUS catheter having at least one angiography marker; acquisition of OCT images of the same point of the vessel to be examined using an OCT catheter; simultaneous acquisition of angiography data of the OCT catheter having at least one angiography marker; registering the IVUS and OCT images; determination of contours of the structures of the vessel under examination based on the OCT images; arithmetic histological analysis of the co-registered IVUS and OCT images using the information about the contours; and display the results.
Owner:SIEMENS AG
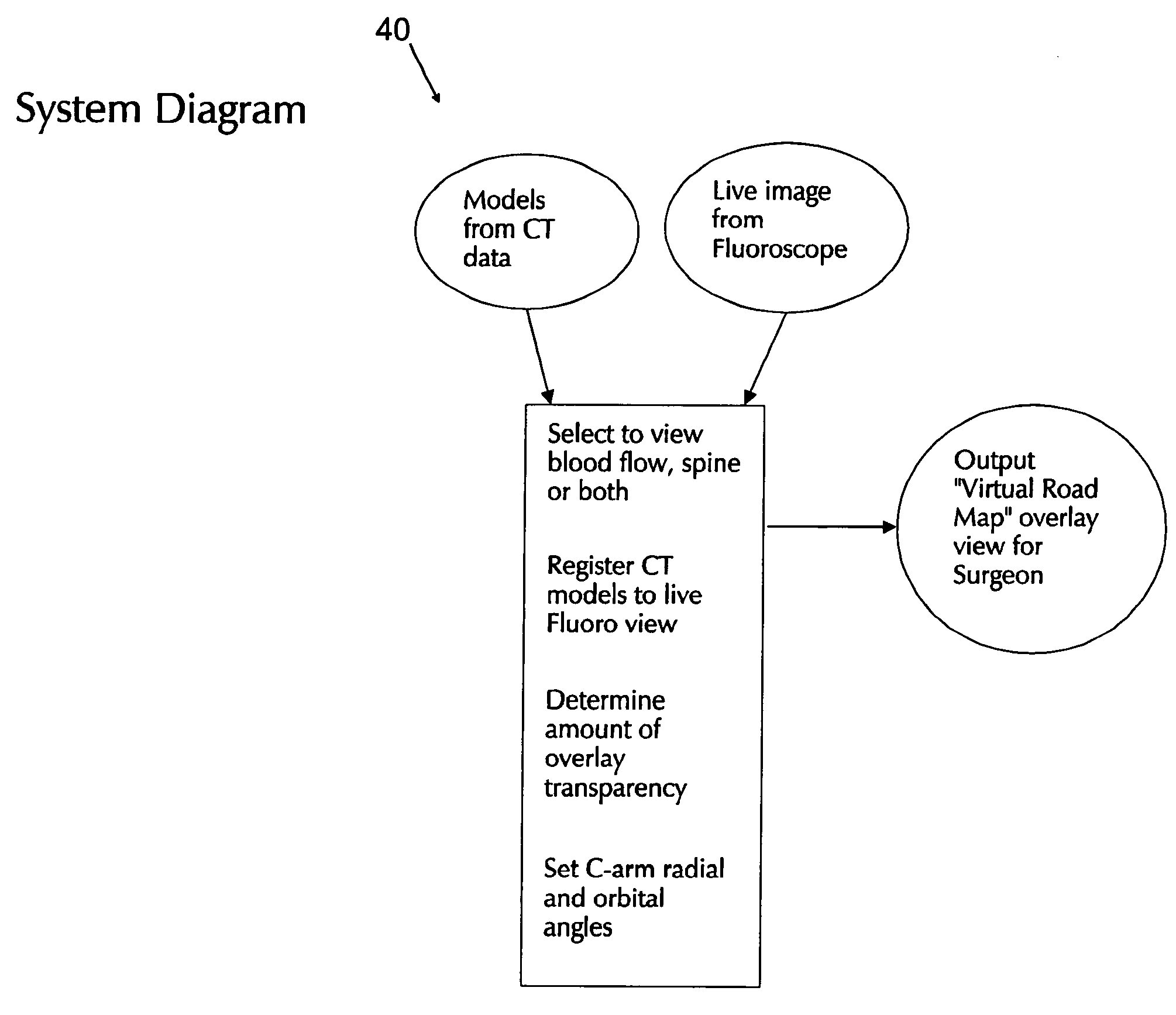
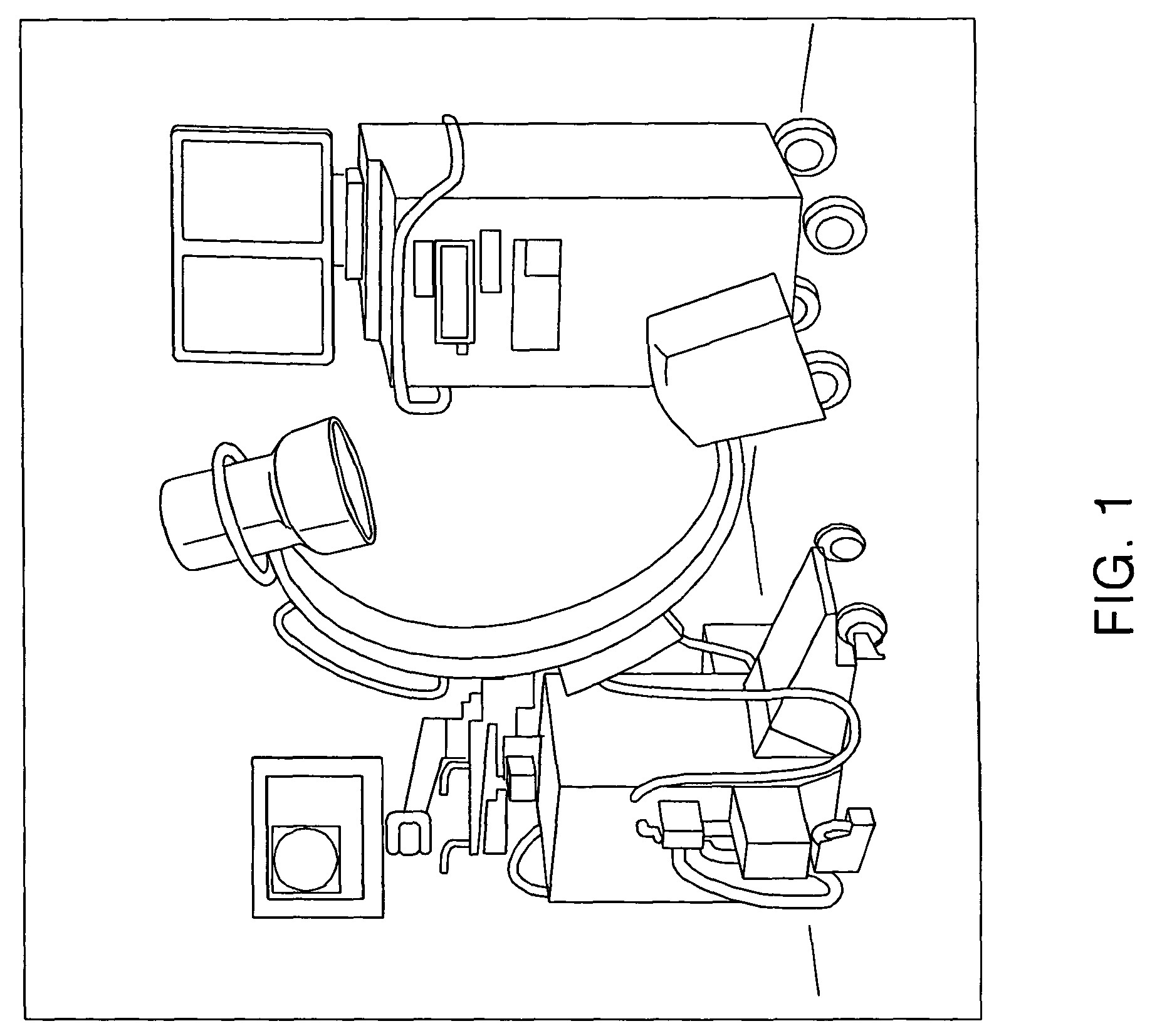
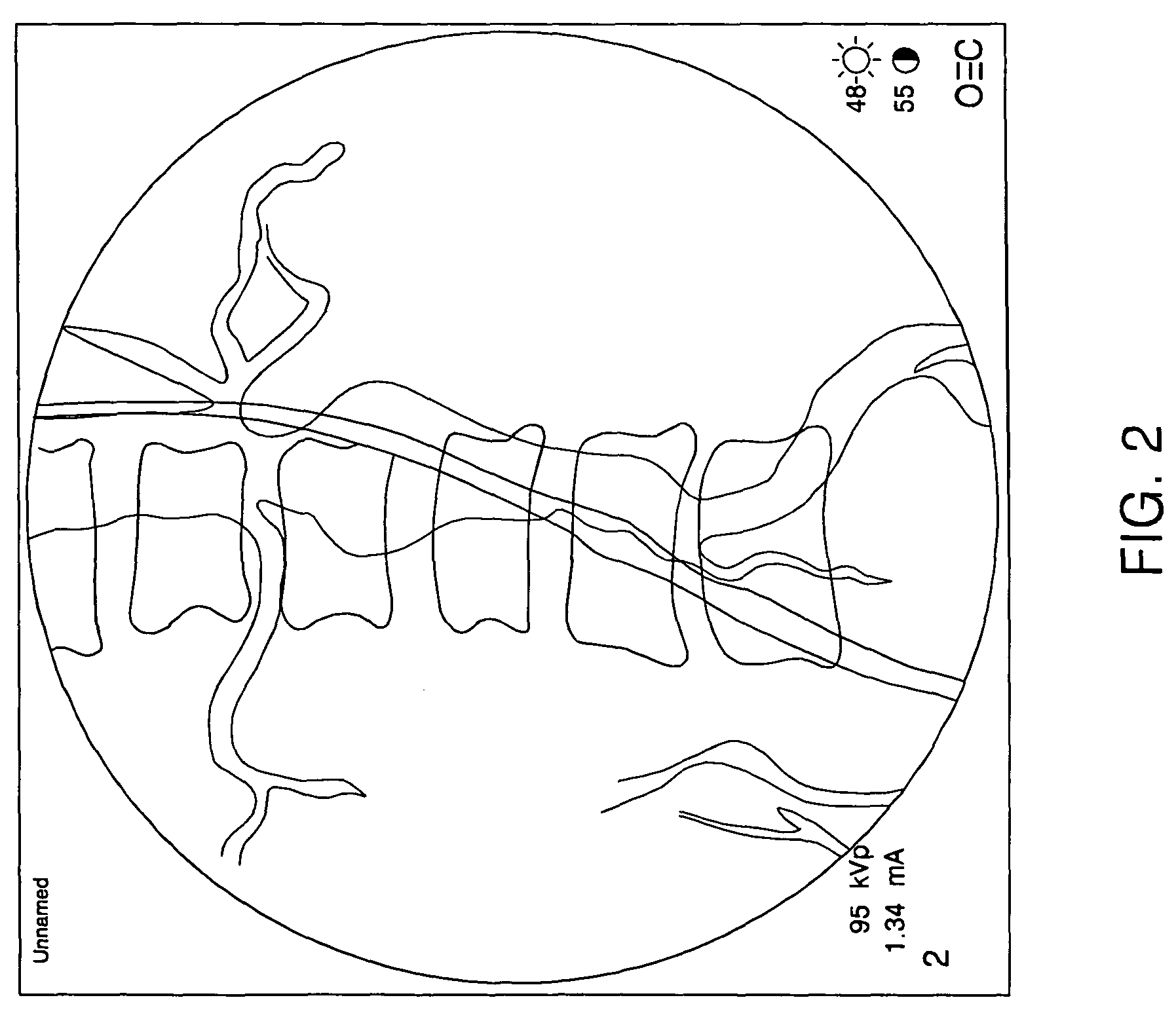
Method and apparatus for visualizing anatomical structures
Apparatus and method for producing a virtual road map of a patient's vascular anatomy comprising a virtual 3D model of the patient's vascular and bony structure in proper registration with one another, a fluoroscope for providing real-time images of the bony structure of the patient, registration apparatus for placing the virtual 3D model in proper registration with the patient space of the fluoroscope, bone mask subtraction apparatus for generating a bone mask of the bony structure, and subtracting the same from the real-time images, whereby to create modified fluoroscope images omitting bony structure, and image generating apparatus for generating the virtual road map comprising a composite image combining (i) images of the virtual 3D structure representing the vascular structure, and (ii) modified fluoroscope images omitting bony structure, wherein the images of the virtual 3D structure representing vascular structure are in proper registration with the modified fluoroscope images omitting bony structure.
Owner:ASTUTE IMAGING LLC
Devices and methods for selective surgical removal of tissue
ActiveUS20060094976A1Improve securityAvoid injuryCannulasAnti-incontinence devicesTissue remodelingLateral recess
Methods and apparatus are provided for selective surgical removal of tissue, e.g., for enlargement of diseased spinal structures, such as impinged lateral recesses and pathologically narrowed neural foramen. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. Once the sharp tip of the needle is in the epidural space, it is converted to a blunt tipped instrument for further safe advancement. A specially designed epidural catheter that is used to cover the previously sharp needle tip may also contain a fiberoptic cable. Further embodiments of the current invention include a double barreled epidural needle or other means for placement of a working channel for the placement of tools within the epidural space, beside the epidural instrument. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. In one variation, a tissue removal device is provided including a thin belt or ribbon with an abrasive cutting surface. The device may be placed through the neural foramina of the spine and around the anterior border of a facet joint. Once properly positioned, a medical practitioner may enlarge the lateral recess and neural foramina via frictional abrasion, i.e., by sliding the tissue removal surface of the ribbon across impinging tissues. A nerve stimulator optionally may be provided to reduce a risk of inadvertent neural abrasion. Additionally, safe epidural placement of the working barrier and epidural tissue modification tools may be further improved with the use of electrical nerve stimulation capabilities within the invention that, when combined with neural stimulation monitors, provide neural localization capabilities to the surgeon. The device optionally may be placed within a protective sheath that exposes the abrasive surface of the ribbon only in the area where tissue removal is desired. Furthermore, an endoscope may be incorporated into the device in order to monitor safe tissue removal. Finally, tissue remodeling within the epidural space may be ensured through the placement of compression dressings against remodeled tissue surfaces, or through the placement of tissue retention straps, belts or cables that are wrapped around and pull under tension aspects of the impinging soft tissue and bone in the posterior spinal canal.
Owner:SPINAL ELEMENTS INC +1
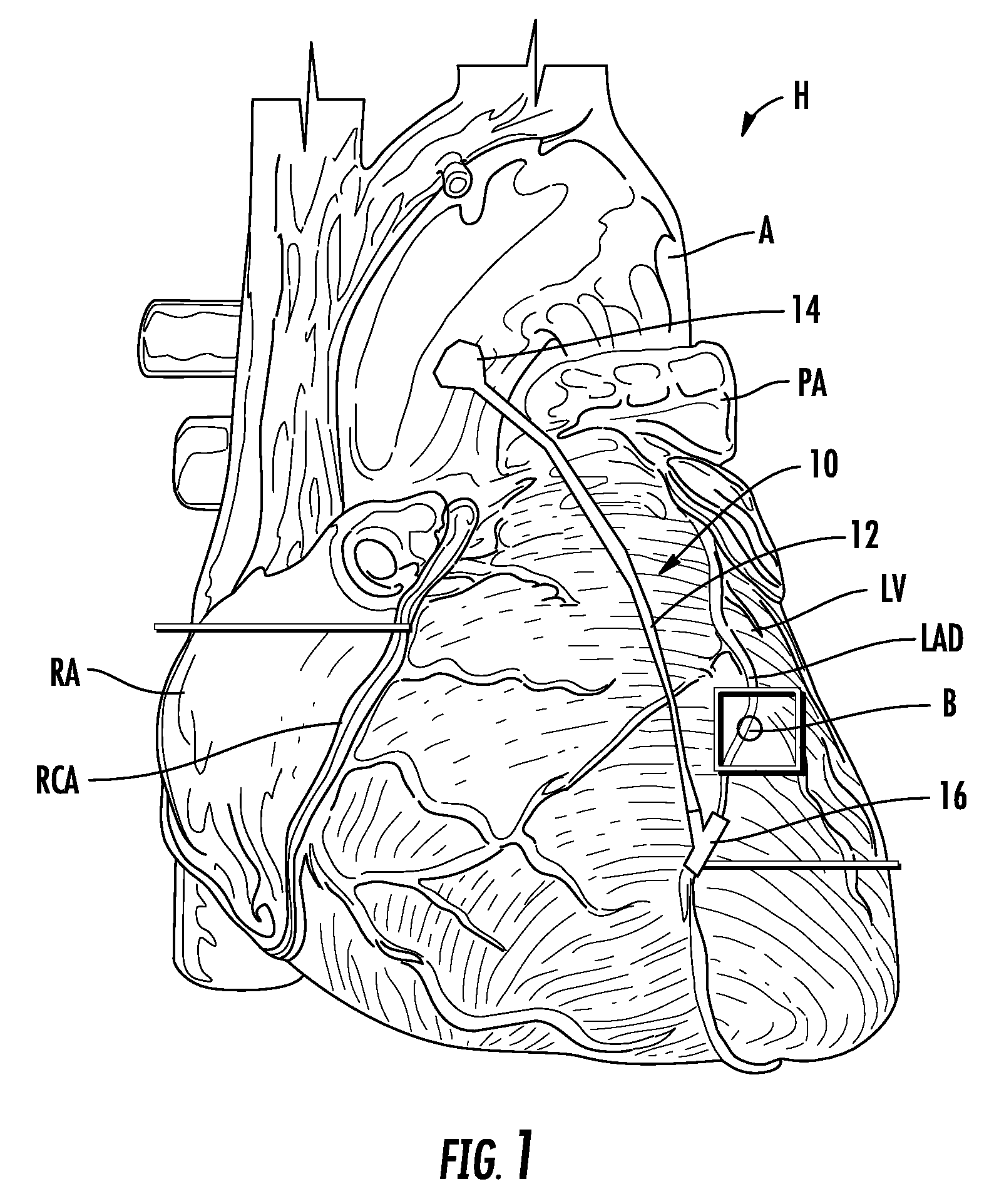
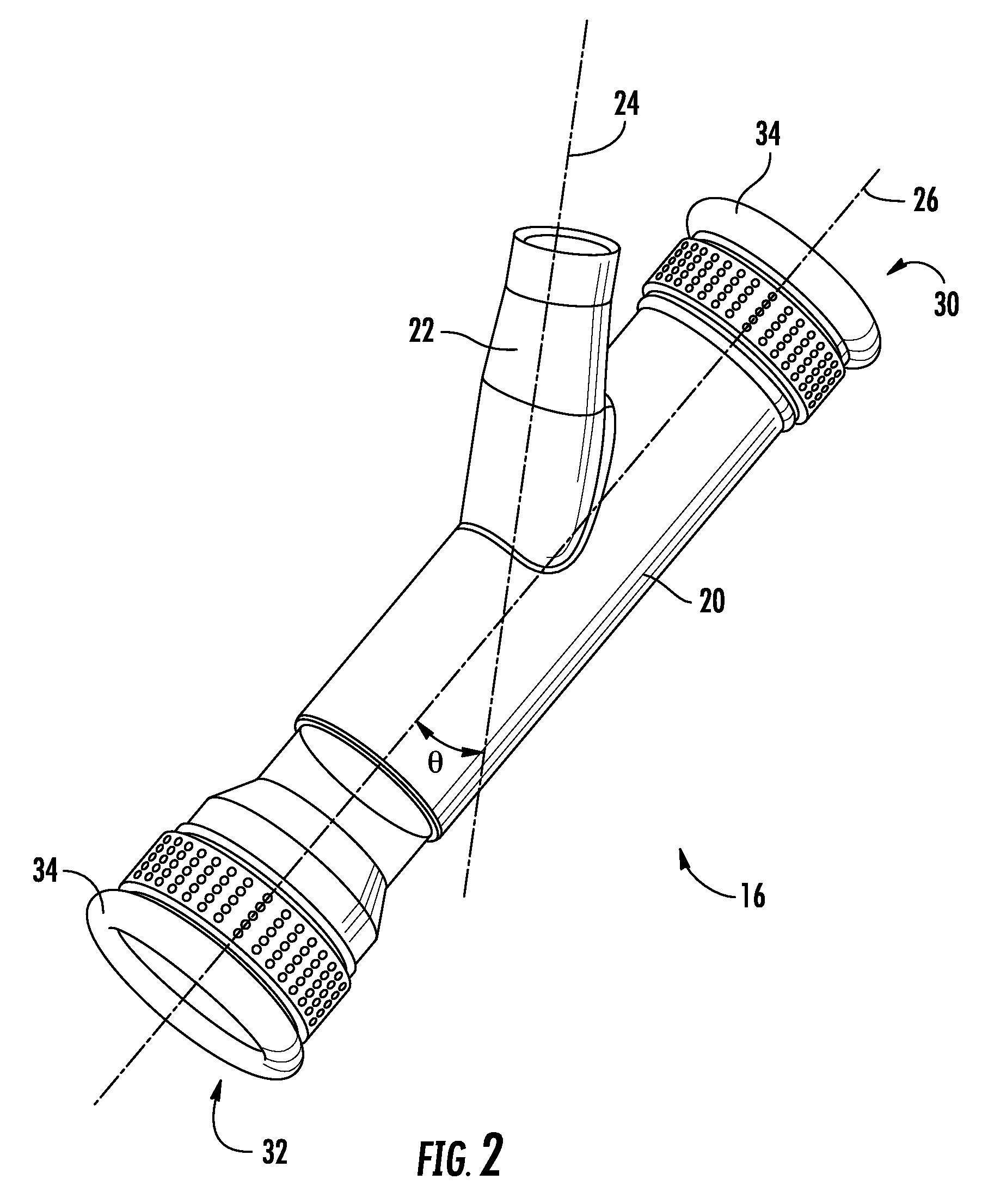
Method and apparatus for bypass graft
InactiveUS20090076531A1Well mixedAuscultation instrumentsBlood vesselsBypass graftsVascular structure
A vascular connector includes a main tube having a channel for fluid flow therethrough and opposed ends adapted to be connected to a vascular structure; and at least one inlet tube having a channel for fluid flow therethrough, a proximal end intersecting the main tube, and a distal end adapted to be connected to a vascular structure.
Owner:RICHARDSON CHARLES L +2
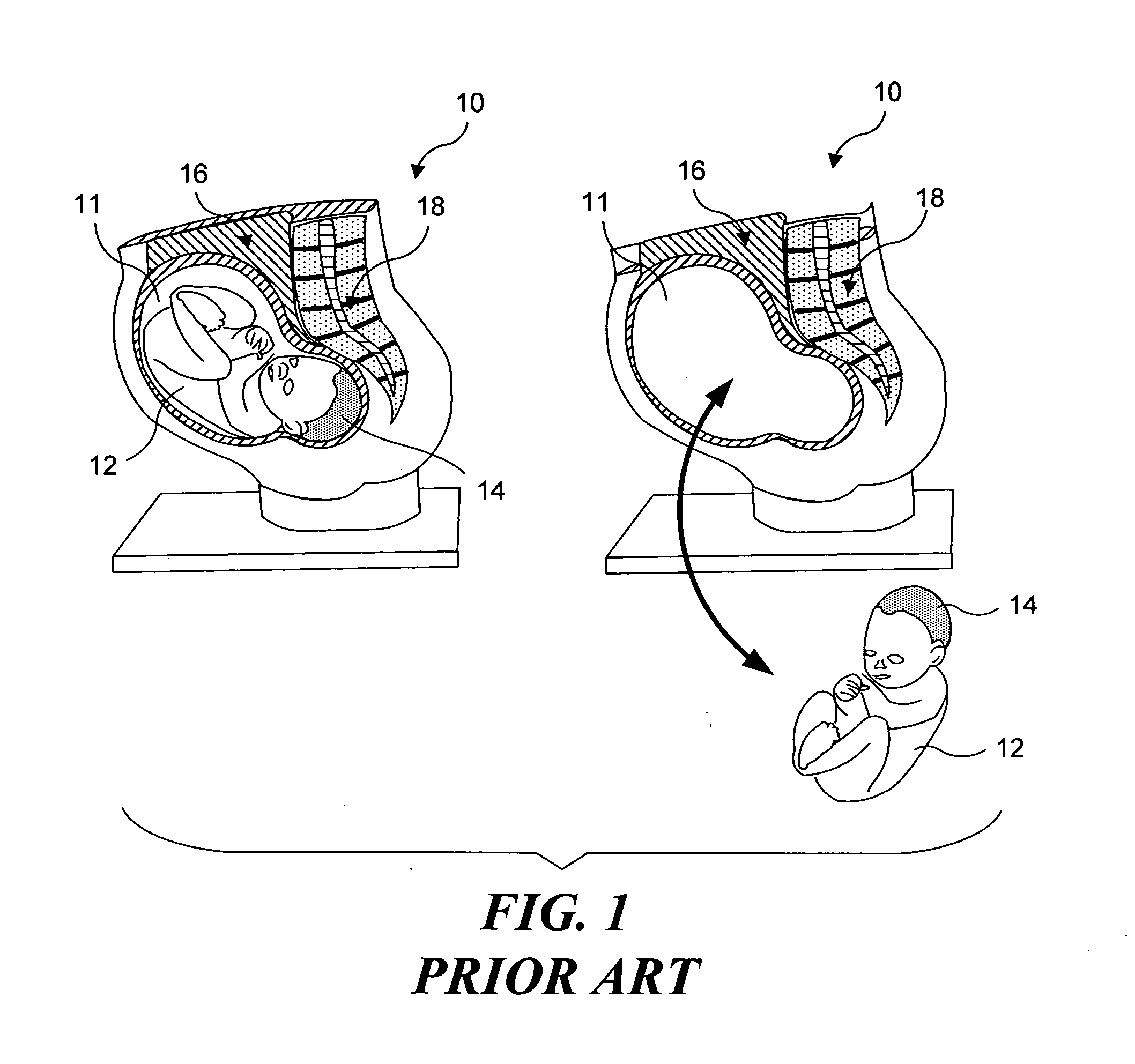
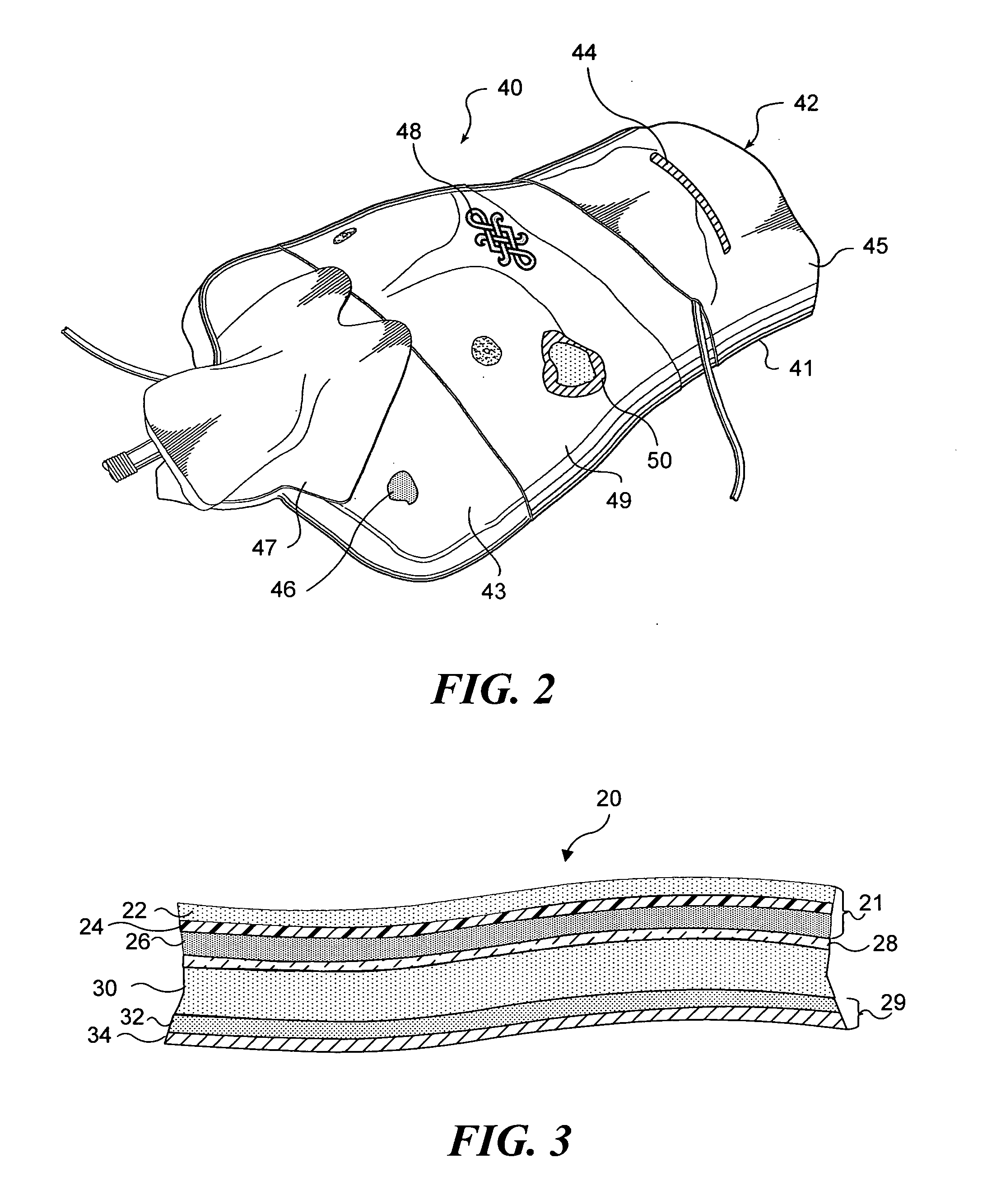
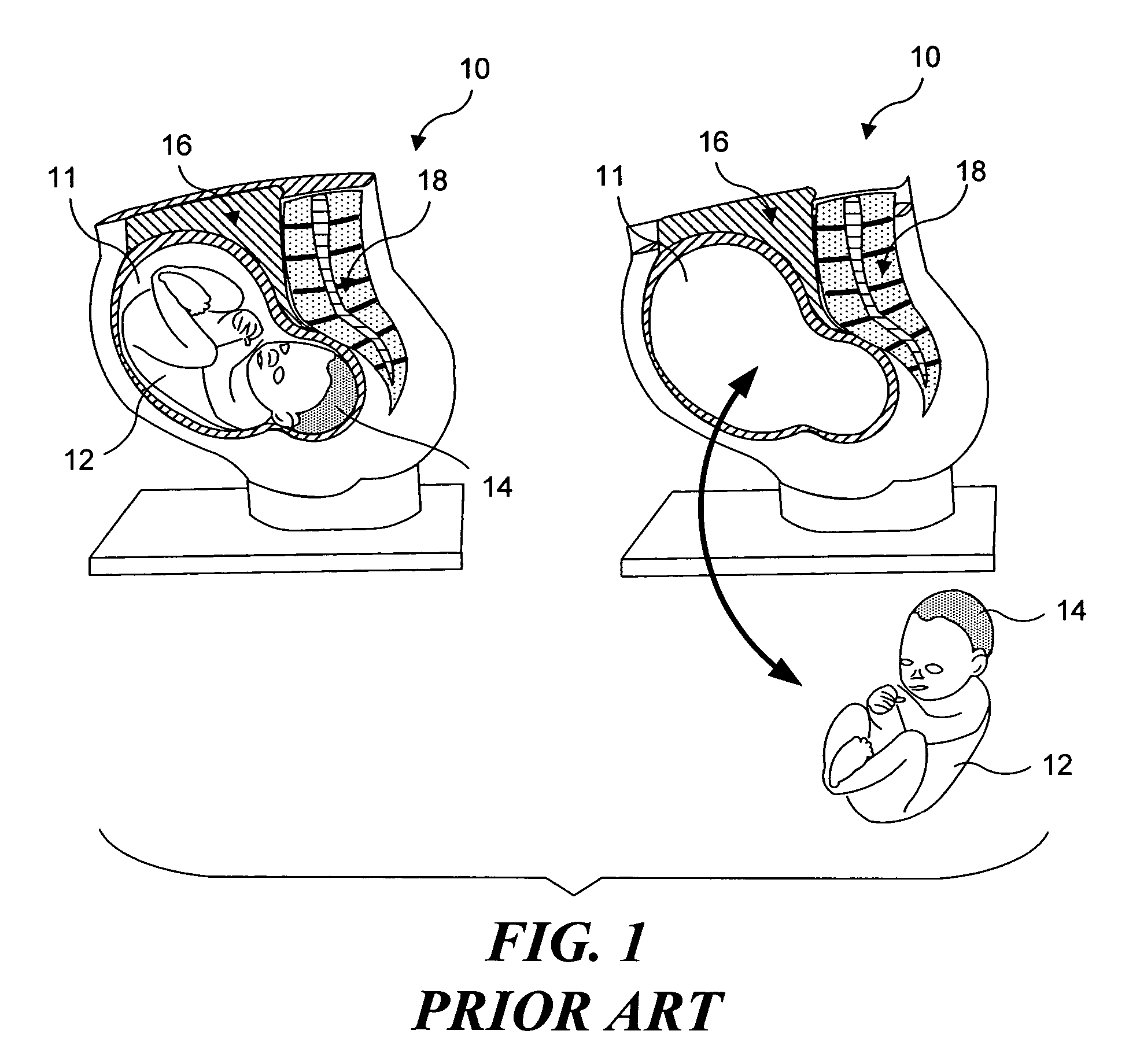
Simulated anatomical structures incorporating an embedded image layer
ActiveUS20050026125A1Improve realismMore resistantEducational modelsAnatomical structuresVascular structure
A simulated physiological structure includes an image layer configured to enhance a visual appearance of the simulated physiological structure. The image layer includes a substrate onto which an image has been printed. Preferably, the substrate is a relatively thin layer, compared to other layers of material in the simulated physiological structure. Where the simulated physiological structure includes surface irregularities, the substrate is preferably sufficiently thin so as to be able to readily conform to the surface irregularities. Particularly preferred substrates include fabrics, fibrous materials, meshes, and plastic sheets. The image, which can be of an actual anatomical element, or a rendering of an anatomical element, is transferred onto the substrate using conventional printing technologies, including ink jet printing. Particularly preferred images illustrate vascular structures and disease conditions. Preferably, the substrate is coupled to an elastomeric material that forms at least part of the simulated physiological structure.
Owner:TOLY CHRISTOPHER C
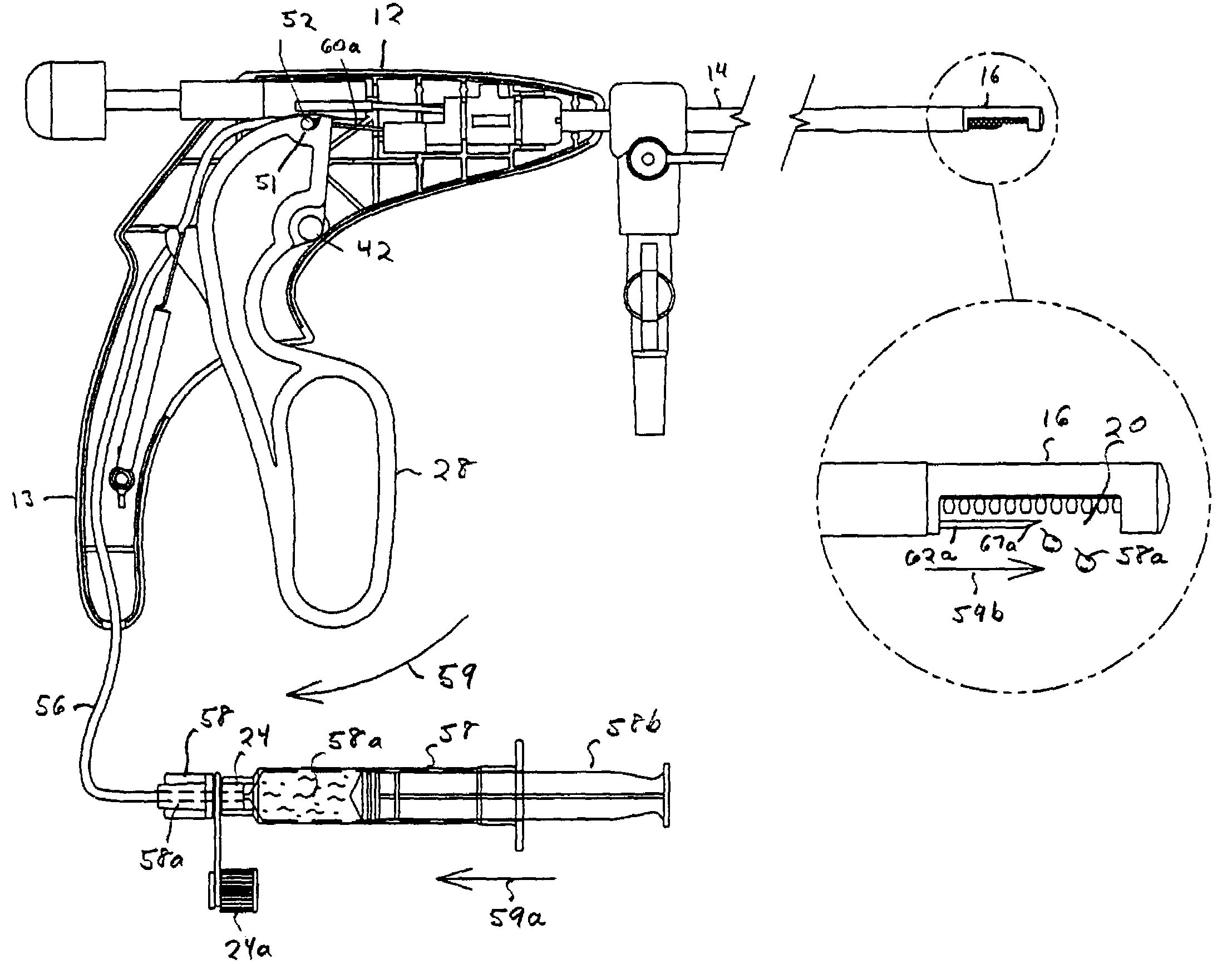
Instrument for surgically cutting tissue and method of use
InactiveUS7481817B2Easy diagnosisFacilitates accurate appositionSurgical needlesVaccination/ovulation diagnosticsVia incisionVascular structure
An instrument for precisely cutting tissue to controlled dimensions (length, width, depth, and shape) is provided for the removal of tissue specimens from remote sites in the body of a patient, such as from the gastrointestinal tract, urinary tract, or vascular structures, or any tissue surface or soft tissue of the body. The instrument has a housing and a substantially flexible shaft extending from the housing to a distal end. The distal end of the instrument has an open cavity into which tissue is receivable. Suction can be communicated along the shaft to the distal end for distribution across the cavity utilizing a manifold having a grated tissue engaging surface with opening(s) for applying the suction, thereby pulling tissue adjacent to the distal end into the cavity against the tissue engaging surface of the manifold. One or more hollow needles are extendable from the housing through the shaft into the cavity to enable infusion of fluid, such as saline or a hemostatic agent, into the tissue. A blade in the distal end is extendable through the cavity over the manifold and across the opening to cut the tissue held by suction and stabilized by the needles in the cavity. The shape and depth of the tissue removed by the cuts is in accordance with the contour of the tissue engaging surface and the size and shape of the cavity at the distal end. The tissue so removed by the instrument may be for therapeutic intervention and / or represent a tissue specimen for biopsy suitable of diagnostic evaluation. The tissue edges in the patient's body left after cutting with this instrument readily avail themselves to apposition for enhanced healing.
Owner:LSI SOLUTIONS
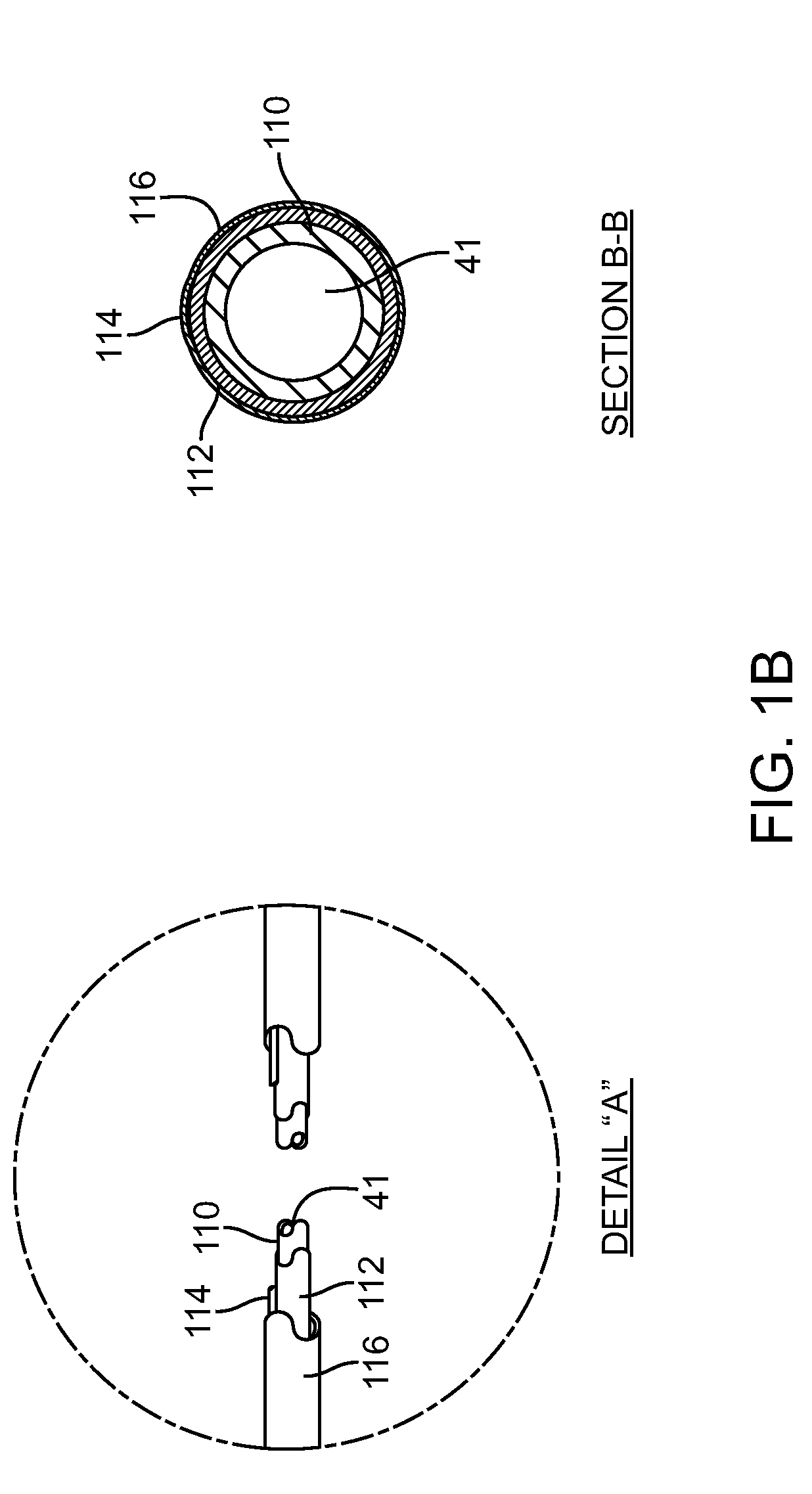
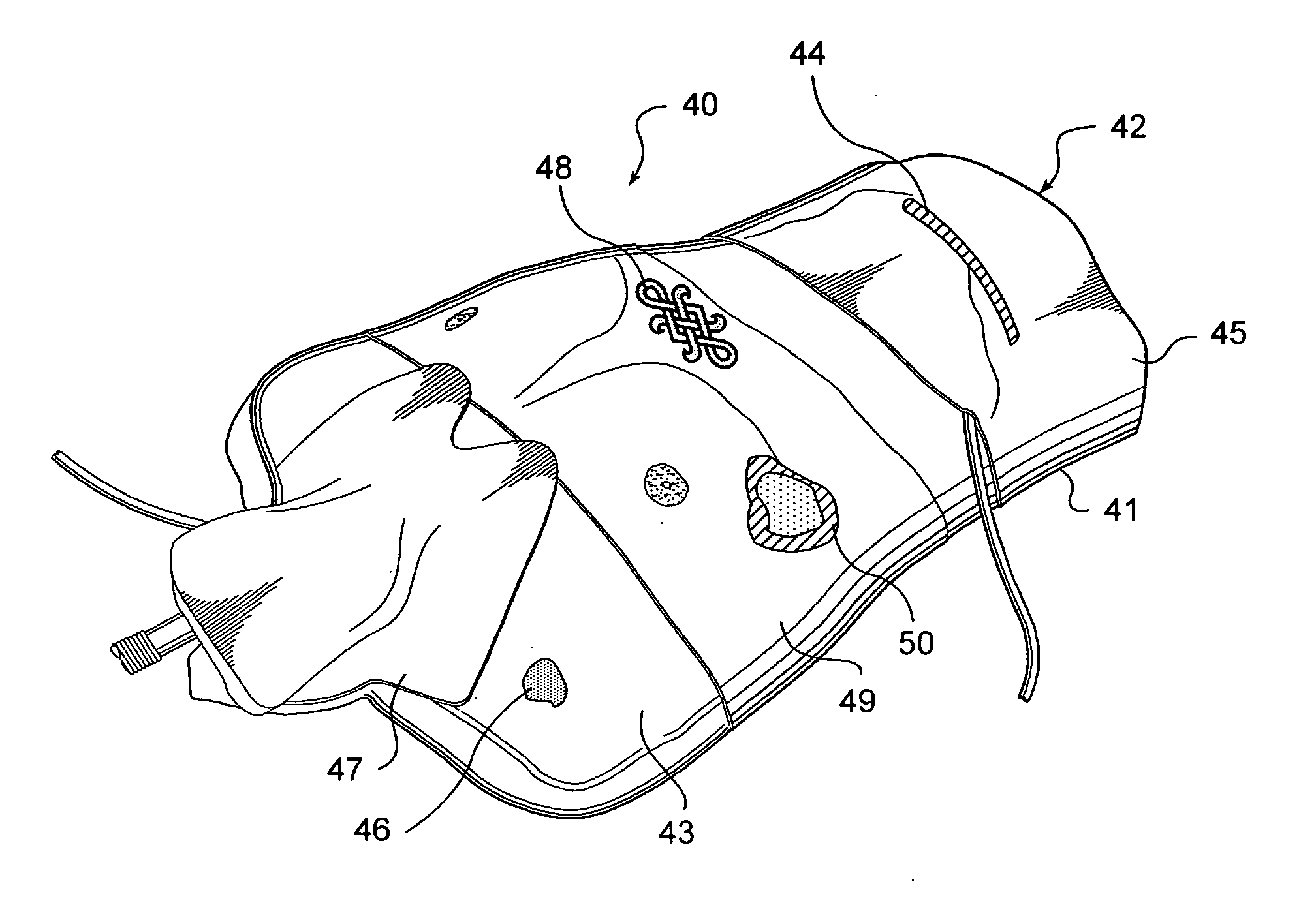
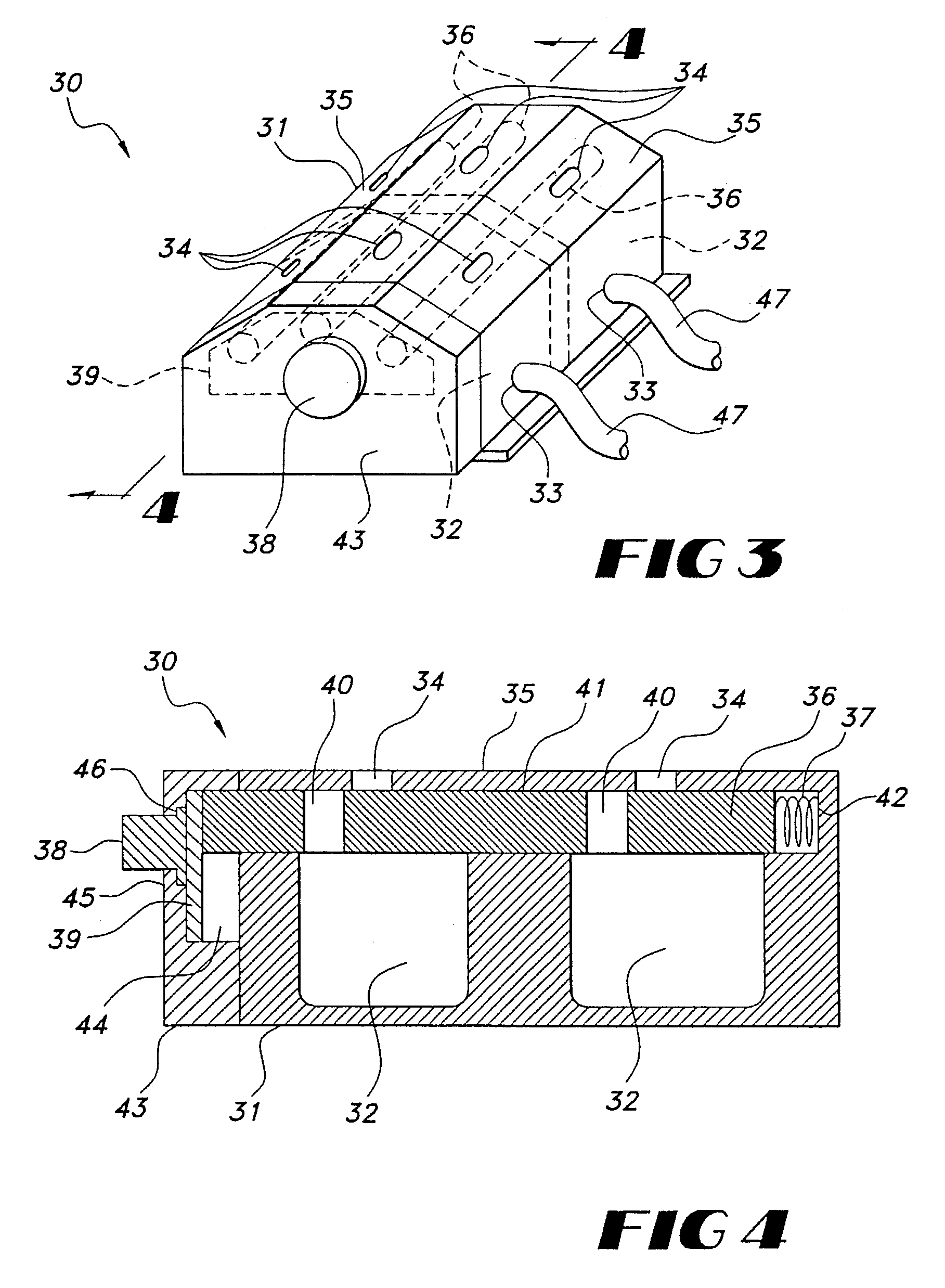
Implantable vascular access device
InactiveUS7252649B2Increase the number ofWithout deteriorationMedical devicesPharmaceutical delivery mechanismVascular Access DevicesSubcutaneous implantation
An implantable vascular access device includes a housing having an inlet, an outlet, an interior chamber defined therein and a valve positioned between the inlet and the interior chamber. The valve is subcutaneously manipulated between an open position, in which fluid can flow between the inlet and the interior chamber, and a closed position in which the valve occludes the inlet. The device may include any combination of multiple inlets, outlets and / or interior chambers. In the preferred embodiment, the housing includes two separate interior chambers suitable for the inflow and outflow of a typical hemodialysis procedure. A method for accessing a vascular structure is provided which includes the steps of subcutaneously implanting the device connecting one end of a cannula to the outlet of the device and another end of the cannula to a selected vascular structure. The valve of the device is manipulated to permit fluid communication between the inlet of the device and the selected vascular structure. A needle is introduced through the inlet opening to access the selected vascular structure.
Owner:NAVILYST MEDICAL
Use of an adhesive as an intestinal barrier for bariatrics
An apparatus for achieving weight loss in a patient is disclosed. The apparatus has a barrier material and an applicator for dispensing the barrier material about the intestine. An injector is used to place the barrier material to block nutrient transfer from the intestine into the blood stream. The barrier material is a polymerizable adhesive that can be injected interstitially between layers of the intestine, or injected into vascular structures to partially block the flow of blood to the nutrient absorbing layers.
Owner:ETHICON ENDO SURGERY INC
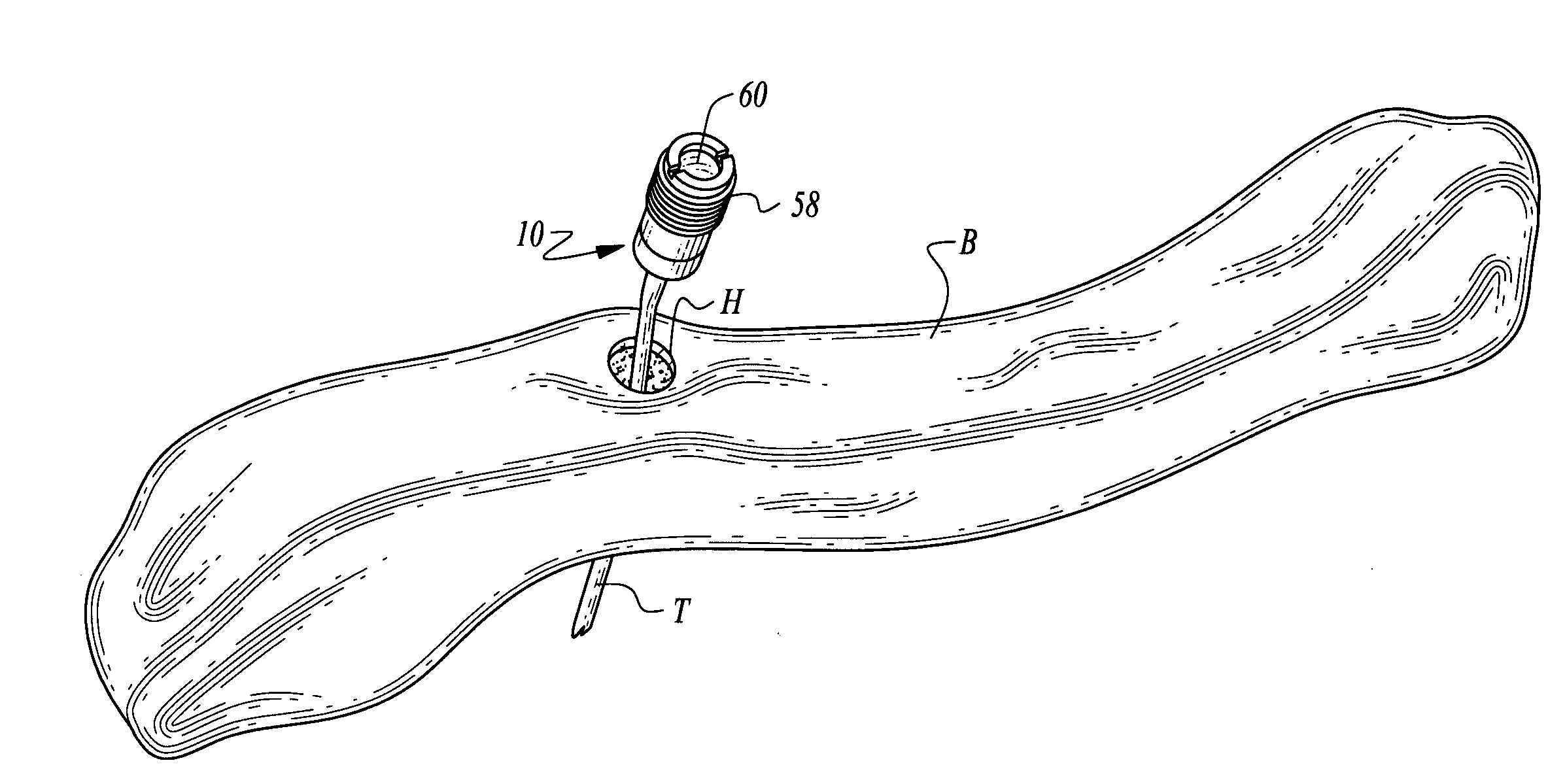
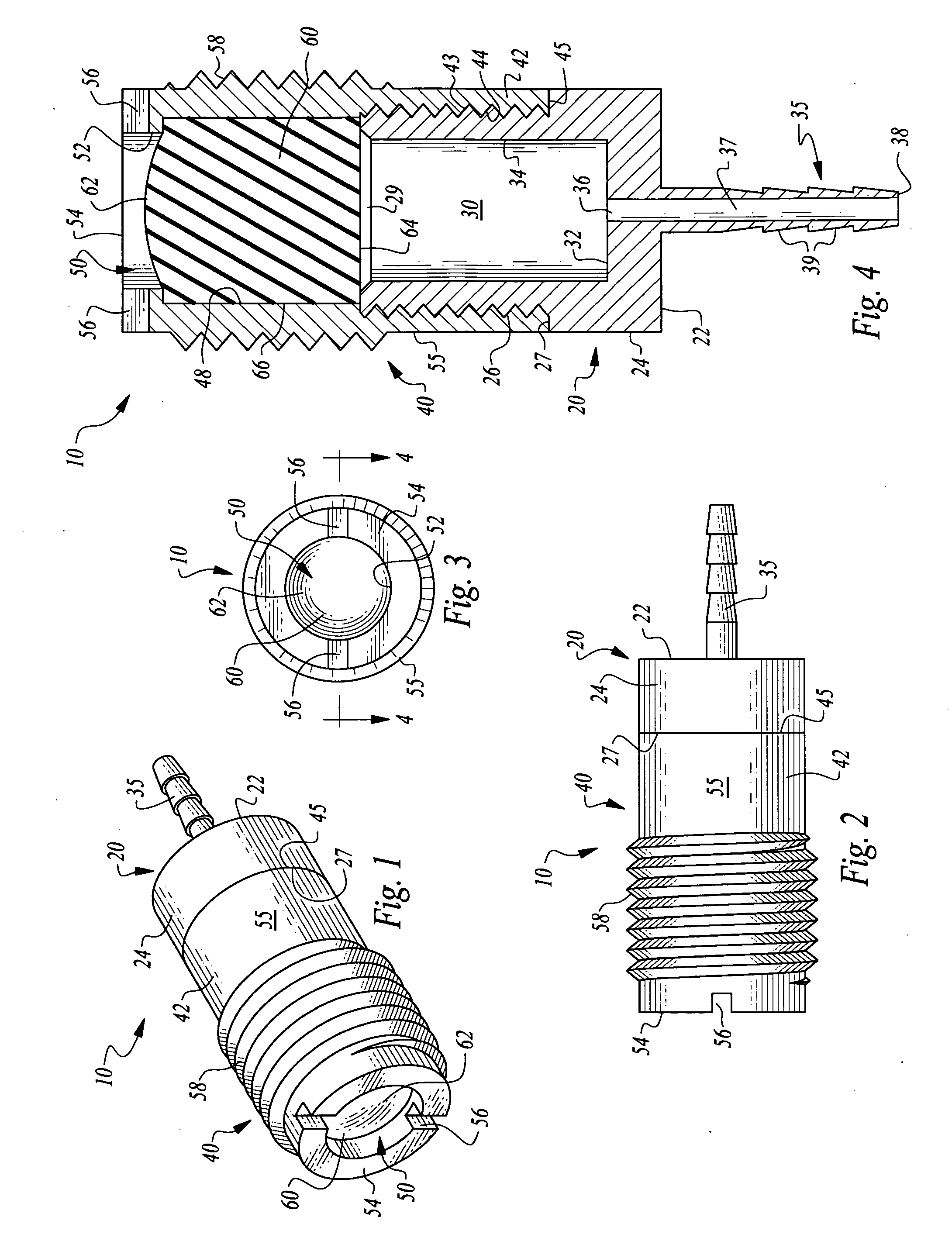
Bone supported vascular access port
InactiveUS20070179456A1Easy to disassembleSecurely holdSurgical needlesMedical devicesVisibilitySubcutaneous implantation
A vascular access port is disclosed for subcutaneous implantation. The port is particularly adapted to be affixed to a bone to securely hold the port in position, to assist medical personnel in finding the port and to decrease a visibility of the port. The port has a chamber therein which is accessed by a needle through a septum adjacent the chamber. The chamber is placed into fluid communication with the vascular structure of the patient, such as through catheter tubing. The chamber is surrounded by a body with an outer surface which is preferably fitted with threads to facilitate secure but removable attachment of the port within a hole in the bone where the port is to be implanted.
Owner:GLENN BRADLEY J
Simulated anatomical structures incorporating an embedded image layer
A simulated physiological structure includes an image layer configured to enhance a visual appearance of the simulated physiological structure. The image layer includes a substrate onto which an image has been printed. Preferably, the substrate is a relatively thin layer, compared to other layers of material in the simulated physiological structure. Where the simulated physiological structure includes surface irregularities, the substrate is preferably sufficiently thin so as to be able to readily conform to the surface irregularities. Particularly preferred substrates include fabrics, fibrous materials, meshes, and plastic sheets. The image, which can be of an actual anatomical element, or a rendering of an anatomical element, is transferred onto the substrate using conventional printing technologies, including ink jet printing. Particularly preferred images illustrate vascular structures and disease conditions. Preferably, the substrate is coupled to an elastomeric material that forms at least part of the simulated physiological structure.
Owner:TOLY CHRISTOPHER C
Devices and methods for selective surgical removal of tissue
ActiveUS20090125036A1Improve securityAvoid injuryCannulasAnti-incontinence devicesSurgical removalVascular structure
Methods and apparatus are provided for selective surgical removal of tissue. In one variation, tissue may be ablated, resected, removed, or otherwise remodeled by standard small endoscopic tools delivered into the epidural space through an epidural needle. The sharp tip of the needle in the epidural space, can be converted to a blunt tipped instrument for further safe advancement. The current invention includes specific tools that enable safe tissue modification in the epidural space, including a barrier that separates the area where tissue modification will take place from adjacent vulnerable neural and vascular structures. A nerve stimulator may be provided to reduce a risk of inadvertent neural abrasion.
Owner:MIS IP HLDG LLC +1
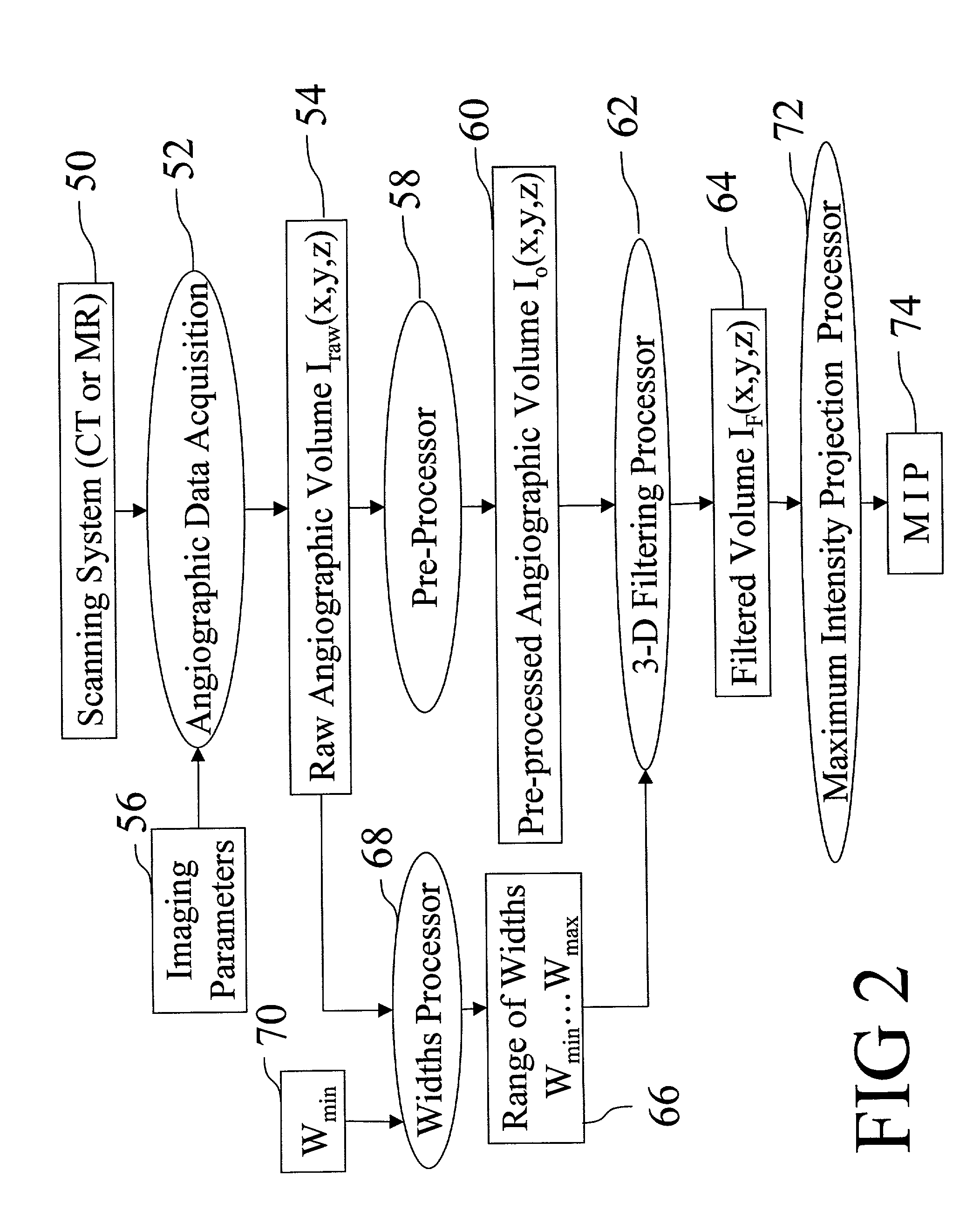
Method and apparatus for three-dimensional filtering of angiographic volume data
InactiveUS7024027B1Eliminate confusionRemove obscuring non-vascular contrastCharacter and pattern recognitionDiagnostic recording/measuringComputer visionVascular structure
A filtering method and apparatus for selectively filtering a gray scale angiographic image volume (54) that images vascular structures and that also contains extraneous non-vascular contrast is disclosed. A minimum vessel width parameter Wmin (70) is selected. A maximum vessel width parameter Wmax (132) is selected. A range of widths (66) are selected such that each vessel width parameter Wi (194) lies between Wmin (70) and Wmax (132) inclusive. For each Wi (194), an image Ii(x,y,z) (198) is generated that selectively retains imaged vascular structures of diameter Wi (194). The images Ii(x,y,z) (198) are combined to form a filtered image IF(x,y,z) (64) that selectively images the vascular structures.
Owner:KONINKLIJKE PHILIPS ELECTRONICS NV +1
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com