Patents
Literature
Hiro is an intelligent assistant for R&D personnel, combined with Patent DNA, to facilitate innovative research.
34 results about "Medicare payment" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
Medical information system for cost-effective management of health care
InactiveUS20100262436A1Rapid collection and analysisAccurately transmitOffice automationMedical imagesBilling systemQuality control
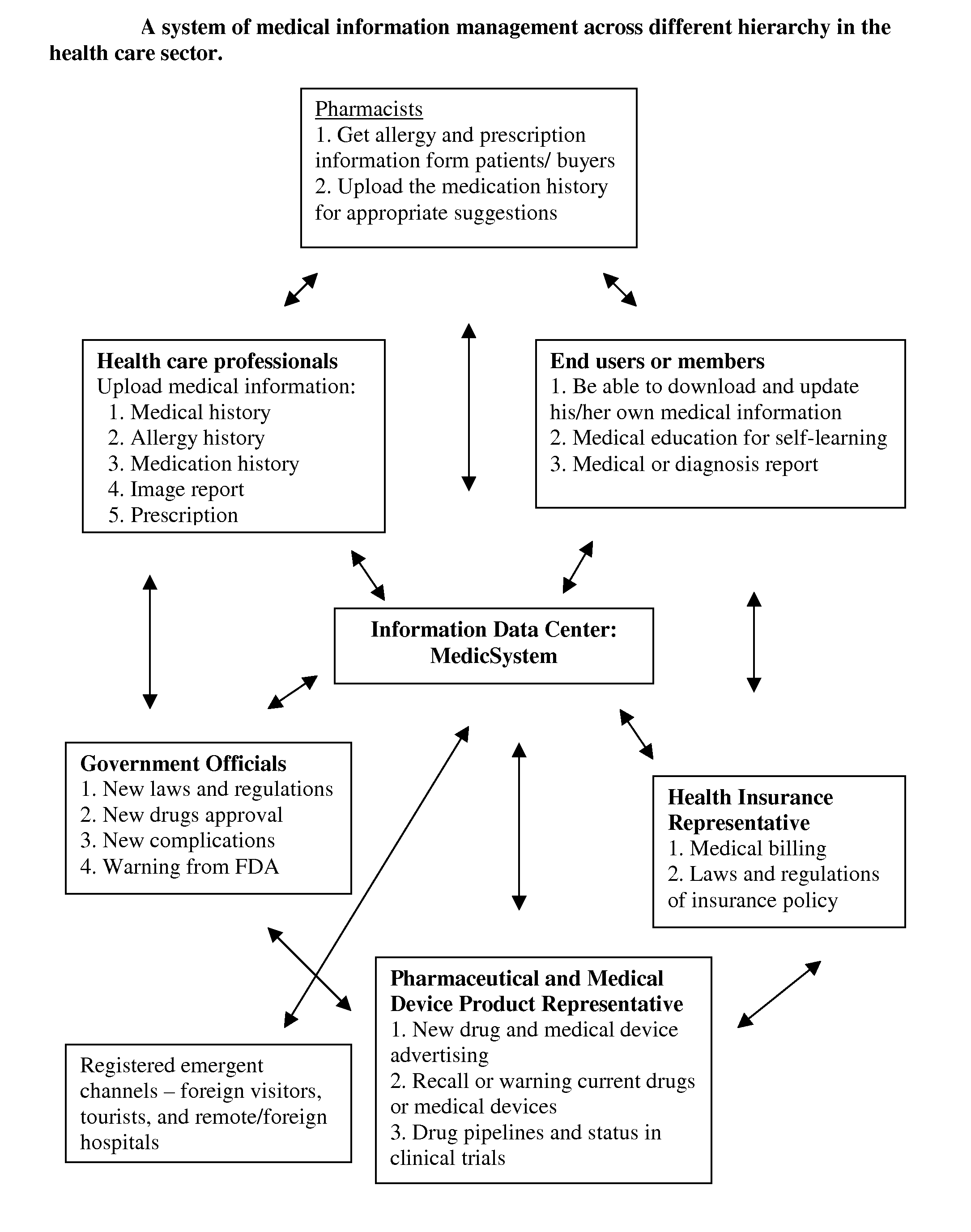
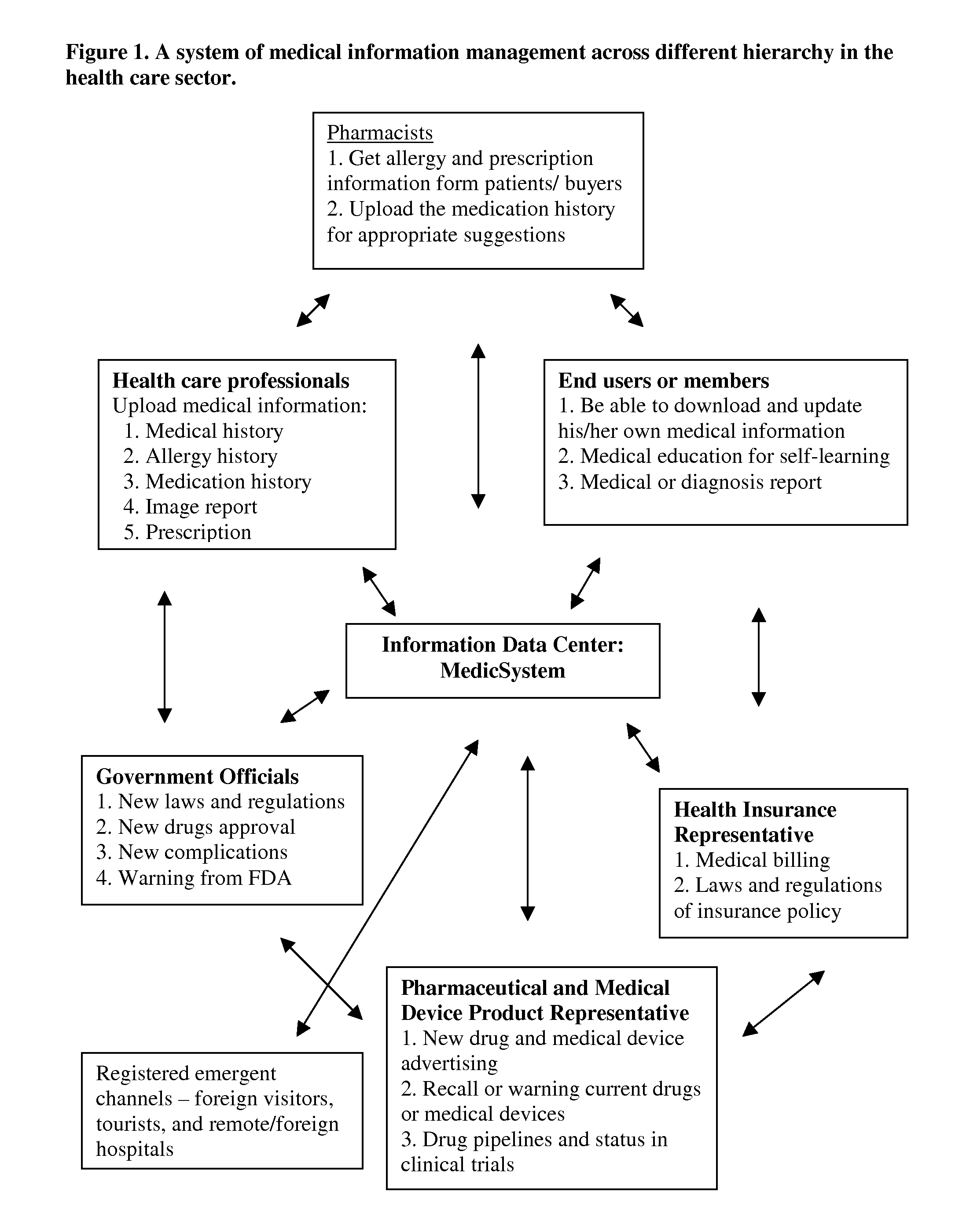
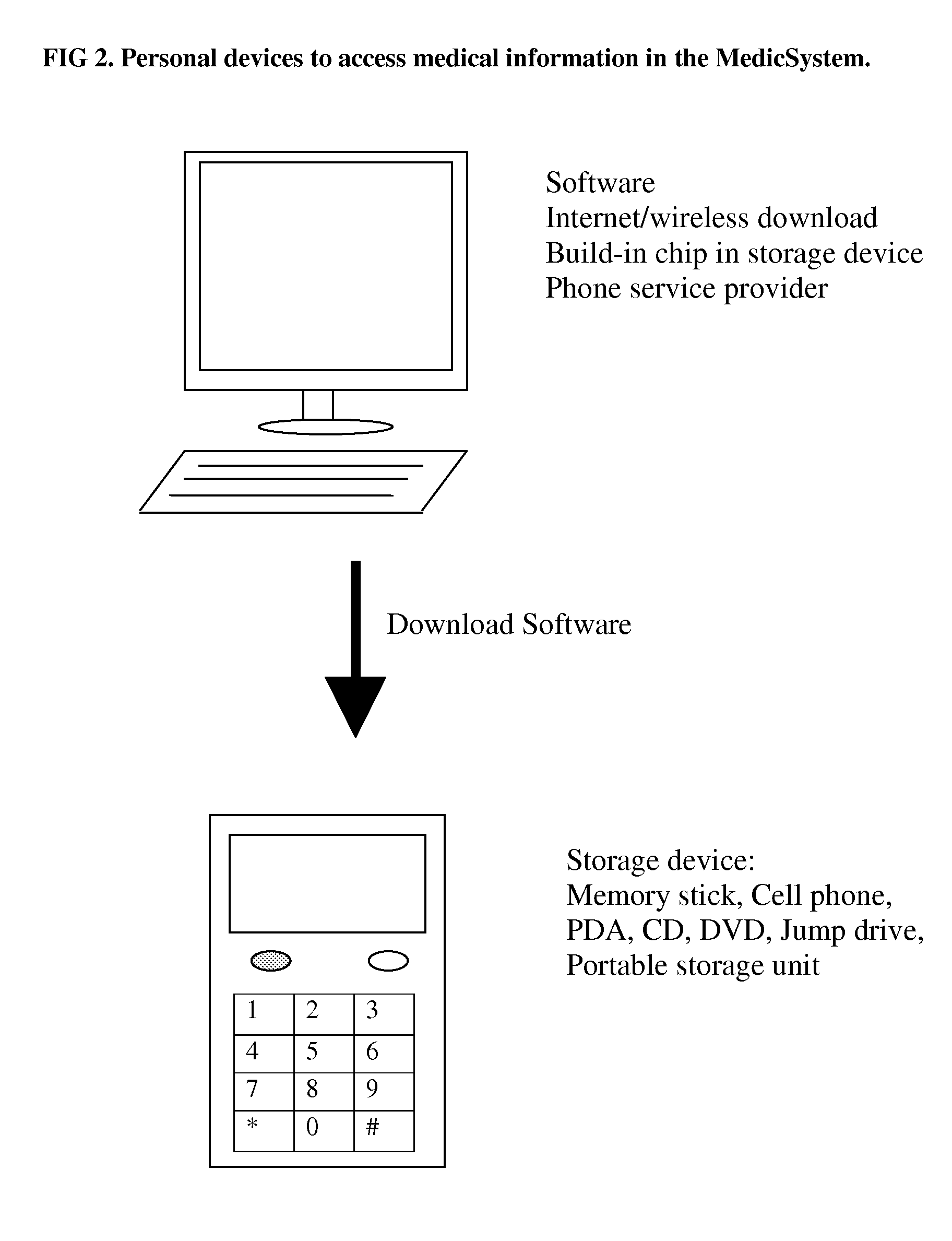
The invention is to solve the high cost problems in the current health care system and to increase efficiency and quality of medical care service by using an integrated medical information management system. The invention allows users or patients to manage their own medical information worldwide in a portable device to enhance medication adherence and self-management of personalized health care. A multi-functional medical information center is developed to manage medical information received from various resources to satisfy stakeholders by improving the efficacy, accuracy, and quality of health care information, but simultaneously operated at a cost-effective manner for stakeholders. In addition, the quality control of medical data management will be guarded by a side-by-side comparison technology to warn inconsistent information in medical billing history to prevent medical insurance fraudulent claims. The invention also makes the medical billing system more transparent and patients can find their desired medical doctors, preferred insurance policy, and price comparison of medical products at ease.
Owner:CHEN YING YU +1
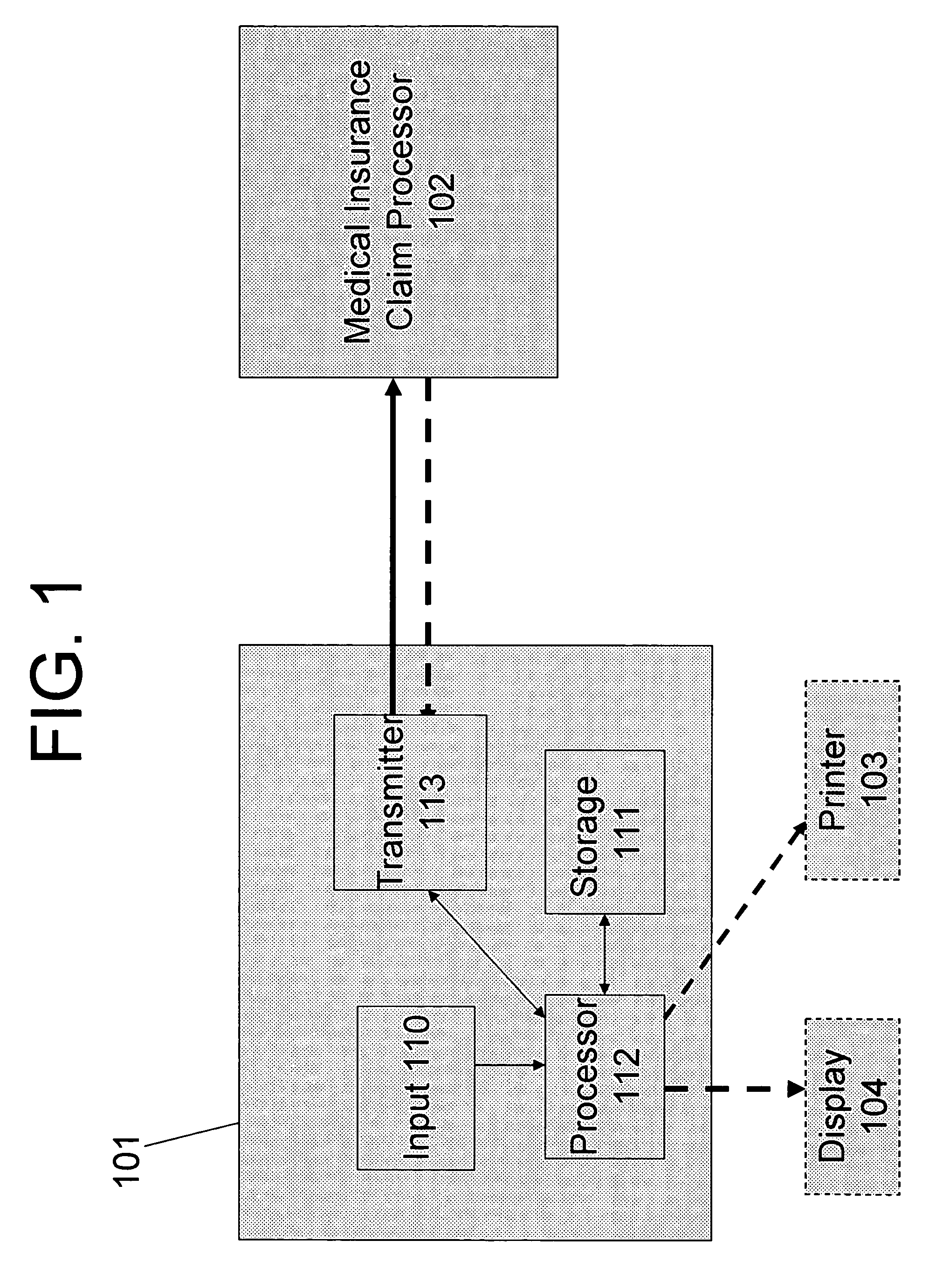
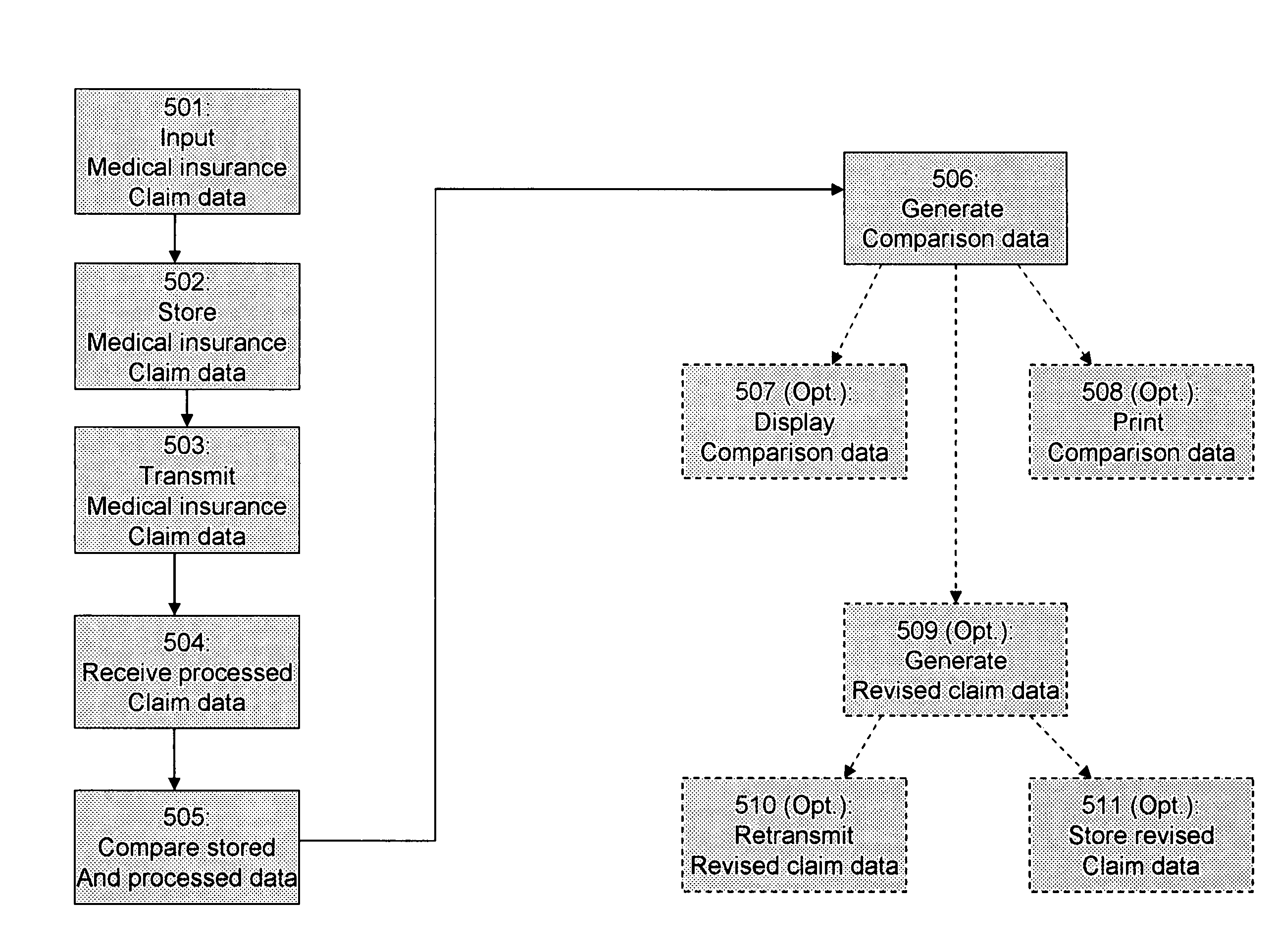
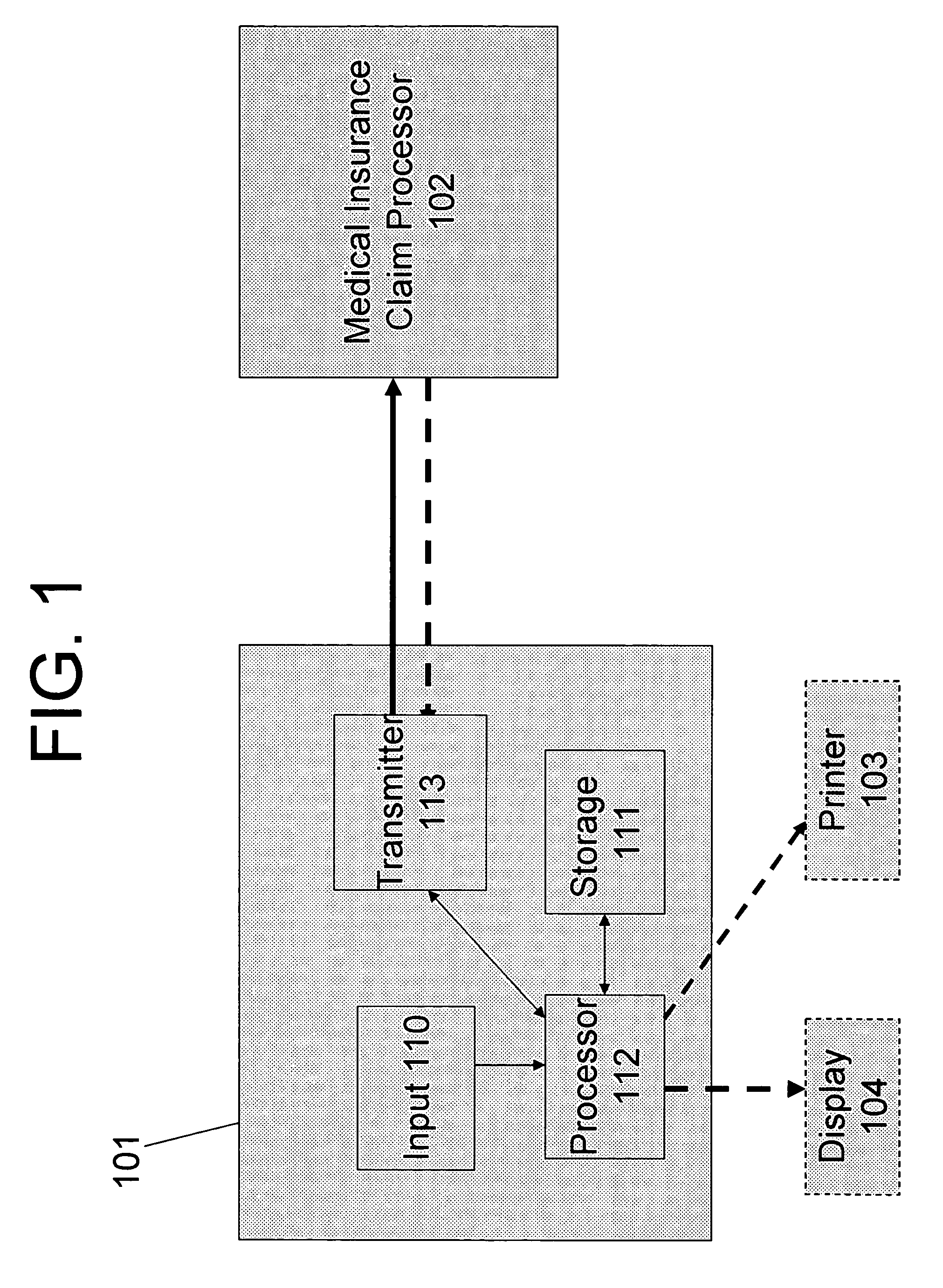
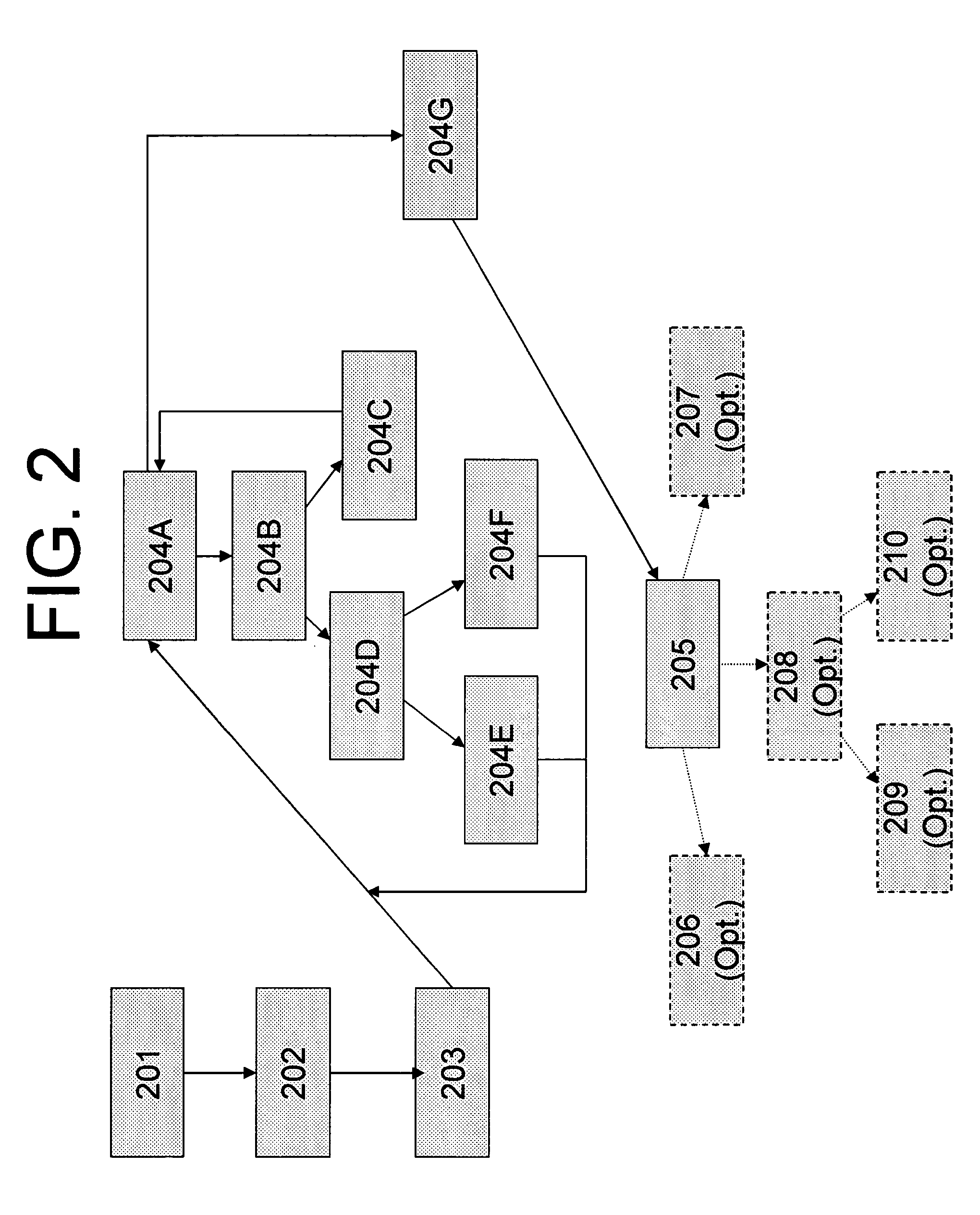
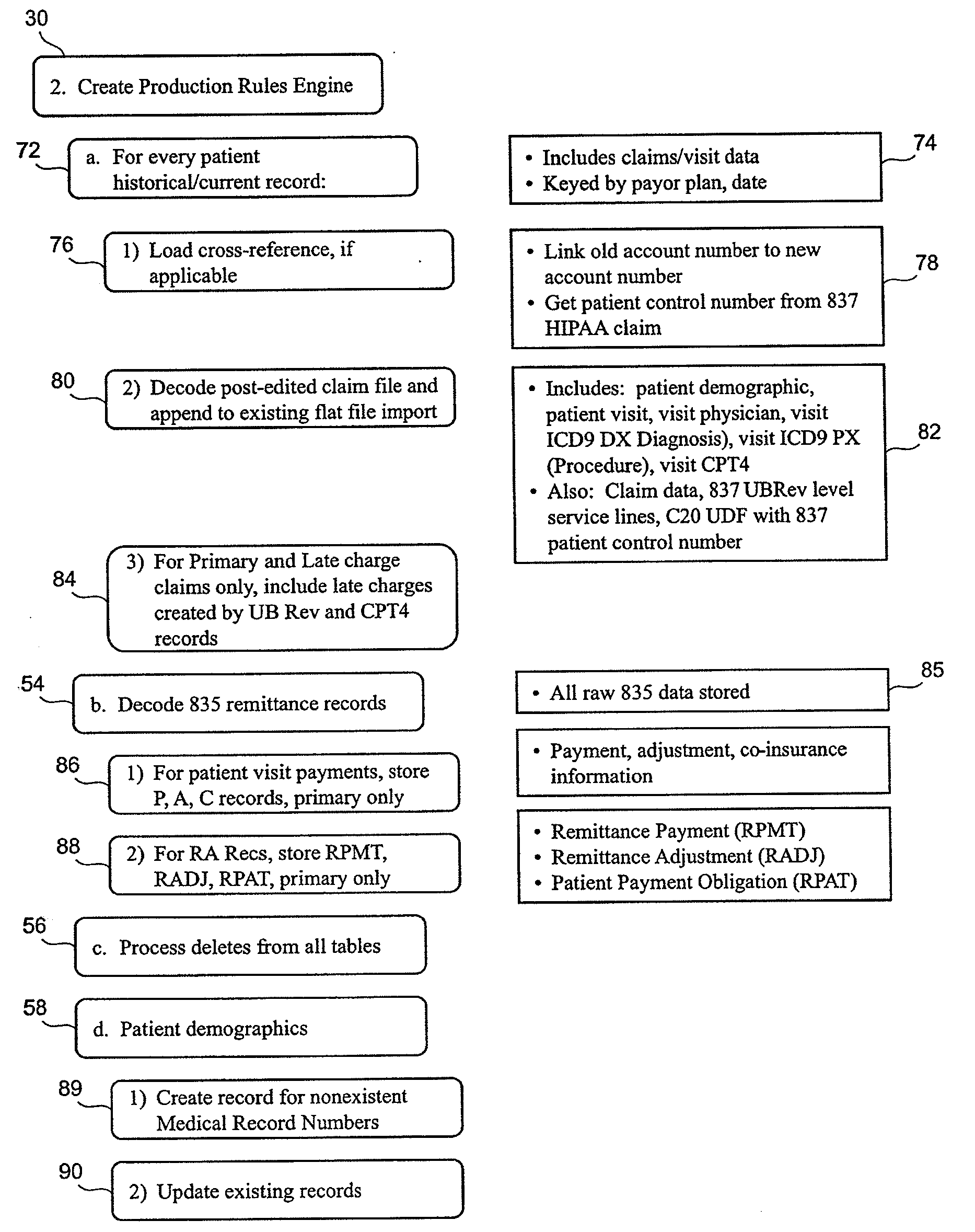
System and method for verifying the accurate processing of medical insurance claims
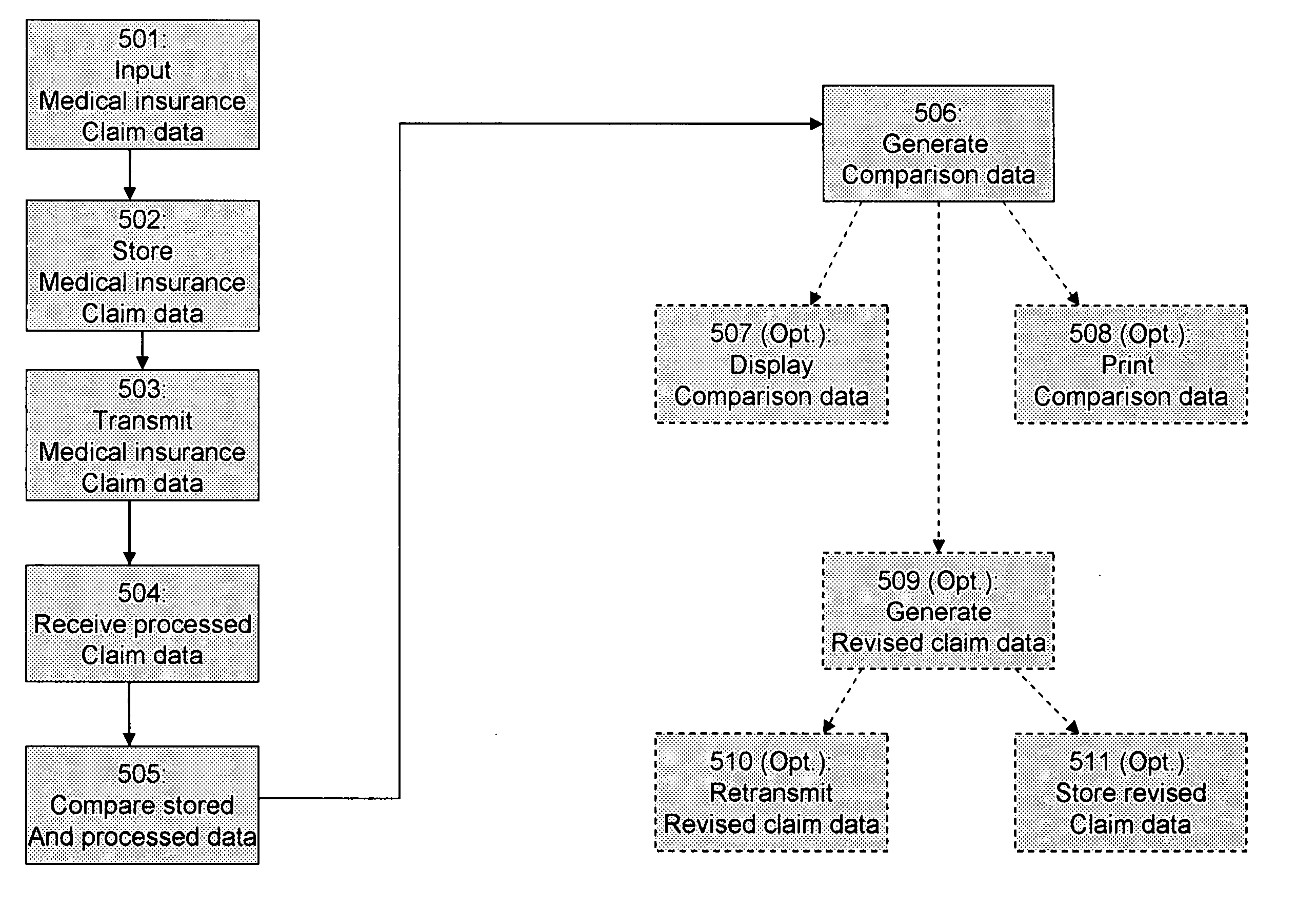
In a system and method for verifying the accurate processing of medical insurance claim data generated by a health care provider, a health care provider enters medical insurance claim information (data) into a health care provider terminal. The medical insurance claim data may include patient identification data and treatment data. The health care provider terminal stores and transmits the medical insurance claim data to a medical insurance claim processor operated by a medical insurance company. The medical insurance claim processor processes the claim data received from the health care provider terminal and generates processed claim data. Processed claim data may include patient identification data, treatment data, and payment data. Upon receipt of the processed claim data, the health care provider terminal compares the processed claim data with the stored medical insurance claim data originally submitted to the medical insurance claim processor. The health care provider terminal then generates comparison data indicating whether the stored medical insurance claim data has been processed in accordance with predetermined claim processing rules, which may be negotiated and agreed to by the health care provider and the medical insurance company. The comparison data also identifies processing errors, if any, in the processed claim data received from the medical insurance claim processor. The health care provider terminal may also generate and retransmit revised medical insurance claim data when the processed claim data has not been processed in accordance with the predetermined processing rules. Also, the health care provider terminal may automatically retransmit the medical insurance claim data to the medical insurance claim processor when the medical insurance claim data have not been processed within a defined period of time. Additionally, the health care provider terminal may verify the accuracy of treatment data prior to transmitting the medical insurance claim data to the medical insurance claim processor.
Owner:EZ FOB
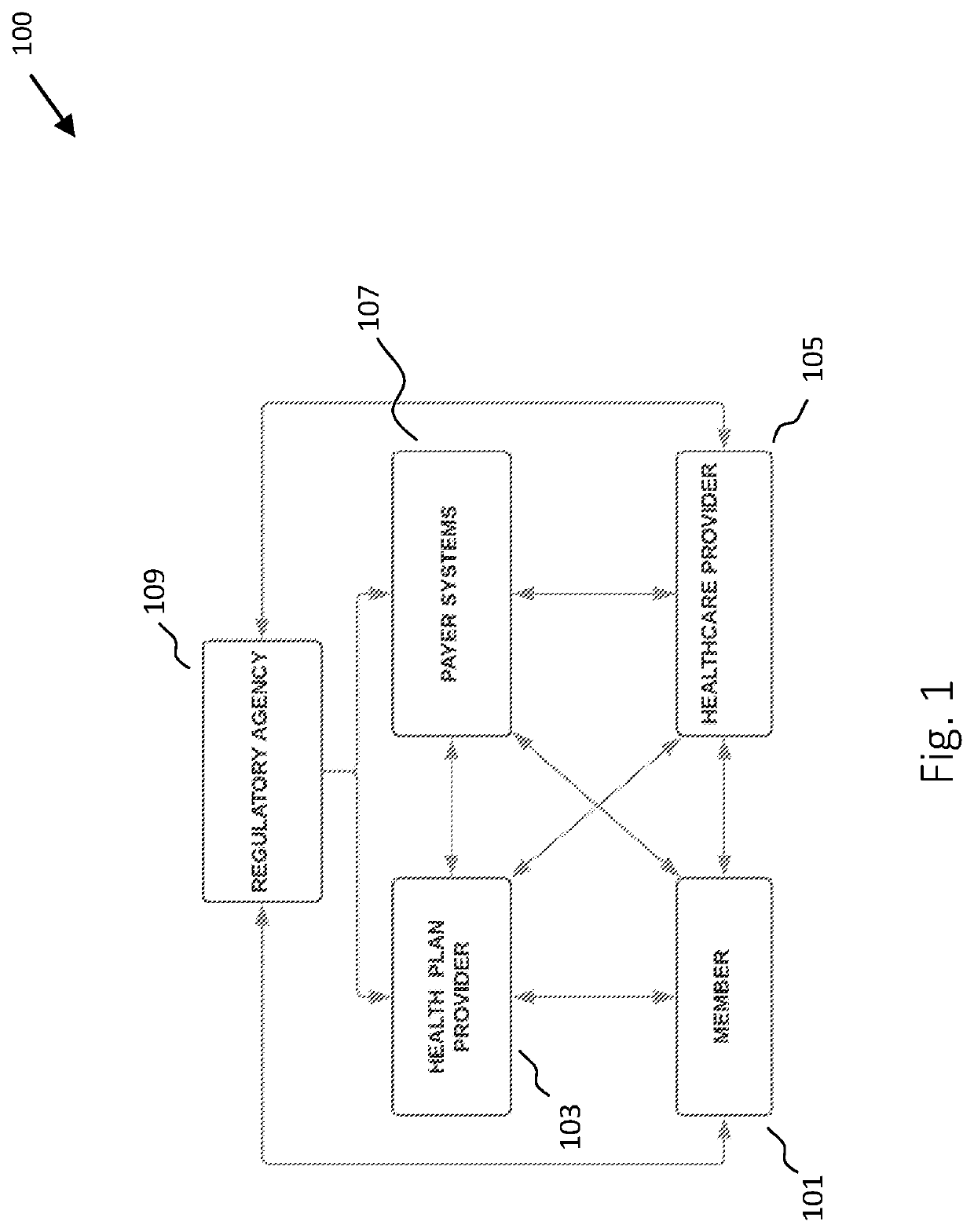
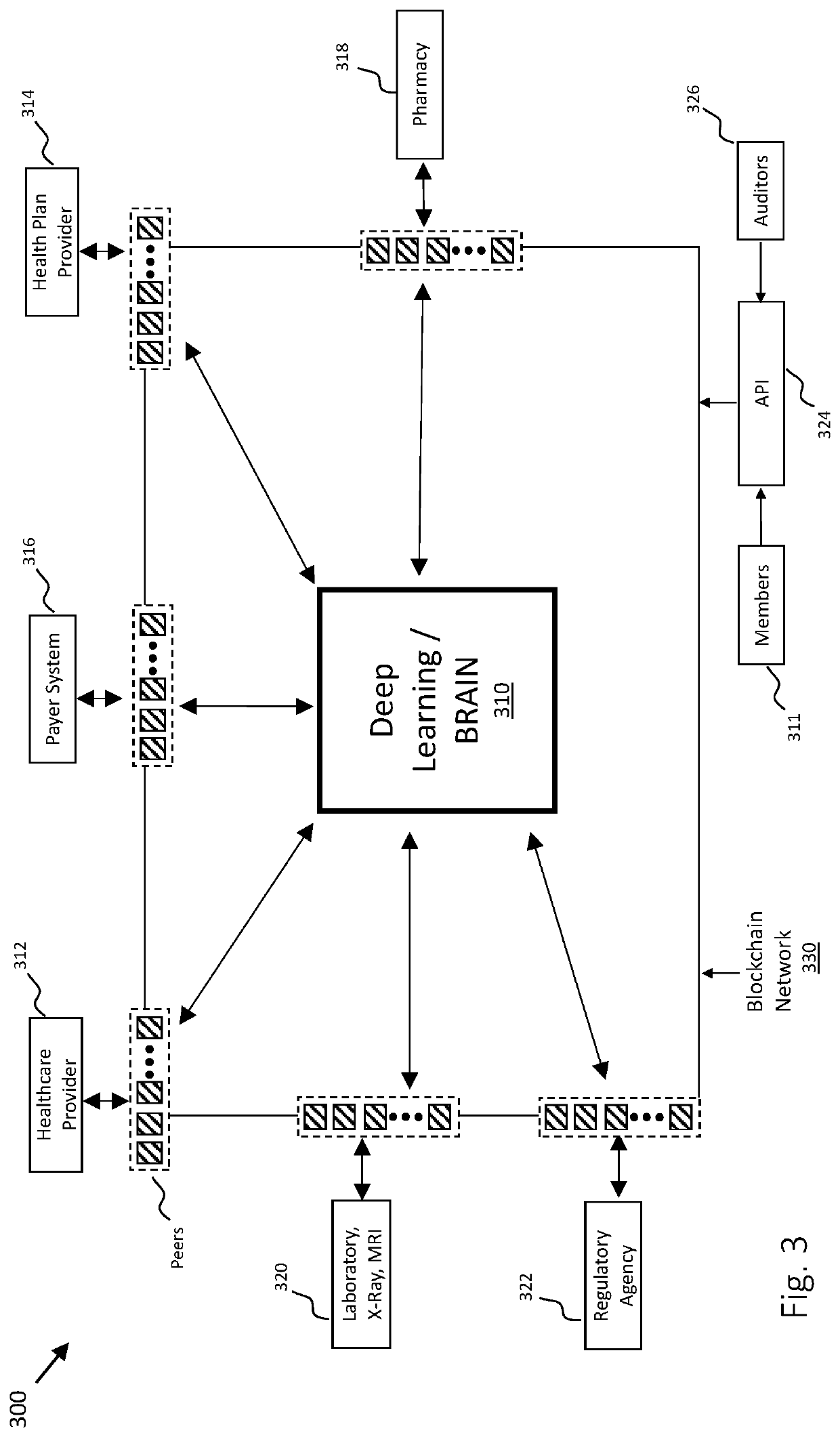
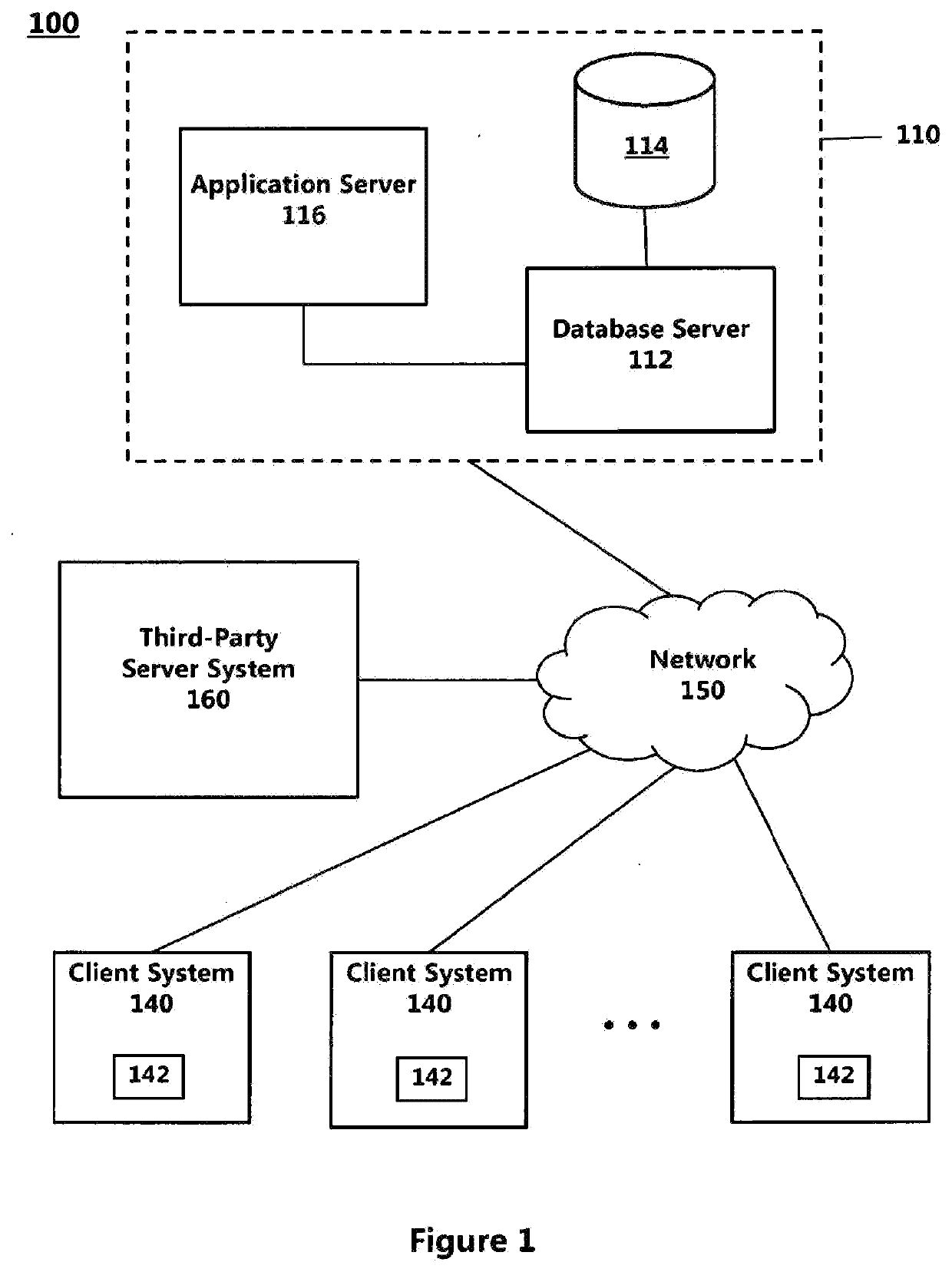
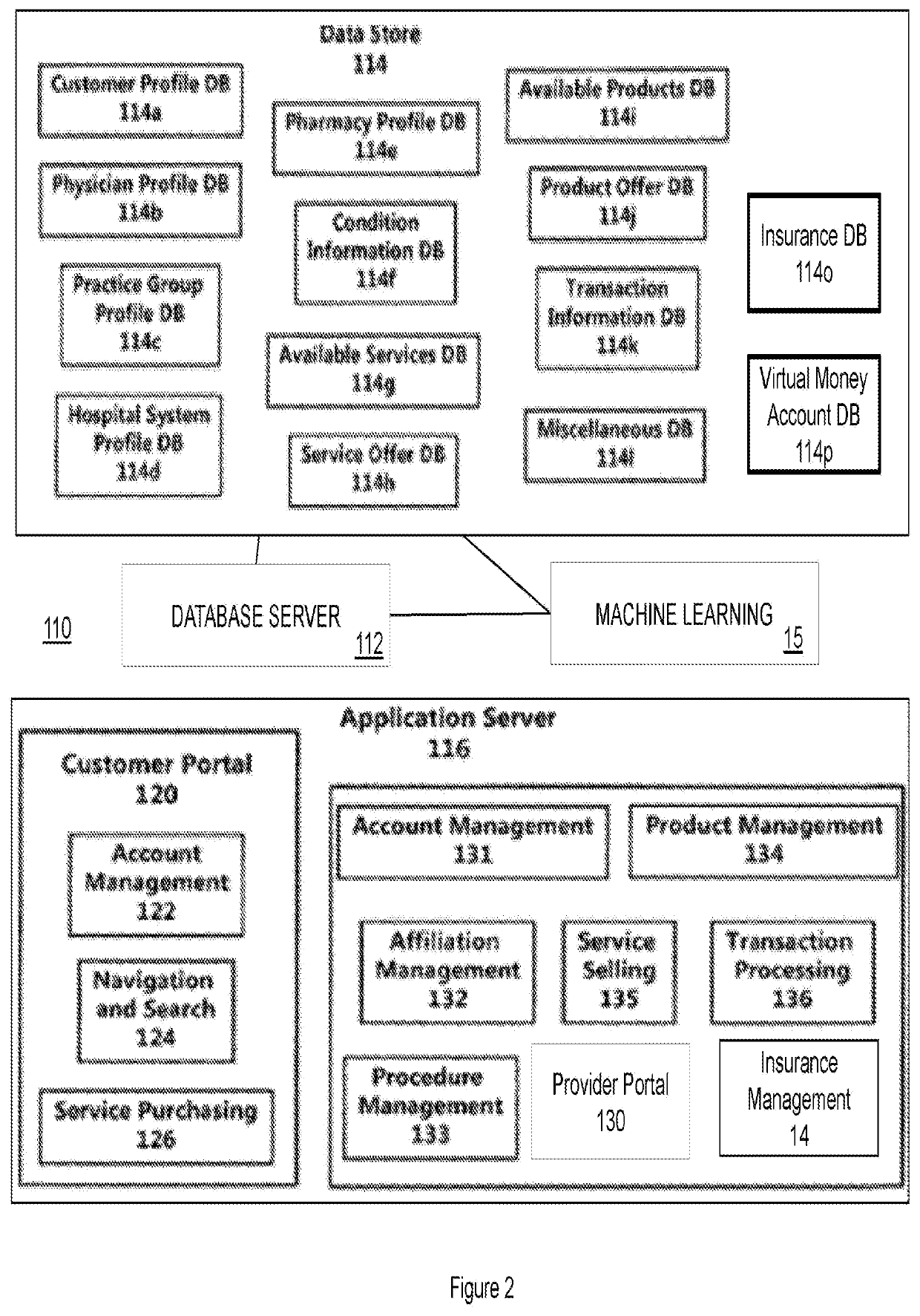
System and Method for Auditing, Monitoring, Recording, and Executing Healthcare Transactions, Communications, and Decisions
Systems and methods are disclosed for monitoring, recording, verifying, auditing, and executing healthcare communications, decisions, and transactions using centralized storage and blockchain technology. The healthcare communications relate to communications between a patient, doctor, specialist, healthcare provider, a private or government entity that processes and reimburses healthcare providers, insurance provider, and a healthcare facility.Systems and methods are disclosed for processing, monitoring, recording, verifying, auditing, and executing healthcare communications, decisions, and transactions using centralized storage and blockchain technology. The healthcare communications relate to communications between a patient, doctor, specialist, healthcare provider, a private or government entity that processes and reimburses healthcare providers, insurance provider, and a healthcare facility.In one embodiment, the system processes a healthcare transaction that relates to medical care provided for a patient that has a medical health plan. The method involves providing a centralized control manager for obtaining, storing, and analyzing healthcare transaction data.The centralized control manager is connected to a central database and utilizes the central database for storing healthcare data. The centralized control manager operates through a processor. The processor executes instructions stored in the database leading to the centralized control manager performing its functions.The centralized control manager is electronically and communicatively connected to at least two entities that are part of the authorized entities within the computer network. These entities may include a patient, doctor, primary physician, specialist, payer system, health plan provider, and government entity such as Medicare. The centralized control manager allows bidirectional communication with the centralized control manager and other authorized entities that are allowed to communicate with the centralized control manager and use an electronic device over a computerized network. Communications directly between the entities is also contemplated.The entities electronically execute a healthcare transaction. The centralized control manager records each executed healthcare transaction into the centralized database as well as posts the transaction to the blockchain. Each entity performing the transaction also posts the details of the transaction to the blockchain. Details include the time and date of transaction, the parties involved, and other details of medical care provided to the patient relating to the transaction.A prediction engine, utilizing machine learning technology, uses the data of all the transactions obtained to continuously enhance and predict the outcome of future transactions and make suggestions as needed. If any transaction deviates above a certain limit, e.g. a medical claim is filed or a medical code is entered that does not fall within a set limit, the prediction engine flags the transaction for review and optionally alerts the entities involved in the transaction.All of the transactions are replicated to the blockchain by multiple entities in the computer network. These include the transacting entity, the receiving entity, and the centralized control manager. Posting to the blockchain allows for verification and authentication of the transactions.System and methods also allow automated claim adjudication and dispute resolution between two parties in the healthcare environment. The claim adjudication and dispute resolution relate to medical care provided for patients who have a medical health plan.The system includes a server computer and a computing device. The server computer is comprised of a central database and a processor as well as a server application that is stored in the central database. The computing device includes an electronic device having a client processor and client database. Both the server and client are communicatively connected.In this embodiment, a Healthcare Provider executes a transaction that is recorded in the centralized database as well as in the blockchain. The server computer electronically stores the data of the healthcare transaction in the central database and provides access of the transaction to the Healthcare Provider, Payer, and other relevant parties.Thereafter, the Healthcare Provider files a dispute with the Payer System. The server computer electronically sends an alert to the relevant and authorized parties informing them that a dispute has been filed. The server processor then obtains data from the central database, blockchain, and any other relevant data provided by other parties in the computer network that relate to the disputed healthcare transaction. The processor then parses the data, resolves the dispute, and posts the results to the centralized server and blockchain.
Owner:PATEL MITESHKUMAR ISHWARBHAI
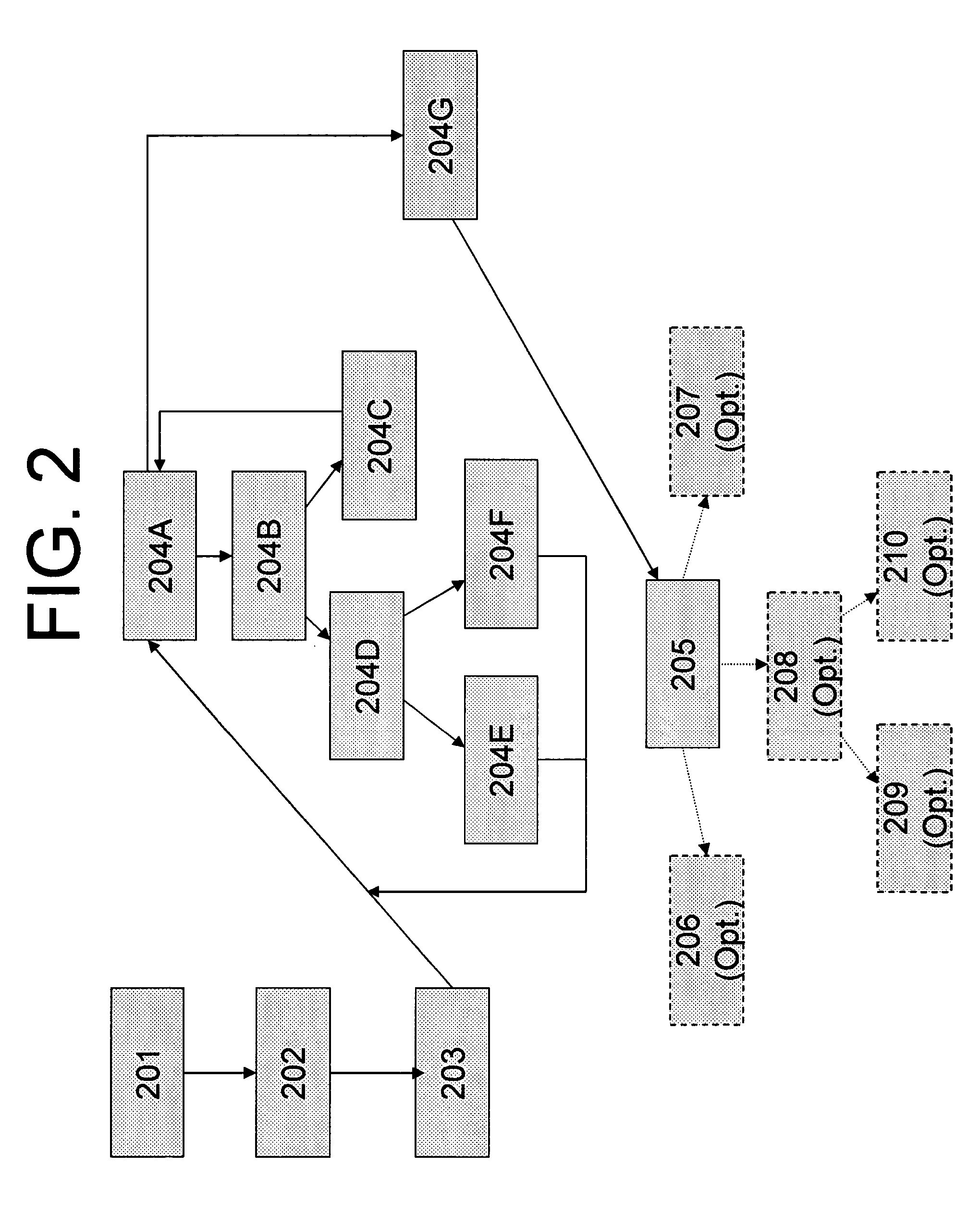
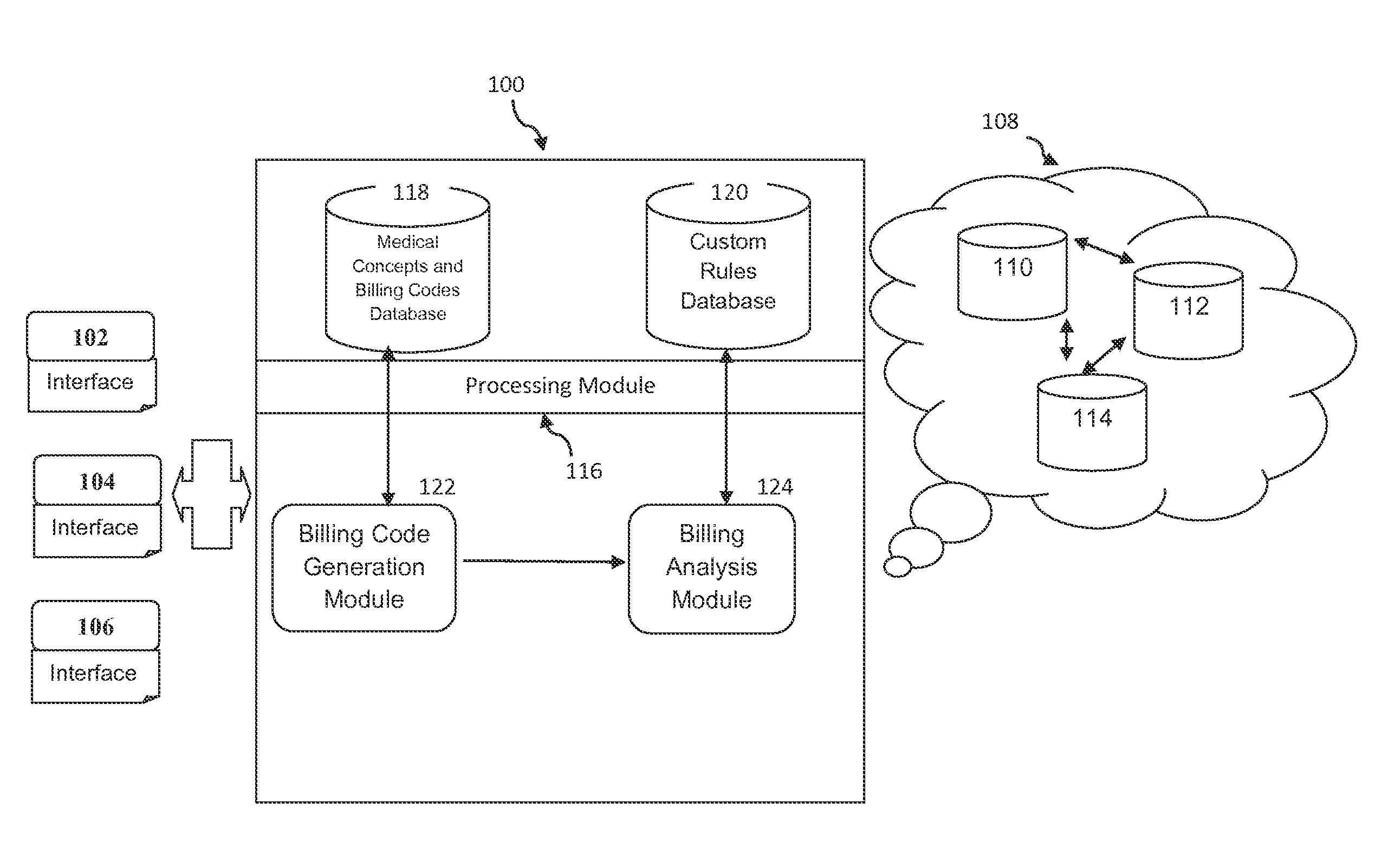
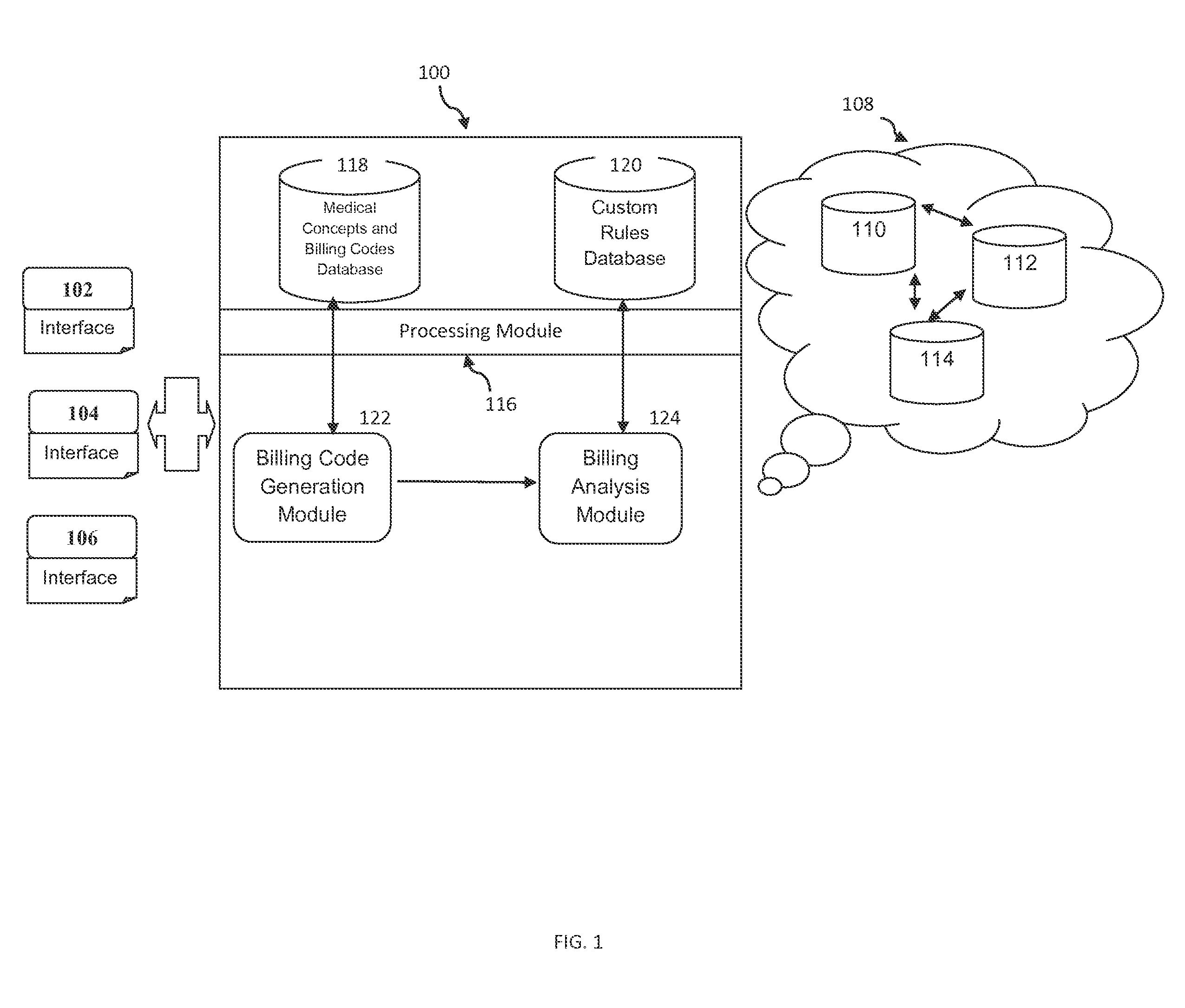
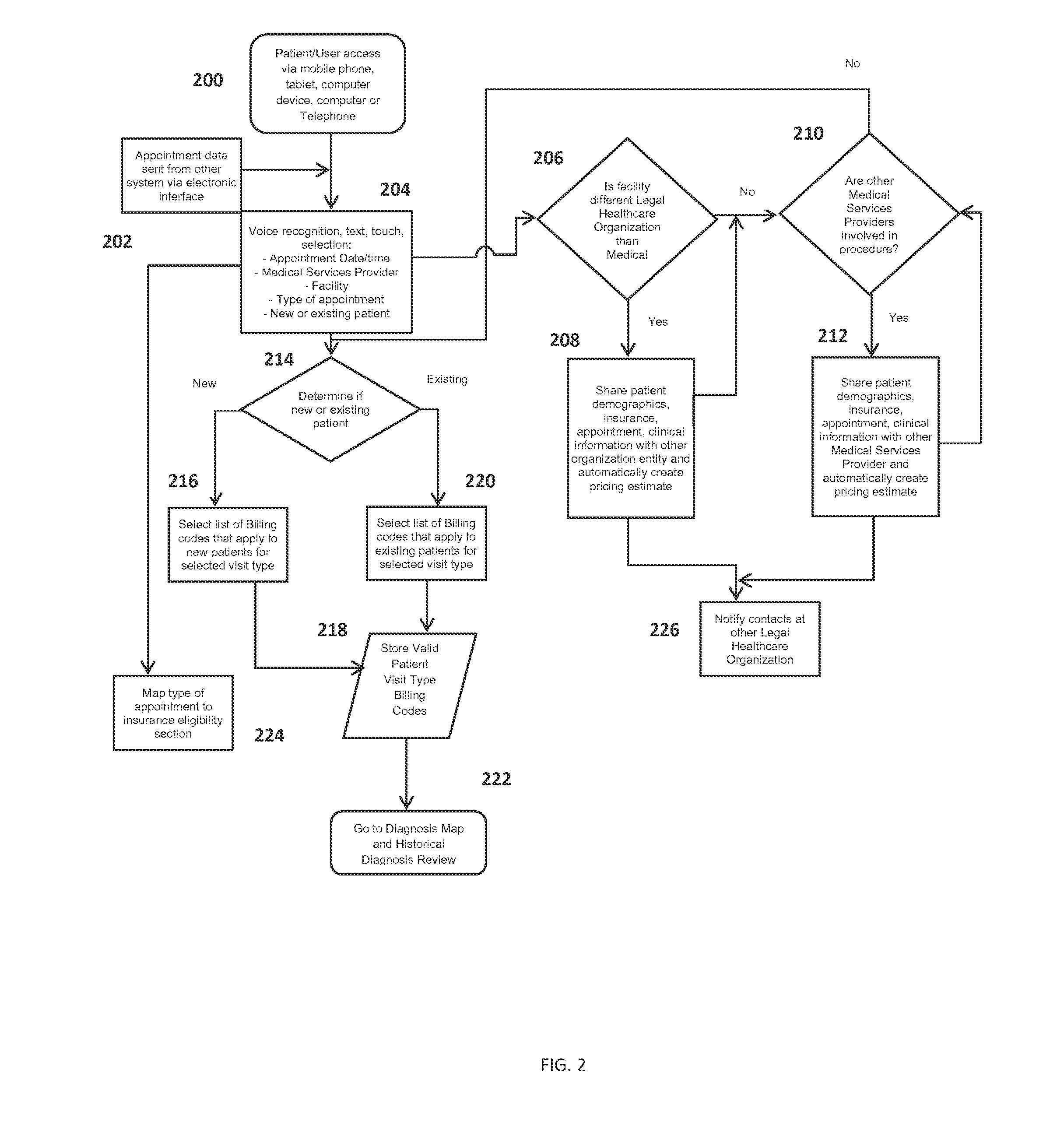
Method and a system for estimation of medical billing codes and patient financial responsibility
A system and method for estimating medical billing codes and patient's financial responsibility for the services availed or to be availed by patients from medical services providers and legal healthcare organizations is provided. The system provides a platform to users such as patients, medical services providers, and legal healthcare organizations to be informed in advance about estimated prices of medical services and medical insurance coverage to be availed by the patients. Patient's financial responsibility is calculated from medical concepts stored in the system and corresponding historical billing codes and medical insurance coverage for a patient. Further, methods of setting custom rules in the system to refine results based on patient demographics and other parameters are provided. Advantageously, the system provides automatic sharing of information among users and notifications on updated information and helps the users to enquire, network and market their services.
Owner:ENABLEDOC LLC
Medical self-service comprehensive service system
InactiveCN104050613AEasy to see a doctorShorten waiting time for medical treatmentData processing applicationsMedicineSelf-service
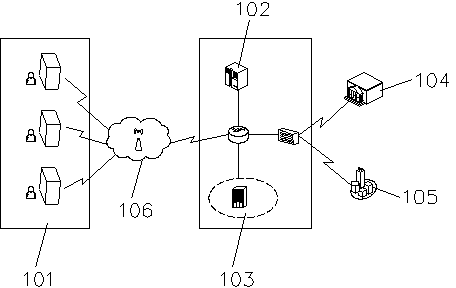
The invention relates to a medical self-service comprehensive service system which comprises a man-machine interaction self-service terminal, a self-service central control server and a hospital information management server. The man-machine interaction self-service terminal is connected with the self-service central control server, the hospital information management server, a medical insurance information management server and a bank financial service server through a communication network. Through operation of a patient at a self-service machine of the man-machine interaction self-service terminal, the man-machine interaction self-service terminal collects information and conducts information interaction with the self-service central control server, the hospital information management server, the medical insurance information management server and the bank financial service server to achieve the medical procedures of appointment, registration, settlement, medicine taking, report printing ad inquiring. The medical self-service comprehensive service system is used for hospital occasions and greatly shortens medical queuing time of patients, a novel diagnosis and treatment mode is provided for hospitals, the patients and family members, and hospitalization is facilitated.
Owner:YLZ INFORMATION TECH CO LTD
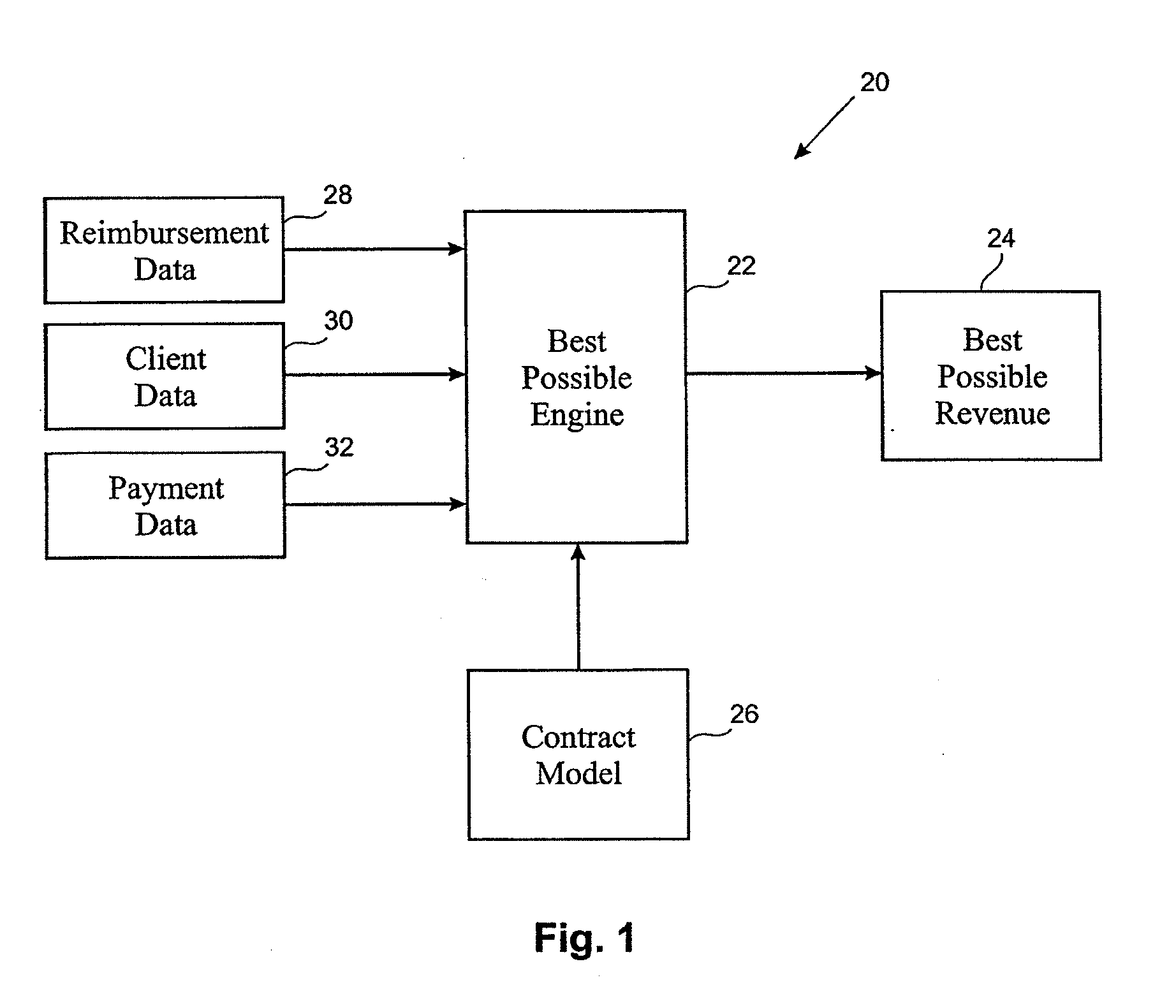
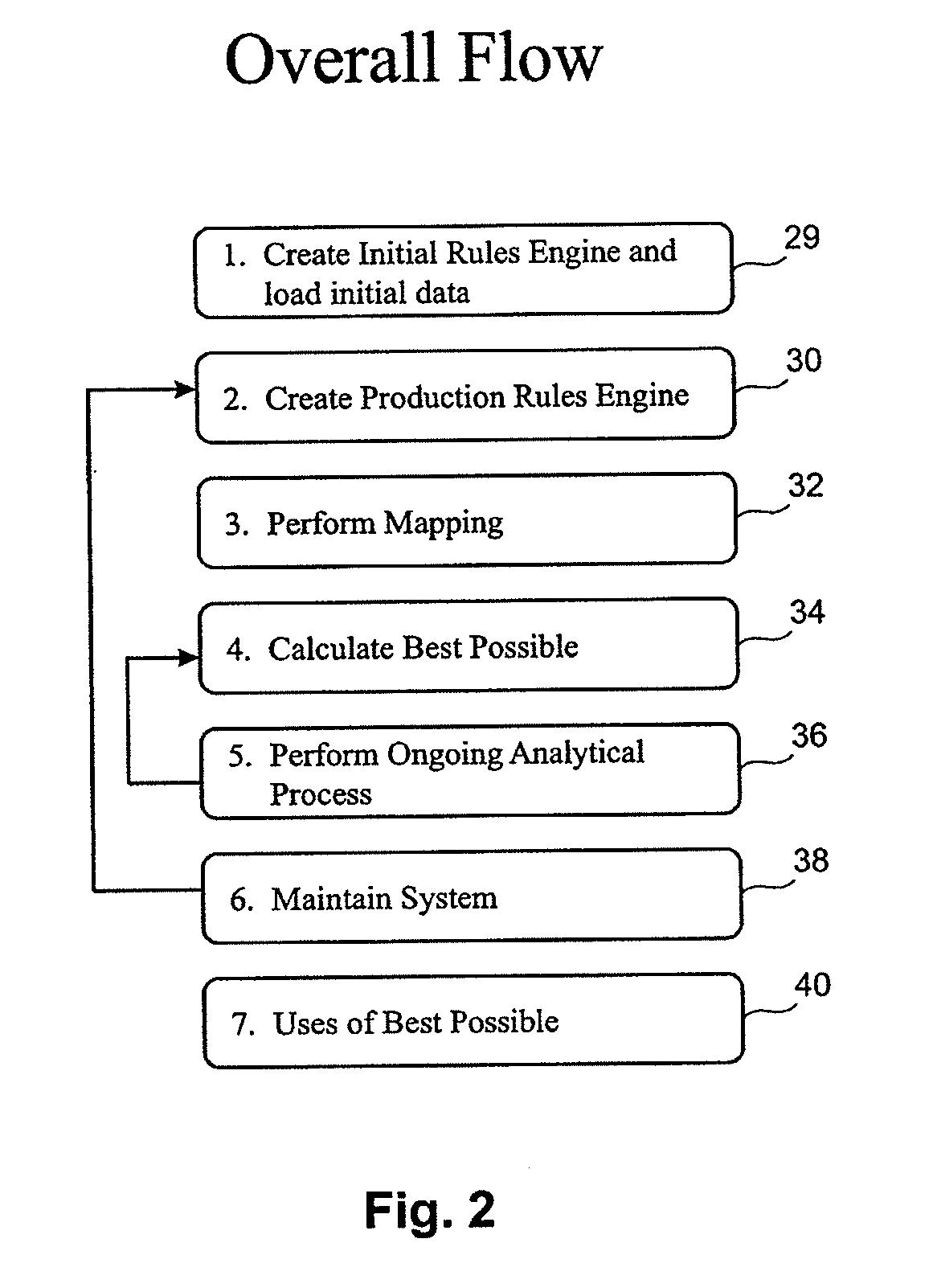
Best possible payment expected for healthcare services
ActiveUS20090326974A1Effectively effectivenessImprove performanceFinanceForecastingThird partyProgram planning
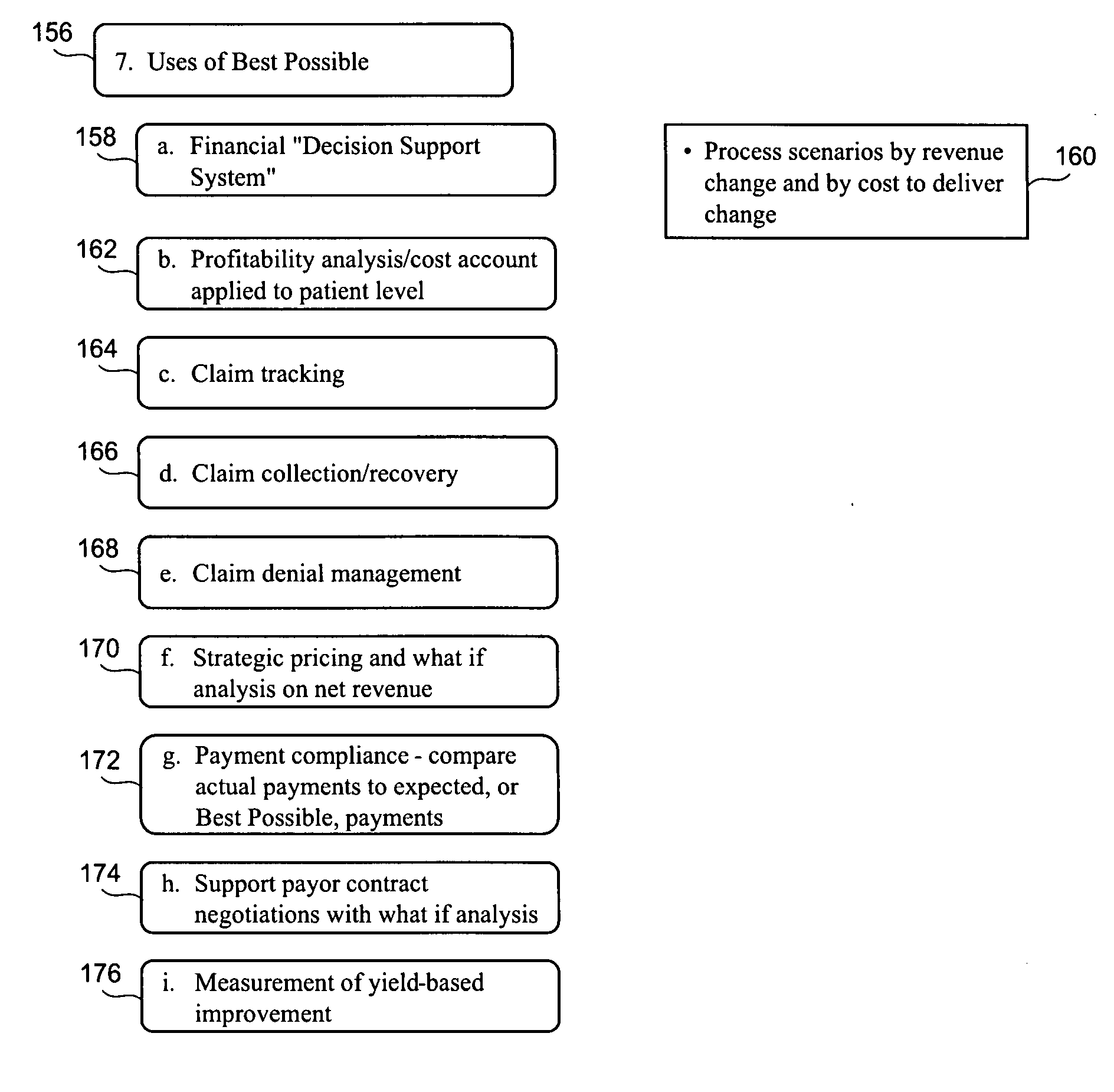
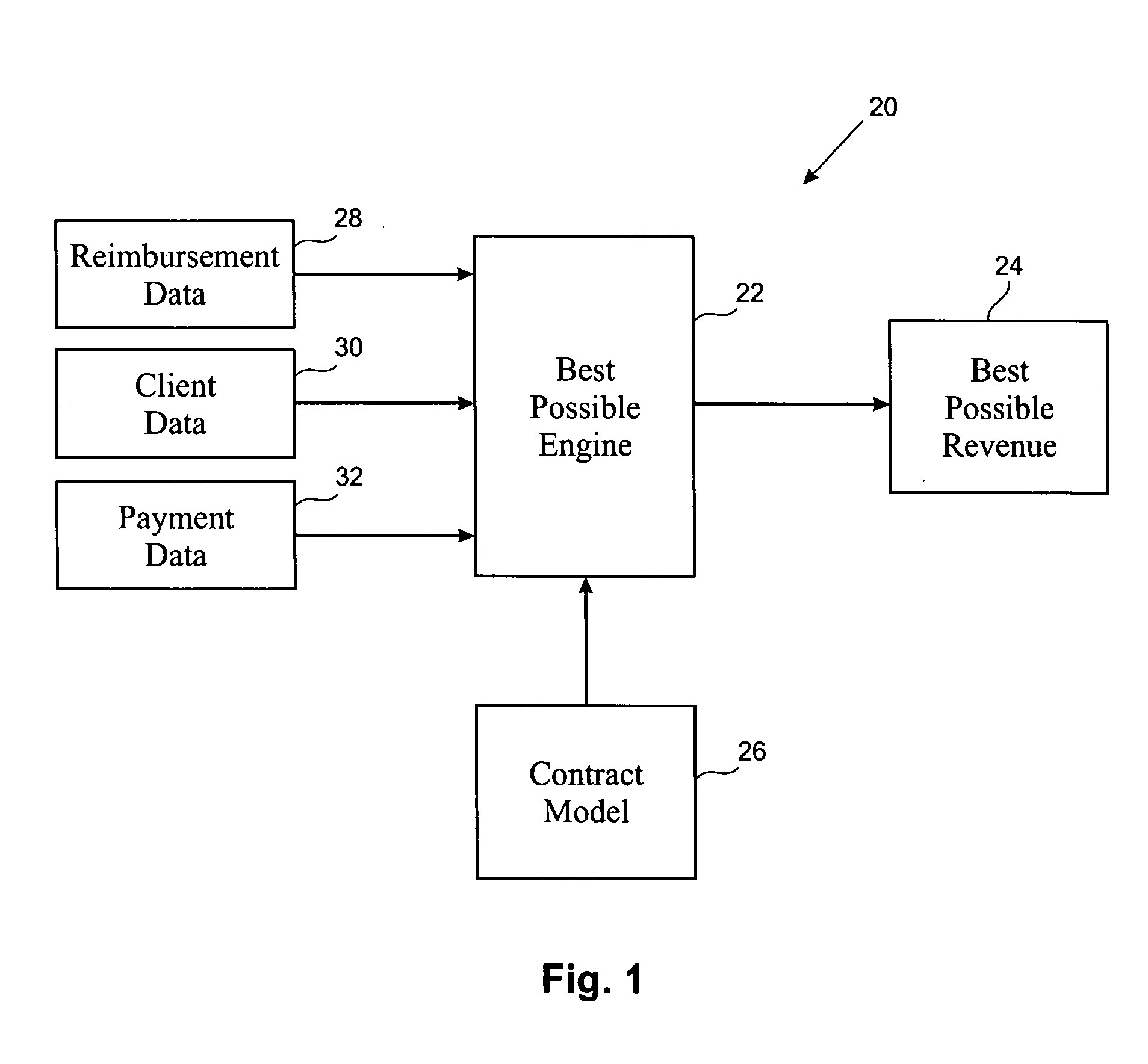
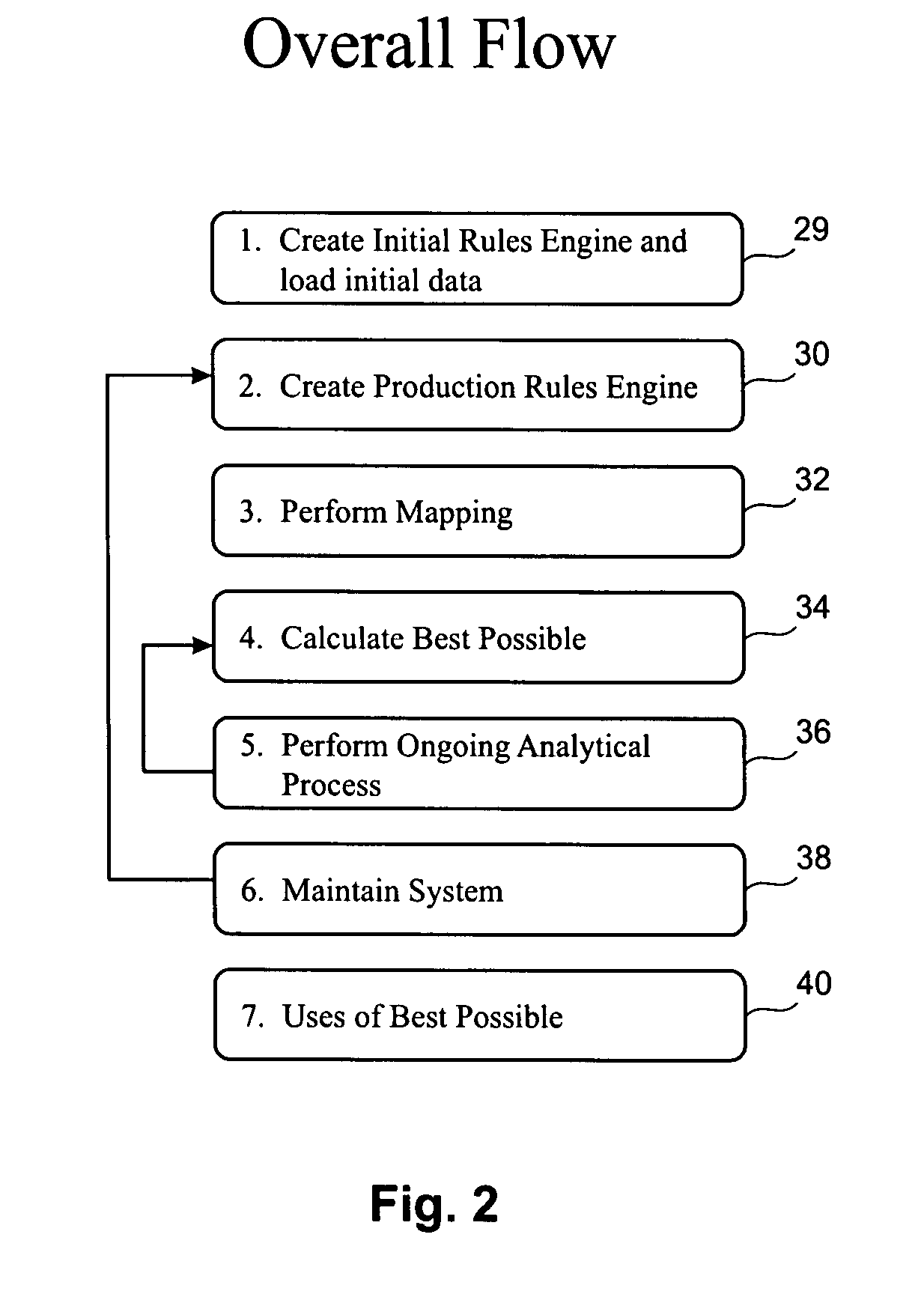
A system is disclosed that is useful by hospitals and other healthcare providers for automatically determining the best possible or maximum amount of payments a healthcare provider can lawfully expect to receive for healthcare resources which takes into account various discounts agreed upon by the healthcare provider with various private insurance companies as well as public (i.e., government) insurance providers, which administer managed healthcare plans including Medicare and Medicaid, all payments received against expected payments and a yield measurement approach for determining the providers performance at a given point in time and across various segments of its operations. In accordance with one aspect of the present invention, contracts between a healthcare provider and all private insurance companies and public insurance providers may be modeled. Various data including healthcare resources provided to patients up to a given point in time, applicable insurance company, and healthcare resource code are entered into the system. The system is able to calculate the best possible revenue that the healthcare provider can lawfully expect to receive taking into account the various discounts negotiated with the various insurance companies. Indeed, once the data is loaded, the system can provide an accurate snapshot of a healthcare provider's best possible expected revenues at any given time based upon services rendered instead of waiting until the healthcare resources have been billed out to insurance companies, patients, and third party payers. It can also provide an accurate snapshot of all payments received against those expected payments to determine yield across various segments of its operations.
Owner:R1 RCM INC
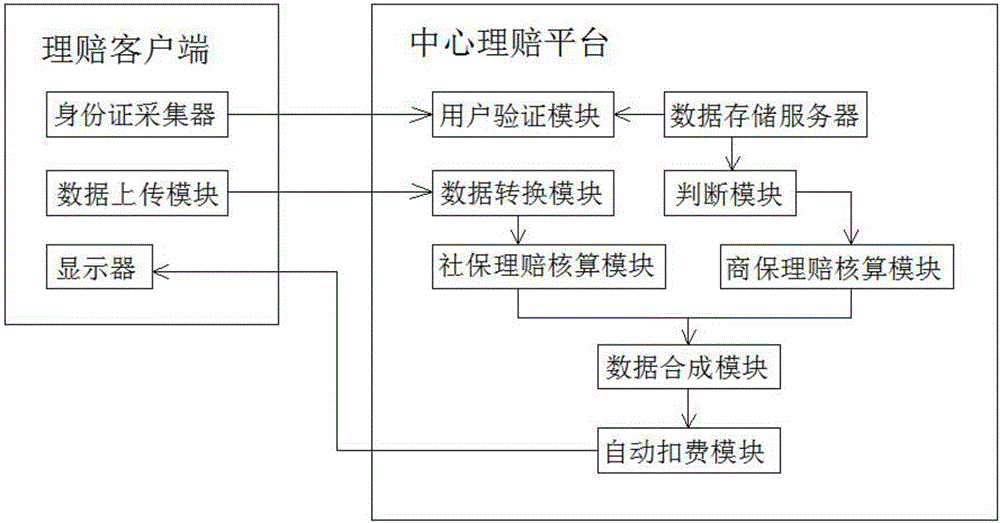
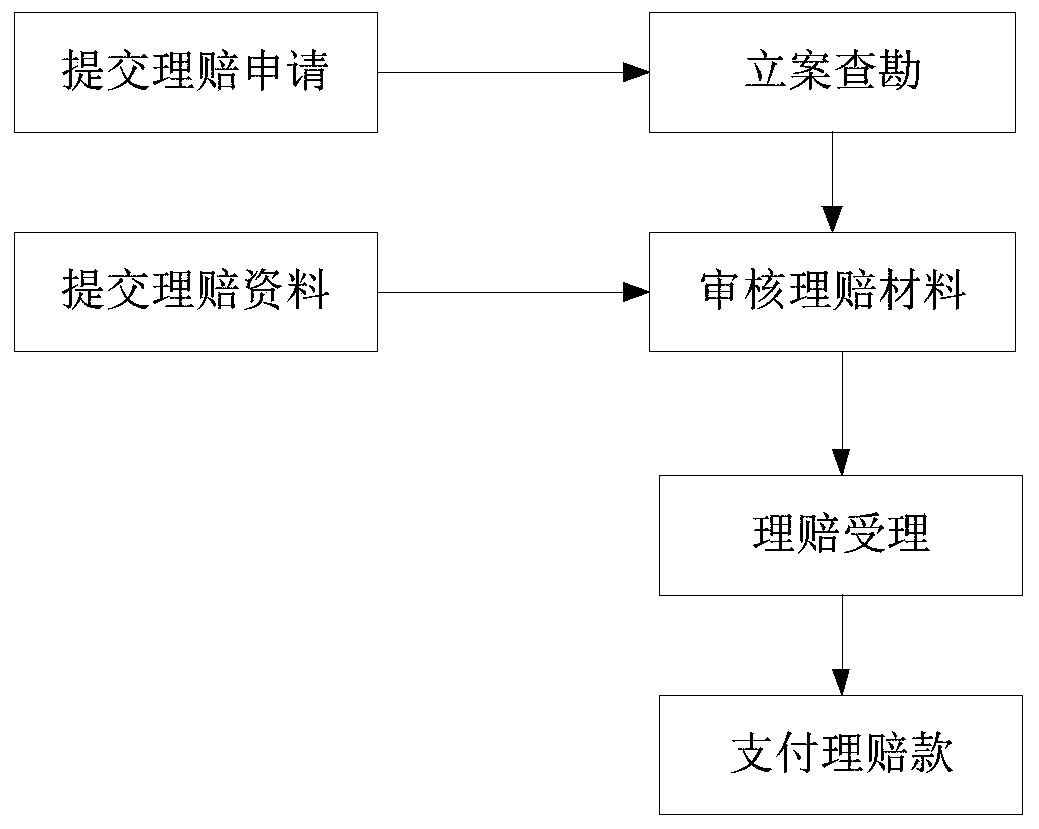
Medical insurance claim settlement management system
InactiveCN106295152ARealize automatic accountingAchieve claimsSpecial data processing applicationsHealth insurance managementAutomatic deductionNetwork communication
The invention discloses a medical insurance claim settlement management system. The medical insurance claim settlement management system comprises a claim settlement client-side and a central claim settlement platform which are connected through network communication. The claim settlement client-side comprises an identity card collector, a data uploading module and a display module. The central claim settlement platform comprises a user identification module, a data storage server, a data conversion module, a social insurance claim settlement check computation module, a judgment module, a commercial insurance claim settlement check computation module, a data synthesis module and an automatic deduction module. The medical insurance claim settlement management system can achieve doctor seeing data parameterization, calculate claim settlement data through an algorithm and automatically deduce claim settlement fees according to synthesized claim settlement data after the check computation is completed, achieves automatic check computation and claim settlement of medical insurances, can improve the working efficiency, reduce the operation cost, improve the risk management and control capability and provide automatic timely claim settlement for clients.
Owner:合肥奇也信息科技有限公司
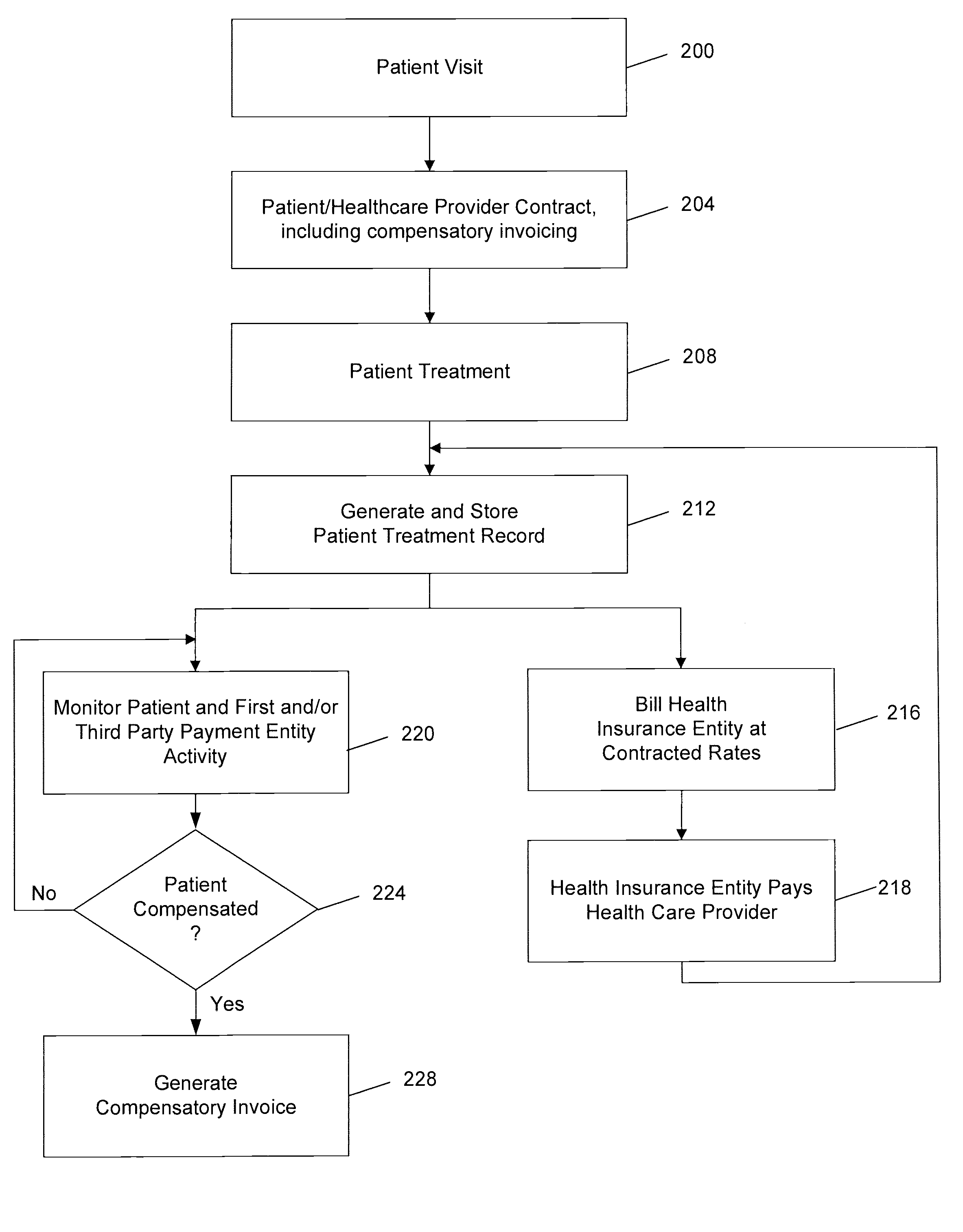
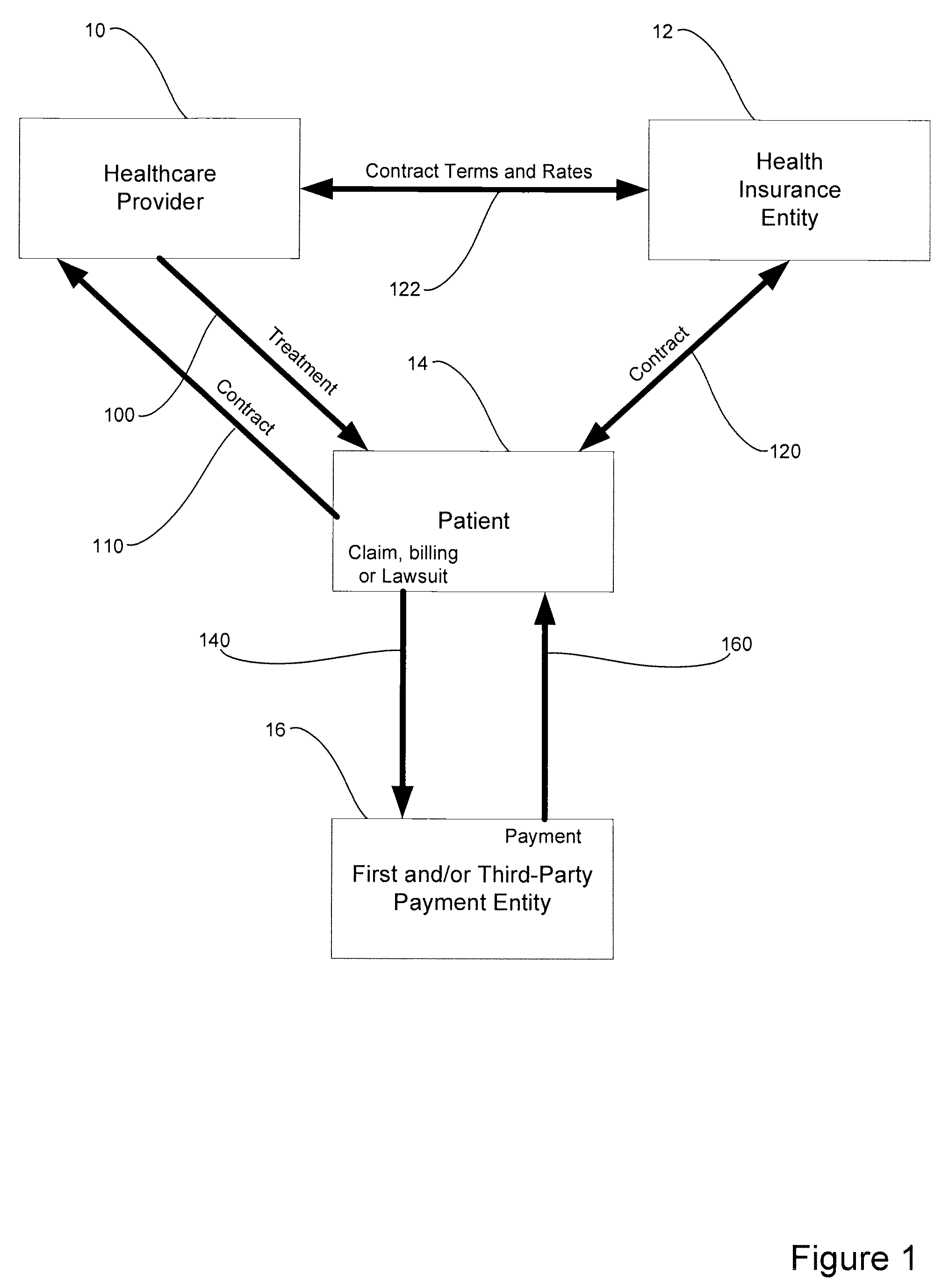
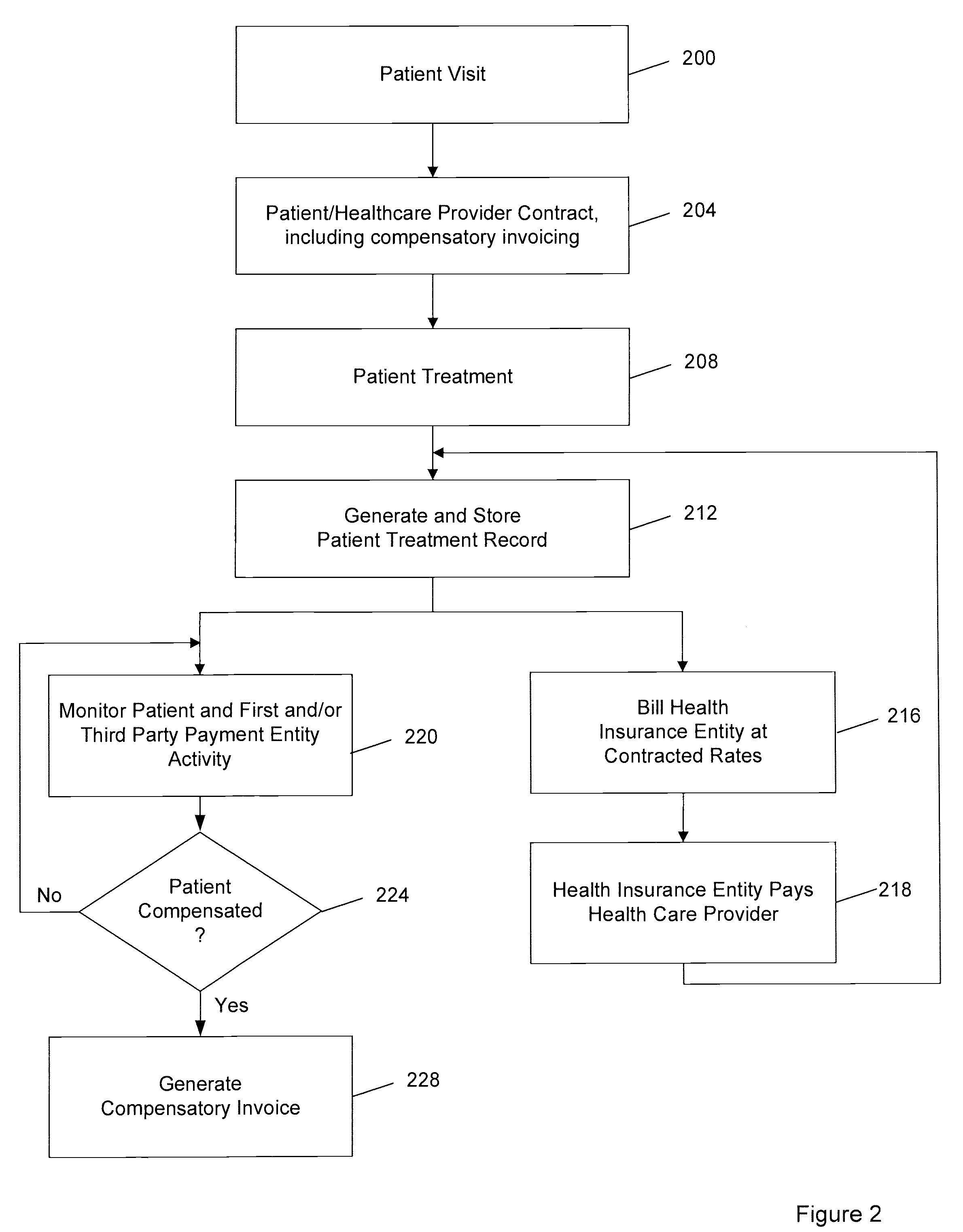
System and method for enabling health care providers to effect compensatory invoicing of patients who use a coverage entity in addition to their health insurer
A system and method is provided for compensatory invoicing of a patient for health care services rendered by a Health Care Provider. The system and method enables a Health Care Provider to obtain payment of Full Rates for services rendered to a patient in circumstances where a Health Insurance Entity provides less than full-rate compensation (e.g., compensation at Contracted Rates) to the Health Care Provider AND the patient has been reimbursed additionally by another payment party for claims already paid for by the Health Insurance Entity. In one implementation, the patient contracts with the Health Care Provider to ensure that the Health Care Provider is fully compensated for the services rendered after the patient receives payments from a First and / or Third Party Payment Entity (e.g., an auto insurance carrier, worker's compensation insurance carrier, Medpay, PIP etc.) for the services. The invention tracks claim(s) filed by the patient against the First and / or Third Party Payment Entity and tracks payment(s) made by the First and / or Third Party Payment Entity to the patient. The patient and / or the First and / or Third Party Payment Entity is then billed for the difference in payments made to the Health Care Provider by the Health Insurance Entity, effecting compensatory invoicing for a Full Rate fee chargeable by the Health Care Provider in cases when a First and / or Third Payment party has reimbursed the patient for similar services as already reimbursed by the Health Insurance Entity.
Owner:AMBROSE STEPHEN D
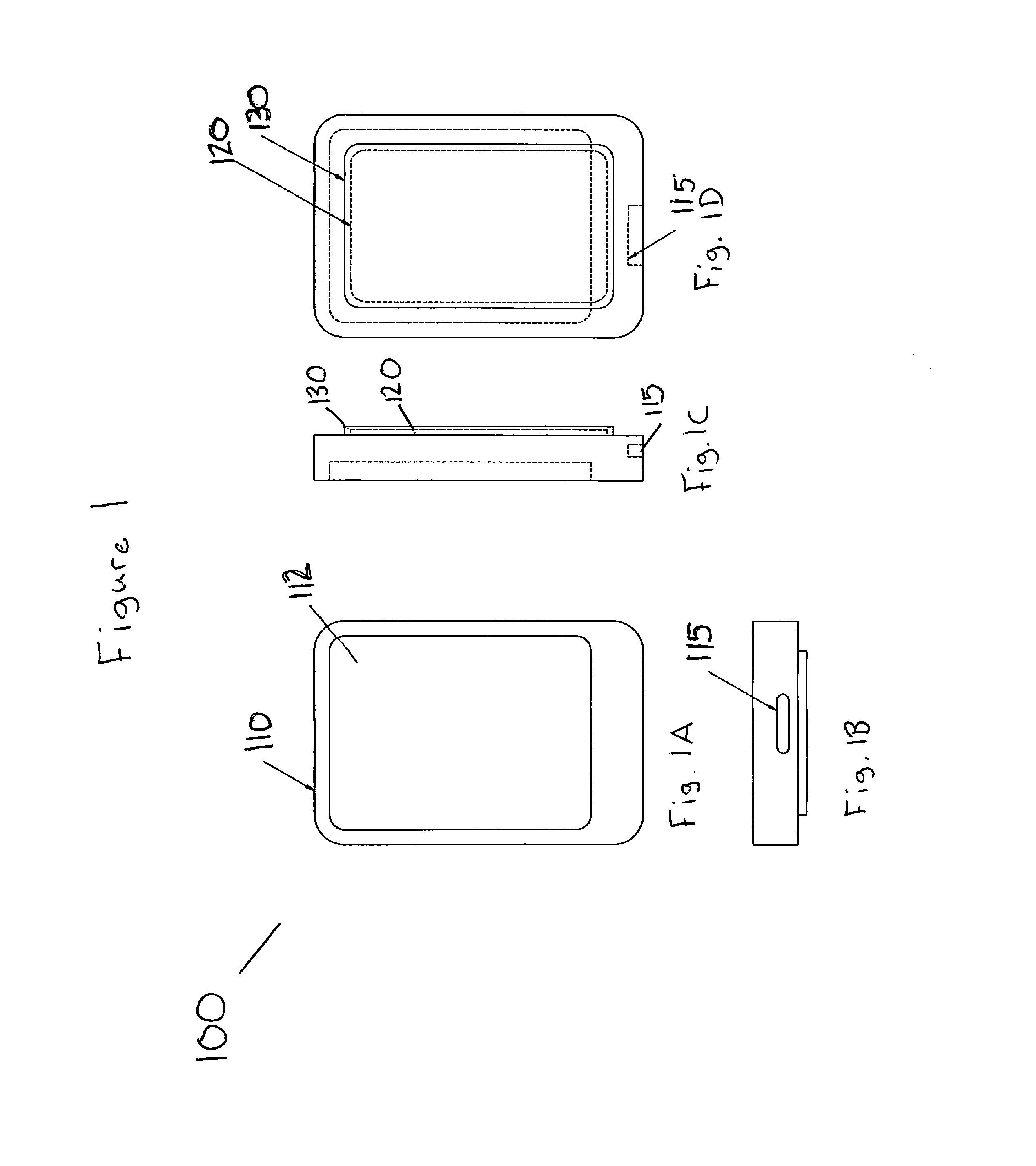
Smart phone casing and information exchange system
InactiveUS8733648B2Data processing applicationsDevices with card reading facilityComputer scienceTelephony
The embodiments of the present invention relate to a smart phone casing and information exchange system which enables a user to carry a single system that merges the digital and telecommunications necessities of the individual with the personalized cards, membership accounts, consumer credit and / or medical insurance or health information in a single source protected both physically with a hardened case, and digitally with appropriate safeguards for electronic protection.
Owner:MELBROD ANASTASIA +1
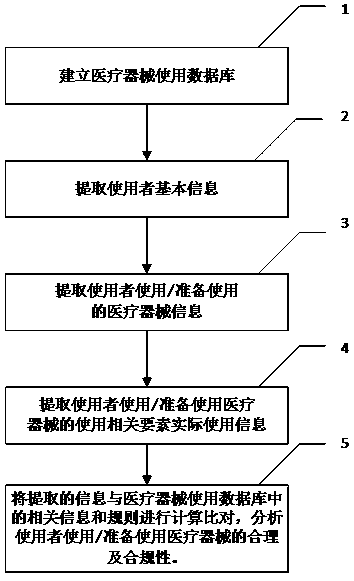
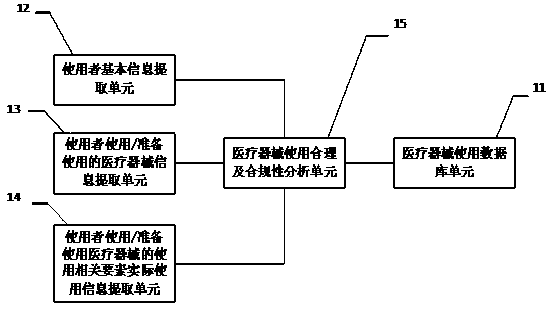
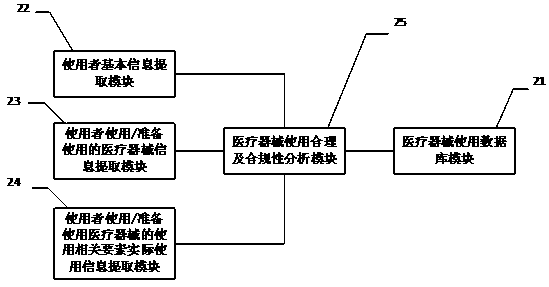
Method, system and equipment for reasonably using and analyzing compliance of medical instrument
PendingCN110717082AEfficient managementEffective paymentOffice automationOther databases queryingApparatus instrumentsCompliance analysis
The invention discloses a method, a system and equipment for reasonably using and analyzing compliance of a medical instrument. By establishing the medical instrument use database, extracting the userinformation, the used medical instrument information and the actual use information of the related elements when the user uses the medical instrument, and comparing the extracted information with themedical instrument use database, the use reasonability and compliance of the medical instrument can be analyzed. According to the method, the system and the equipment for analyzing the use reasonability and the compliance of the medical instruments, analysis results are provided for different users in different forms, the users are assisted to realize effective management of use of the medical instruments, and the users are helped to use the medical instruments safely, effectively, economically and properly; a medical administrative department, a medical insurance management institution, a medical institution, an insurance company, a market / quality supervision and management department, a commercial circulation management department and a production enterprise are helped to better manageuse, payment, sales and production of medical instruments.
Owner:曹庆恒
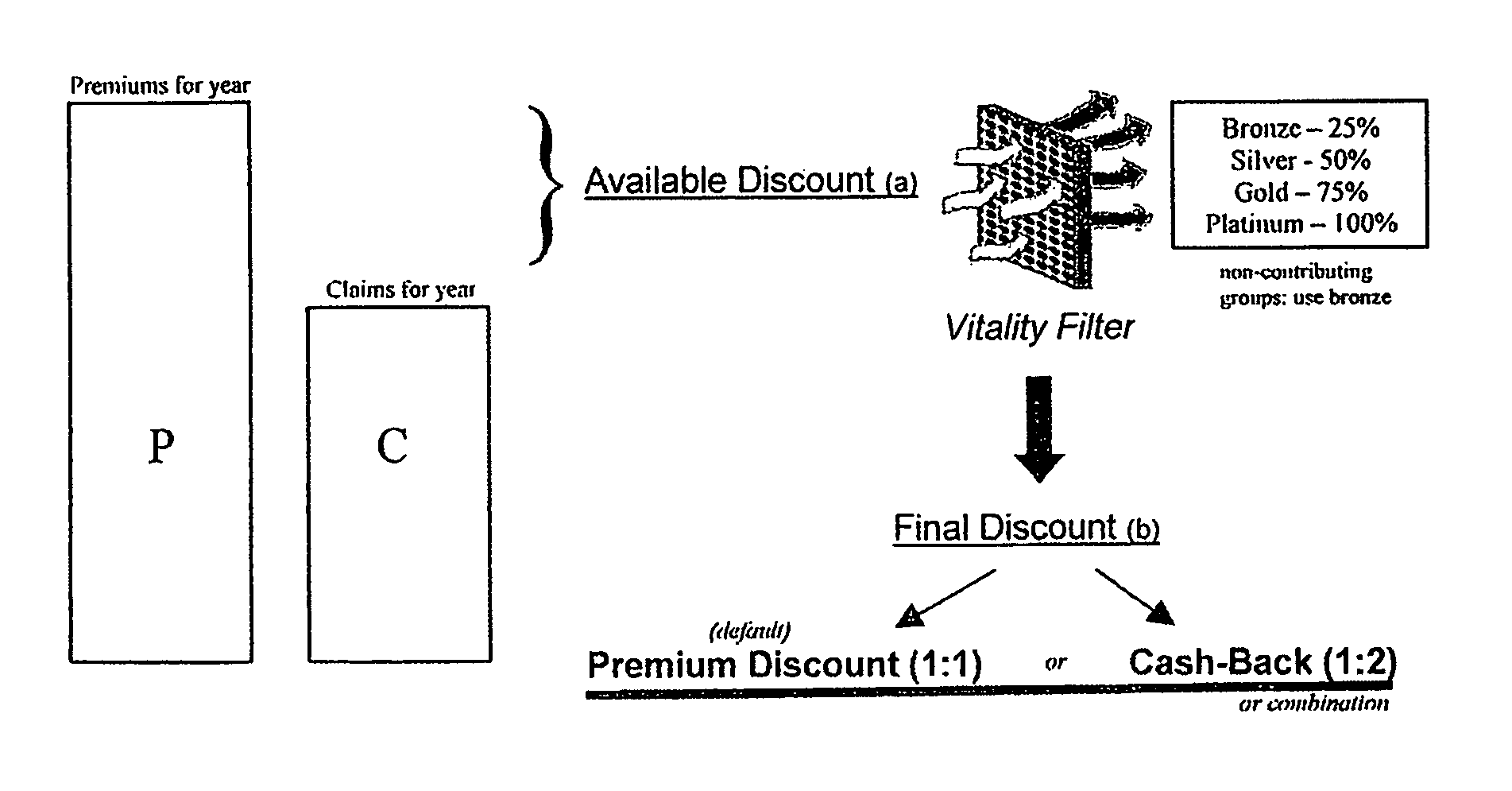
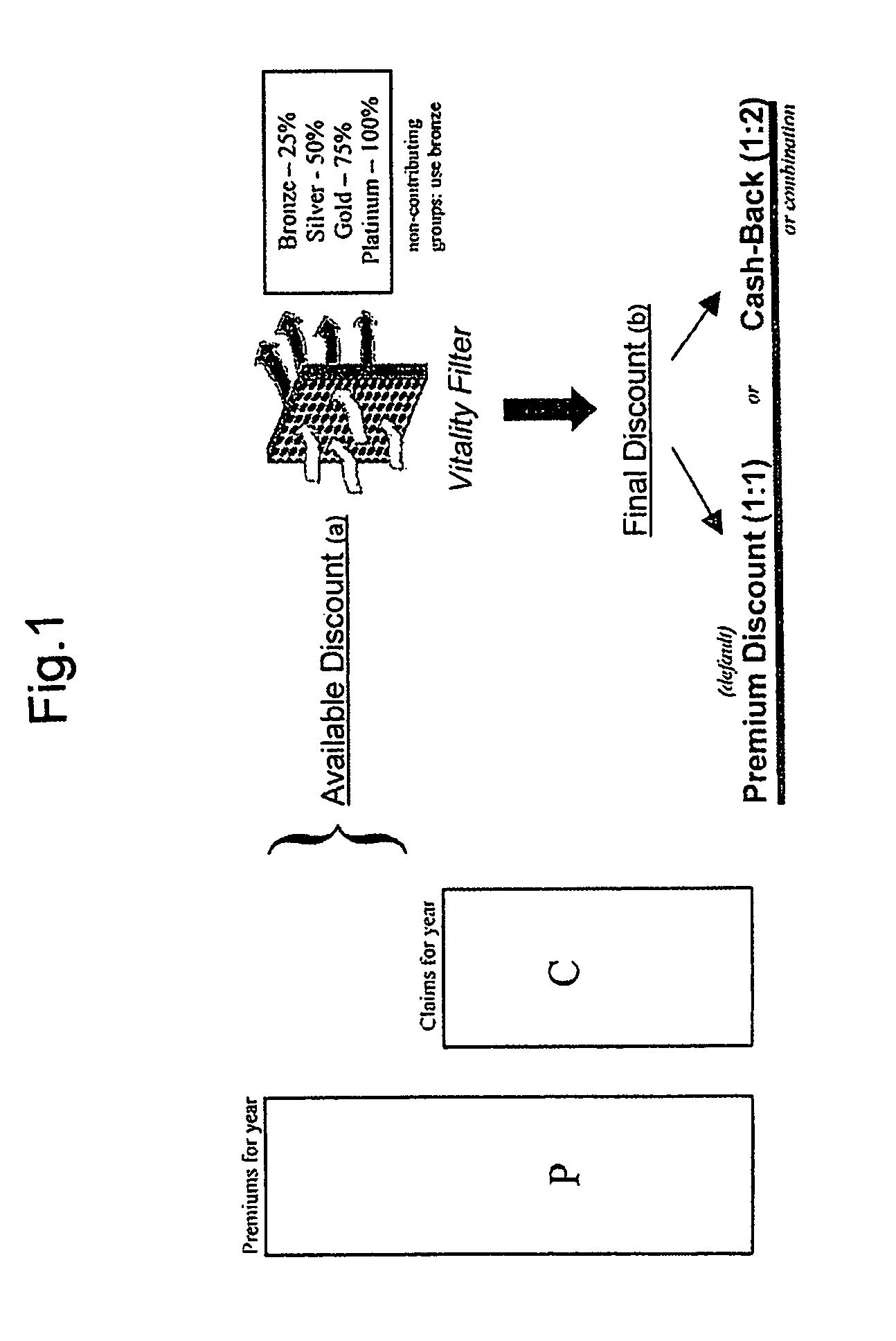
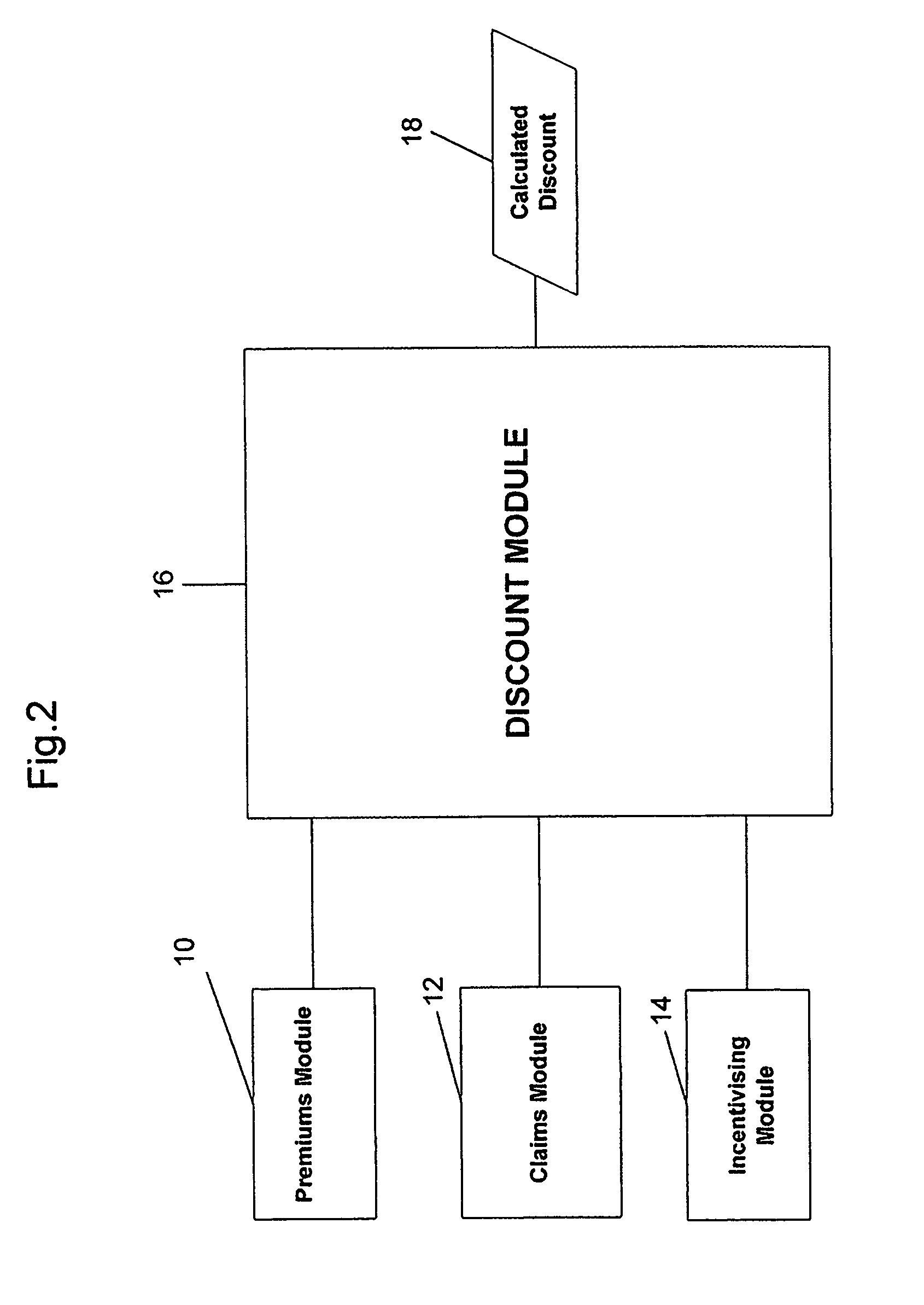
Data processing system for accurately calculating a policyholder's discount in a medical insurance plan and a method therefor
A data processing system for accurately calculating a discount in a medical insurance plan comprises a premiums module adapted to access data regarding the amount of premiums paid by a policyholder of the medical insurance plan for a predetermined period. A claims module is adapted to access data regarding the amount of claims paid by the medical insurance plan to the policyholder for the predetermined period, the claims module being further adapted to access data to determine if there have been any claims submitted by a policyholder which have not yet been paid, and if so to apply a set of rules to each submitted claim which has not been paid to determine if it is likely to be paid, and if the claim is likely to be paid then adding the amount of the claim to the amount of claims already paid for the predetermined period. Finally, a discount module adapted to receive data from the premiums module and the claims module and to use the data to calculate a discount amount.
Owner:VITALTY GRP INT INC
System and method for verifying the accurate processing of medical insurance claims
InactiveUS7904305B2Avoiding delay and burdenEasy to processFinanceOffice automationData transportEngineering
Owner:EZ FOB
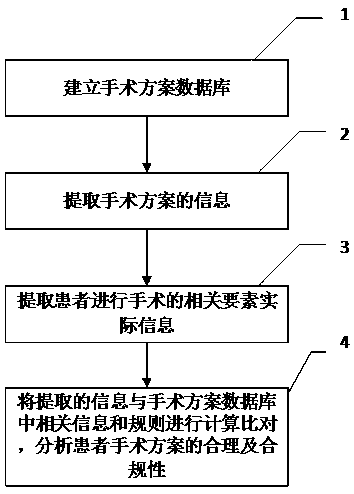
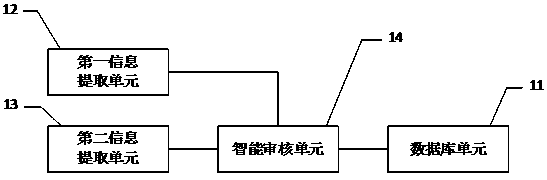
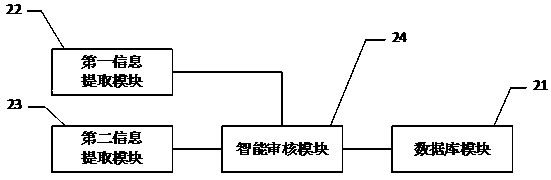
Method, system and equipment for intelligently auditing operation scheme
PendingCN111028915AAvoid unreasonable and non-compliant situationsEfficient managementMechanical/radiation/invasive therapiesMedical practises/guidelinesMedical institutionReoperative surgery
The invention discloses a method, a system and equipment for intelligently auditing an operation plan. The method comprises the following steps: establishing an operation plan database, extracting information of an operation plan and actual information of related elements of an operation performed by a patient, comparing the extracted information with related rules in the operation plan database,and analyzing the reasonability and compliance of the operation plan of the patient. The invention discloses a method, a system and equipment for intelligently auditing an operation scheme. The situation that an operation scheme is unreasonable and substandard due to insufficient professional skills of medical staff, individual differences of patients, human errors and the like can be avoided, a user is assisted in achieving effective management of the operation scheme, and the patient is helped to receive an operation safely, effectively, economically and properly; and a medical administrative department, a medical insurance management institution, a medical institution, an insurance company and a market / quality supervision and management department are helped to better manage the operation and payment.
Owner:曹庆恒
Best possible payment expected for healthcare services
InactiveUS20100070301A1Effectively effectivenessImprove performanceFinanceForecastingThird partyProgram planning
Owner:TOLAN MARY A +3
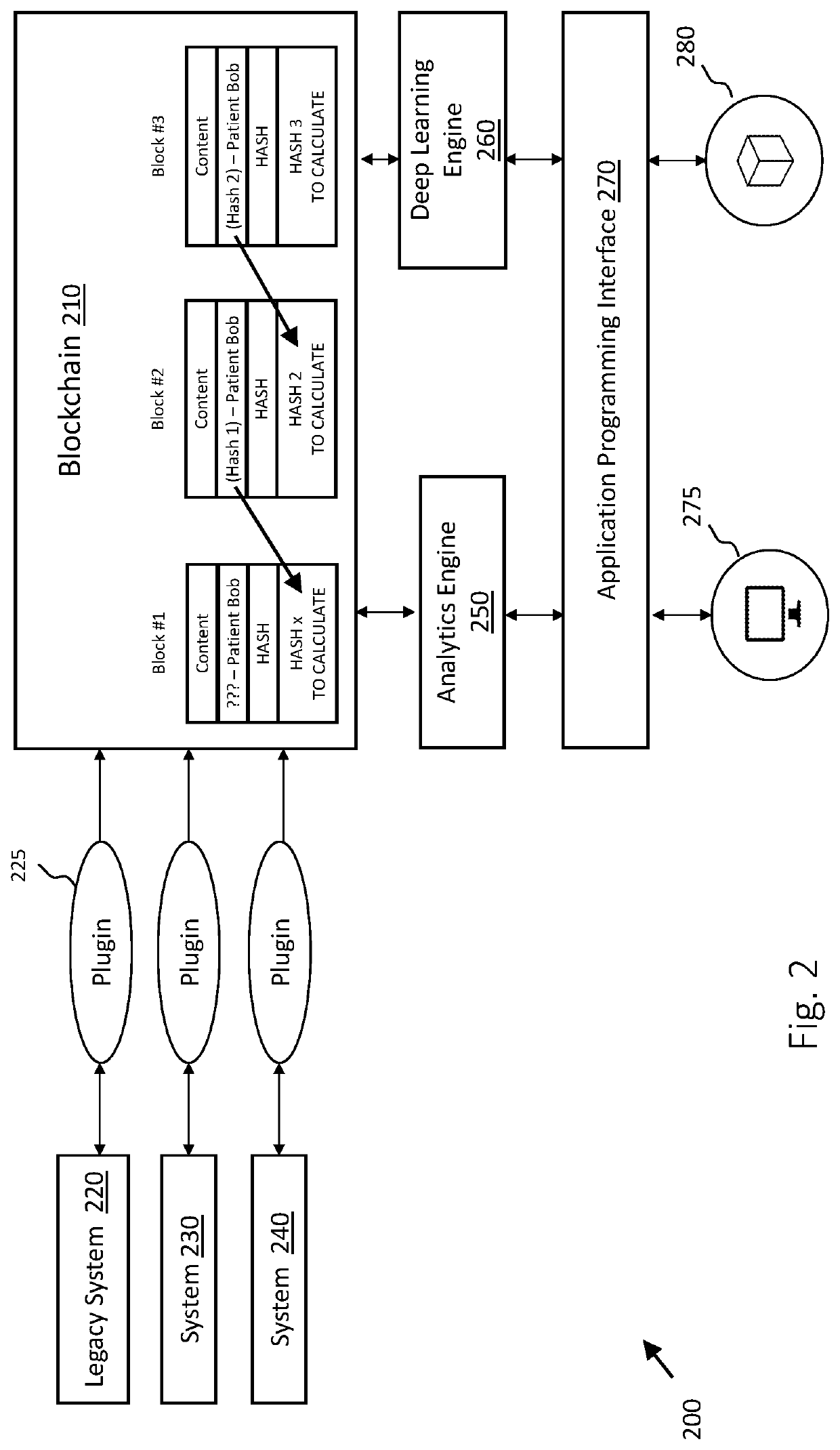
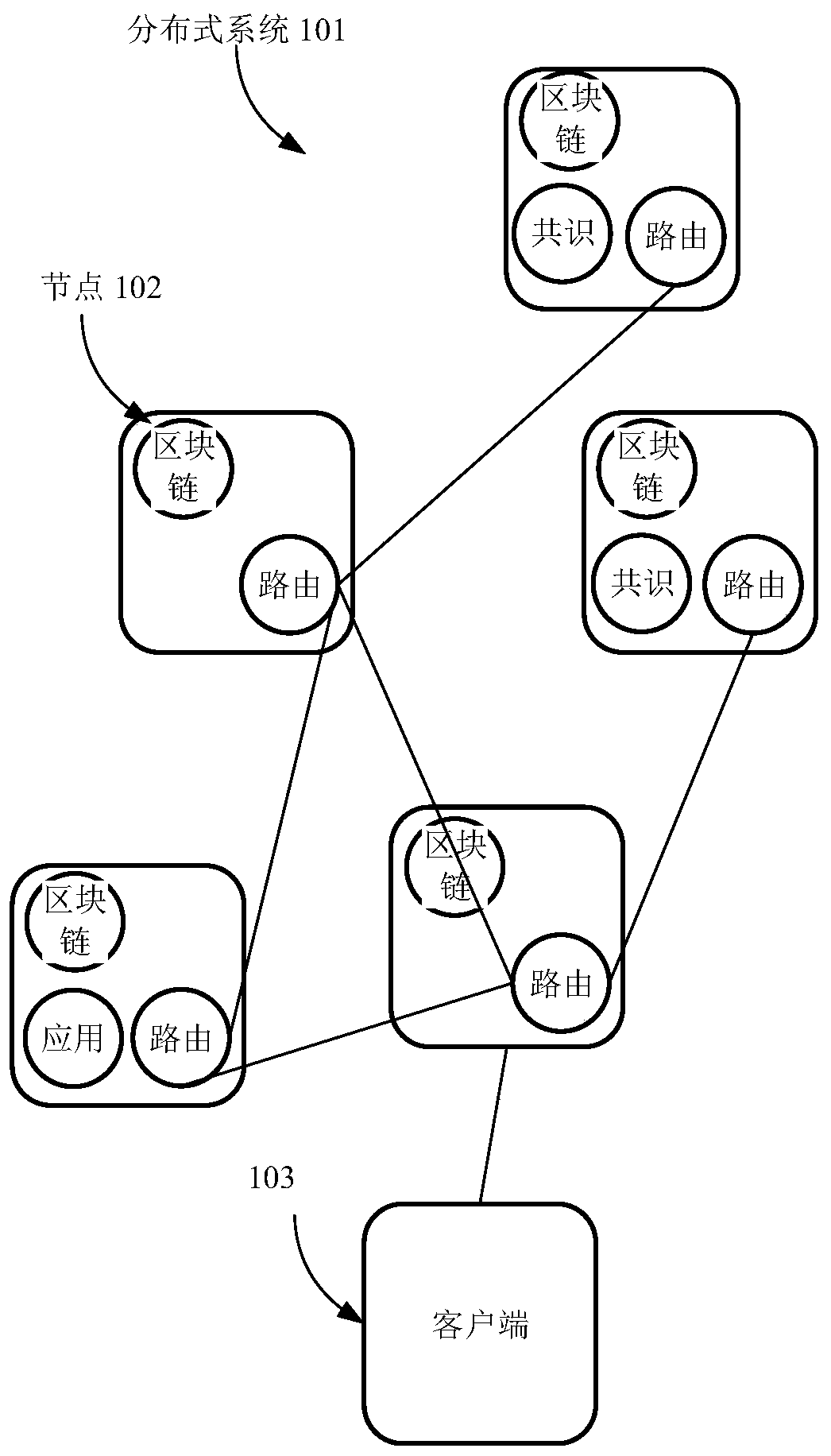
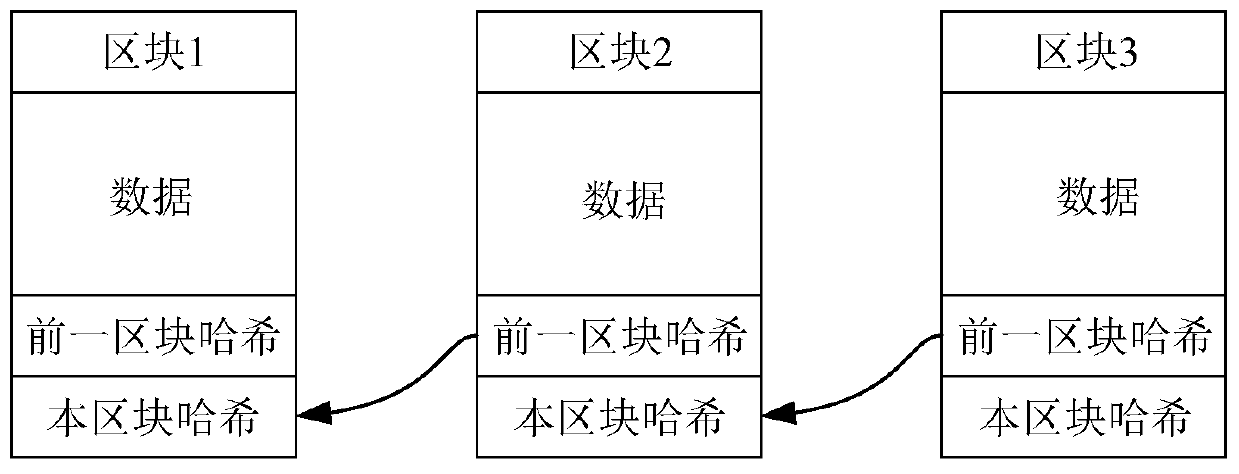
Medical insurance claim settlement processing method, device and system based on block chain and storage medium
PendingCN111507851AReduce verification timeImprove claims efficiencyFinanceDatabase distribution/replicationElectronic contractsInternet privacy
The invention relates to a medical insurance claim settlement processing method, device and system based on a block chain and a storage medium. The method comprises the following steps: receiving a first claim settlement verification request containing a first object identifier, wherein the first object identifier is used for identifying the first claim settlement object; obtaining a first insurance electronic contract corresponding to the first object identifier from a target blockchain account book; wherein the target blockchain account book is a blockchain account book shared with the insurance institution node; performing claim settlement verification on the first claim settlement object according to the first insurance electronic contract; and when the claim settlement verification ispassed, sending a first claim settlement request to the insurance institution node, so that the insurance institution node allocates a corresponding claim settlement fund according to the first claimsettlement request. According to the scheme, the medical institution node can automatically complete the treatment of the claim settlement object, thereby effectively reducing the verification time of the medical insurance, and improving the claim settlement efficiency of the medical insurance.
Owner:TENCENT TECH (SHENZHEN) CO LTD
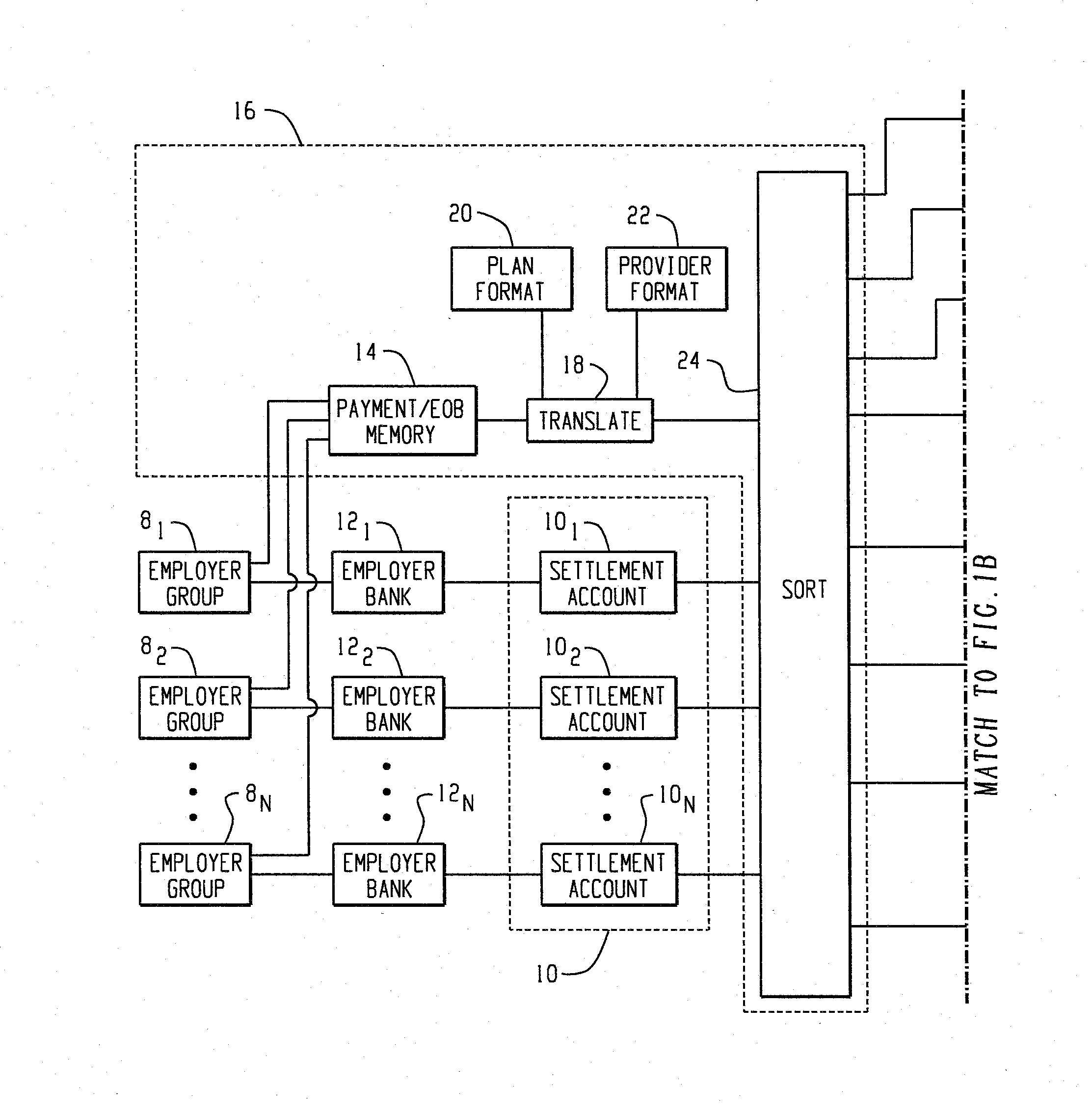
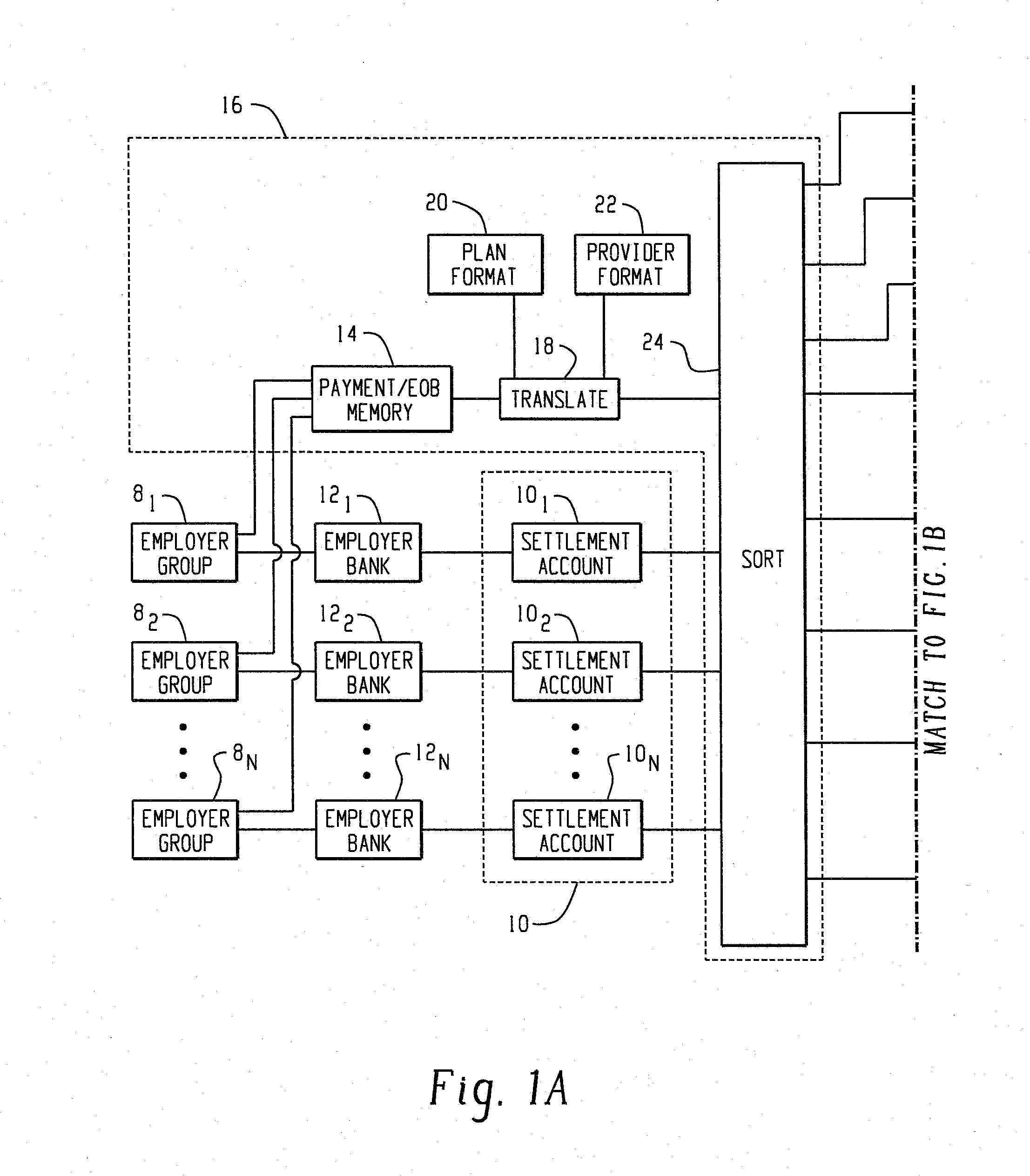
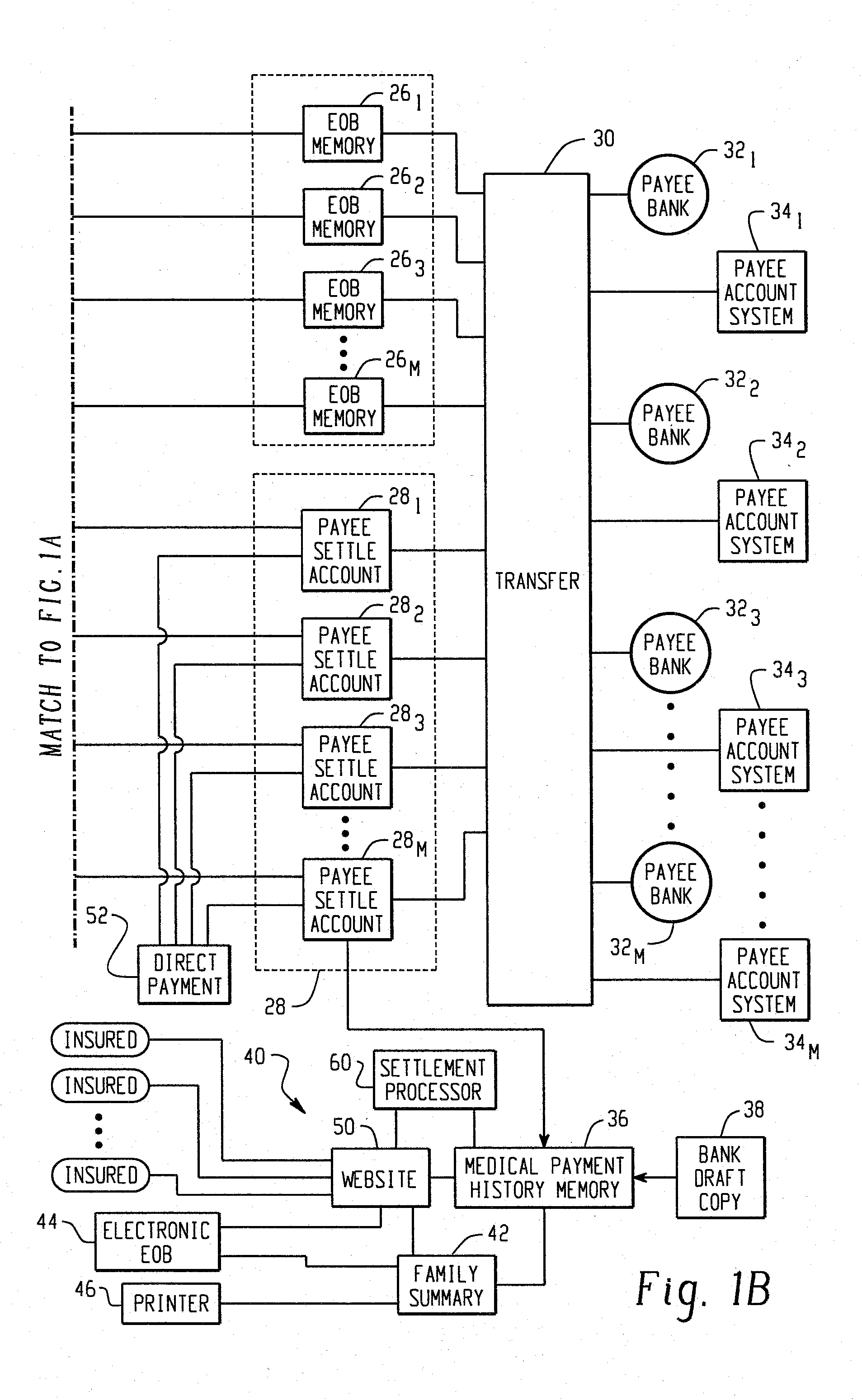
Medical claims payment system with payment consolidation from multiple employer accounts
InactiveUS20140088999A1Reduce in quantityReduce processFinancePayment architectureComputer sciencePayment system
Segregated employer group settlement accounts (101, 102, . . . , 10N) receive payments for medical insurance claims and an explanation of benefits (EOB) memory (14) receives an explanation of the medical services of multiple medical service providers against which parts of the payment are to be applied and explanations of amounts due by individual patients. An electronic sorting and transfer processor (16) in accordance with the explanations of benefits, electronically transfers funds from each of the employer group settlement accounts into each of a plurality of medical service provider settlement accounts (261, 262, . . . 26M) without co-mingling funds. The funds from the service provider settlement accounts are transferred (30) to each medical service provider's banking institution (32) concurrently with an electronic transfer of the corresponding EOBs to the medical service provider's accounting system (34).
Owner:ELECTRONICS COMMERCE FOR HEALTHCARE ORG
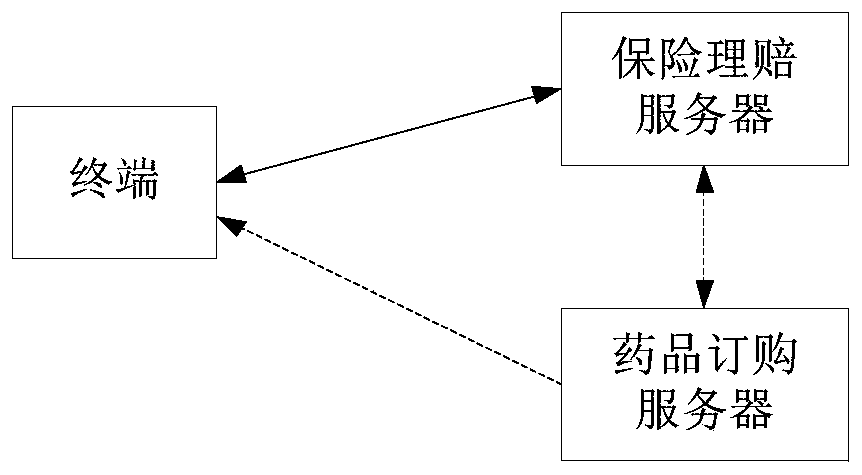
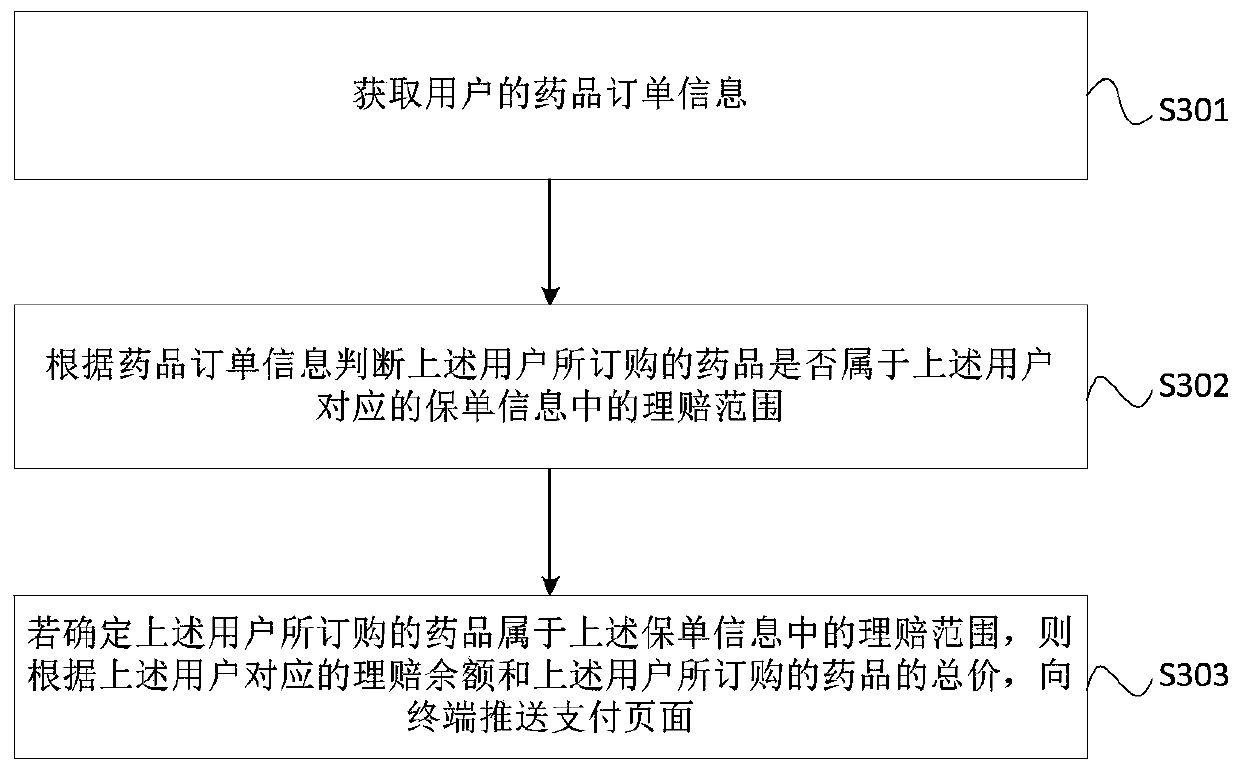
Medical insurance claim settlement method, device and equipment and storage medium
The invention provides a medical insurance claim settlement method, device and equipment and a storage medium. The method comprises the steps: obtaining the drug order information of a user, and judging whether a drug ordered by the user belongs to a claim settlement range in insurance policy information corresponding to the user or not according to the drug order information; further, if it is determined that the medicine ordered by the user belongs to the claim settlement range in the insurance policy information; If yes, pushing a payment page to the terminal according to the claim settlement balance corresponding to the user and the total price of the medicine ordered by the user, so that the user can know the claim settlement amount and the payment amount needing to be paid by the user through the payment page. Visibly, according to the embodiment of the invention, the online real-time claim settlement of the medical insurance is completed by the user in the process of purchasingthe medicine, and the claim settlement procedure is simple, so that the claim settlement efficiency of the medical insurance is improved.
Owner:TAIKANG LIFE INSURANCE CO LTD +1
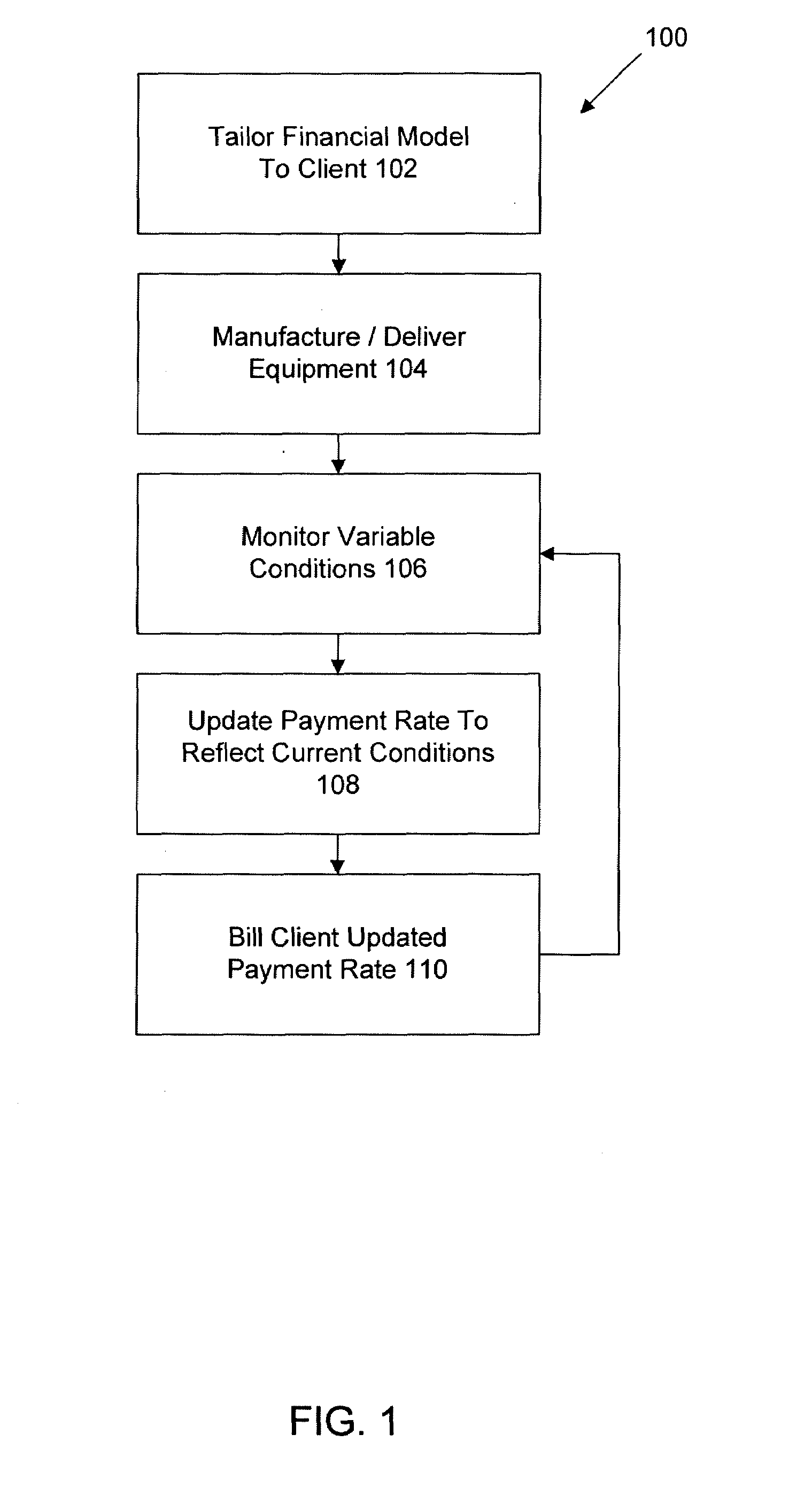
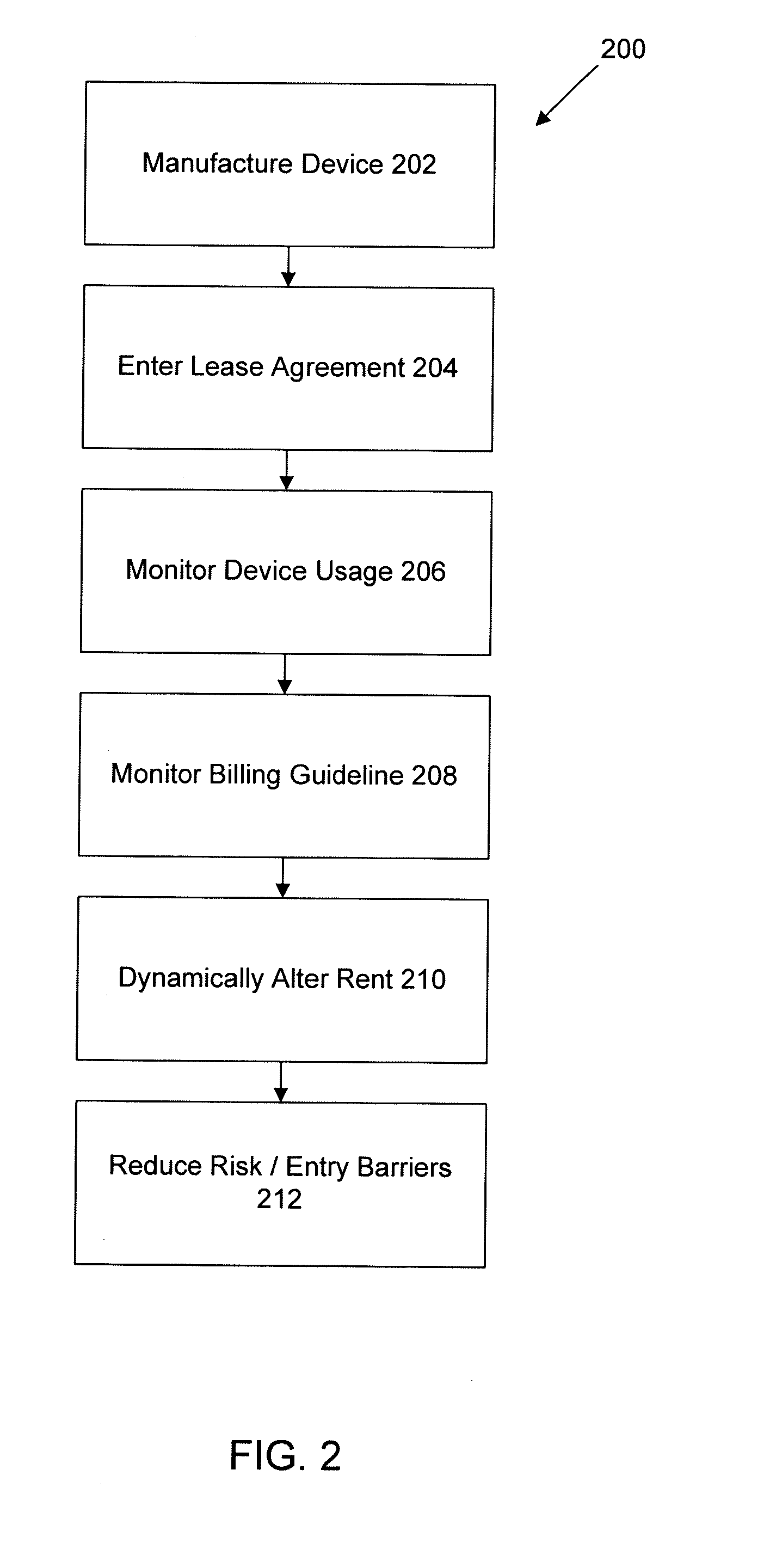
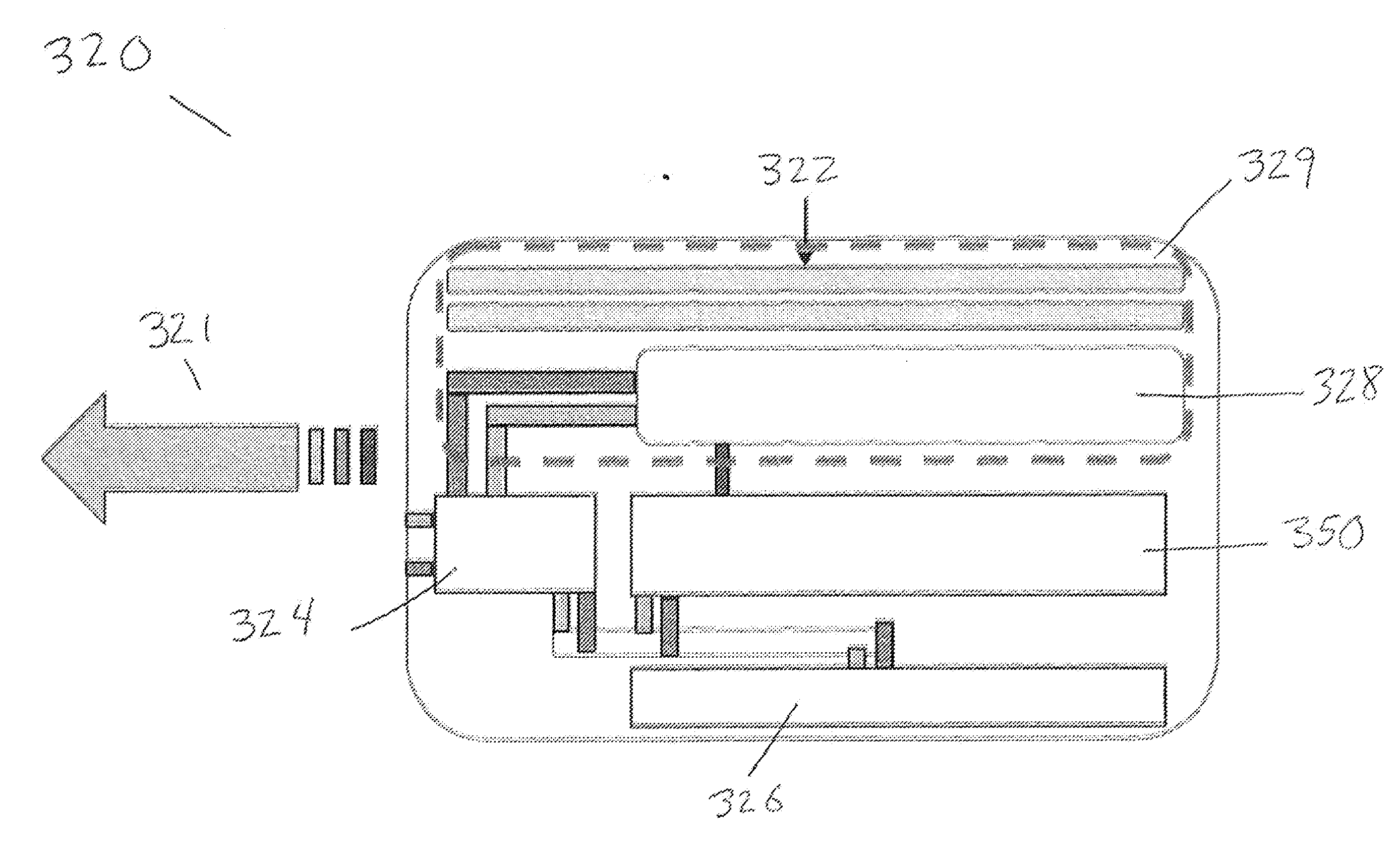
Business model of a billing procedure for renting medical equipment
InactiveUS20090094144A1Reduce financial riskReduce significant barrierComplete banking machinesFinancePaymentMedical equipment
A system and method relate to dynamic financial models associated with financing, such as leasing or purchasing, equipment and / or services. The financial models may dynamically update a rate of payment based upon variable conditions. In one aspect, the financial models facilitate the lease of medical equipment. A rental rate for a piece of medical equipment being leased may be adjusted to account for changing conditions. The rental rate may be updated as a function of fluctuating health care insurance re-imbursement rates, fluctuating billing or other medical guidelines, the number and / or type of procedures being performed with medical equipment being leased, interest rates, and / or other factors. The dynamic calculation of the rental rate to reflect actual conditions may reduce financial risk posed to a medical practitioner or facility. Accordingly, a significant barrier of entering a highly specialized market associated with medical equipment and the medical services provided thereby may be alleviated.
Owner:SIEMENS AG
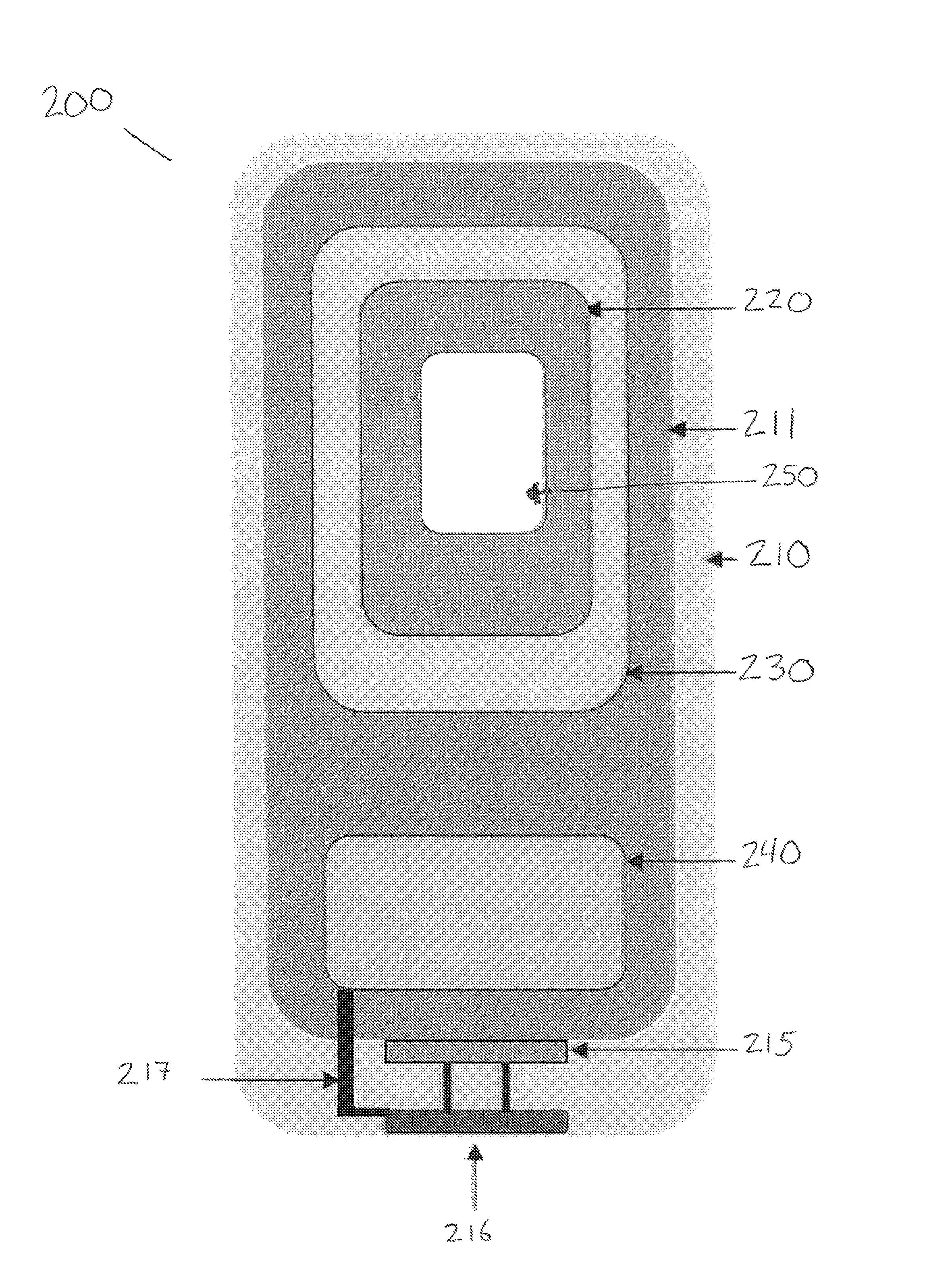
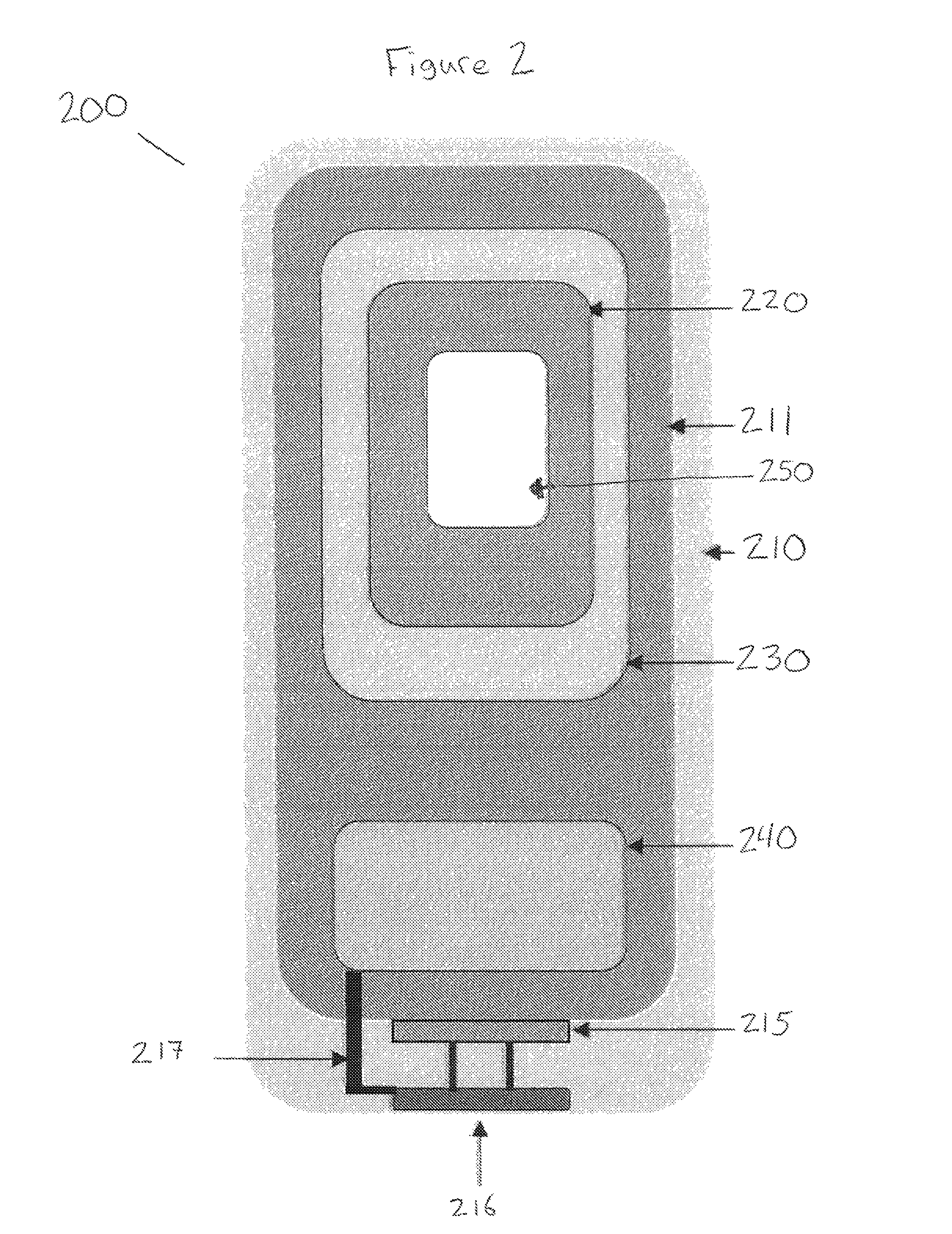
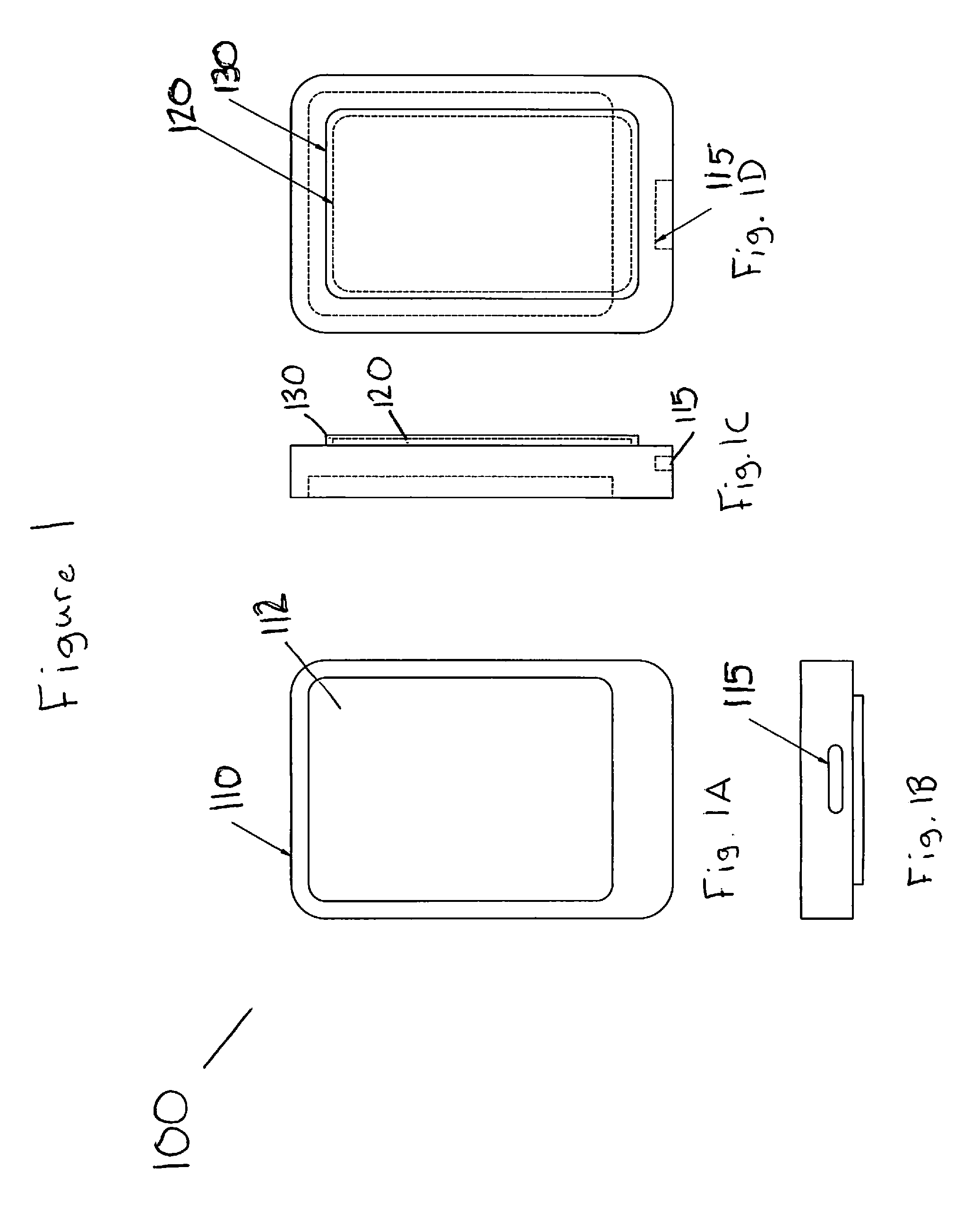
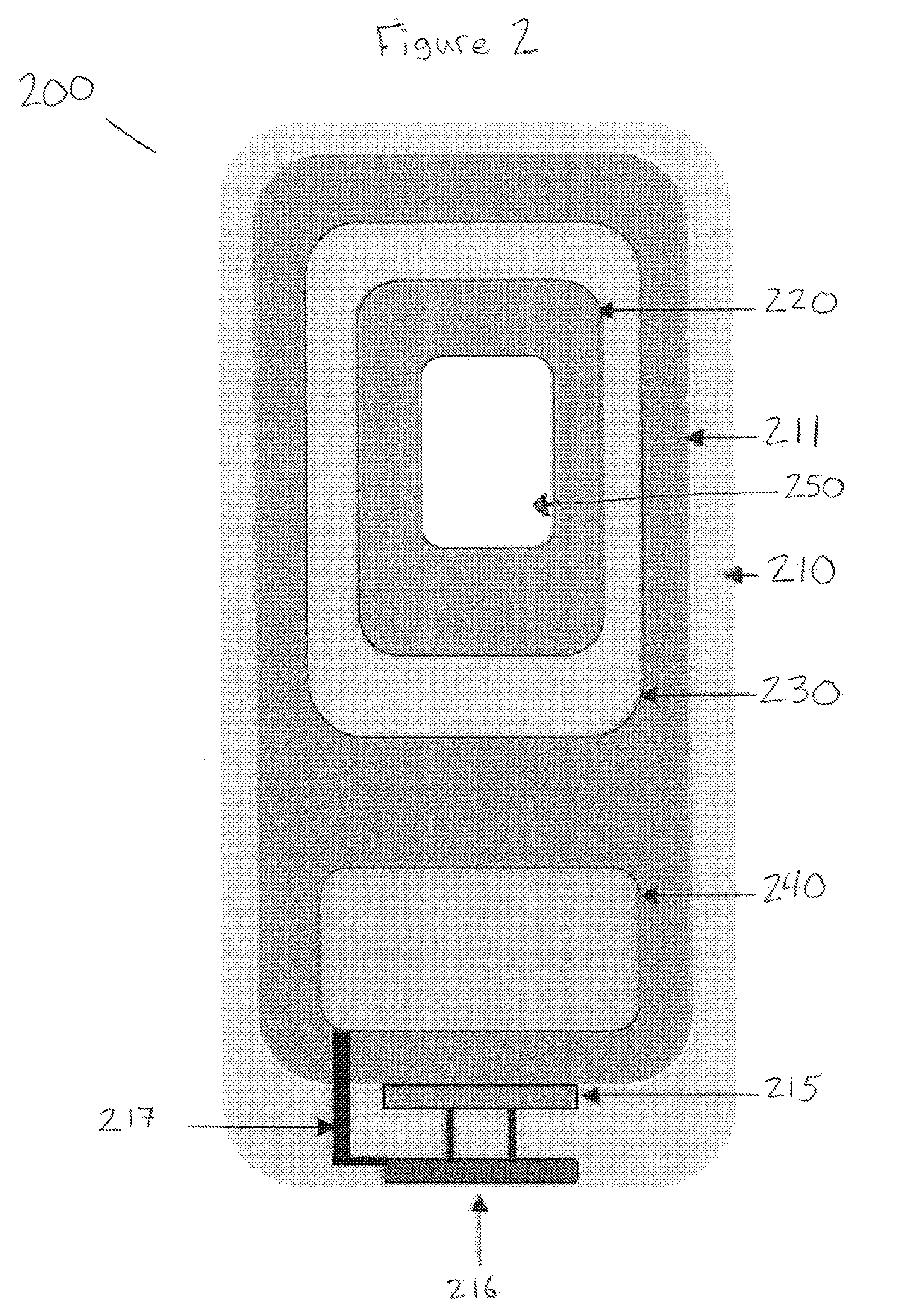
Smart phone casing and information exchange system
InactiveUS20140367467A1Devices with card reading facilitySensing record carriersPersonalizationDigital protection
The embodiments of the present invention relate to a smart phone casing and information exchange system which enables a user to carry a single system that merges the digital and telecommunications necessities of the individual with the personalized cards, membership accounts, consumer credit and / or medical insurance or health information in a single source protected both physically with a hardened case, and digitally with appropriate safeguards for electronic protection.
Owner:MELBROD ANASTASIA +1
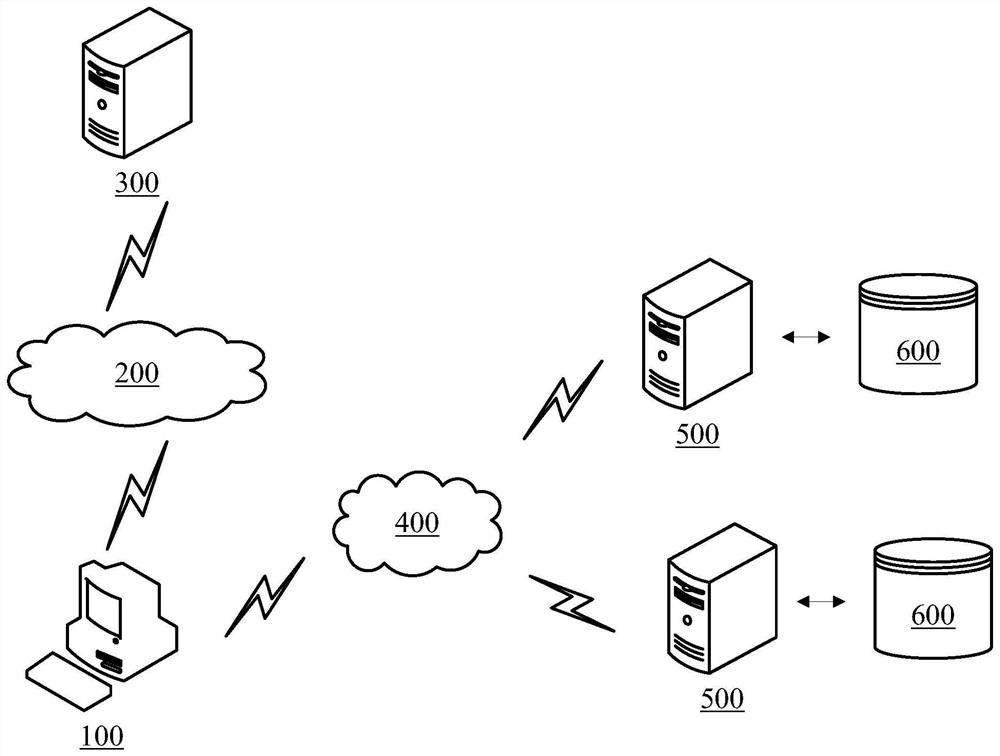
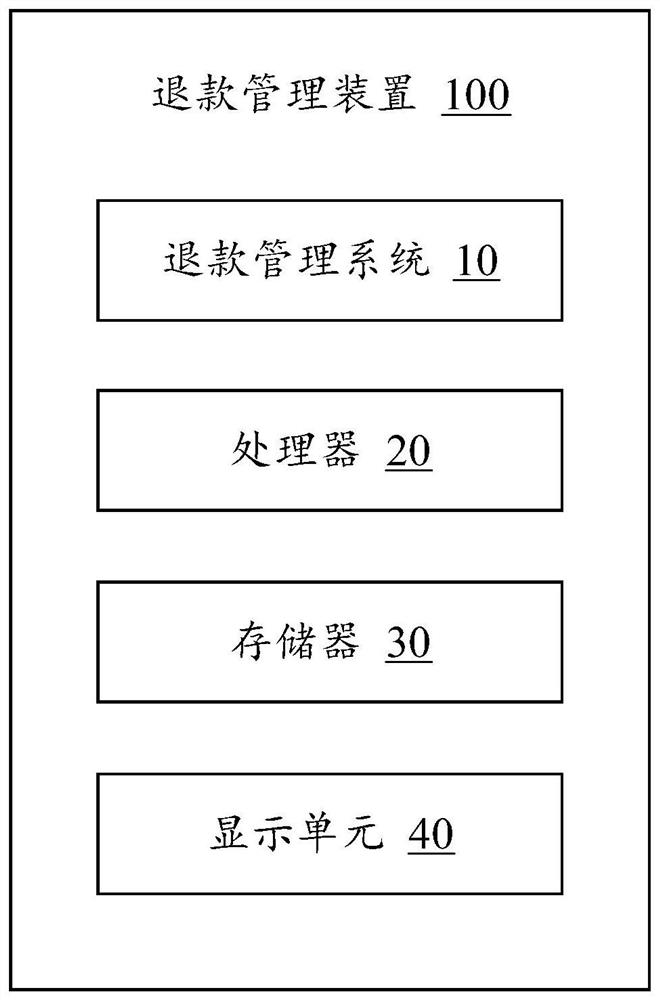
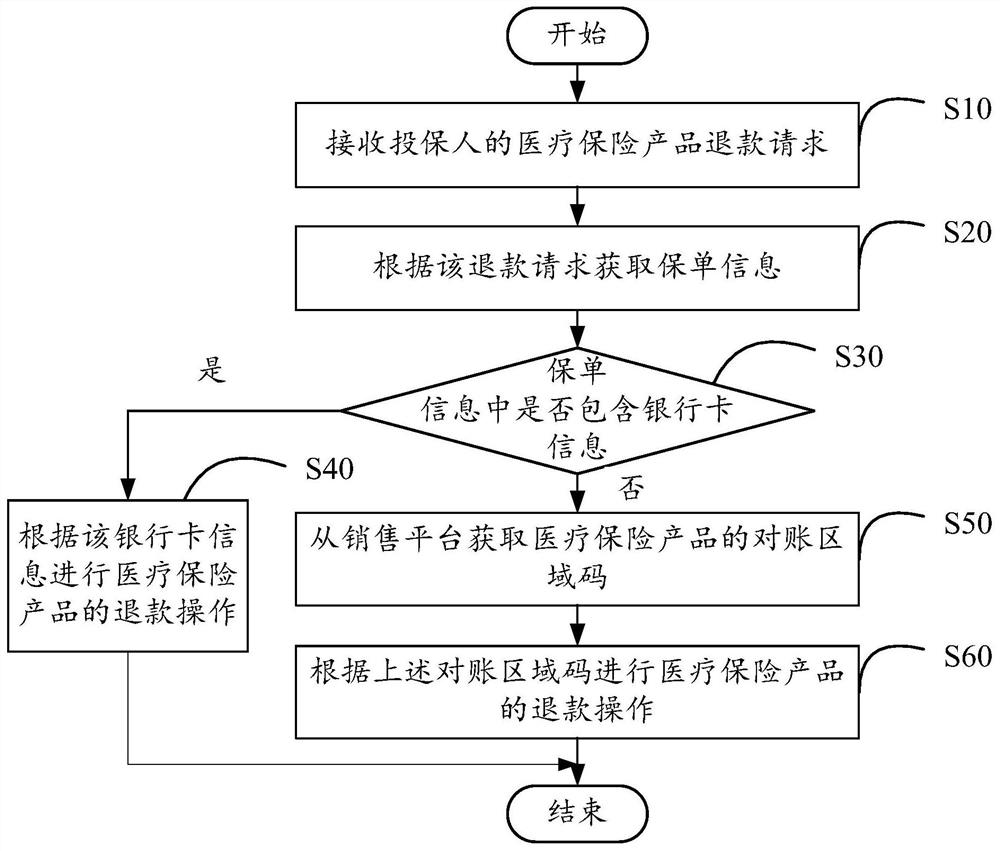
Refund management method, device and storage medium
The present invention provides a refund management method, which is applied to a refund management device, and the refund management device communicates with an external server and an internal server. The method includes the following steps: receiving a medical insurance product refund request sent by a sales platform , the sales platform runs on an external server or an internal server; according to the refund request, the policy information is obtained from the core system of the internal server; when the policy information does not contain bank card information, the sales platform or the core The system obtains the reconciliation area code of the medical insurance product; and obtains the account information of the corresponding third-party payment platform from the financial system of the internal server according to the above reconciliation area code, and controls the financial system to return the refund amount to the third-party payment platform in the account. The invention also provides a refund management device and a computer-readable storage medium.
Owner:CHINA PING AN LIFE INSURANCE CO LTD
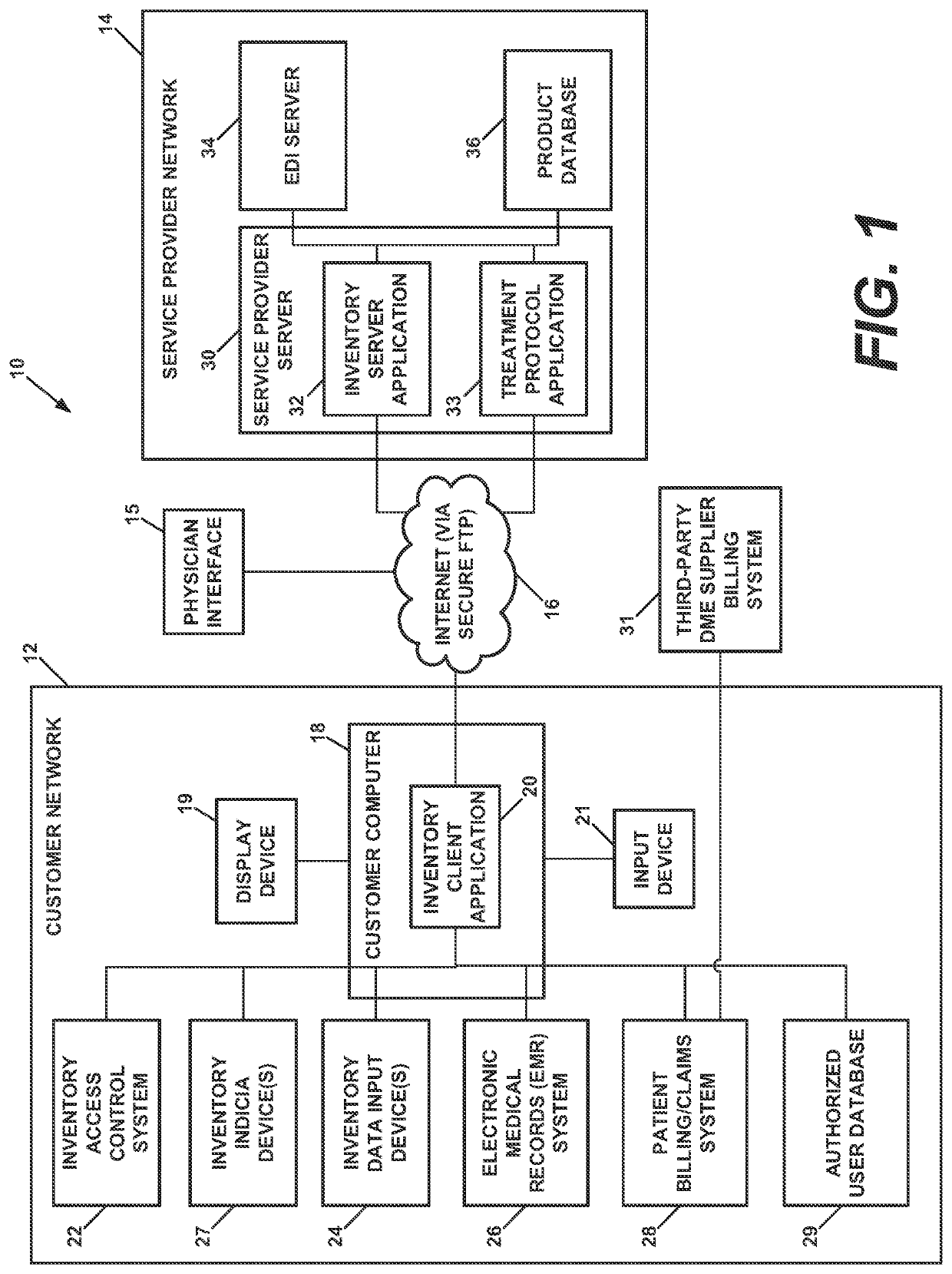
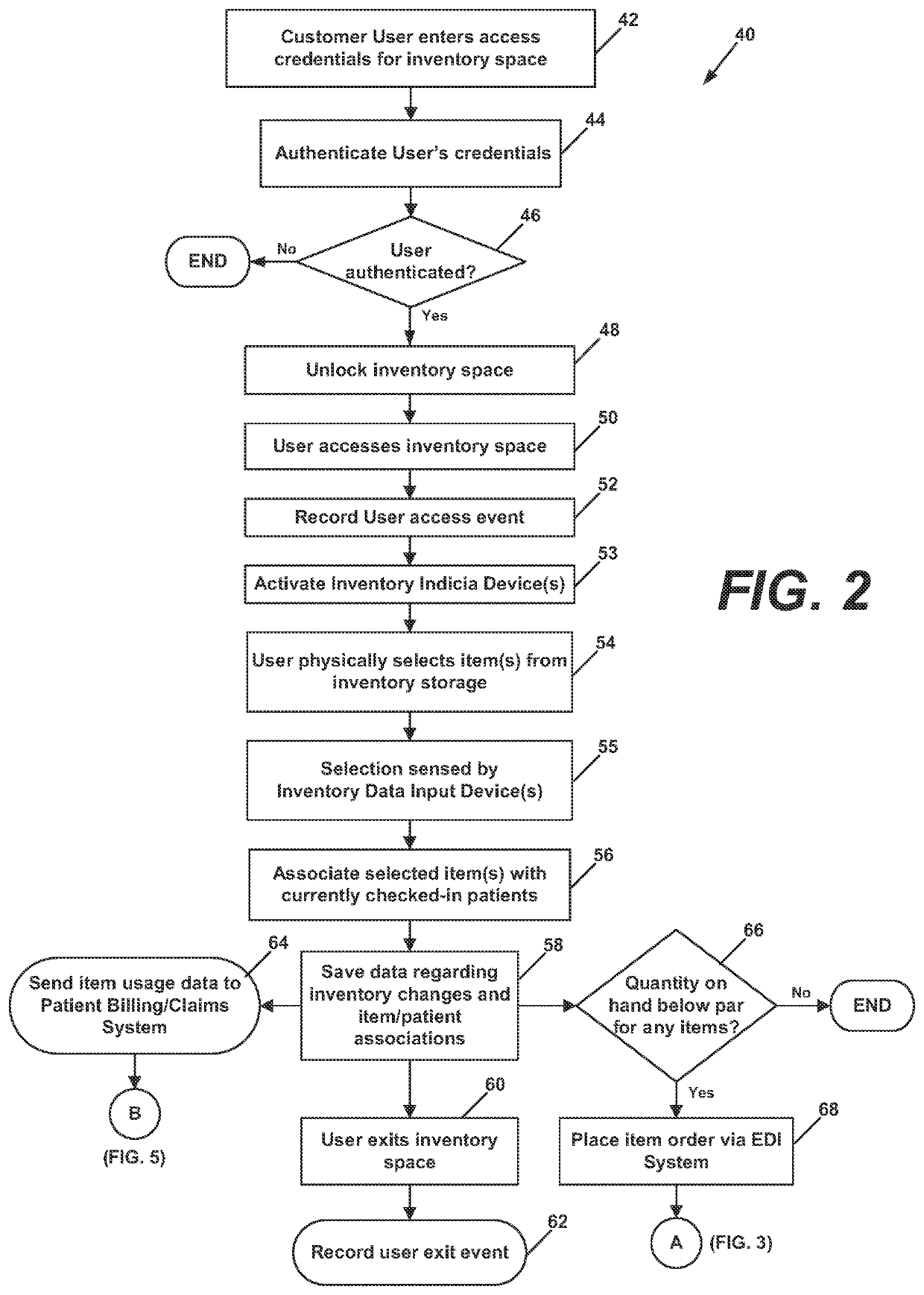
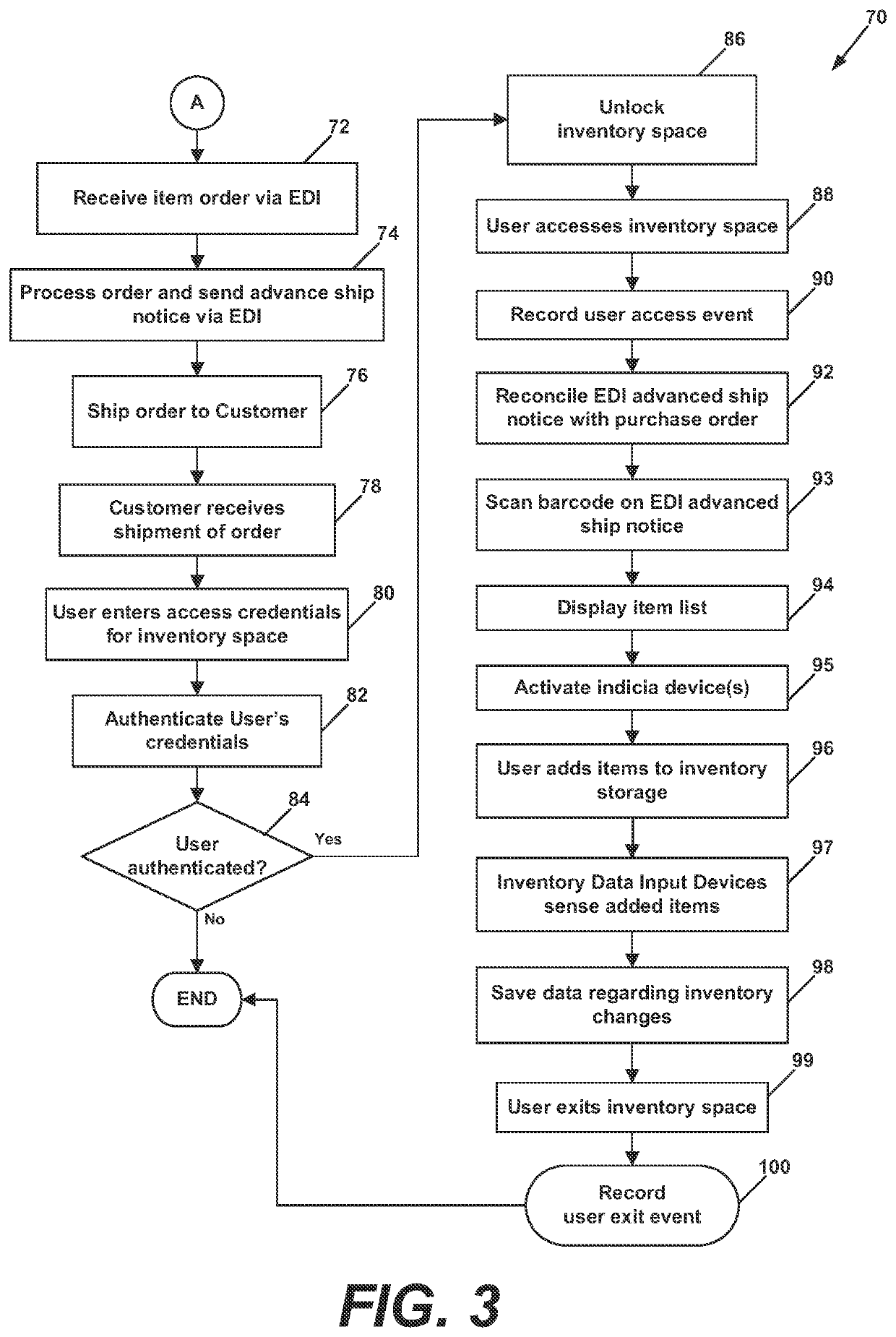
Automated system for medical item dispensing, billing, and inventory management
An inventory management system manages information regarding medical items dispensed to a patient in a medical facility. Inventory sensors sense removal of medical items from an inventory space to be dispensed to the patient. Software instructions associate item information with patient information that identifies the patient, determine billing codes associated with the dispensed items, generate billing information including the patient information and the billing codes, and generate an invoice directed to the patient's medical insurance provider. The instructions also verify that the billing codes are associated with medical items appropriate for treatment of the patient's condition indicated by diagnostic codes included in the billing information, and generate an alert message if the billing codes are associated with medical items that are not reimbursable or are inappropriate for treatment of the diagnosed condition. The alert message is sent to the physician who diagnosed the patient and provided the diagnostic code.
Owner:DEROYAL INDUSTRIES INC
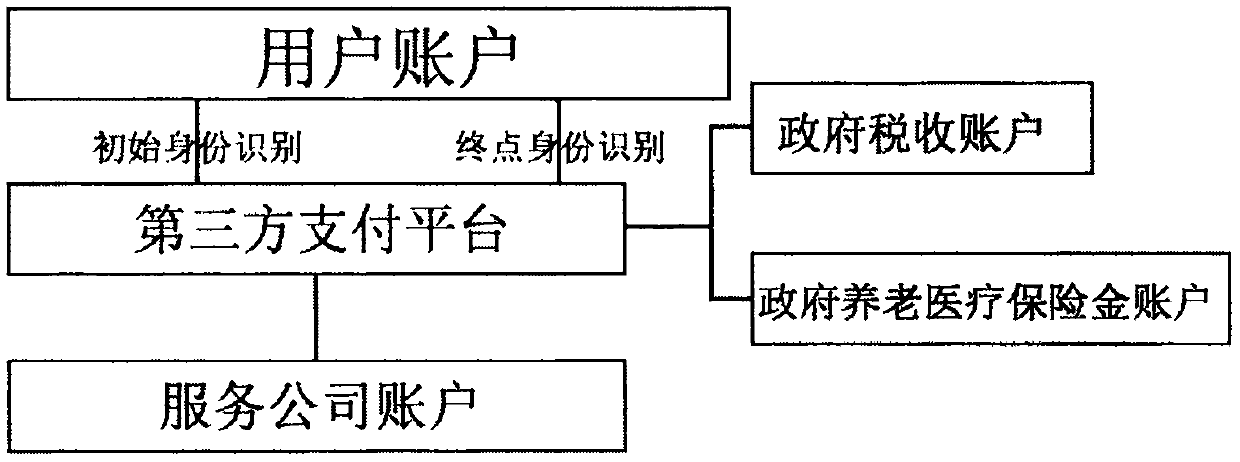
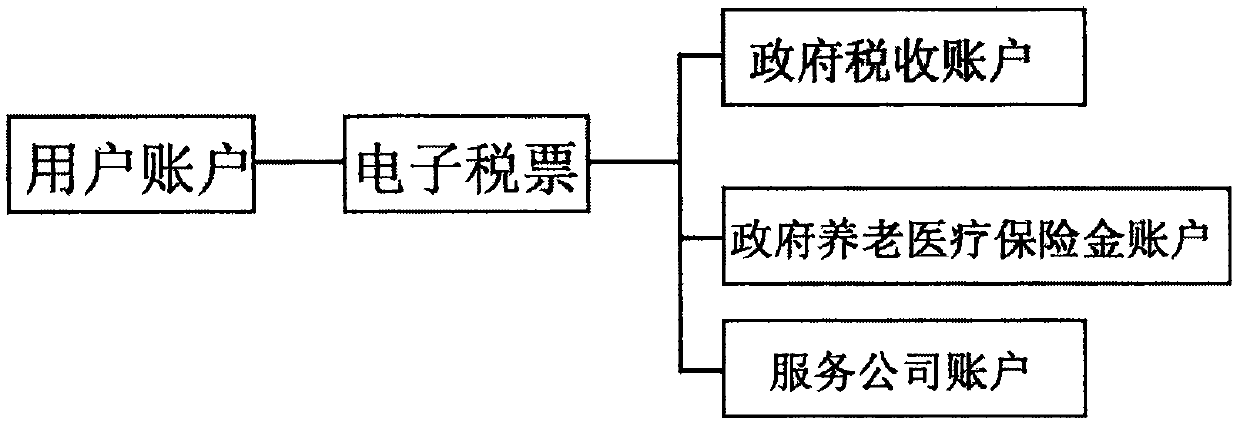
Tax withholding system for confirming payment according to secondary identity authentication and identification of tax payment identification code
The invention discloses a tax withholding and paying system for confirming payment according to secondary identity identification of a tax payment identification code. The system comprises a third-party payment platform, a bank account, user main bodies registered by using the tax payment identification code, a government tax institution account and a government pension medical insurance account.Secondary identification confirmation charging refers to high-speed charging, bus and subway charging, parking lot charging and the like which need to judge the amount and confirm the identity according to the distance or duration. The identity confirmation needs to bind a license plate according to the tax payment identification code, or a fingerprint or a face of a user, identity recognition hardware is scanned twice through an initial terminal and an end terminal to confirm that payment should be carried out, and the third-party payment platform withdraws tax fee for payment according to the tax recognition code and transfers the tax fee to a related charging company account, a government tax institution account and a government pension medical insurance fund account.
Owner:周维平
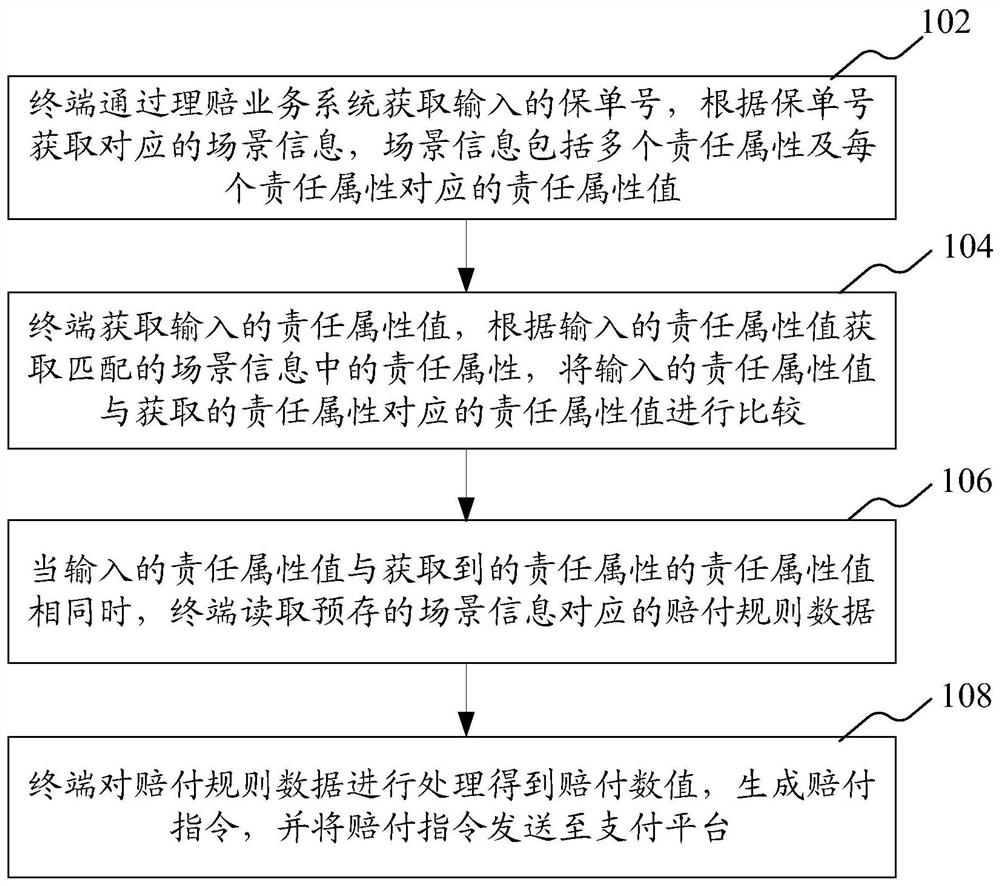
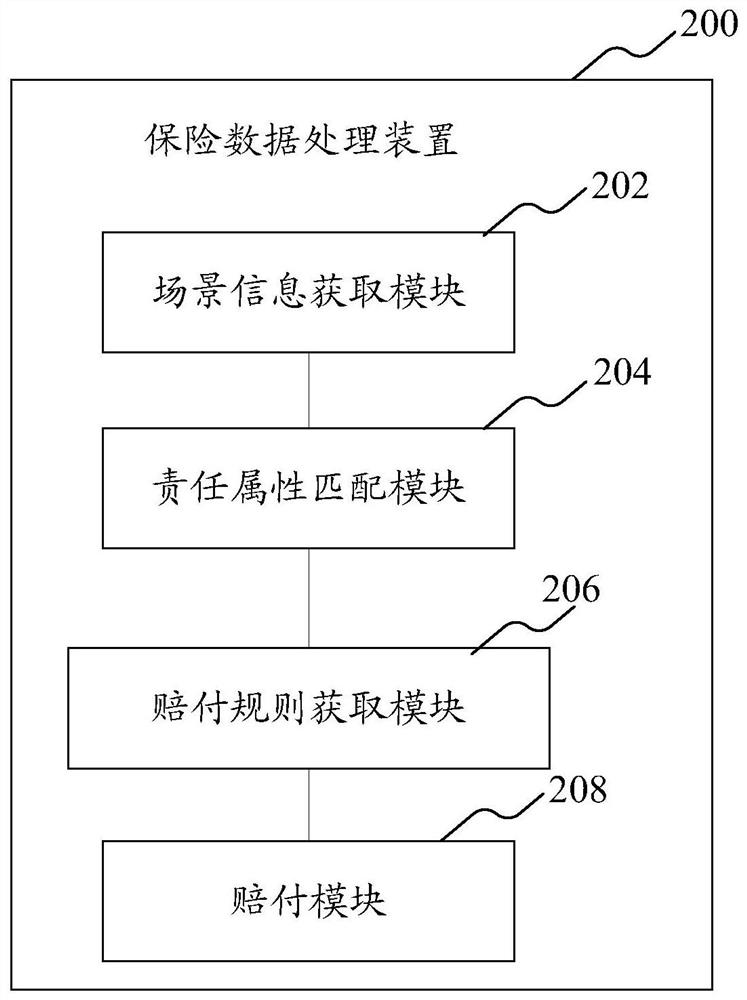
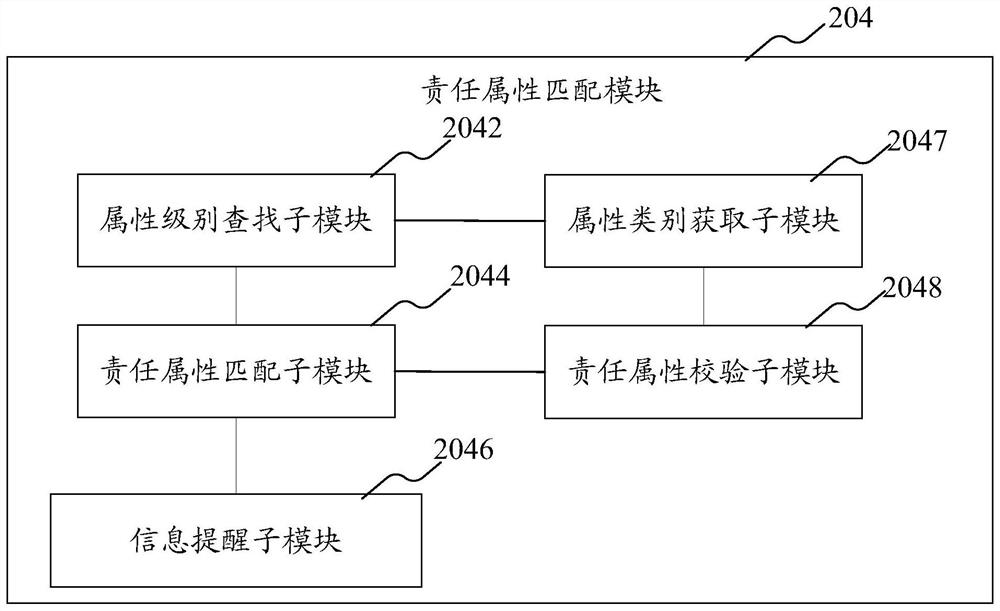
Insurance data processing method and device
ActiveCN108510141BRealize automatic claims settlementImprove claims efficiencyFinancePayment architectureEngineeringData mining
Disclosed is an insurance data processing method, comprising: a terminal acquiring an input insurance policy number, and acquiring corresponding scene information according to the insurance policy number, wherein the scene information comprises multiple responsibility attributes, and responsibility attribute values corresponding to each of the responsibility attributes; the terminal acquiring an input responsibility attribute value, and acquiring, according to the input responsibility attribute value, a responsibility attribute in matched scene information, and comparing the input responsibility attribute value with the responsibility attribute value corresponding to the acquired responsibility attribute; when the input responsibility attribute value is identical to the responsibility attribute value of the acquired responsibility attribute, reading pre-stored compensation rule data corresponding to the scene information; and processing the compensation rule data to obtain a compensation numeric value, generating a compensation instruction, and sending the compensation instruction to a payment platform.
Owner:PING AN TECH (SHENZHEN) CO LTD
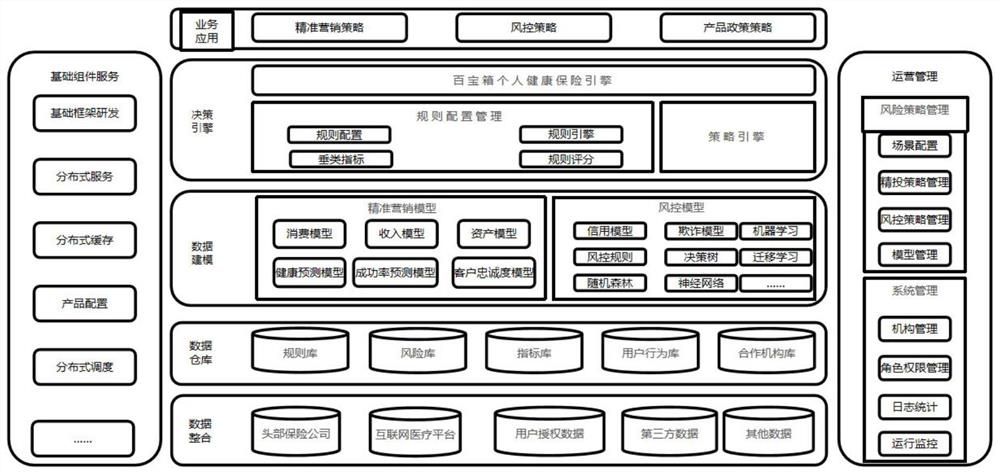
Personal medical insurance precision marketing and risk control method
The invention discloses a personal medical insurance precision marketing and risk control method, and the method comprises the following specific steps: carrying out the analysis of a plurality of factors of Internet medical customers, building a big data risk control model, classifying the customers, calculating the personal medical activities through the big data risk control model, and determining the additional insurance amount of common medical treatment. According to the method, corresponding price preferential strategies are made for clients with different grades, it is ensured that large-area loss does not occur to businesses, and finally, a white list system is opened by utilizing the technical advantages of the three parties, and customized personal health insurance services are provided for the clients needing the businesses; internet medical institution data is fully utilized, a big data precision marketing model is established, compliance third-party data is connected, an anti-fraud and risk control model is established, and the potential risk of personal health insurance is controlled.
Owner:上海百保箱网络科技有限公司 +1
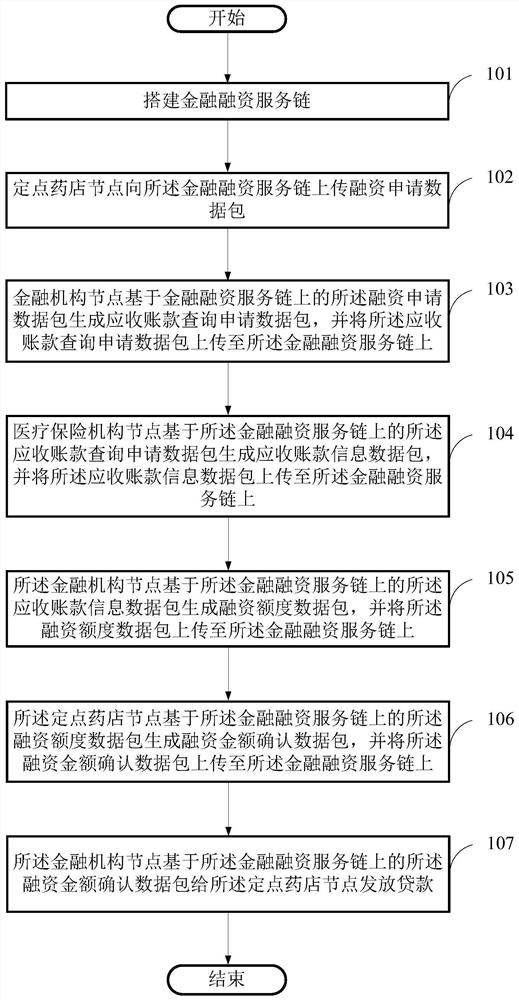
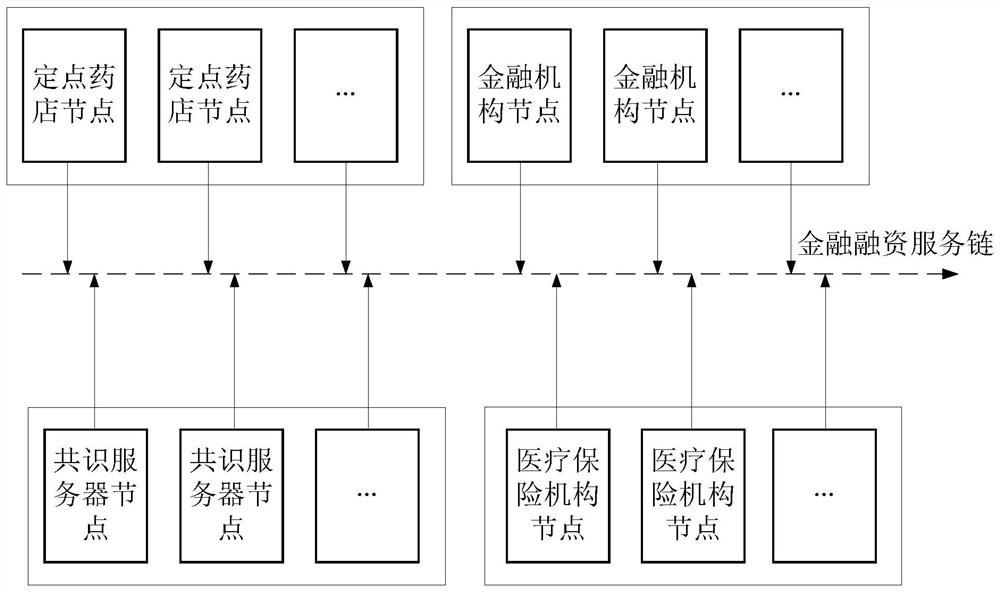
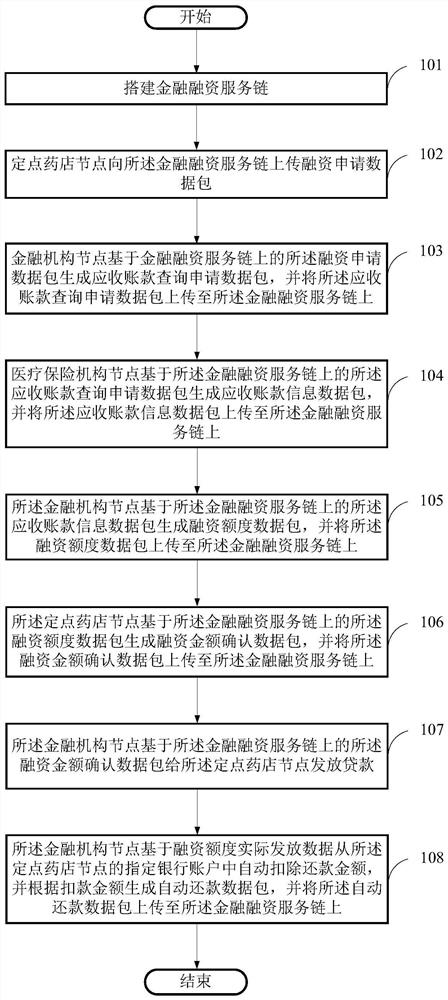
Blockchain-based fixed-point pharmacy financing method, storage medium and computer equipment
The invention provides a fixed-point pharmacy financing method based on a block chain, a storage medium and a computer device. The method comprises: buidling a financial financing service chain; The fixed-point pharmacy node uploads a financing application data packet to the financial financing service chain; The financial institution node generates an account receivable query application data packet based on the financing application data packet on the financial financing service chain; The medical insurance institution node generates an account receivable information data packet based on theaccount receivable query application data packet on the financial financing service chain; The financial institution node generates a financing limit data packet based on the account receivable information data packet on the financial financing service chain; The fixed-point pharmacy node generates a financing amount confirmation data packet based on the financing amount data packet on the financial financing service chain; And the financial institution node issues a loan to the fixed-point pharmacy node based on the financing amount confirmation data packet on the financial financing servicechain. The problems that an existing financing system is prolonged in service process, not transparent and low in safety and processing efficiency are solved.
Owner:易保互联医疗信息科技(北京)有限公司
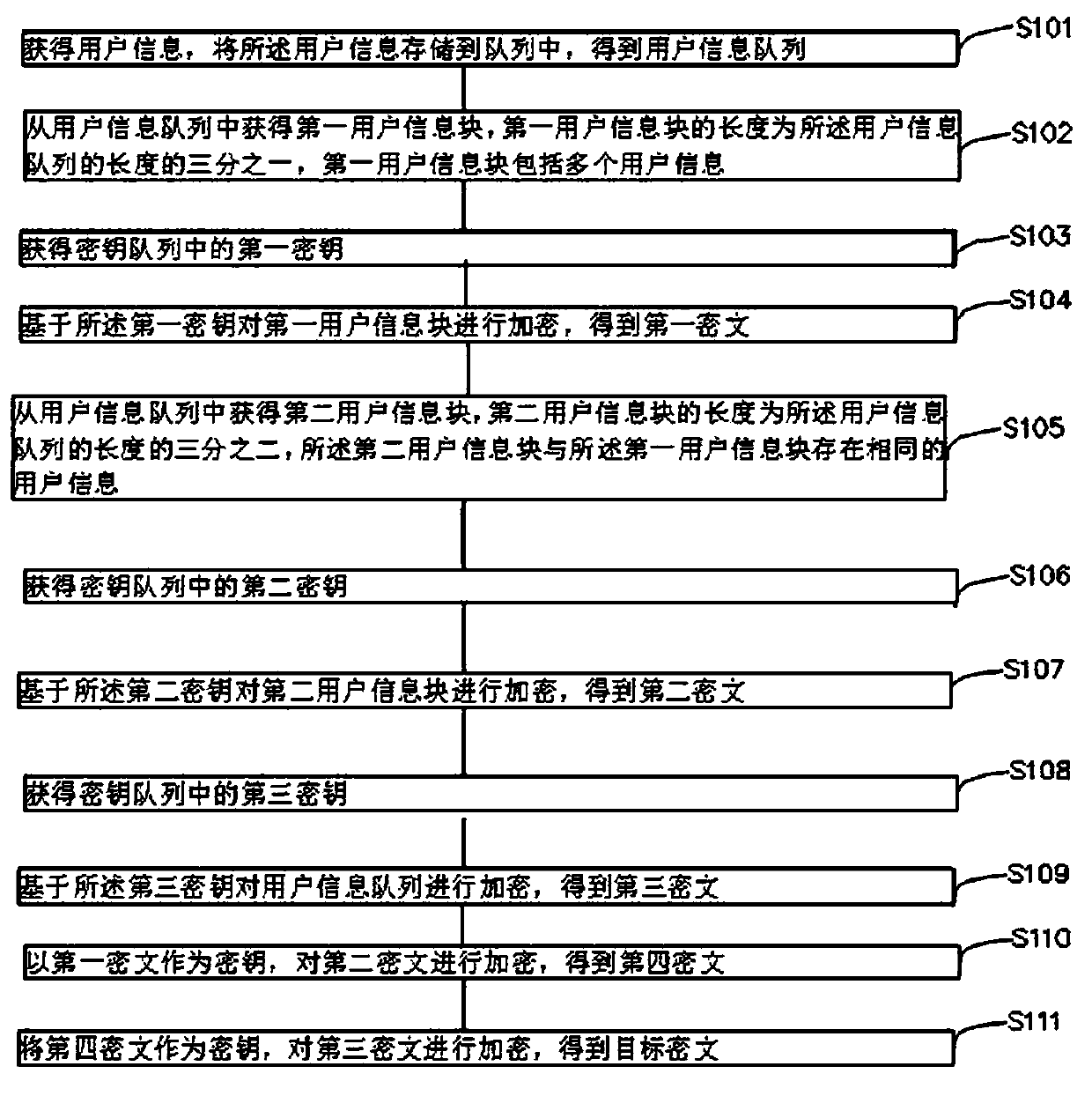
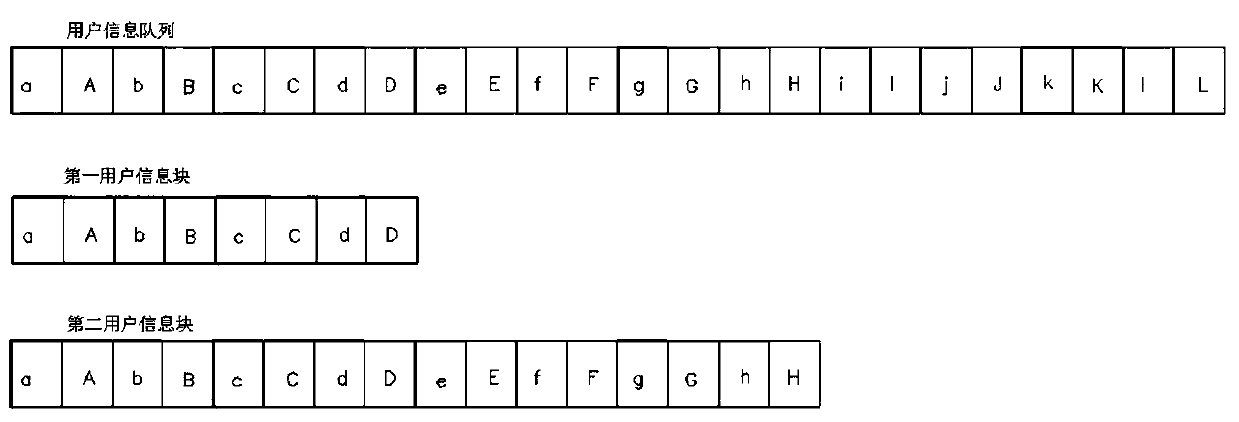
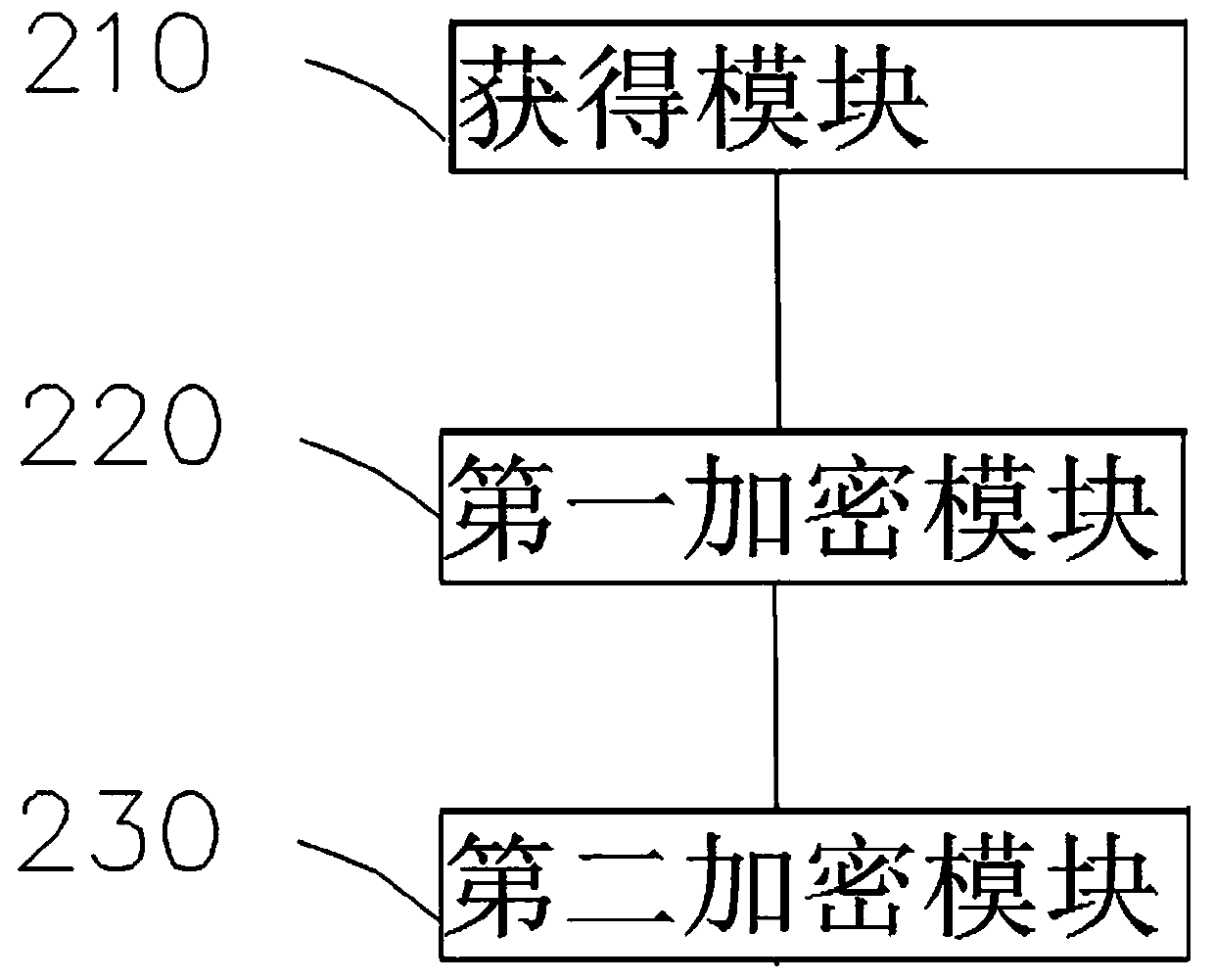
Medical insurance financial user information encryption method and system based on big data
ActiveCN111368323AEncryption improvedPromote reductionInterprogram communicationDigital data protectionCiphertextEngineering
The embodiment of the invention provides a medical insurance financial user information encryption method and system based on big data. According to the method, the first number of characters in the first character string are sequentially stored in the queue, and then the second number of characters in the second character string are stored in the queue, so that the user name and the user passwordcan be restored from the user information queue more easily. According to the method, the characters in the first character string are randomly stored in the queue, so that the encryption of the userinformation is improved, the target ciphertext is not easy to crack, and the security of the user information is improved.
Owner:上海竞动科技有限公司
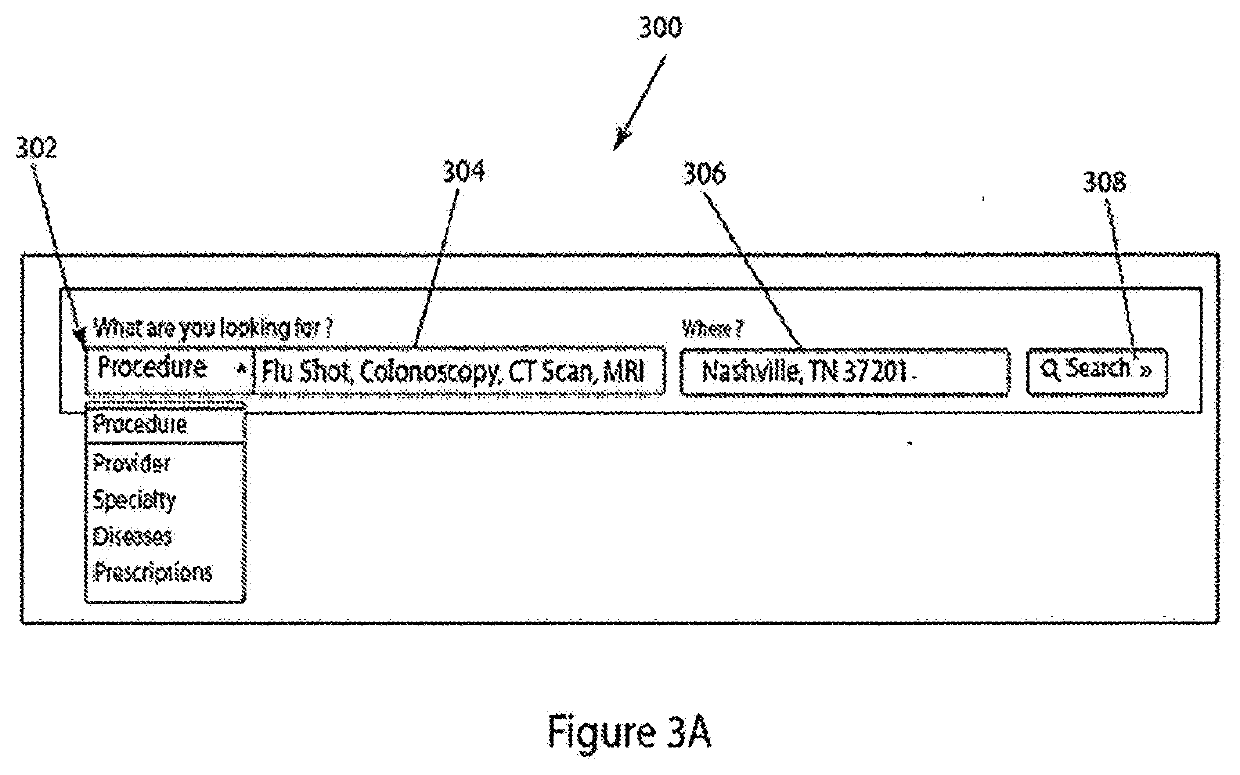
Network-based marketplace service pricing tool for facilitating purchases of bundled services and products
Apparatus and associated methods relate to generating a purchase data record, selectively redeemable by a user to receive a pre-paid healthcare service, in response to receiving payment at a price based on the service location, and applying the pre-paid amount to the user's health insurance deductible. The payment may be a virtual funds or actual currency payment. The service may be specified based on physician, facility, location, and time, permitting price adjustment based on geographical cost variance. Some implementations may provide a marketplace system configured to permit creation, transfer, redemption, and exchange of virtual funds for pre-paid services and actual currency. The user may receive the prepaid service, based on redeeming the voucher. Various implementations may exchange healthcare bundles, including service and drugs, for a price discounted based on the bundle. A healthcare bundle may be presented in shopping cart format, permitting the user to pre-pay for a customized bundle.
Owner:MDSAVE SHARED SERVICES INC
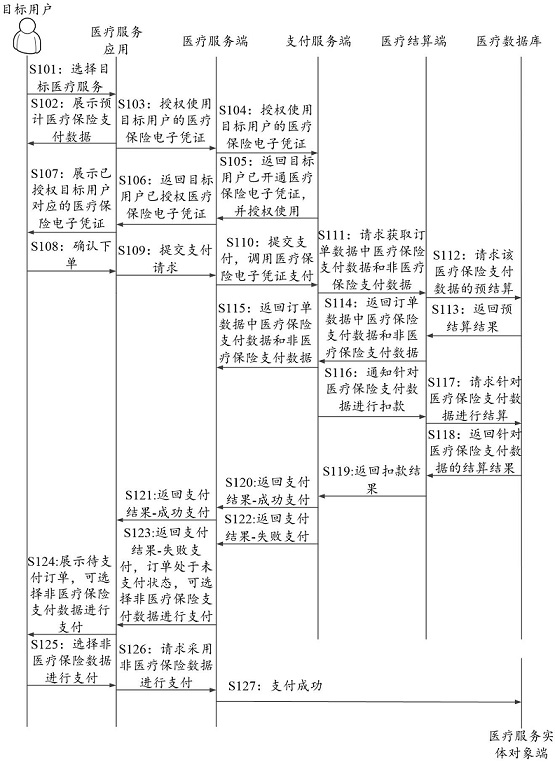
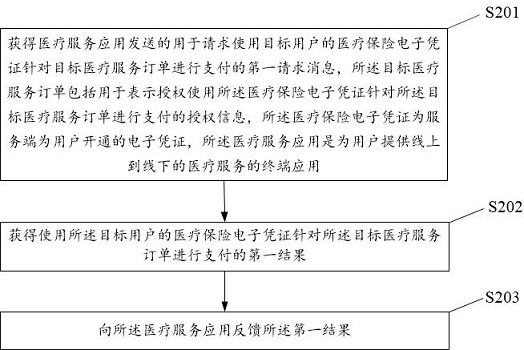
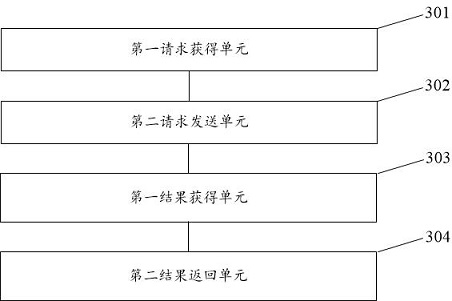
Medical service order processing method and device and electronic equipment
ActiveCN113989060AImprove experienceIncrease usageFinanceBuying/selling/leasing transactionsEngineeringOrder processing
The embodiment of the invention provides a medical service order processing method. The method comprises: obtaining a first request message which is sent by a medical service application and is used for requesting to use a medical insurance electronic certificate of a target user to perform payment for a target medical service order; obtaining a first result of payment for the target medical service order by using the medical insurance electronic certificate of the target user; and feeding back the first result to the medical service application. According to the method, the medical insurance electronic certificate is adopted to pay the target medical service order of the target user, the medical insurance electronic certificate is the electronic certificate opened for the user by the server side, and in the process of paying the target medical service order, the target user does not need to input offline medical insurance card information; and convenient conditions are provided for the user to purchase the target medical service in the medical service application, the experience feeling of the user on an online medical service platform is improved, and the utilization rate of the medical service application by the user is also improved.
Owner:ZHEJIANG KOUBEI NETWORK TECH CO LTD
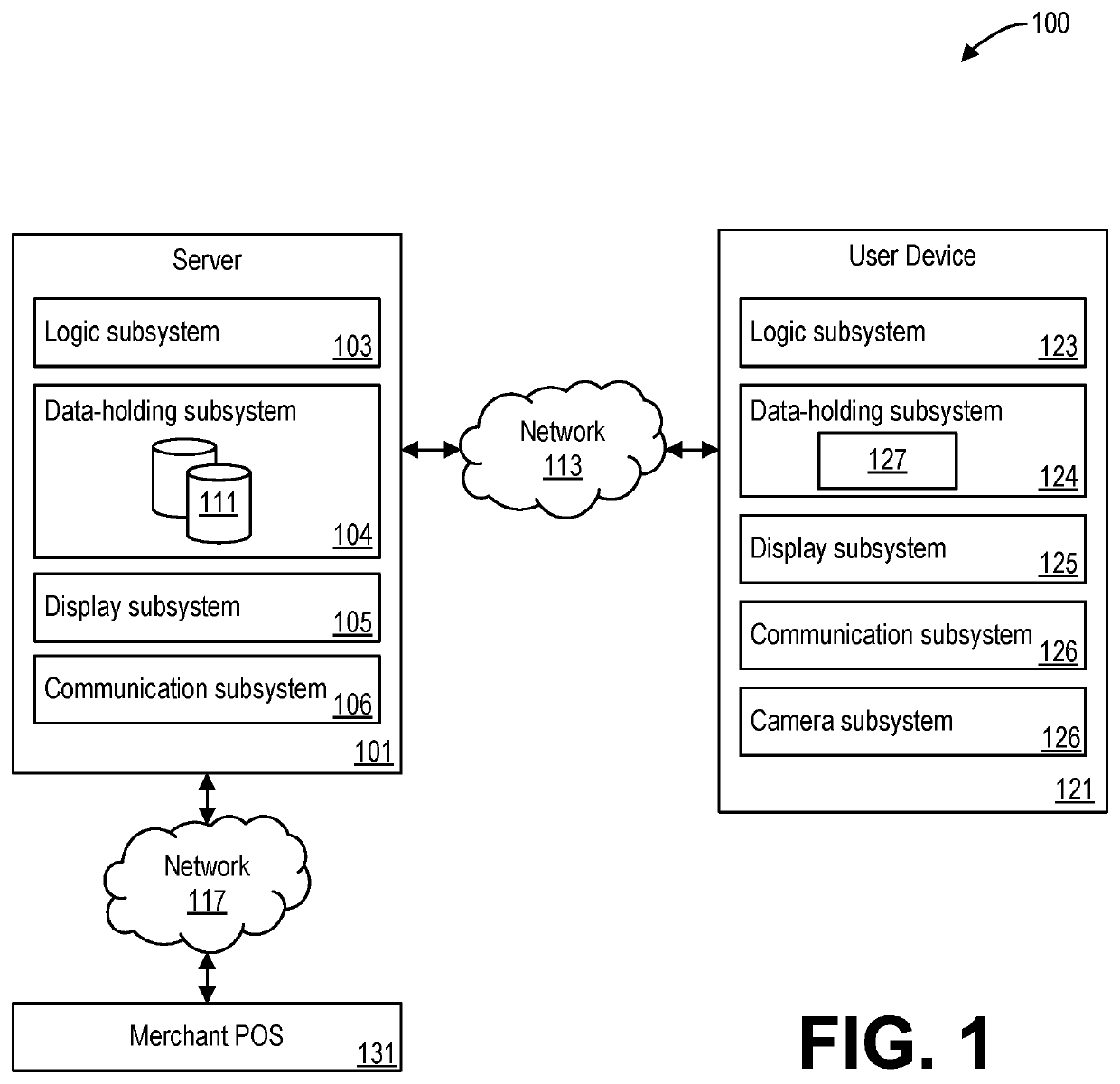
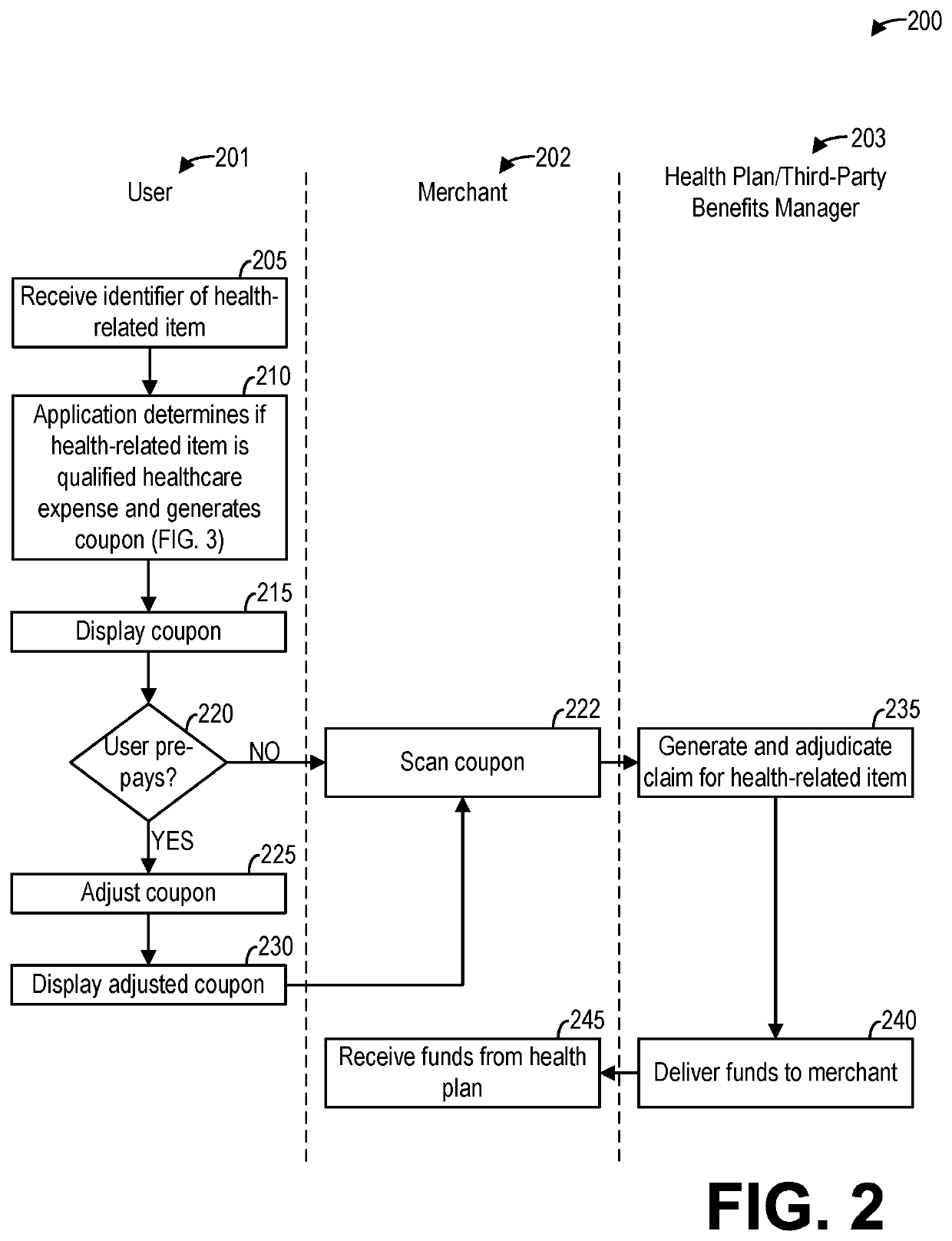
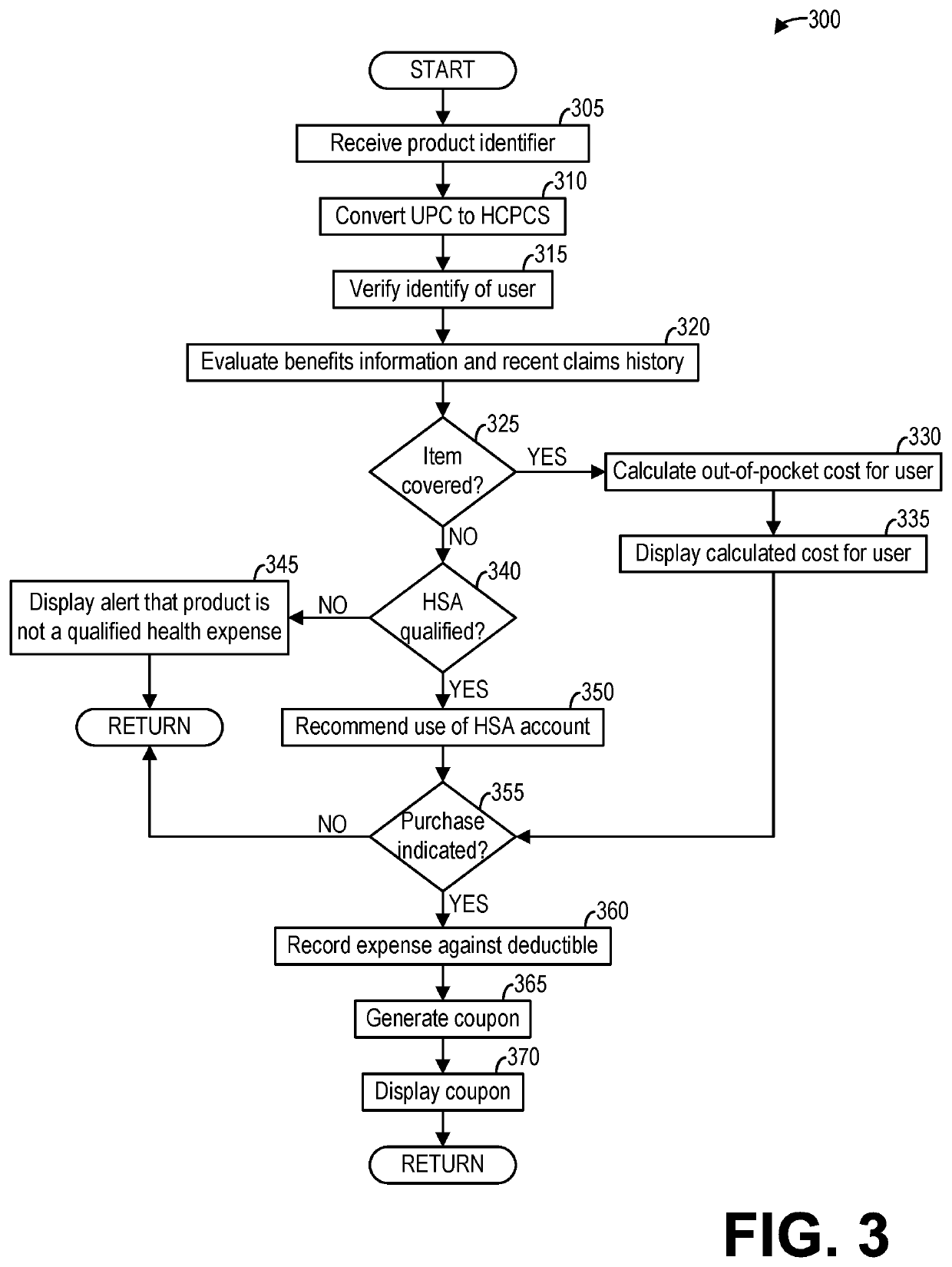
Methods and systems for facilitating purchase of a health-related product
In particular, systems and methods for facilitating the purchase of health-related items such as durable medical equipment are provided. In one embodiment, a method comprises: responsive to a selection of a health-related product input by a user, automatically determining if the health-related product is a qualified healthcare expense; calculating an out-of-pocket cost to the user of the healthcare product based on a health insurance plan of the user; and generating a coupon for the health-related product that discounts a retail cost of the health-related product to the out-of-pocket cost responsive to a merchant accepting the coupon. In this way, a healthcare consumer may utilize their healthcare insurance benefits to purchase health-related products such as durable medical equipment from retail merchants.
Owner:THE REGENCE GROUP
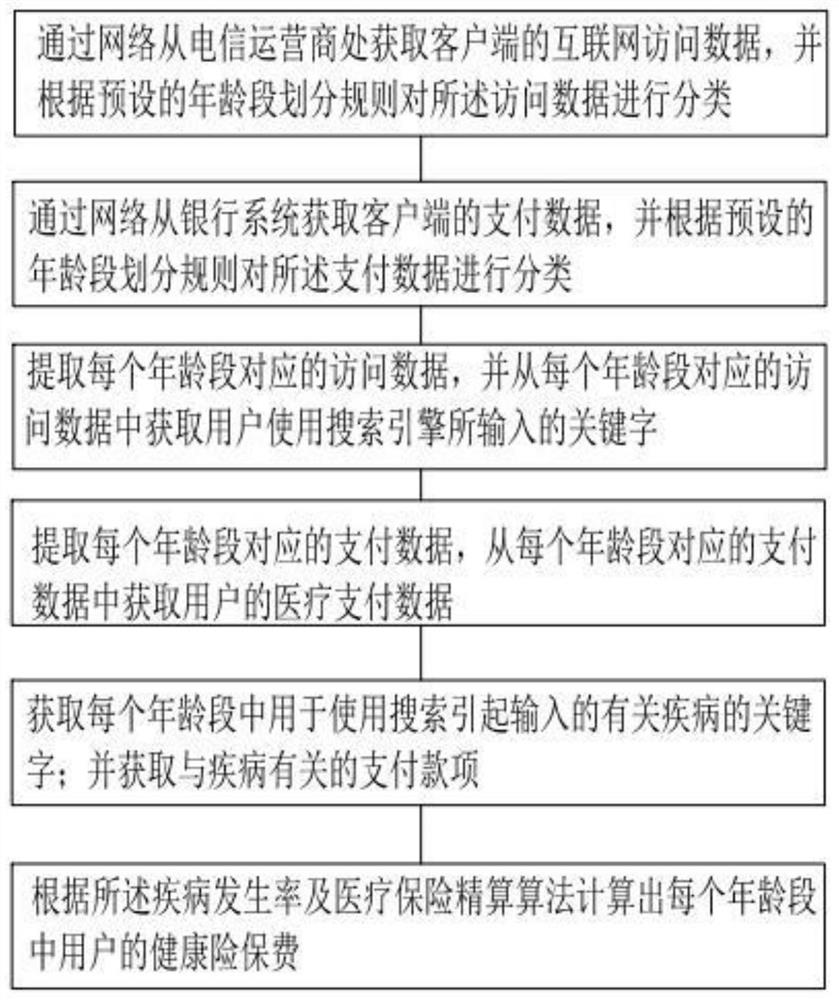
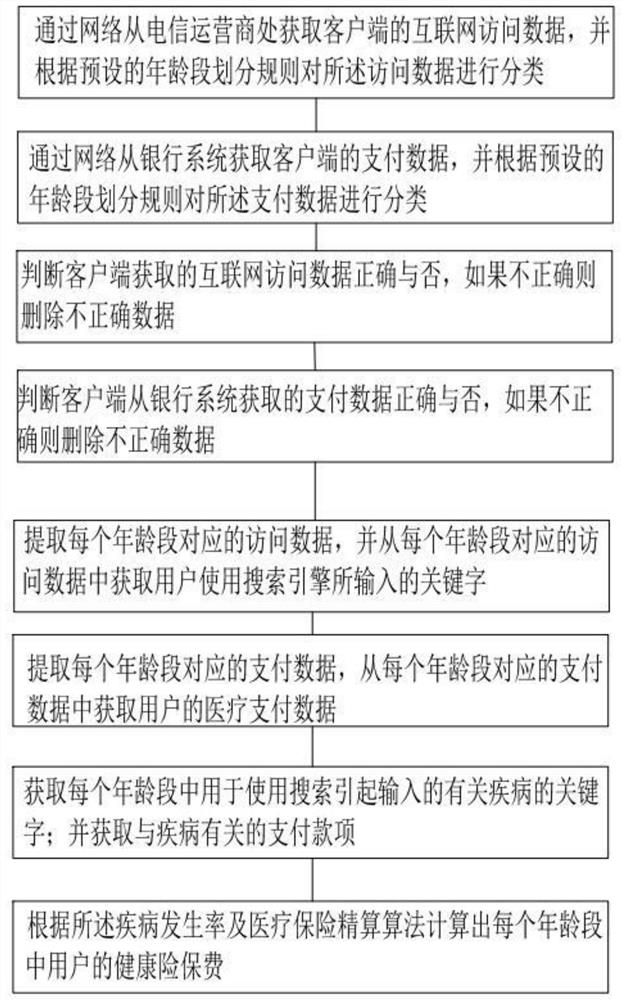
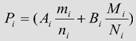
Actuarial insurance method based on big data
PendingCN113011987AImprove accuracyIncrease profitabilityFinanceWeb data queryingOperations researchData science
The invention discloses an actuarial insurance method based on big data, and relates to the technical field of insurance analysis, the method is operated in a data processing center, the disease incidence rate is calculated by integrating search data and payment data, the accuracy of calculation of the disease incidence rate is improved, and the accuracy of calculation of the disease incidence rate is improved. And the premium of the medical insurance is correspondingly adjusted according to the disease risk rate, so that the risk of the medical insurance can be effectively reduced, and the profitability of an insurance company is improved.
Owner:北京爱选信息科技有限公司
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com