Patents
Literature
Hiro is an intelligent assistant for R&D personnel, combined with Patent DNA, to facilitate innovative research.
616 results about "Artificial joints" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
More women and men are turning to artificial joints for a second lease on an active life. By Gina Shaw. ... WebMD does not provide medical advice, diagnosis or treatment.
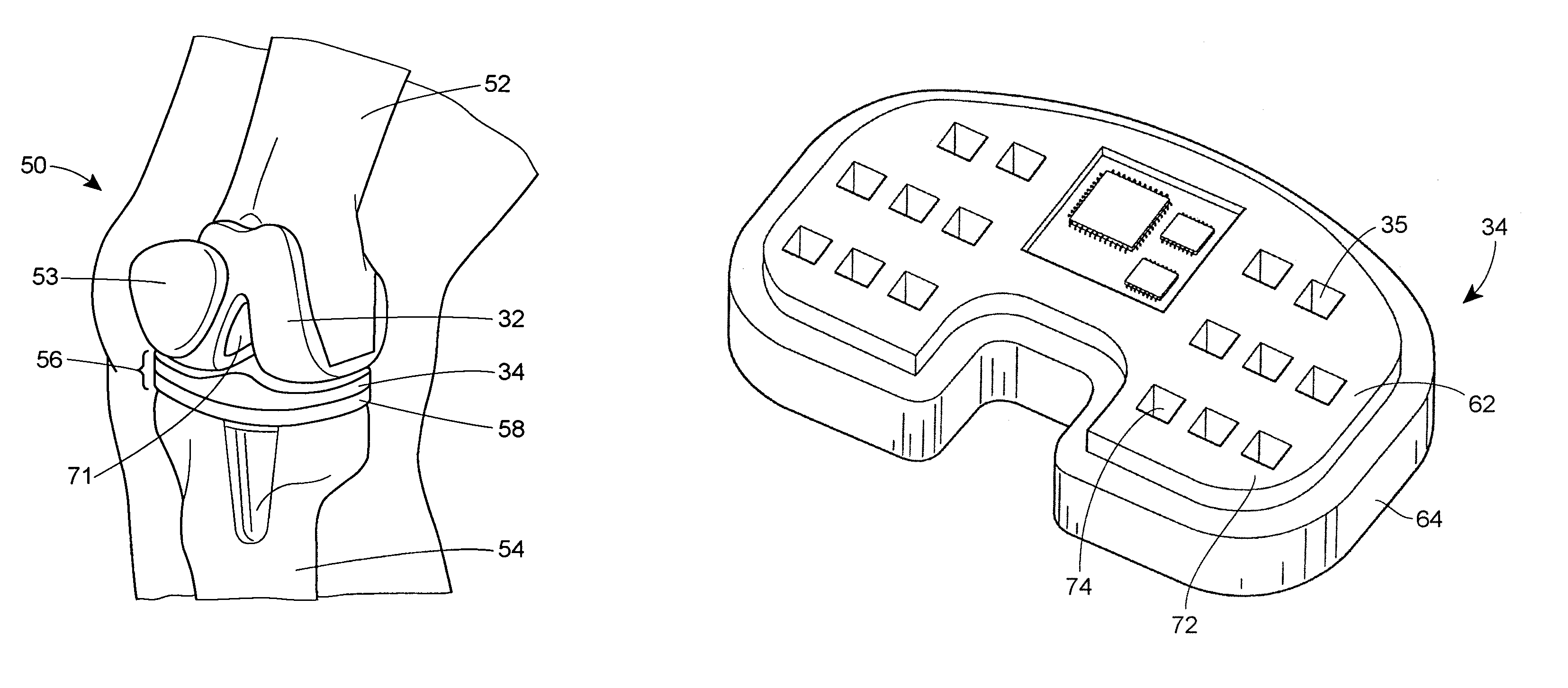
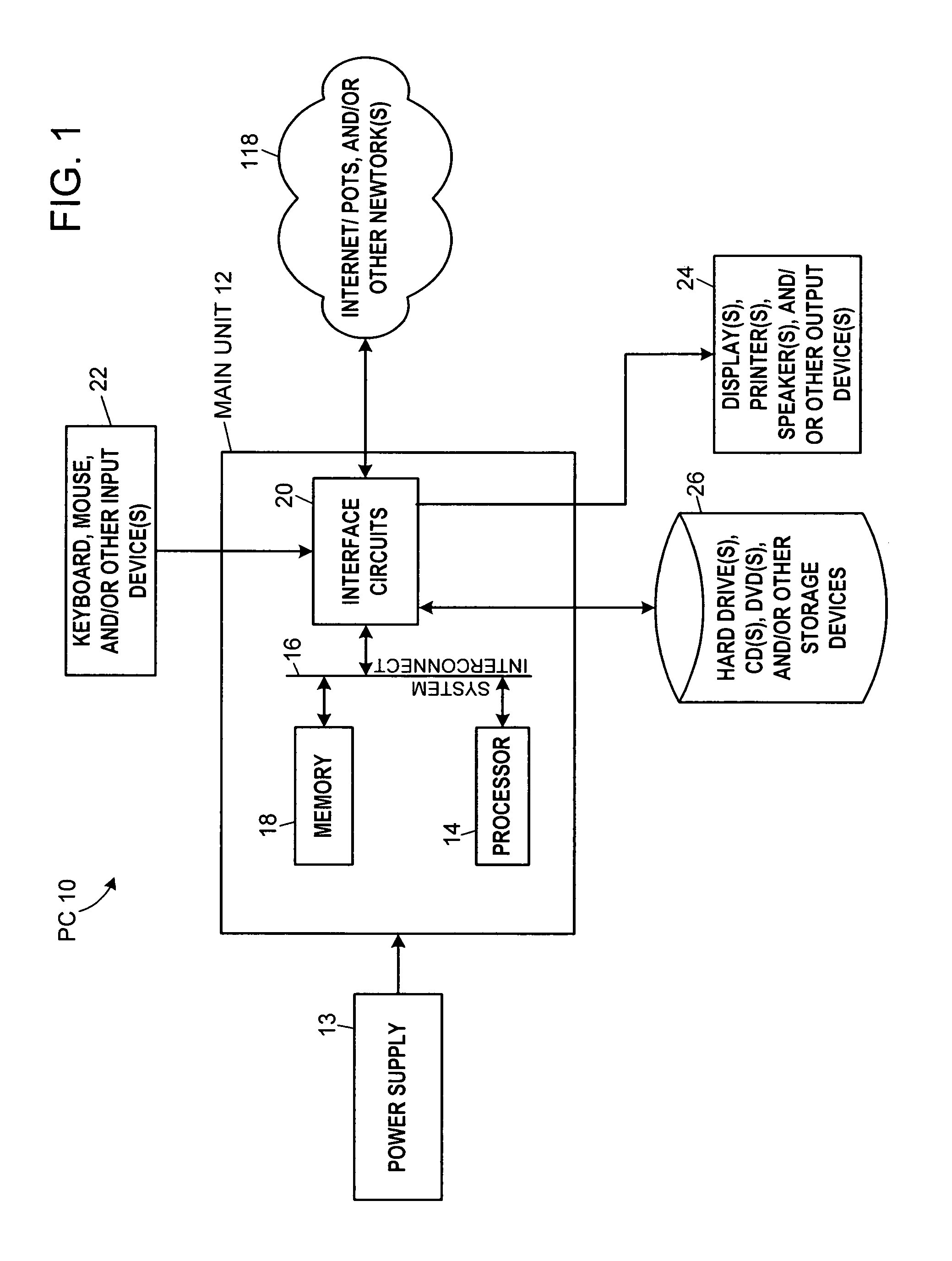
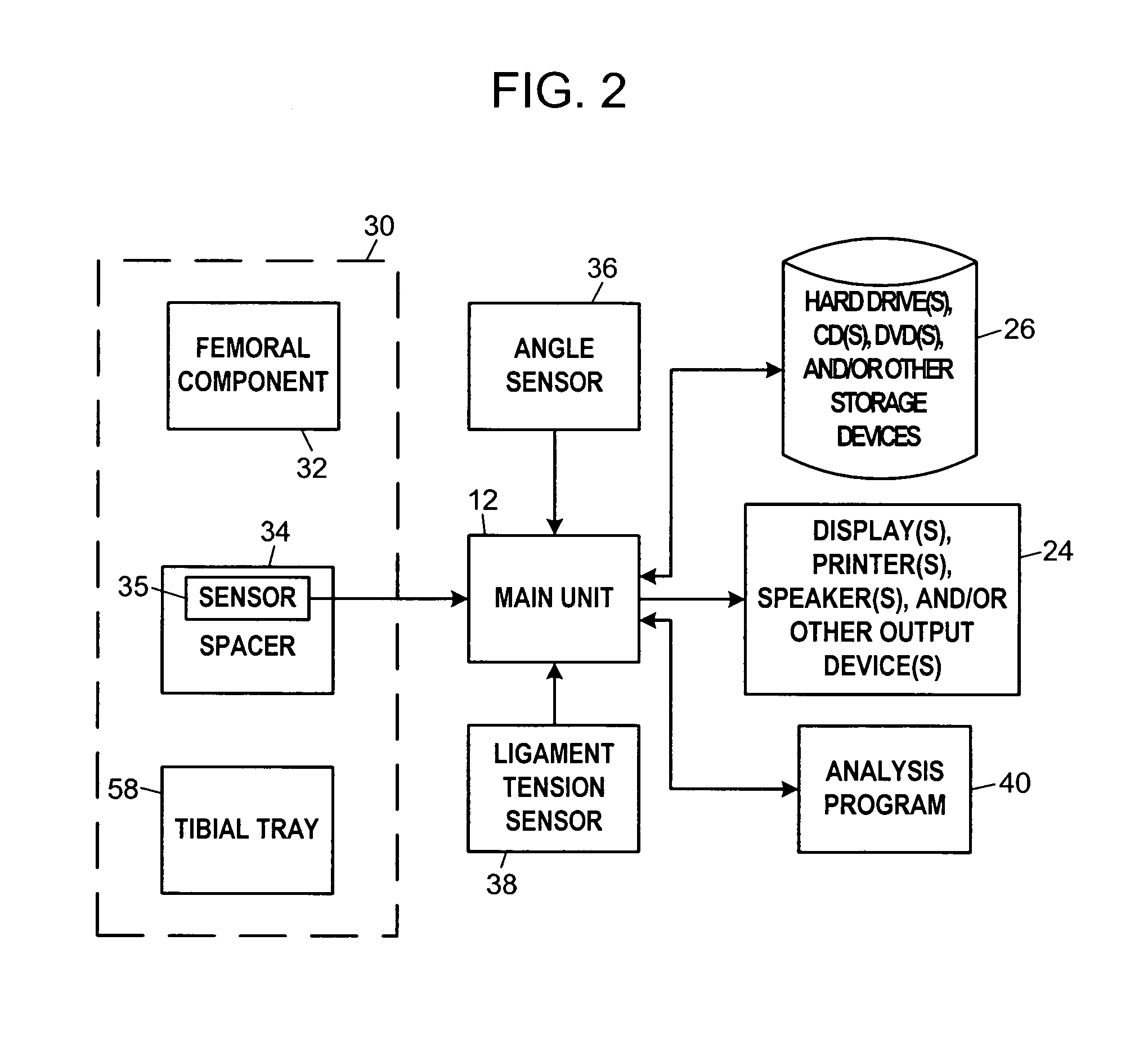
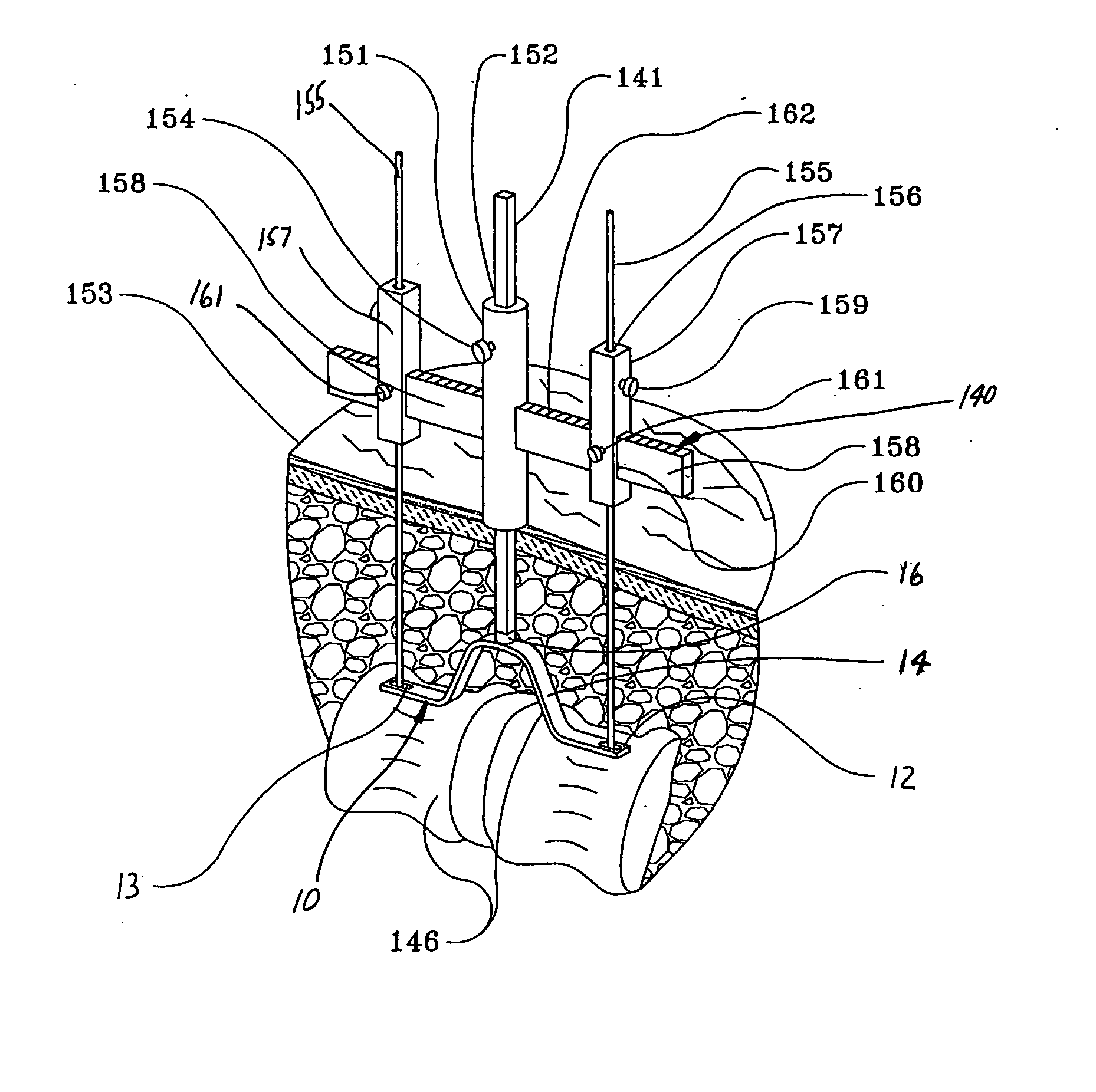
System and method for prosthetic fitting and balancing in joints
InactiveUS7575602B2Physical therapies and activitiesFinger jointsProsthesis fittingArtificial joints
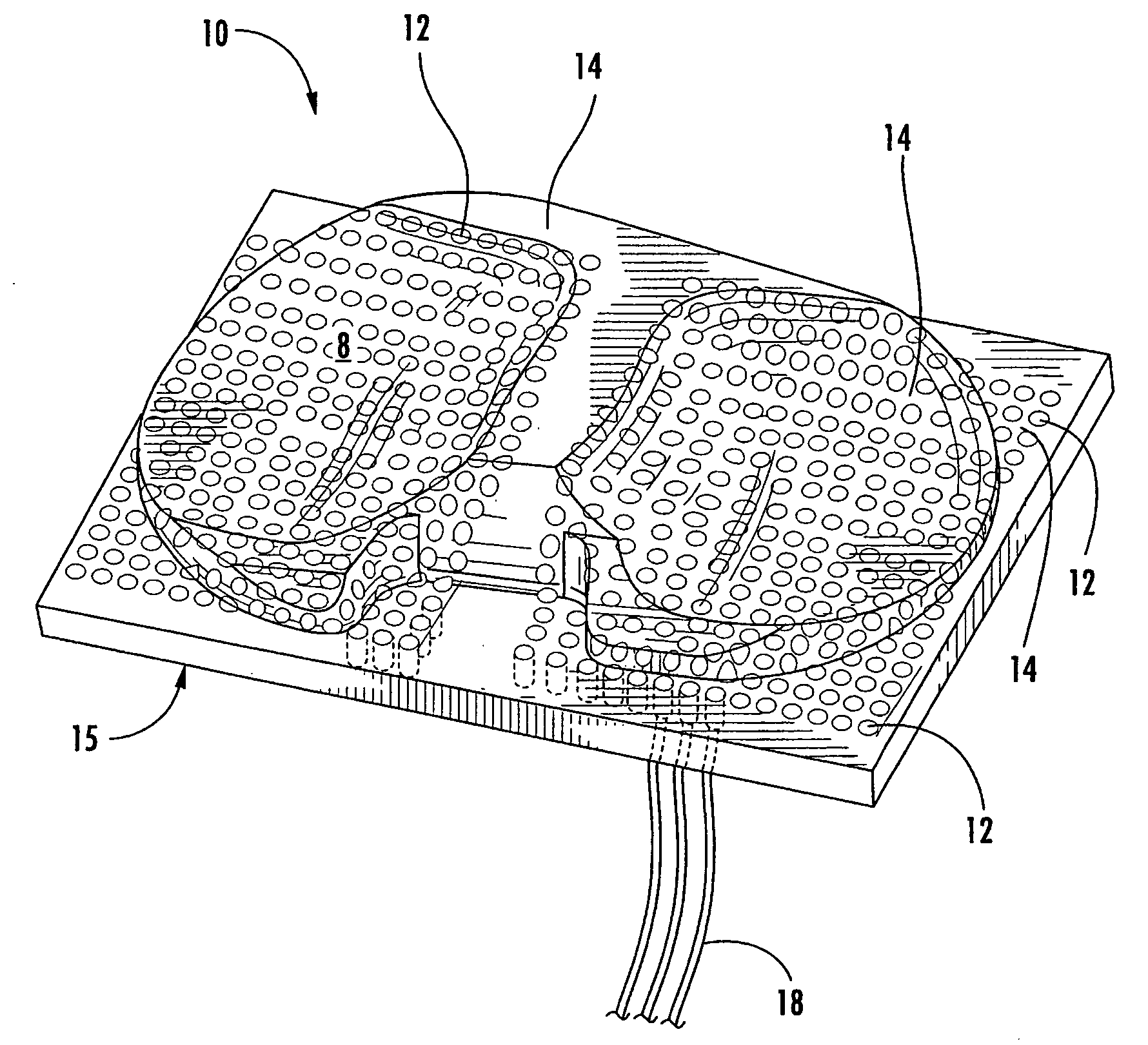
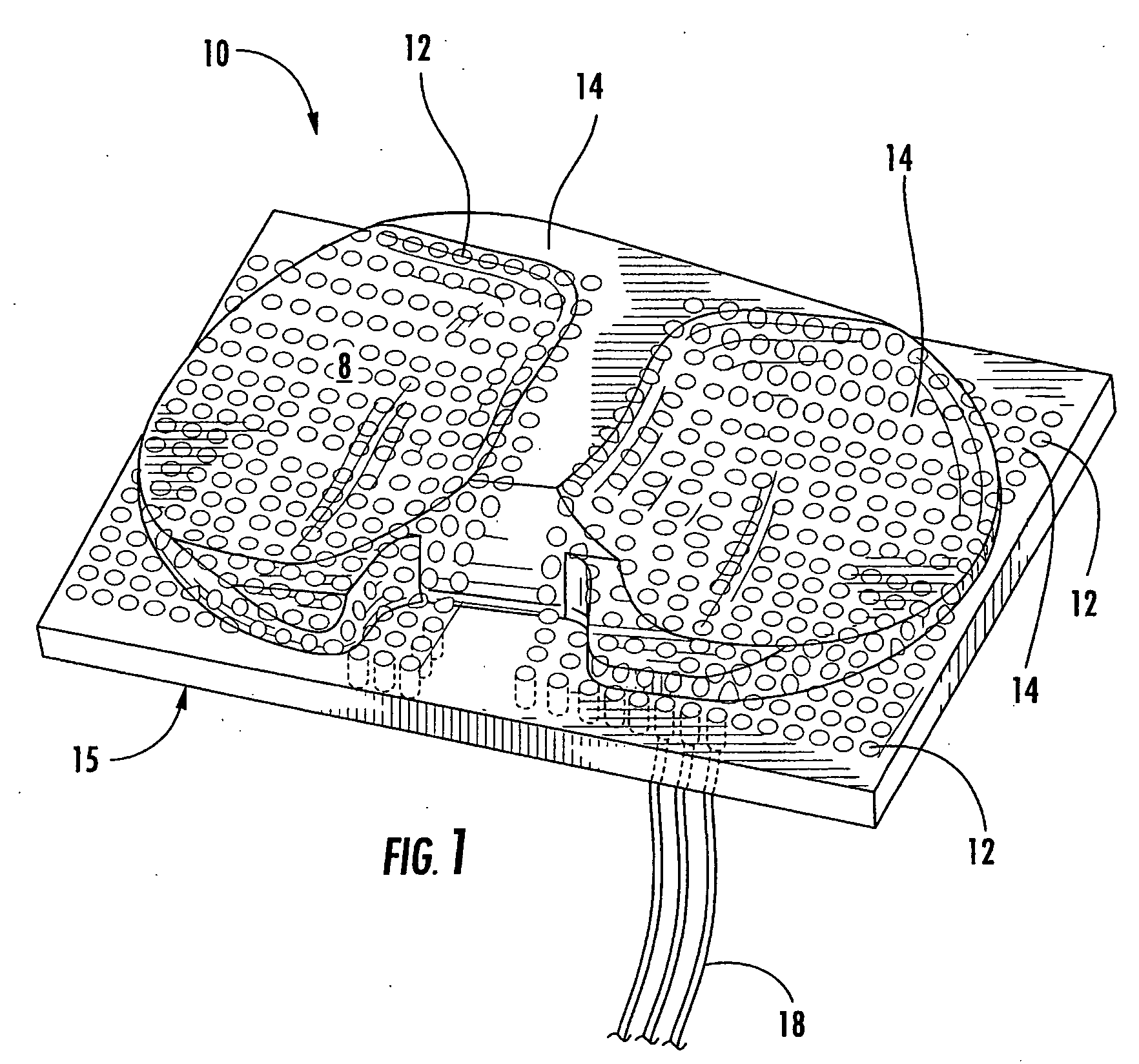
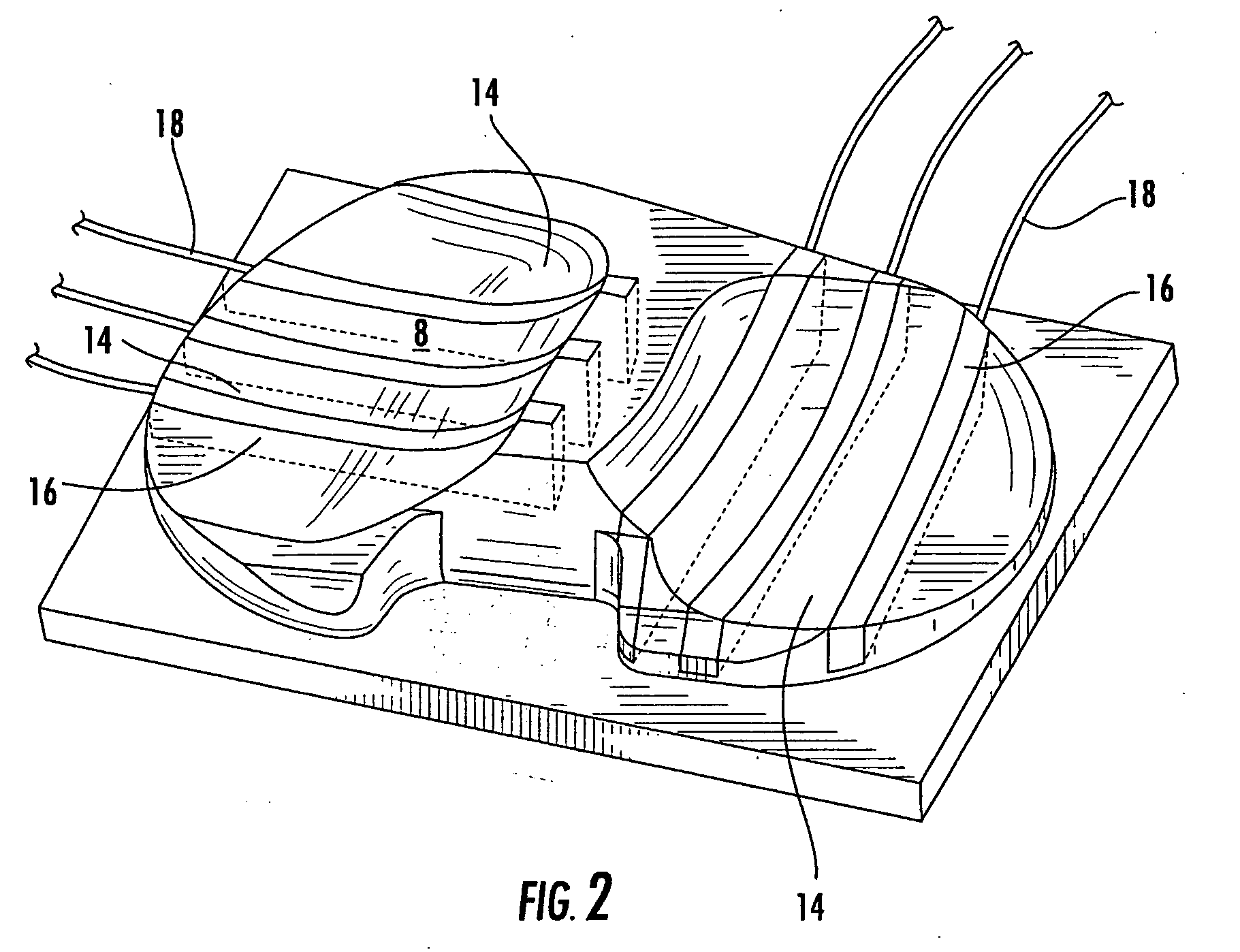
A system and method for prosthesis fitting in joints comprising an artificial condyle and a spacer which cooperates with the condyle to form an artificial joint. The spacer embedded with at least one sensor which is responsive to a force generated between the condyle and the spacer. The artificial joint is adapted to move between a flexed position and an extended position defining a range of motion. The sensor is responsive to the force and generates an output representative of that force. The output is transmitted, either wirelessly or other, to a processor which utilizes an analysis program to display a representation of the forces applied. A practitioner utilizing the displayed analysis may intraoperatively determine the adjustments and balancing required within the artificial joint. The system may also utilize a ligament tension sensor which generates data representative of tension on a ligament of the artificial joint, and a joint angle sensor responsive to the range of motion of the artificial joint. The processor may be adapted to store the outputted sensor data to provide the practitioner with statistically relevant historical data.
Owner:THE BOARD OF TRUSTEES OF THE UNIV OF ILLINOIS
Artificial joints using agonist-antagonist actuators
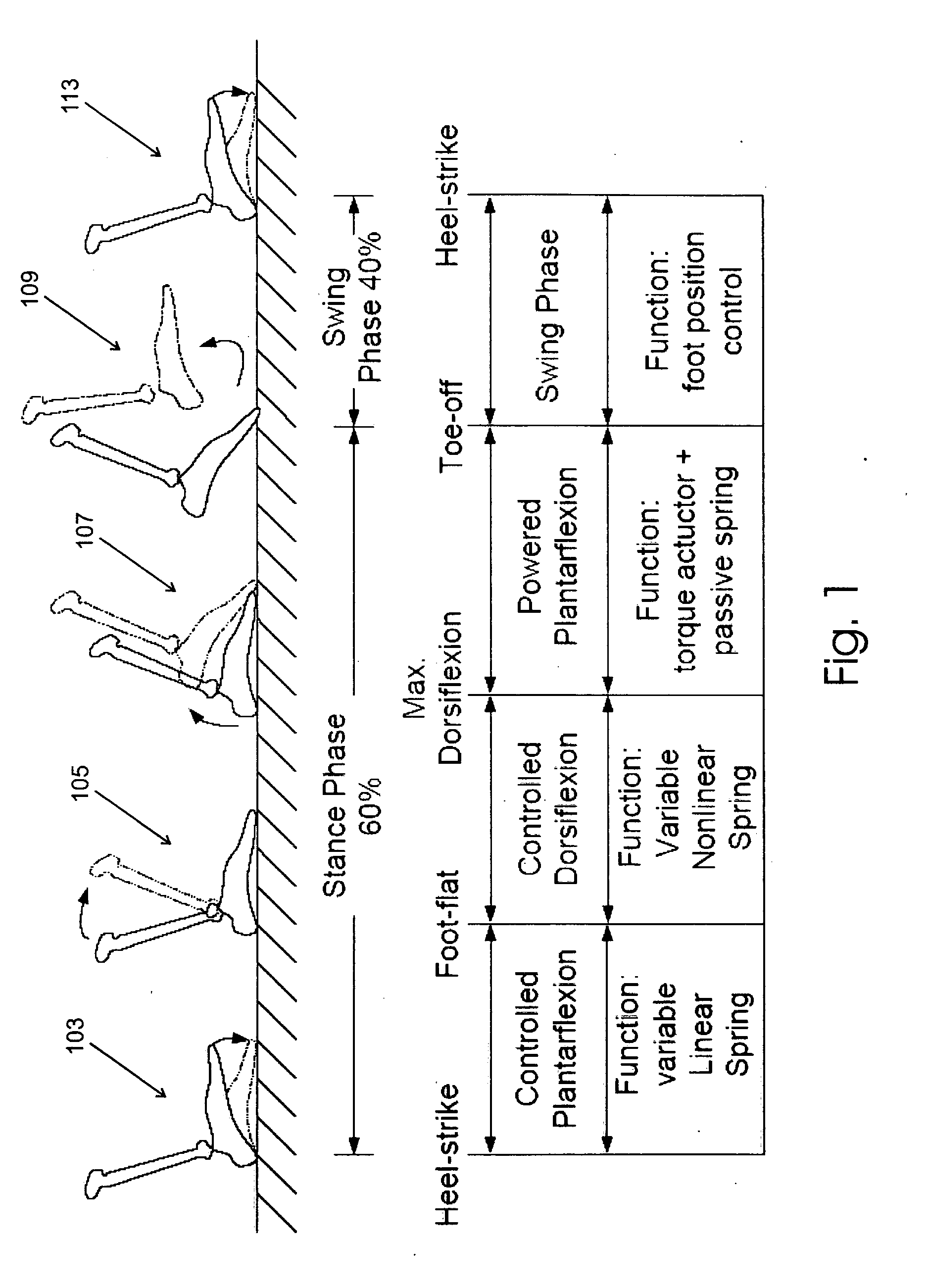
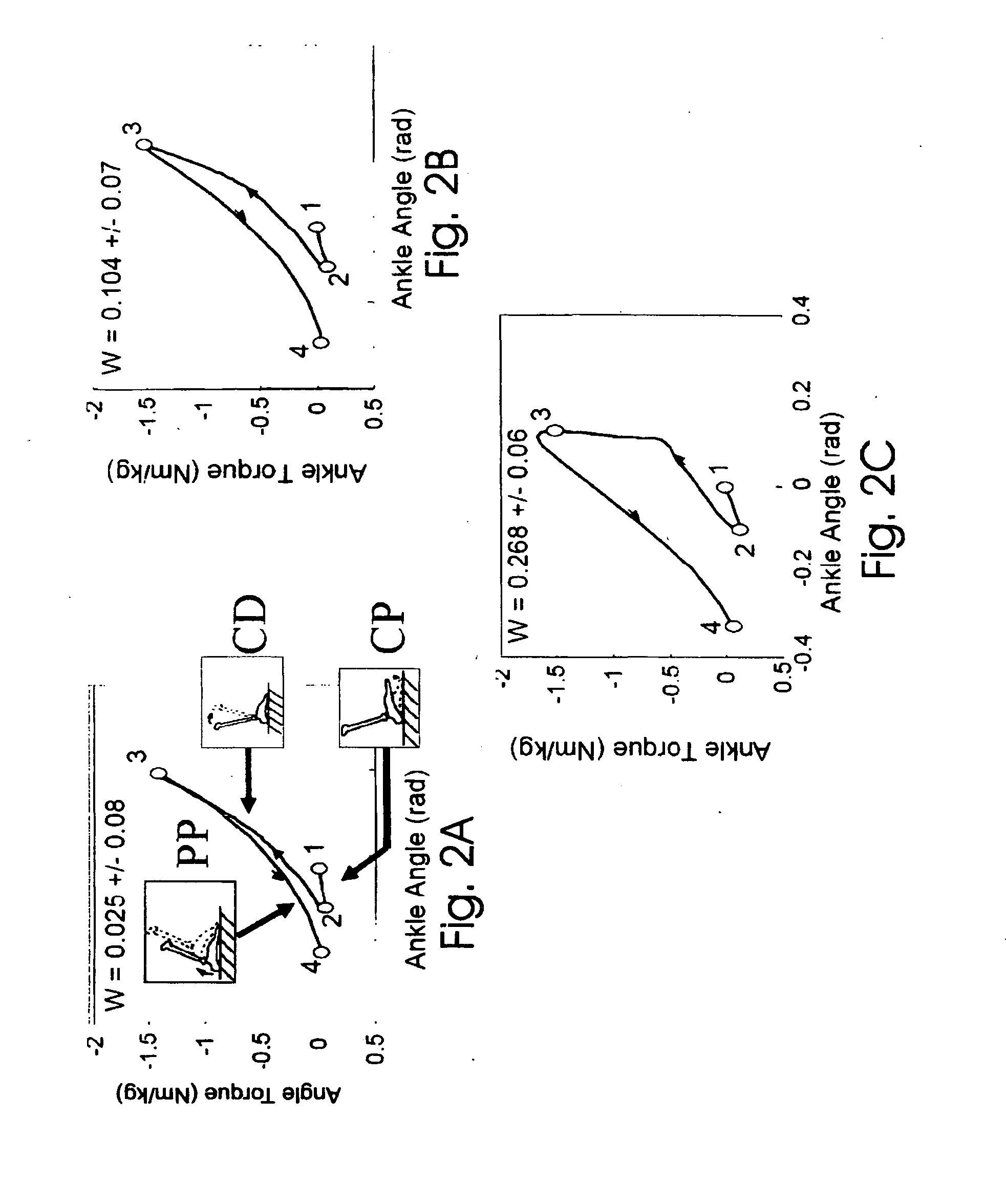
InactiveUS20070162152A1Increase the angleReduce the angleArtificial legsManipulatorArtificial jointsSacroiliac joint
Artificial limbs and joints which behave like a biological limbs and joints employ a synthetic actuator which consume negligible power when exerting zero force, consume negligible power when outputting force at constant length (isometric) and while performing dissipative, nonconservative work, are capable of independently engaging flexion and extension tendon-like, series springs, are capable of independently varying joint position and stiffness, and exploit series elasticity for mechanical power amplification.
Owner:MASSACHUSETTS INST OF TECH
Method of Designing and Manufacturing Artificial Joint Stem with Use of Composite Material
InactiveUS20080234833A1Low costIncreased durabilityJoint implantsTomographyArtificial jointsEngineering
The method of designing and manufacturing the artificial joint stem, comprising steps of performing analysis of the internal stress of the artificial joint stem and bone and the adhesive stress of the artificial stem and bone, using the computer, based on the three dimension data indicating the structure of the bone formed by using plural tomographic images of the bone, the design condition involving the form and stiffness of the artificial joint stem configured by using at least one of the tomographic images and the three dimension data, wherein if the result of the analysis does not satisfy the design condition, the condition is changed to have the computer reanalyze and if the result of the analysis satisfies the design condition, the artificial joint stem is designed and manufactured with the stem data based on the result of analysis and the design condition.
Owner:B I TEC
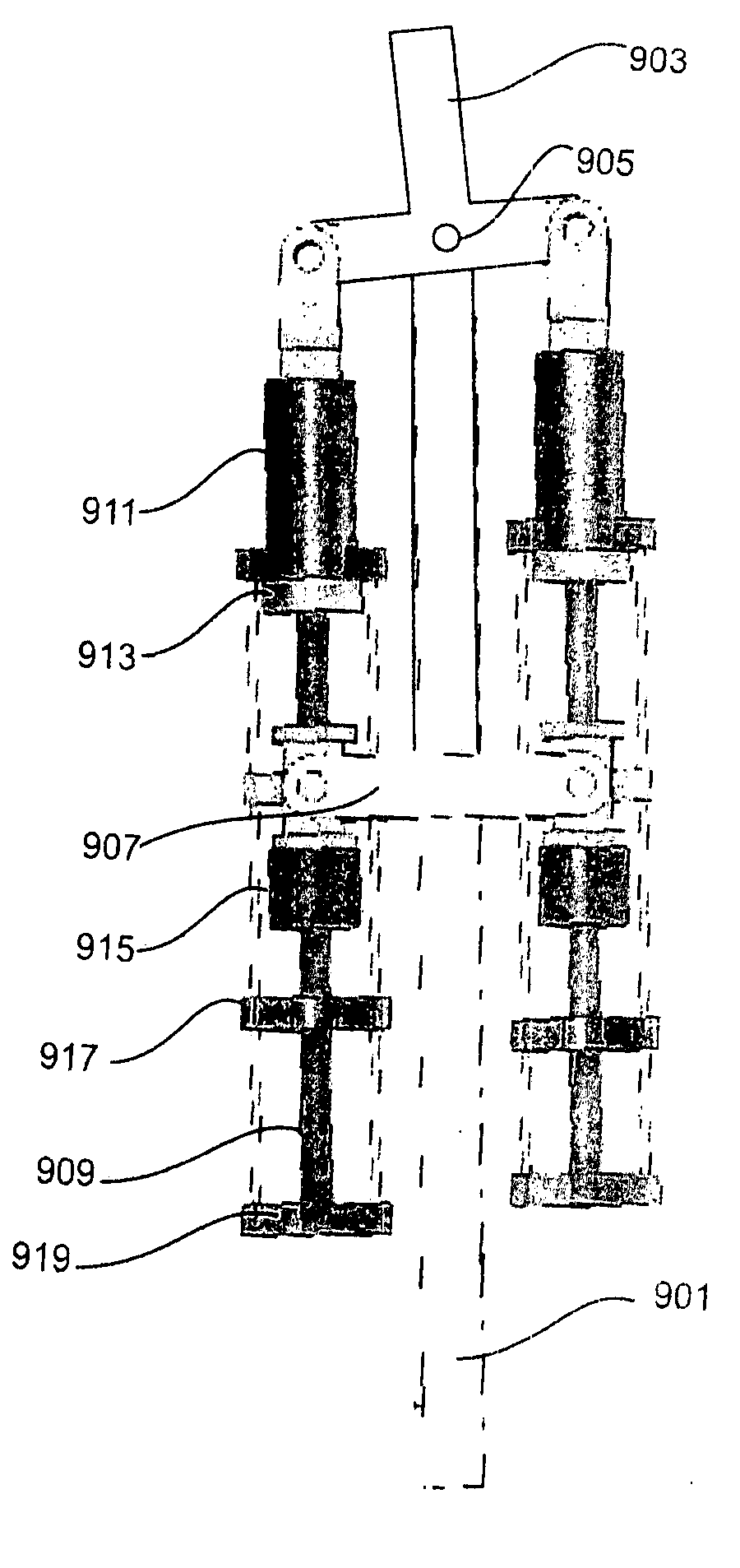
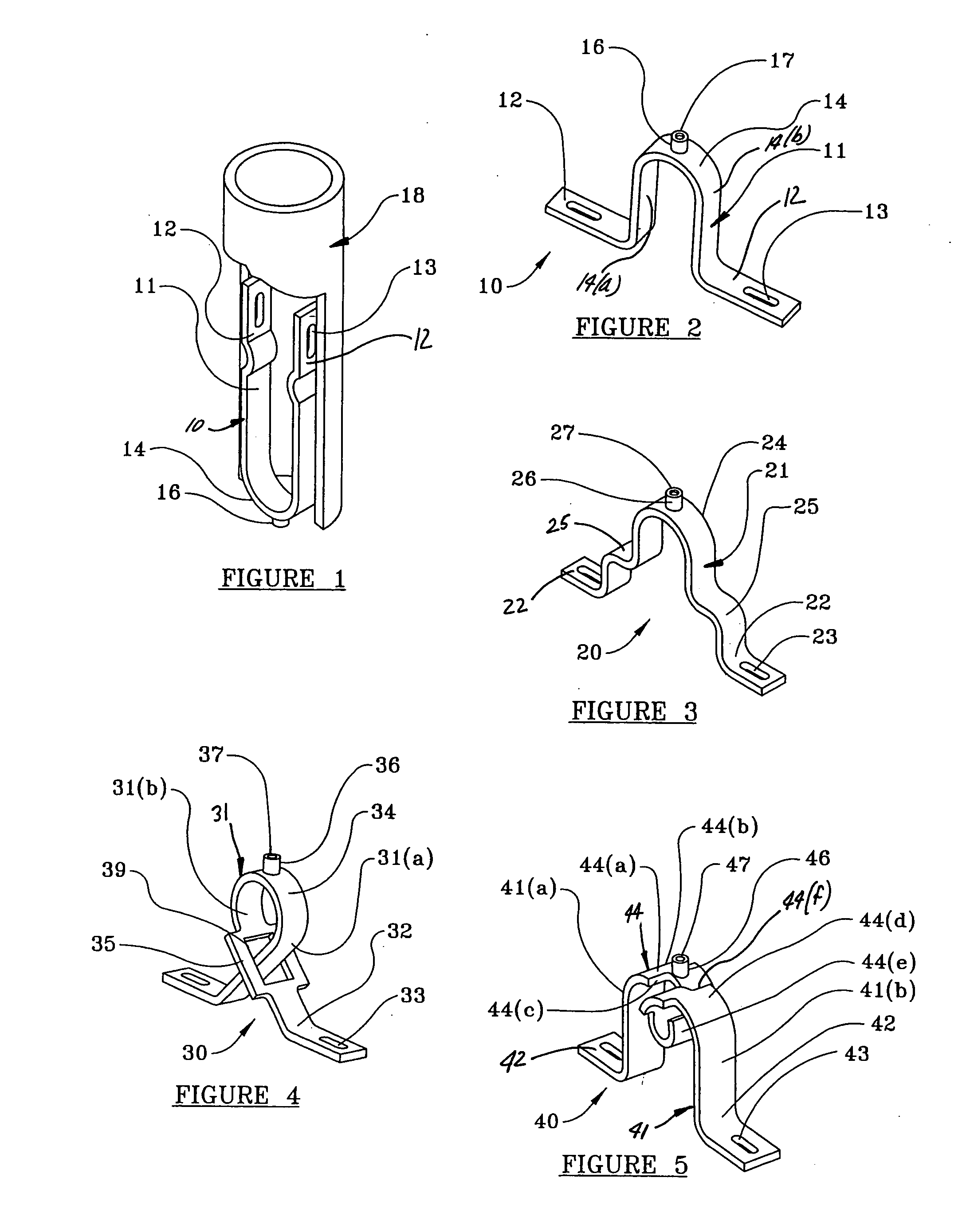
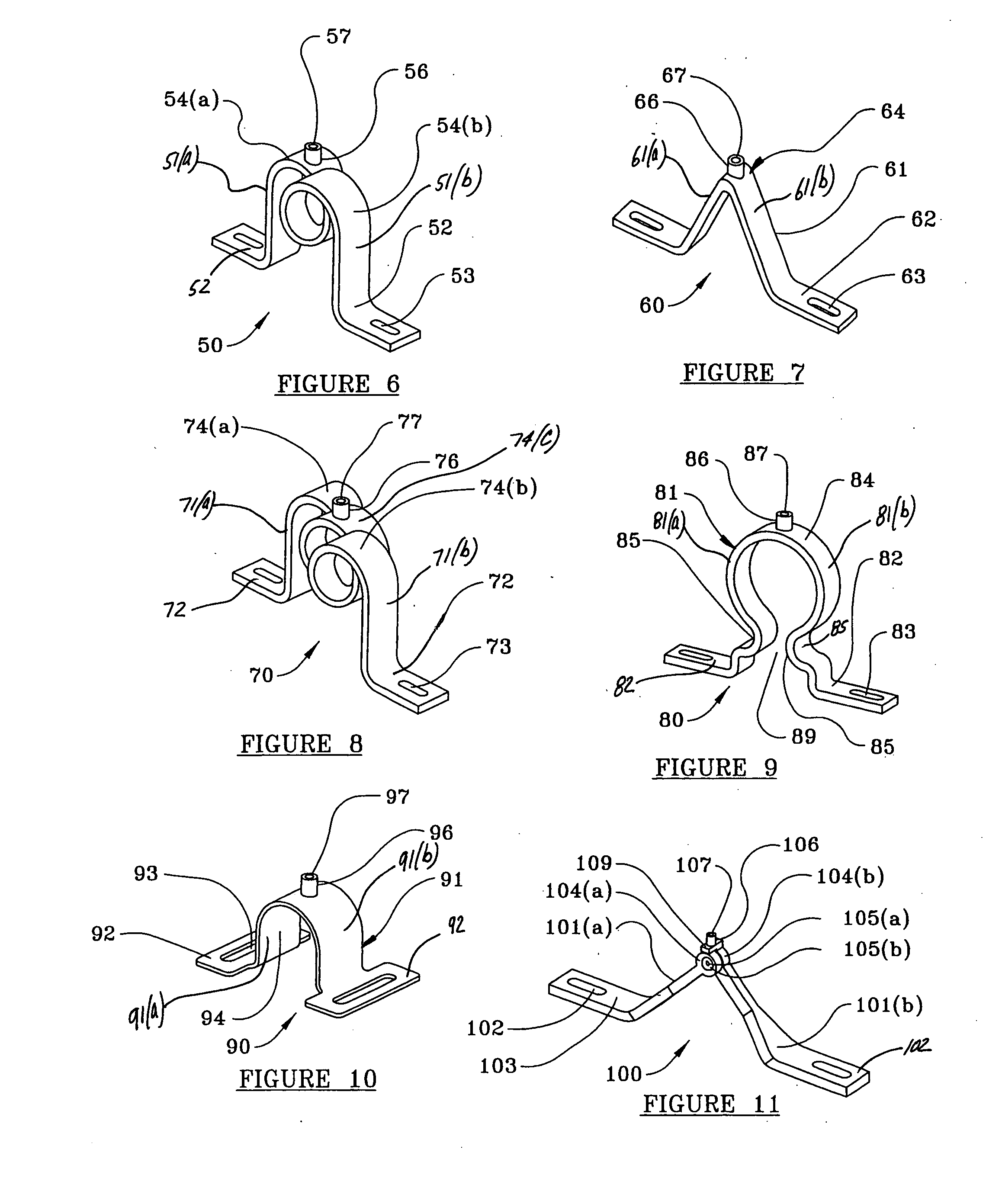
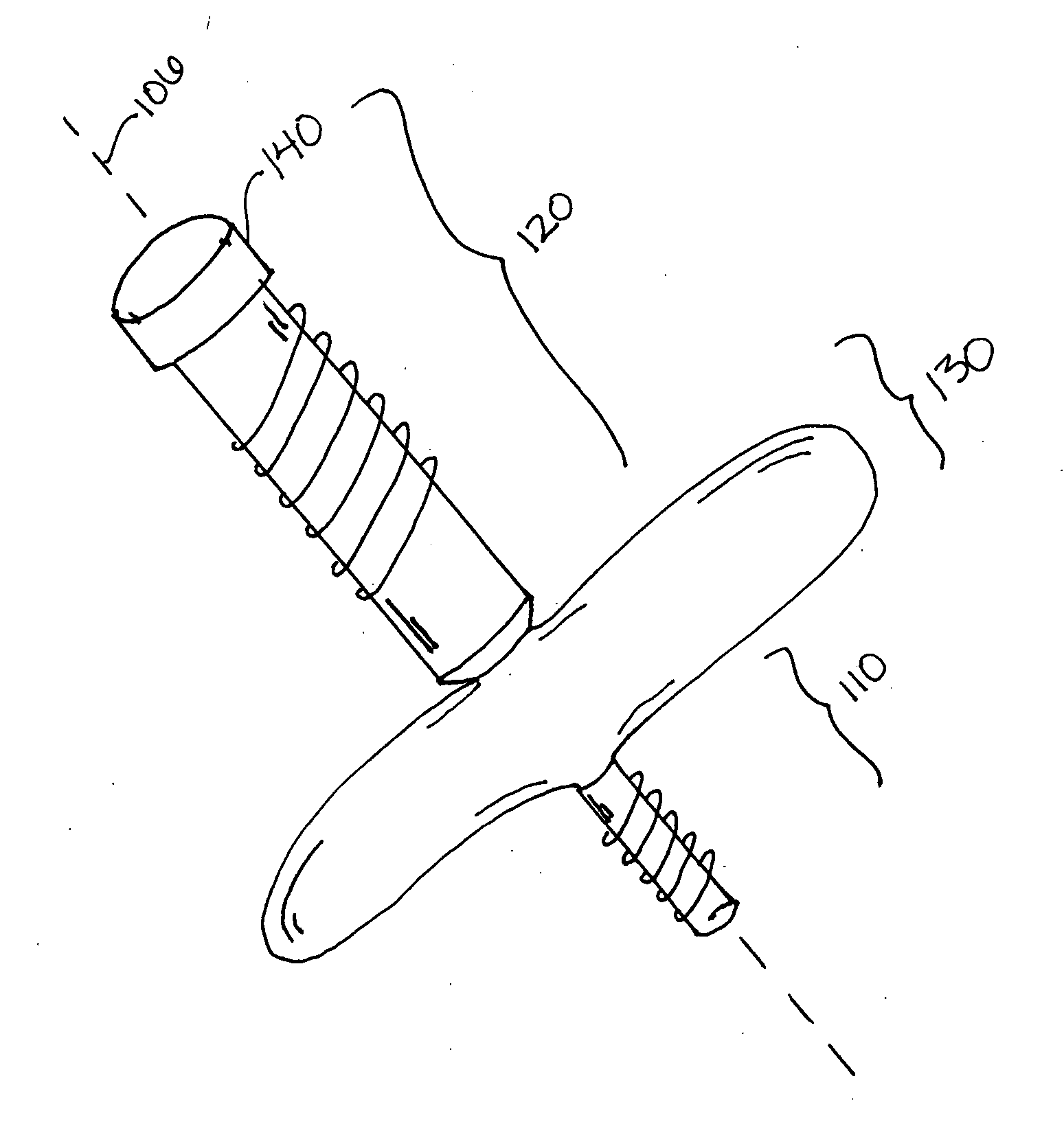
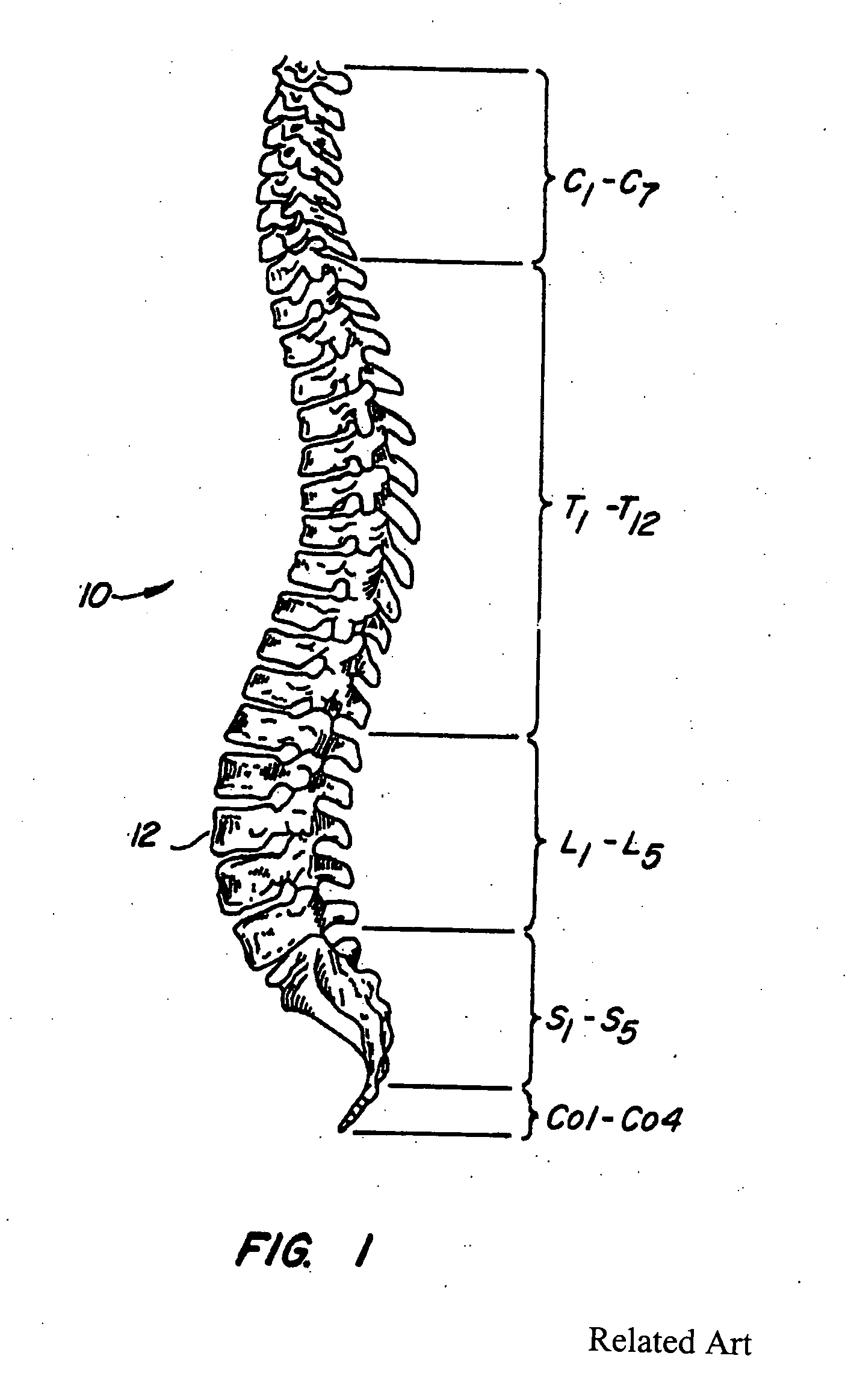
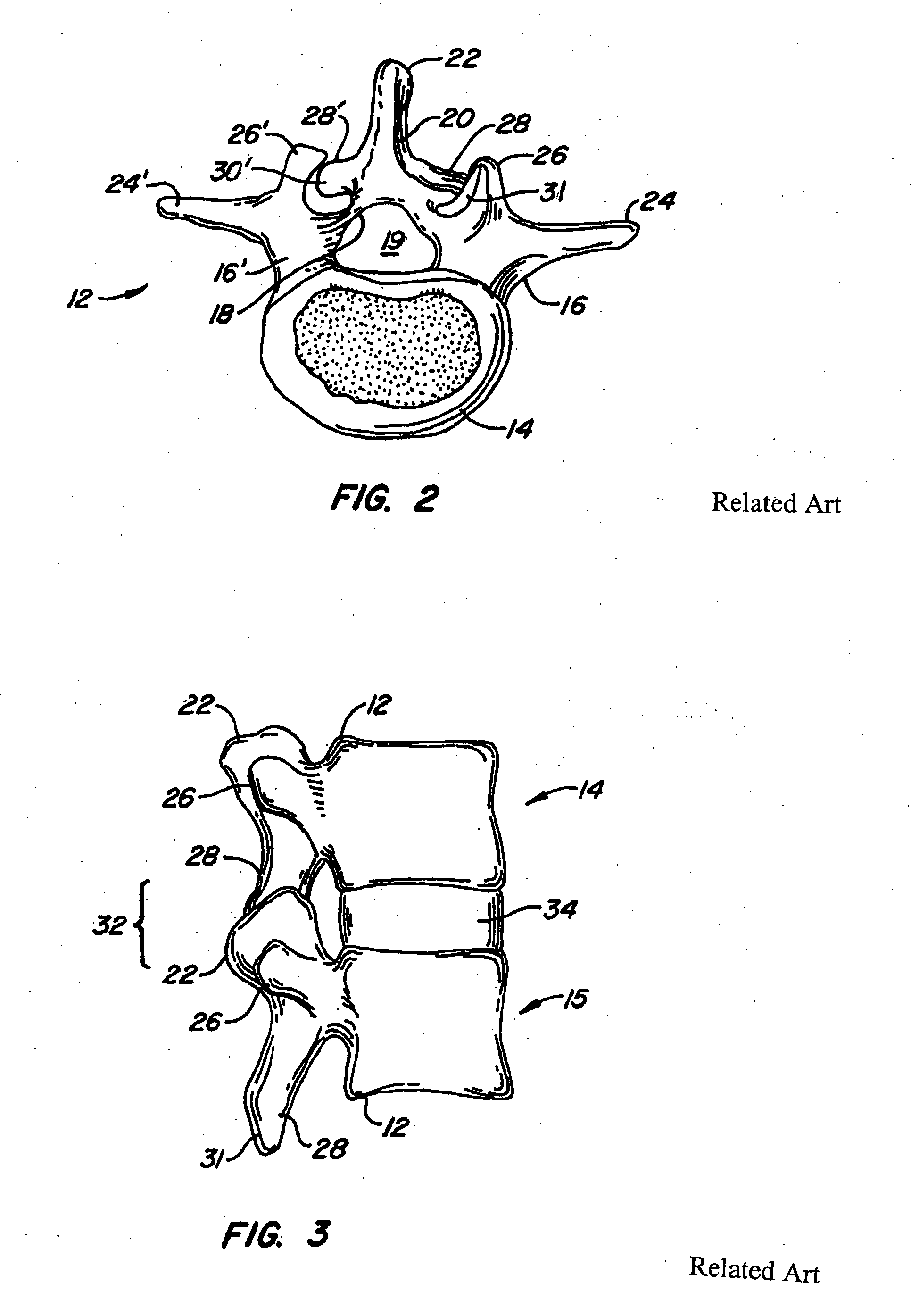
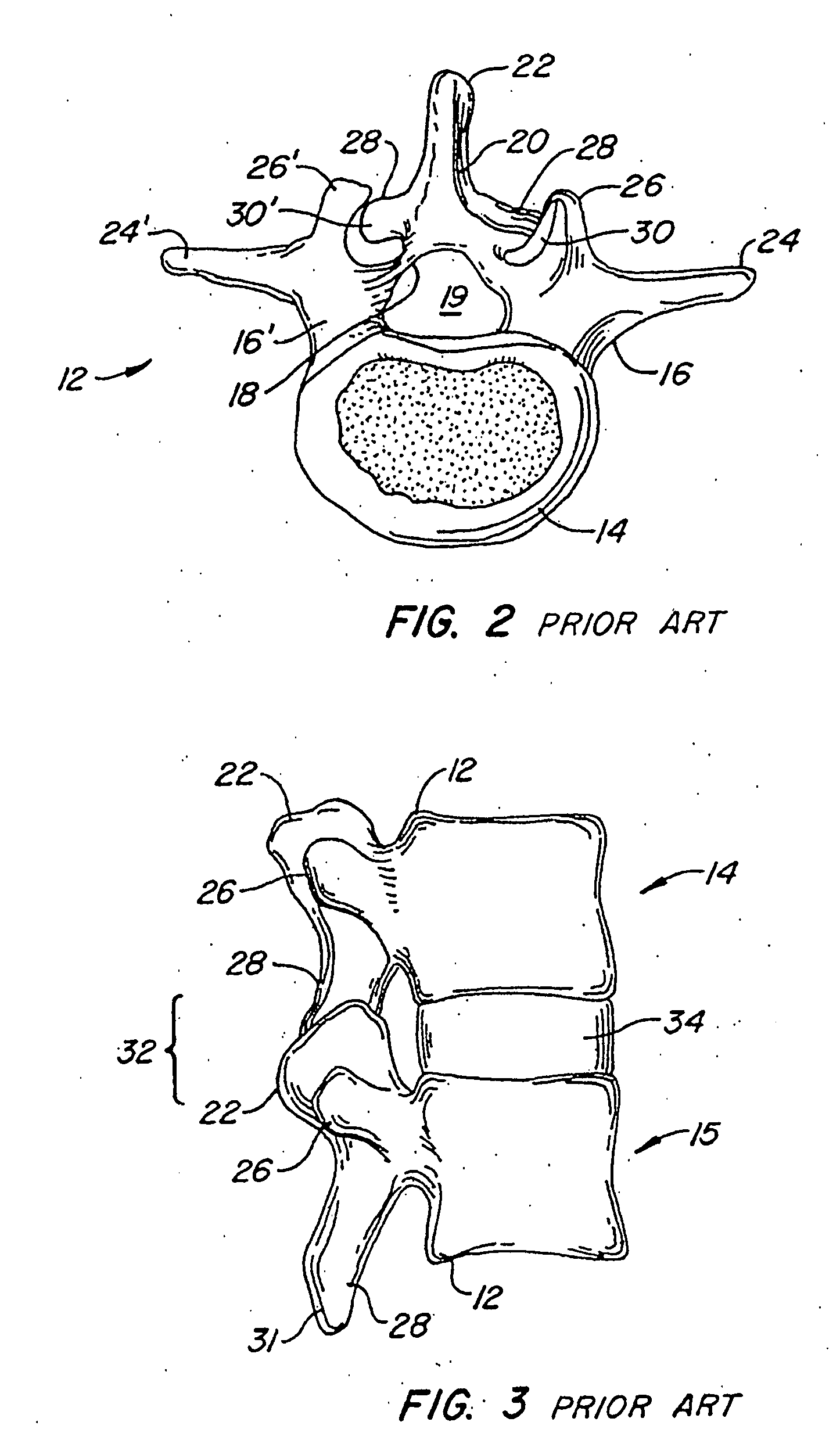
Artificial spinal joints and method of use
InactiveUS20050209694A1Preventing subluxationMaintain strengthInternal osteosythesisJoint implantsFiberCarbon fibers
An artificial spinal joint, consisting of a flexible or rigid member or a pair of moveably-joined, flexible or rigid segments, is formed into a spring-like shape, whose distal ends have feet with slots through which screws can be inserted to attach the artificial joint to vertebra whose facets (joints) are non-functional. The artificial spinal joint is able to prevent subluxation of the spine, while retaining the mobility of the spine and permitting angular deflection of the vertebra above and below a non-functional spinal joint. A jig is used to position tools and make passageways for screws to attach the artificial spinal joint to the vertebra or its pedicles or facets in a minimally invasive procedure. The rigid members or segments are bio-compatible and may be made of titanium, a titanium alloy, tantalum, medical grade stainless steel or carbon fibers in a matrix of a rigid, durable plastic. The flexible members or segments may be made of spring steel coated with a durable, bio-compatible material, small diameter carbon fibers in a flexible, durable plastic matrix, or a single shape or dual shape, superelastic memory metal. The feet, made of any of the rigid or flexible materials described above, may also be moveably attached to the proximal ends of the members or segments. Having the feet moveably attached to the segments facilitates insertion of the artificial spinal joint into the body by folding the feet parallel to the axis of the segments during insertion, and then unfolding the feet for attachment to the vertebra or its pedicles or facets. The artificial spinal joint may be inserted and attached to vertebra whose facets are non-functional in minimally invasive, moderately invasive or conventional surgical procedures.
Owner:TRIMEDYNE
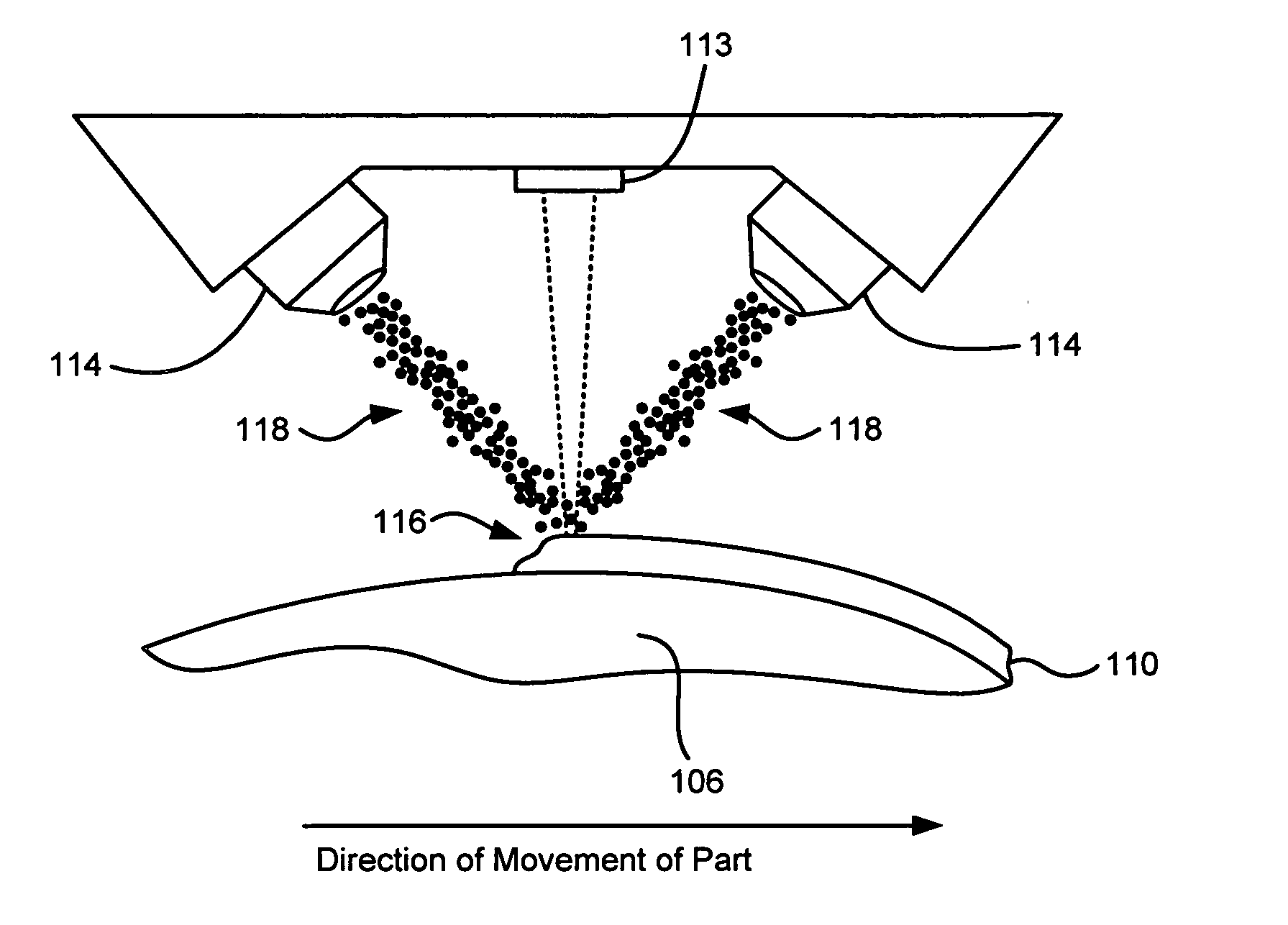
Laser based metal deposition of implant structures
InactiveUS20050123672A1Improved bearing propertyIncrease bone ingrowth propertyDental implantsFinger jointsArtificial jointsBone ingrowth
Owner:MEDICINELODGE
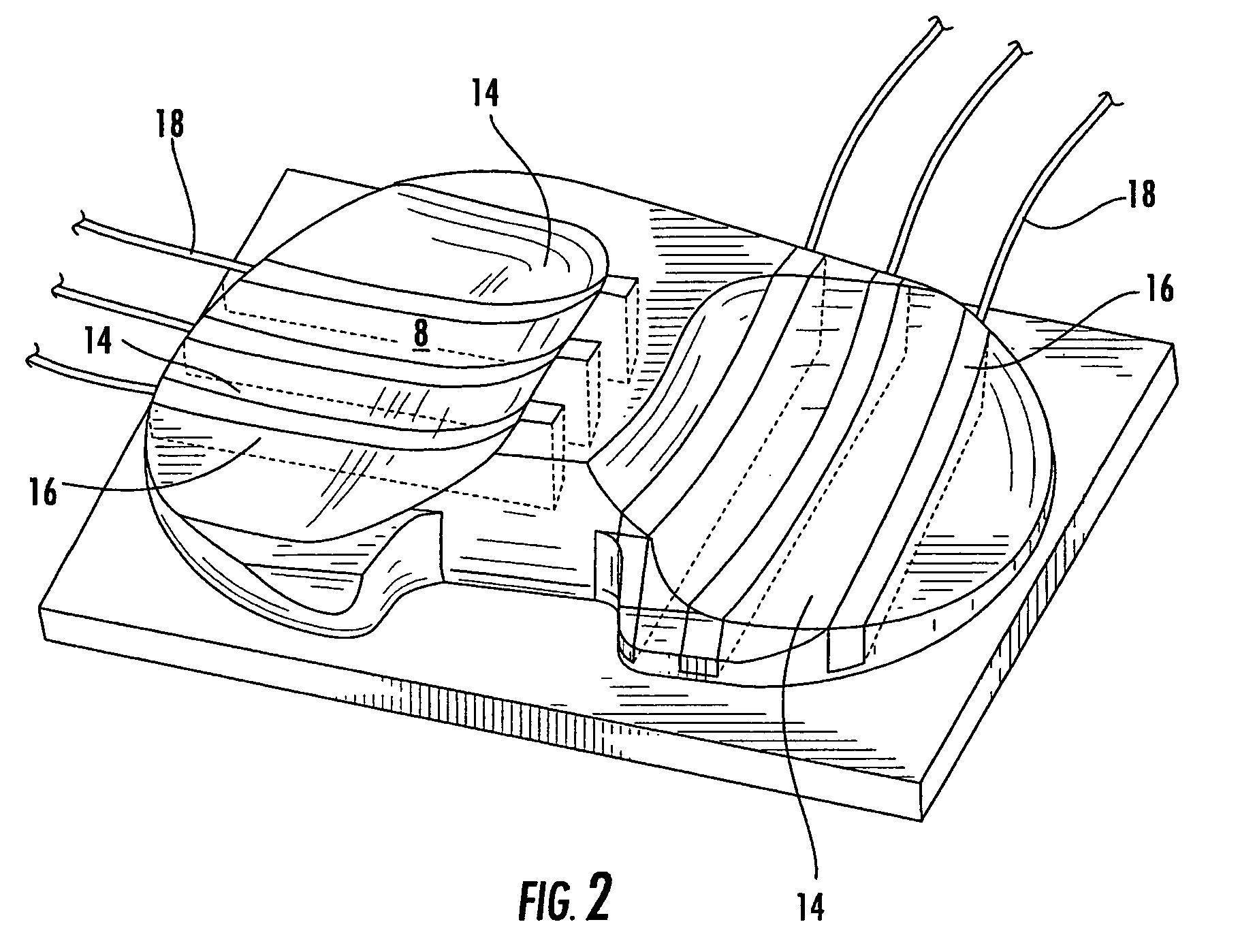
Polymeric joint complex and methods of use
InactiveUS20060085075A1Increase and decrease constraintEasy for flexibilityFinger jointsWrist jointsHuman bodyArtificial joints
The invention describes a variety of implantable artificial joint complexes adapted for implantation within a target joint space within a human body. The joint complexes comprise: an expandable joint segment adapted to fit within the target joint space; and at least one of a first cannulated anchor adapted to engage the expandable joint segment and adapted to engage a bony structure adjacent the target joint space; and a second anchor adapted to engage the expandable joint segment and adapted to engage a bony structure adjacent a target joint space. The invention also discloses methods of implanting a patient specific artificial joint complex. The methods include the steps of: accessing a target joint space by creating an access hole through an adjacent bony structure; inserting a joint complex device having a cannulated anchor and an expandable joint segment through the access hole with the expendable joint segment being positioned between the surfaces forming the joint; injecting material into the expandable joint segment; and sealing access to the target joint space.
Owner:GMEDELAWARE 2
Implantable biomedical devices including biocompatible polyurethanes
Disclosed are implantable devices that include biocompatible polyurethane materials. In particular, the disclosed polyurethane materials can maintain desired elastomeric characteristics while exhibiting thermoset-like behavior and can exhibit improved characteristics so as to be suitable in load-bearing applications. For example, the disclosed polyurethane materials can be suitable for use in artificial joints, including total joint replacement applications. The disclosed polyurethane materials include biocompatible cross-linking agents as chain extenders, more particularly chain extenders comprising a terminal group capable of side reactions and further comprising an electron withdrawing group immediately adjacent the terminal group. In addition, the reaction materials and conditions can be selected to encourage intermediate levels of cross-linking without the use of traditional cross-linking trifunctional reagents. In addition, the chain extenders can also include substantially inflexible moieties so as to increase the rigidity of the product polyurethanes.
Owner:CLEMSON UNIVERSITY +1
Immobilizing mediator molecules via anchor molecules on metallic implant materials containing oxide layer
A mediator molecule is immobilized on the surface of a metallic or ceramic implant material. An anchor molecule such as a dialdehyde having a functional group that covalently binds the mediator molecule is covalently bound to the surface, and the mediator molecule is coupled to the functional group of the anchor molecule. The implant material may be composed of titanium, titanium alloy, aluminum, stainless steel or hydroxylapatite. Oxide units on the surface of the implant material can be increased preferably by treating with hot chromic-sulphuric acid for 0.5 to 3 hours at a temperature between 100 to 250° C. prior to binding the anchor molecule. Also, prior to binding the anchor molecule, the surface of the implant material can be activated by reacting with a silane derivative. Mediator molecules include BMP protein, ubiquitin and antibiotics, and the implant material may be an artificial joint or coronary vessel support such as a stent.
Owner:MORPHOPLANT
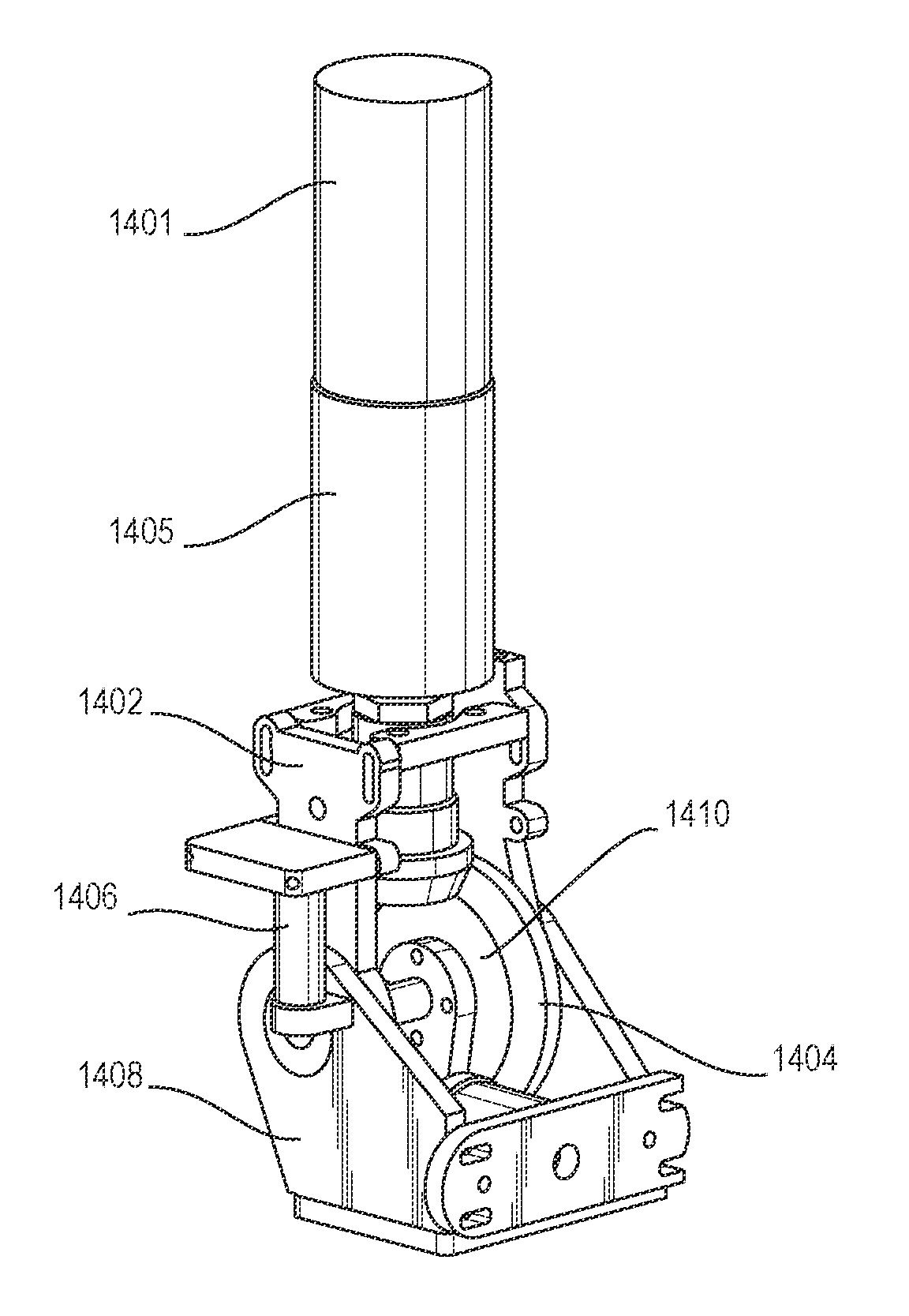
Parallel linkage and artificial joint device using the same
InactiveUS7118601B2Reduce the burden onReduce wearProgramme-controlled manipulatorJointsArtificial jointsEngineering
There are provided an artificial joint device that can realize an artificial limb enabling twisting motion without a drive source, and when with the drive source, reduce the size and costs of the device, and a parallel linkage that can realize the device. The linkage connects a foot portion and a mounting plate spaced from each other. A fixed link has one end fixed to the plate, and the other end connected to the foot portion via a ball joint, making the angle of the fixed link relative to the foot portion changeable in any direction. Expansible links extend between the foot portion and the plate in an expansible / contractible manner and each have opposite ends connected to the plate and the foot portion via respective upper and lower ball joints, making respective angles thereof relative to the foot portion and the plate changeable in any direction.
Owner:HONDA MOTOR CO LTD
Prosthetic devices employing oxidized zirconium and other abrasion resistant surfaces contacting surfaces of cross-linked polyethylene
Orthopedic implants which include the components of zirconium or zirconium-based alloys having surfaces coated with oxidized zirconium or alternatively, other orthopedic implants comprising abrasion resistant surfaces contacting surfaces of cross-linked polyethylene are disclosed. Such implants provide low friction, highly wear resistant coatings especially useful in artificial joints, such as hip joints, knee joints, elbows, etc., but also useful in other implant devices as well. The implants also find use as vertebral disc prostheses.
Owner:SMITH & NEPHEW INC
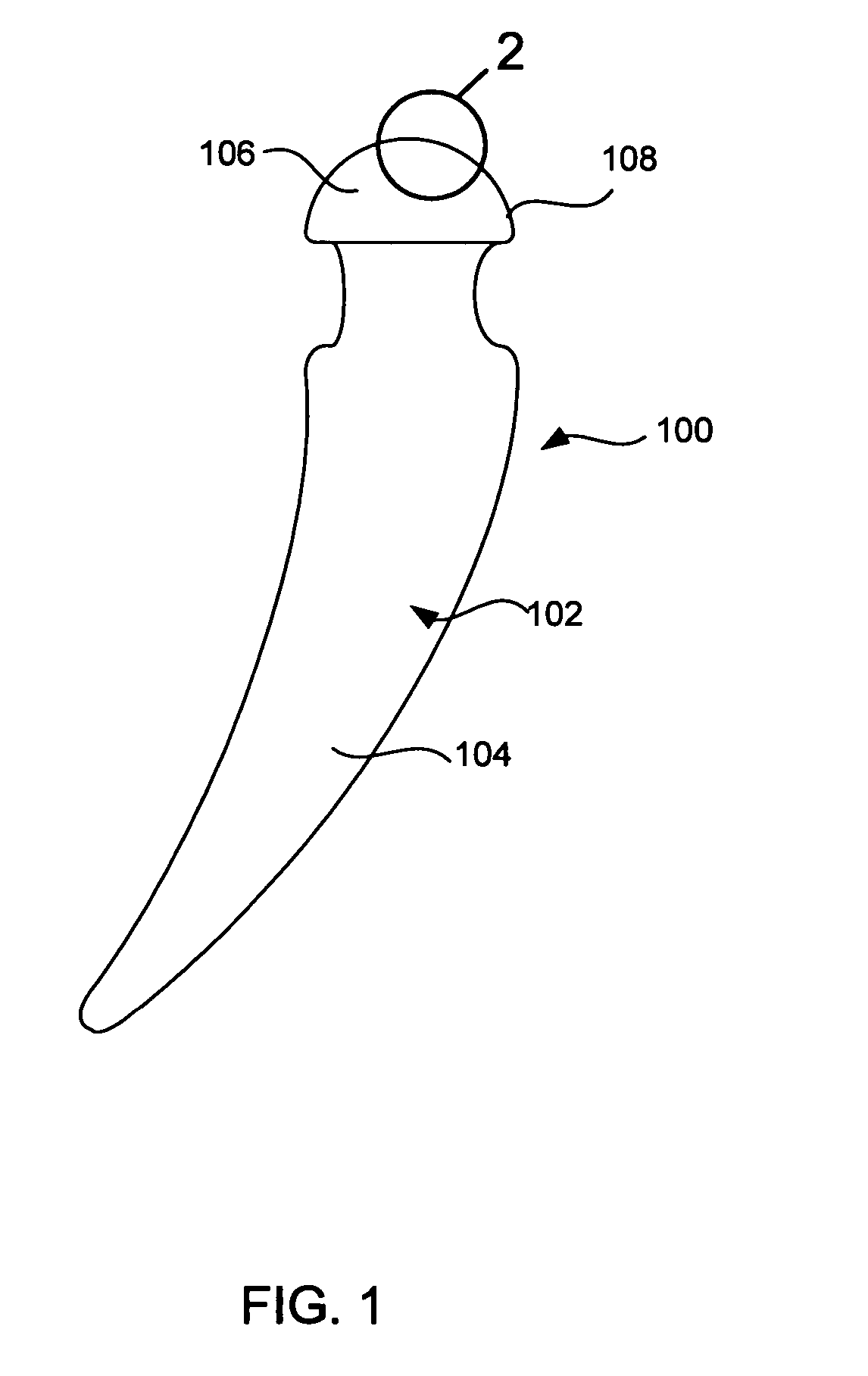
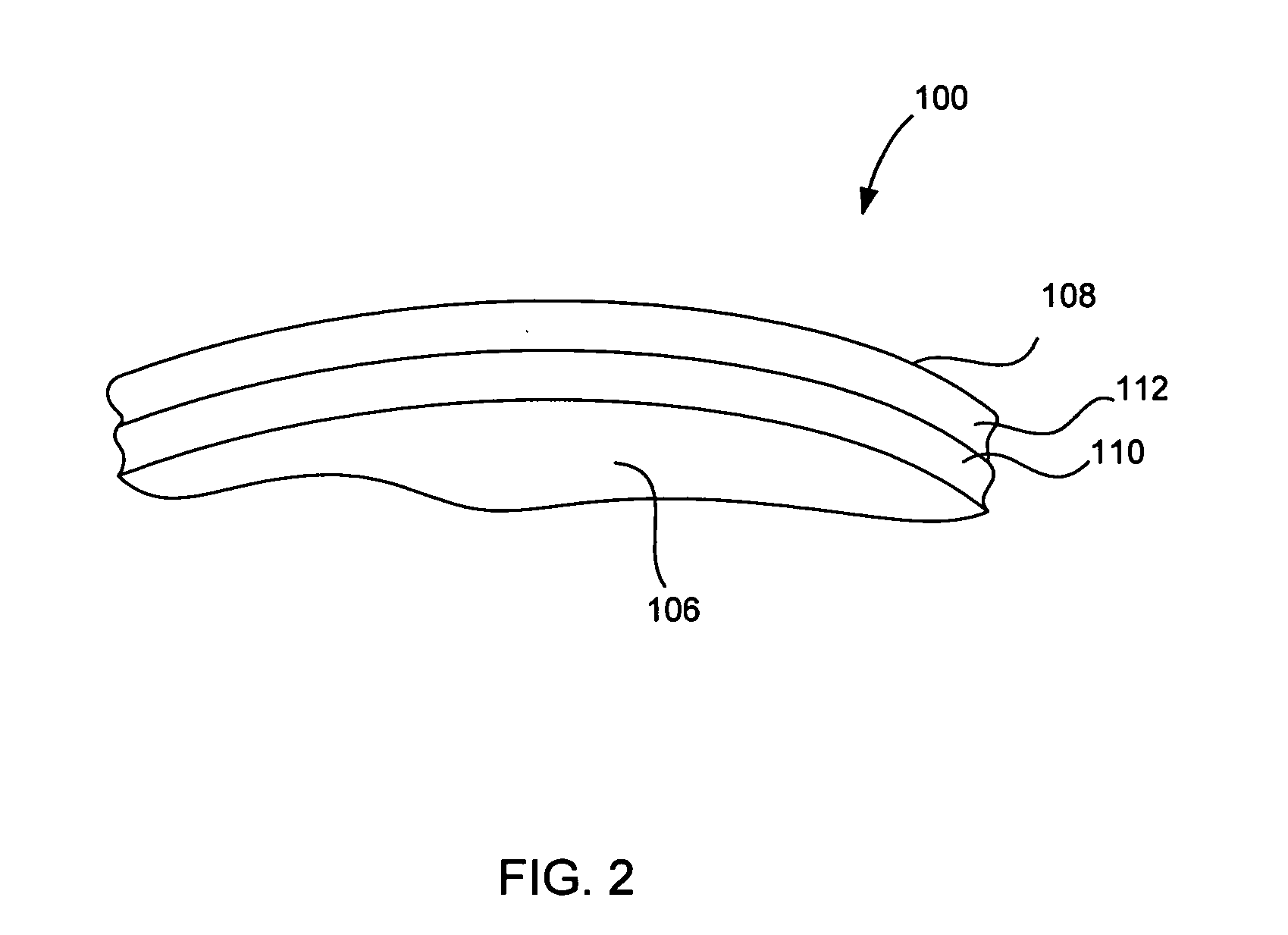
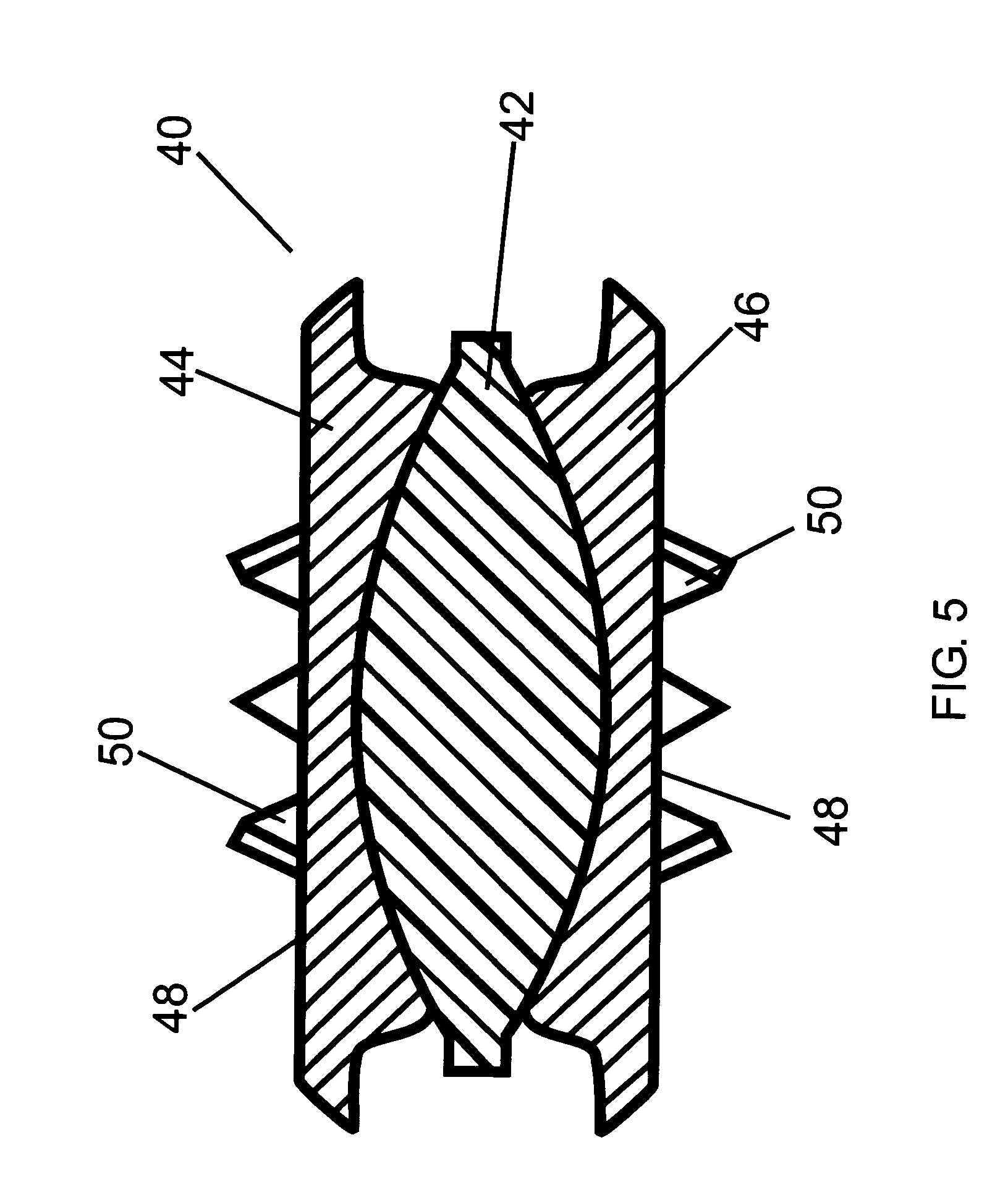
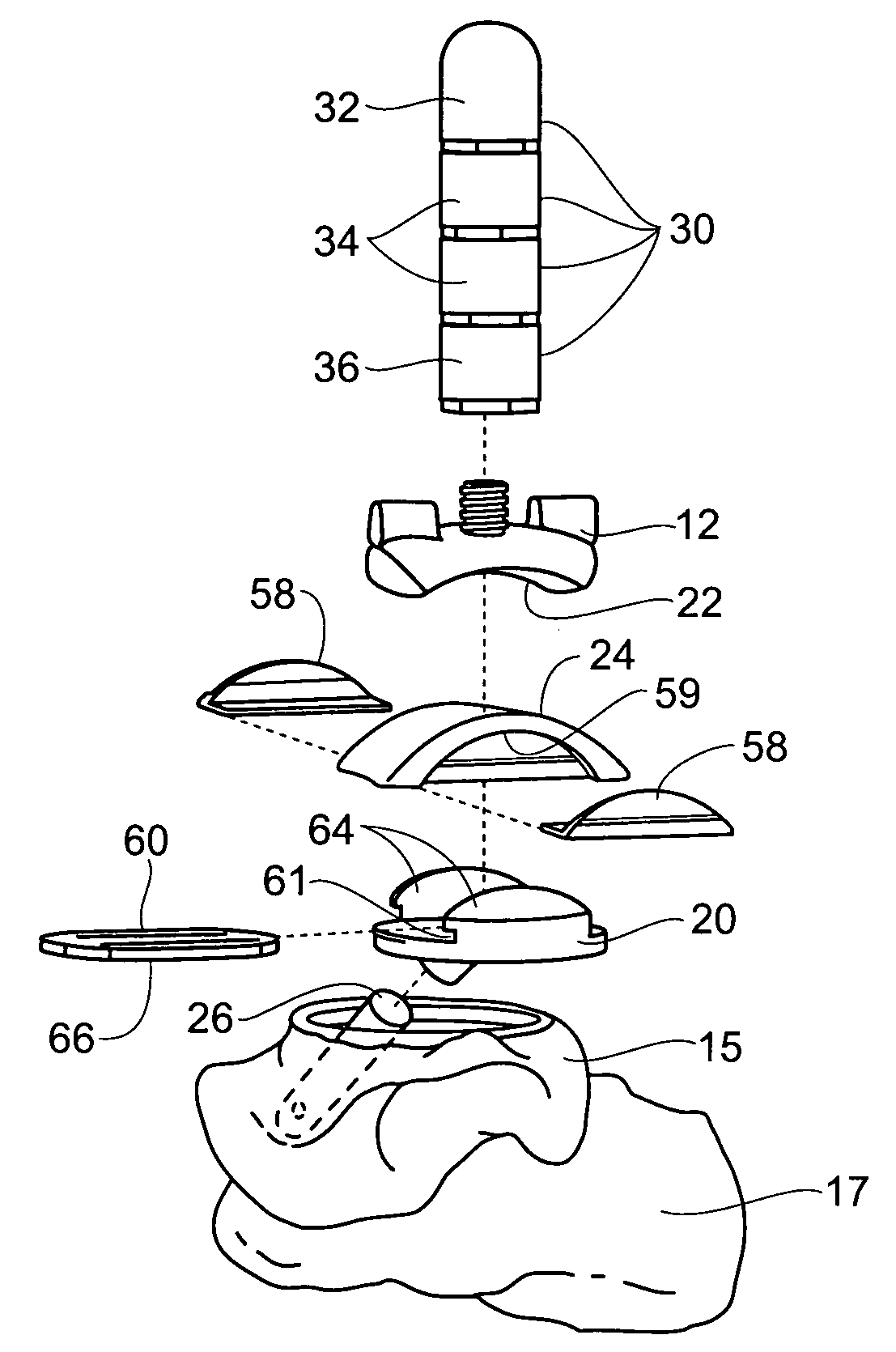
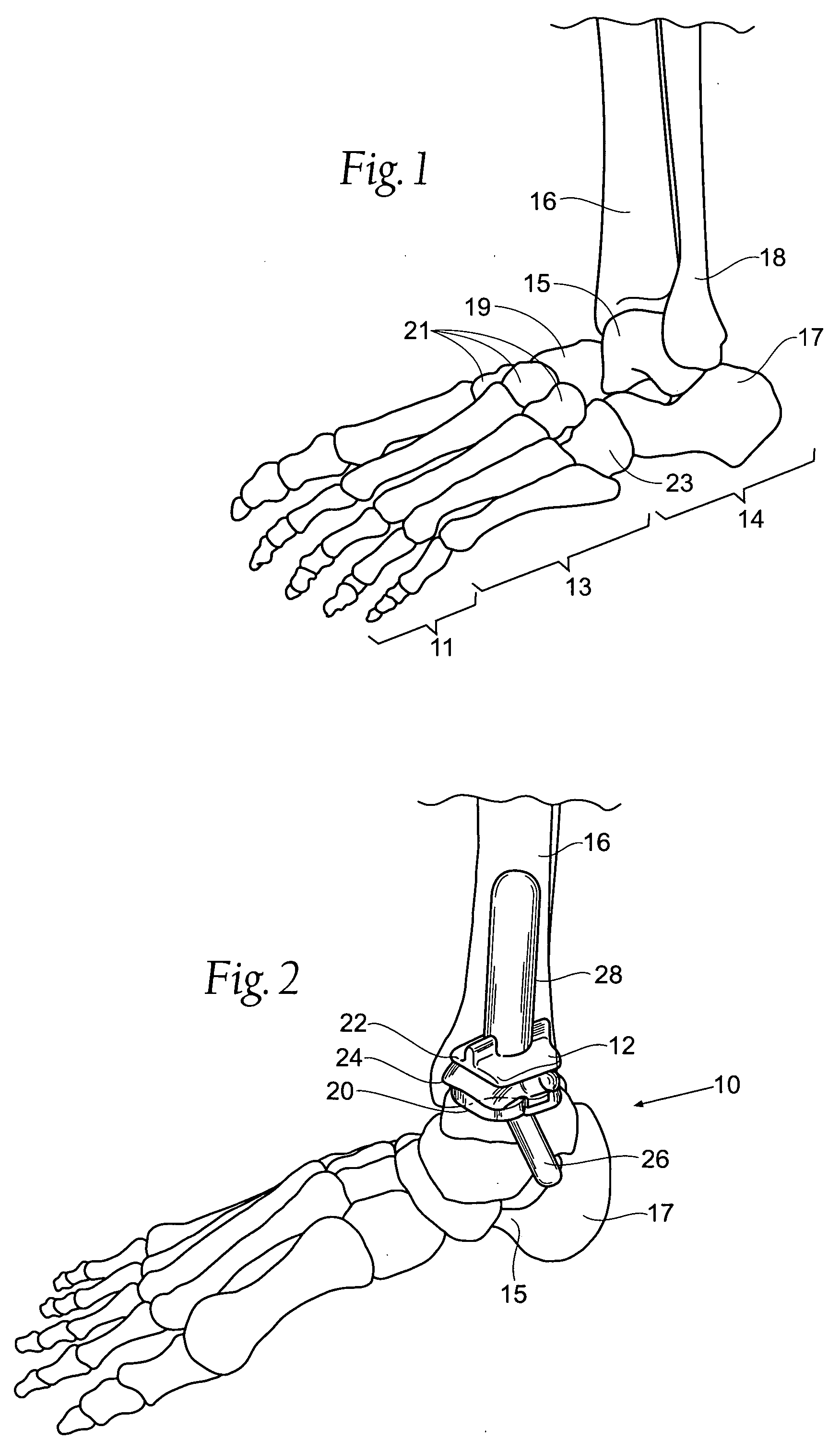
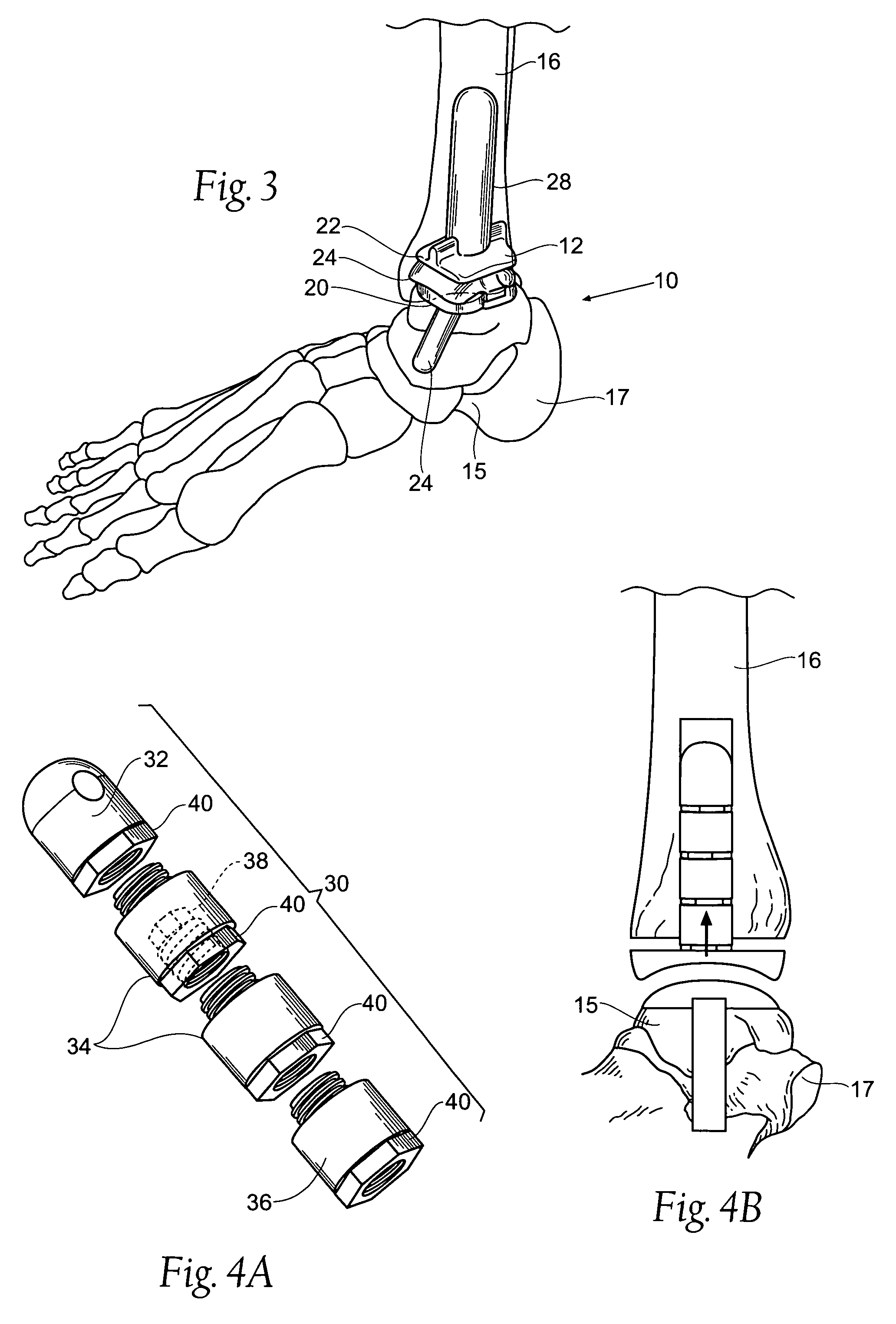
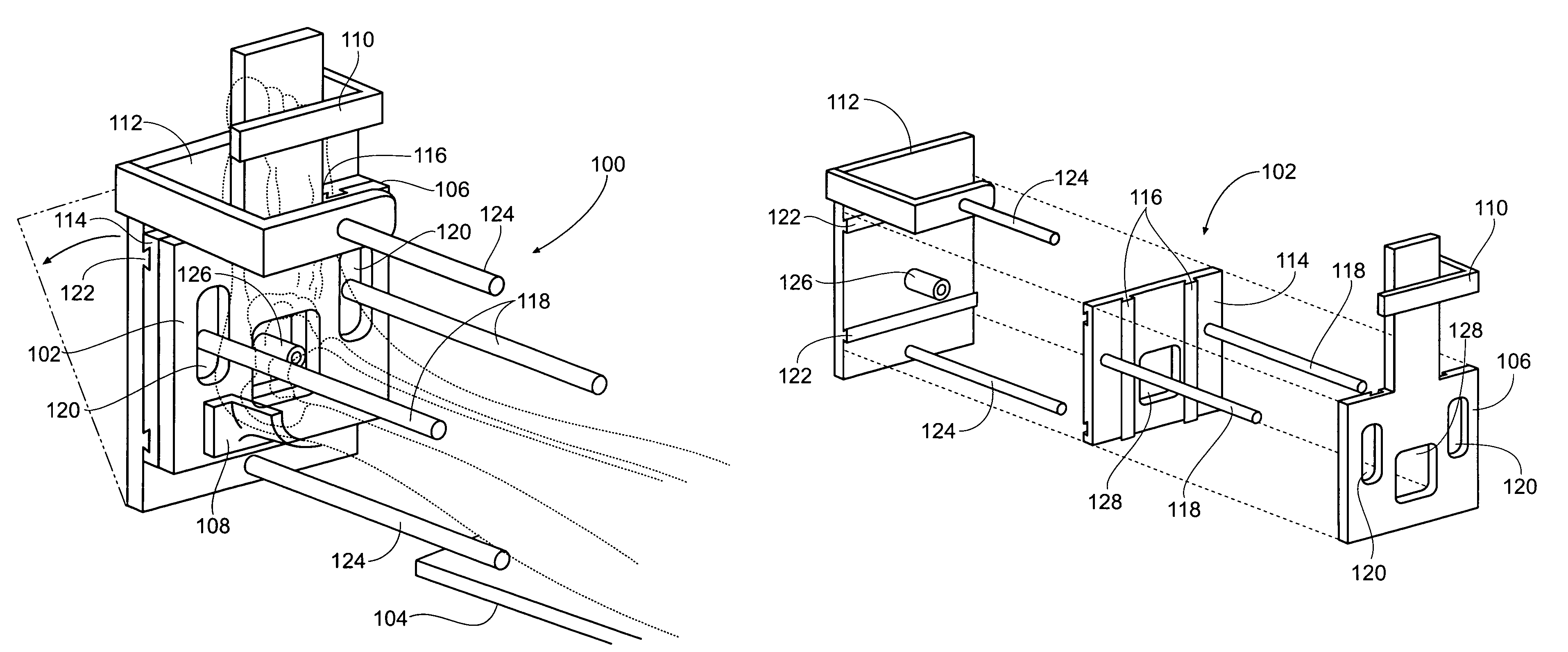
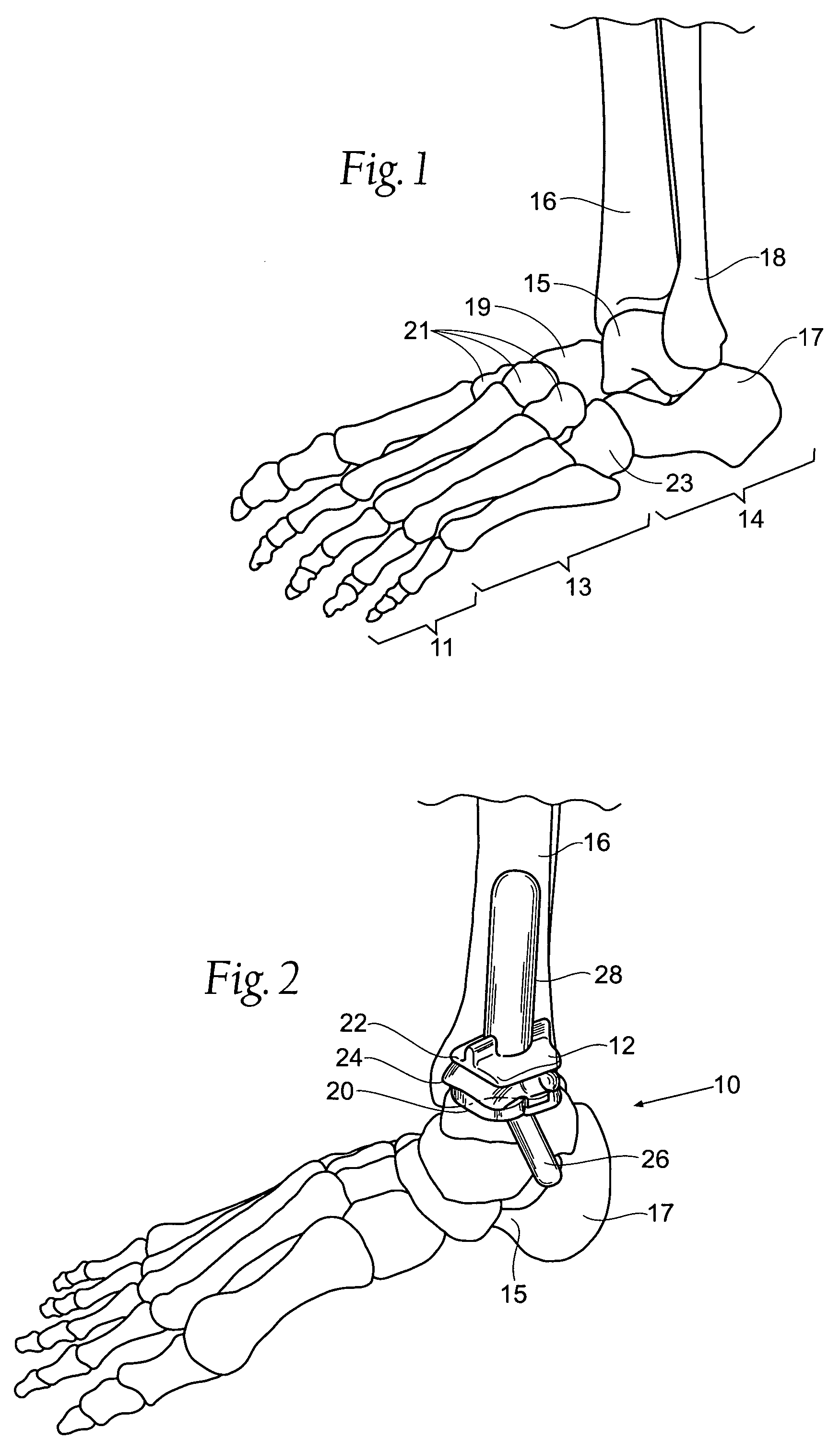
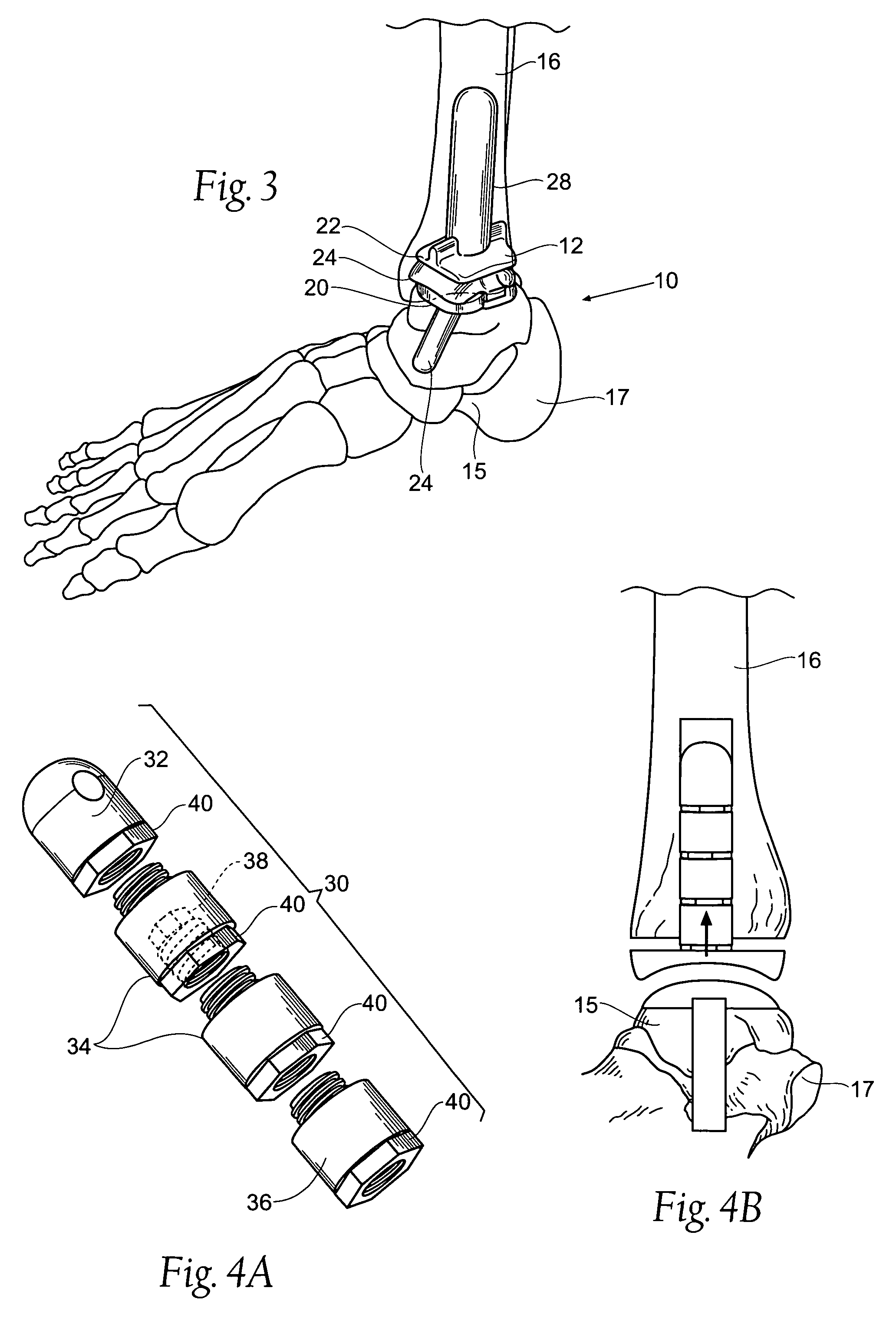
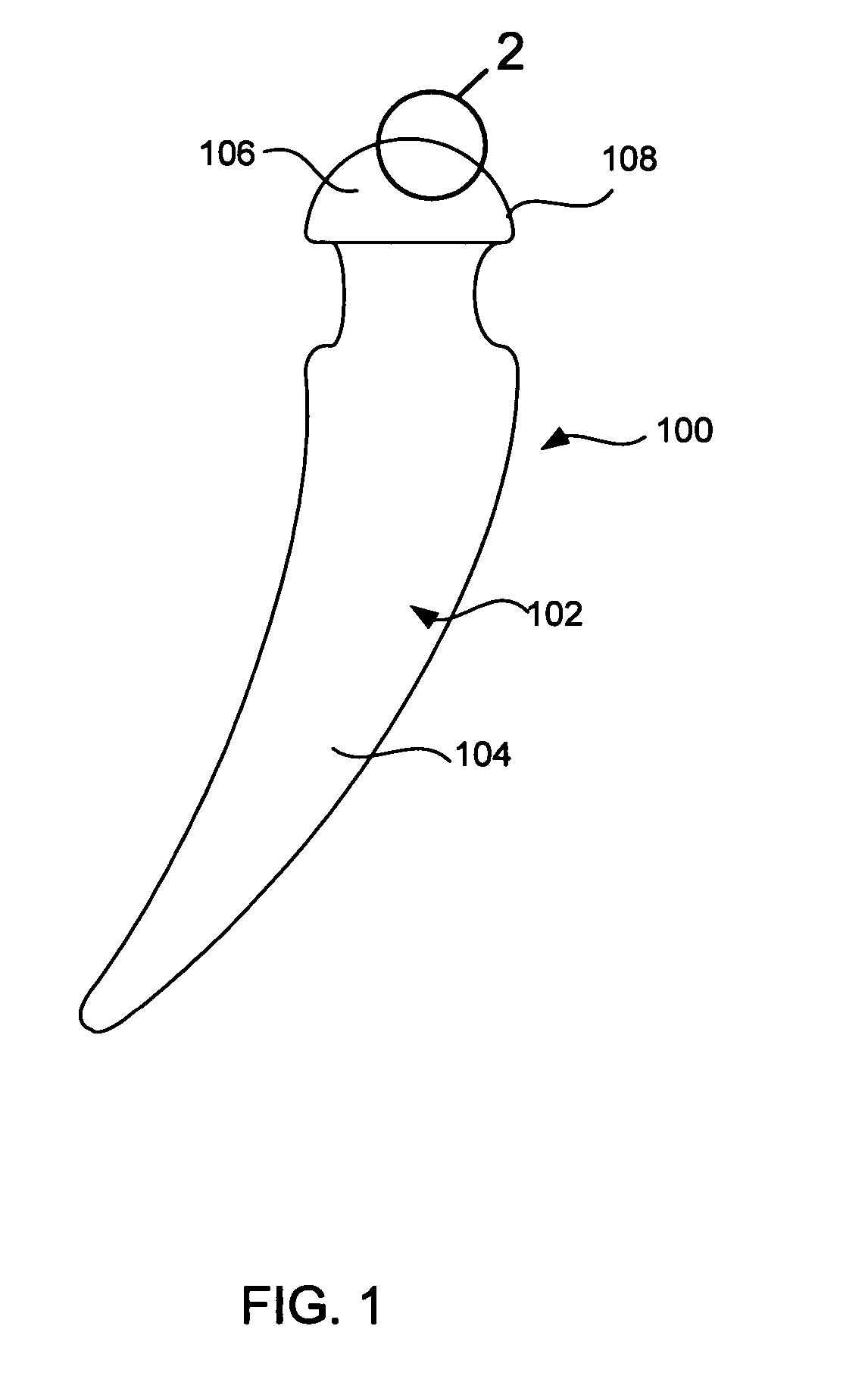
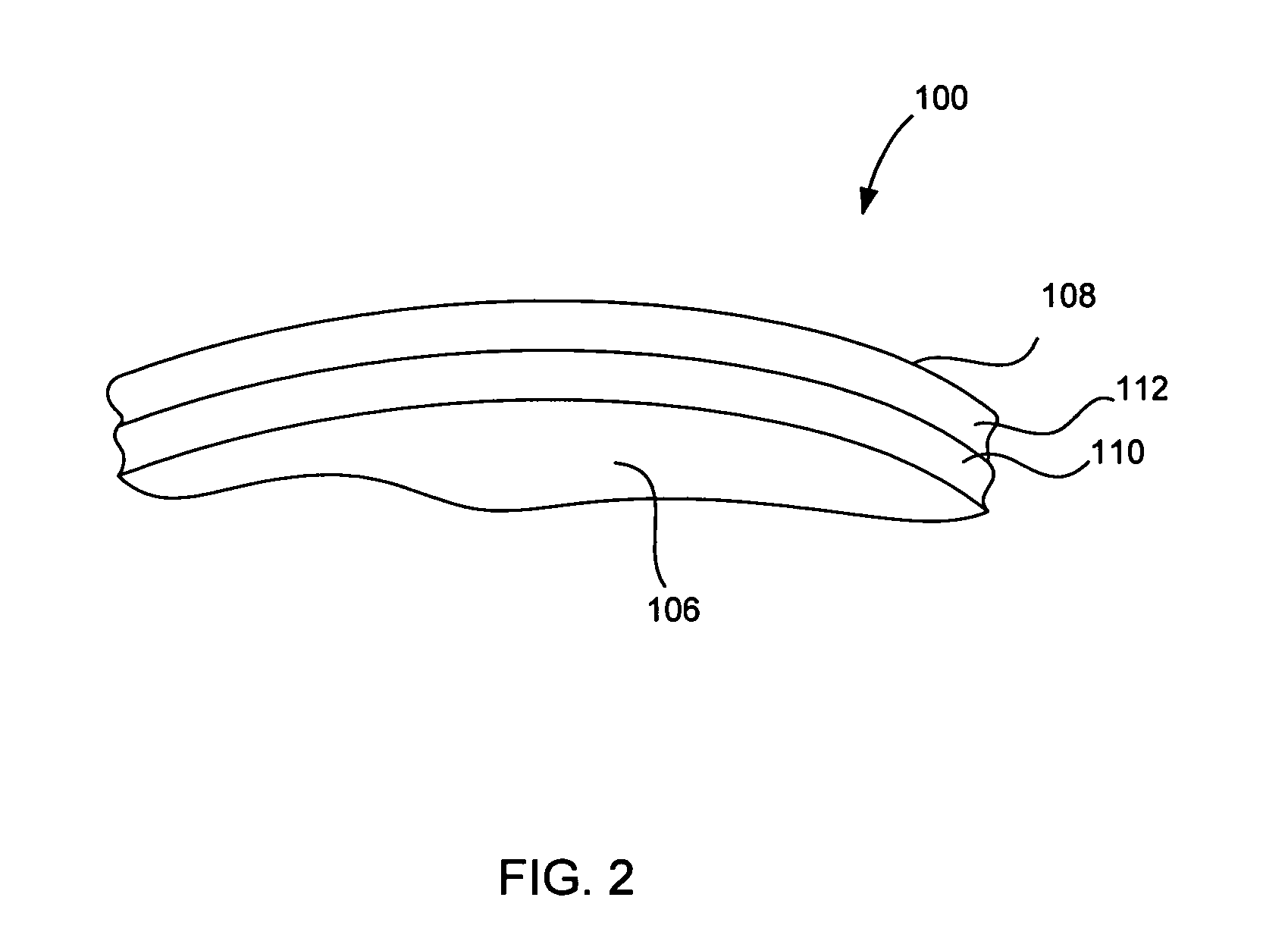
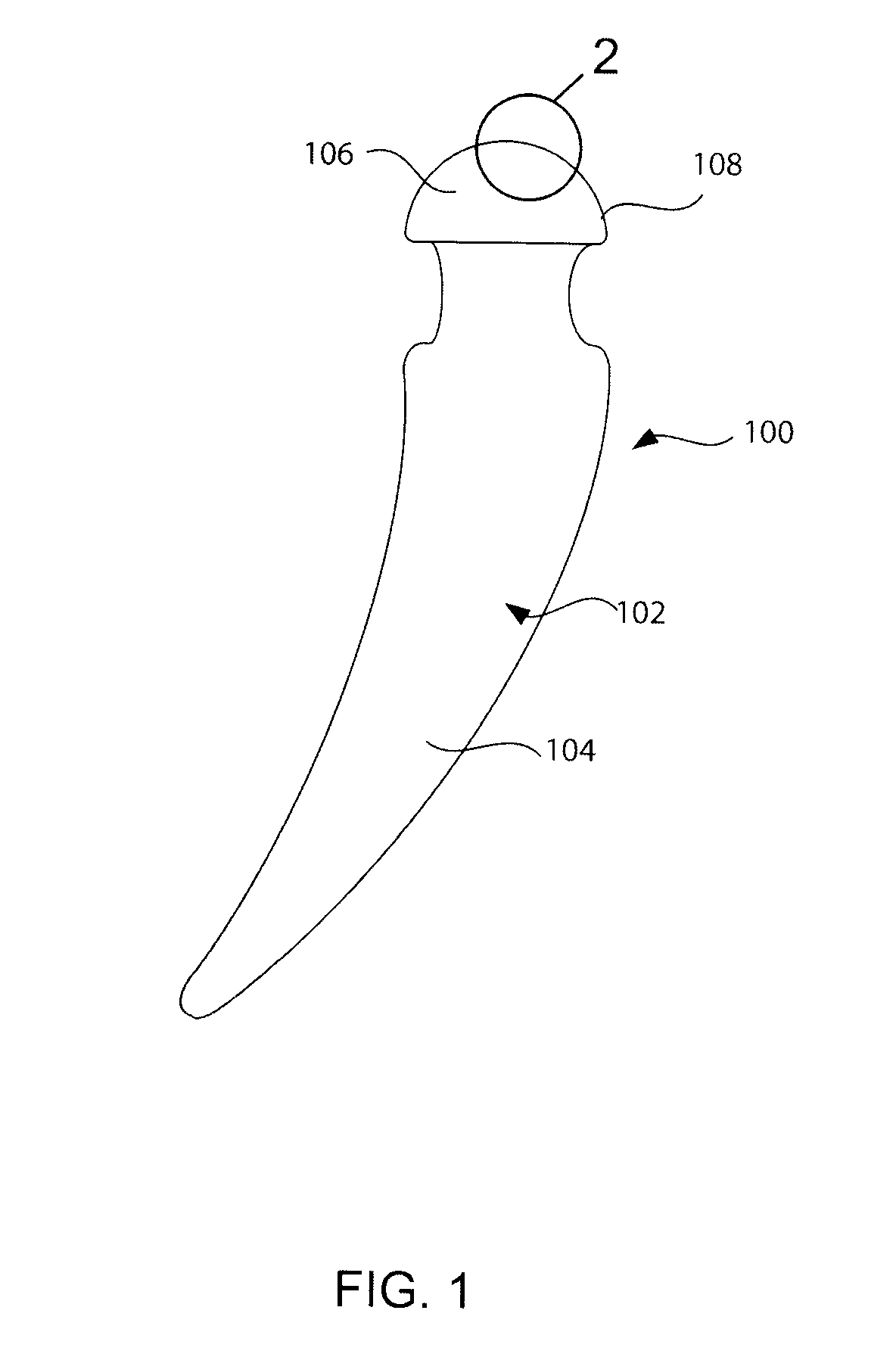
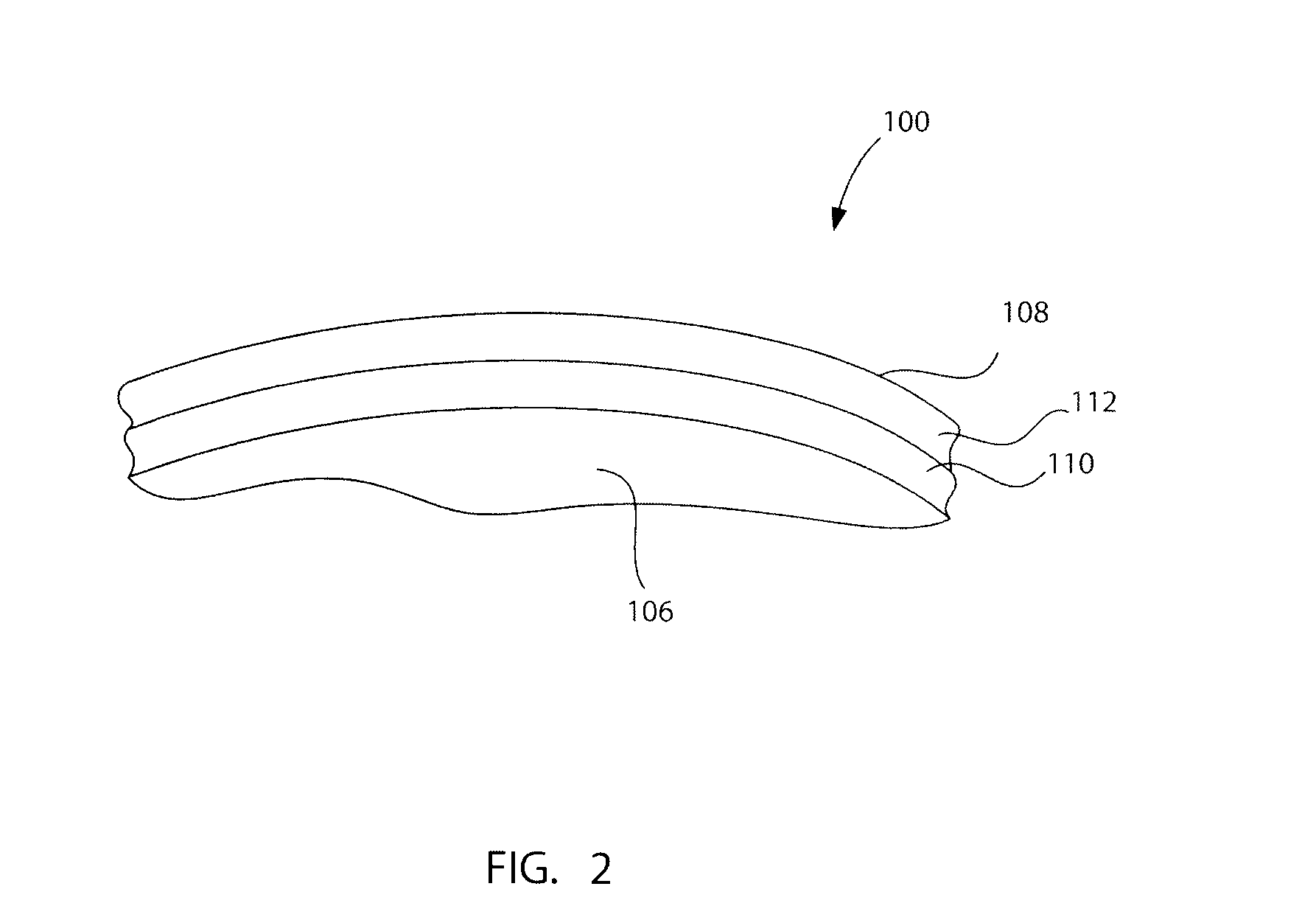
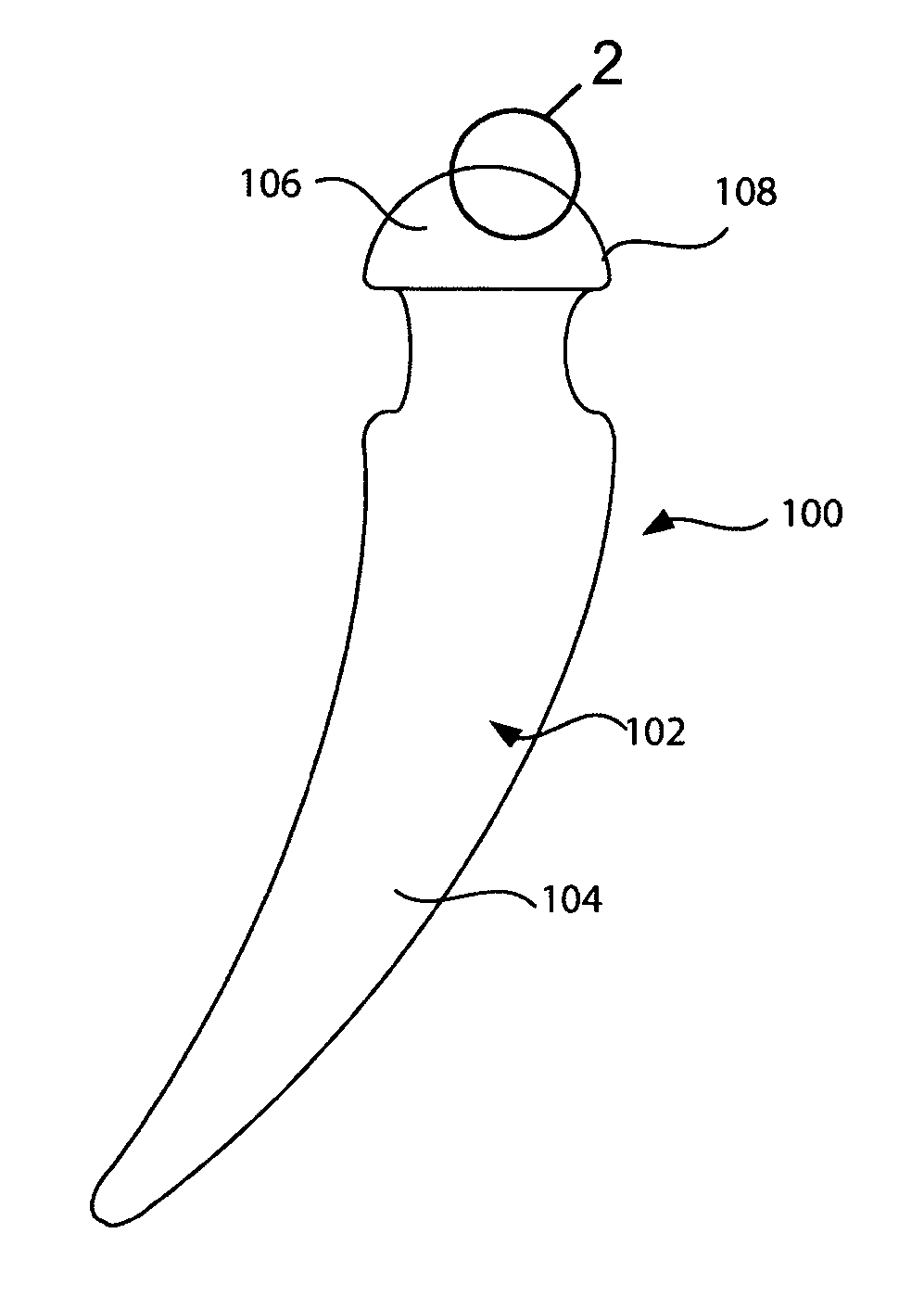
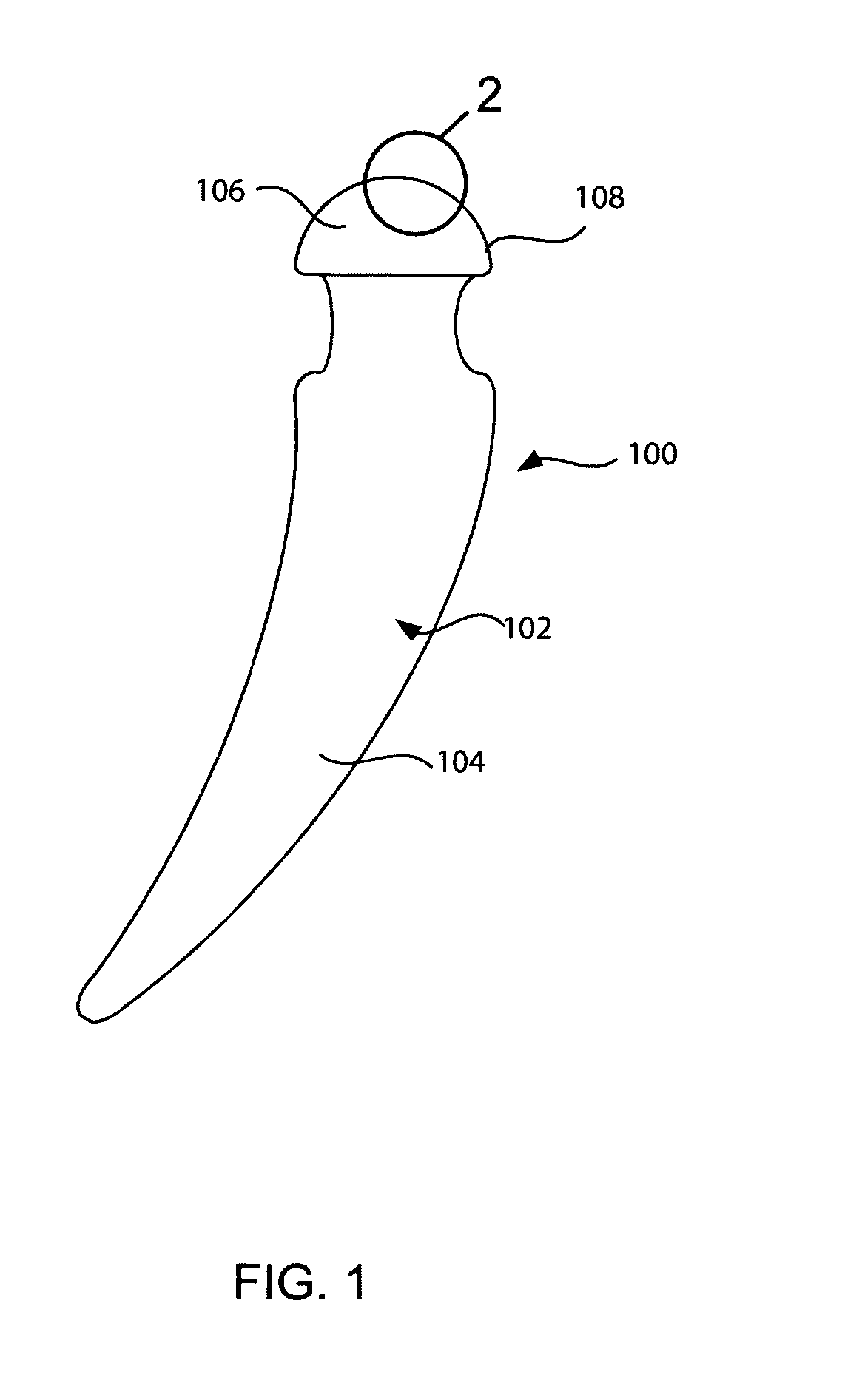
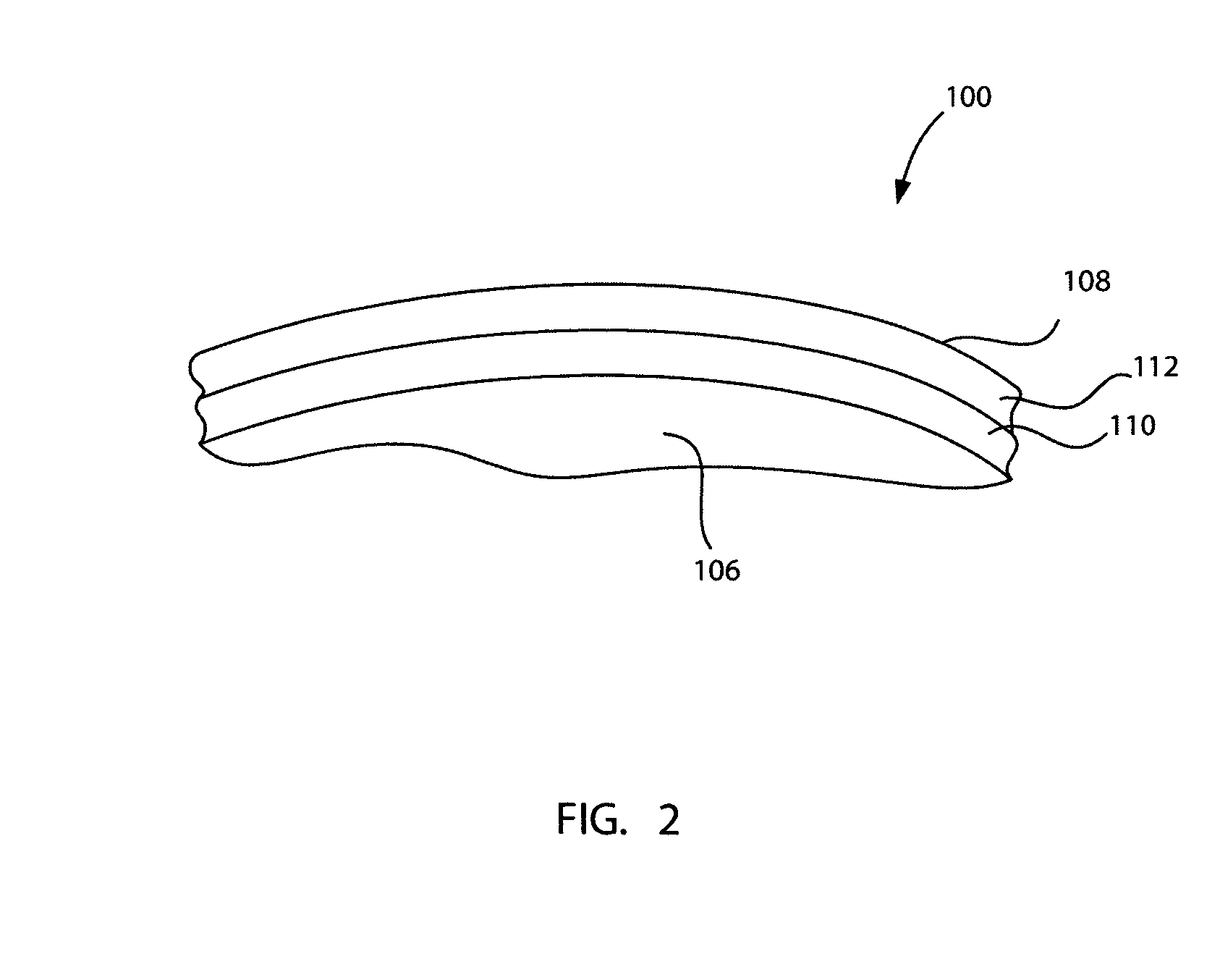
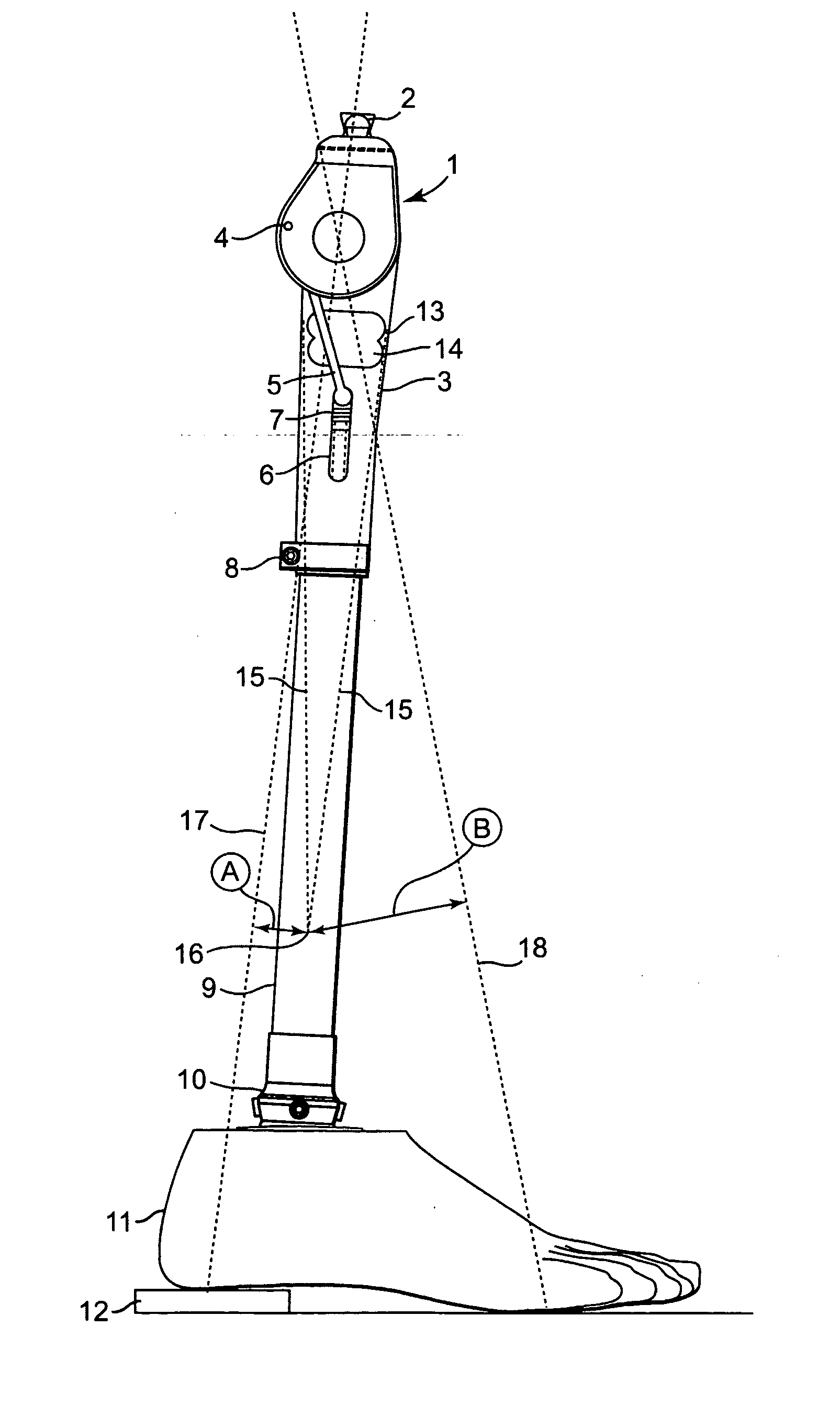
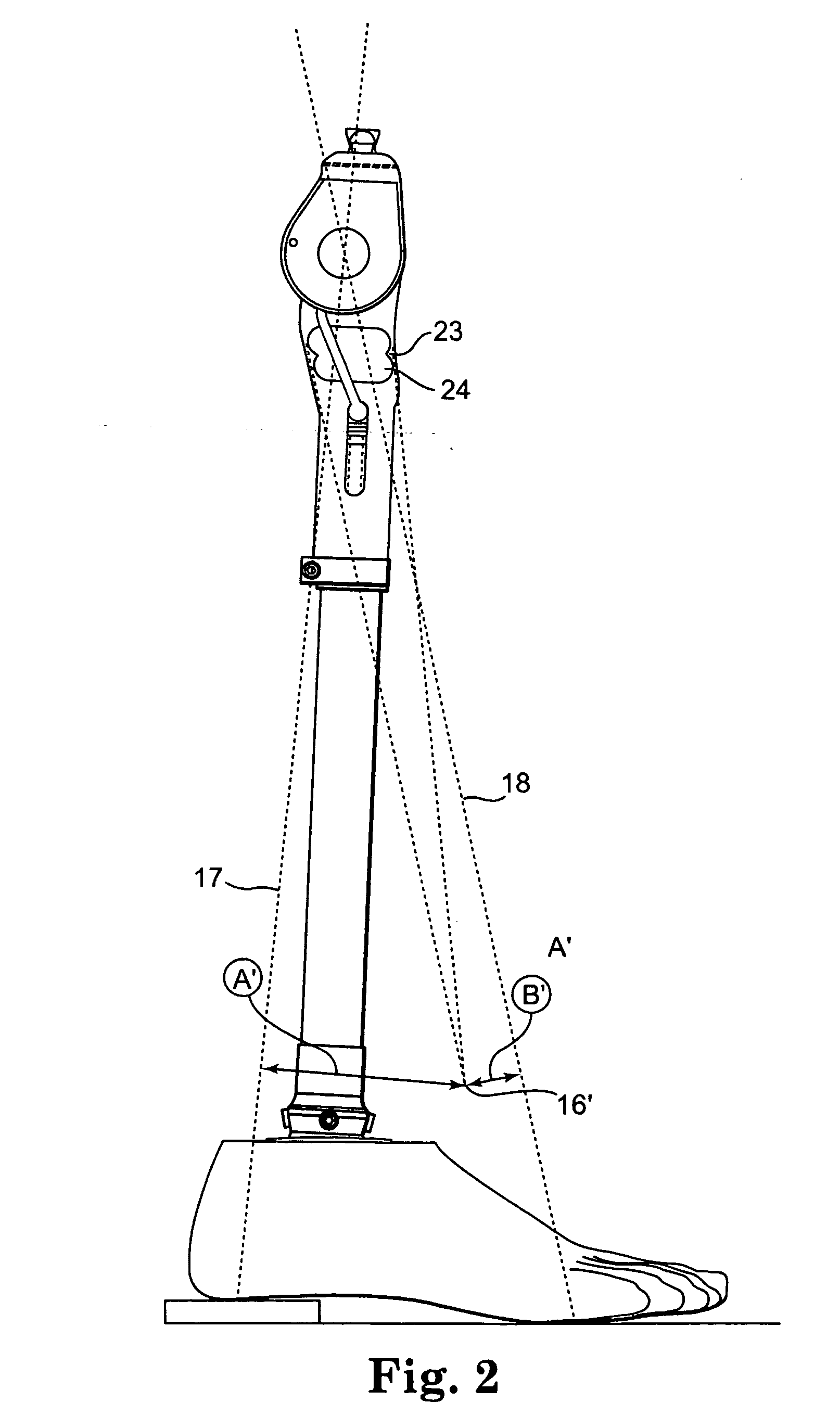
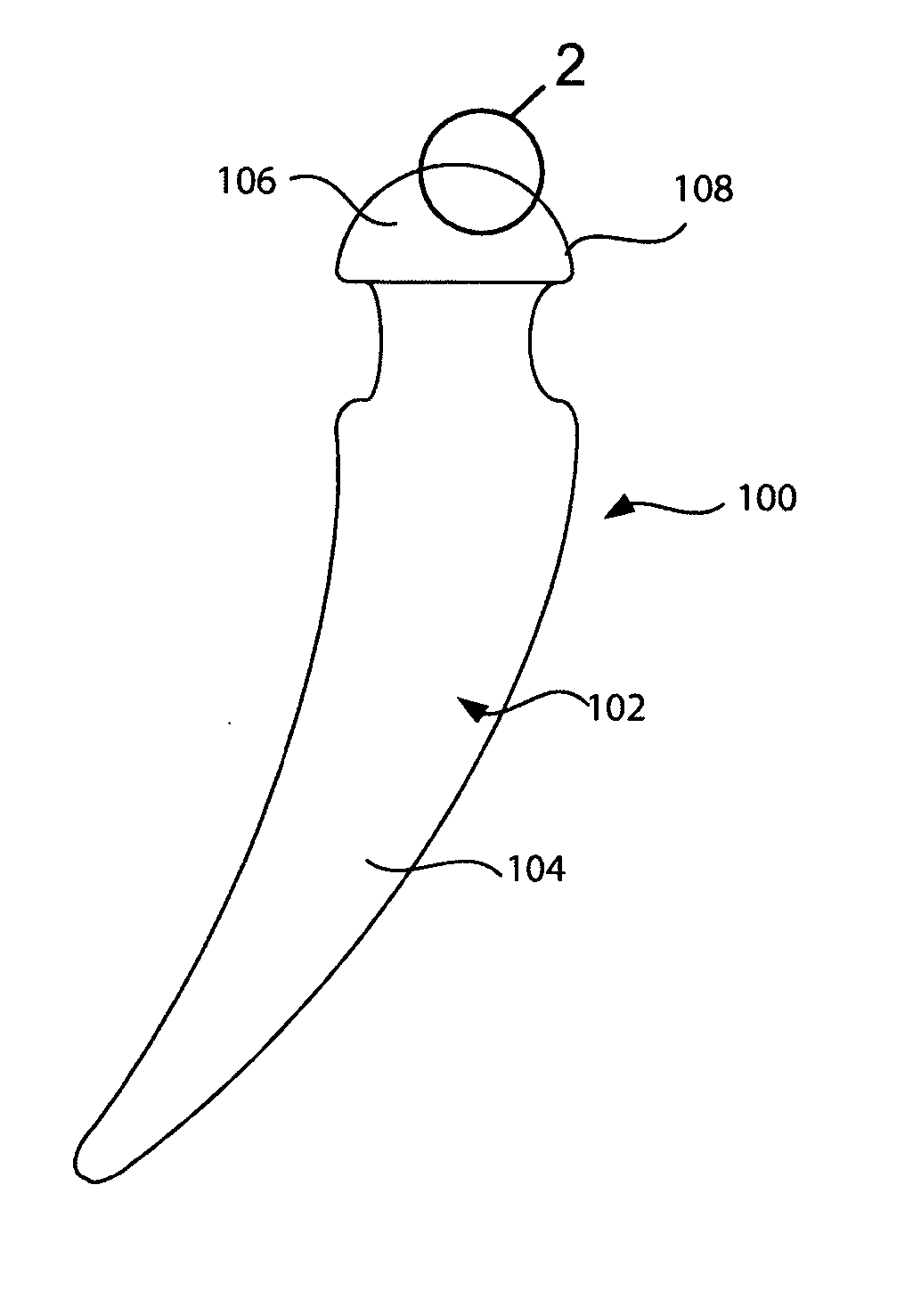
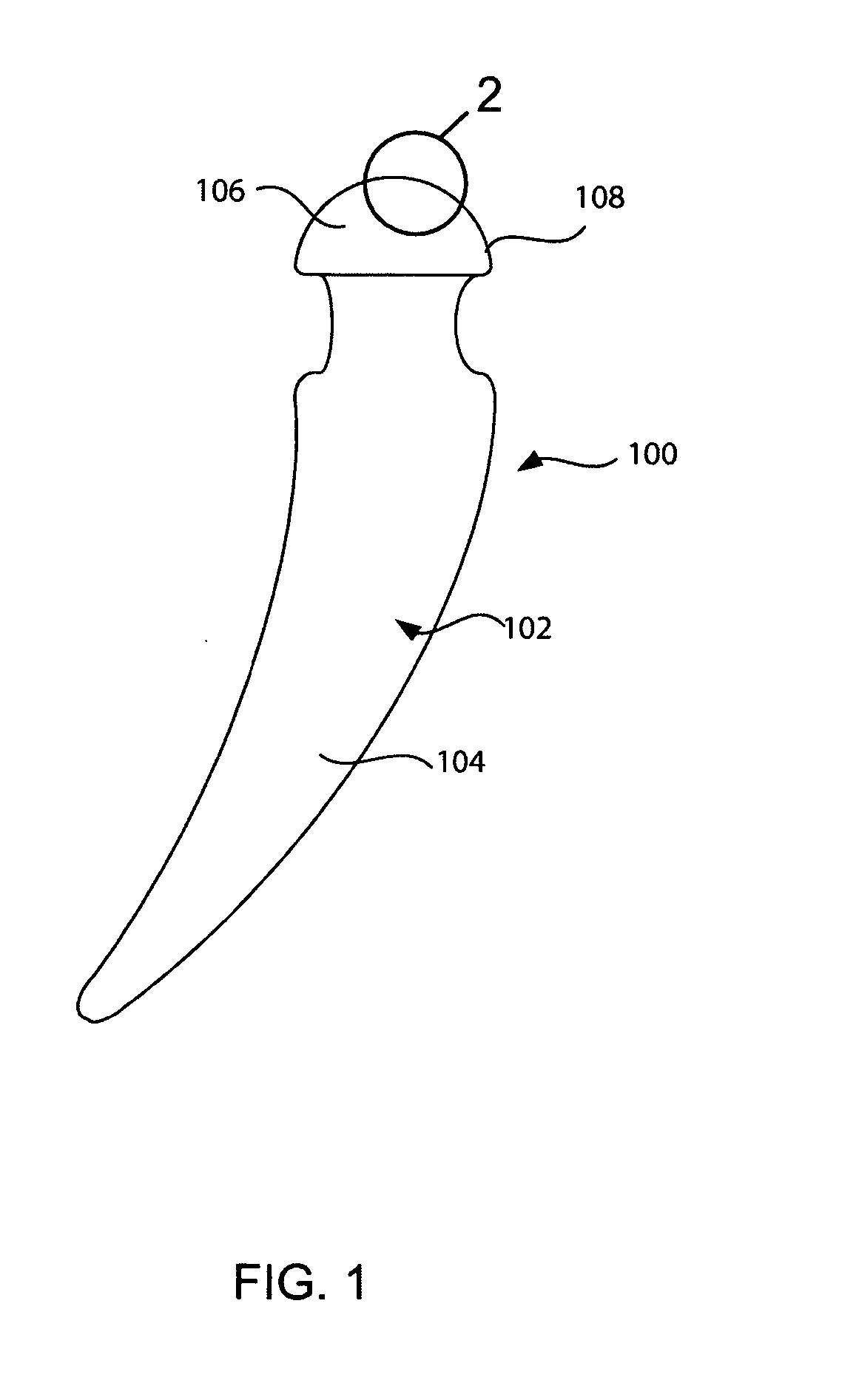
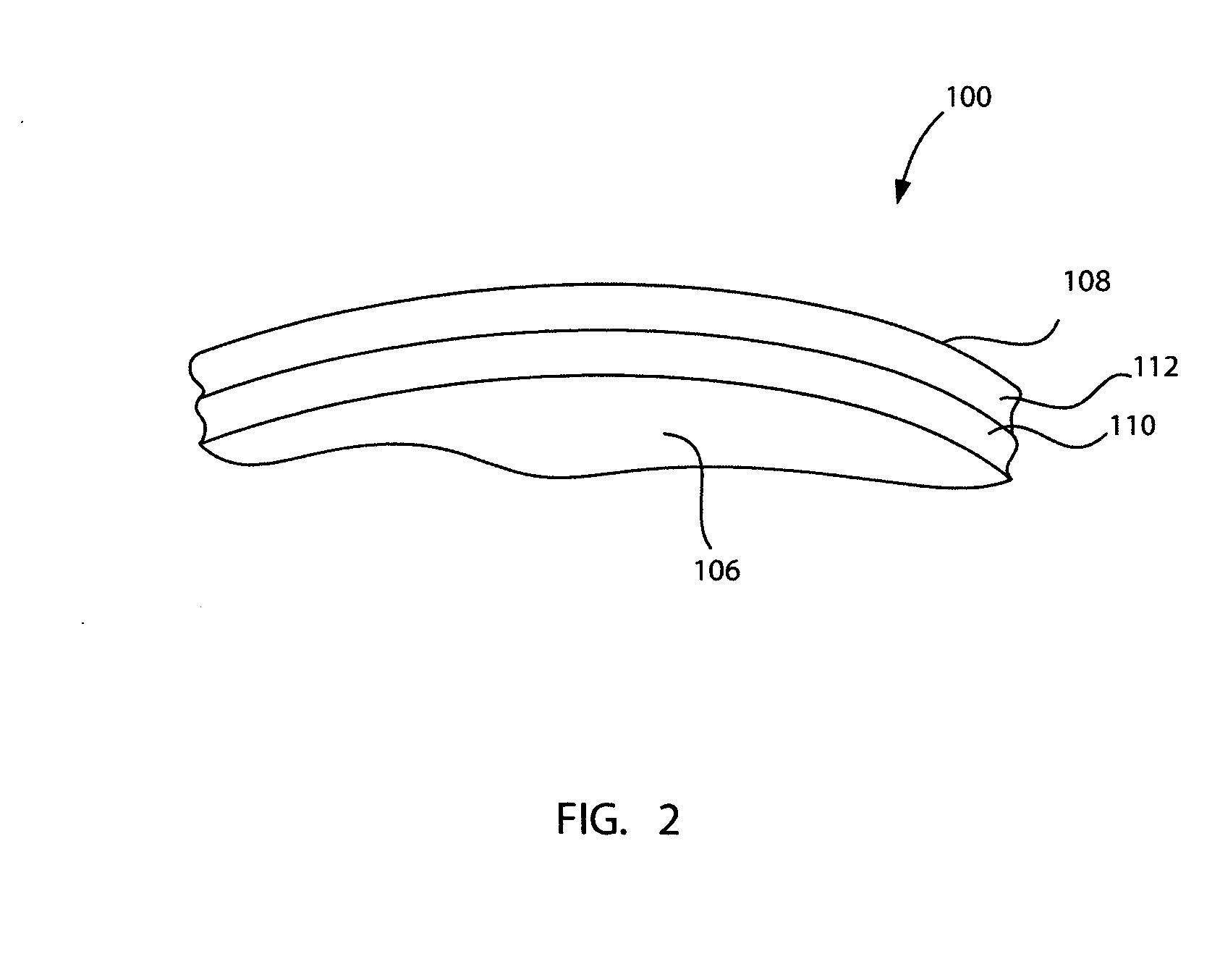
Ankle replacement system
ActiveUS20060229730A1Improved long-term resultPrecise positioningWrist jointsAnkle jointsCalcaneusAnkle joint replacement
A prosthesis suited for orthopedic implantation possesses a multi-piece stem component that supports an artificial joint surface that can articulate with another artificial joint surface in various ways. The prosthesis can be assembled in a snap fit and / or interlocking fashion that provides positive locking means without the use of screws or other fasteners. The prosthesis can accommodate fitment of a plastic joint surface made, e.g., from ultra high molecular weight polyethylene. The prosthesis is well suited for use in an ankle replacement system that can be installed using minimally invasive intramedullary guidance established with respect to the major axis of the tibia by minimally invasive access through the calcaneus, through an incision in the bottom of the foot. The prosthesis makes possible the installation of a total ankle system using minimally invasive anterior access to the ankle joint for making bony cuts and to install prosthesis components.
Owner:INBONE TECH
Ankle replacement system
ActiveUS7534246B2Function maximizationMaximize longevityWrist jointsAnkle jointsArticular surfacesAnkle joint replacement
A prosthesis suited for orthopedic implantation possesses a multi-piece stem component that supports an artificial joint surface that can articulate with another artificial joint surface in various ways. The prosthesis can be assembled in a snap fit and / or interlocking fashion that provides positive locking means without the use of screws or other fasteners. The prosthesis can accommodate fitment of a plastic joint surface made, e.g., from ultra high molecular weight polyethylene. The prosthesis is well suited for use in an ankle replacement system that can be installed using minimally invasive intramedullary guidance established with respect to the major axis of the tibia by minimally invasive access through the calcaneus, through an incision in the bottom of the foot. The prosthesis makes possible the installation of a total ankle system using minimally invasive anterior access to the ankle joint for making bony cuts and to install prosthesis components.
Owner:INBONE TECH
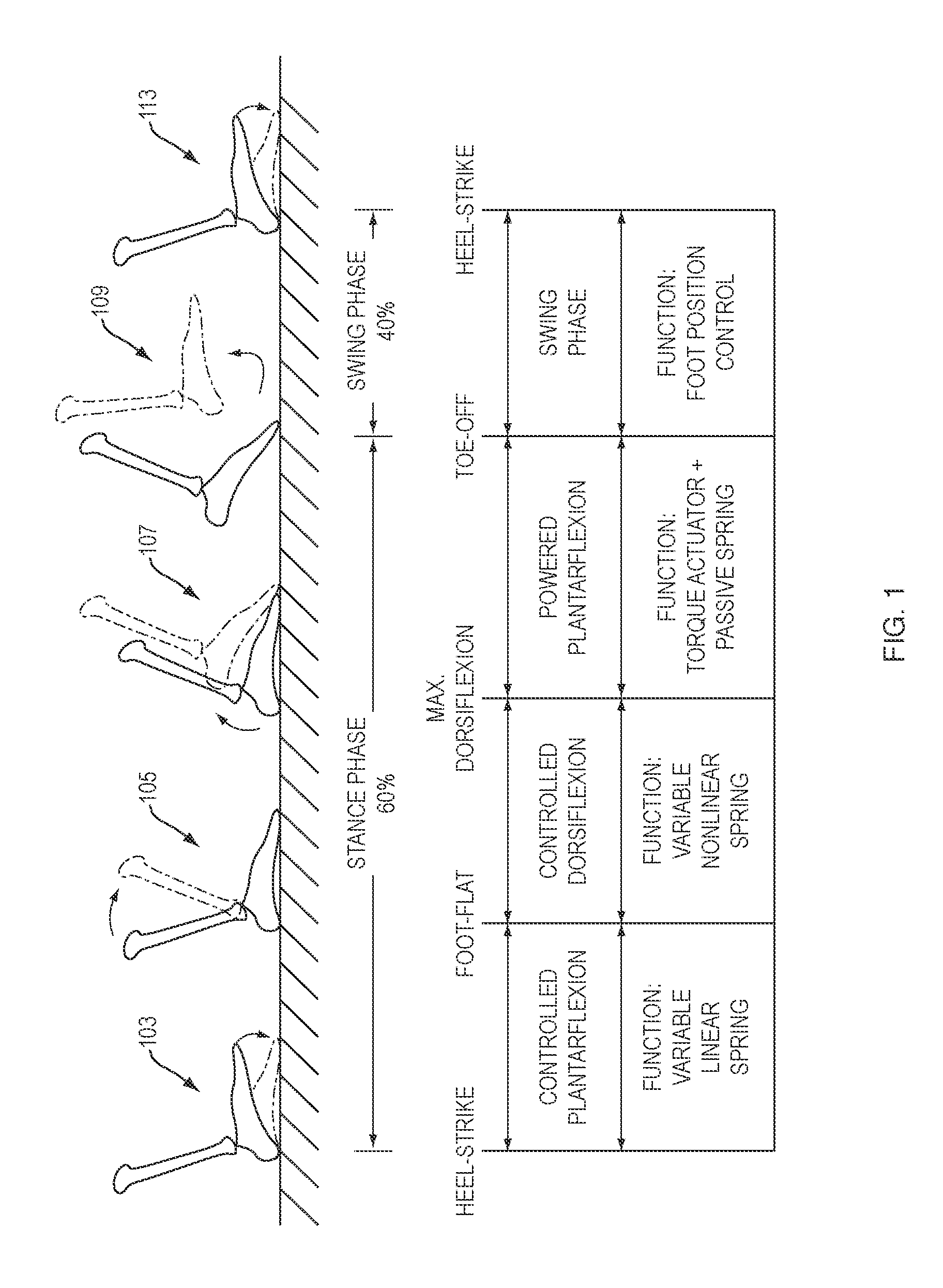
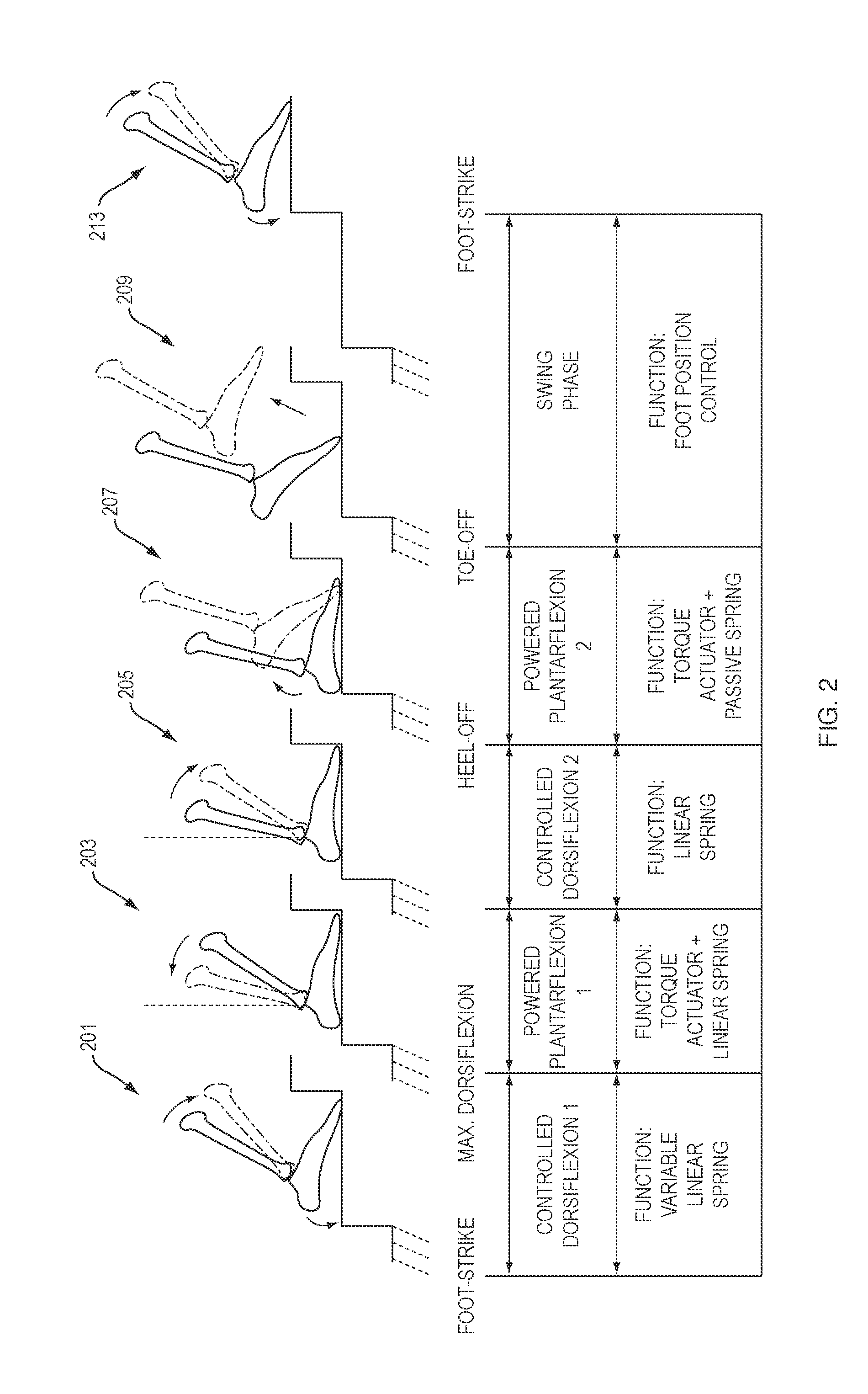
Artificial Human Limbs and Joints Employing Actuators, Springs, and Variable-Damper Elements
ActiveUS20110264230A1Improve performanceLight weightJoint implantsArtificial legsMusculoskeletal structureArtificial joints
Biomimetic Hybrid Actuators employed in biologically-inspired musculoskeletal architectures employ an electric motor for supplying positive energy to and storing negative energy from an artificial joint or limb, as well as elastic elements such as springs, and controllable variable damper components, for passively storing and releasing energy and providing adaptive stiffness to accommodate level ground walking as well as movement on stairs and surfaces having different slopes.
Owner:MASSACHUSETTS INST OF TECH
Tibia plateau for a replacement joint
ActiveUS7066963B2Restrict movementAvoid lateral displacementJoint implantsKnee jointsTibiaArticular surfaces
Owner:LIMA CORPORATE SPA
Laser based metal deposition of implant structures
InactiveUS7001672B2Minimize adverse effectsFine grain structureFinger jointsDental implantsArtificial jointsWear resistant
Owner:MEDICINELODGE
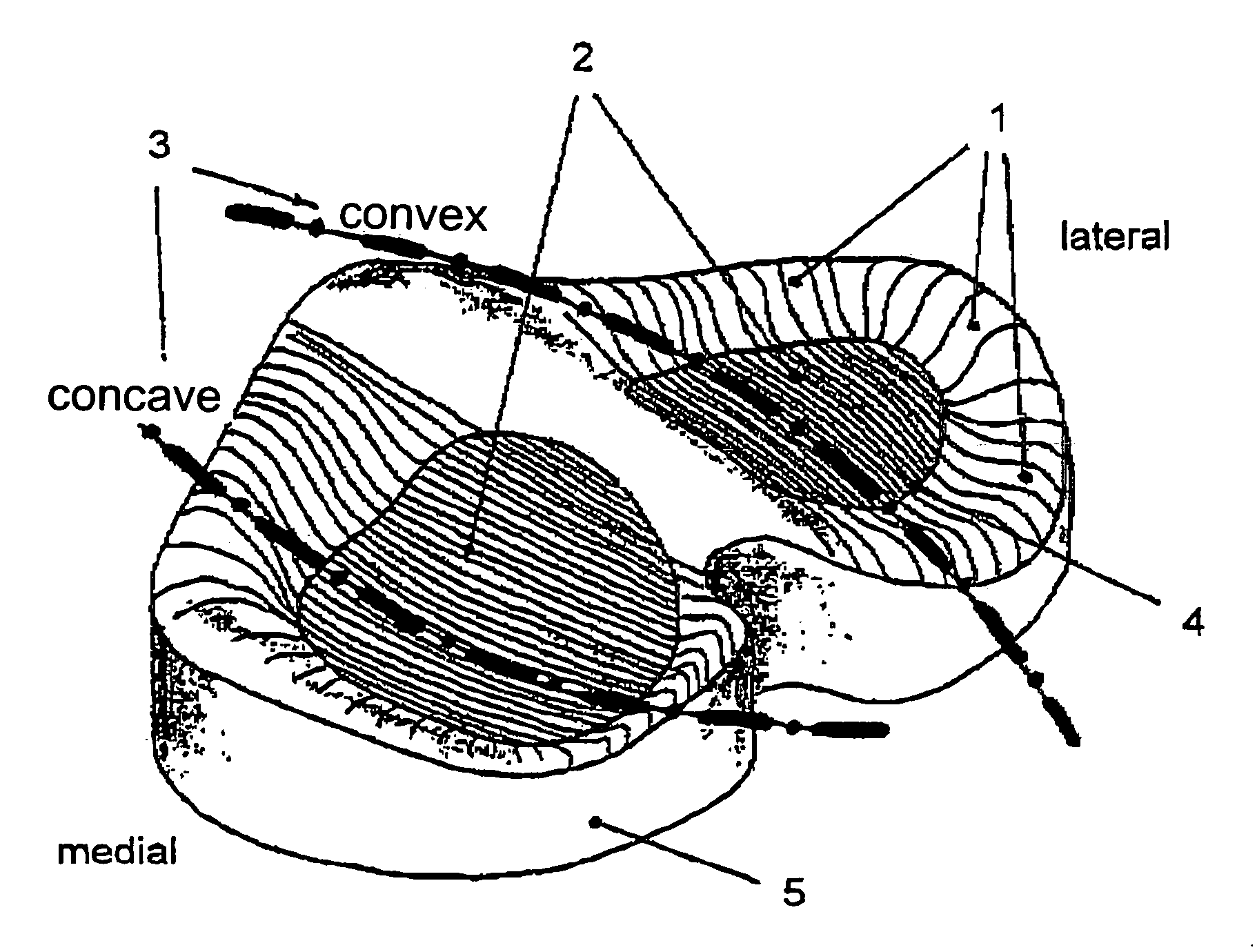
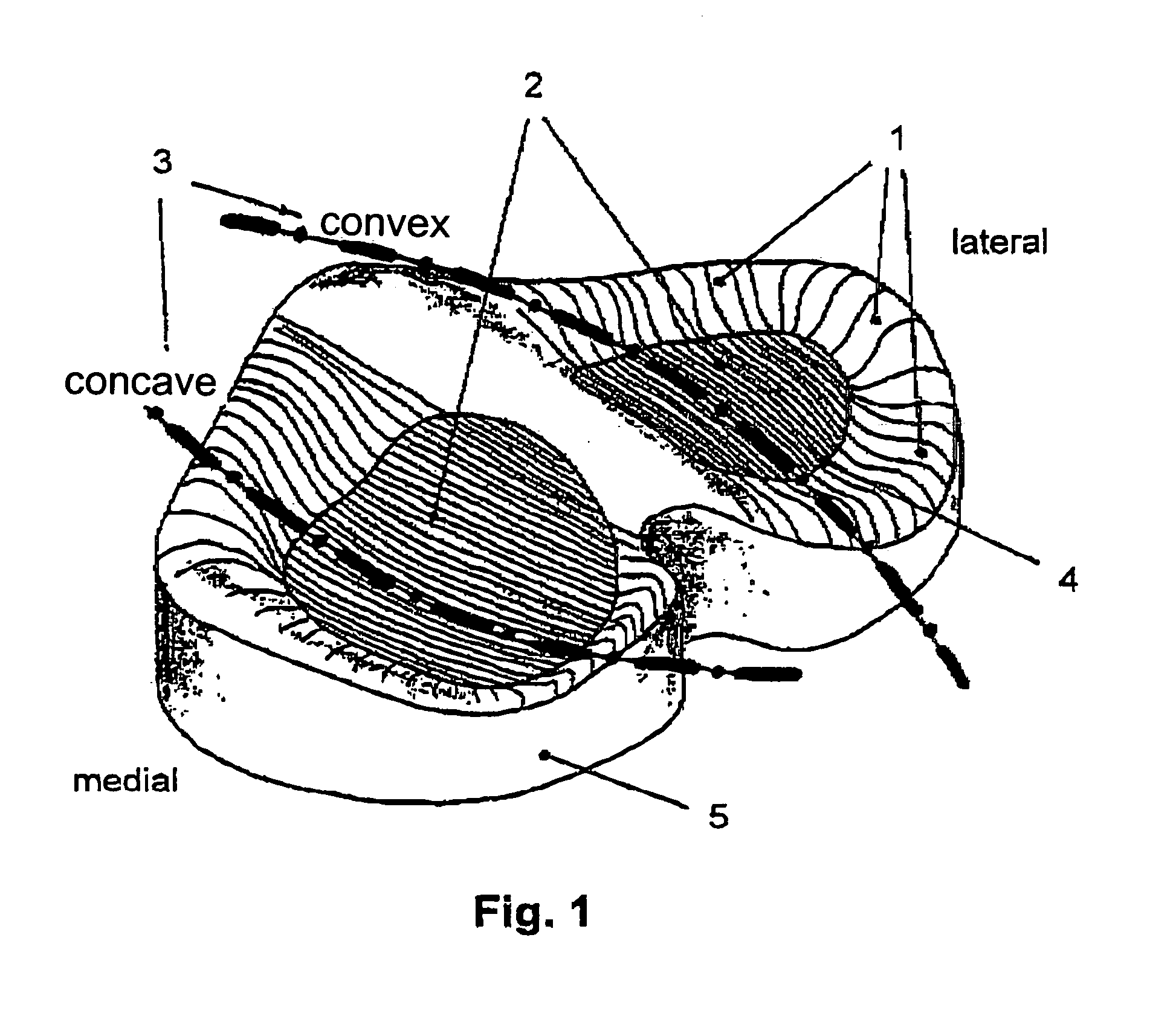
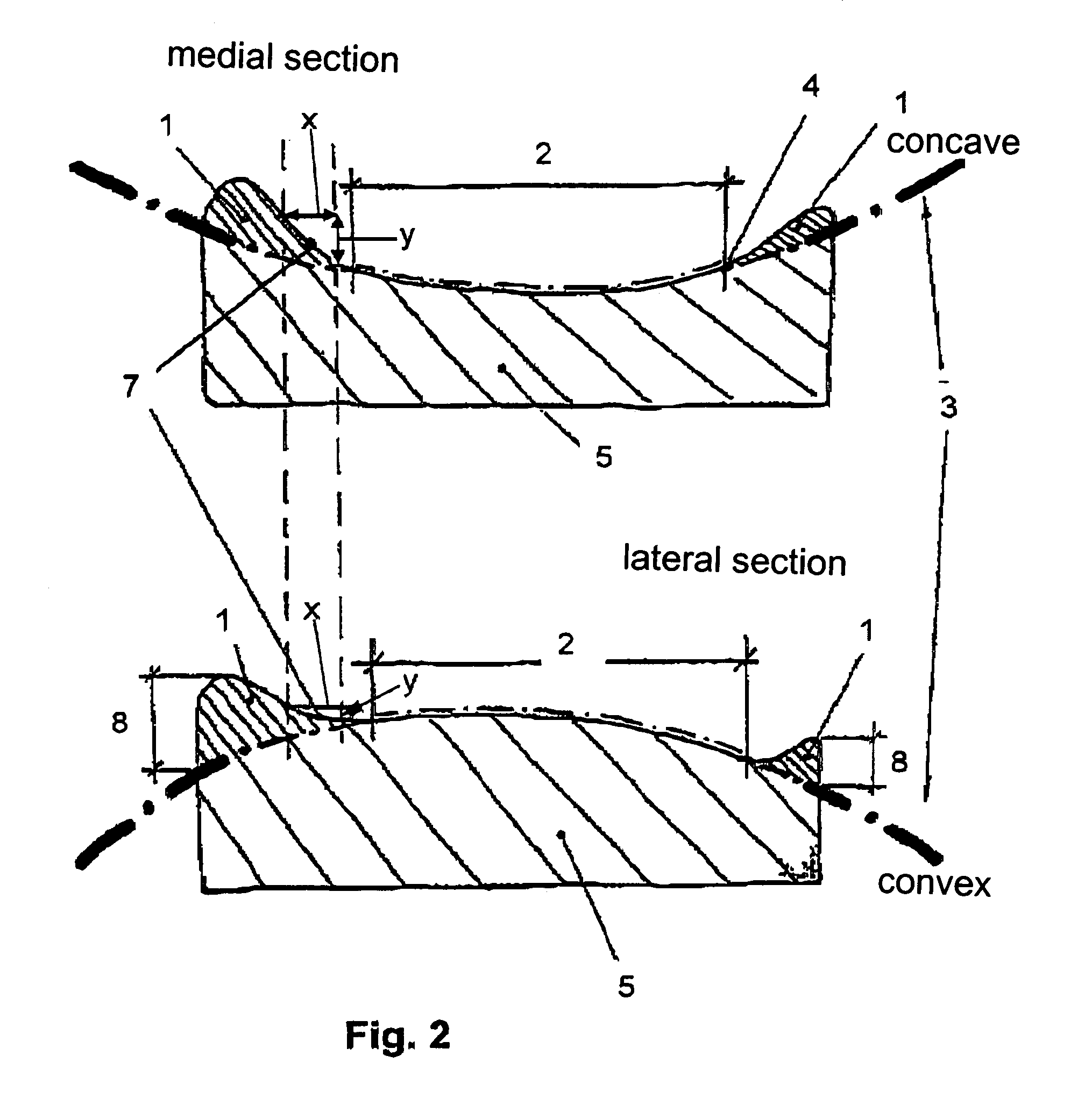
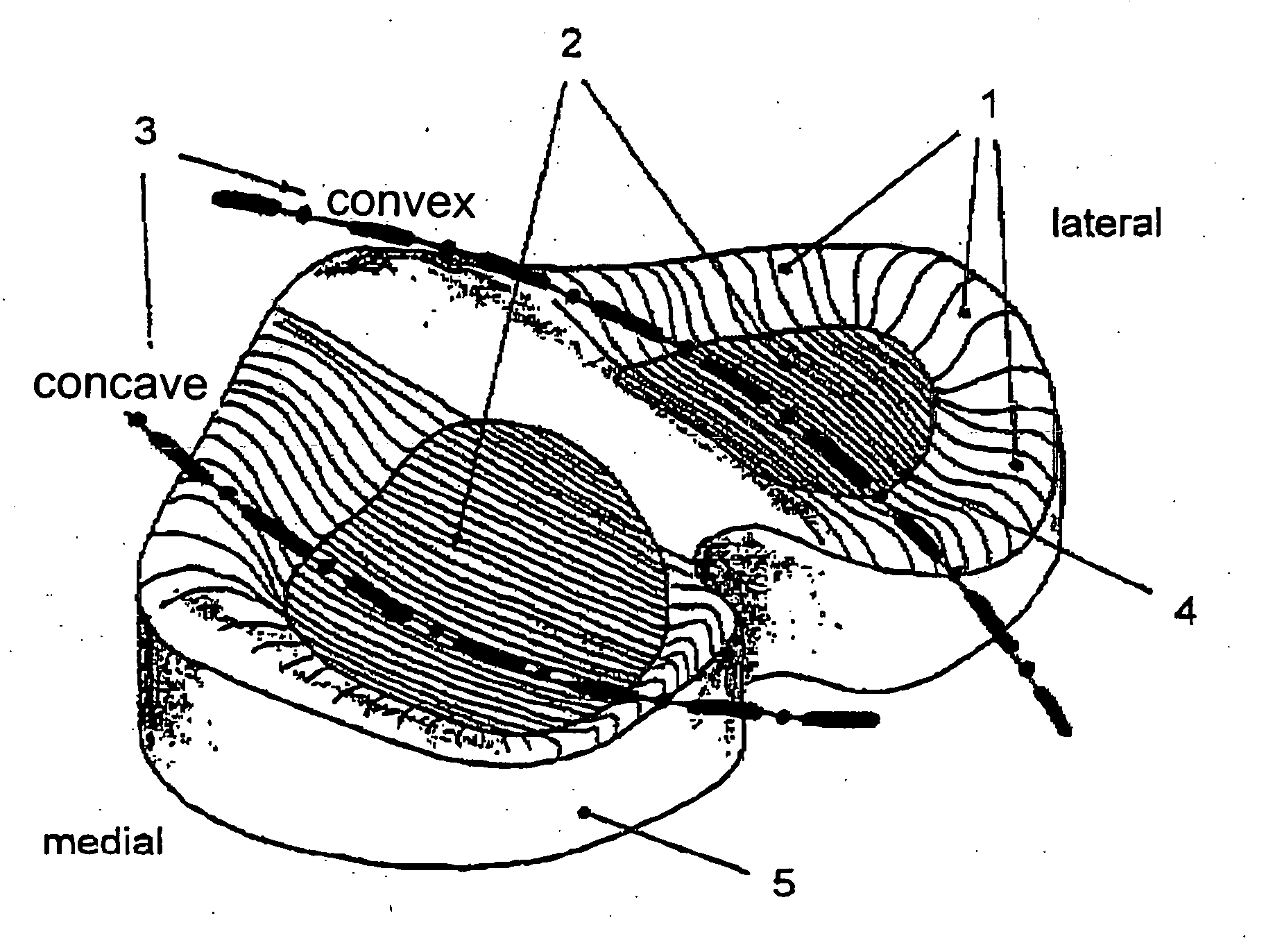
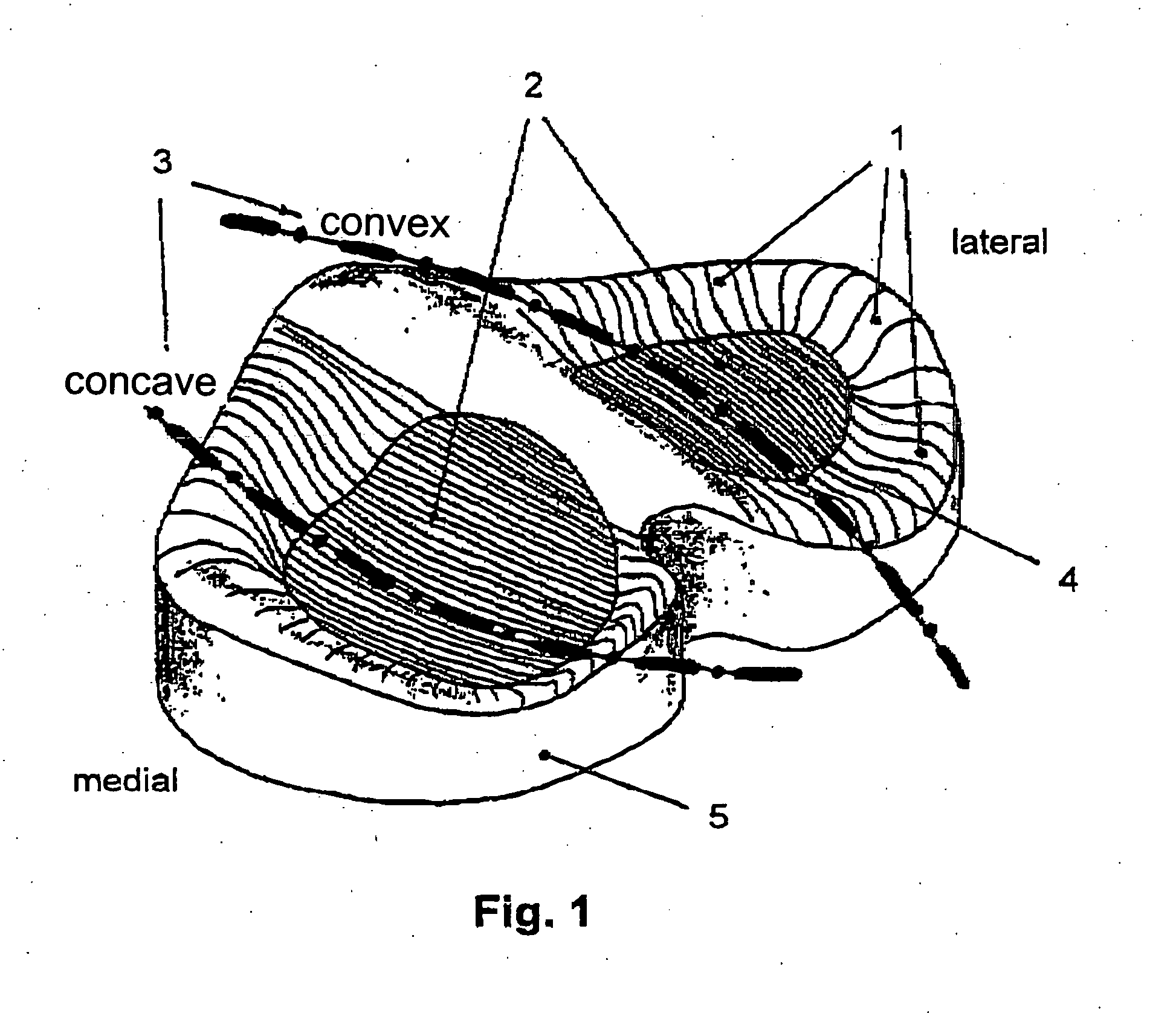
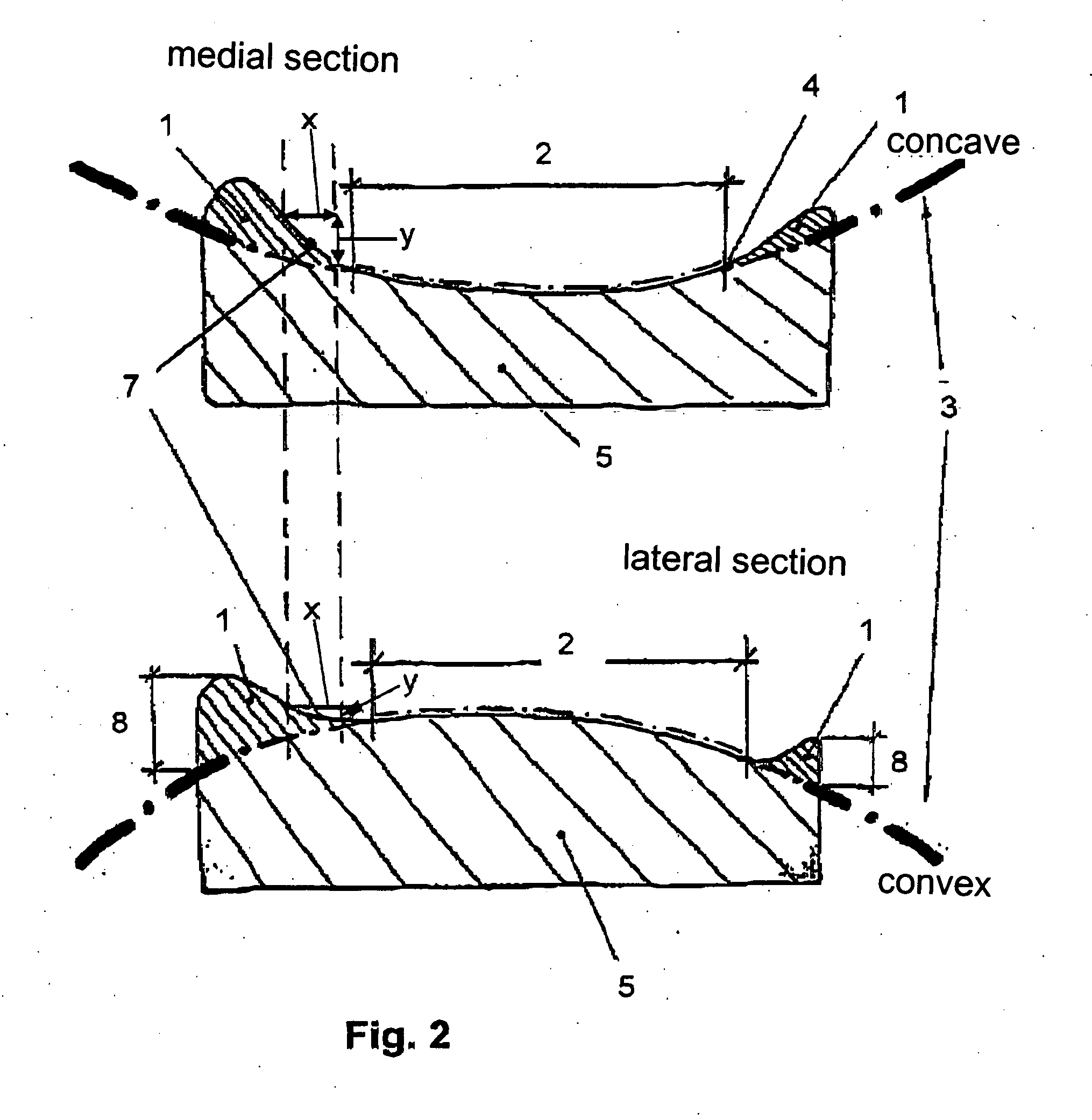
Tibia plateau for a replacement joint
ActiveUS20050197710A1Restrict movementAvoid lateral displacementJoint implantsKnee jointsTibiaArtificial joints
A tibia plateau for a replacement joint, particularly an endoprosthesis for a human knee joint, in which the head and socket artificial joint parts have convex and concave articulation surfaces, respectively, and the articulation surfaces are arranged in pairs, so that the functional surfaces which are formed can roll against one another along a curved contact line, especially a circularly arcuate contact line, formed on each articulation surface. A gently sloping bulge (1) is formed in the area (4) adjacent the functional surfaces (2) which bulge prevents excessive rolling movement and lateral displacement of the joint parts relative to each other.
Owner:LIMA CORPORATE SPA
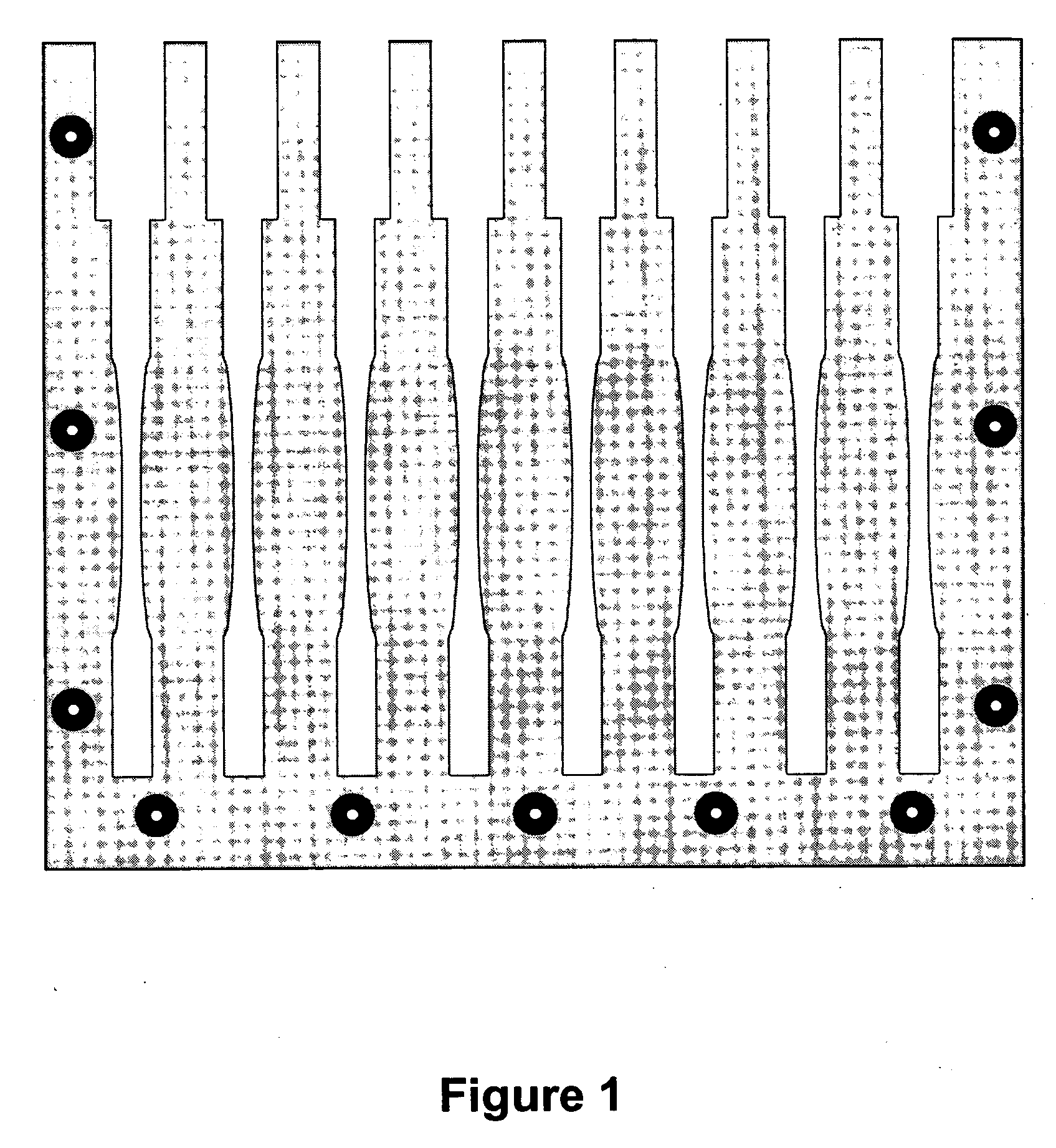
Contact sensors and methods for making same
InactiveUS20060184067A1SurgeryForce measurementElectrical resistance and conductanceArtificial joints
The present invention is directed to novel contact sensors. The contact sensors of the invention include a conductive composite material formed of a polymer and a conductive filler. In one particular embodiment, the composite materials can include less than about 10 wt % conductive filler. Thus, the composite material of the contact sensors can have physical characteristics essentially identical to the polymer, while being electrically conductive with the electrical resistance proportional to the load on the sensor. If desired, the sensors can be formed of the same polymeric material as the bearing that is being examined. The sensors can provide real time dynamic contact information for joint members under conditions expected during use. In one particular embodiment, the sensors can be used to examine dynamic wear characteristics of artificial joint bearings such as artificial knee, hip, or shoulder bearings.
Owner:CLEMSON UNIV RES FOUND
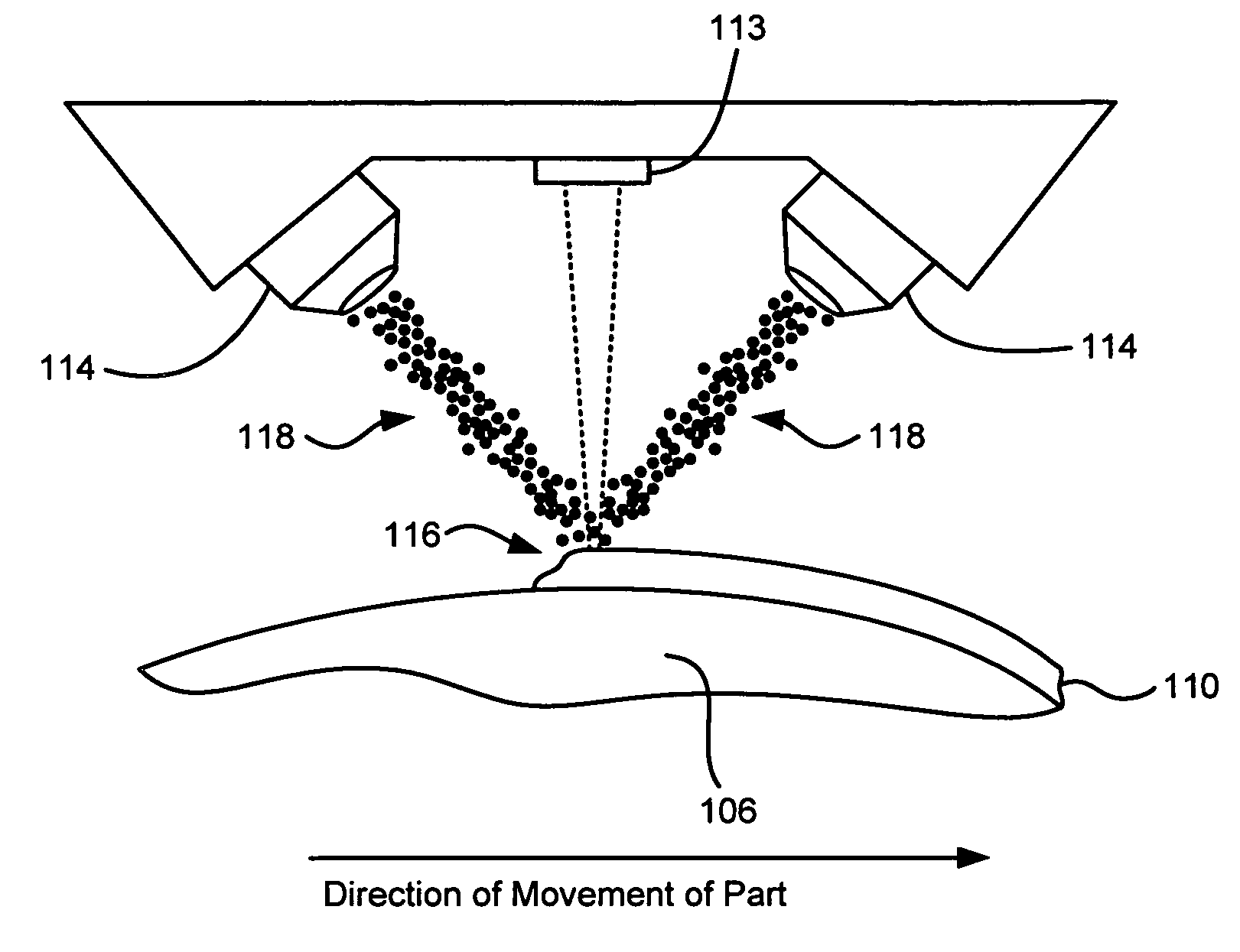
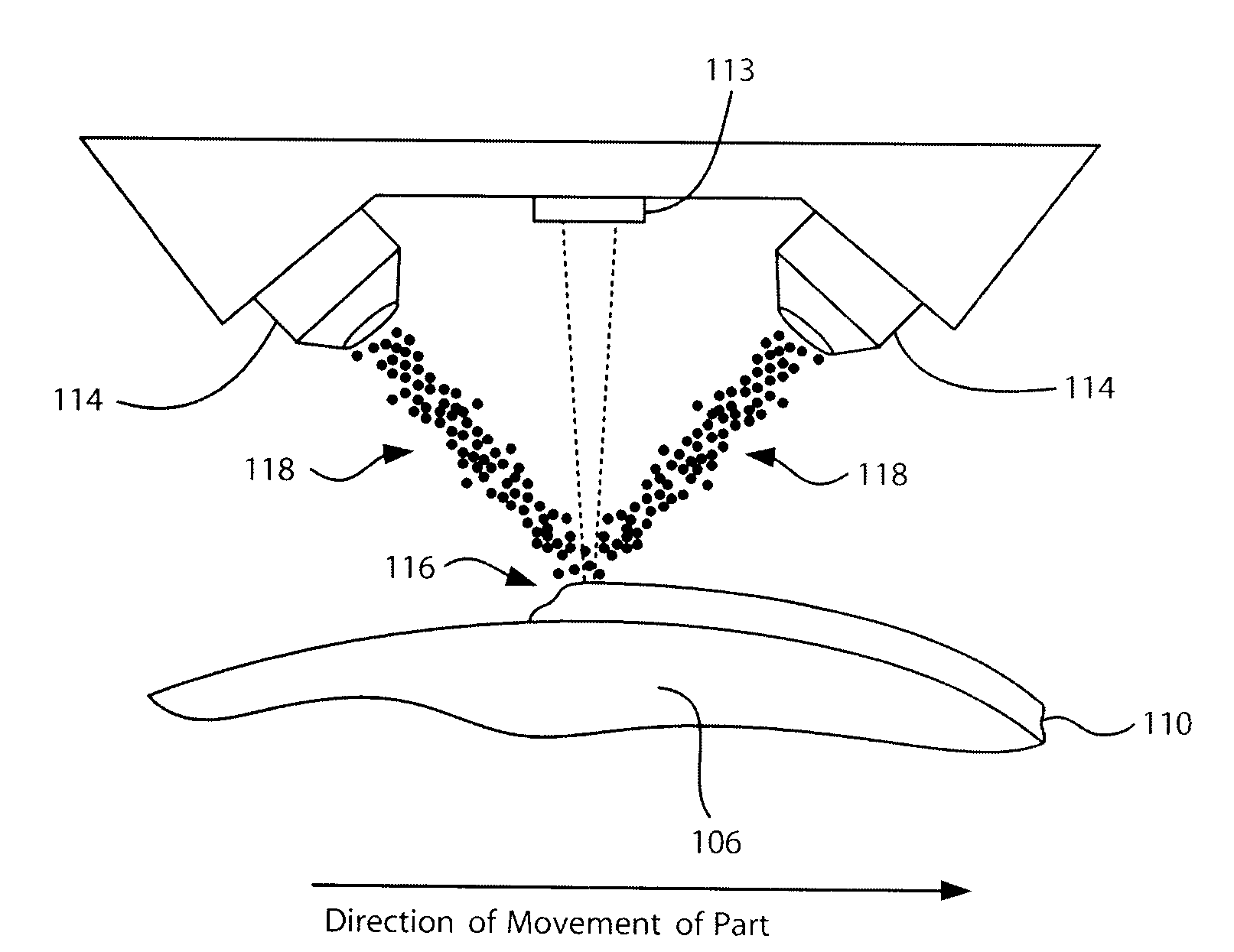
Laser based metal deposition (LBMD) of antimicrobials to implant surfaces
InactiveUS20070287027A1Improved bearing propertyImprove propertiesFinger jointsDental implantsWear resistantBearing surface
A method is provided for depositing a hard wear resistant surface onto a porous or non-porous base material of a medical implant. The wear resistant surface of the medical implant device may be formed by a Laser Based Metal Deposition (LBMD) method such as Laser Engineered Net Shaping (LENS). The wear resistant surface may include a blend of multiple different biocompatible materials. Further, functionally graded layers of biocompatible materials may be used to form the wear resistant surface. Usage of a porous material for the base may promote bone ingrowth to allow the implant to fuse strongly with the bone of a host patient. The hard wear resistant surface provides device longevity, particularly when applied to bearing surfaces such as artificial joint bearing surfaces or a dental implant bearing surfaces. An antimicrobial material such as silver may be deposited in combination with a metal to form an antimicrobial surface deposit.
Owner:MEDICINELODGE
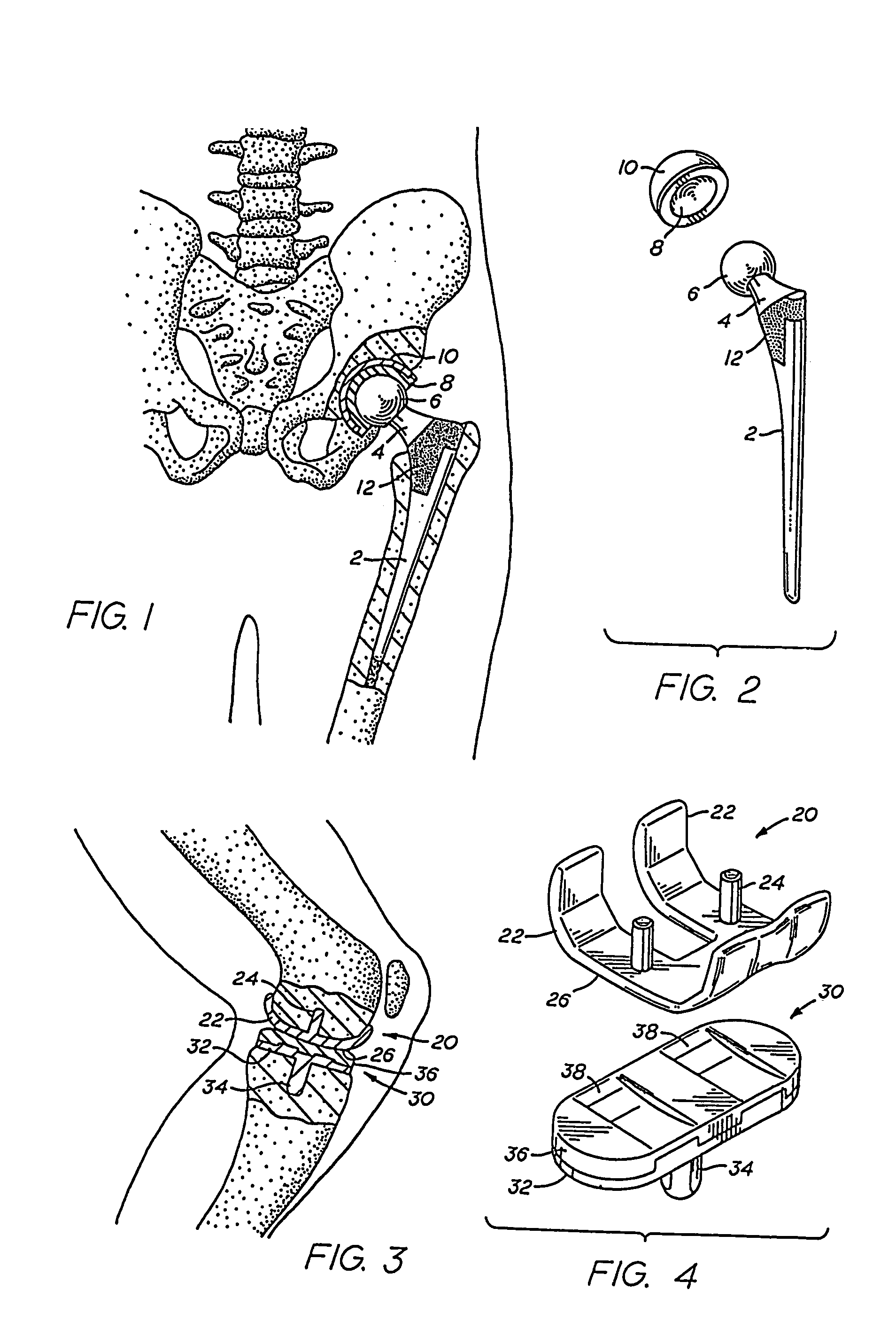
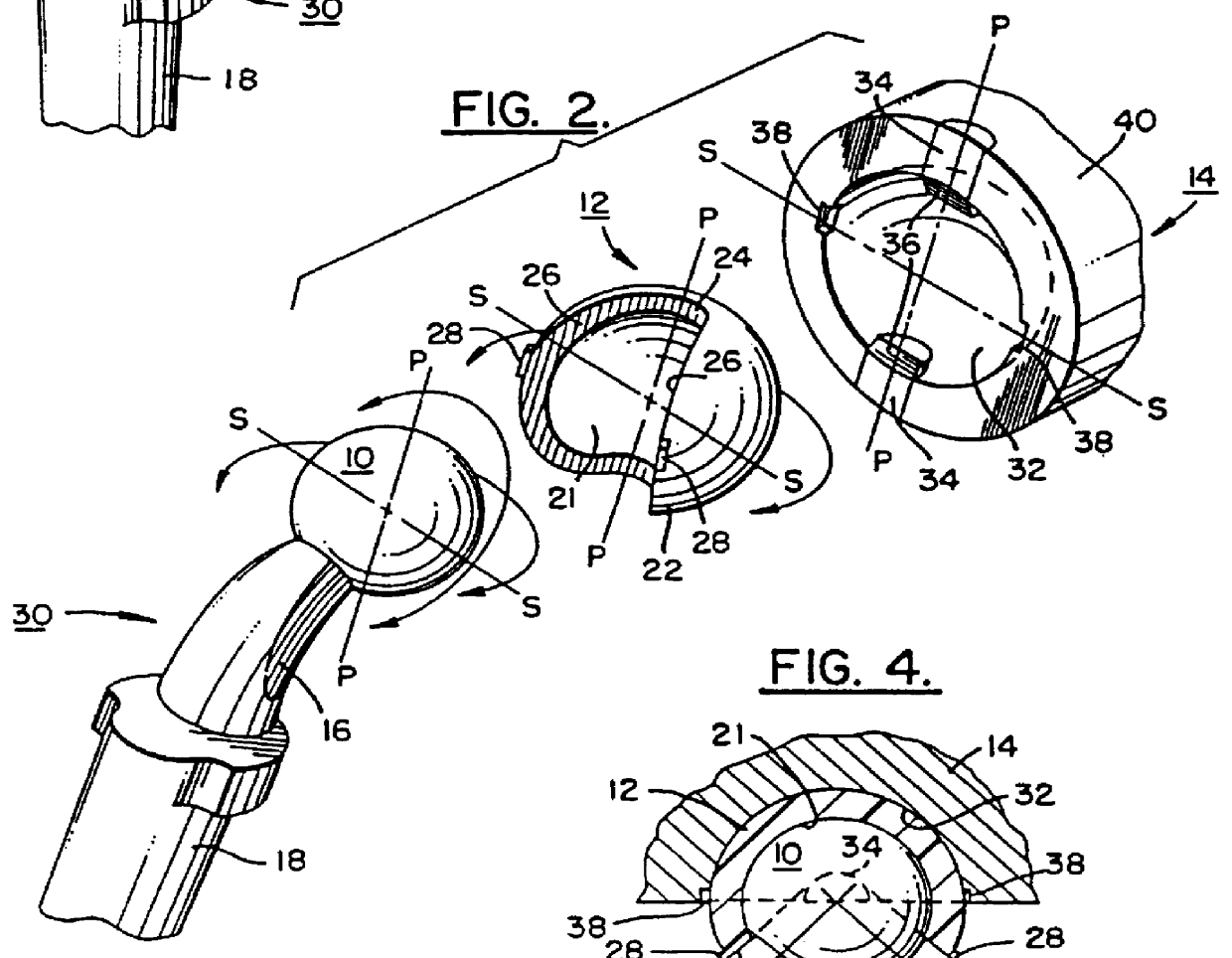
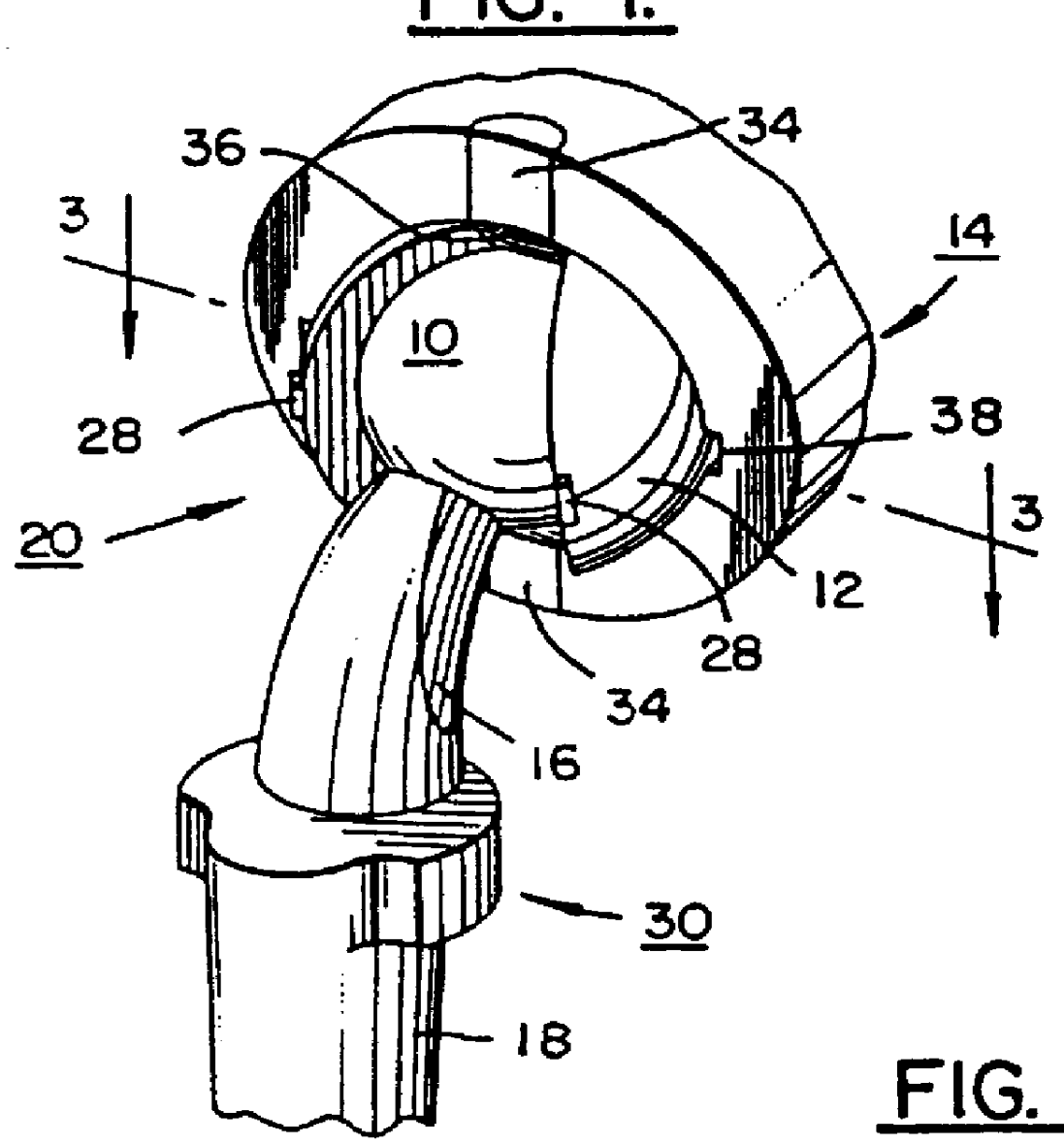
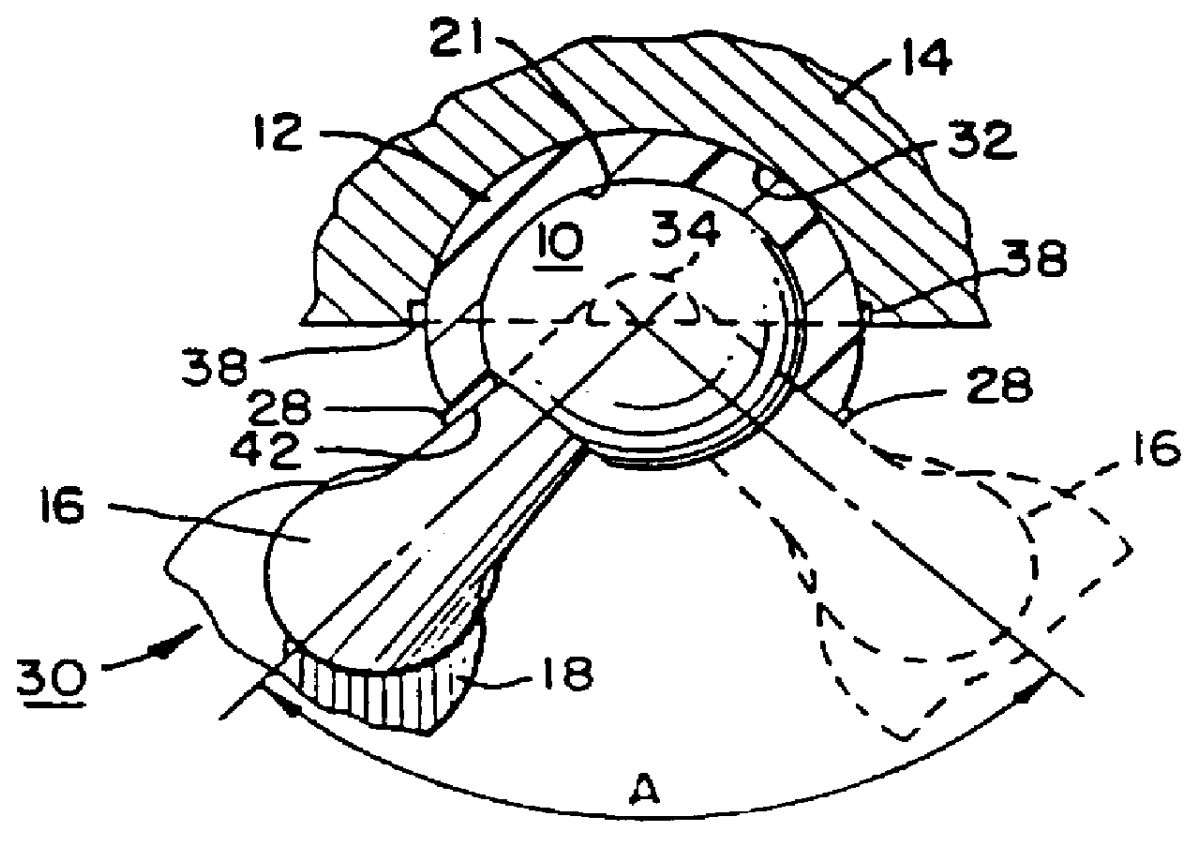
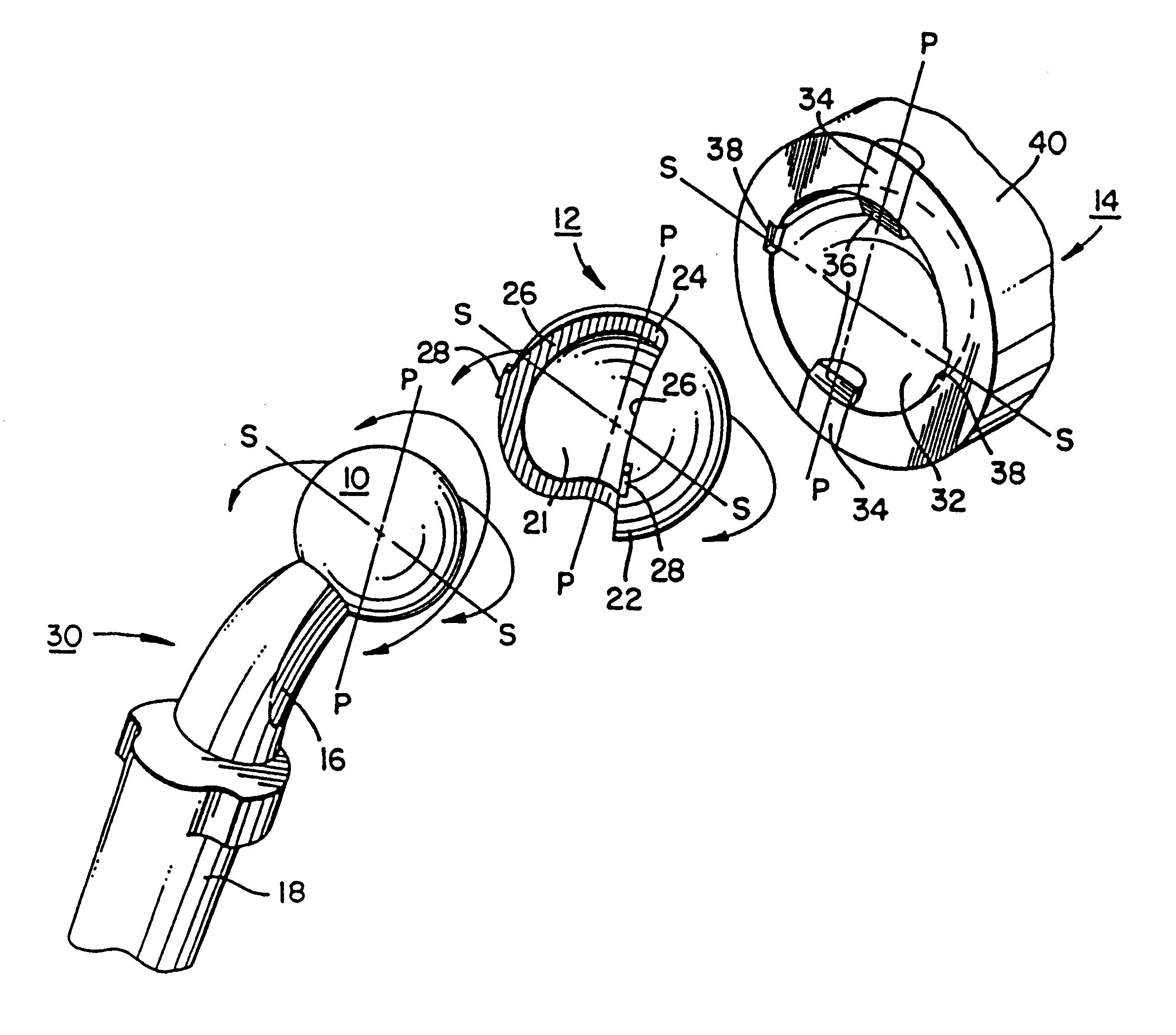
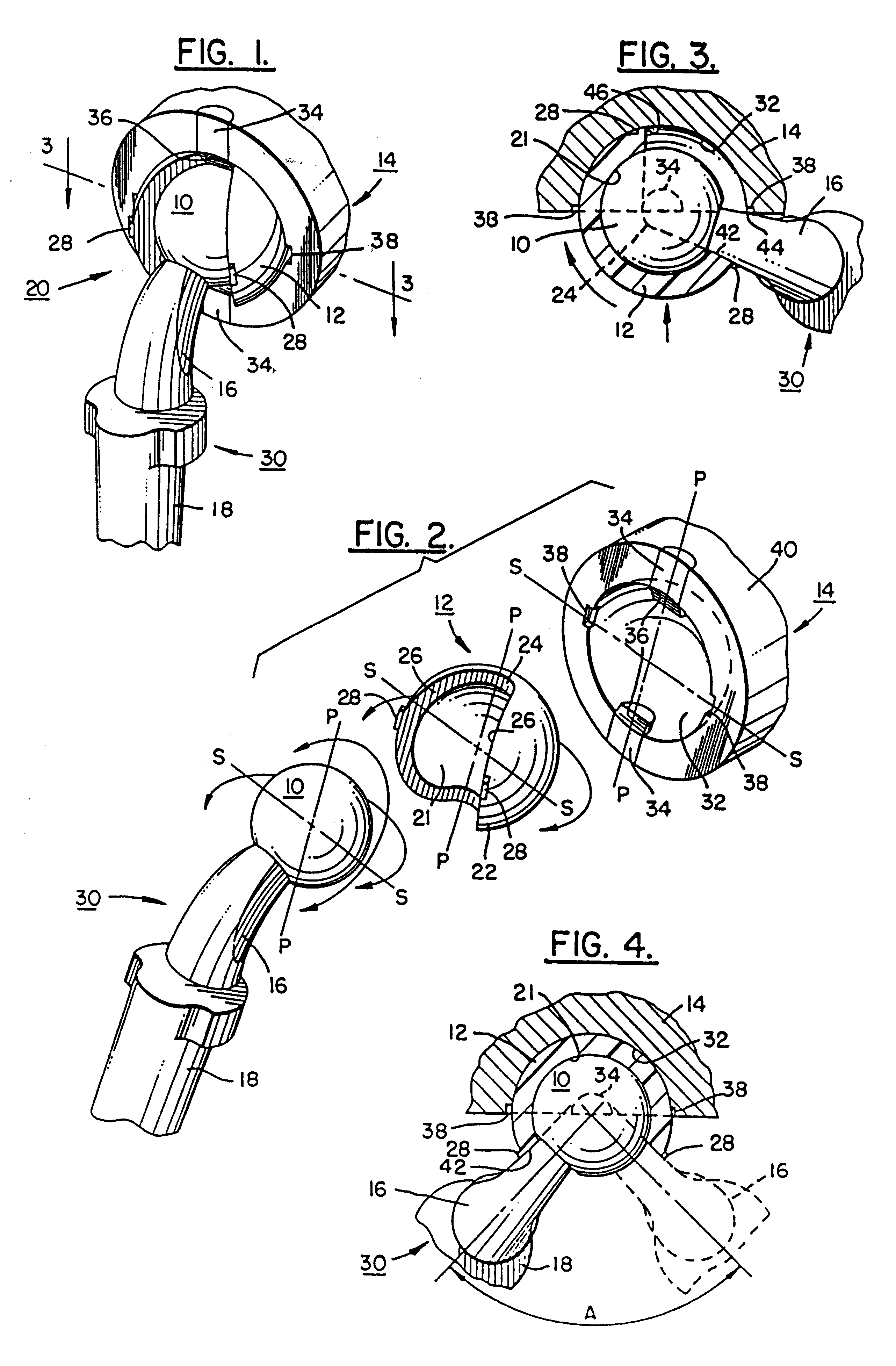
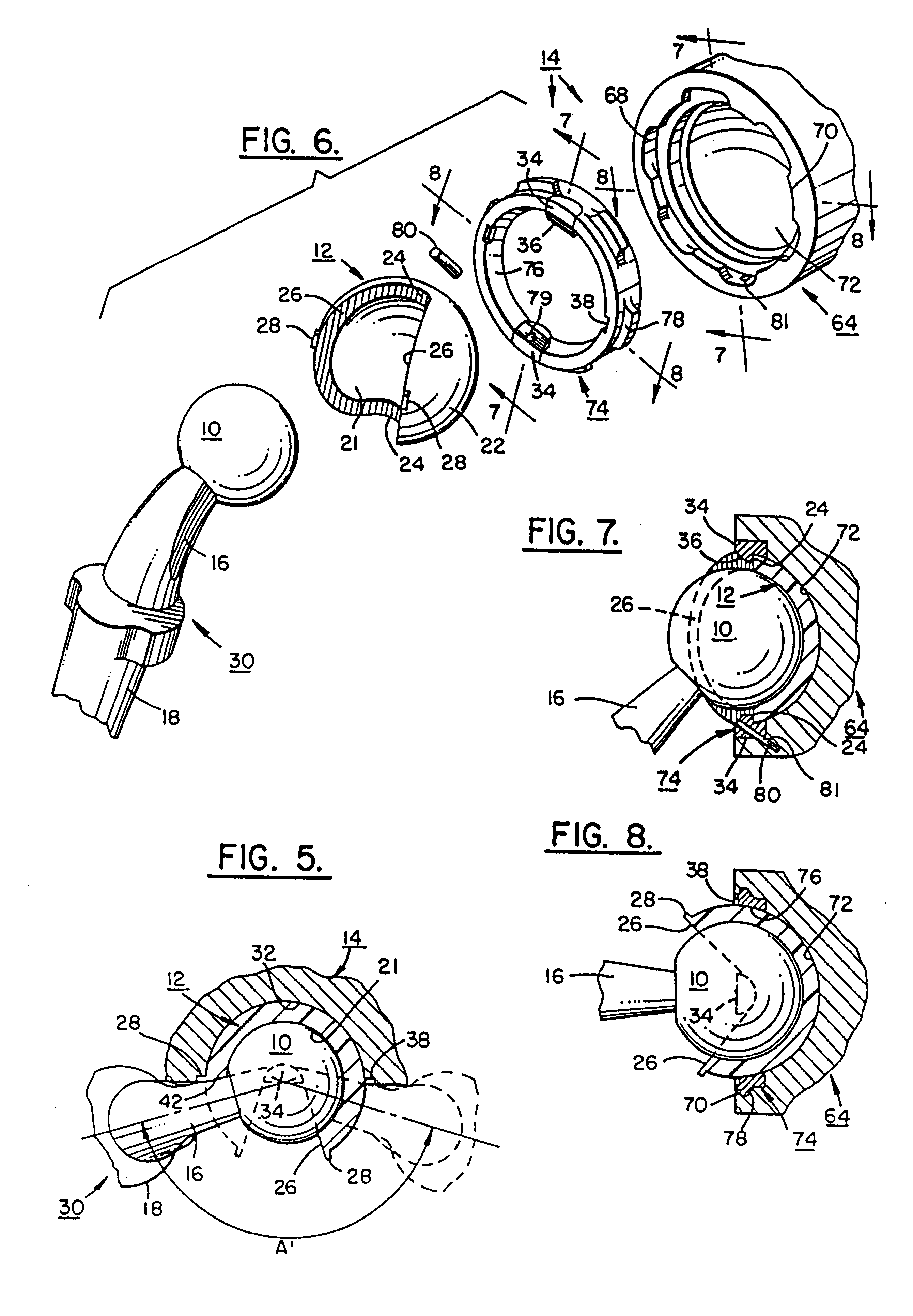
Ball and socket bearing for artificial joint
InactiveUS6042611ALarge range of motionRestrains the ball within the socketJoint implantsFemoral headsArtificial jointsSacroiliac joint
A ball and socket joint for implanting in the body is provided wherein the sooket portion of the joint can have various orientations with respect to the patient's anatomy, and the orientation used for a particular patient can be selected and / or changed in situ, that is, during or after implantation of the joint. In addition, the configuration of the joint, e.g., constrained versus semi-constrained, as well as the materials making up the socket portion of the joint, e.g., plastic versus metal, can be selected and / or changed in situ.
Owner:JOINT MEDICAL PROD
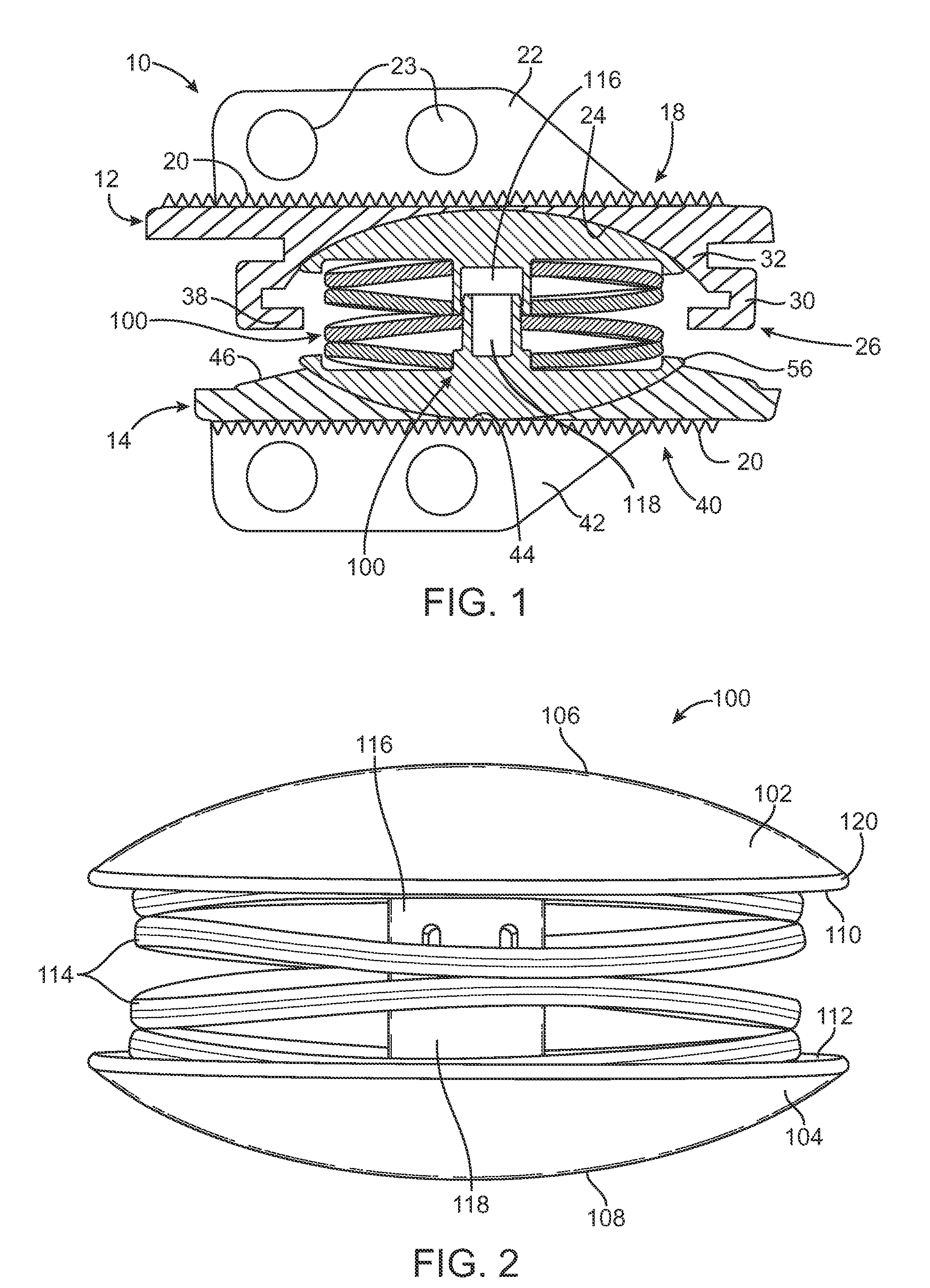
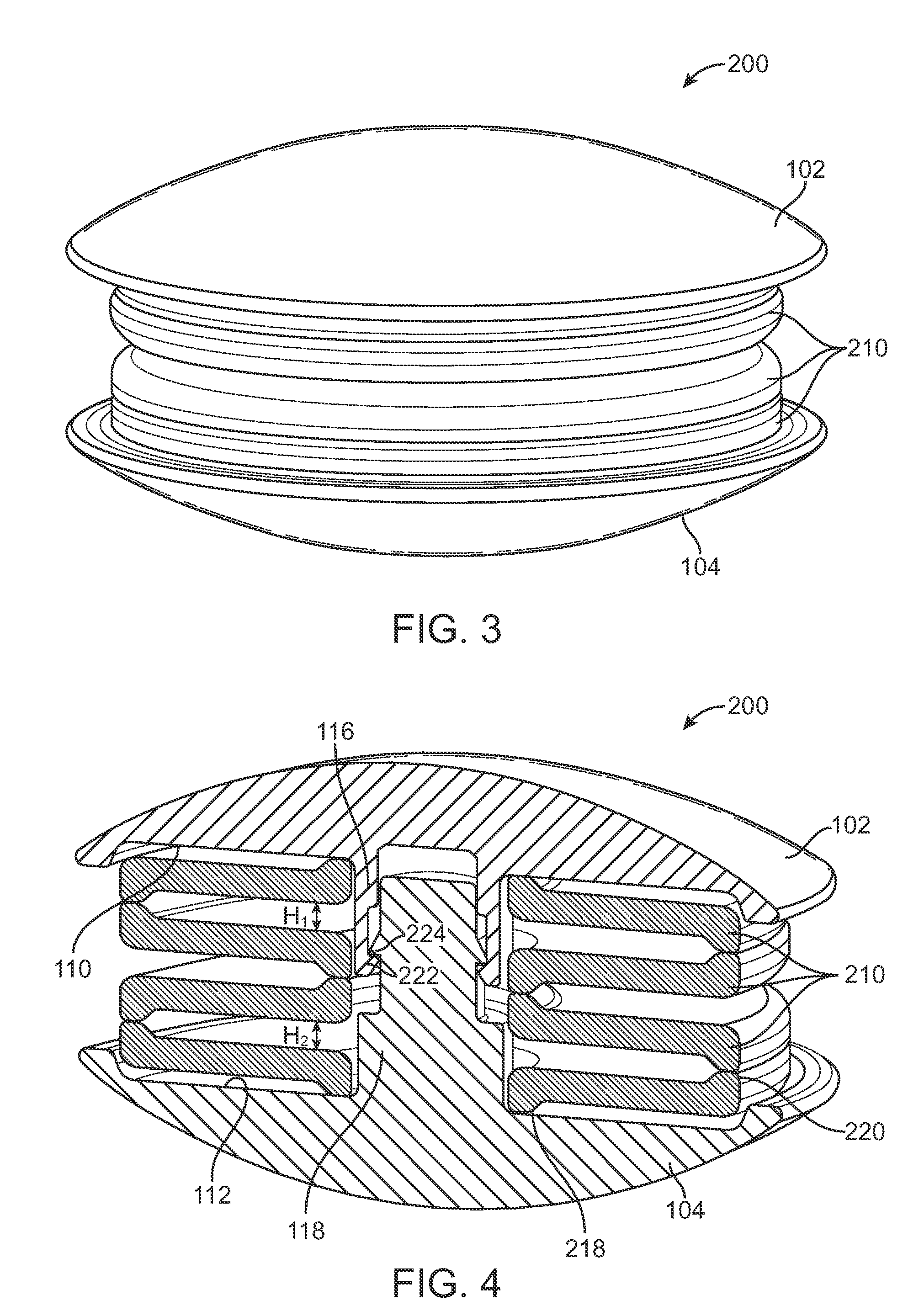
Compliant Implantable Prosthetic Joint With Preloaded Spring
An implantable prosthetic joint has a first component for attaching to a first bone and a second component for attaching to a second bone wherein the first and second components are connected in an articulating manner to provide the motion of a prosthetic joint. The joint includes at least one spring to provide compliance to the prosthetic joint. The at least one spring is preloaded in the artificial joint such that the spring is not allowed to move to a completely relaxed position. This preloading of the spring allows the maximum deflection of the spring to be used for shock absorption because the spring does not deform substantially when the implanted prosthetic joint is moved from an at rest position to a loaded or standing position. The prosthetic joints according to the present invention can include artificial hips, knees, shoulders, ankles, and intervertebral discs.
Owner:SIMPLIFY MEDICAL PTY LTD
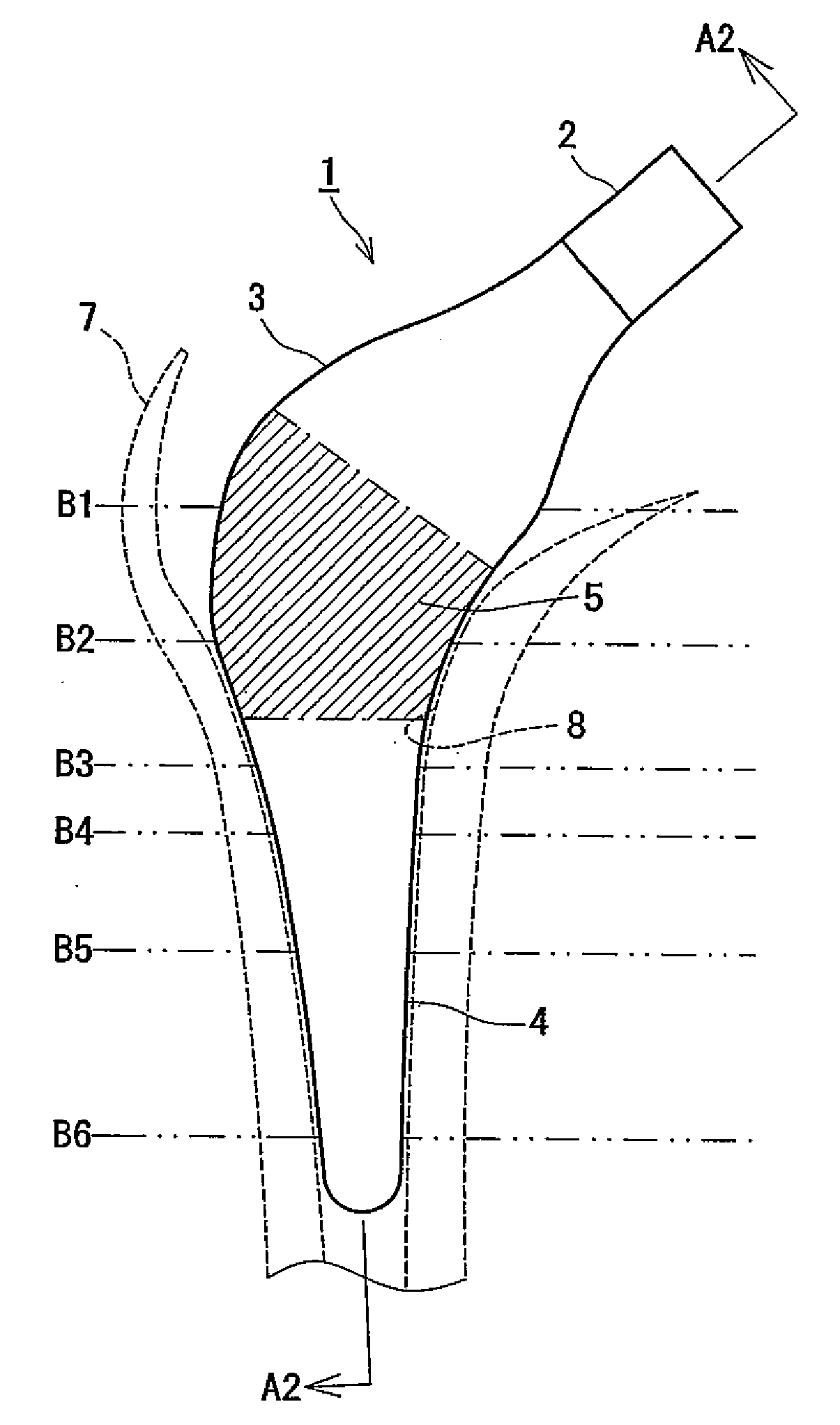
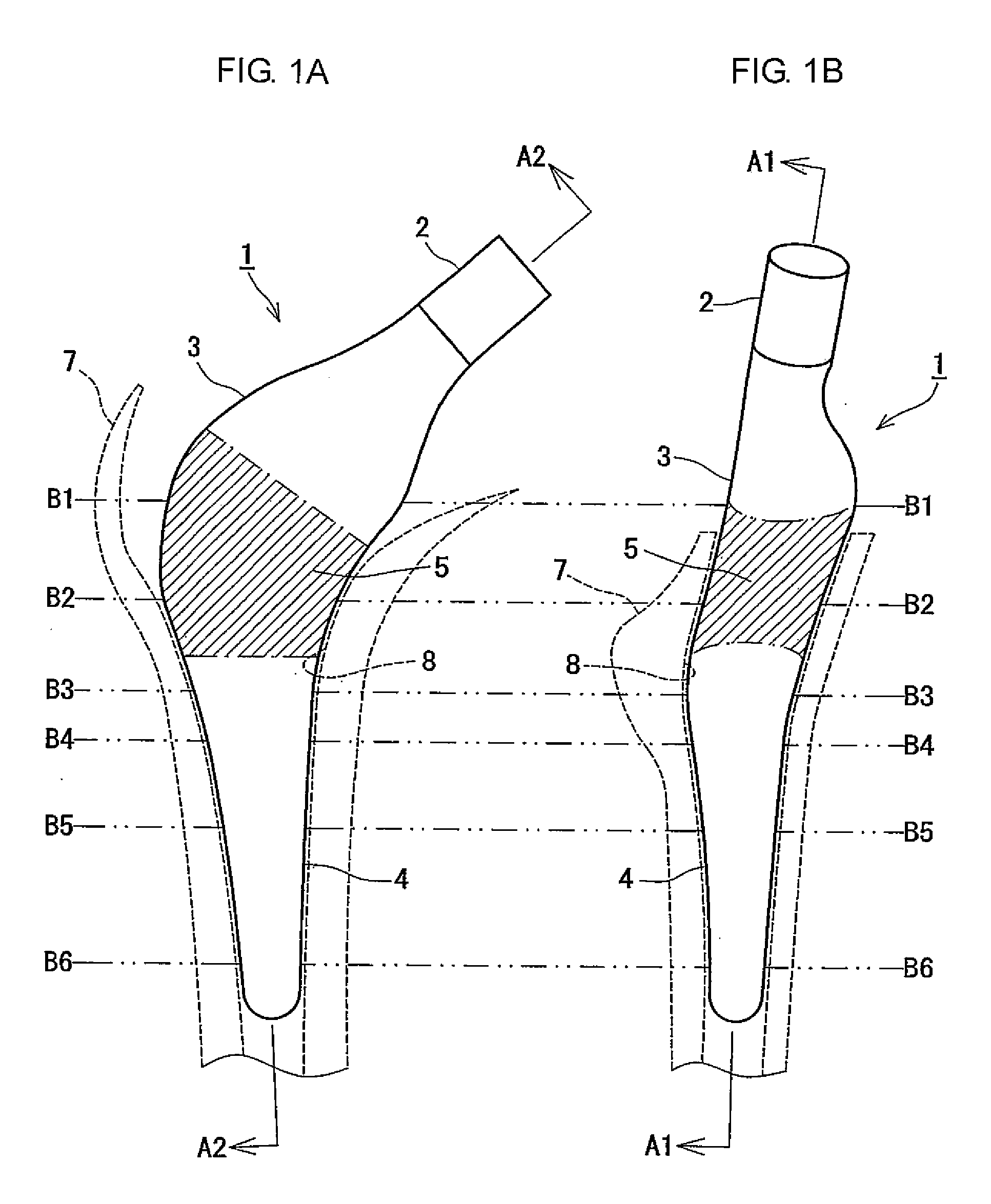
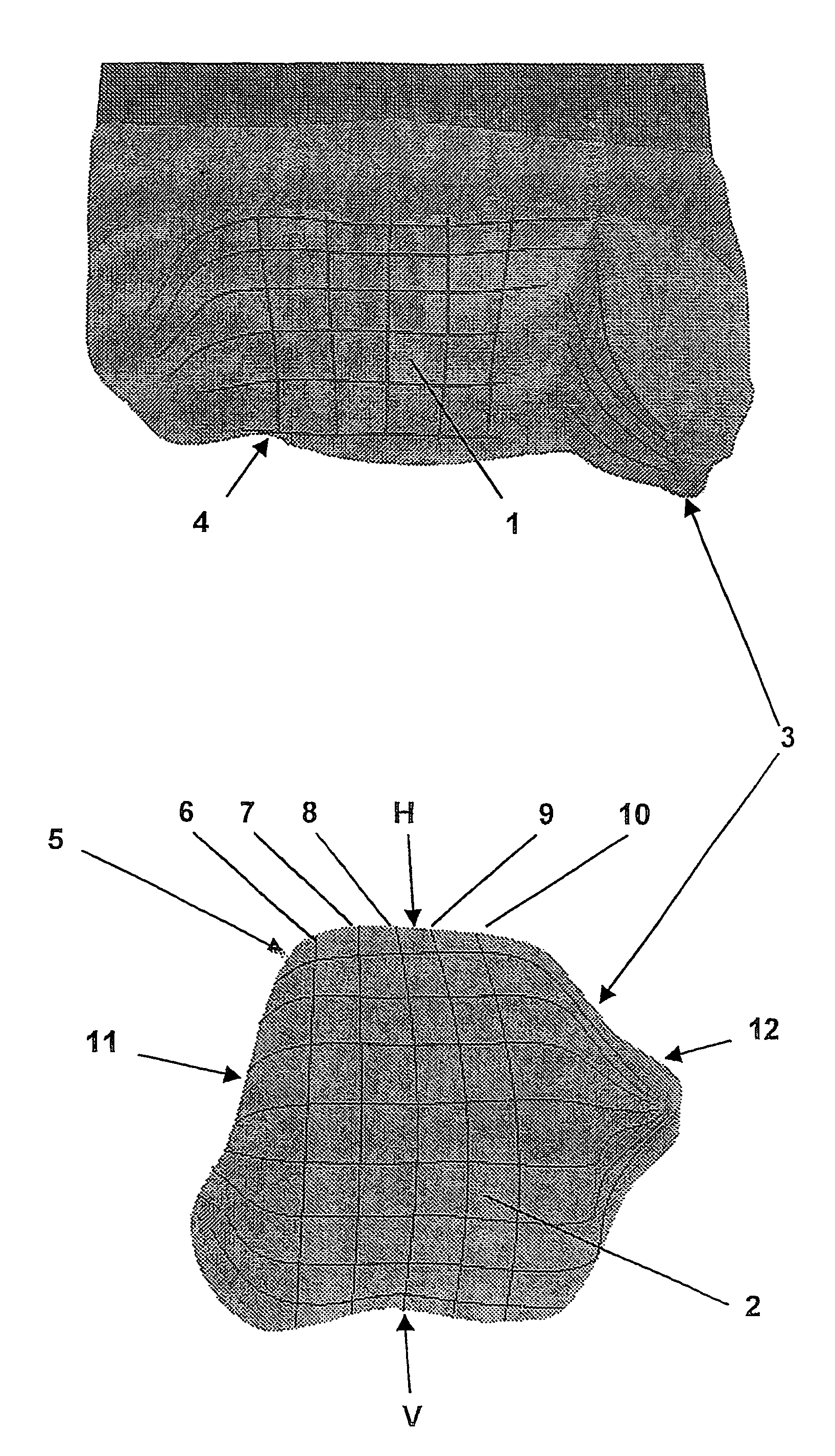
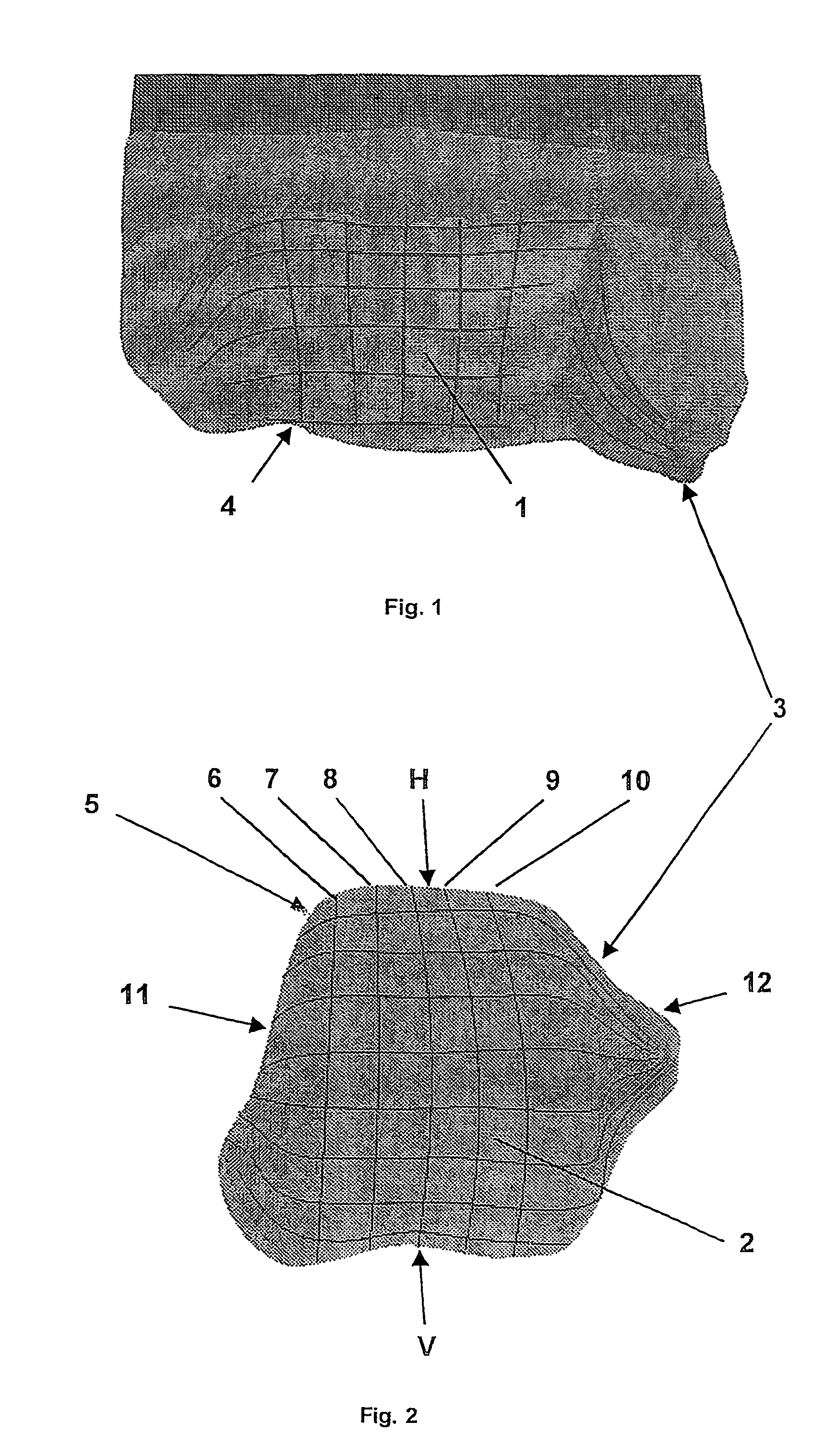
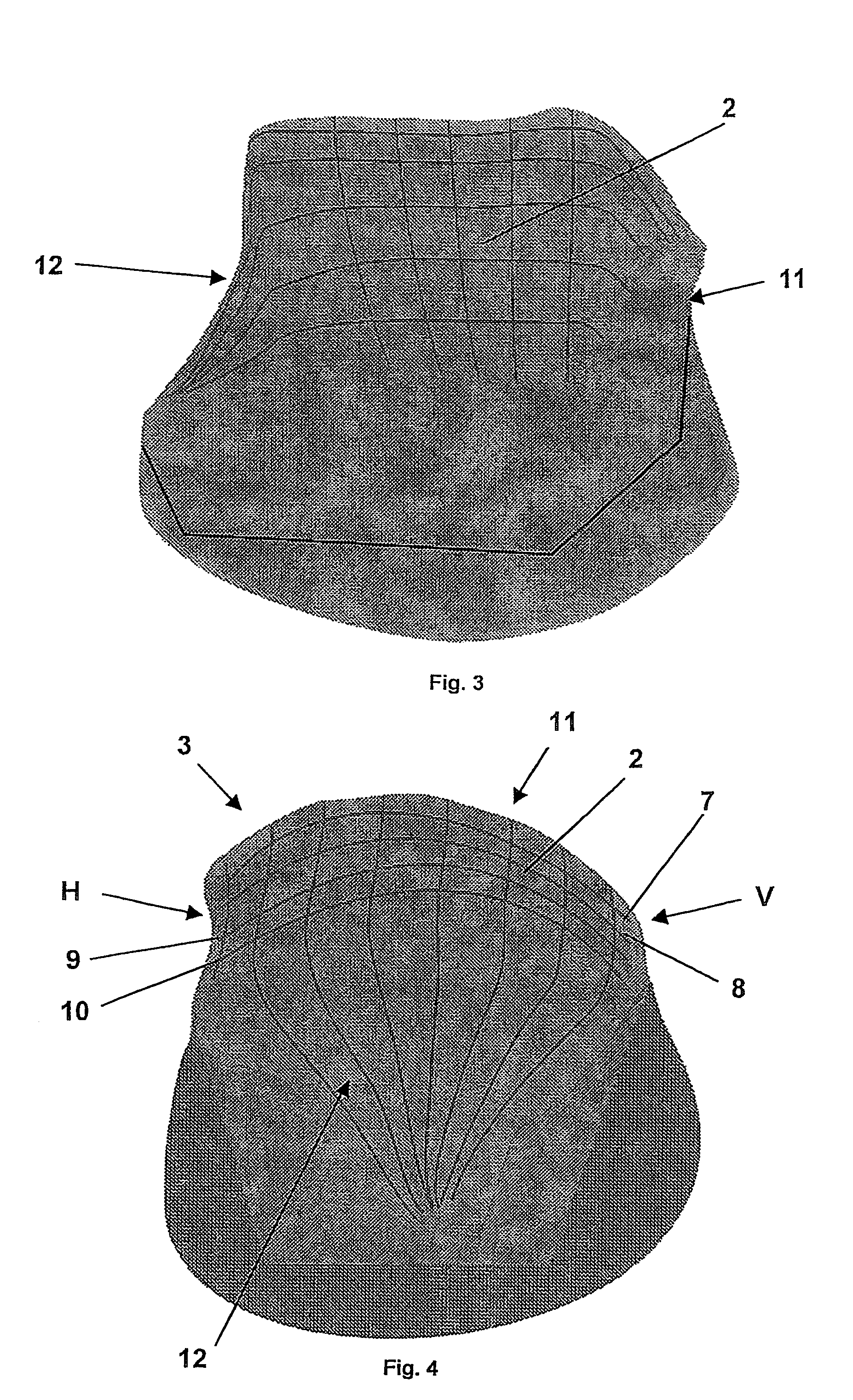
Artificial joint
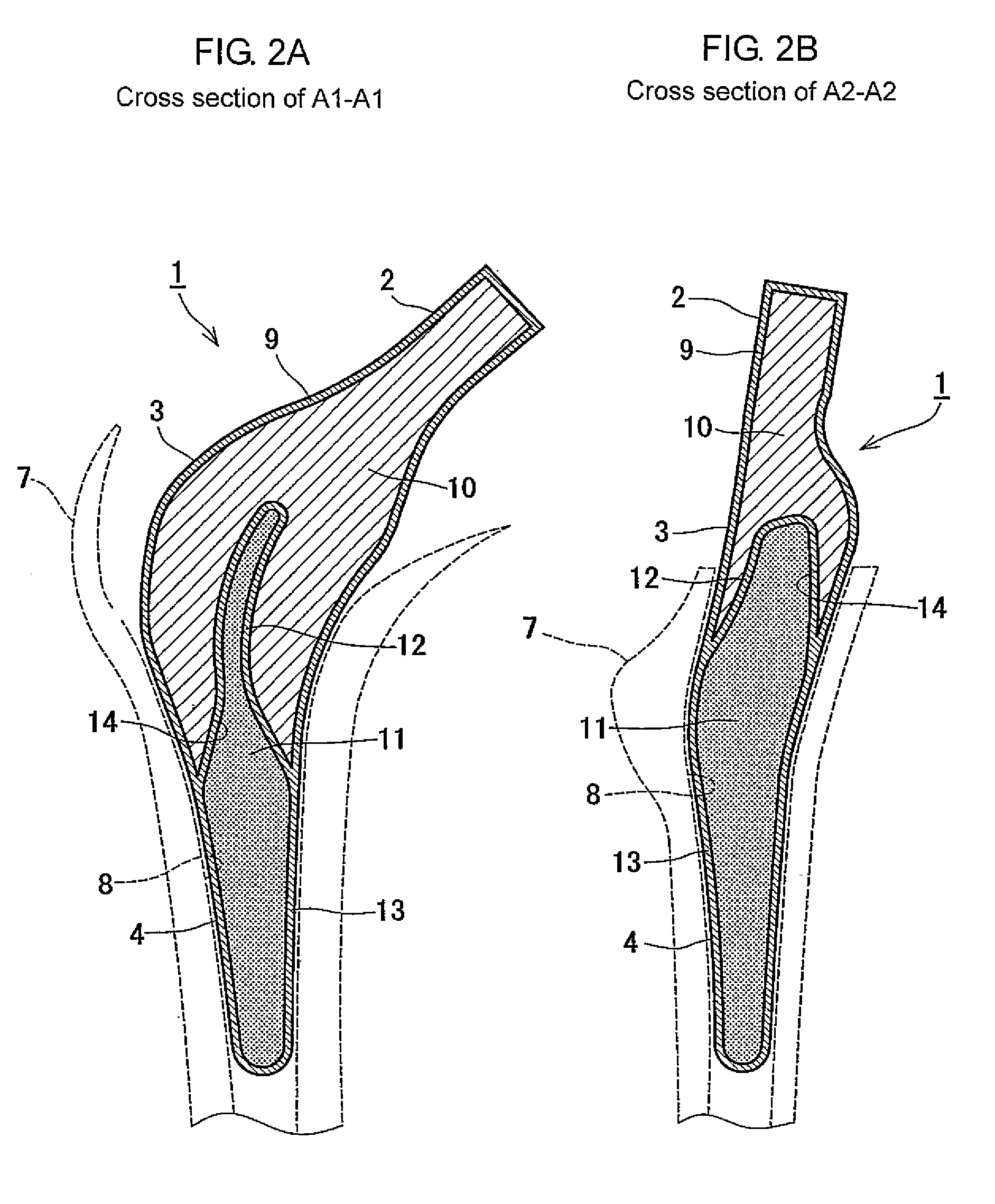
InactiveUS7615082B2Improve mobilityIncreased durabilityAnkle jointsJoint implantsTibiaArticular surfaces
An artificial joint (3), particularly for replacing a talocrural joint, including a first primary joint surface (1) that forms an articular fossa (4) particularly for replacing the tibia composed of concave curvatures extending parallel to a primary function plane of the joint (3), which corresponds to the sagittal plane, and a second primary joint surface (2) which cooperates with the first primary joint surface (1) as a component of a condoyle (5) that replaces the talus and has convex curvatures (7, 8, 9, 10) on the primary function plane that are adapted to the first primary joint surface (1). To achieve high stress resistance and optimal joint mobility, depending on the position of the joint, the radii of the curvatures (7, 8, 9, 10) are calculated such that the differential amounts arising between the corresponding radii of the first and second primary joint surfaces (1, 2) in an ascending angular position (V) relative to a descending angular position and also simultaneously between a medial face (11) and a lateral face (12) of the joint (3) deviate from one another.
Owner:HJS GELENK SYST
Ball and socket bearing for artificial joint
InactiveUSRE38409E1Wide rangeIncrease choiceJoint implantsFemoral headsArtificial jointsSacroiliac joint
A ball and socket joint for implanting in the body is provided wherein the socket portion of the joint can have various orientations with respect to the patient's anatomy, and the orientation used for a particular patient can be selected and / or changed in situ, that is, during or after implantation of the joint. In addition, the configuration of the joint, e.g., constrained versus semi-constrained, as well as the materials making up the socket portion of the joint, e.g., plastic versus metal, can be selected and / or changed in situ. The questions raised in reexamination request Nos. 90 / 004,732, filed Aug. 26, 1997 and 90 / 005,596, filed Jun. 22, 1999, have been considered and the results are reflected in this reissue.
Owner:JOINT MEDICAL PROD
Laser based metal deposition (LBMD) of implant structures
InactiveUS7666522B2Minimize adverse effectsFine grain structureFinger jointsDental implantsWear resistantBone ingrowth
Owner:IMDS CORPORATION
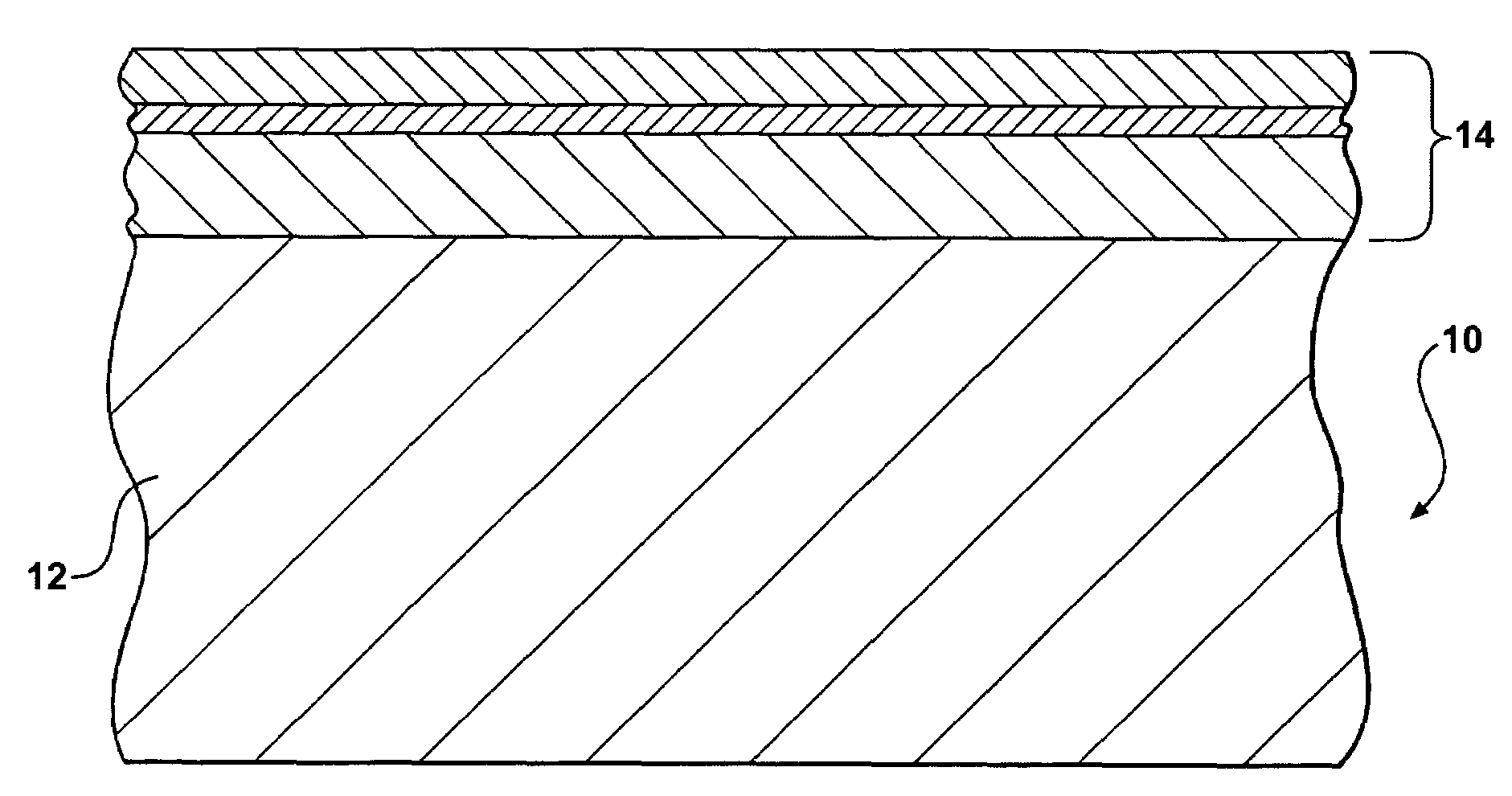
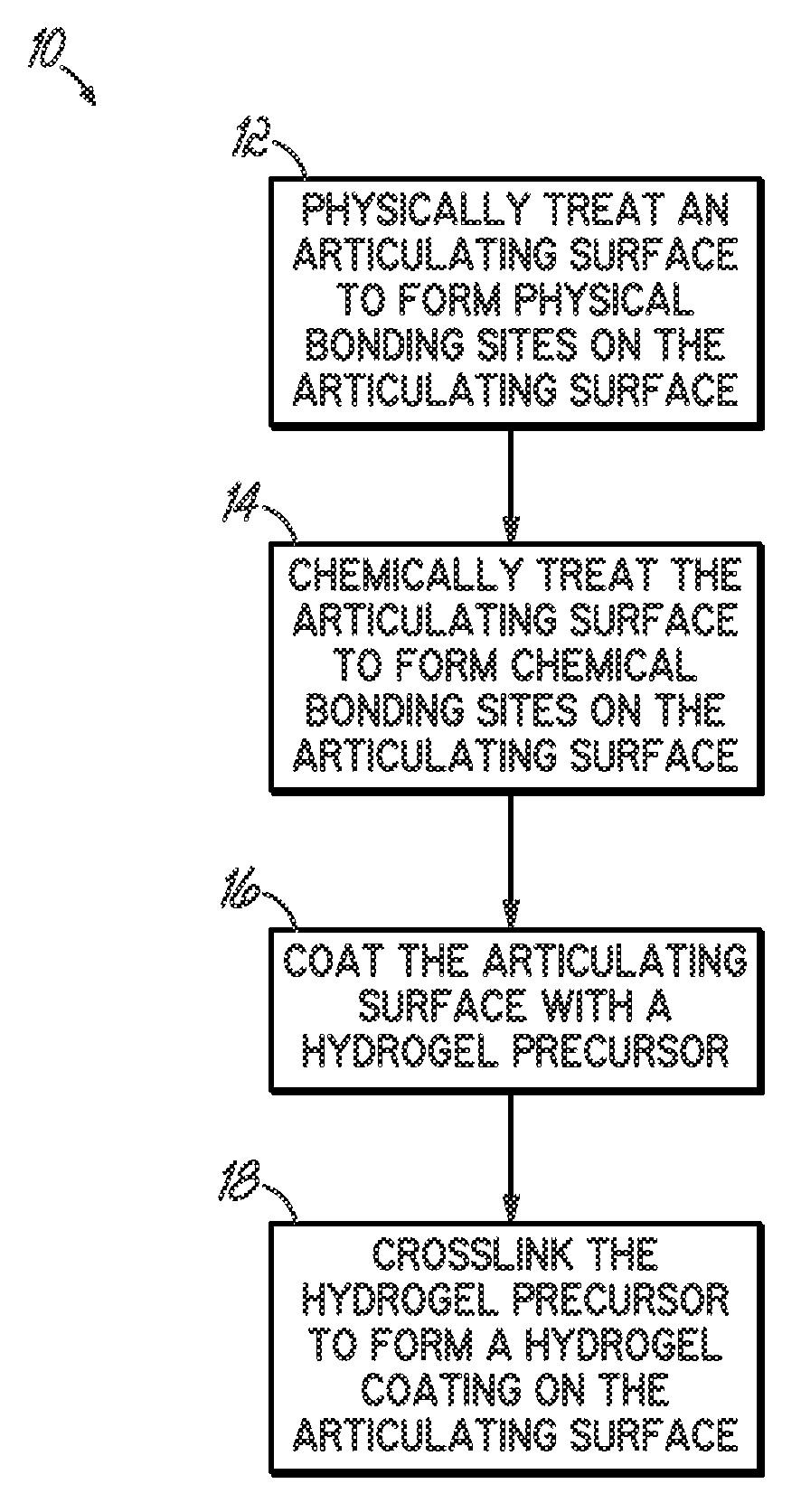
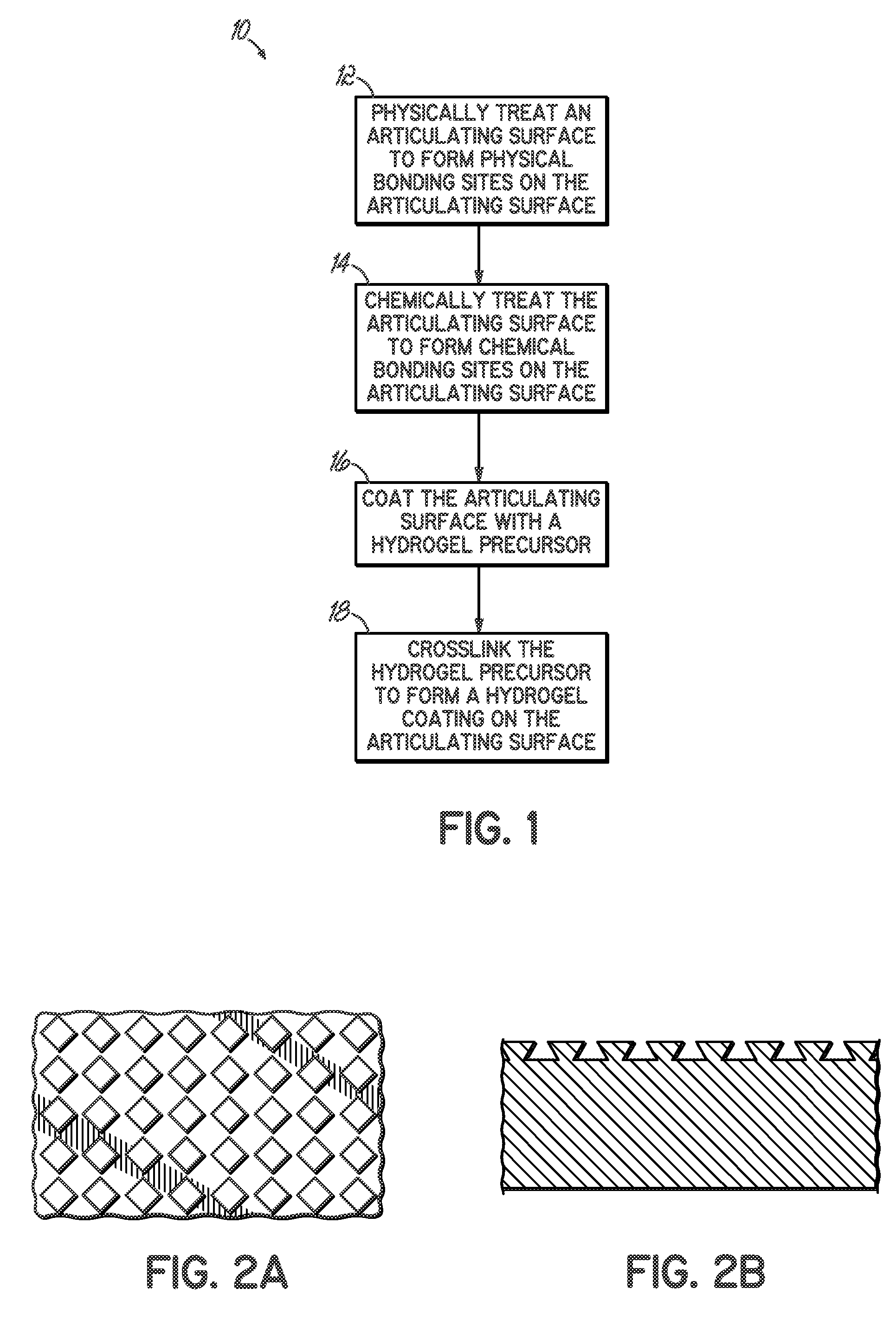
Methods of preparing hydrogel coatings
The present invention provides hydrogel coated, implantable medical devices and methods of coating hydrogels onto implantable medical devices. In one embodiment, a hydrogel coated medical device is formed by physically treating a surface of the medical device, chemically treating the surface, applying a hydrogel precursor and then crosslinking the hydrogel precursor to form a hydrogel coating on the surface of the medical device. The present invention may be particularly applicable for coating articulating surfaces on implantable medical devices such as artificial joints.
Owner:ZIMMER INC
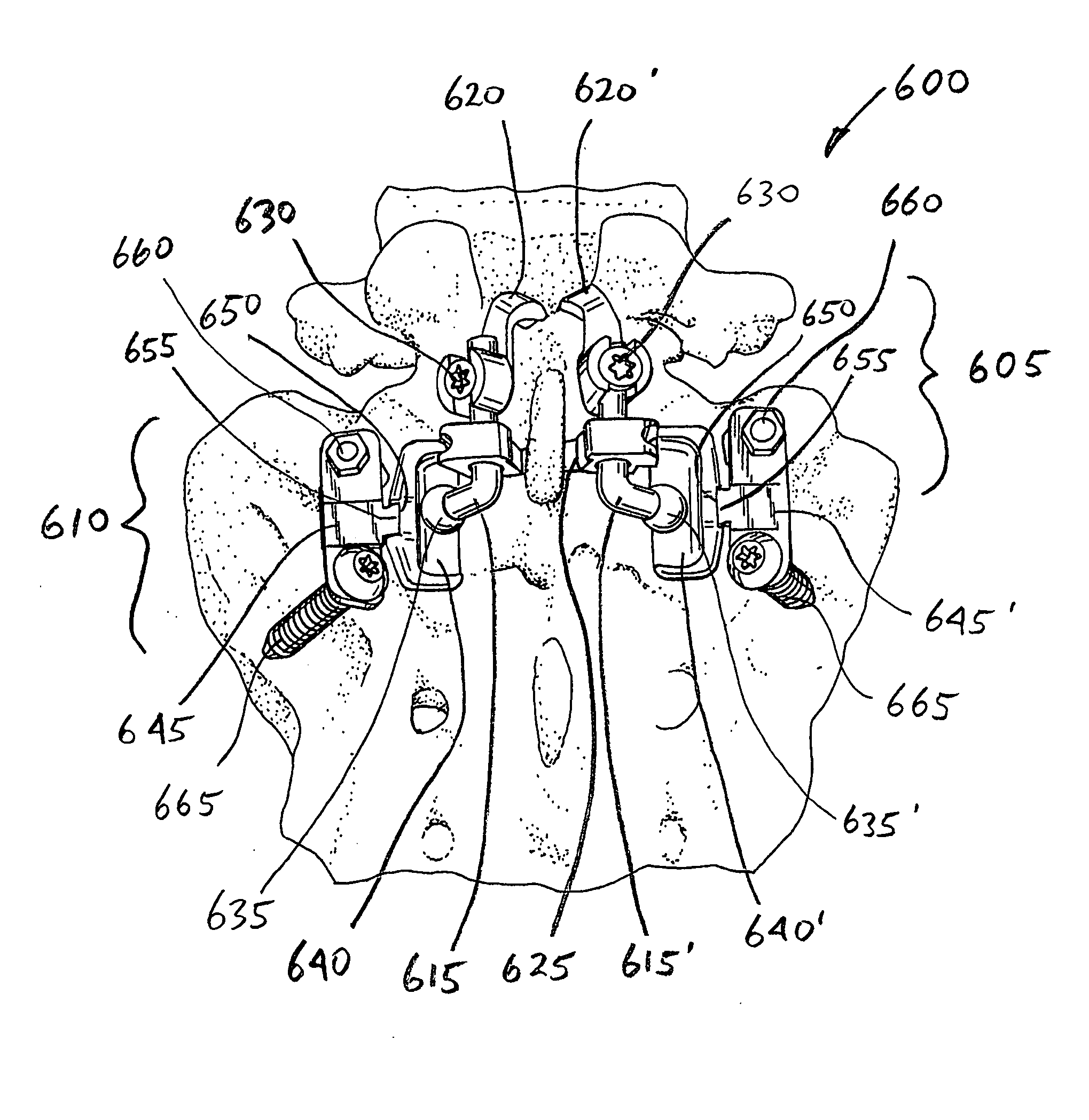
Facet and disc arthroplasty system and method
InactiveUS20070233256A1Easy to useInternal osteosythesisJoint implantsHybrid systemTranspedicular fixation
The invention discloses devices, methods and systems for implanting articulating devices on the human spine. In some embodiments, three or more vertebrae are movable interconnected with artificial joints. Some embodiments are particularly well suited for implanting in the lumbosacral area of the spine. Some embodiments employ hybrid systems combining translaminar fixation with pedicular fixation of the device components. Some embodiments combine facet joint replacement with disc replacement.
Owner:GLOBUS MEDICAL INC
Contact sensors and methods for making same
The present invention is directed to novel contact sensors. The contact sensors of the invention include a conductive composite material formed of a polymer and a conductive filler. In one particular embodiment, the composite materials can include less than about 10 wt % conductive filler. Thus, the composite material of the contact sensors can have physical characteristics essentially identical to the polymer, while being electrically conductive with the electrical resistance proportional to the load on the sensor. If desired, the sensors can be formed of the same polymeric material as the bearing that is being examined. The sensors can provide real time dynamic contact information for joint members under conditions expected during use. In one particular embodiment, the sensors can be used to examine dynamic wear characteristics of artificial joint bearings such as artificial knee, hip, or shoulder bearings.
Owner:CLEMSON UNIV RES FOUND
Torque Sensor
ActiveUS20050166685A1Reduce disadvantagesImprove stabilityWork measurementVolume/mass flow by dynamic fluid flow effectArtificial jointsTransducer
A torque sensor for measuring a torque at a predetermined location of a structural element, in particular of a prosthesis, can be arranged outside the measurement location by virtue of the fact that it is constructed as a sensor structure (13, 13′, 23) that forms a virtual pivot axis (16, 16′) outside the sensor. The sensor structure is provided with measurement transducers (29) which detect deformations of the sensor structure (13, 13′, 23) and are used to determine a torque about the virtual pivot axis (16, 16′). A preferred application for the torque sensor is its incorporation in a prosthesis for the purpose of controlling an artificial joint.
Owner:OTTOBOCK SE & CO KGAA
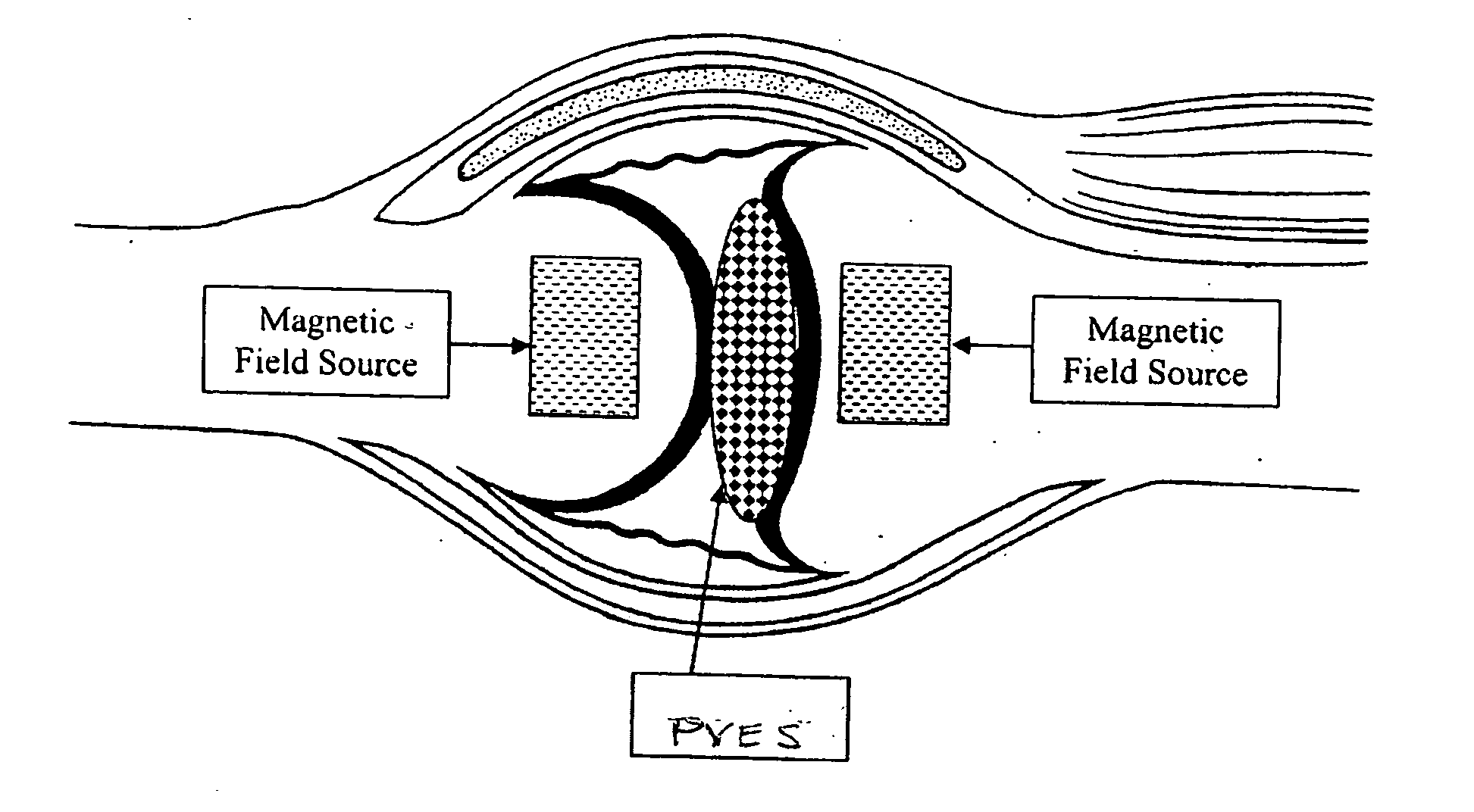
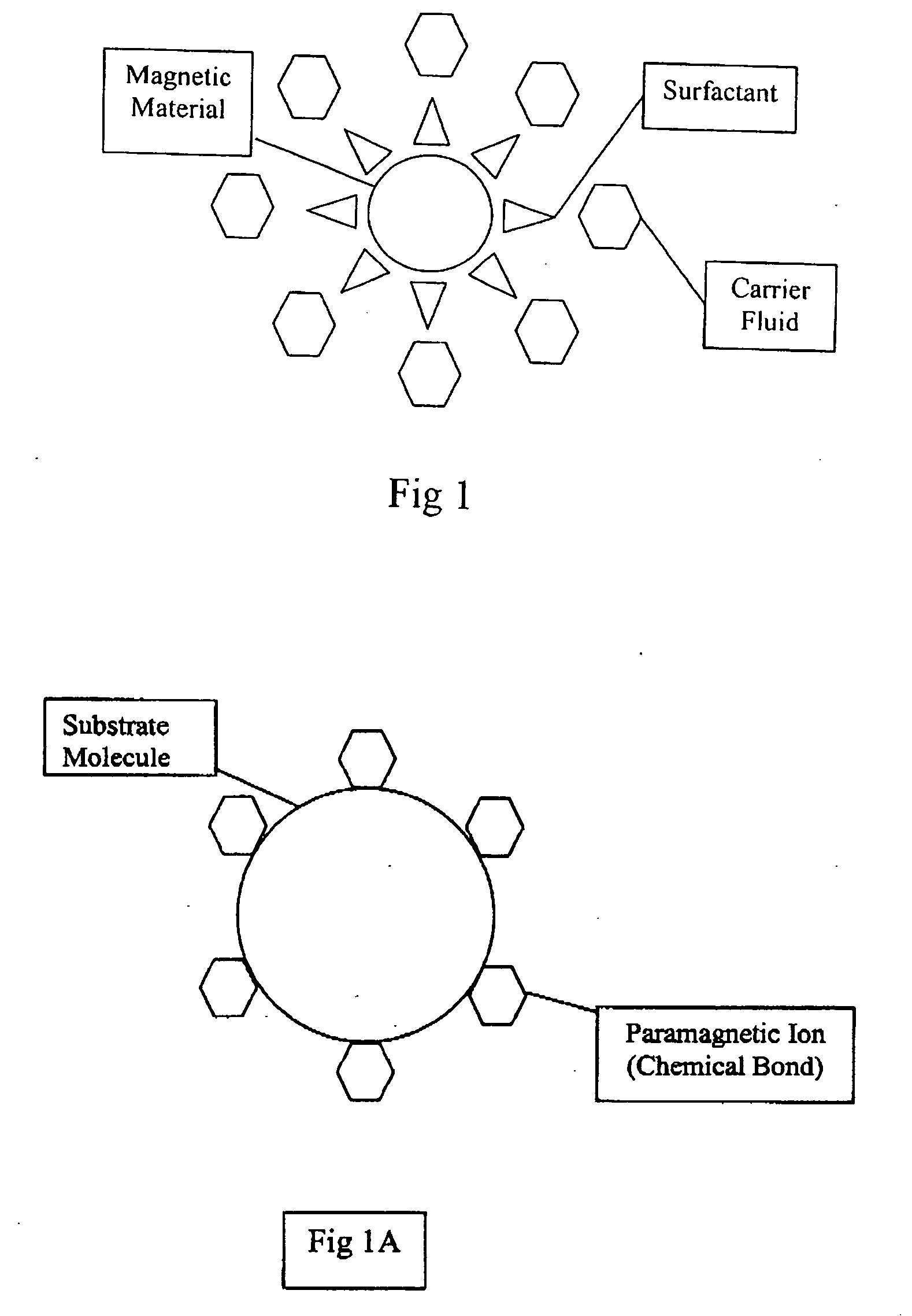
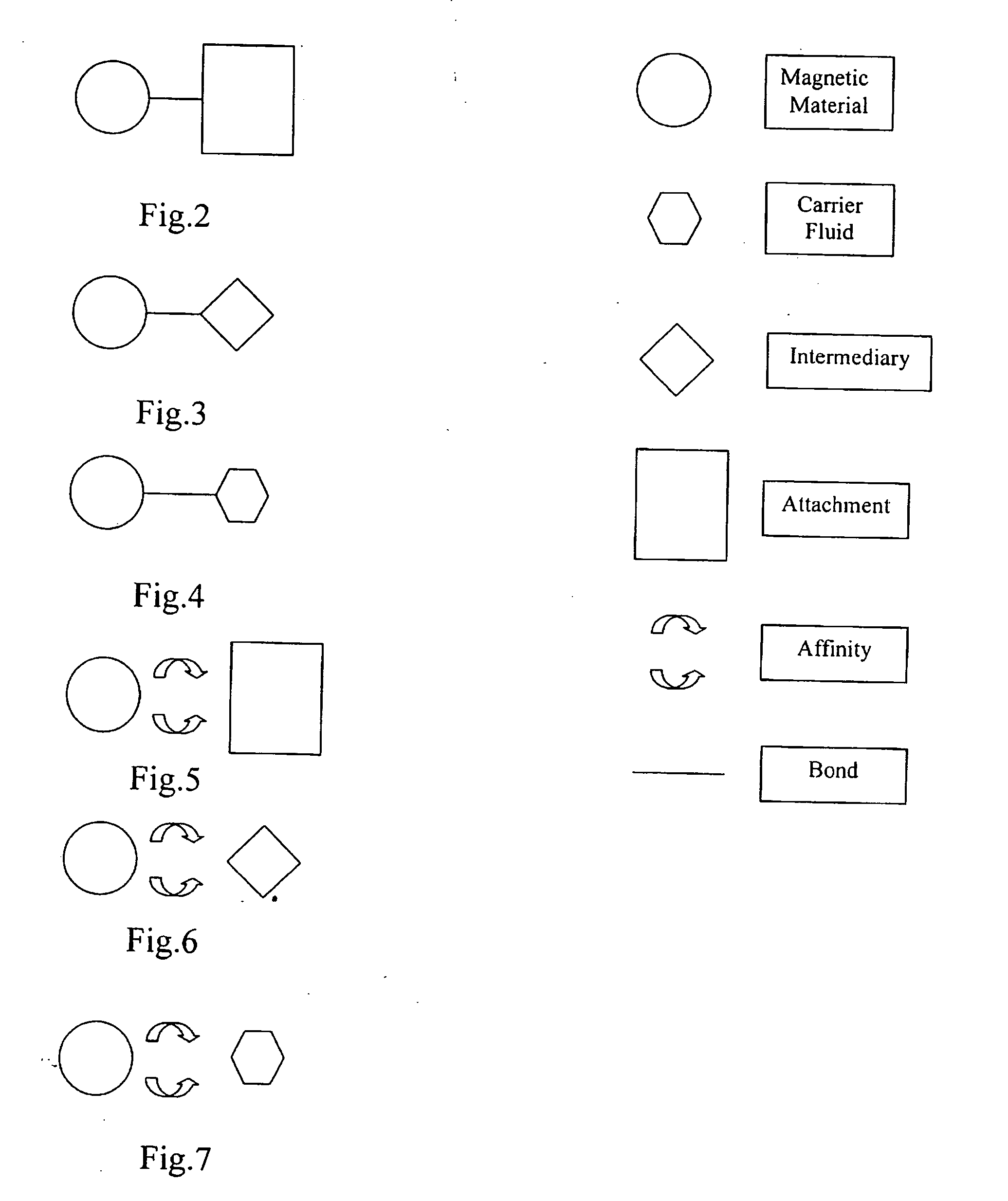
Paramagnetic liquid interface
InactiveUS20070100457A1Improve rheologyExtended durationFinger jointsWrist jointsArticular surfacesEngineering
Natural joint interfaces wear out and / or are damaged causing pain and disability. They can be currently replaced by artificial surfaces made of materials or in the near future by magnetic fields. They would benefit from a PVES (paramagnetic visco-viscoelastic supplement) that can replace or augment natural joint interfaces or augment total joint replacements. Joint replacement components can be modular and would benefit from a PVES to decrease wear and damp impact between modular parts of a single component. The PVES is a dynamic interface allowing components to be less rigid. Energy transmission is reduced. PVES can act as an interface between natural damaged joint surfaces obviating the need for classic total joint replacement or between the surfaces of artificial joint components to improve or supplement their function. These PVES can be controlled by magnetic fields with respect to their location, physical properties, loads, etc. PVES are typically made of paramagnetic ions and a substrate molecule. One such PVES can be made of gadolinium ions and hyaluronic acid to form gadolinium hyaluronate.
Owner:HYDE EDWARD R JR
Laser based metal deposition (LBMD) of implant structures
InactiveUS20070202351A1High porosityMinimize adverse effectsFinger jointsDental implantsArtificial jointsWear resistant
A method is provided for depositing a hard wear resistant surface onto a porous or non-porous base material of a medical implant. The wear resistant surface of the medical implant device may be formed by a Laser Based Metal Deposition (LBMD) method such as Laser Engineered Net Shaping (LENS). The wear resistant surface may include a blend of multiple different biocompatible materials. Further, functionally graded layers of biocompatible materials may be used to form the wear resistant surface. Usage of a porous material for the base may promote bone ingrowth to allow the implant to fuse strongly with the bone of a host patient. The hard wear resistant surface provides device longevity, particularly when applied to bearing surfaces such as artificial joint bearing surfaces or a dental implant bearing surfaces.
Owner:IMDS CORPORATION
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com