Patents
Literature
Hiro is an intelligent assistant for R&D personnel, combined with Patent DNA, to facilitate innovative research.
85 results about "Tissue thickness" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
Tissue thickness was significantly different (p<0.01) at each location with the antrum being the thickest at 2.70 mm, followed by the midbody at 2.33 mm, and the fundus was the thinnest at 1.97 mm.
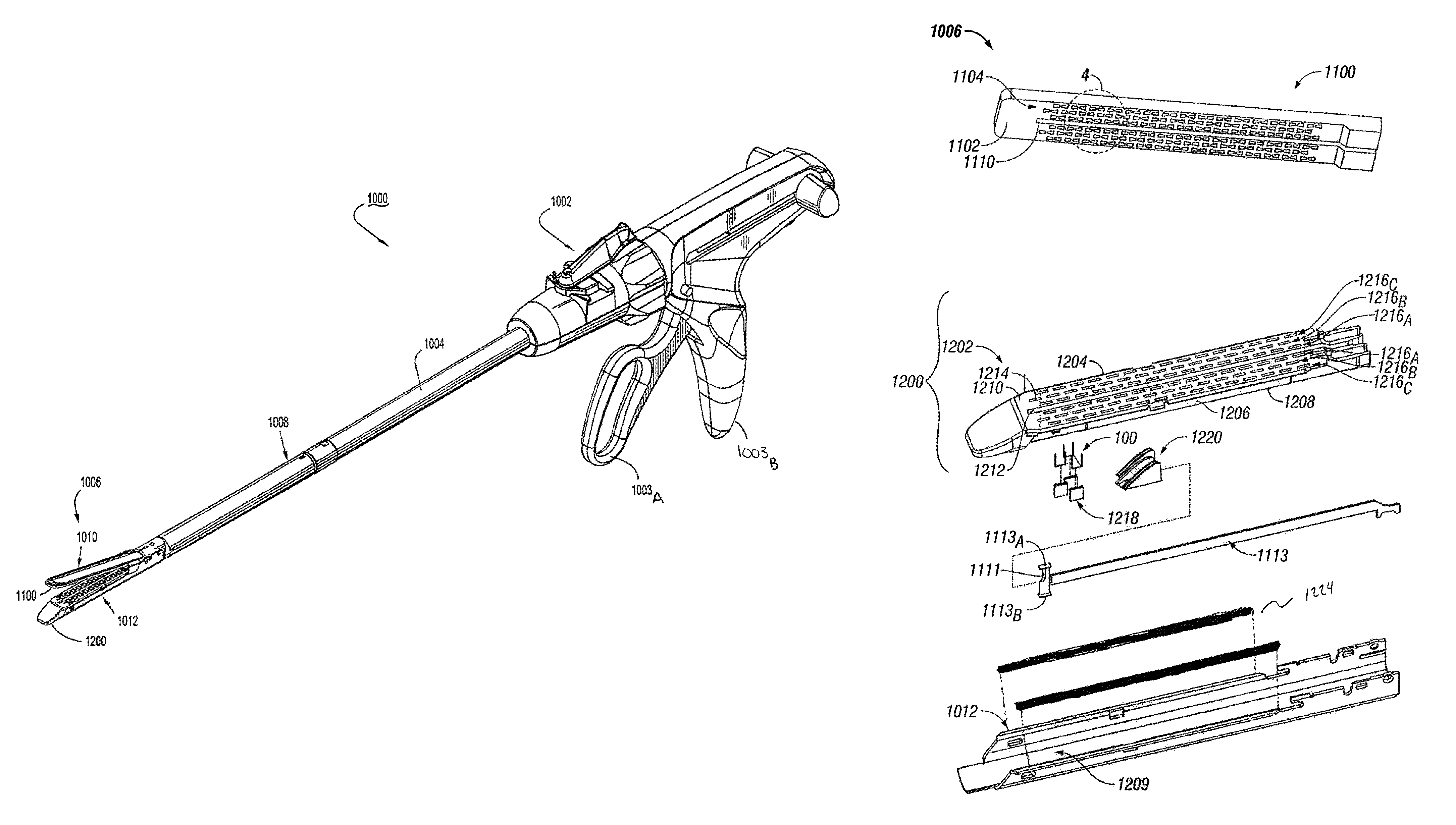
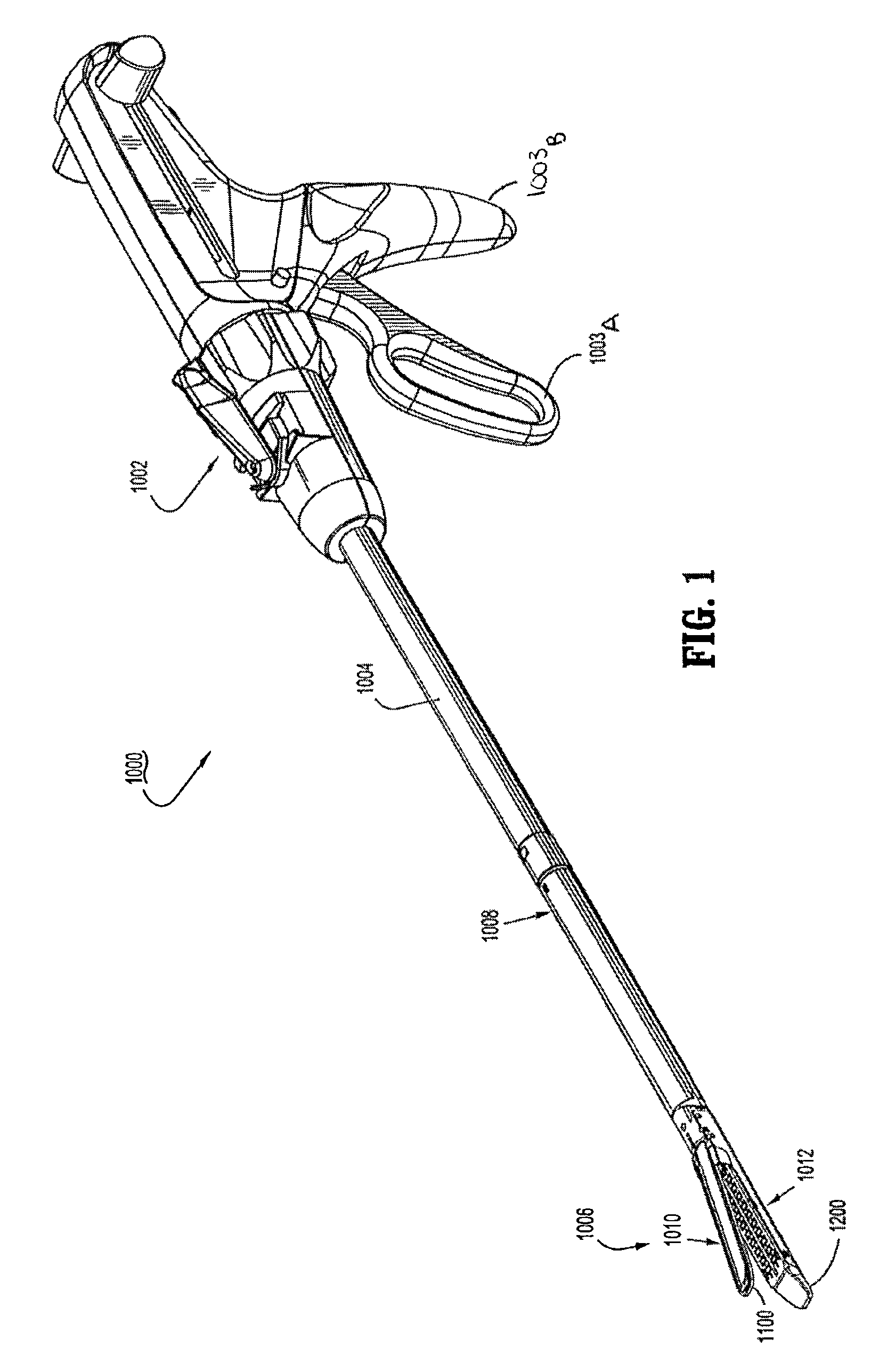
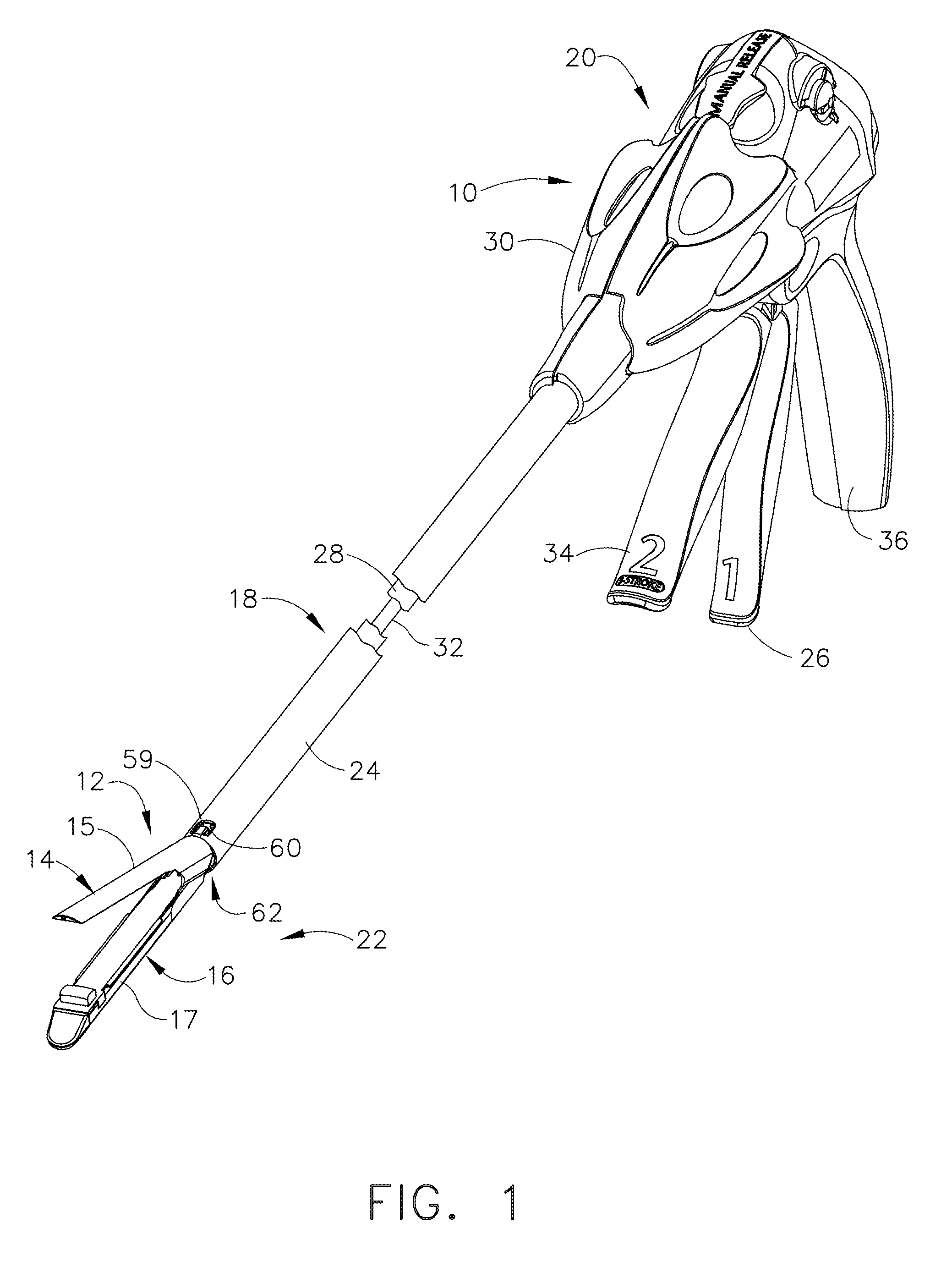
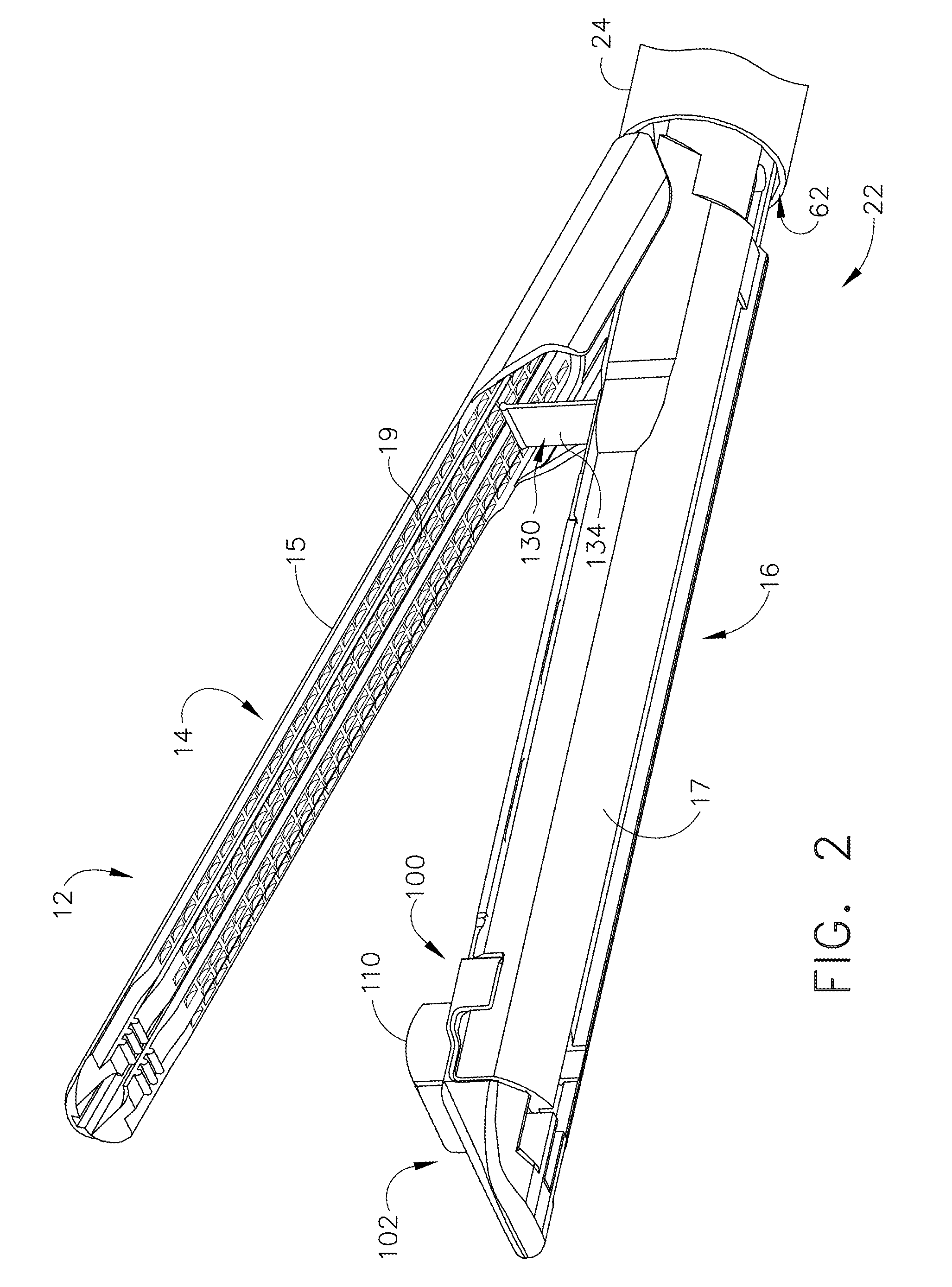
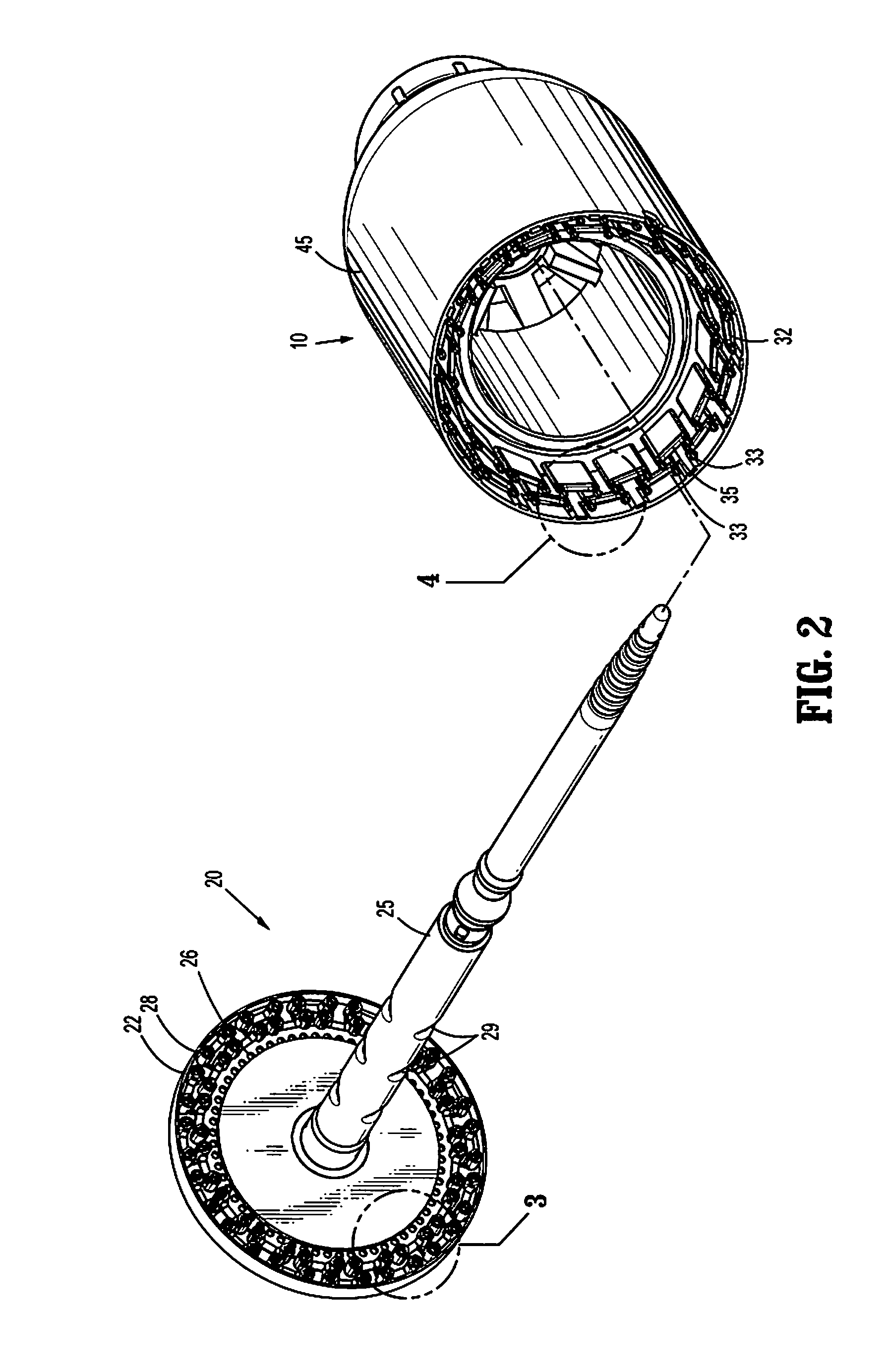
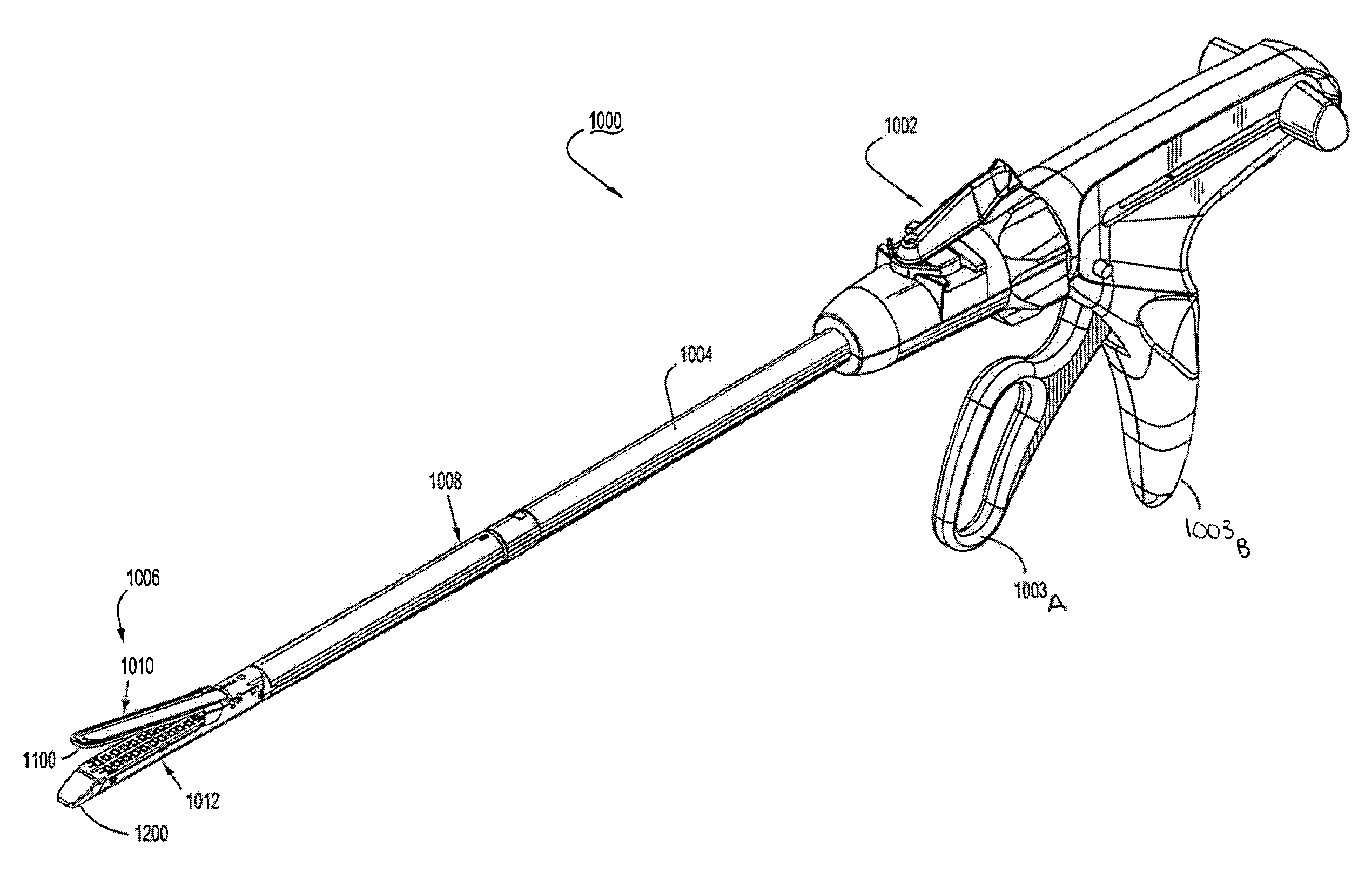
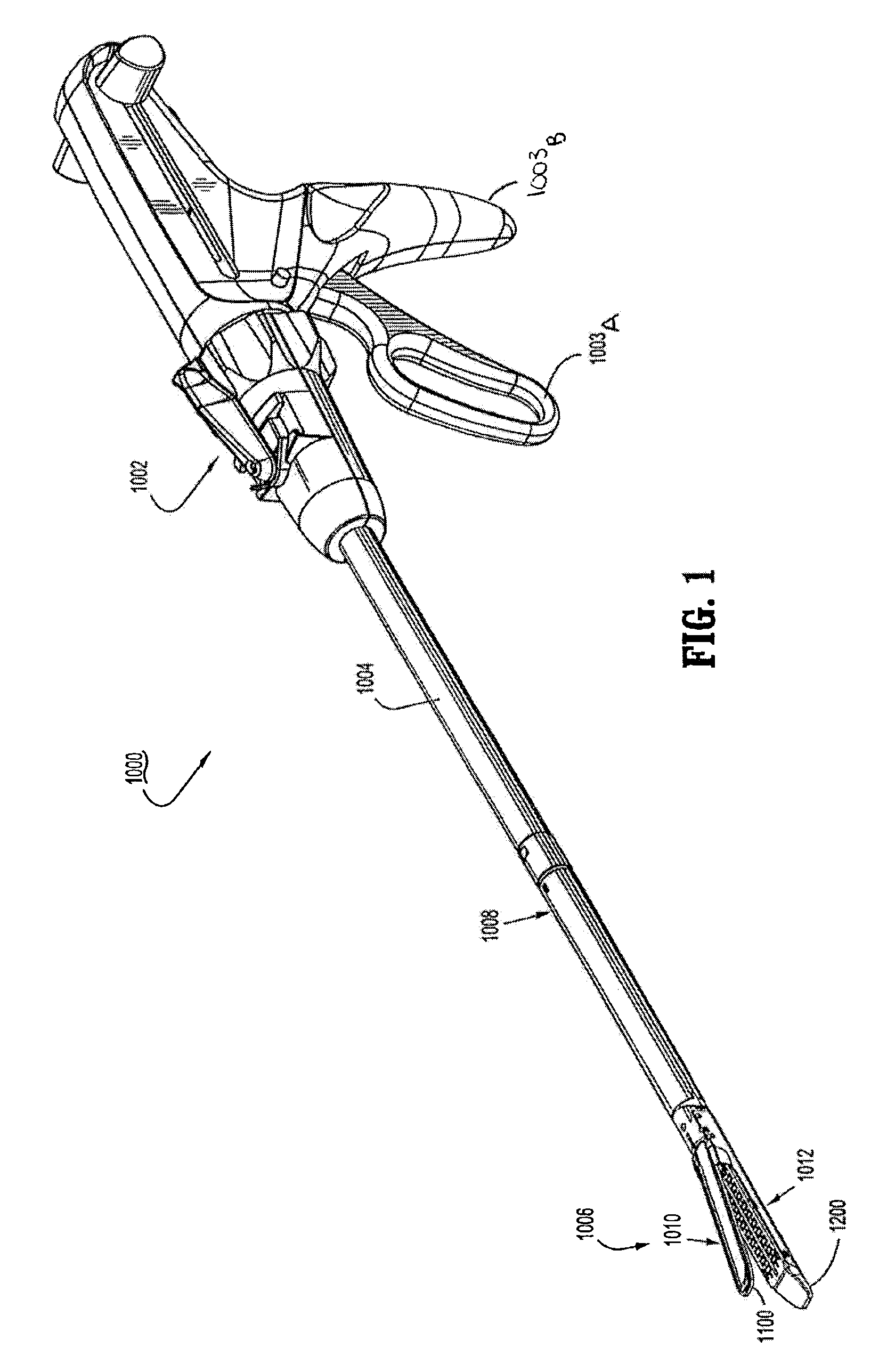
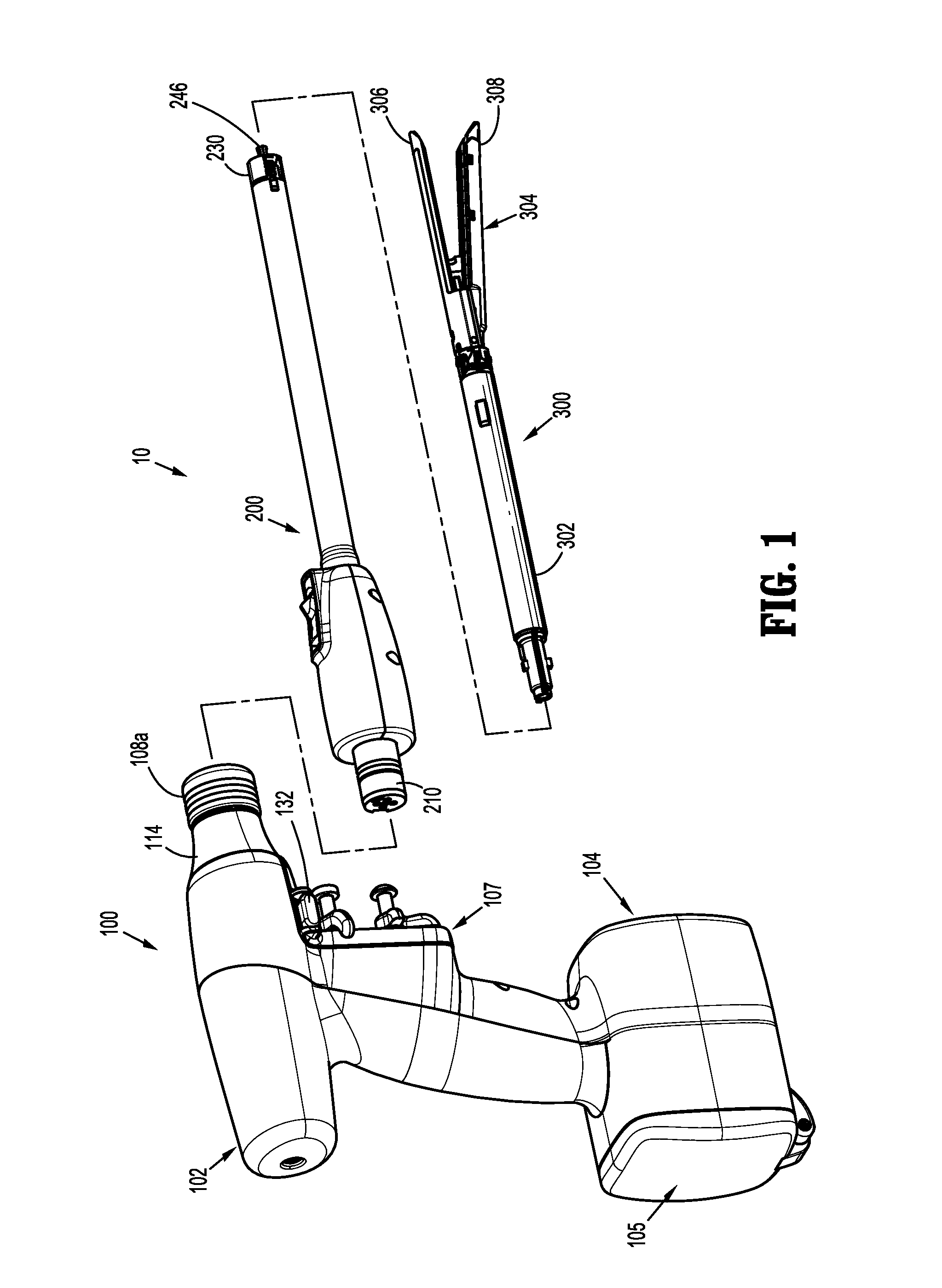
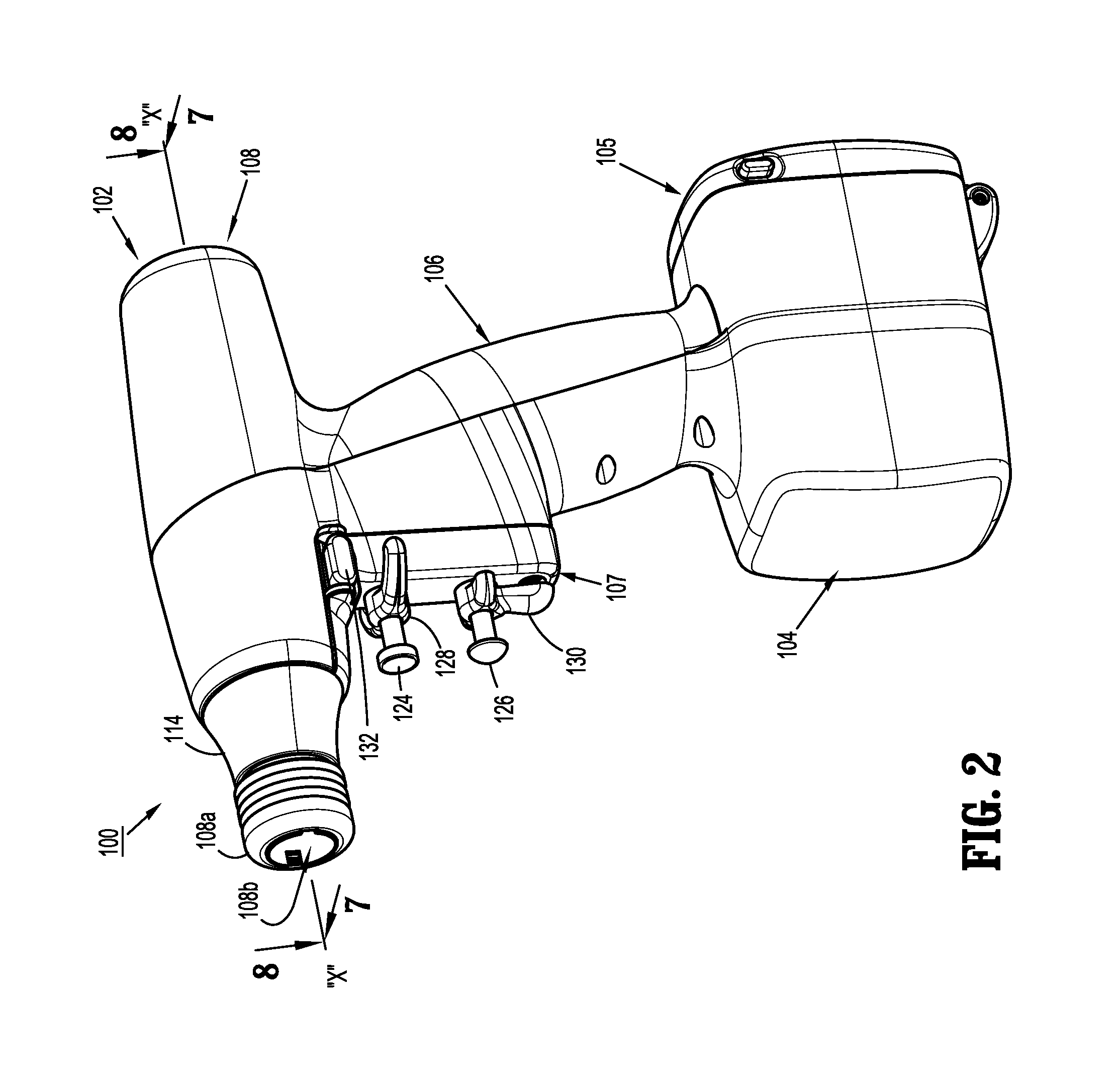
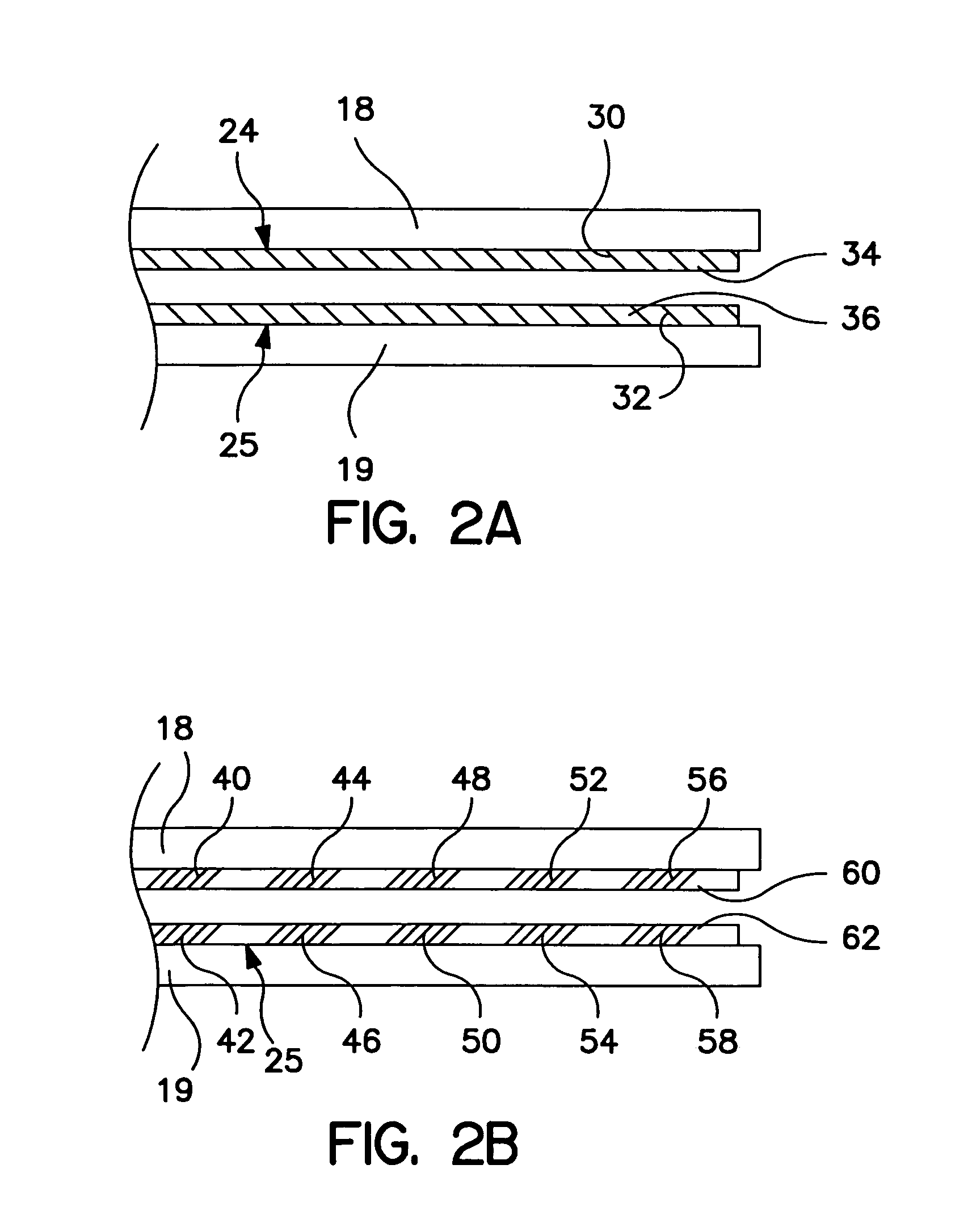
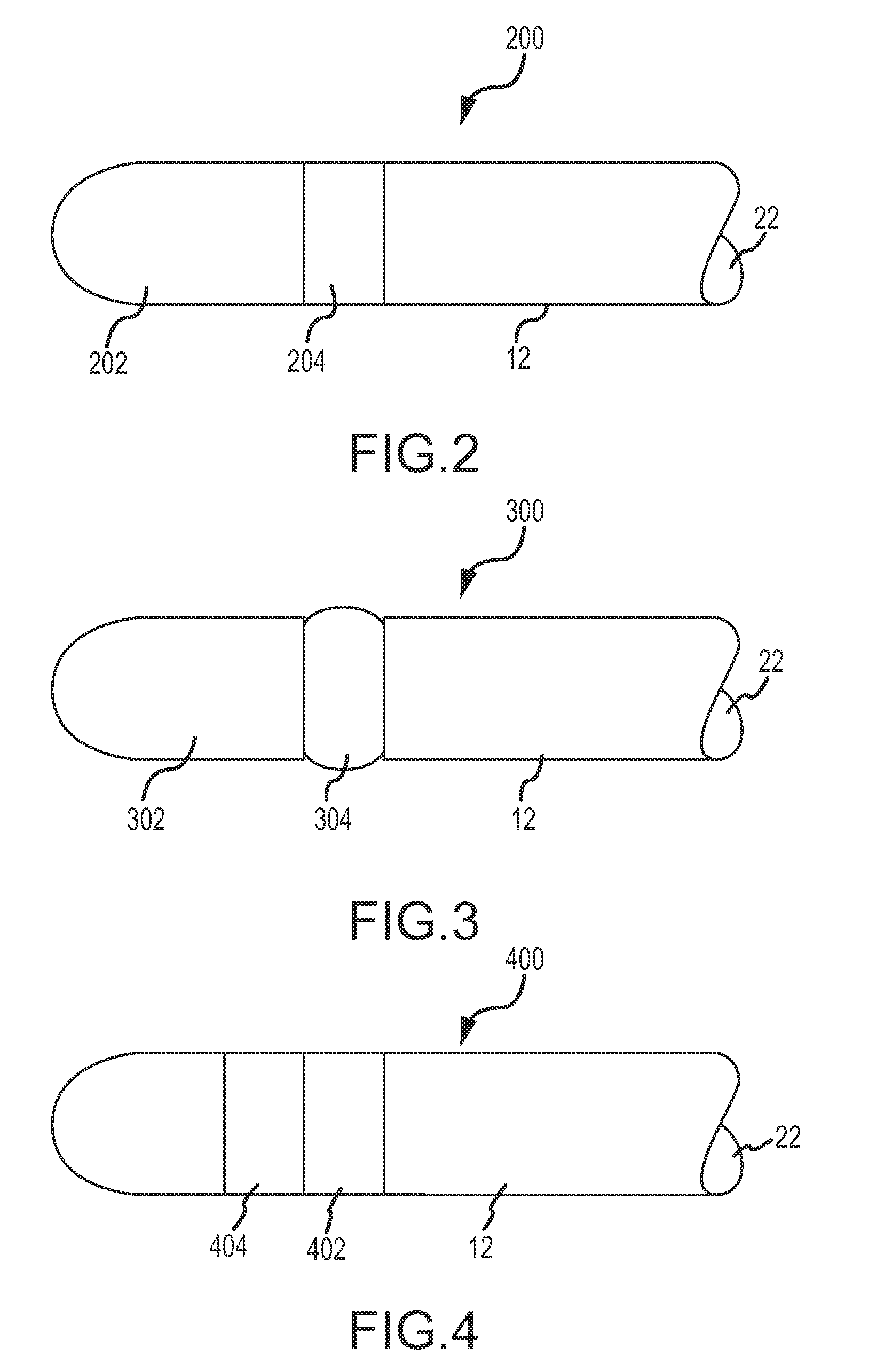
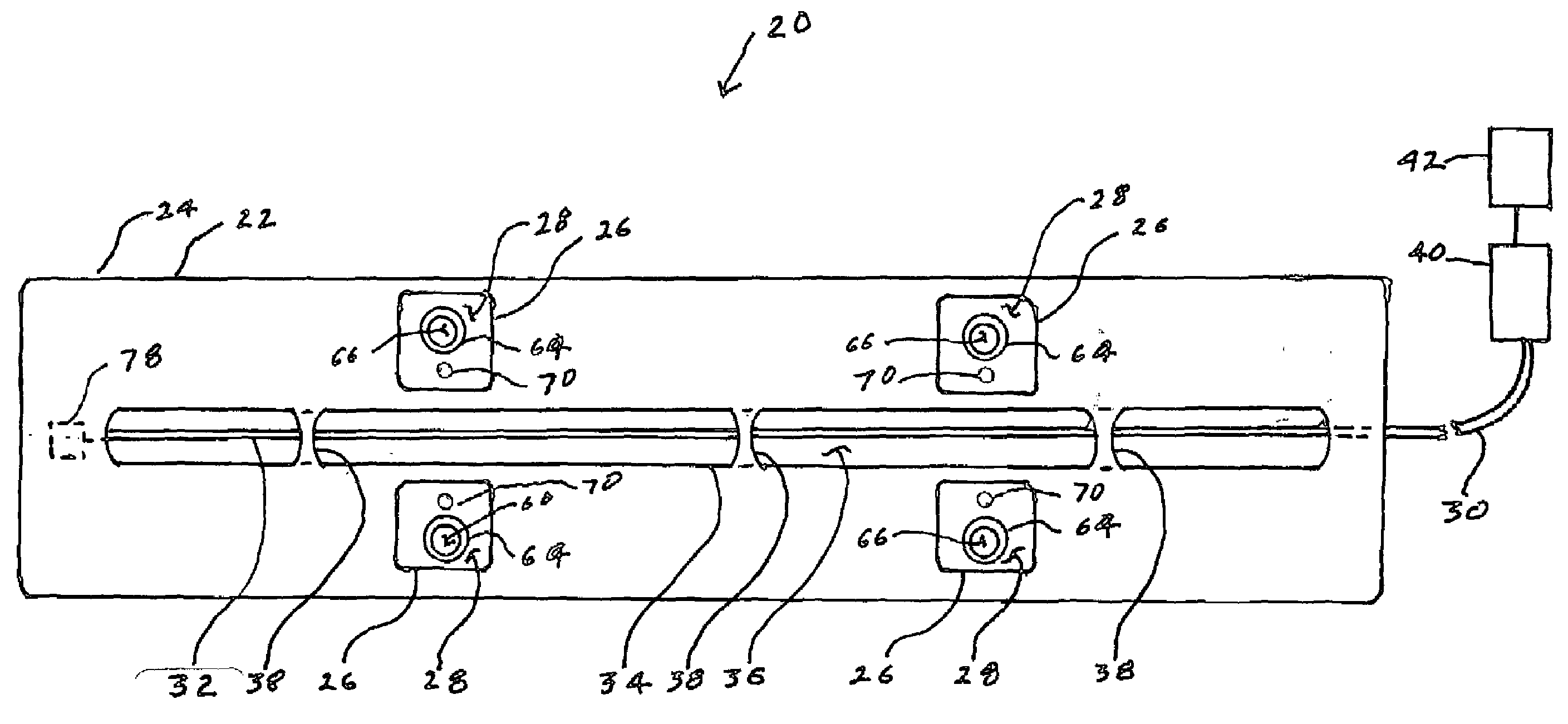
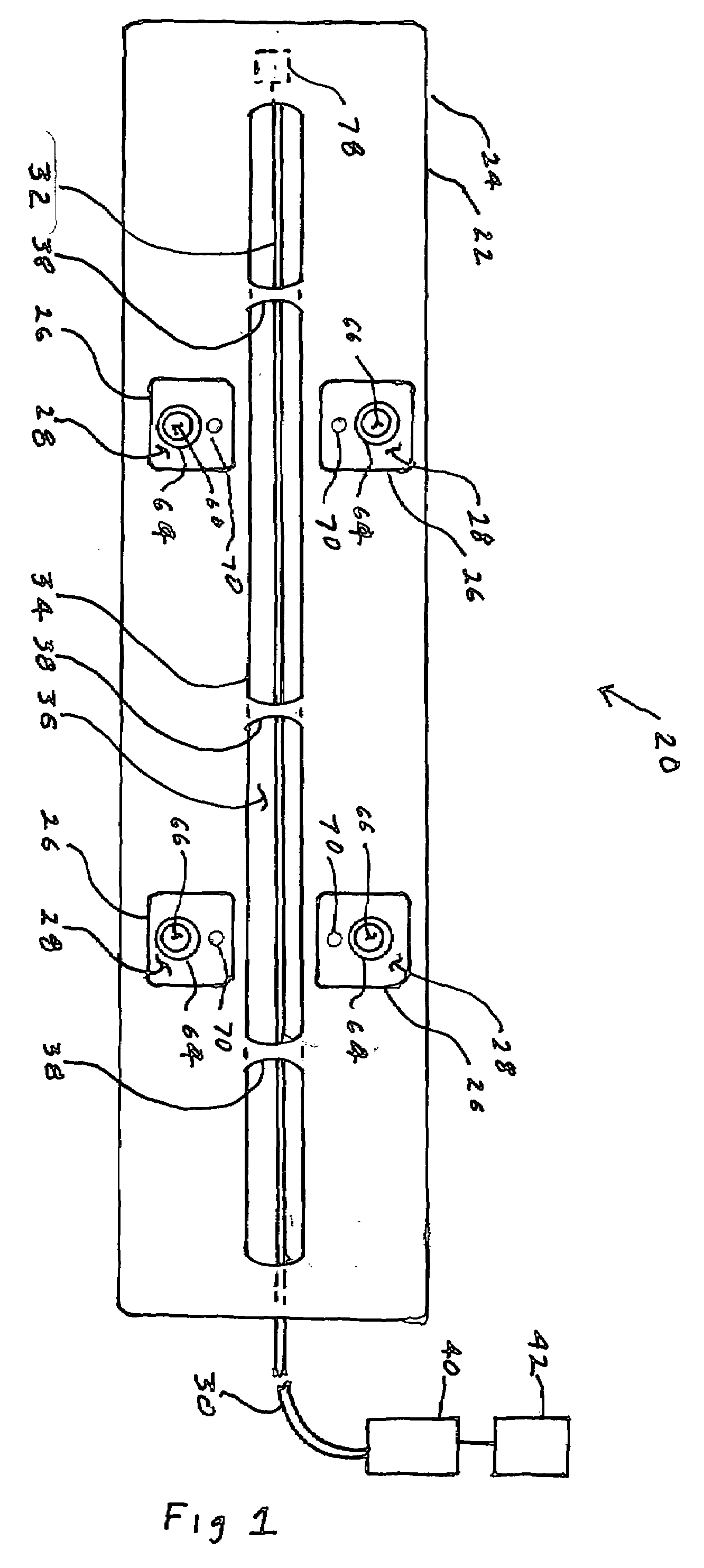
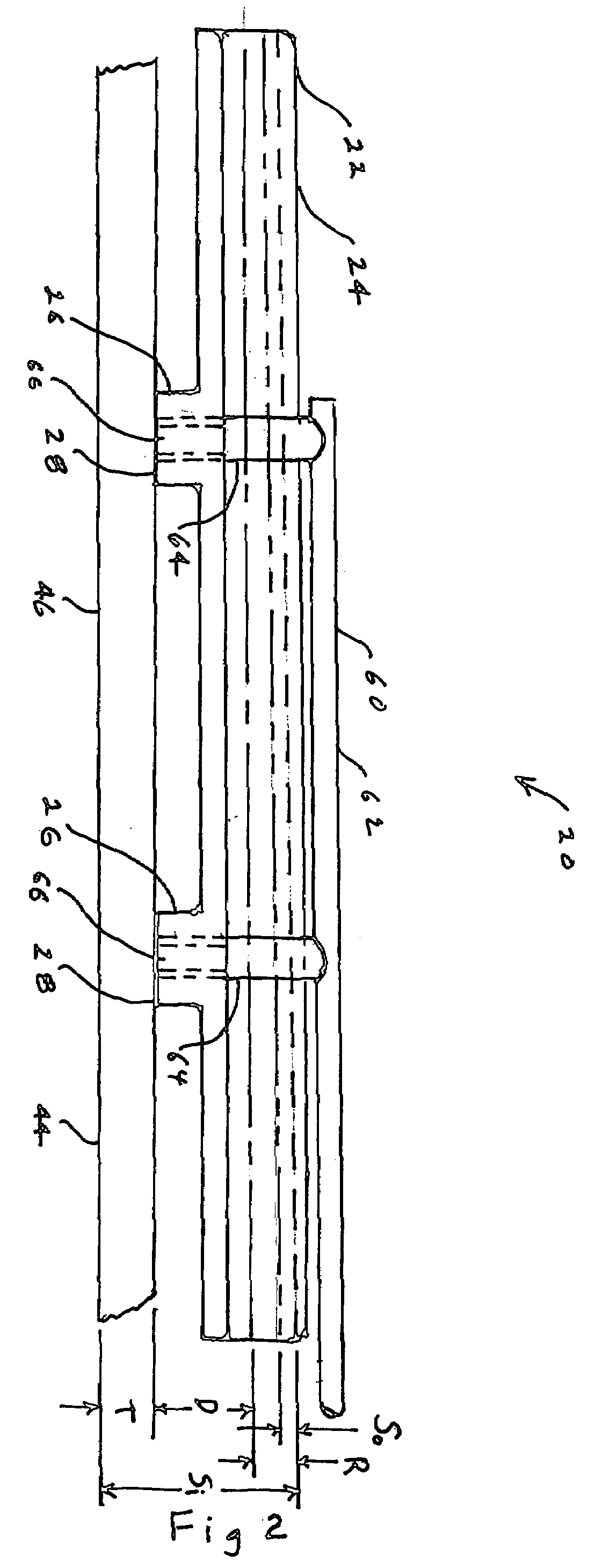
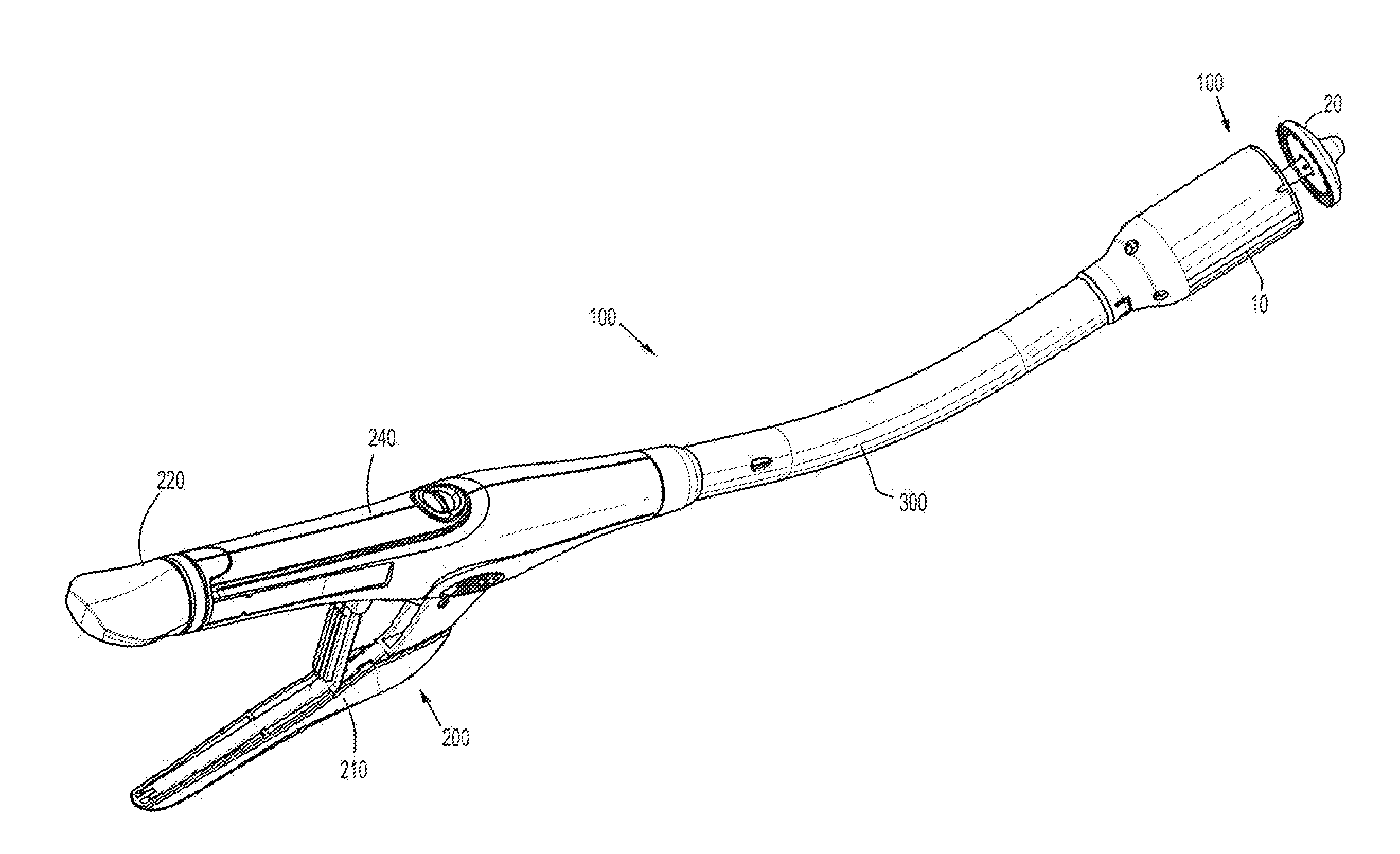
Varying tissue compression aided by elastic members
The present disclosure relates to surgical fastener applying apparatus, and the application of variable compression to tissue. More specifically, the presently disclosed surgical fastener applying apparatus including a first jaw having proximal and distal ends and including an anvil member, the anvil member extending along a longitudinal axis and including a tissue contacting surface and a second jaw having proximal and distal ends movably coupled to the first jaw, the second jaw including a cartridge member and a channel. The surgical fastener applying apparatus further includes a pair of elastic members positioned between the cartridge member and the channel of the second jaw, the pair of elastic members configured and dimensioned to apply and maintain constant compressive forces to tissue regardless of tissue thickness.
Owner:COVIDIEN LP
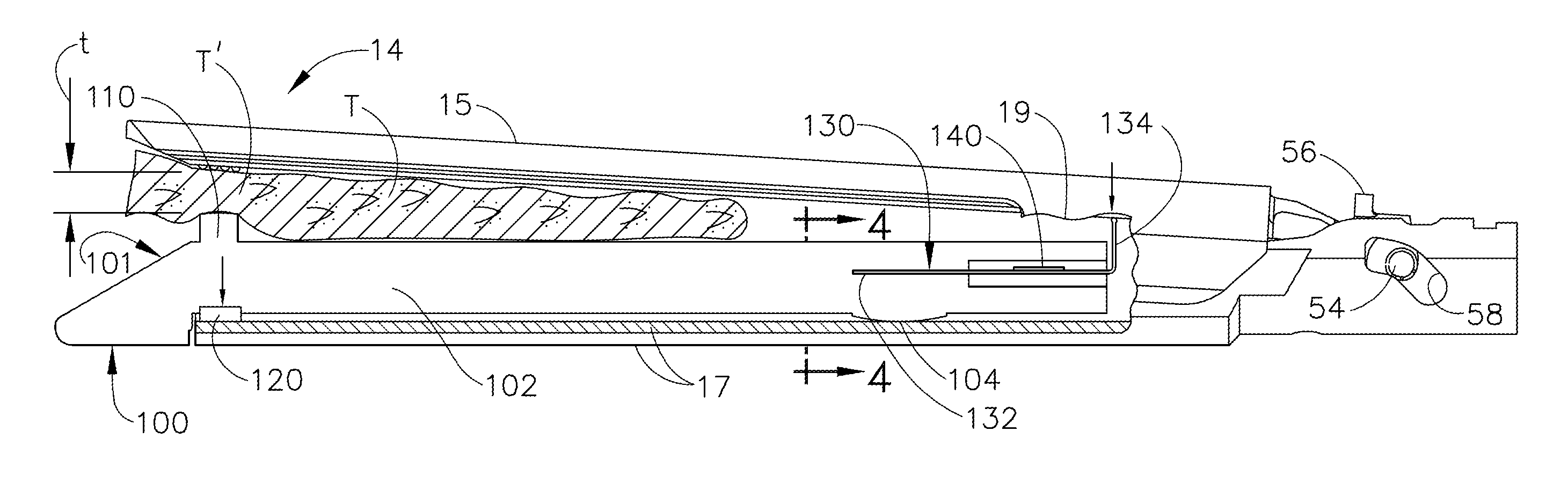
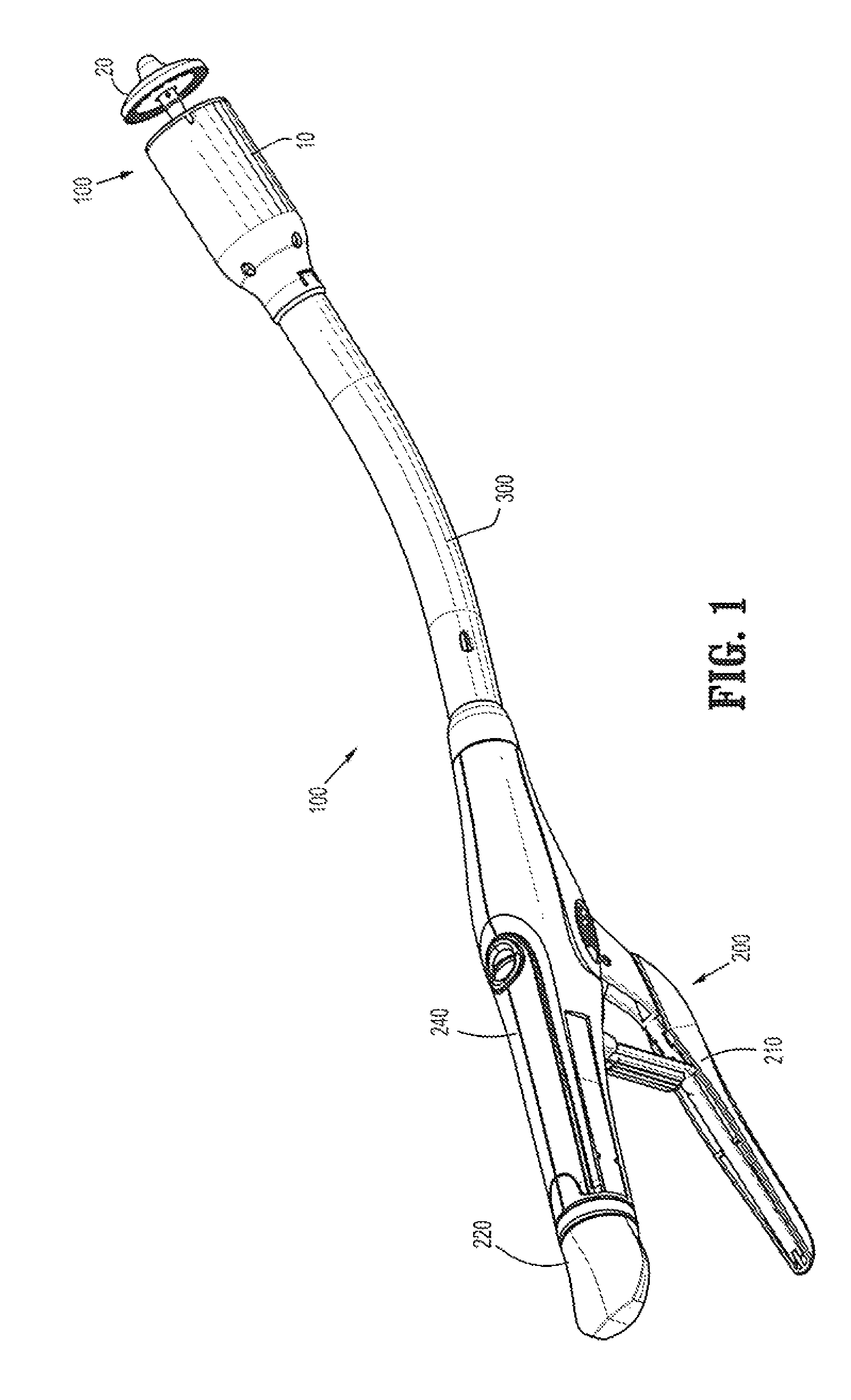
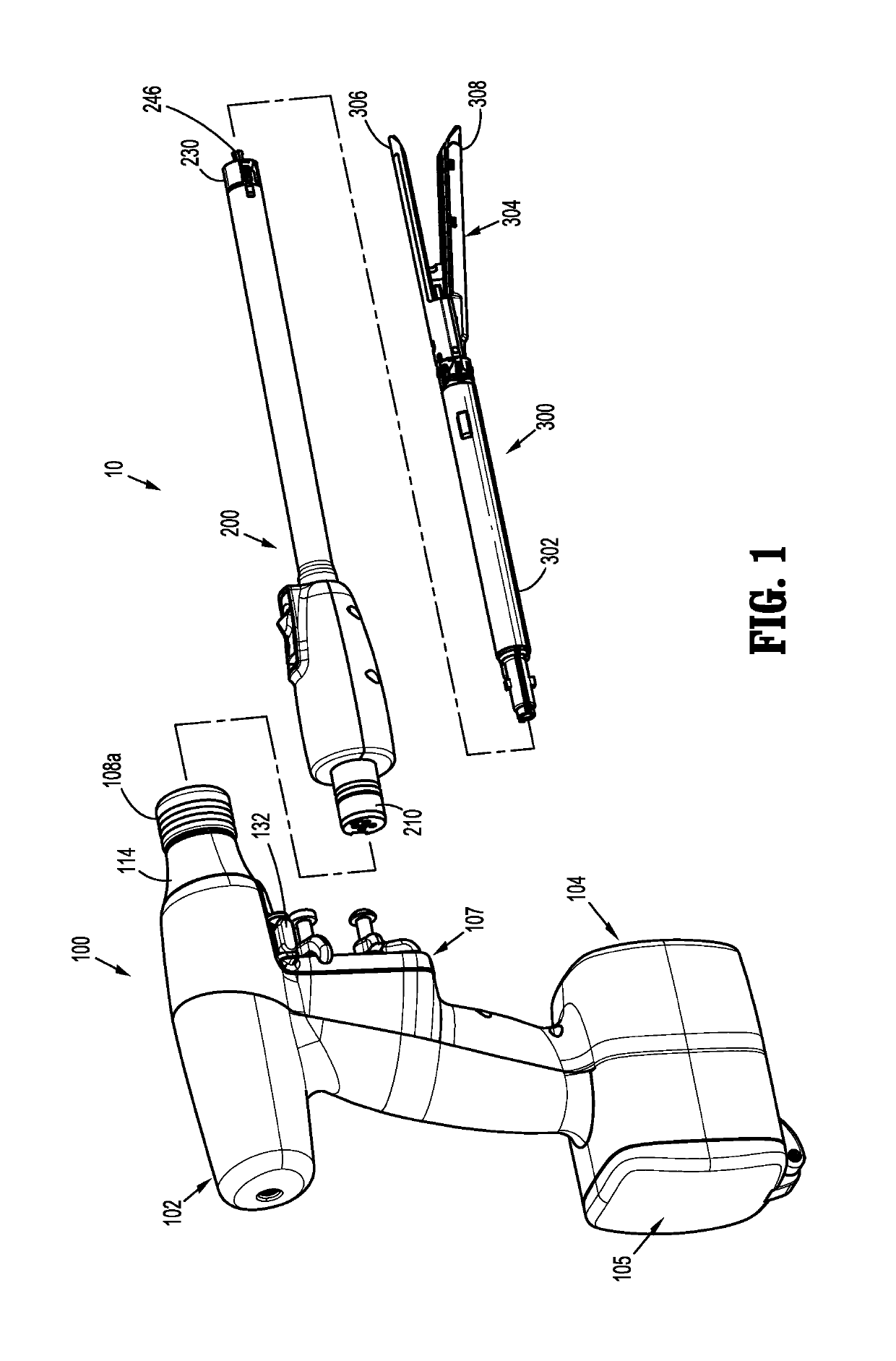
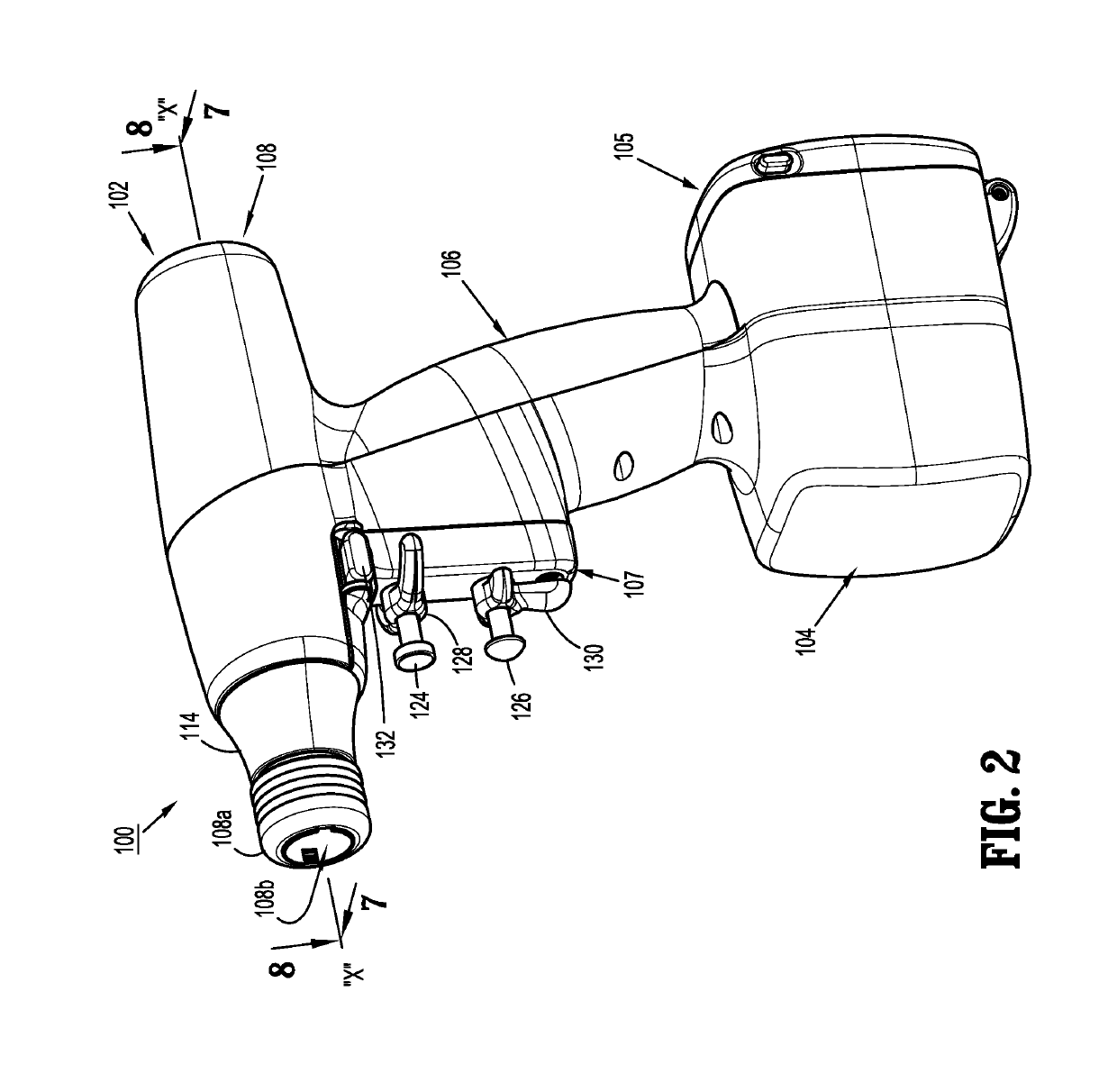
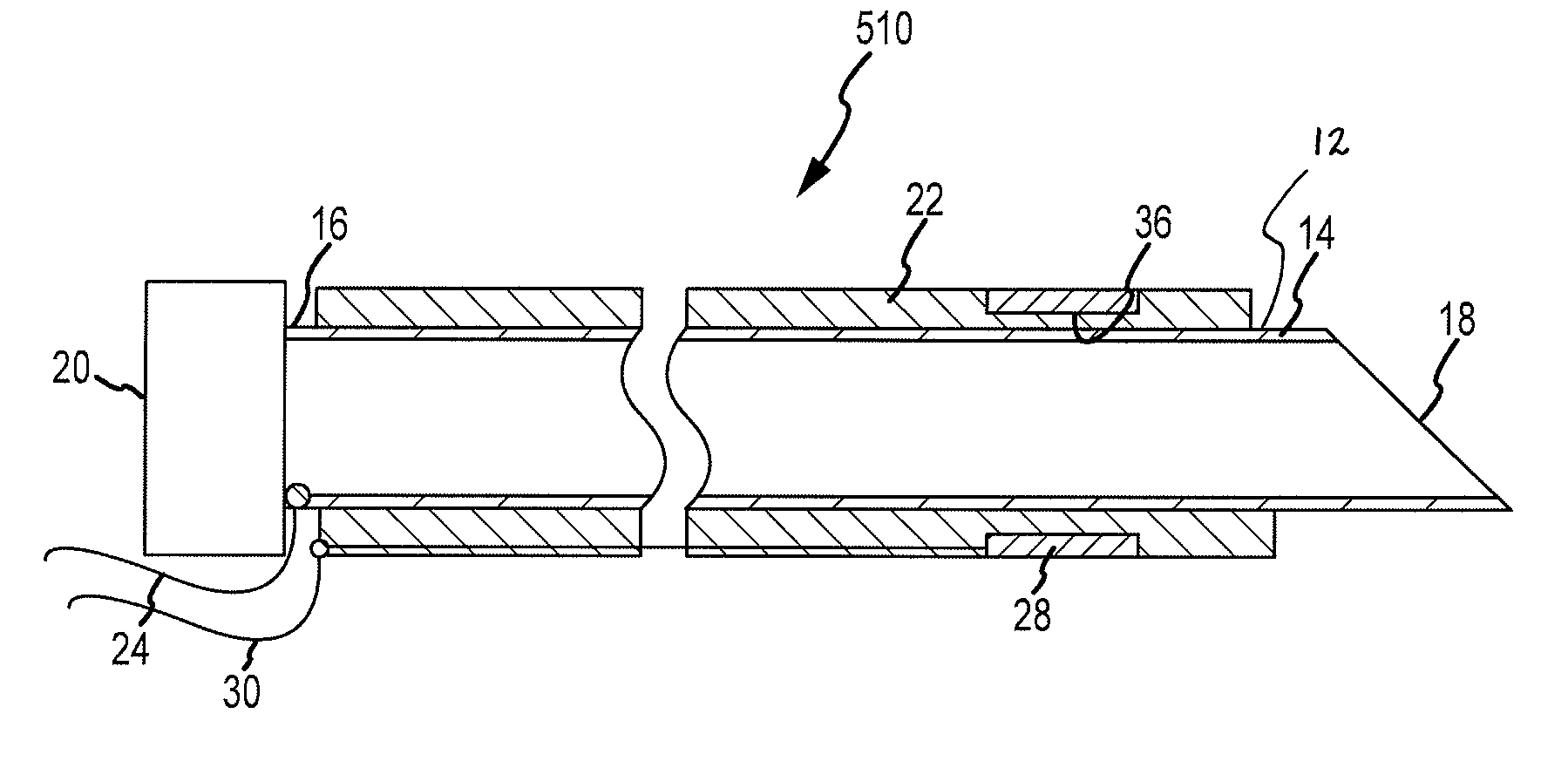
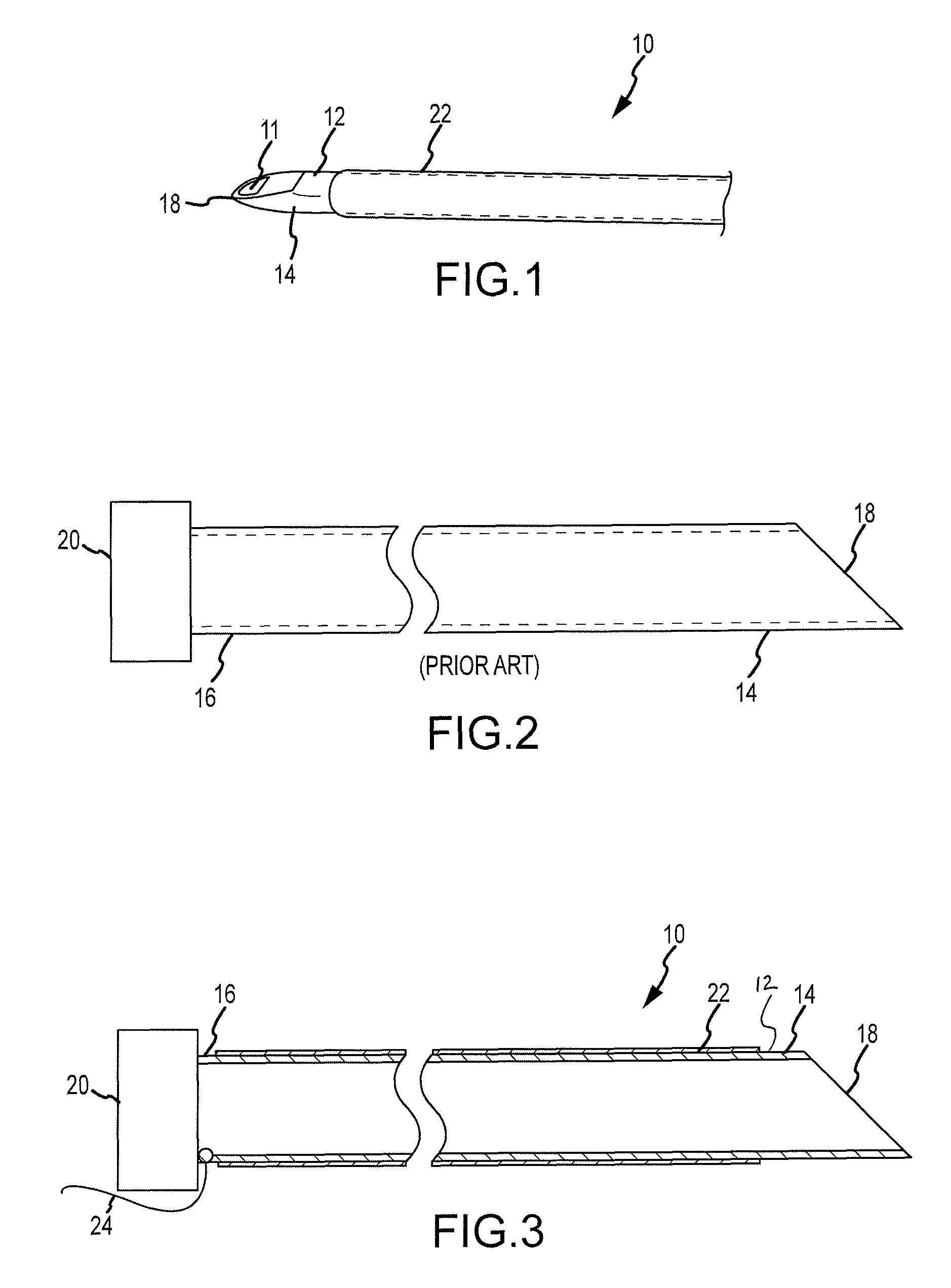
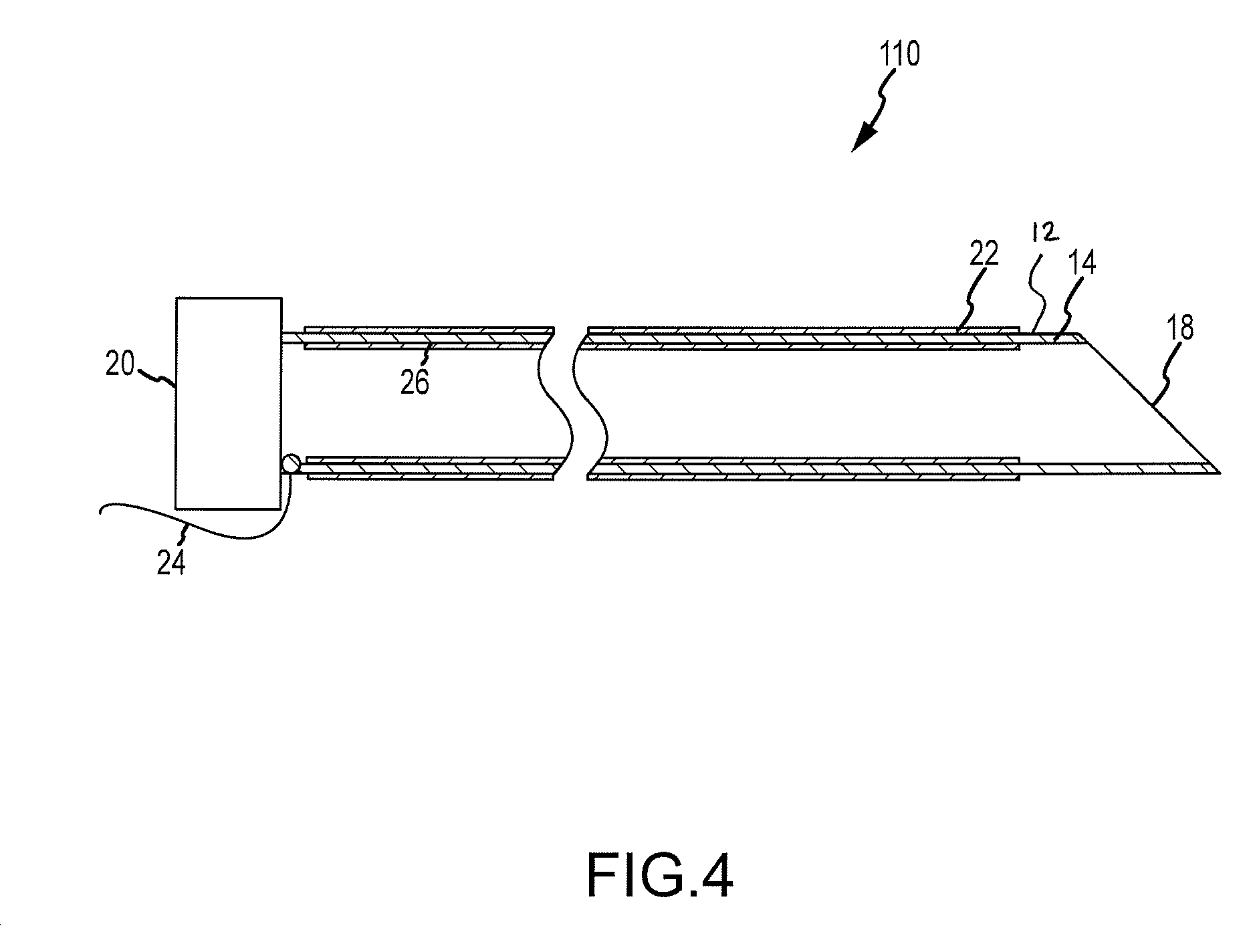
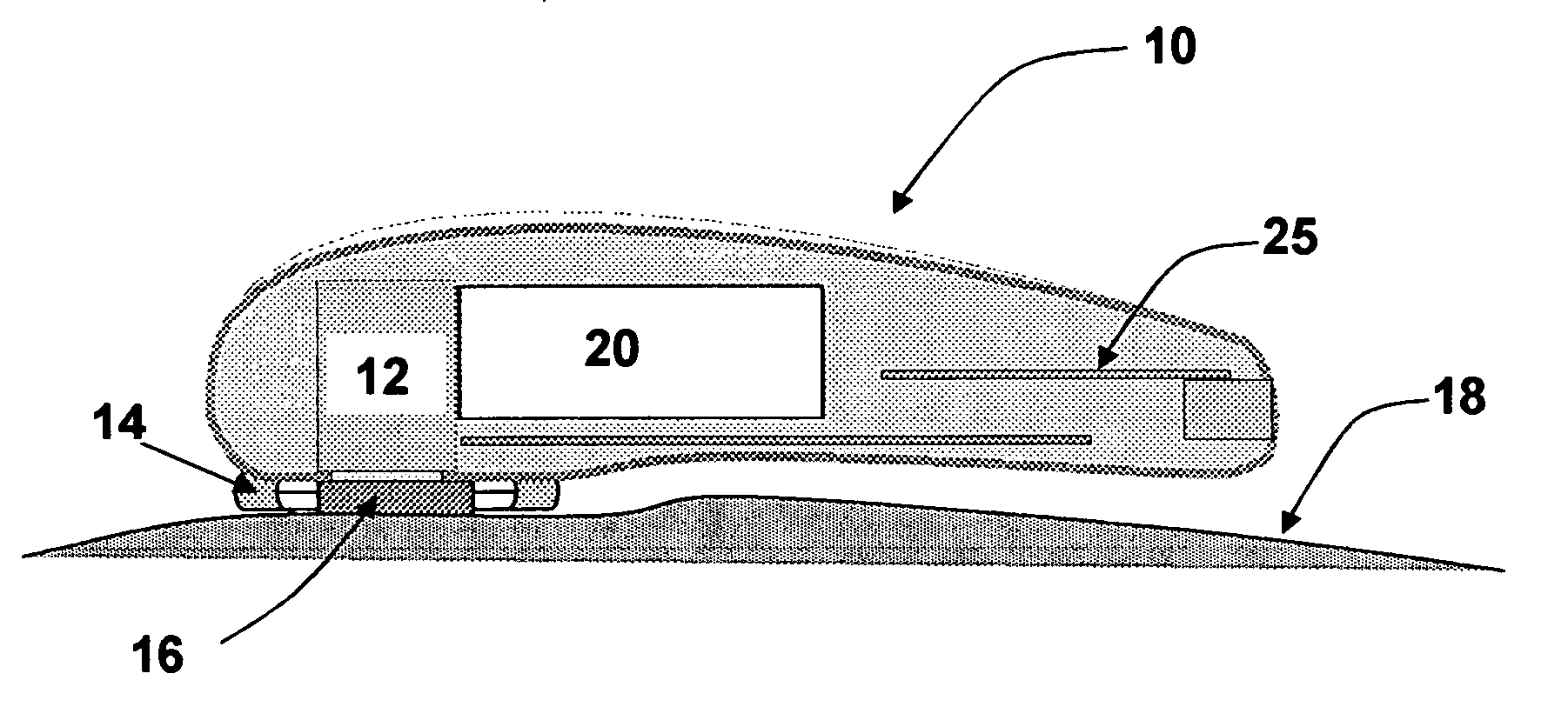
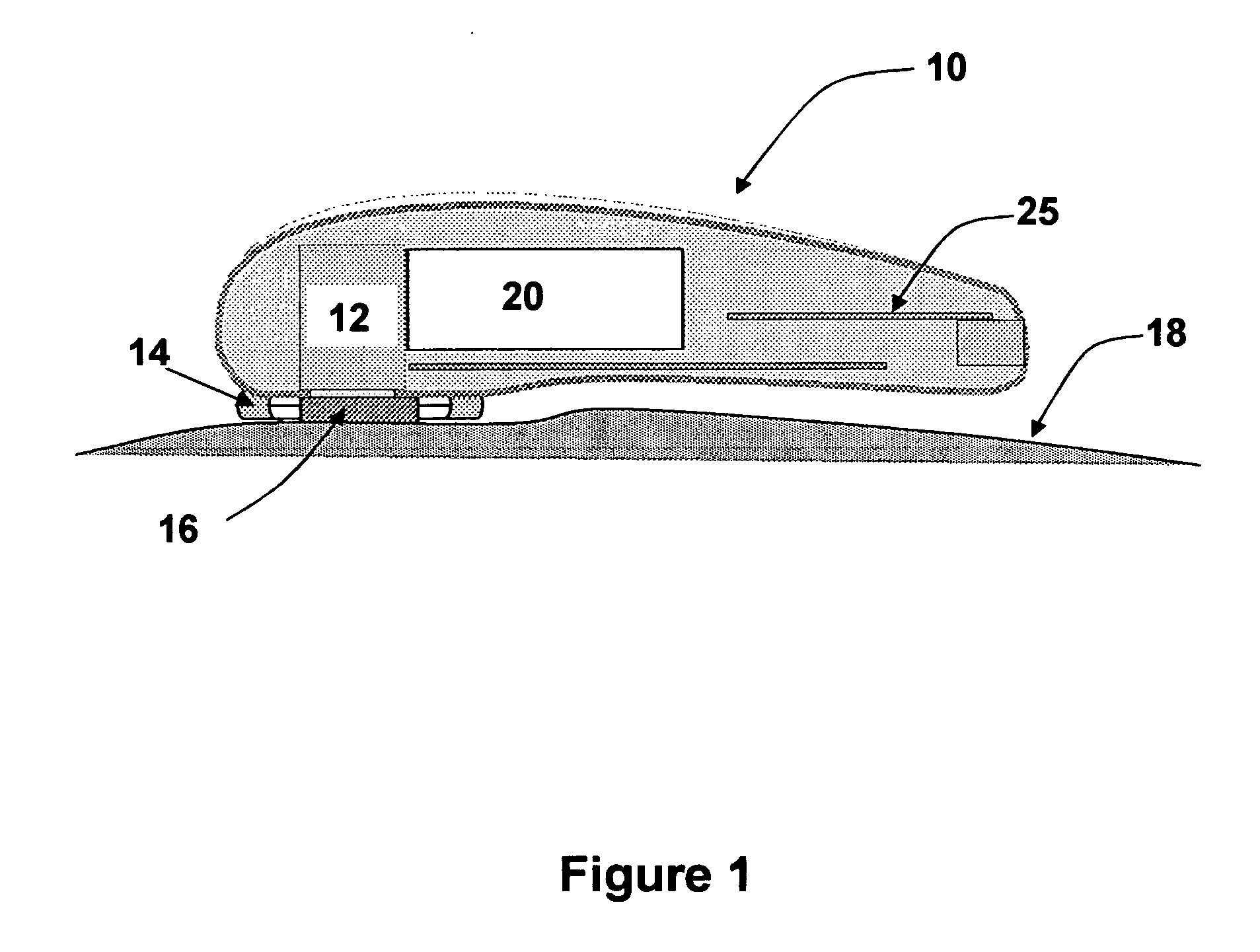
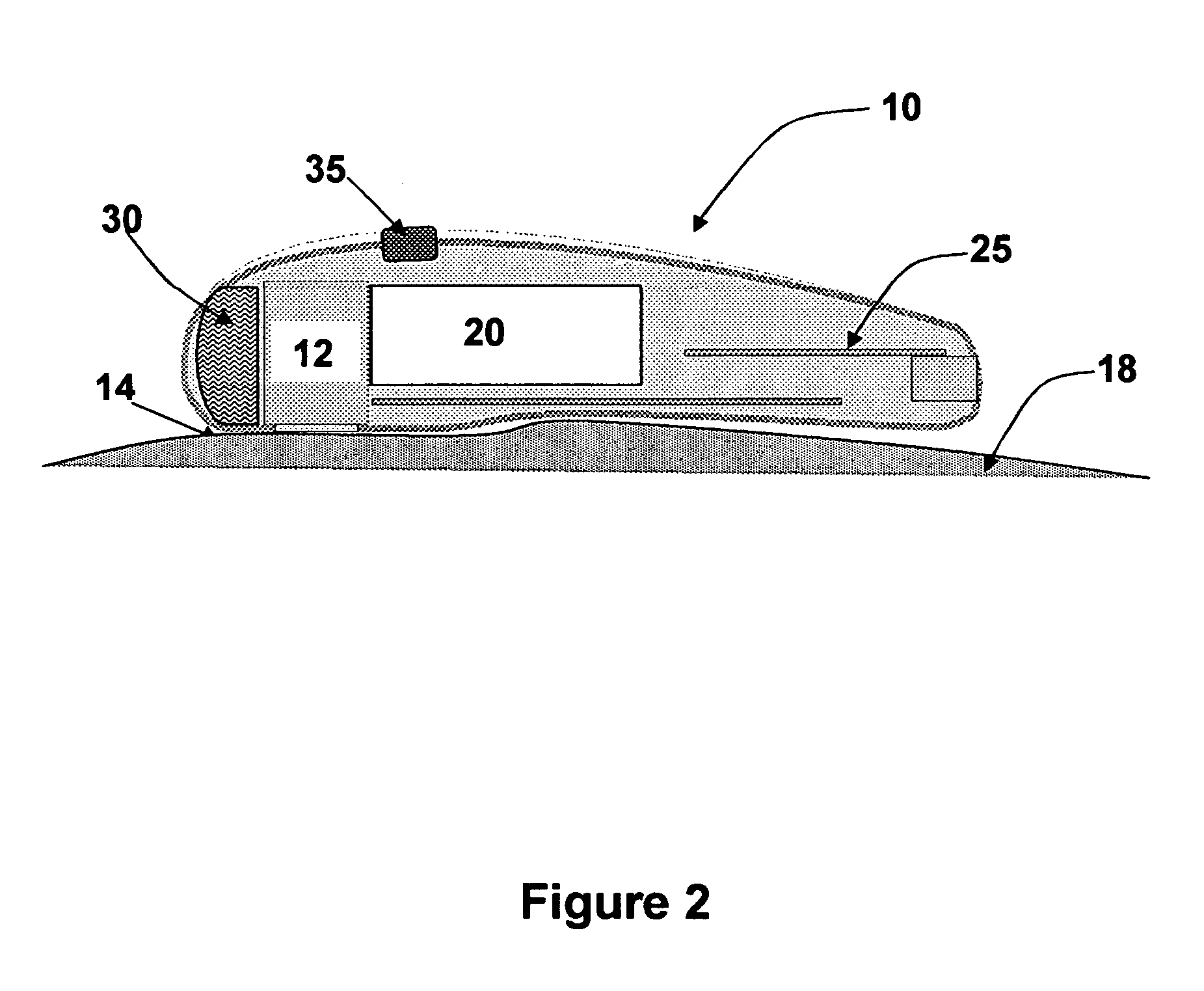
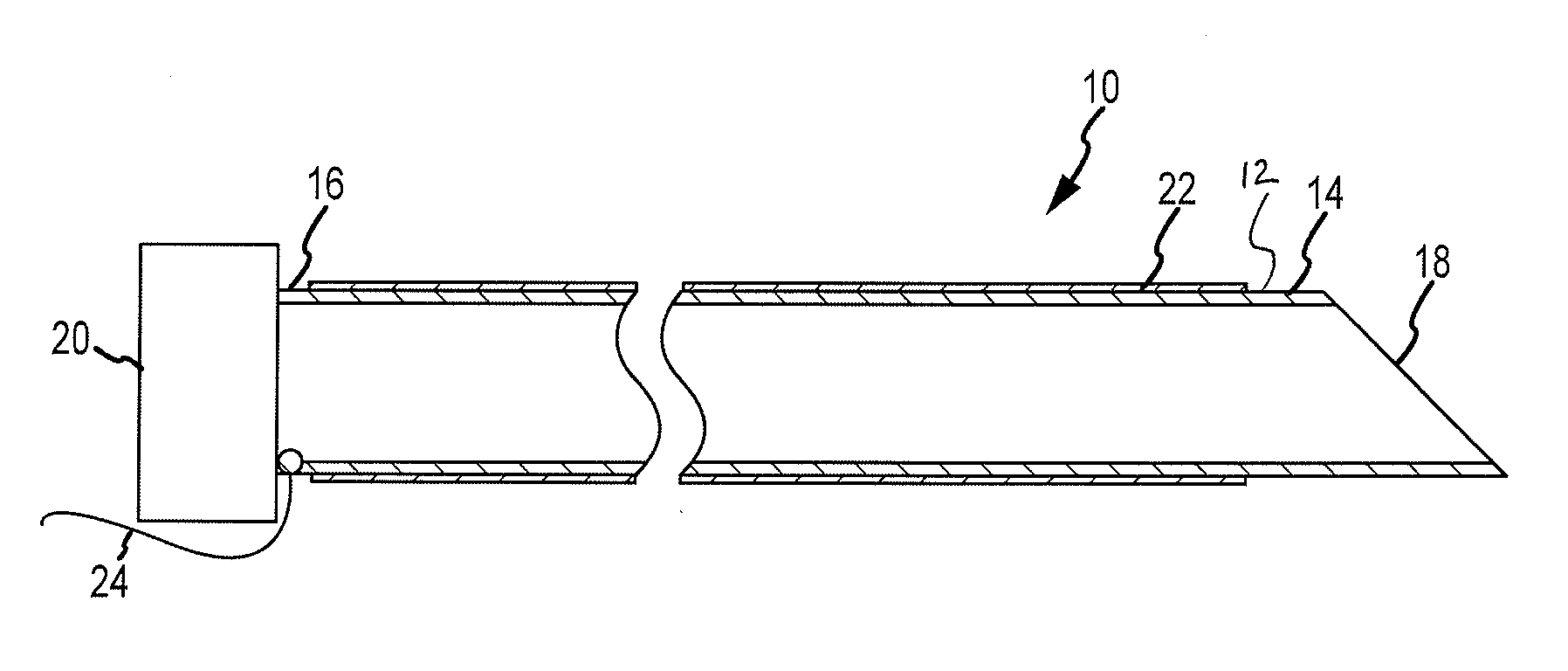
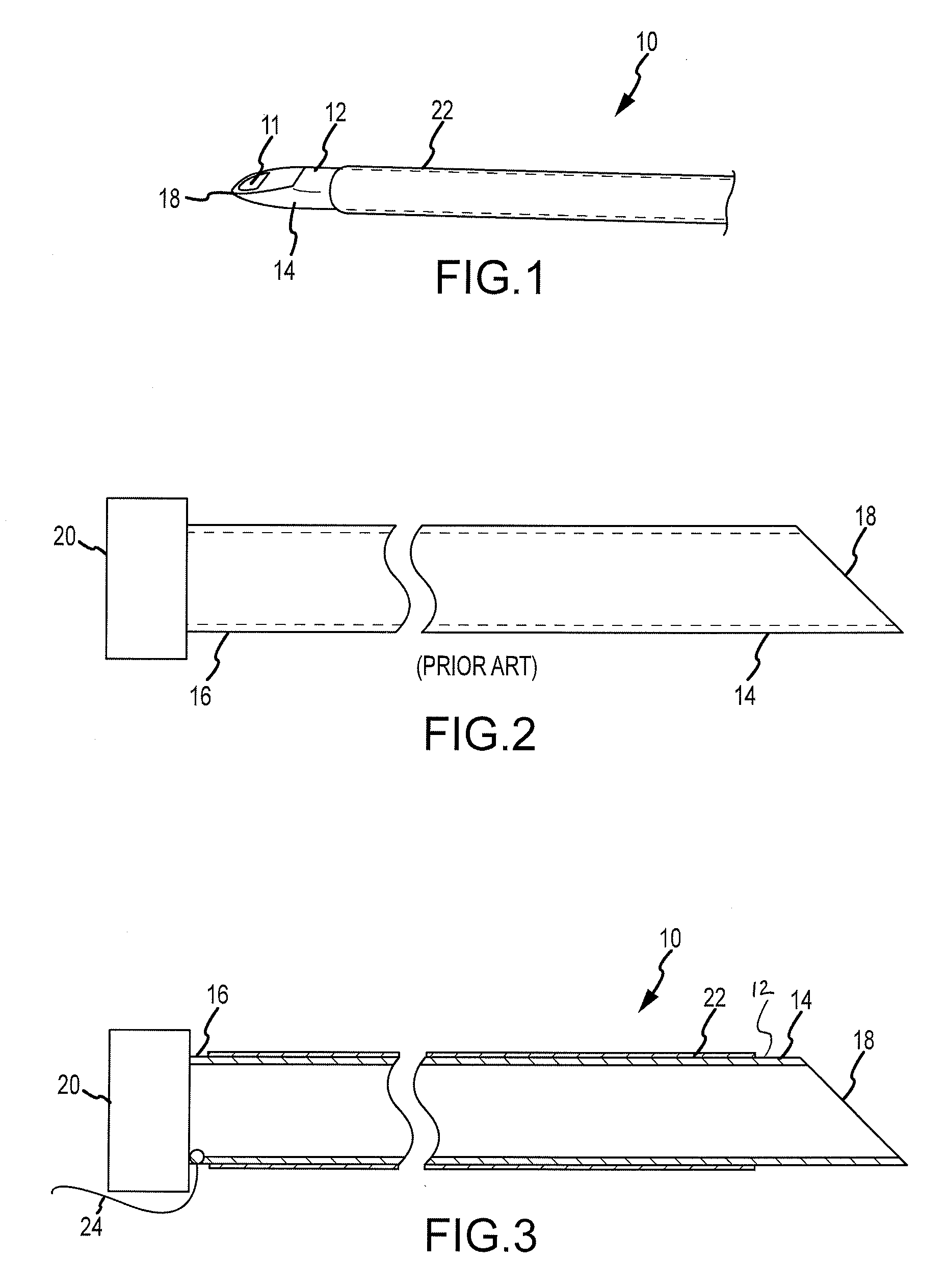
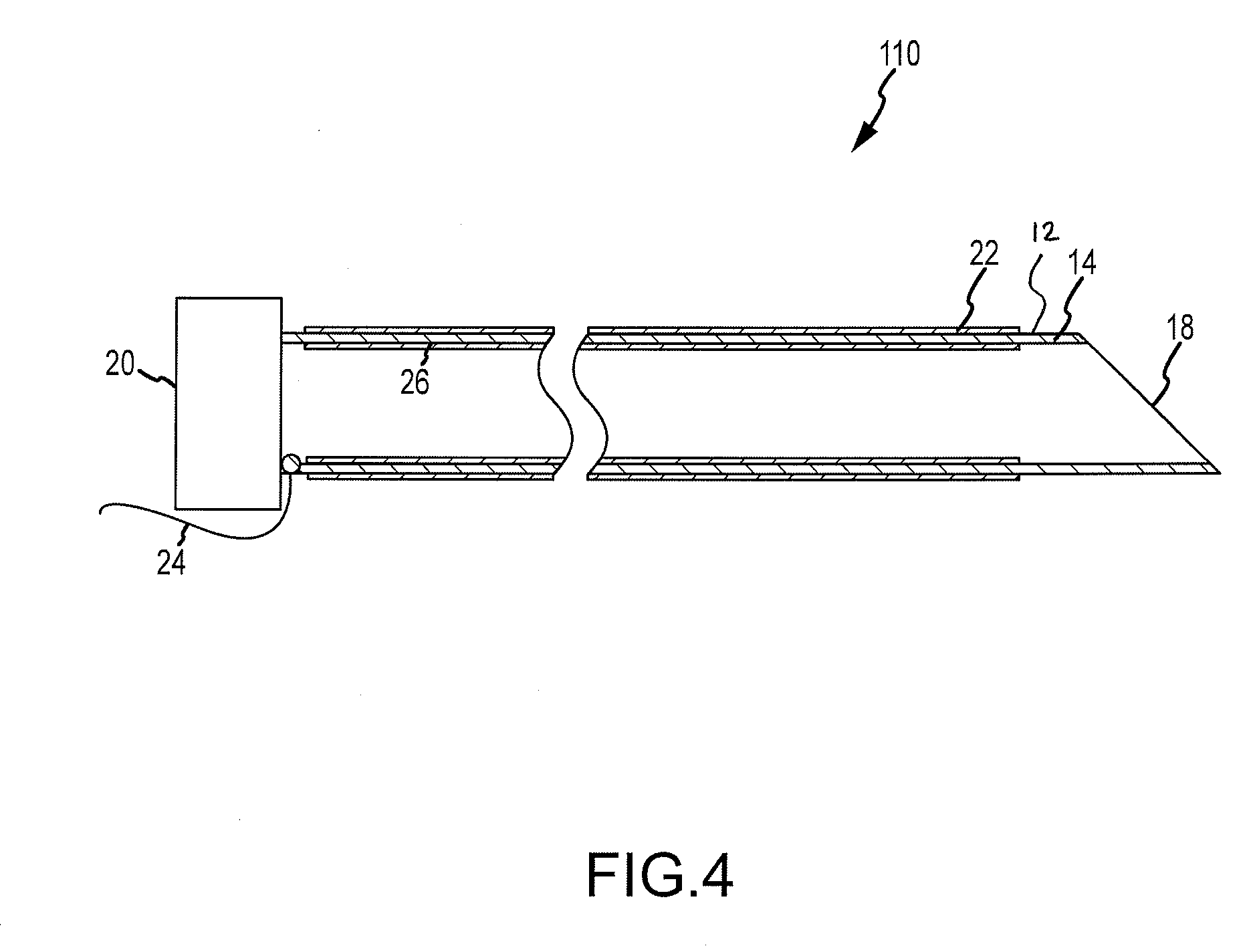
Laparoscopic tissue thickness and clamp load measuring devices
A surgical instrument having opposed jaws that can be selectively moved between open and closed positions. Various embodiments include components for measuring the thickness of tissue clamped between the opposed jaws. Some embodiments are configured to ascertain the amount of compressive force that is being applied to the tissue while the thickness of the tissue is being determined. The tissue thickness data is displayed on the instrument itself and / or on a display that is remote from the instrument. The various embodiments may comprise different types of surgical instruments such as surgical staplers and graspers. A jaw arrangement with jaws shaped to define a cradle that corresponds to a cross-sectional shape of an object is also disclosed. The components that generate the thickness data may be electrically or mechanically actuated.
Owner:CILAG GMBH INT
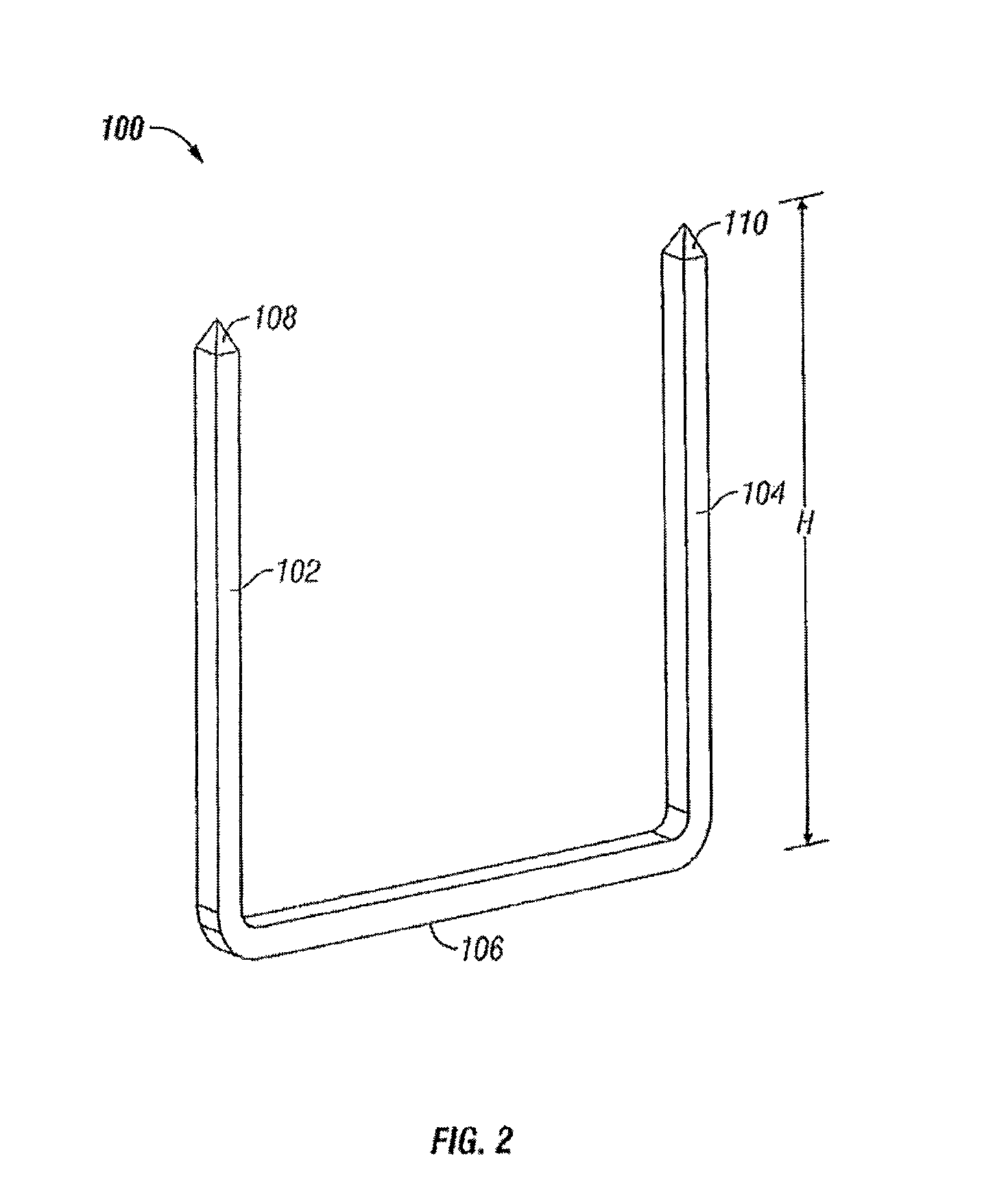
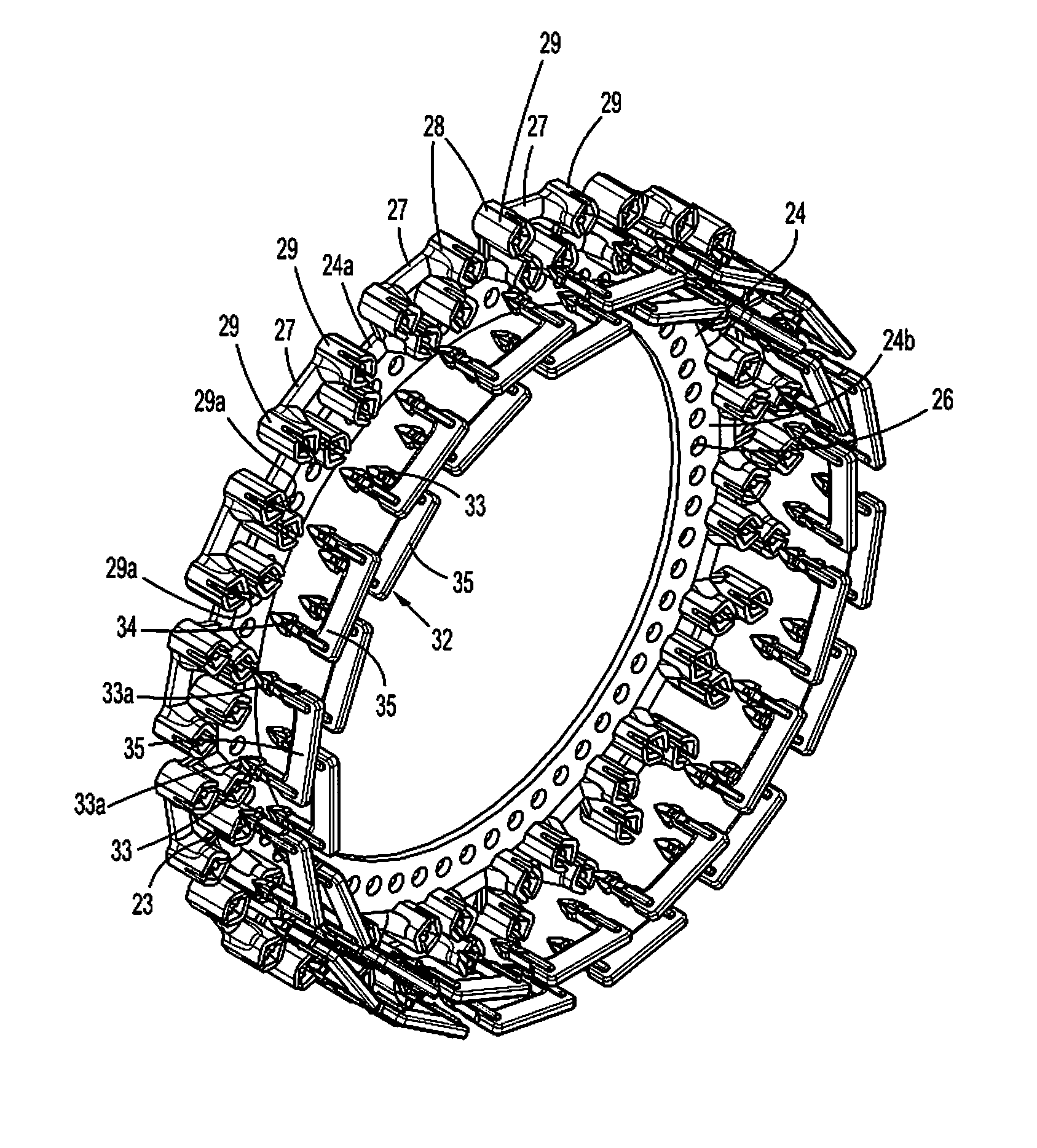
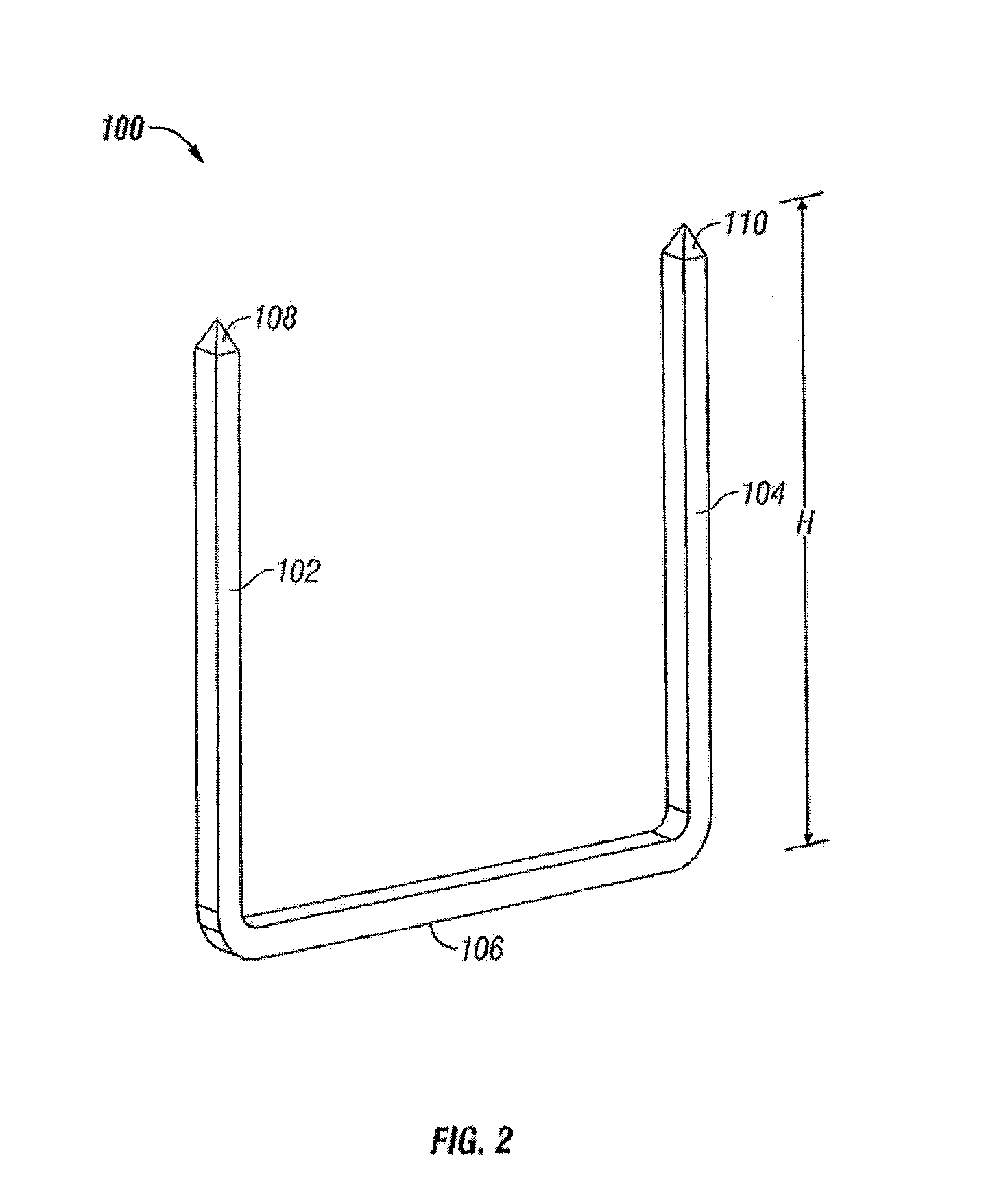
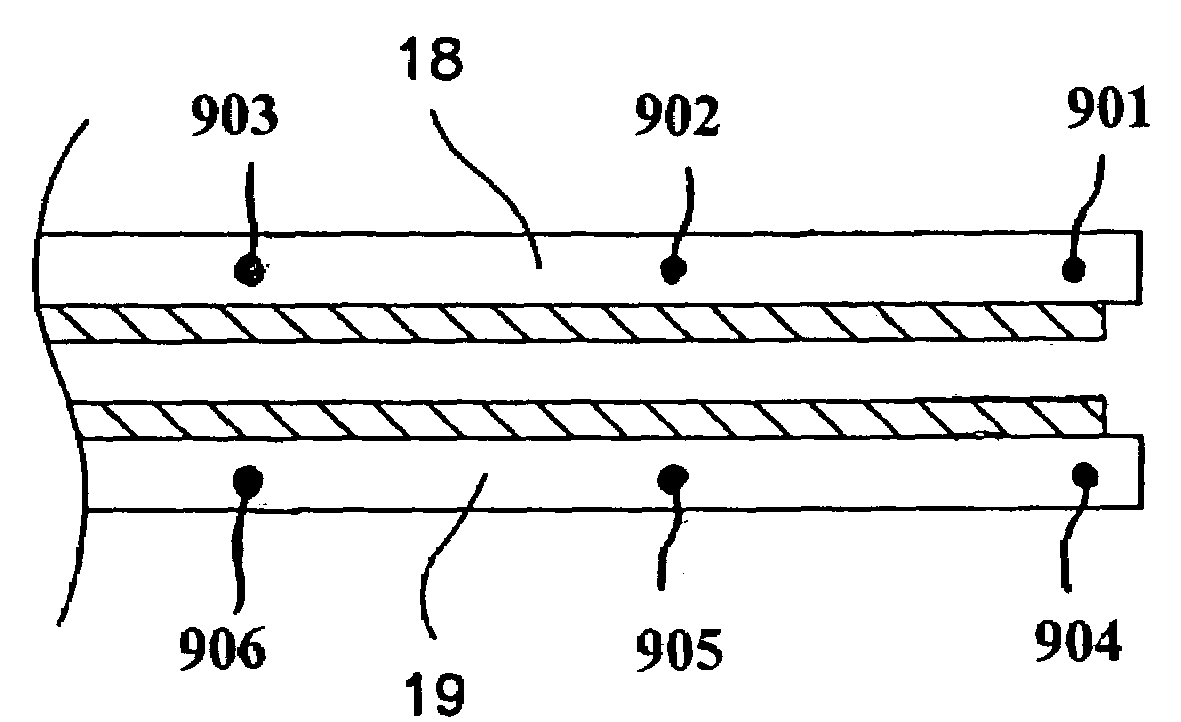
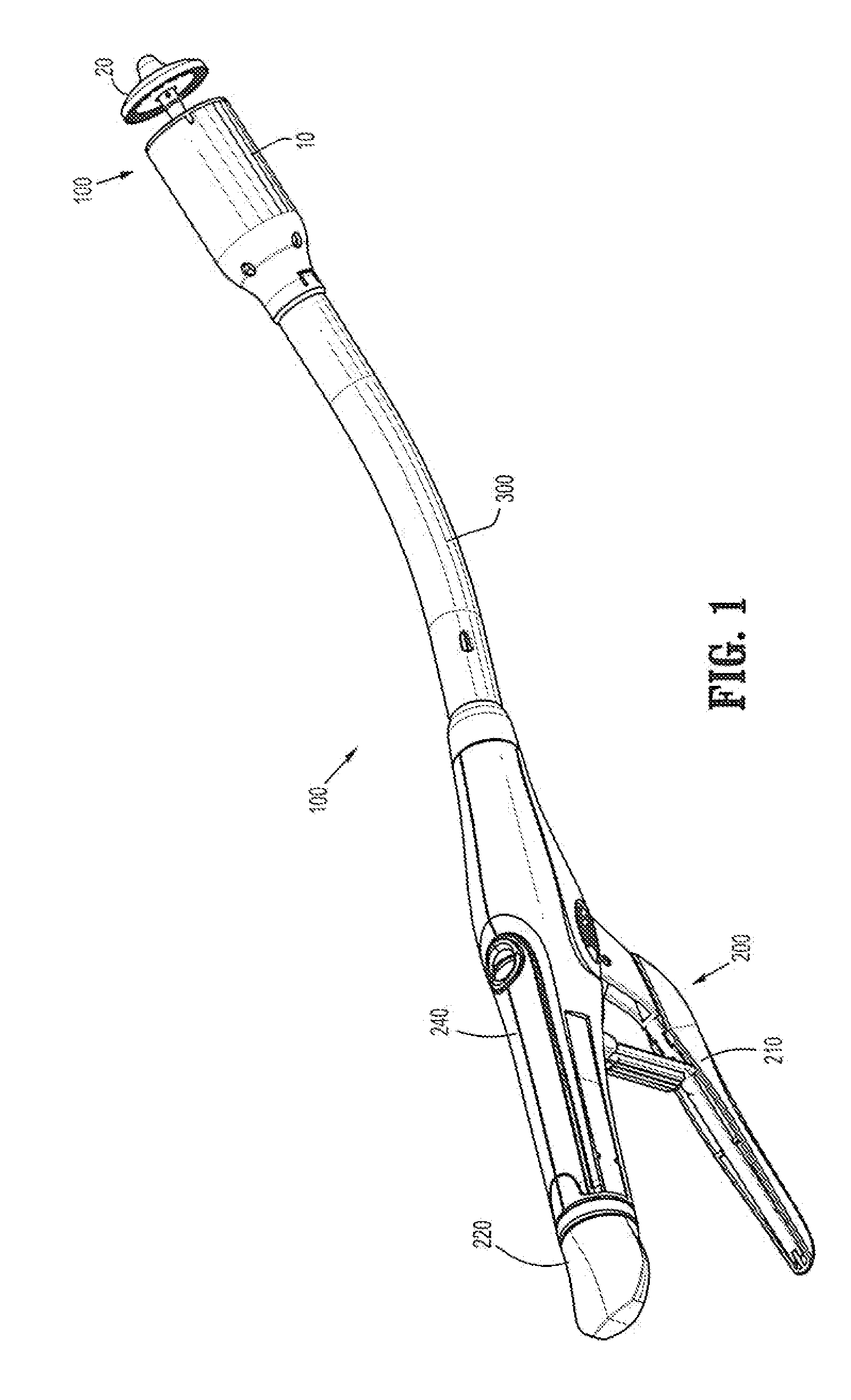
Surgical fastening apparatus
A surgical fastening apparatus including a fastener receiving frame including a plurality of spaced apart openings formed therein and a fastener supporting member containing a plurality of surgical fasteners extending therefrom. The surgical fasteners are engagable with the plurality of openings to mate with the fastener receiving frame to fasten tissue therebetween. The fasteners are engageable with the openings in a plurality of positions dependent on a tissue thickness between the fastener receiving frame and the fastener supporting member.
Owner:TYCO HEALTHCARE GRP LP
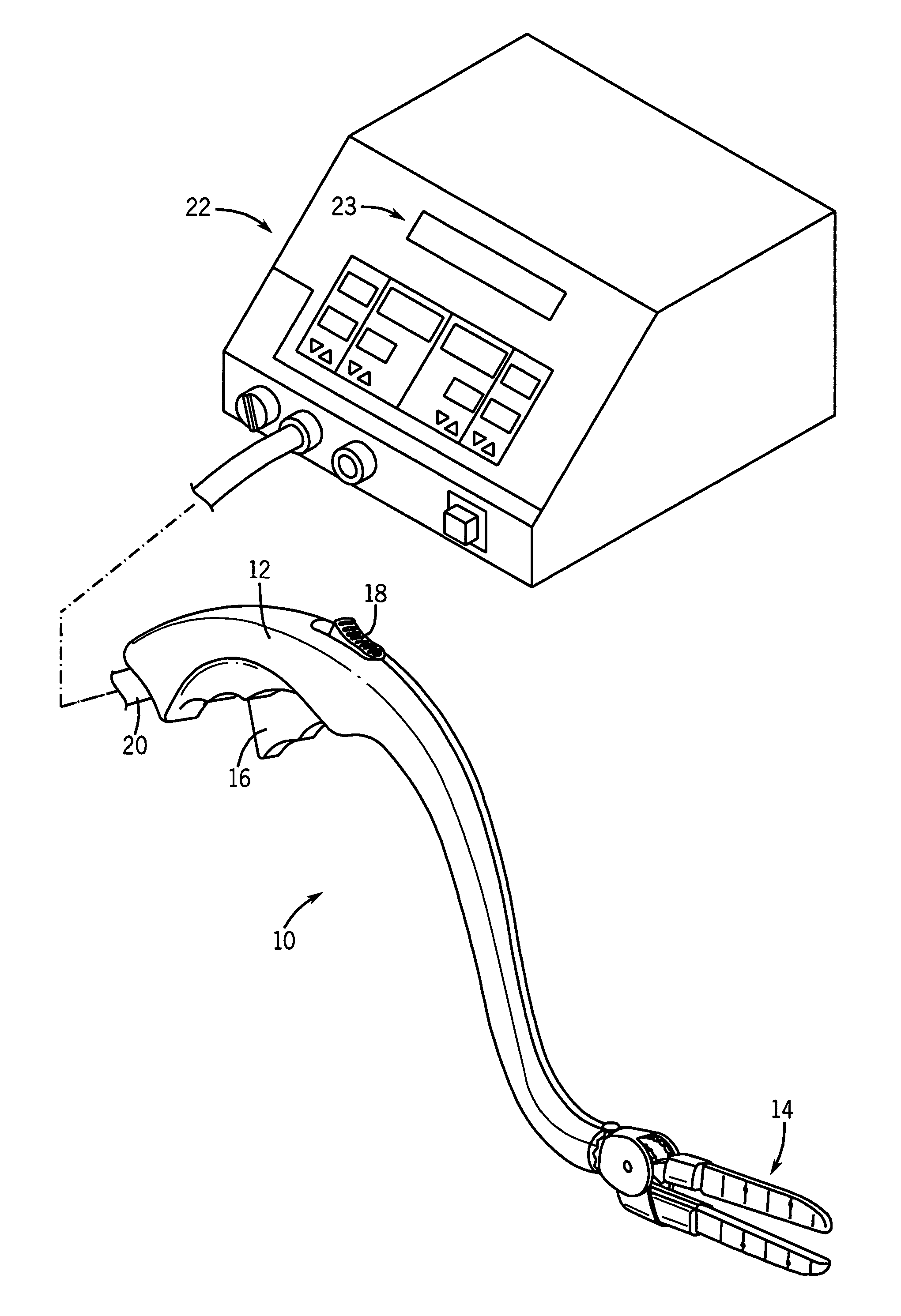
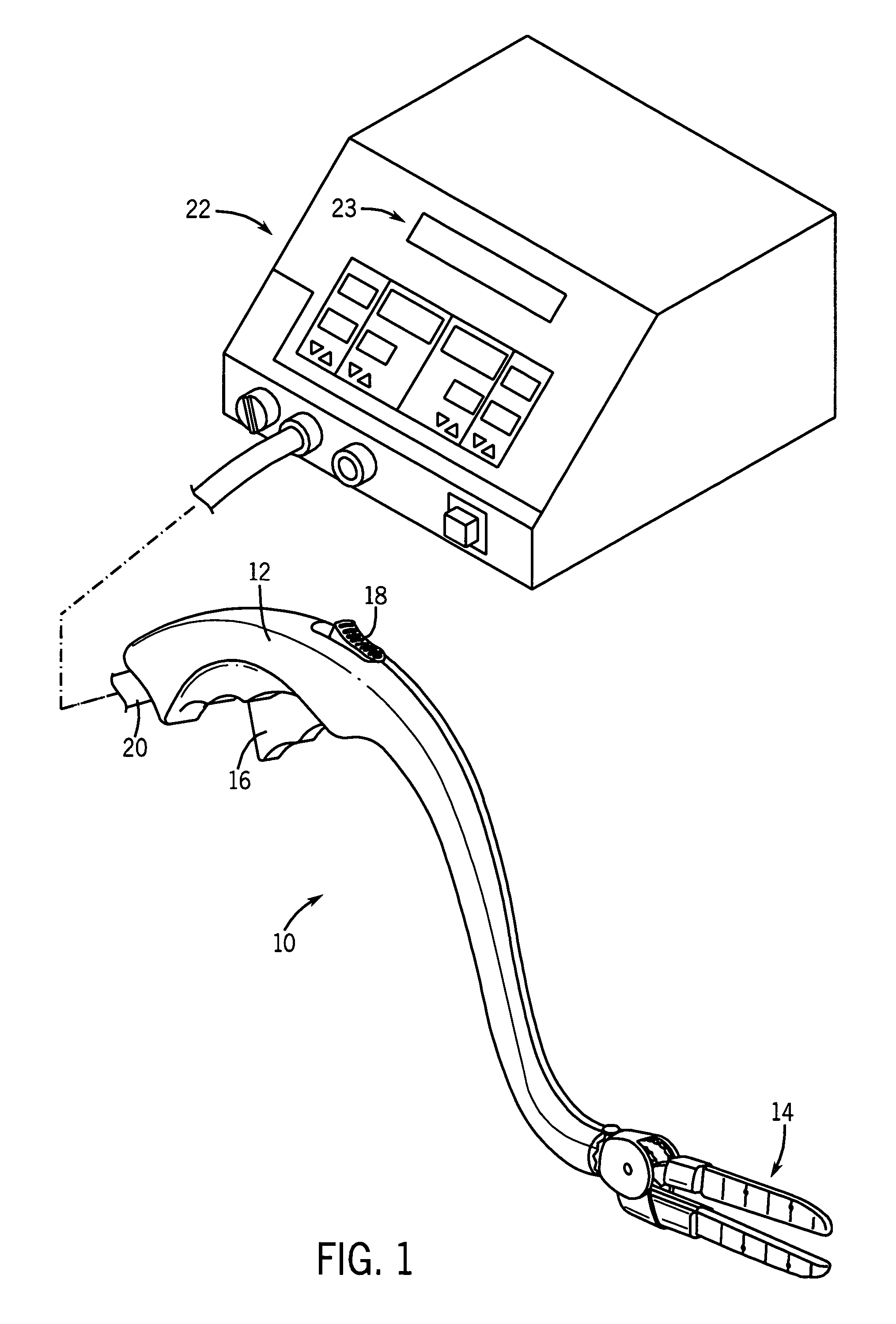
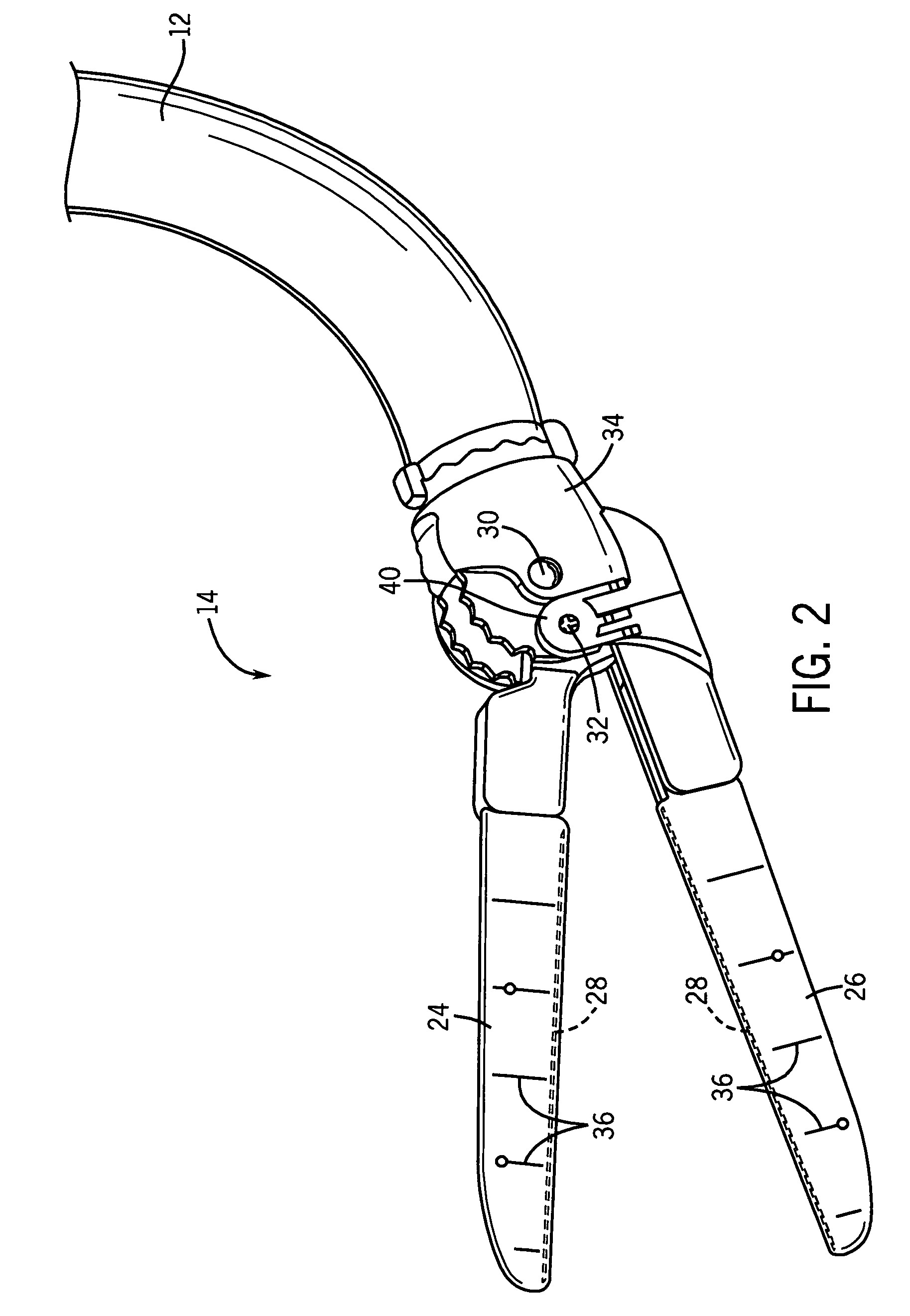
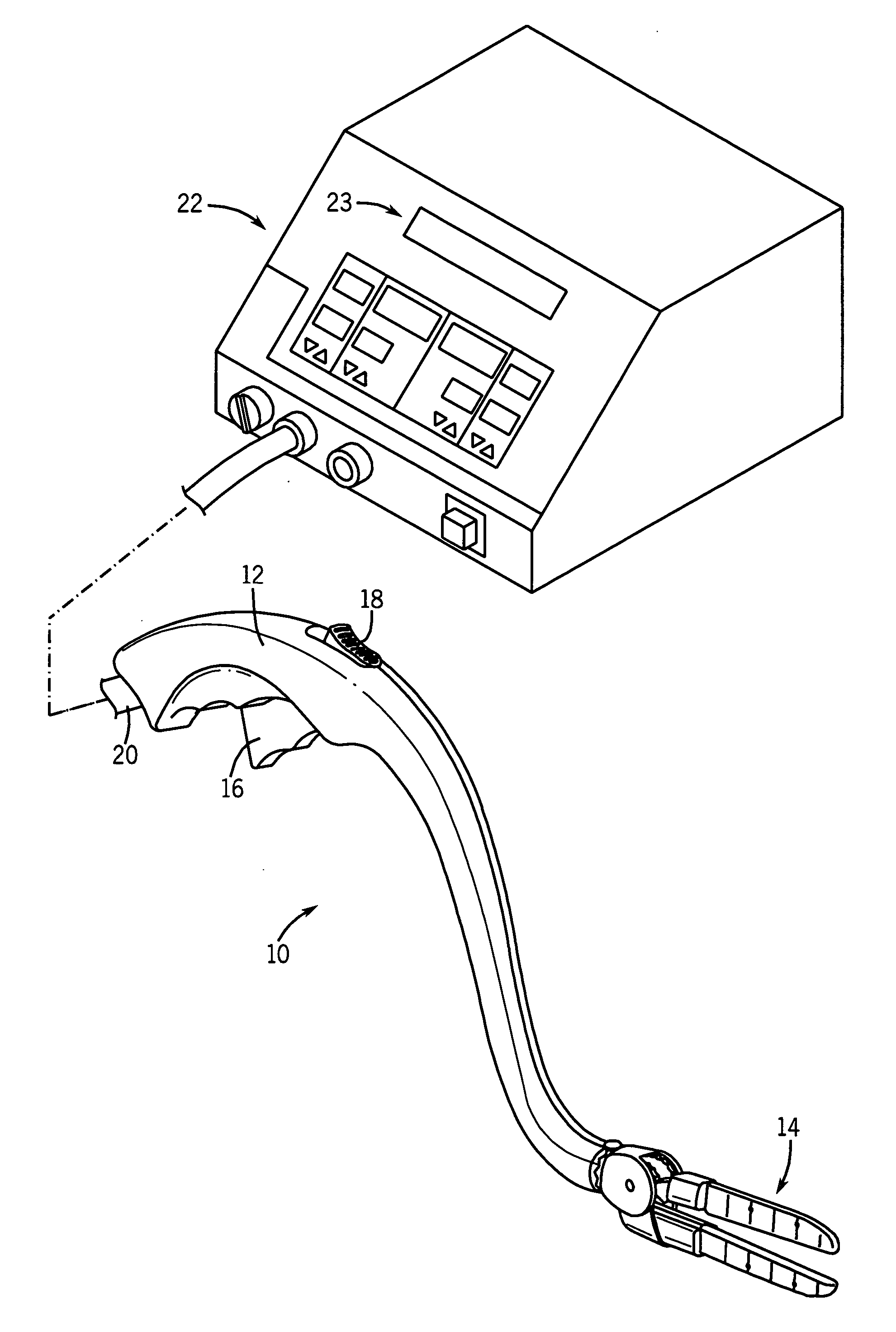
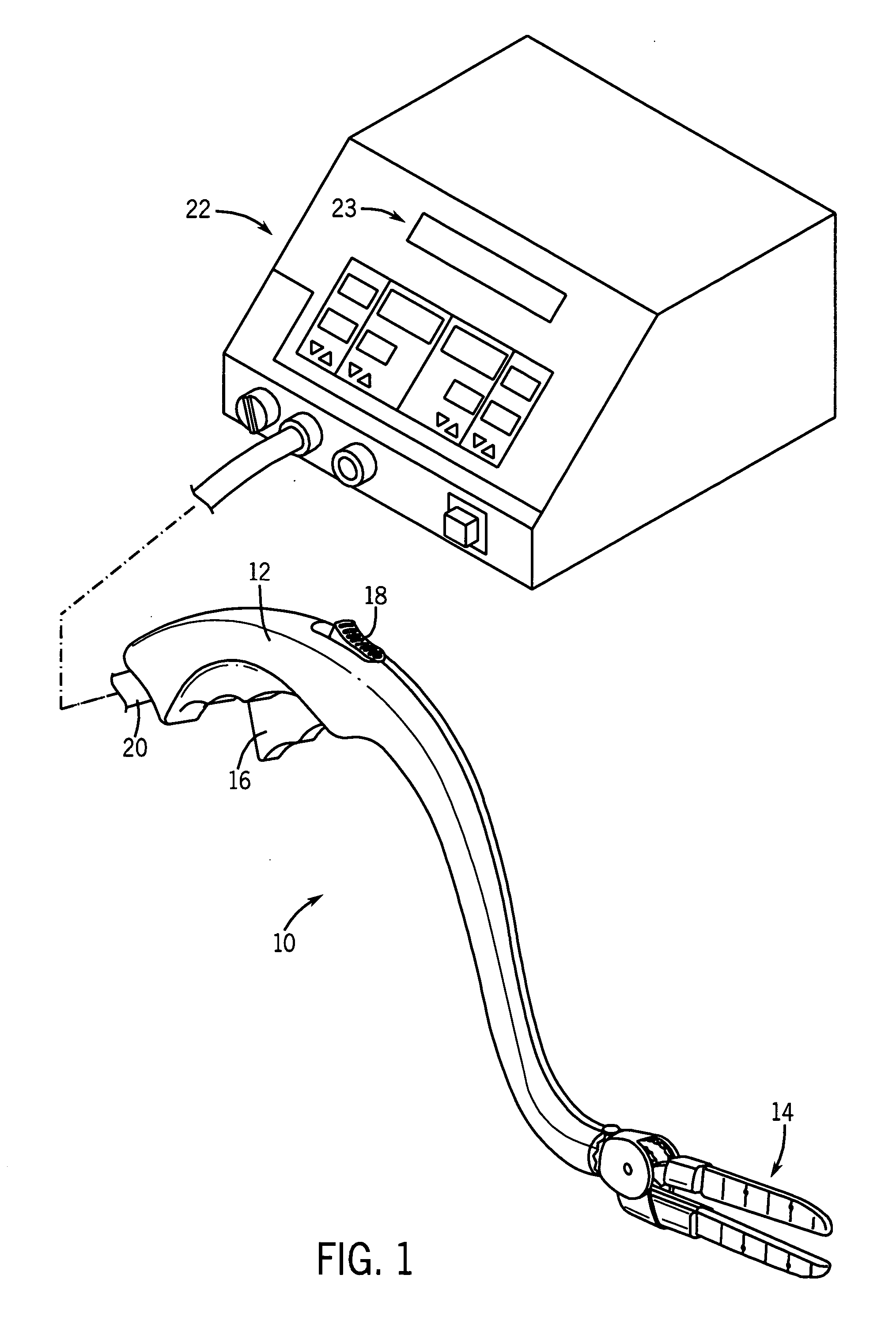
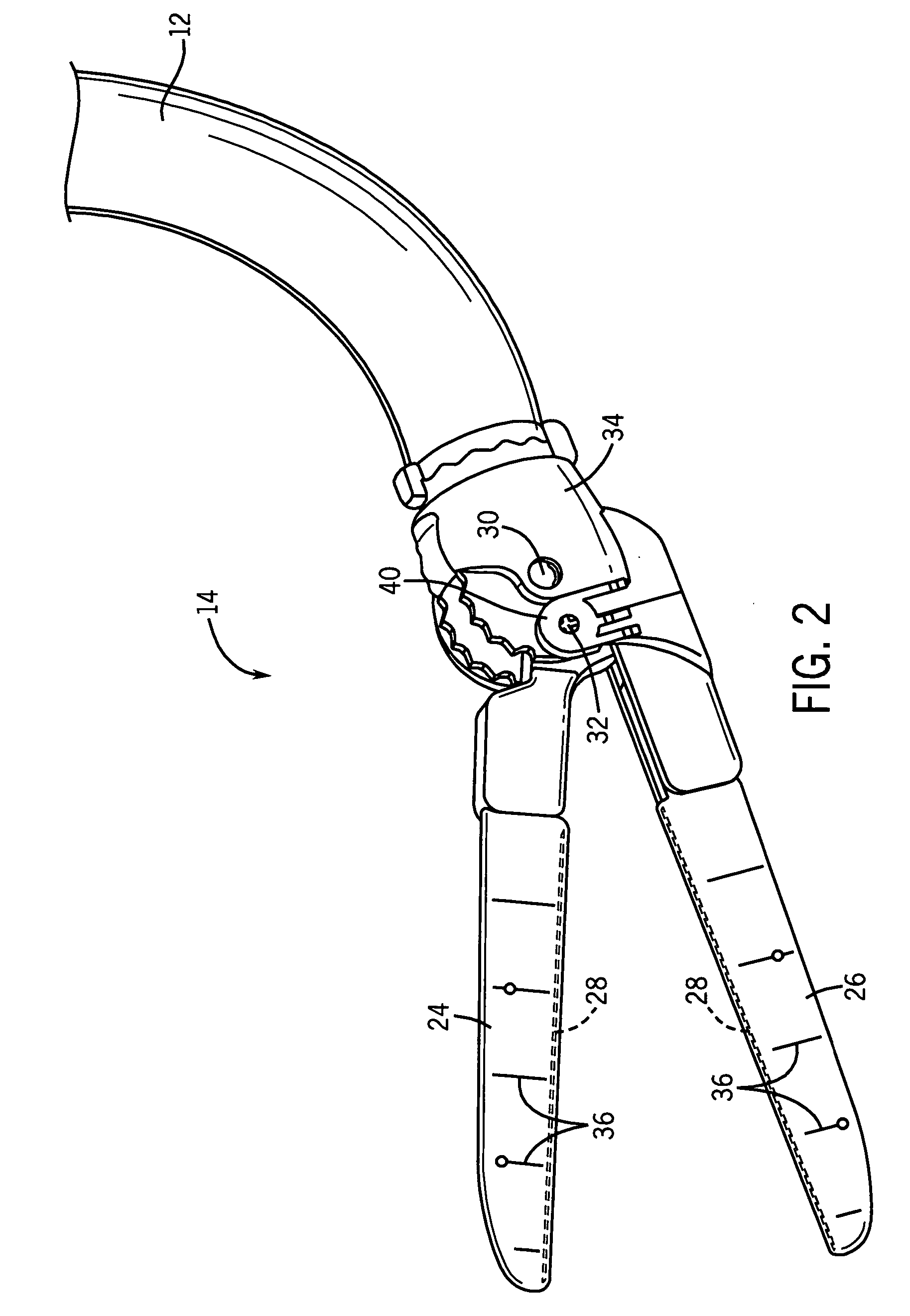
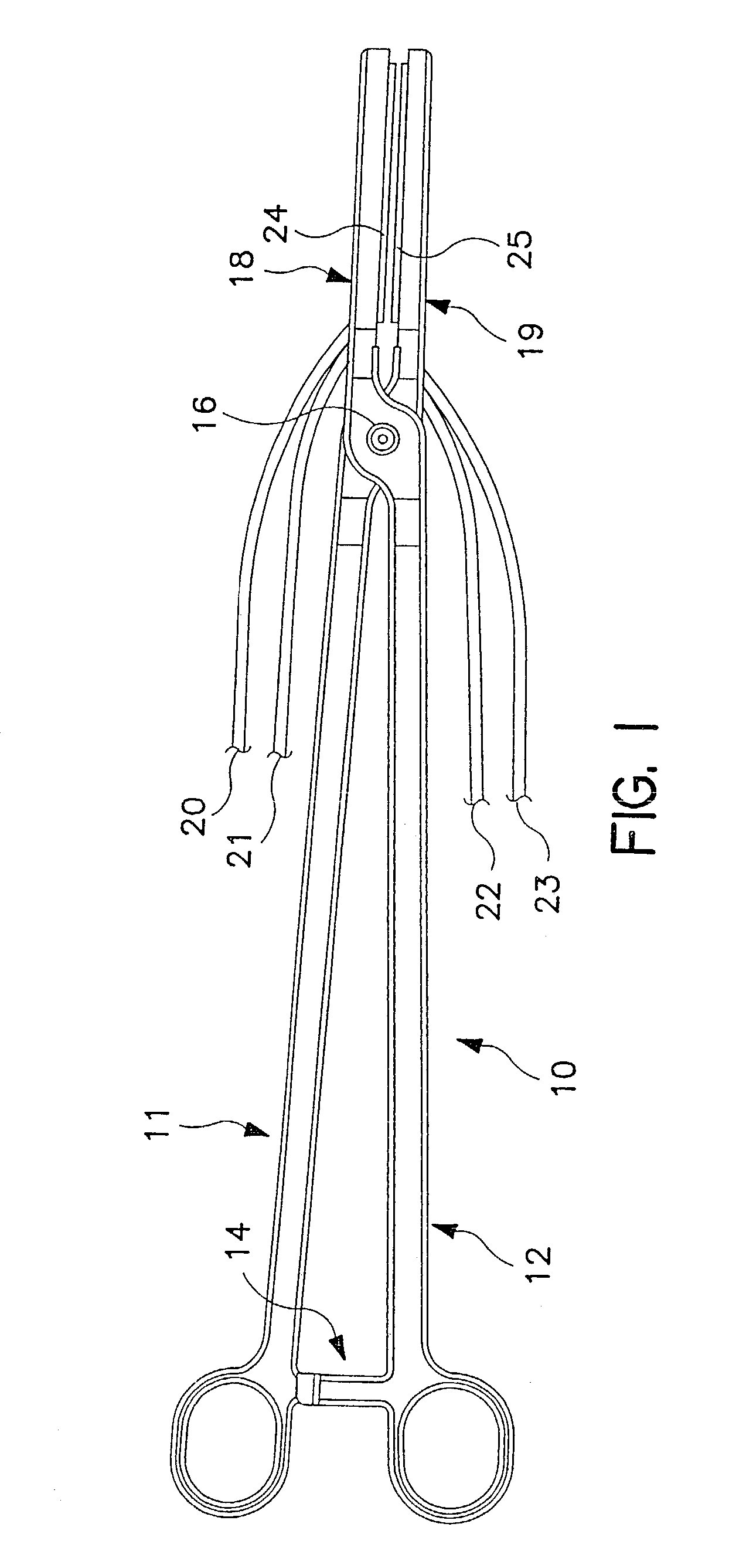
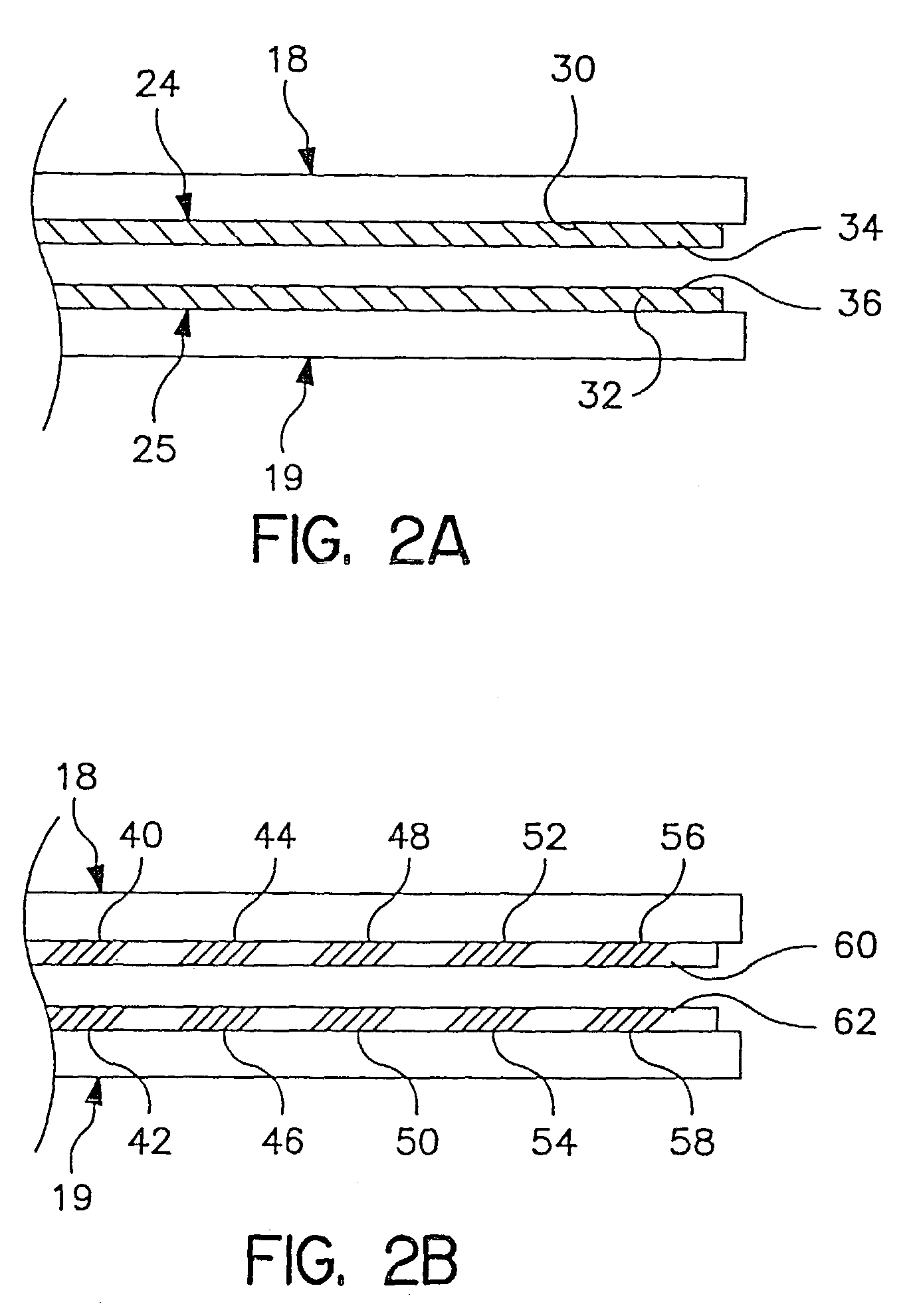
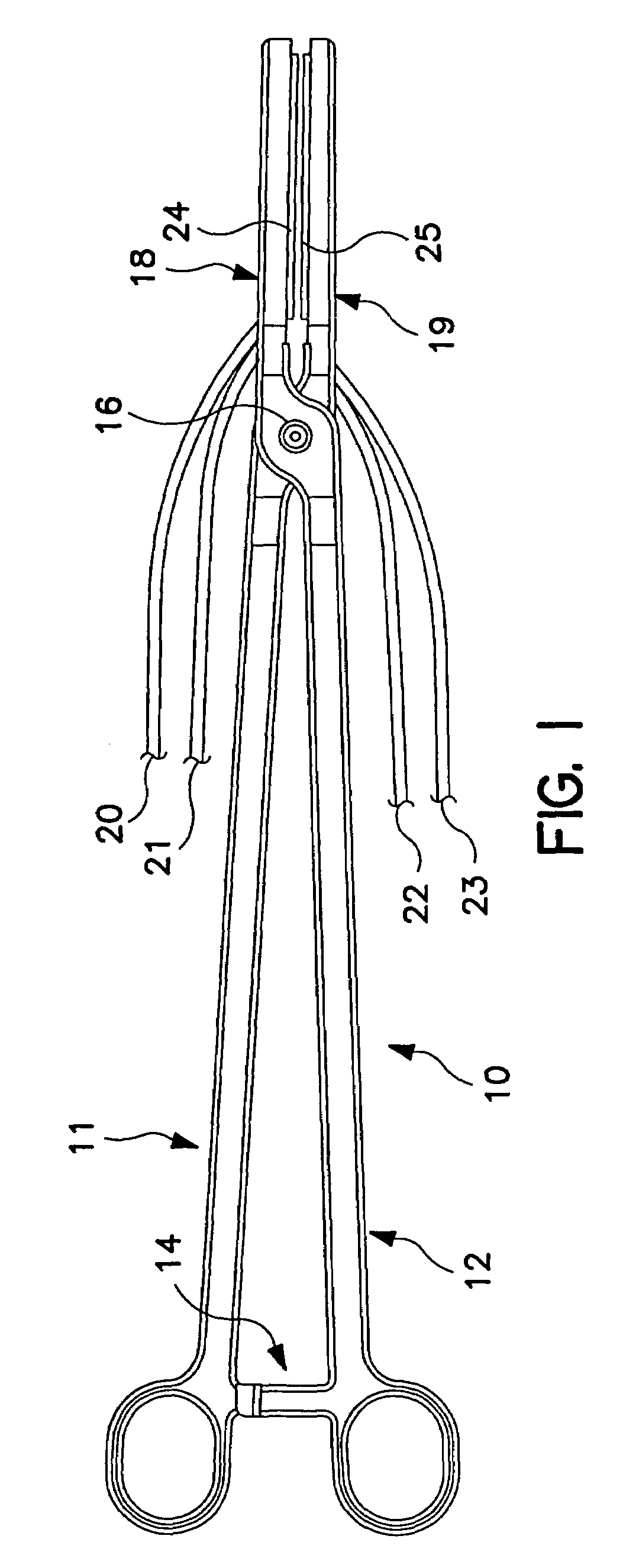
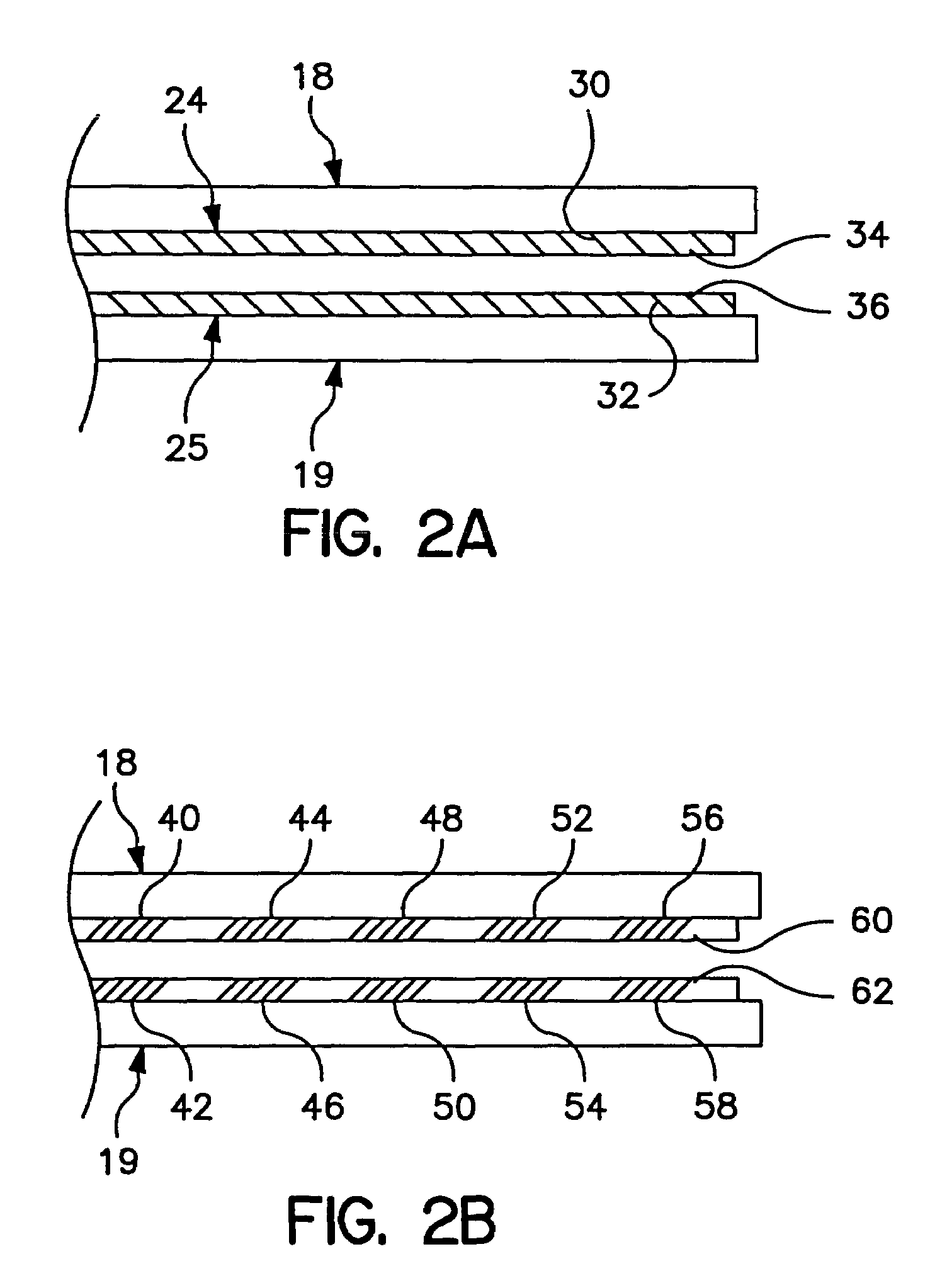
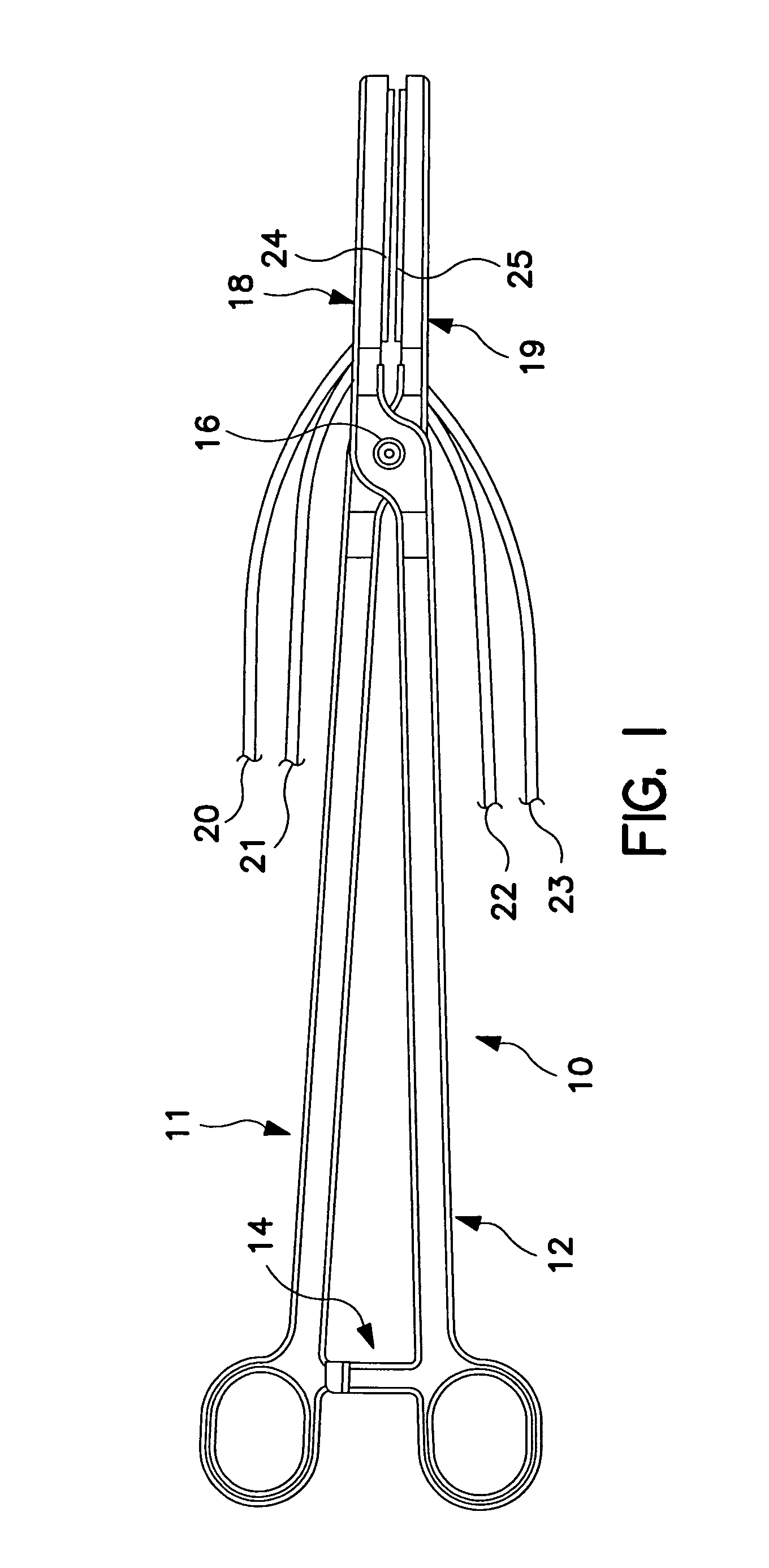
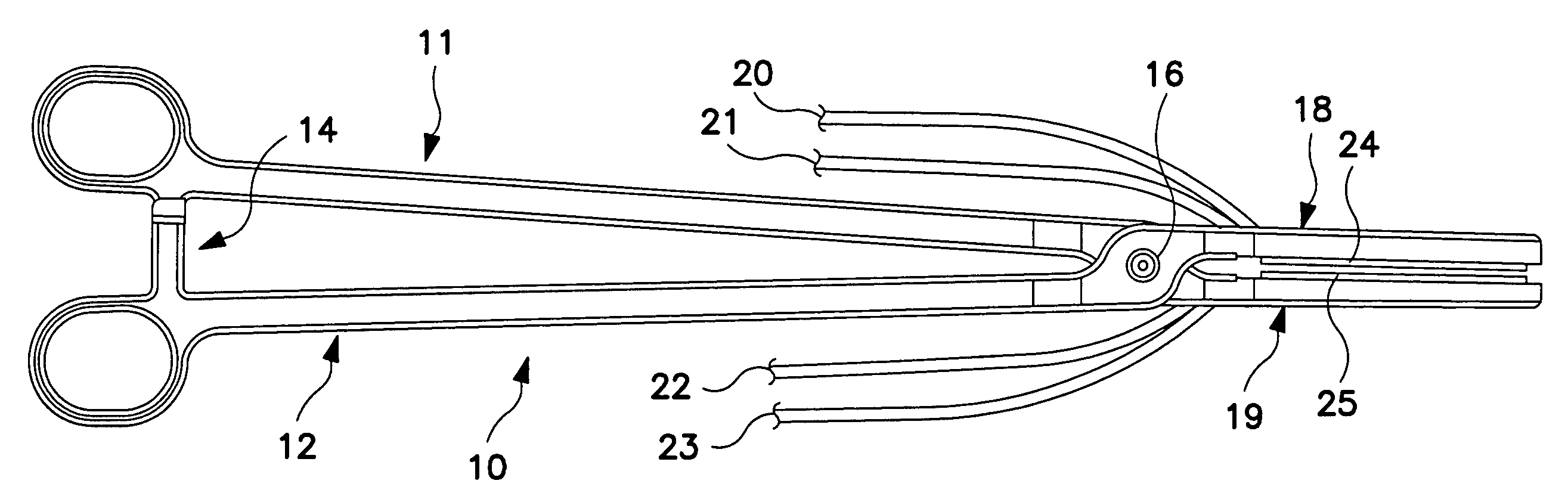
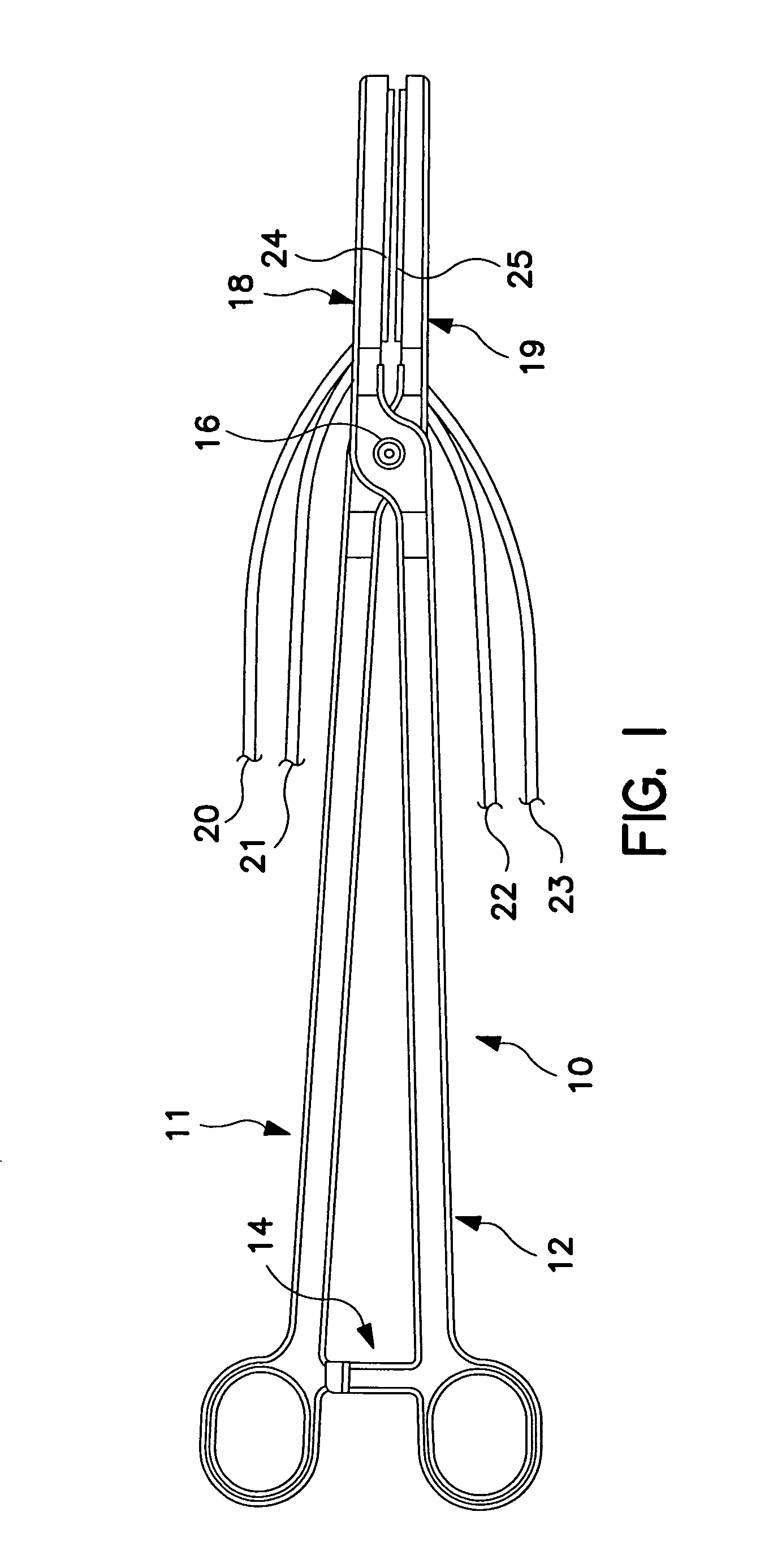
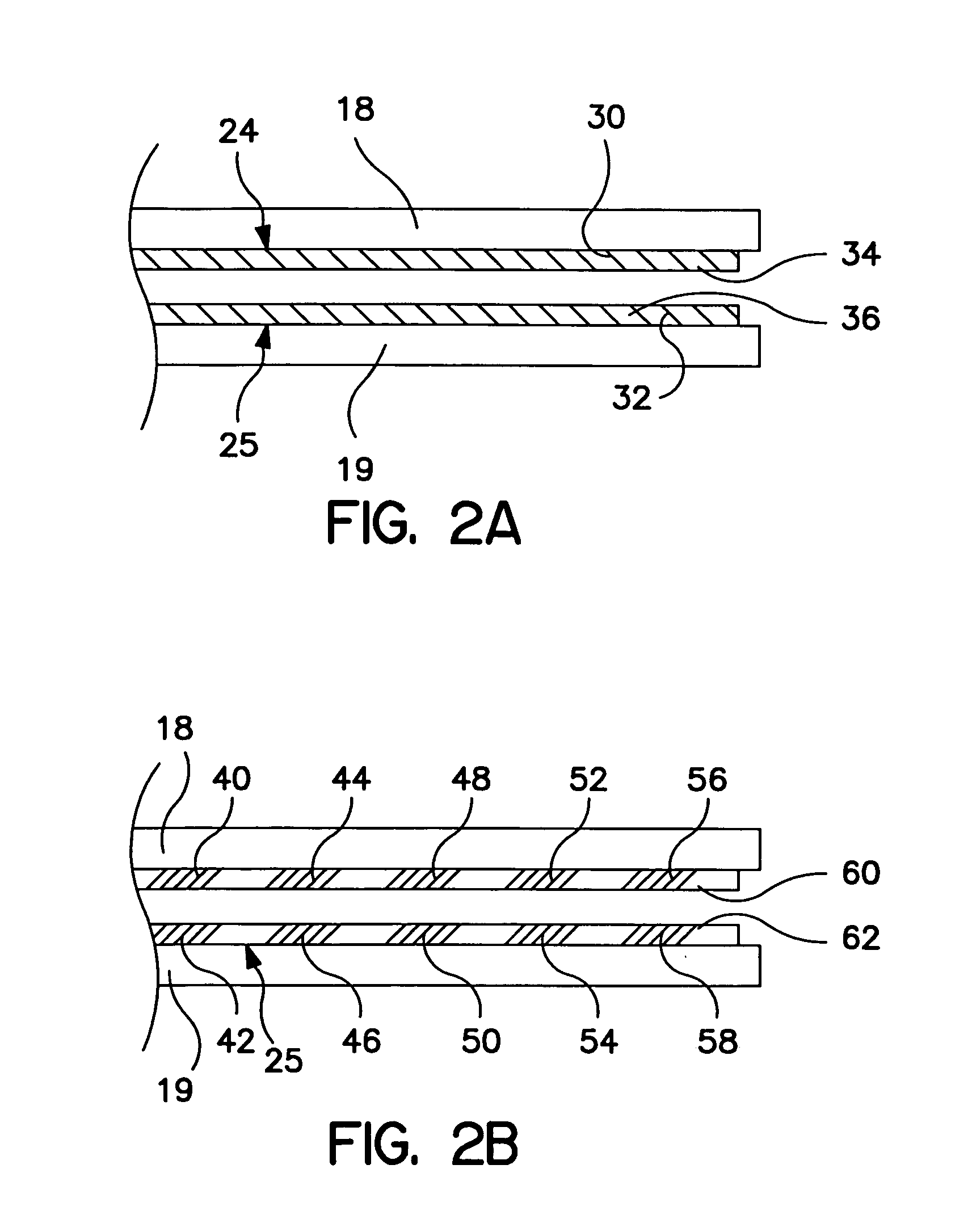
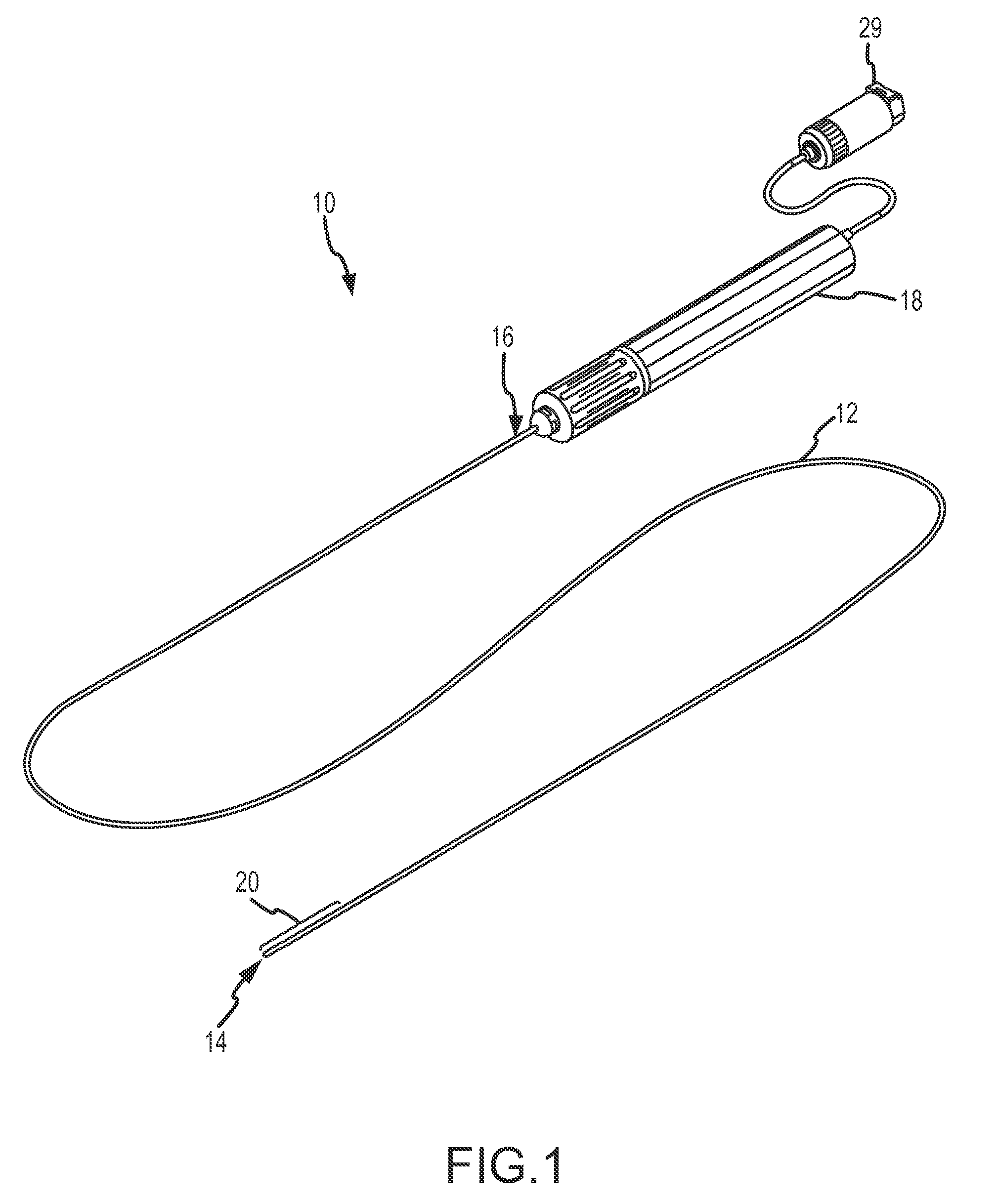
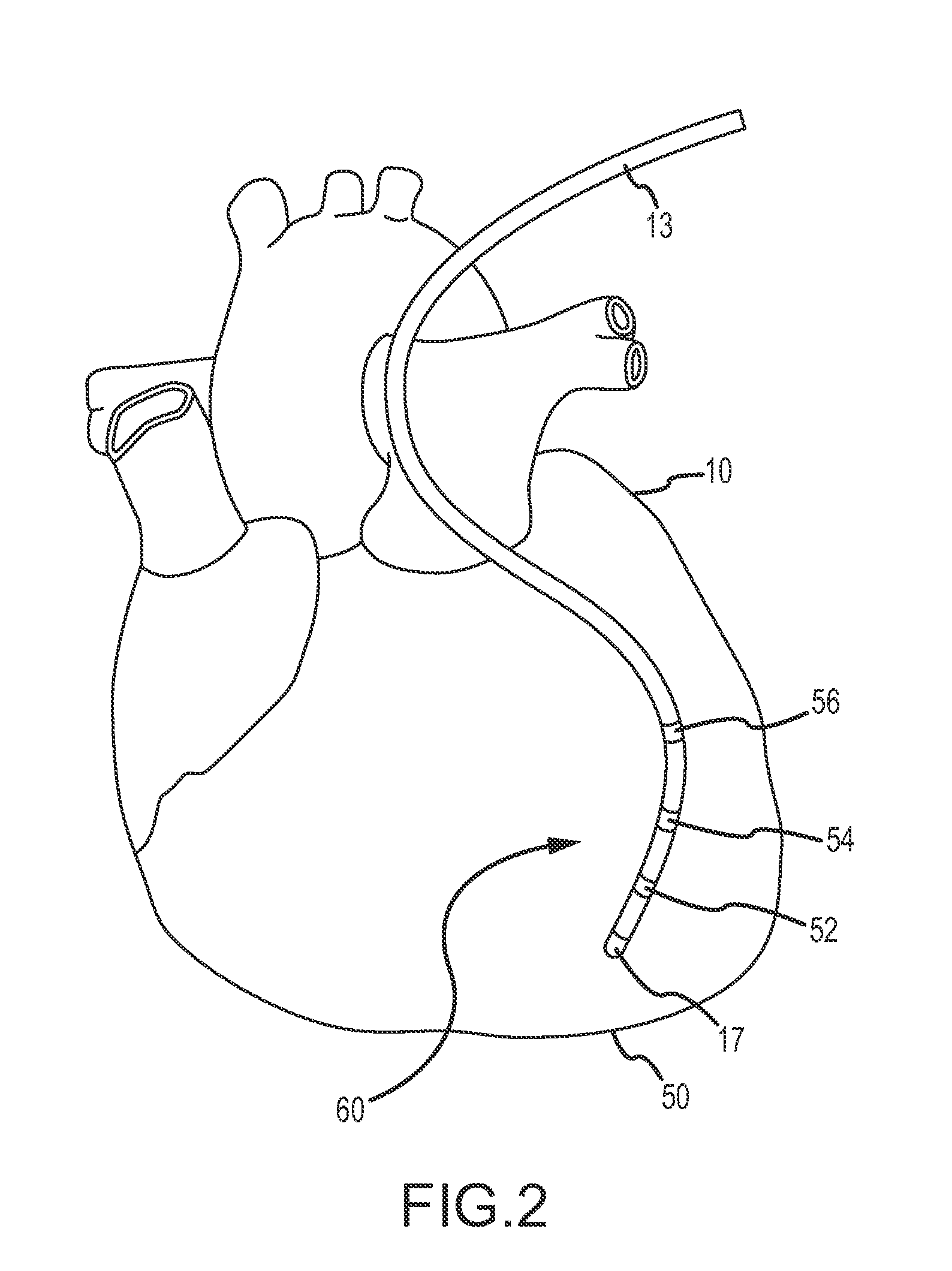
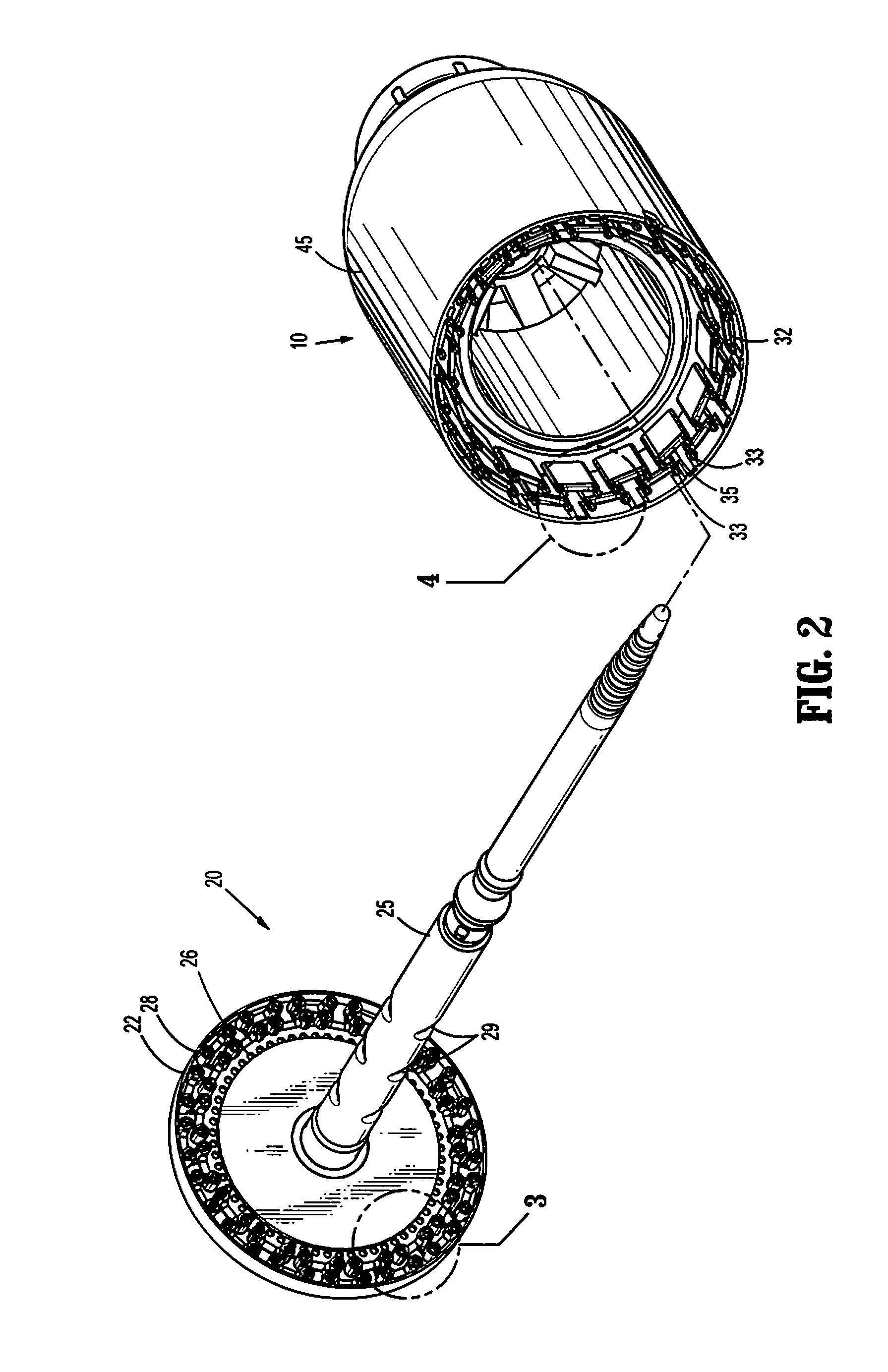
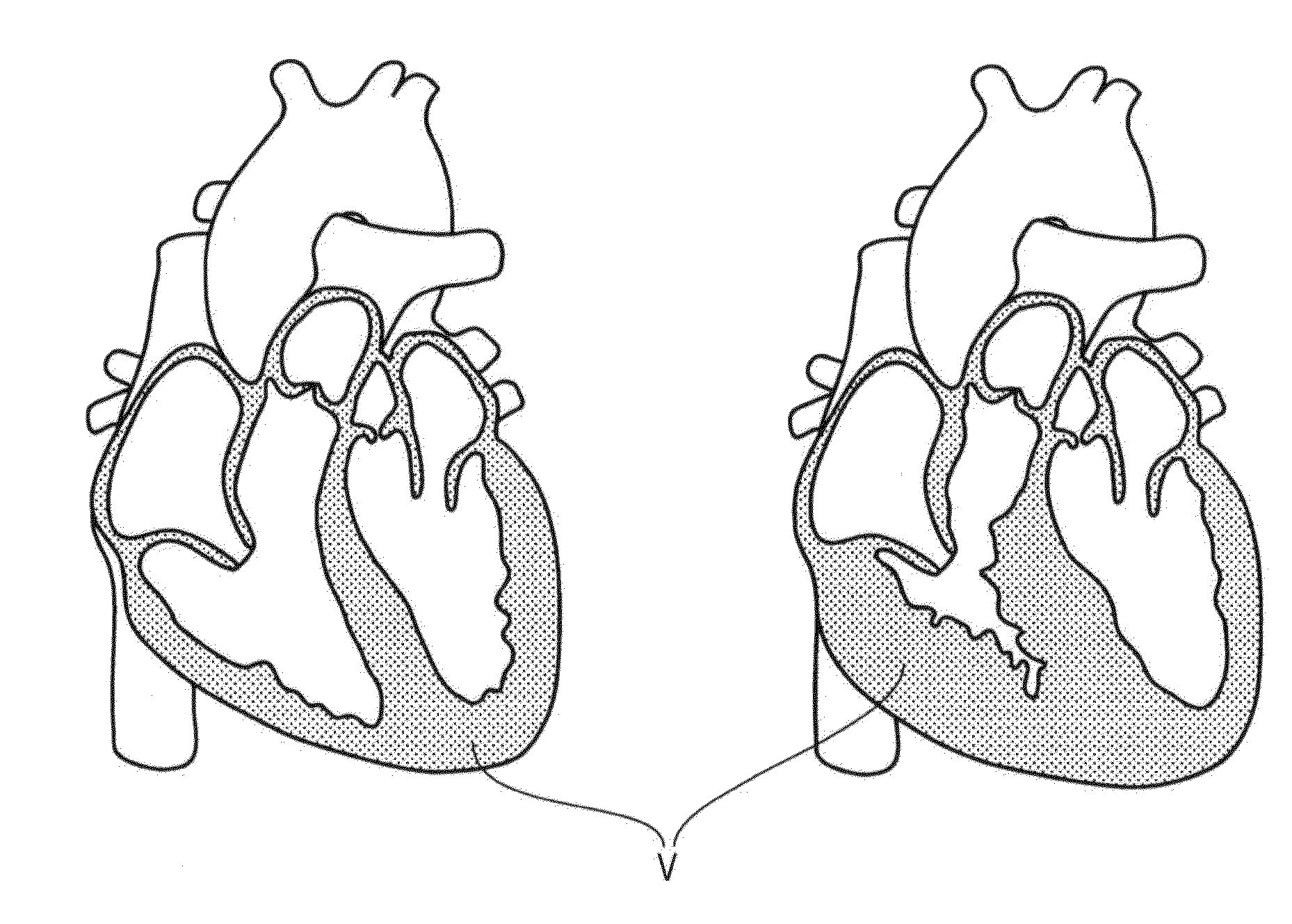
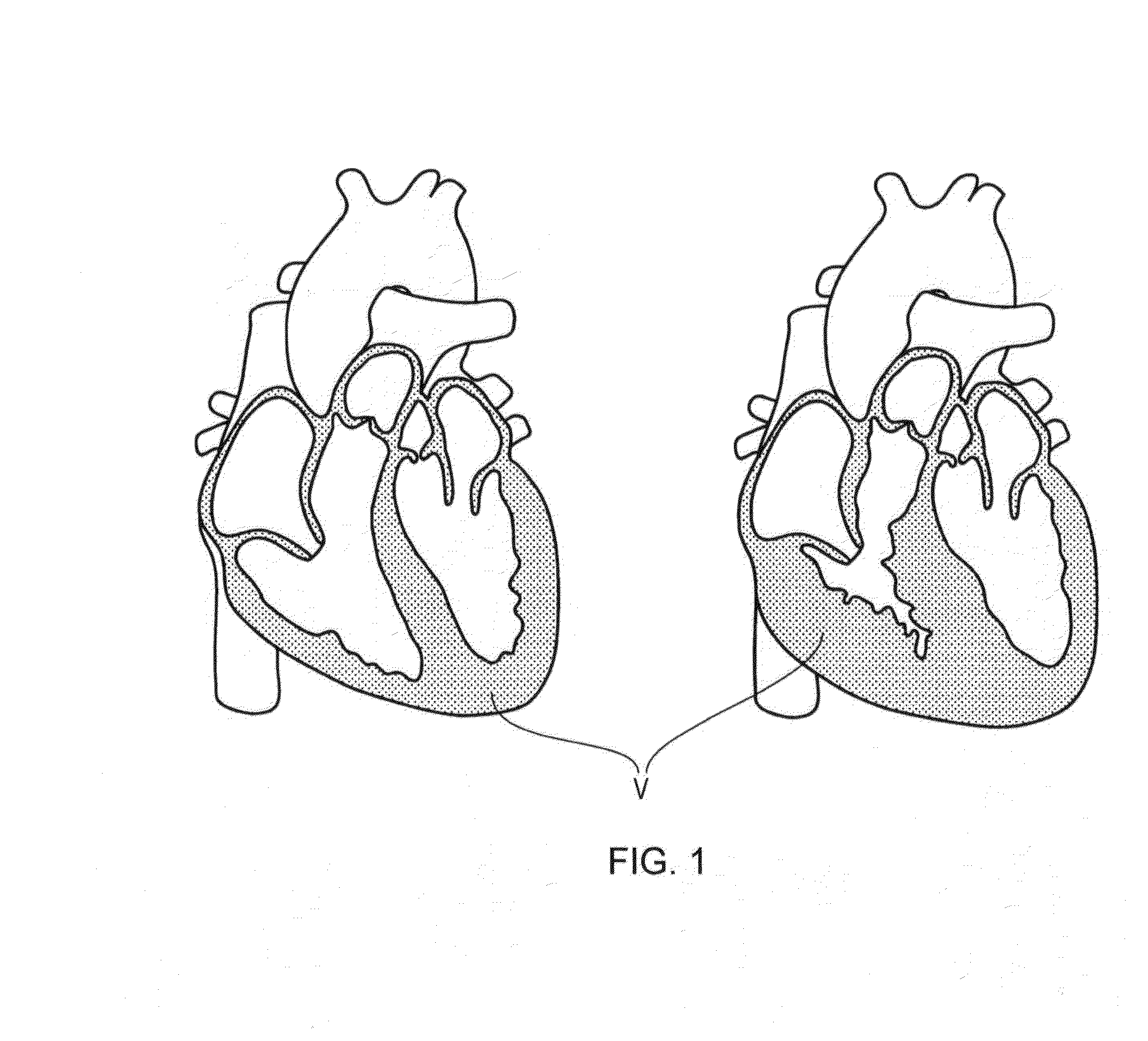
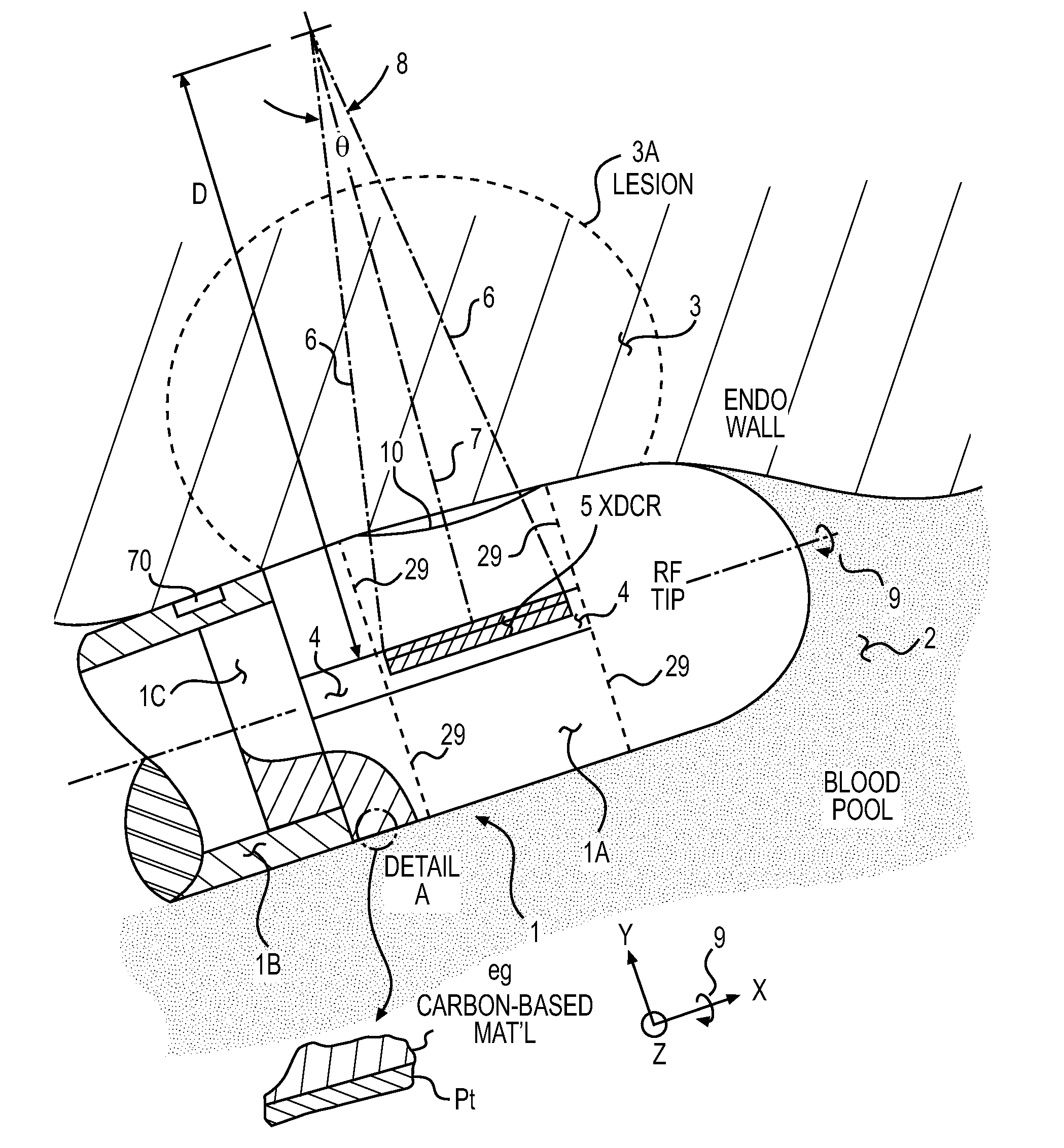
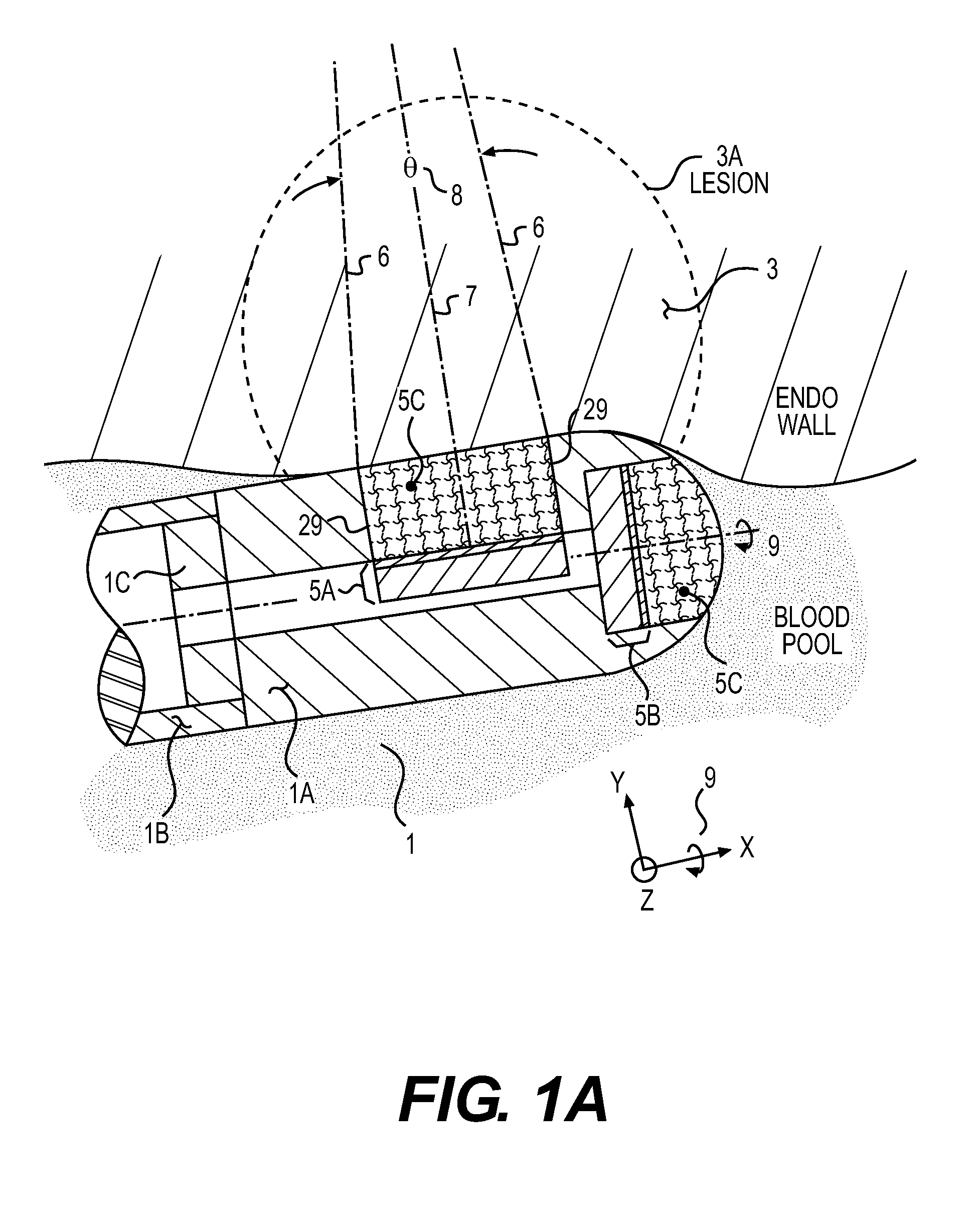
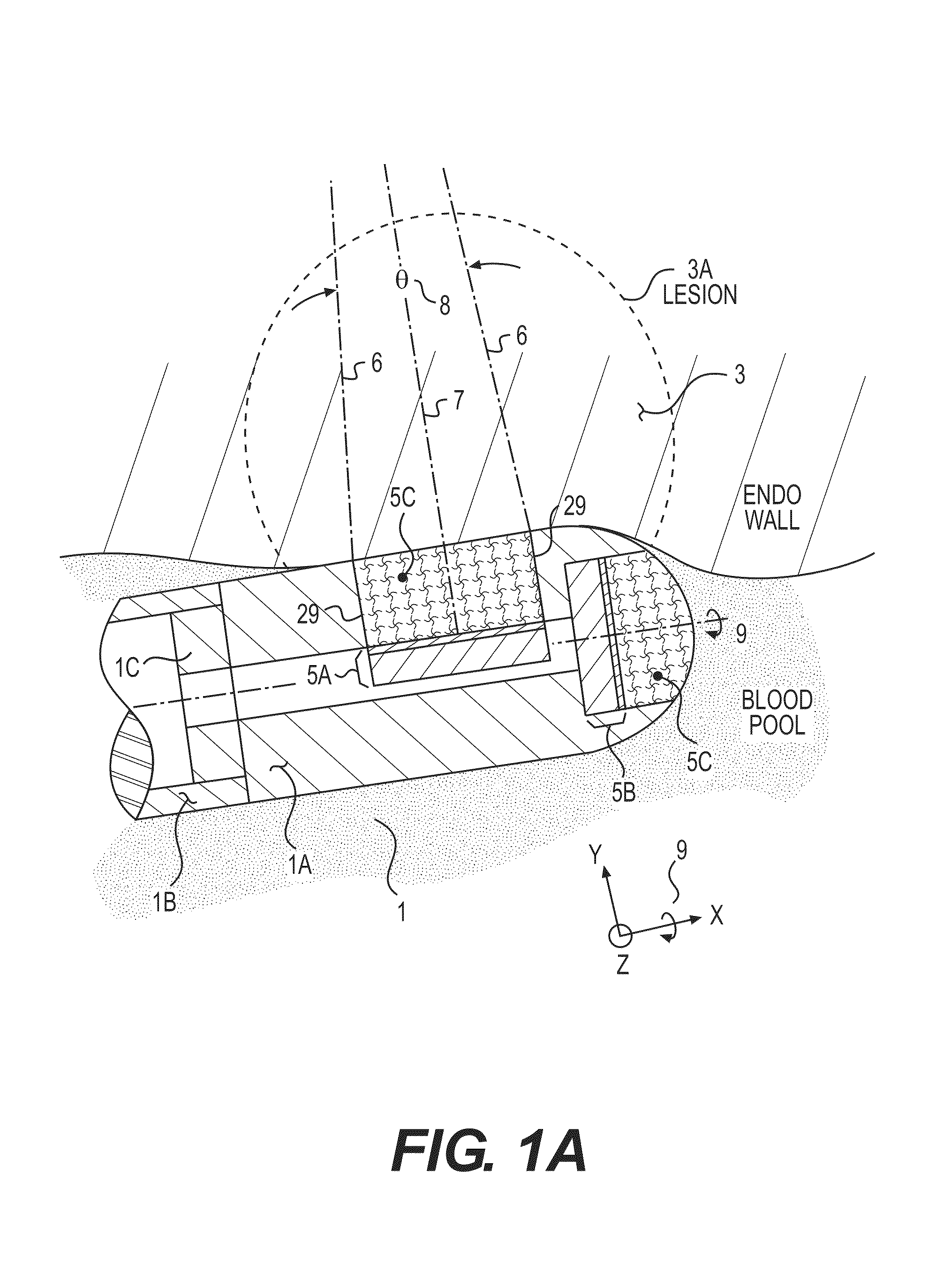
Device and method for determining tissue thickness and creating cardiac ablation lesions
A tissue ablation device has a handle and an ablation head coupled to the handle. The ablation head has a first jaw, a second jaw, and an ablative element coupled to at least one of the first and second jaws. A thickness measurement device may be coupled to the ablation device to indicate the distance separating the first and second jaws. Further, a force measurement device may be coupled to the ablation device to measure the force being applied by the first and second jaws to a piece of tissue. Further, a strain measurement device may be coupled to the ablation device to indicate the strain resulting in a piece of tissue disposed between the first and second jaws when a stress is applied to the tissue.
Owner:MEDTRONIC INC
Varying Tissue Compression Aided By Elastic Members
ActiveUS20110084112A1Readily apparentSuture equipmentsStapling toolsTissue thicknessTissue compression
The present disclosure relates to surgical fastener applying apparatus, and the application of variable compression to tissue. More specifically, the presently disclosed surgical fastener applying apparatus including a first jaw having proximal and distal ends and including an anvil member, the anvil member extending along a longitudinal axis and including a tissue contacting surface and a second jaw having proximal and distal ends movably coupled to the first jaw, the second jaw including a cartridge member and a channel. The surgical fastener applying apparatus further includes a pair of elastic members positioned between the cartridge member and the channel of the second jaw, the pair of elastic members configured and dimensioned to apply and maintain constant compressive forces to tissue regardless of tissue thickness.
Owner:TYCO HEALTHCARE GRP LP
Device and method for determining tissue thickness and creating cardiac ablation lesions
A tissue ablation device has a handle and an ablation head coupled to the handle. The ablation head has a first jaw, a second jaw, and an ablative element coupled to at least one of the first and second jaws. A thickness measurement device may be coupled to the ablation device to indicate the distance separating the first and second jaws. Further, a force measurement device may be coupled to the ablation device to measure the force being applied by the first and second jaws to a piece of tissue. Further, a strain measurement device may be coupled to the ablation device to indicate the strain resulting in a piece of tissue disposed between the first and second jaws when a stress is applied to the tissue.
Owner:MEDTRONIC INC
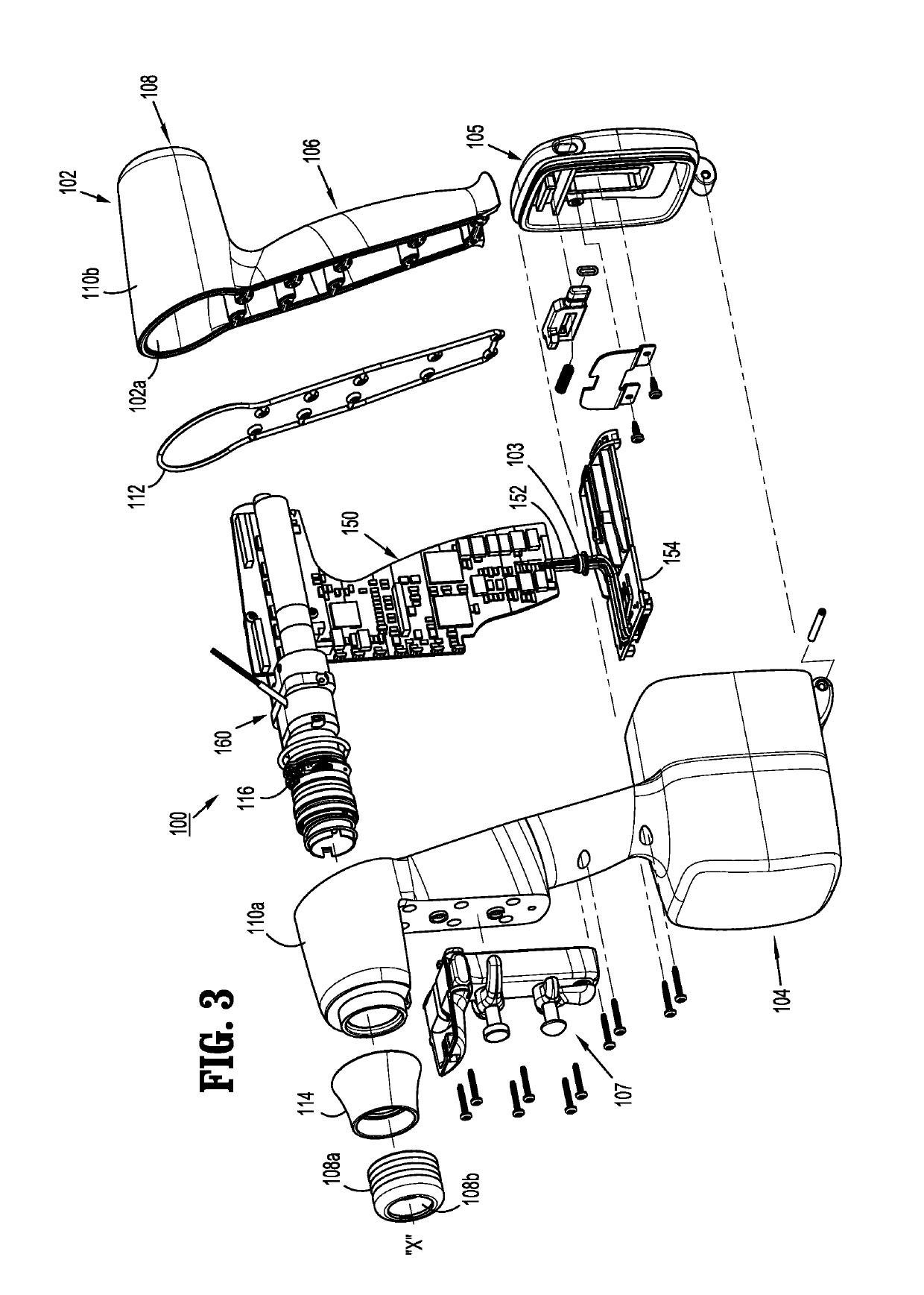
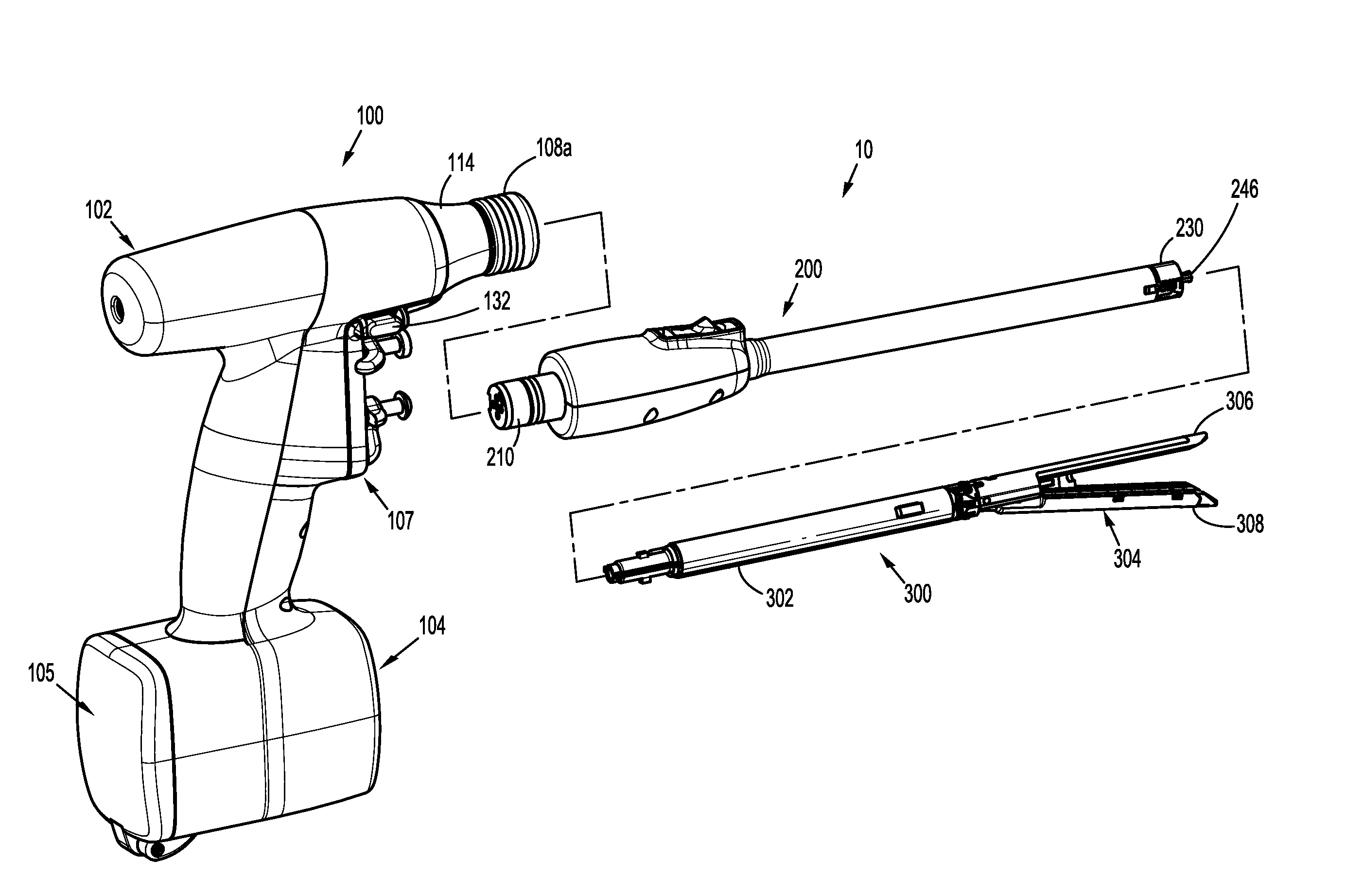
Apparatus and method for tissue thickness sensing
A surgical instrument is provided. The surgical instrument includes: a test end effector including a test jaw assembly having a pair of jaws configured to clamp about tissue and at least one sensor configured to measure at least one tissue property; and a handle assembly configured to couple to the treatment end effector. The handle assembly includes: a drive assembly; a motor operatively coupled to the drive assembly; and a controller operatively coupled to the motor, the controller configured to control operation of the motor to actuate the test end effector to measure the at least one tissue property and to determine, based on the at least one tissue property, at least one suitable treatment end effector.
Owner:TYCO HEALTHCARE GRP LP
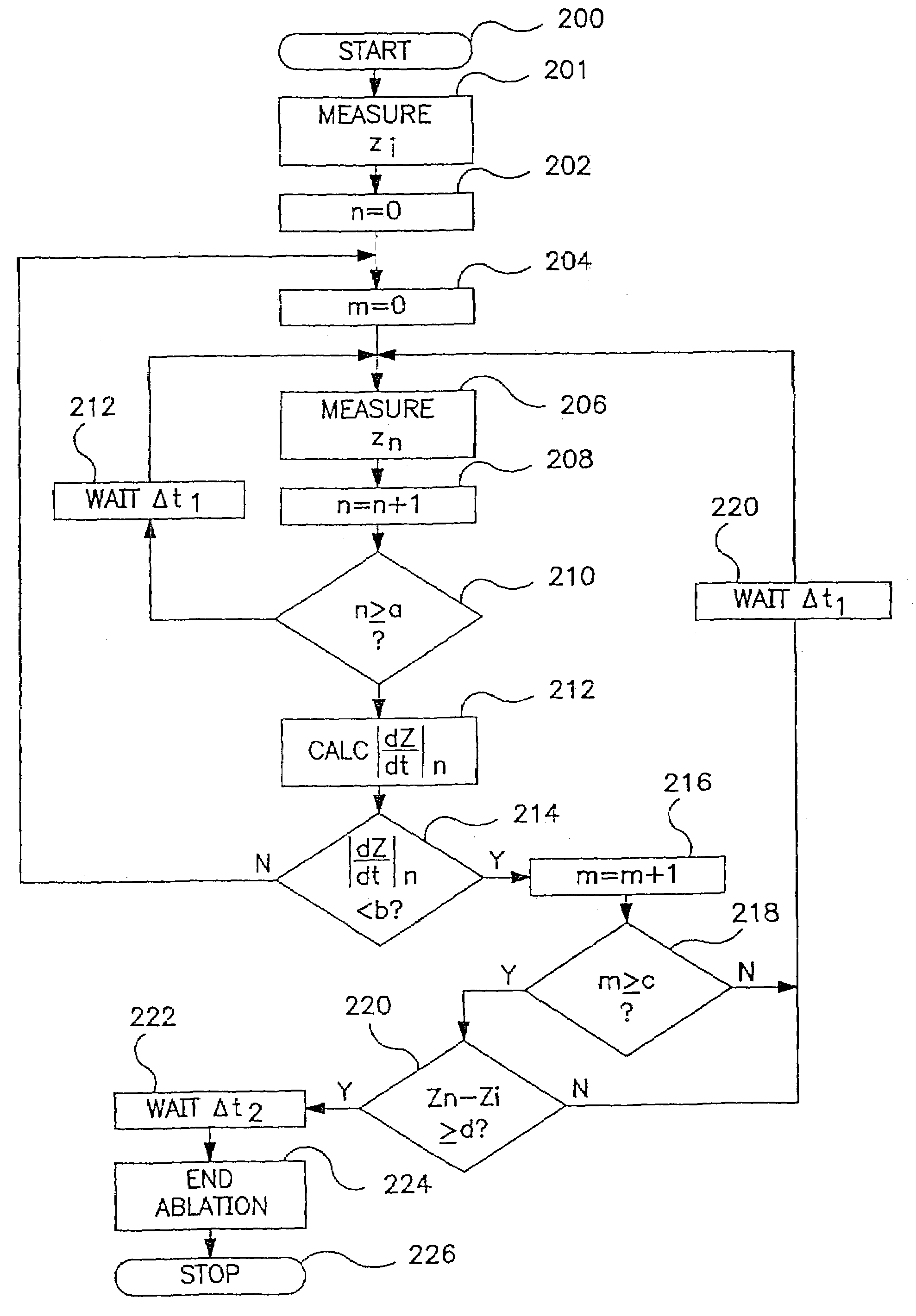
Ablation system and method of use
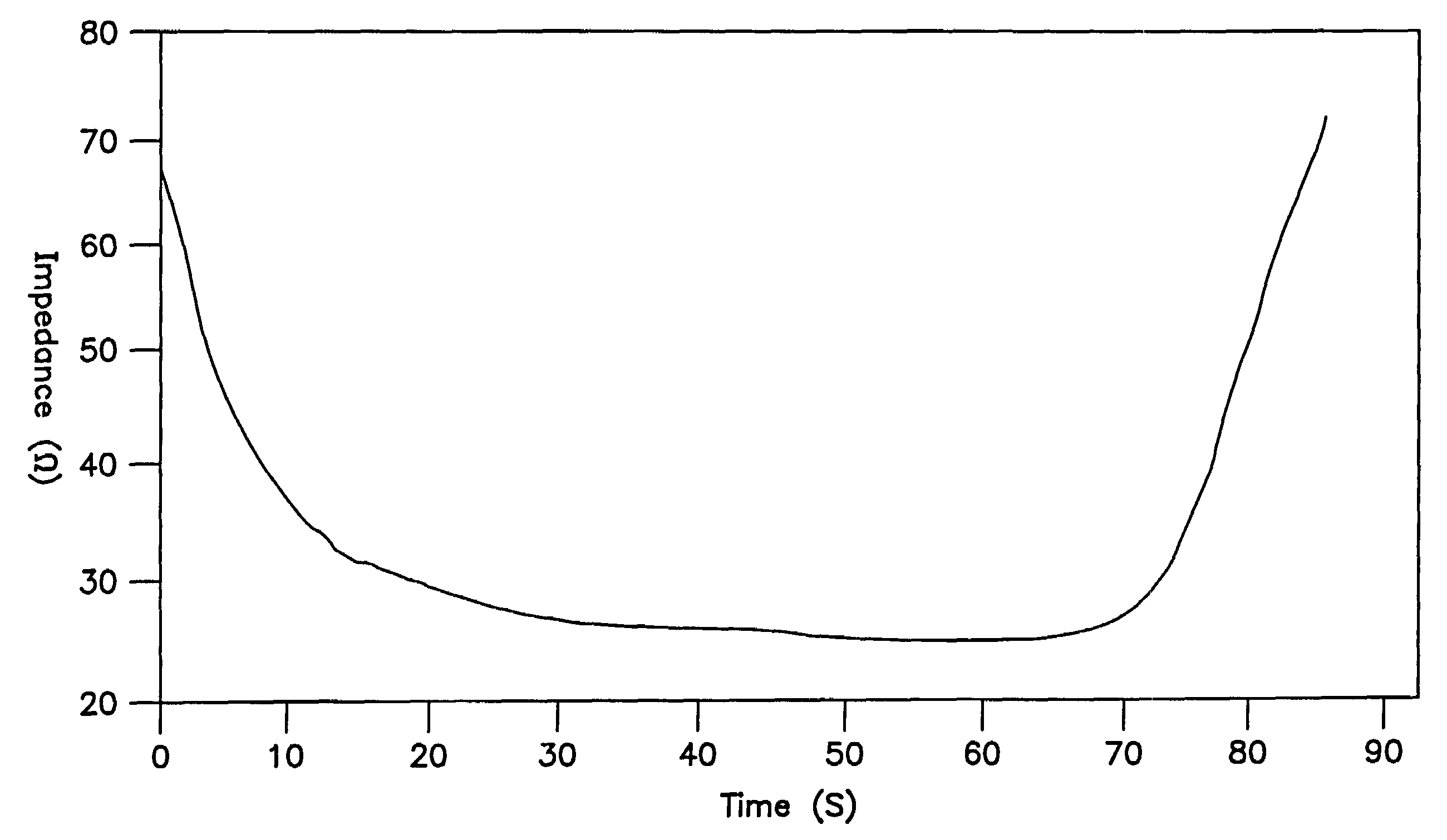
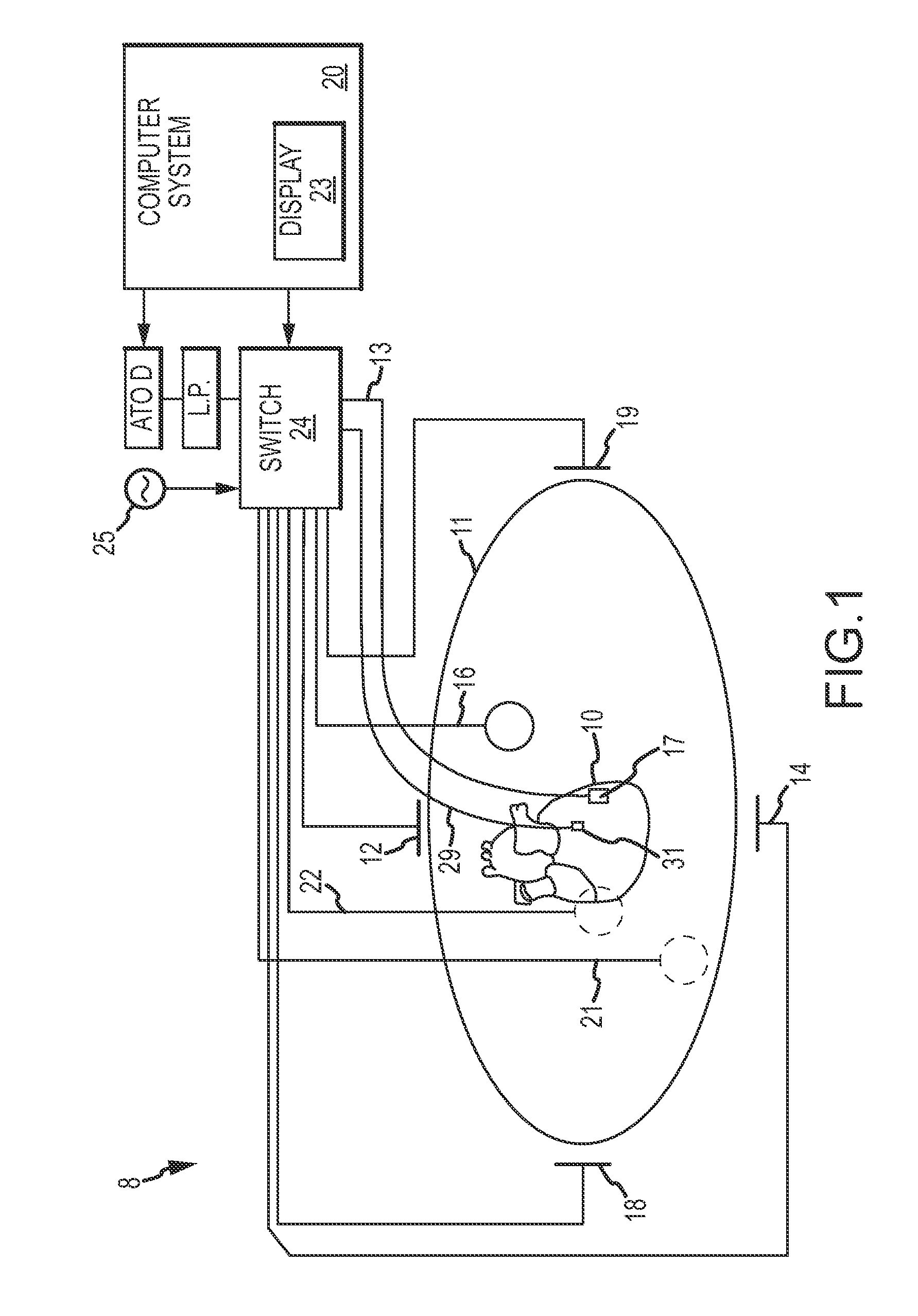
InactiveUS6989010B2Simple systemImproving impedanceDiagnosticsSurgical instruments for heatingEngineeringPlateau
A system and method for creating lesions and assessing their completeness or transmurality. Assessment of transmurality of a lesion is accomplished by monitoring the impedance of the tissue to be ablated. Rather than attempting to detect a desired drop or a desired increase impedance, completeness of a lesion is detected in response to the measured impedance remaining at a stable level for a desired period of time, referred to as an impedance plateau. The mechanism for determining transmurality of lesions adjacent individual electrodes or pairs may be used to deactivate individual electrodes or electrode pairs, when the lesions in tissue adjacent these individual electrodes or electrode pairs are complete, to create an essentially uniform lesion along the line of electrodes or electrode pairs, regardless of differences in tissue thickness adjacent the individual electrodes or electrode pairs.
Owner:MEDTRONIC INC
Ablation system
A system for creating lesions and assessing their completeness or transmurality. Assessment of transmurality of a lesion is accomplished by monitoring the impedance of the tissue to be ablated. Rather than attempting to detect a desired drop or a desired increase impedance, completeness of a lesion is detected in response to the measured impedance remaining at a stable level for a desired period of time, referred to as an impedance plateau. The mechanism for determining transmurality of lesions adjacent individual electrodes or pairs may be used to deactivate individual electrodes or electrode pairs, when the lesions in tissue adjacent these individual electrodes or electrode pairs are complete, to create an essentially uniform lesion along the line of electrodes or electrode pairs, regardless of differences in tissue thickness adjacent the individual electrodes or electrode pairs.
Owner:MEDTRONIC INC
Apparatus and method for tissue thickness sensing
A surgical instrument is provided. The surgical instrument includes: a test end effector including a test jaw assembly having a pair of jaws configured to clamp about tissue and at least one sensor configured to measure at least one tissue property; and a handle assembly configured to couple to the treatment end effector. The handle assembly includes: a drive assembly; a motor operatively coupled to the drive assembly; and a controller operatively coupled to the motor, the controller configured to control operation of the motor to actuate the test end effector to measure the at least one tissue property and to determine, based on the at least one tissue property, at least one suitable treatment end effector.
Owner:TYCO HEALTHCARE GRP LP
Ablation system and method of use
A system and method for creating lesions and assessing their completeness or transmurality. Assessment of transmurality of a lesion is accomplished by monitoring the impedance of the tissue to be ablated. Rather than attempting to detect a desired drop or a desired increase impedance, completeness of a lesion is detected in response to the measured impedance remaining at a stable level for a desired period of time, referred to as an impedance plateau. The mechanism for determining transmurality of lesions adjacent individual electrodes or pairs may be used to deactivate individual electrodes or electrode pairs, when the lesions in tissue adjacent these individual electrodes or electrode pairs are complete, to create an essentially uniform lesion along the line of electrodes or electrode pairs, regardless of differences in tissue thickness adjacent the individual electrodes or electrode pairs. Complete or partial submersion in a fluid of the ablating portion of the ablation device may be detected prior to, during or following an ablation procedure.
Owner:MEDTRONIC INC
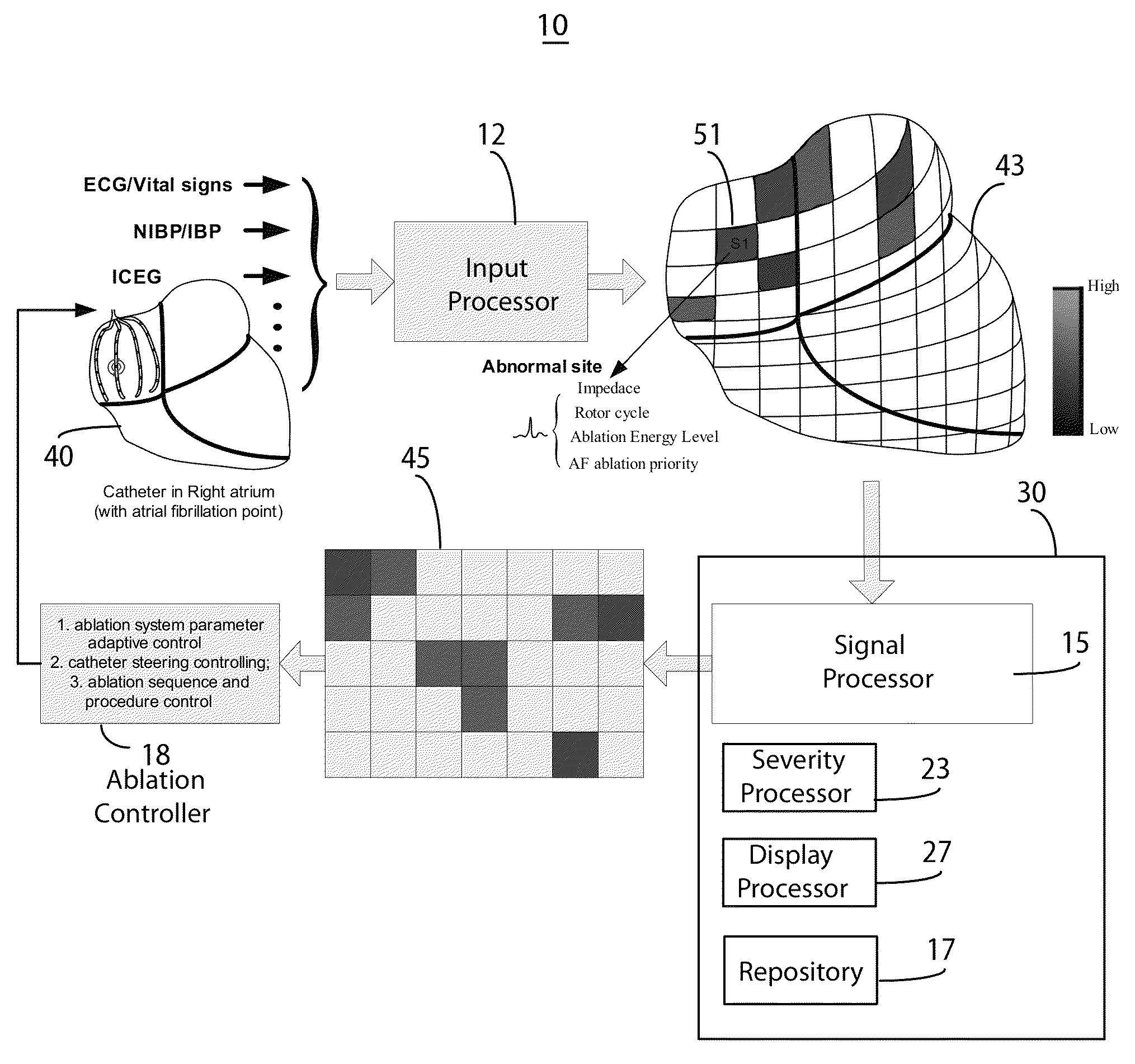
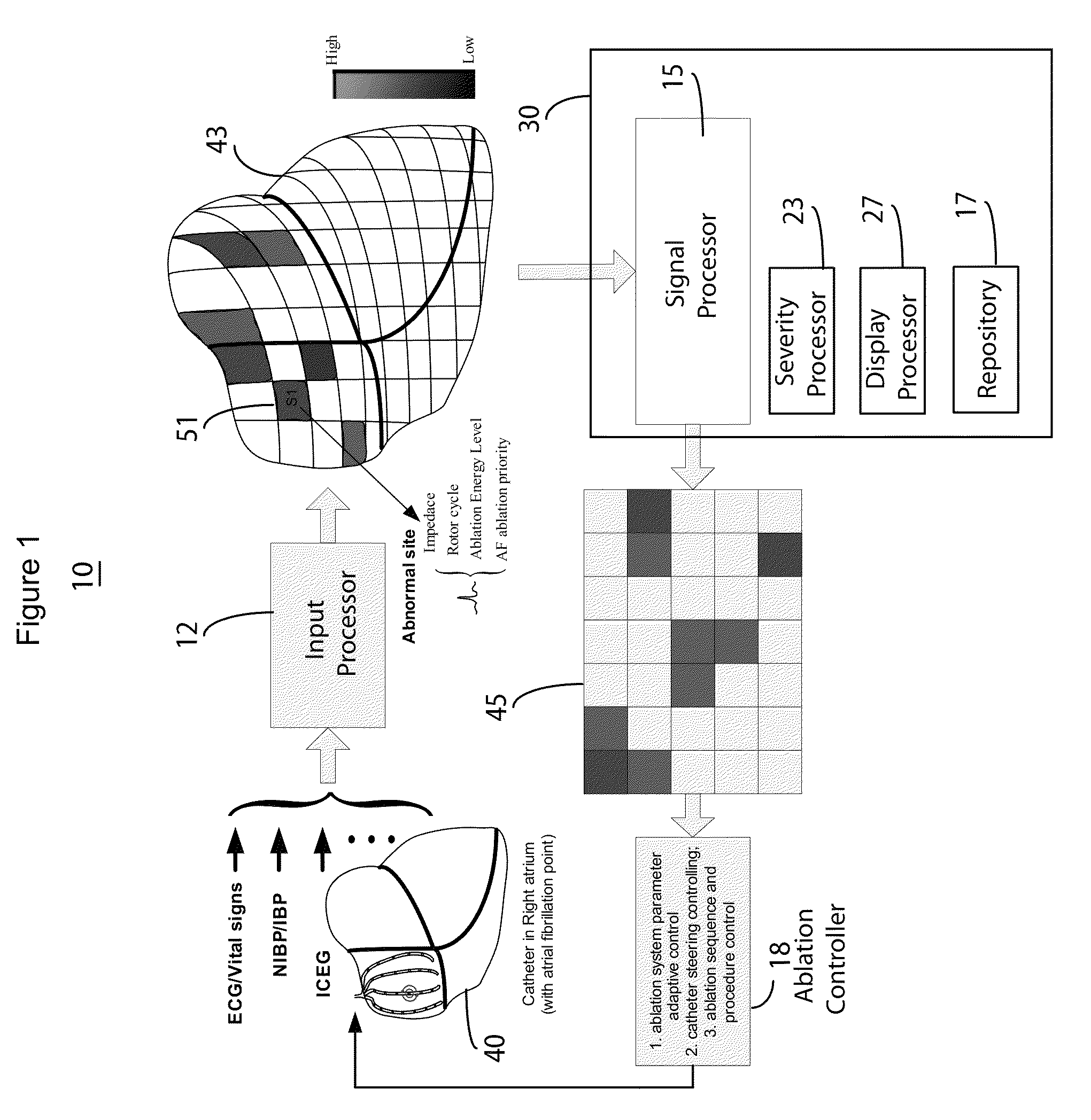
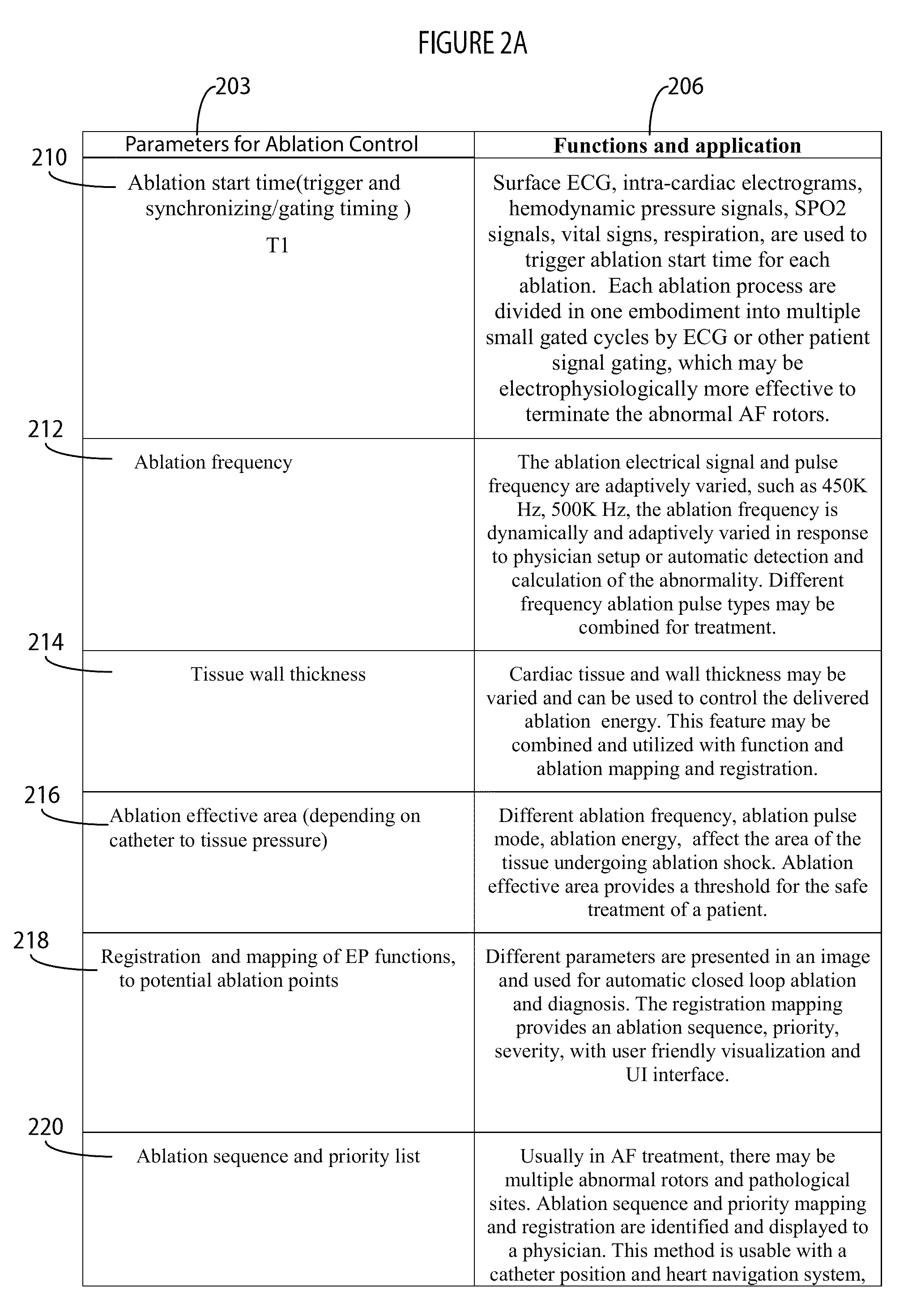
System for automatic medical ablation control
ActiveUS9277956B2Surgical systems user interfaceComputer-aided planning/modellingElectricityControl system
A system provides heart ablation unit control. The system includes an input processor for acquiring electrophysiological signal data from multiple tissue locations of a heart and data indicating tissue thickness at the multiple tissue locations. A signal processor processes the acquired electrophysiological signal data to identify location of particular tissue sites of the multiple tissue locations exhibiting electrical abnormality in the acquired electrophysiological signal data and determines an area of abnormal tissue associated with individual sites of the particular sites. An ablation controller automatically determines ablation pulse characteristics for use in ablating cardiac tissue at an individual site of the particular tissue sites in response to the acquired data indicating the thickness of tissue and determined area of abnormality of the individual site.
Owner:PIXART IMAGING INC
Ablation system and method of use
A system and method for creating lesions and assessing their completeness or transmurality. Assessment of transmurality of a lesion is accomplished by monitoring the impedance of the tissue to be ablated. Rather than attempting to detect a desired drop or a desired increase impedance, completeness of a lesion is detected in response to the measured impedance remaining at a stable level for a desired period of time, referred to as an impedance plateau. The mechanism for determining transmurality of lesions adjacent individual electrodes or pairs may be used to deactivate individual electrodes or electrode pairs, when the lesions in tissue adjacent these individual electrodes or electrode pairs are complete, to create an essentially uniform lesion along the line of electrodes or electrode pairs, regardless of differences in tissue thickness adjacent the individual electrodes or electrode pairs. Complete or partial submersion in a fluid of the ablating portion of the ablation device may be detected prior to, during or following an ablation procedure.
Owner:MEDTRONIC INC
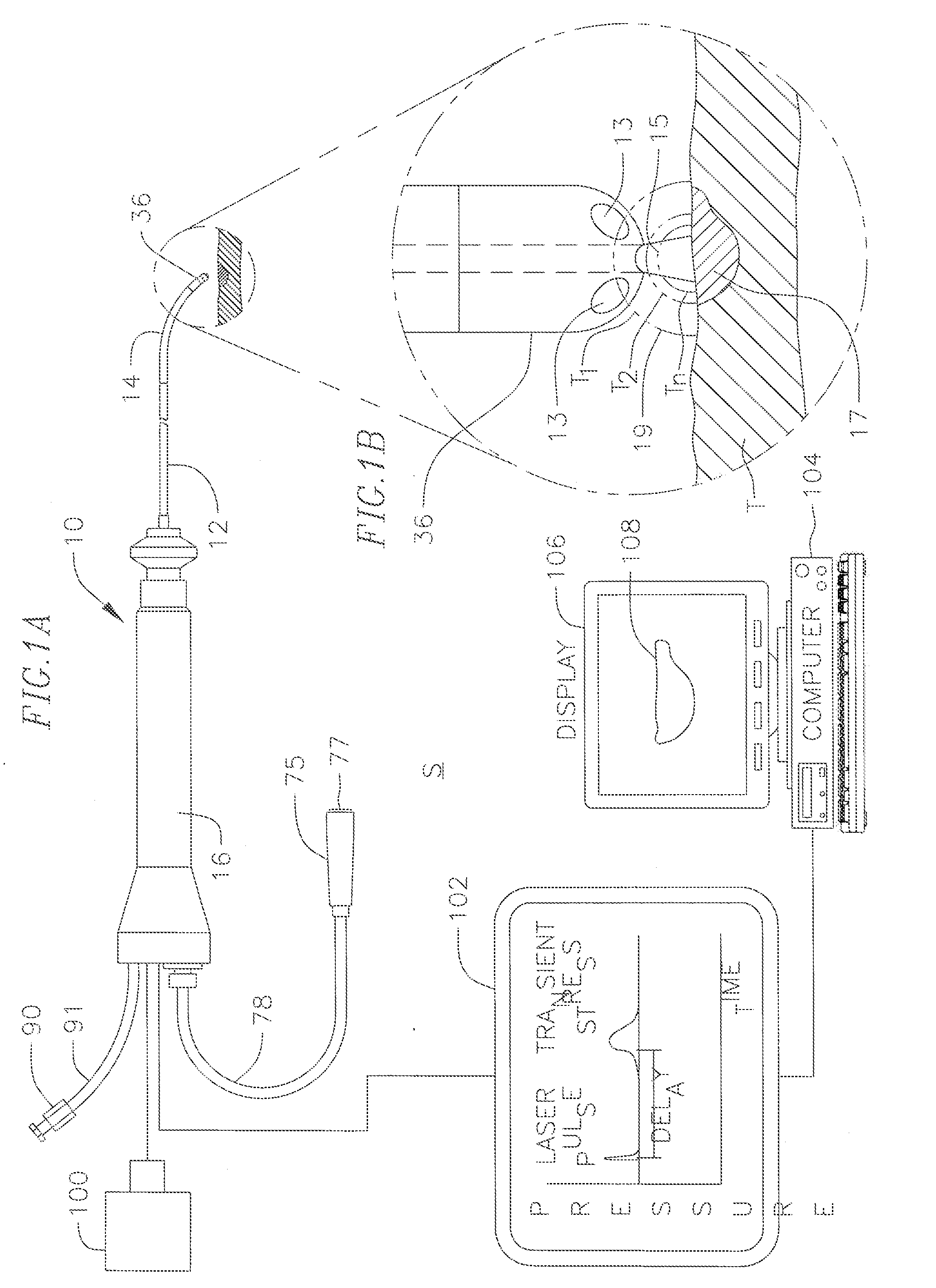
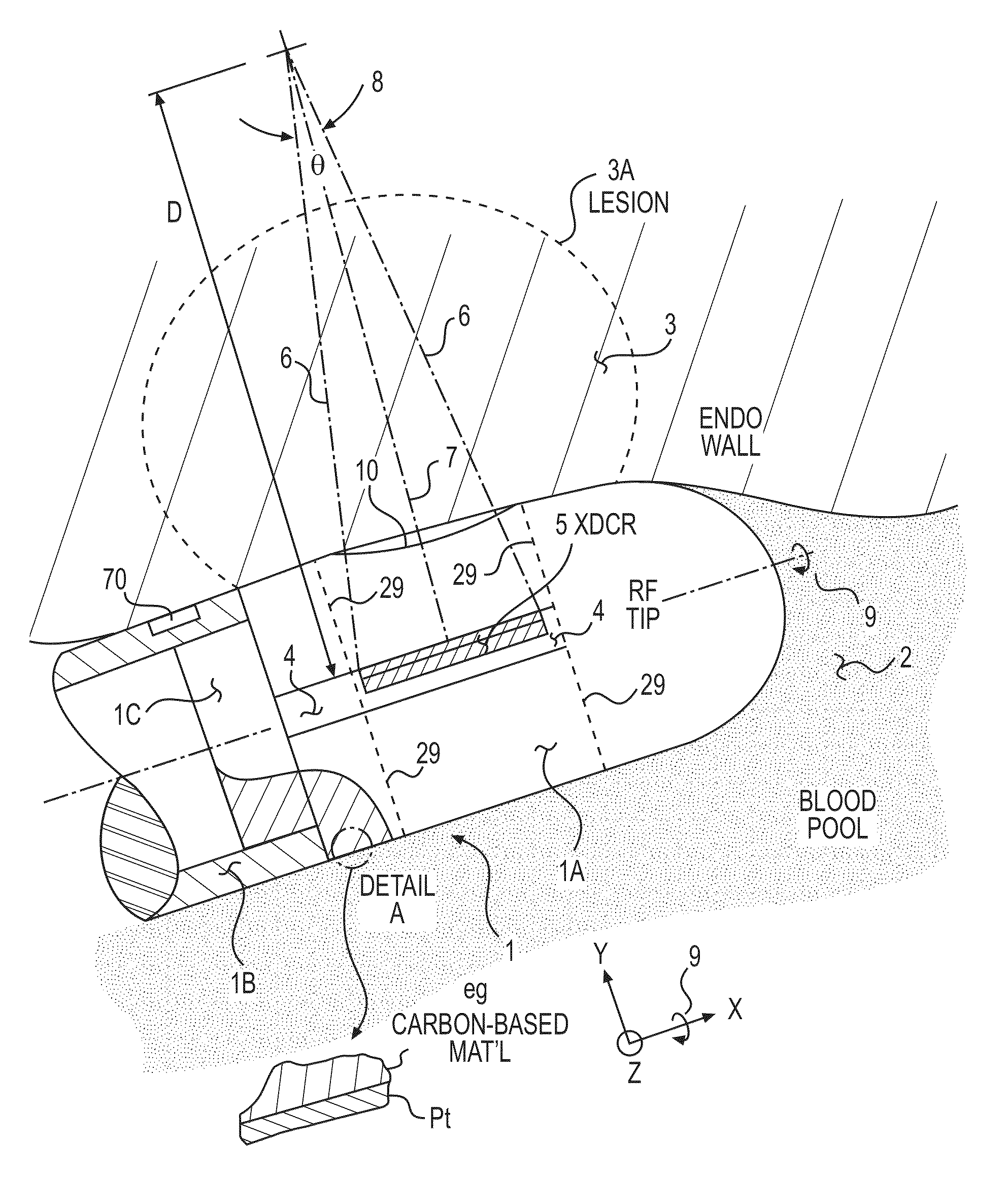
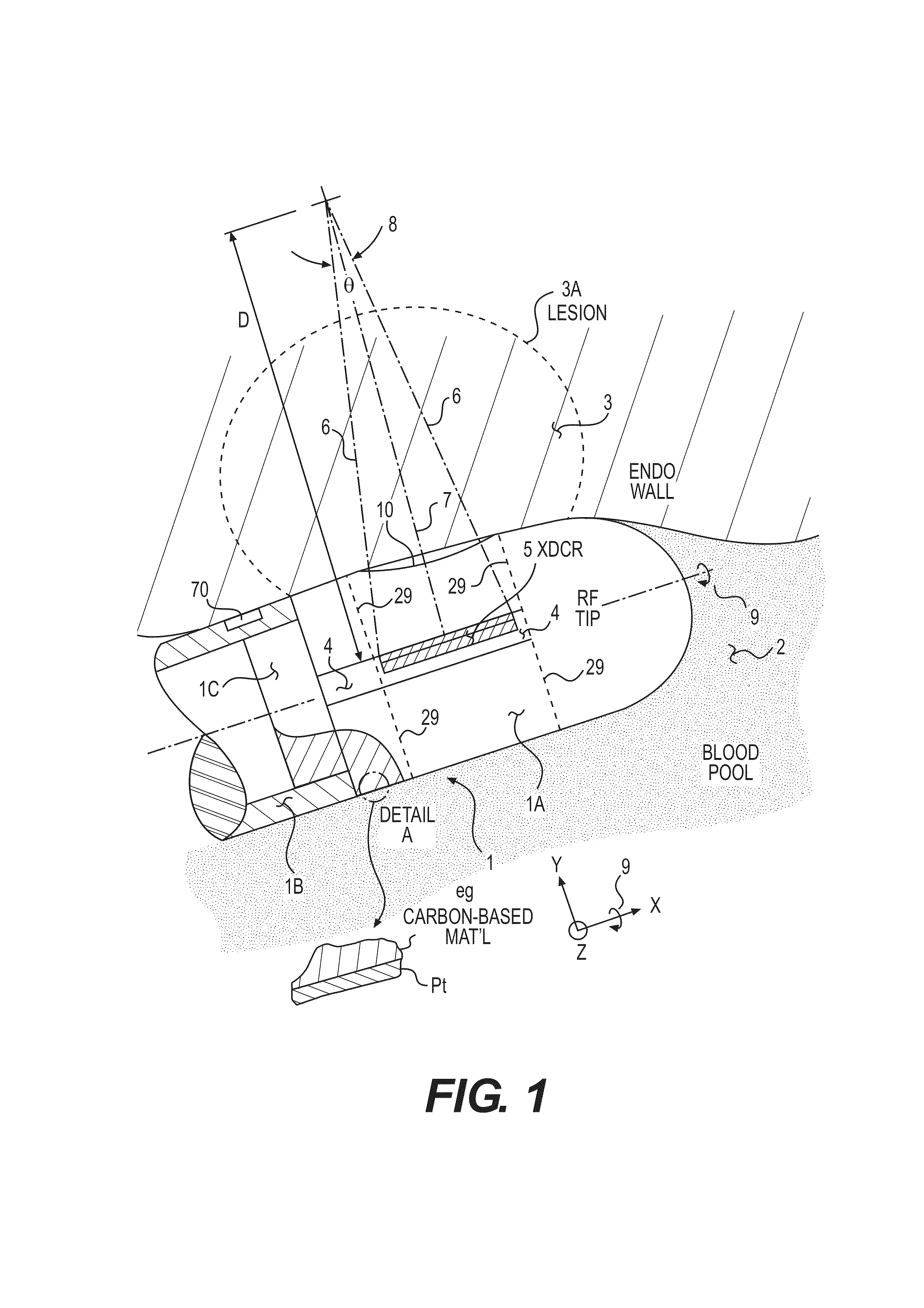
Apparatus and Methods for Acoustic Monitoring of Ablation Procedures
InactiveUS20100168572A1Easy to collectFacilitates presentationUltrasonic/sonic/infrasonic diagnosticsAuscultation instrumentsContact forceInterface position
A system for ablating tissue includes a catheter having an elongate body, with at least one ablation element (e.g., RF electrode) and at least one acoustic transducer located within the body's tip region. The transducer receives acoustic signals from proximate the tip region. The system also includes a monitoring unit coupled to the transducer to interpret the received acoustic signals as data regarding at least one therapeutic parameter (e.g., pre-pop detection, lesion making progress, tissue interface detection, tissue contact force, tissue contact establishment, bubble spatial distribution, bubble depth, bubble size, bubble size distribution, tissue interface distance, tissue interface position, tissue attenuation, tissue thickness, lesion spectral fingerprint). The monitoring unit is operable to provide feedback to a practitioner, such as graphical, audible, and / or haptic output of sensed data, and may also be operable to control operation of the at least one ablation element in response thereto.
Owner:ST JUDE MEDICAL ATRIAL FIBRILLATION DIV
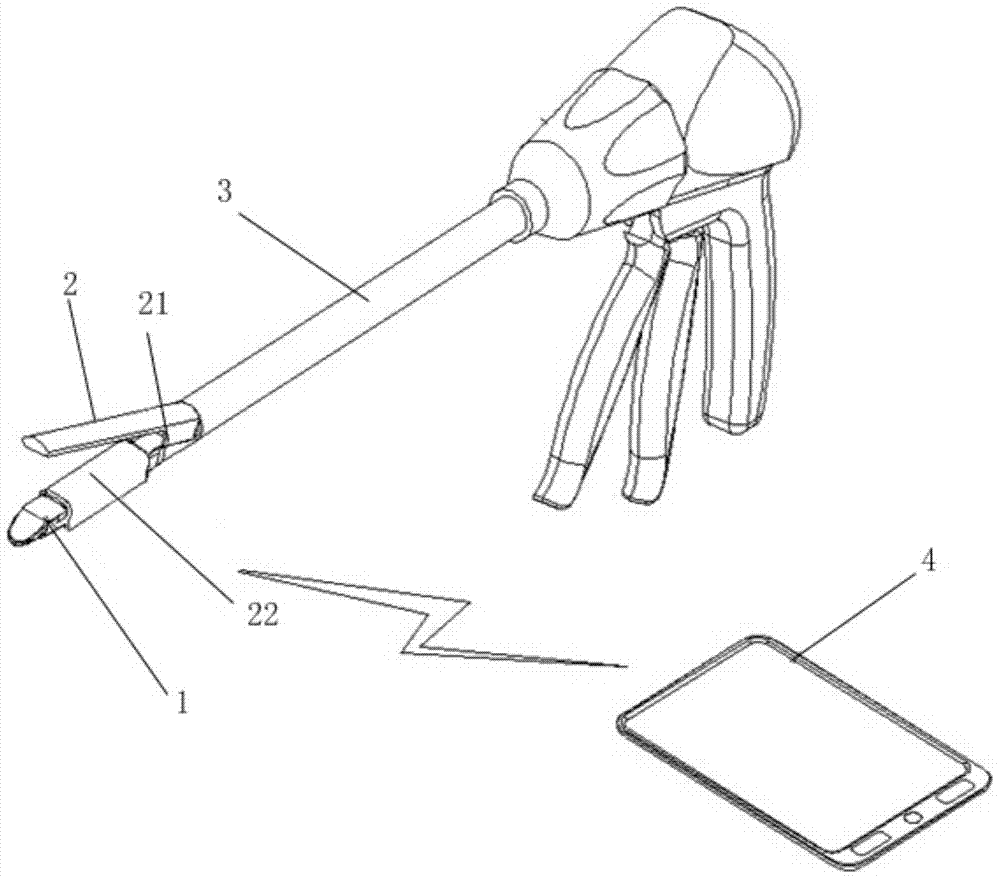
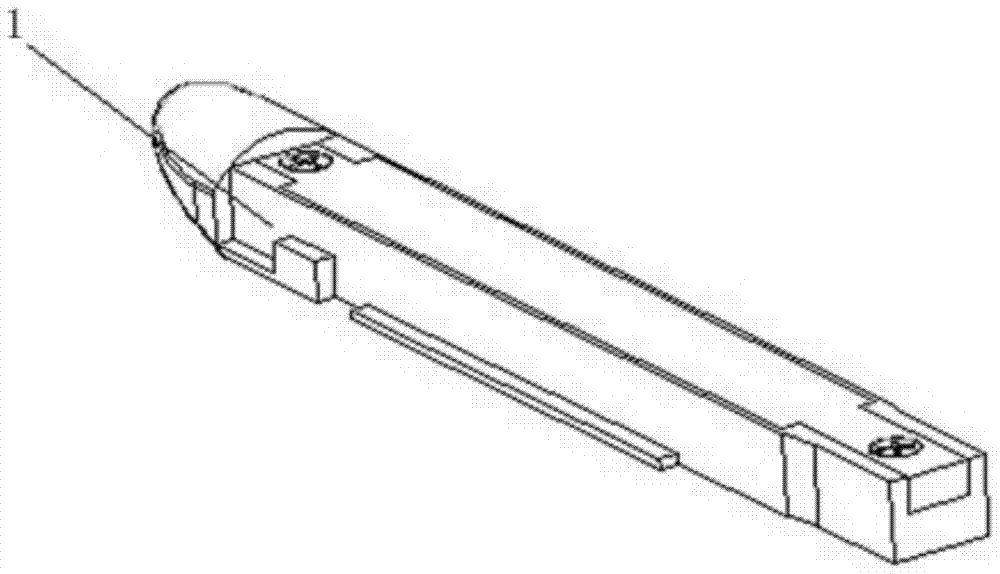
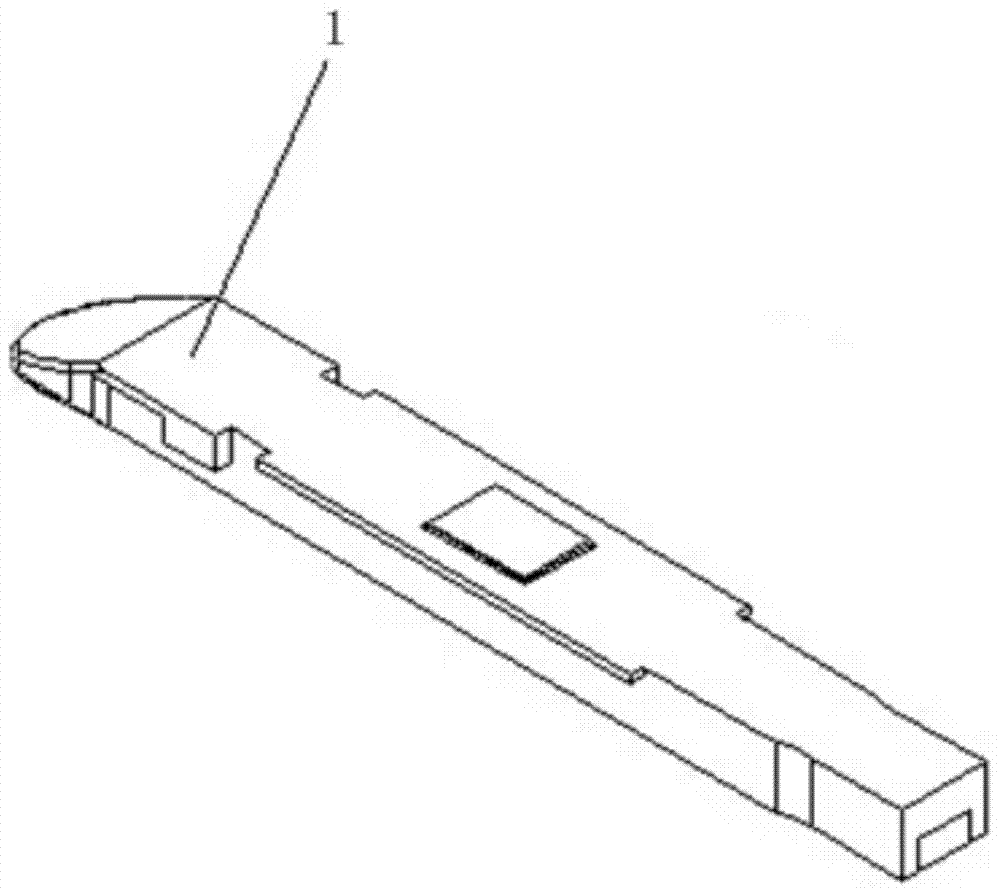
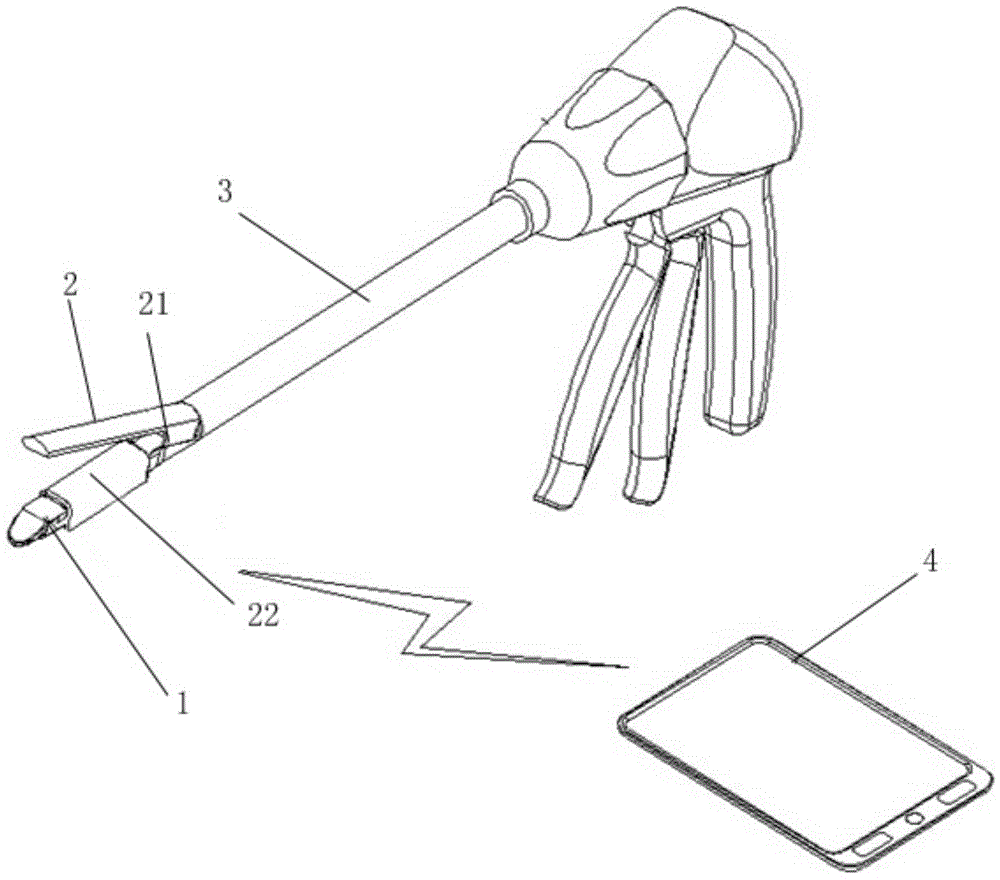
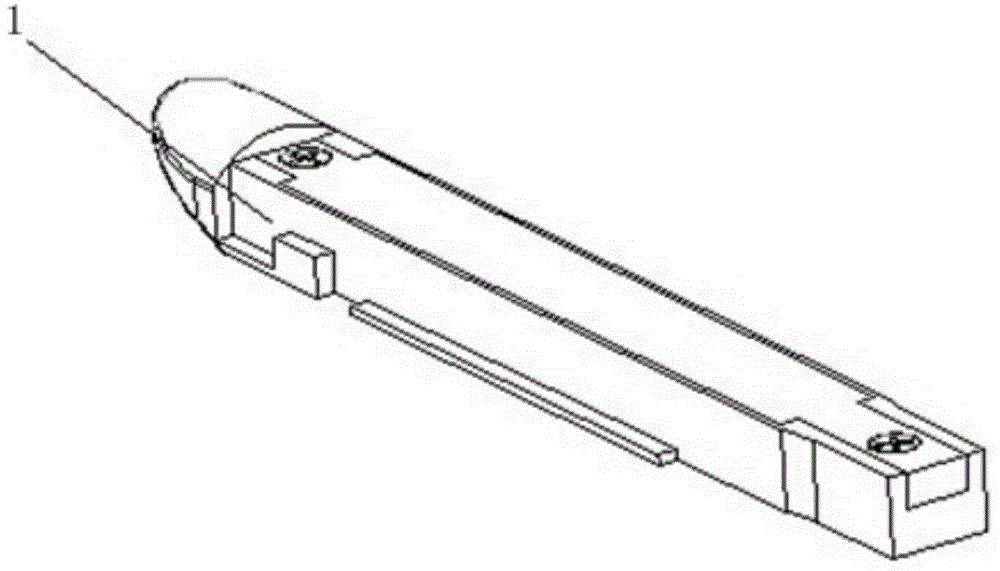
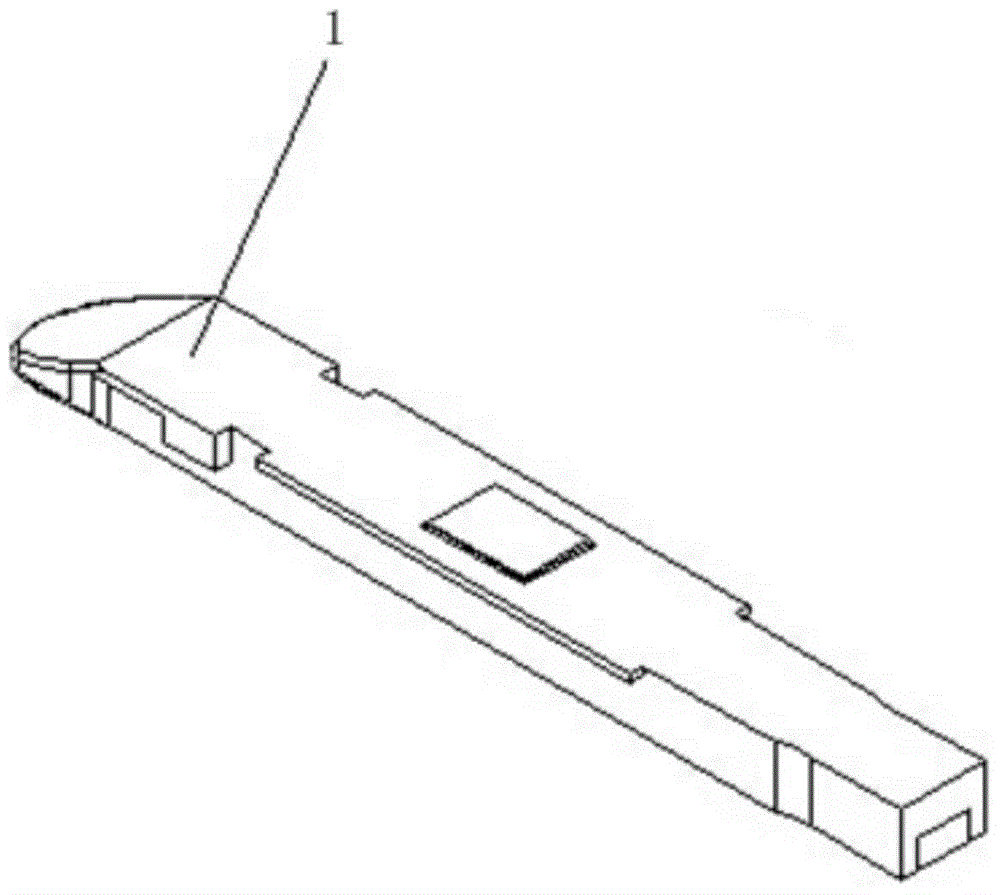
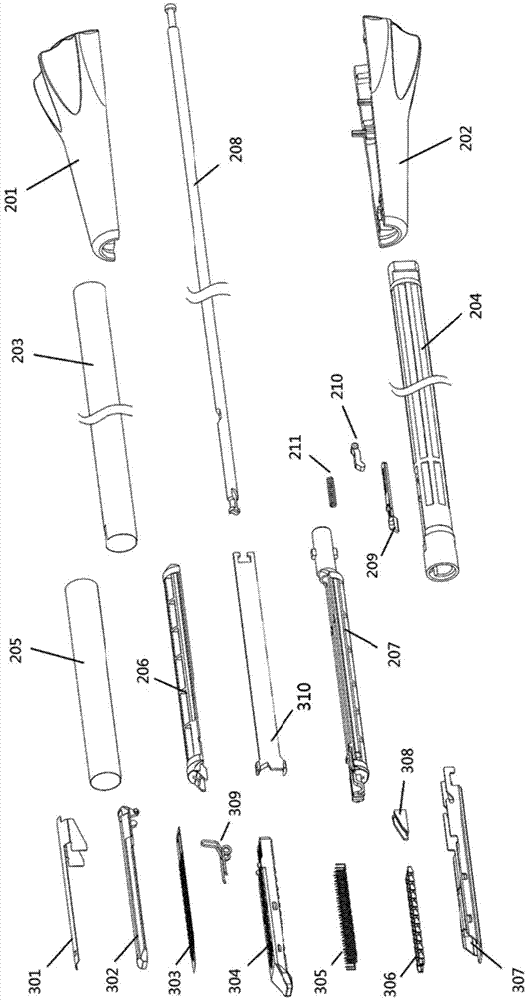
Smart device to measure tissue thickness
InactiveCN104921730BWon't hurtNo tissue damageDiagnostic recording/measuringSensorsButton batteryMeasuring instrument
The invention relates to an intelligent instrument for measuring the tissue thickness. The intelligent instrument comprises a button cell type intelligent thickness measuring clip or an external power supply type intelligent thickness measuring clip, a linear incision anastomat or a manual thickness measuring instrument or an automatic thickness measuring instrument, and a staple anvil. The button cell type intelligent thickness measuring clip comprises an outer shell, a pressing key, waterproof soft glass, an integrated circuit board and a bottom cover. The waterproof soft glass is arranged between the pressing key and the integrated circuit board and covers the surface of the pressing key. A button cell, a power module, a display module, a tissue pressure intensity measuring module, a tissue thickness measuring module, a control module and a wireless transmission module are mounted on the back face of the integrated circuit board. An eddy-current transducer and a pressure sensor are mounted on the front face of the integrated circuit board. The button cell type intelligent thickness measuring clip is matched with a wireless transmission device. The intelligent instrument for measuring the tissue thickness has the advantages that the tissue thickness can be measured in a quantitative mode, tissue thickness measurement is accurate, corresponding anastomotic staple cartridges can be selected conveniently, and the success rate of anastomotic surgery is increased.
Owner:UNIV OF SHANGHAI FOR SCI & TECH
Intelligent instrument for measuring tissue thickness
InactiveCN104921730AWon't hurtNo tissue damageDiagnostic recording/measuringSensorsWireless transmissionButton battery
The invention relates to an intelligent instrument for measuring the tissue thickness. The intelligent instrument comprises a button cell type intelligent thickness measuring clip or an external power supply type intelligent thickness measuring clip, a linear incision anastomat or a manual thickness measuring instrument or an automatic thickness measuring instrument, and a staple anvil. The button cell type intelligent thickness measuring clip comprises an outer shell, a pressing key, waterproof soft glass, an integrated circuit board and a bottom cover. The waterproof soft glass is arranged between the pressing key and the integrated circuit board and covers the surface of the pressing key. A button cell, a power module, a display module, a tissue pressure intensity measuring module, a tissue thickness measuring module, a control module and a wireless transmission module are mounted on the back face of the integrated circuit board. An eddy-current transducer and a pressure sensor are mounted on the front face of the integrated circuit board. The button cell type intelligent thickness measuring clip is matched with a wireless transmission device. The intelligent instrument for measuring the tissue thickness has the advantages that the tissue thickness can be measured in a quantitative mode, tissue thickness measurement is accurate, corresponding anastomotic staple cartridges can be selected conveniently, and the success rate of anastomotic surgery is increased.
Owner:UNIV OF SHANGHAI FOR SCI & TECH
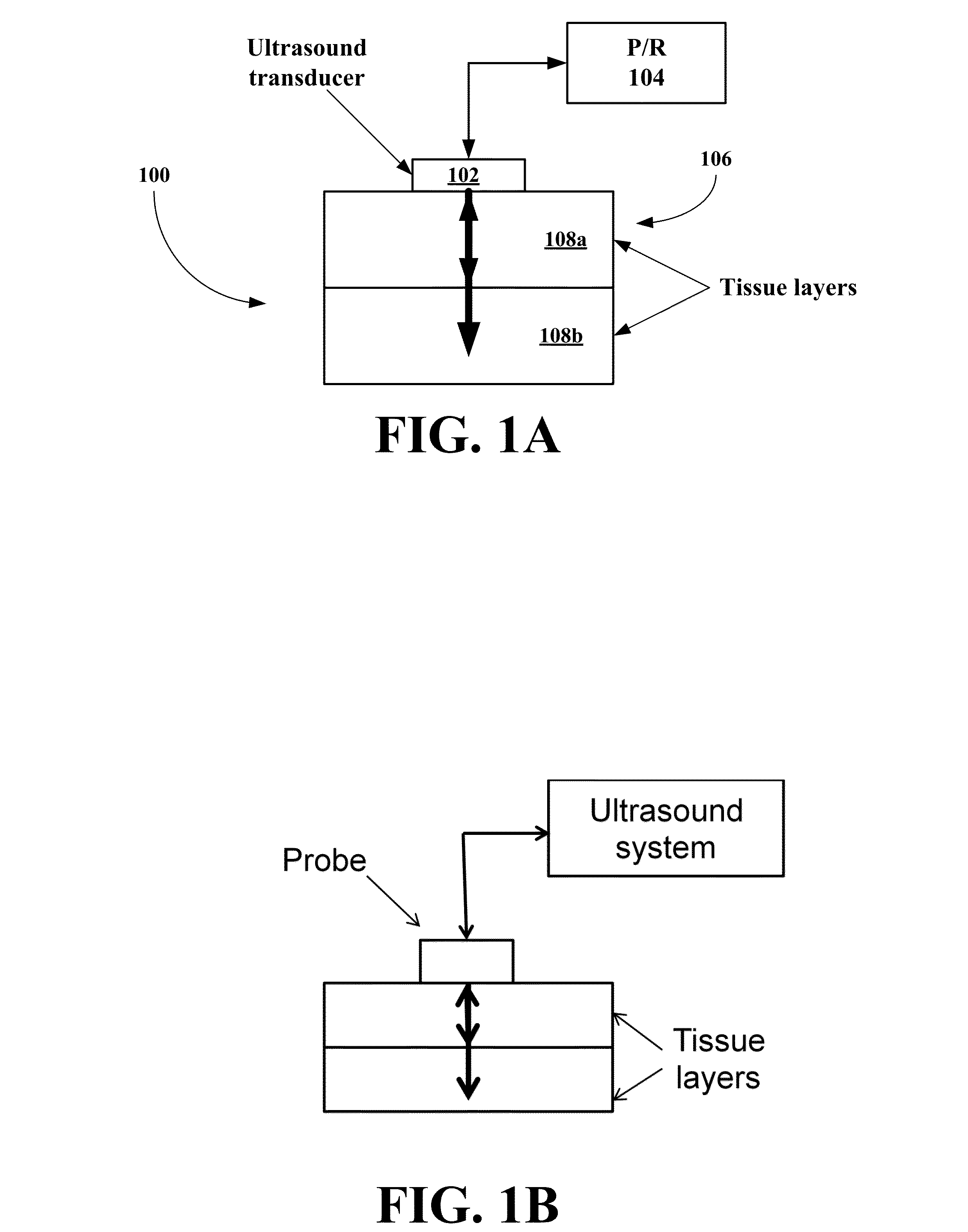
Methods and Apparatus for Detecting and Mapping Tissue Interfaces
InactiveUS20110028848A1Facilitates measuring tissue thicknessesImprove accuracyUltrasonic/sonic/infrasonic diagnosticsUltrasound therapyAcoustic energyMedicine
A device for measuring a spatial location of a tissue surface, such as the interface between different types of tissues or between tissue and body fluids, generally includes an elongate catheter body having a distal end portion, a plurality of localization elements carried by the distal end portion, and at least one pulse-echo acoustic element carried by the distal end portion. The localization elements allow the catheter to be localized (e.g., position and / or orientation) within a localization field, while the acoustic element allows for the detection of tissue surfaces where incoming acoustic energy will reflect towards the acoustic element. A suitable controller can determine the location of the detected tissue surface from the localization of the distal end portion of the catheter body. Tissue thicknesses can be derived from the detected locations of multiple (e.g., near and far) tissue surfaces. Maps and models of tissue thickness can also be generated.
Owner:ST JUDE MEDICAL ATRIAL FIBRILLATION DIV
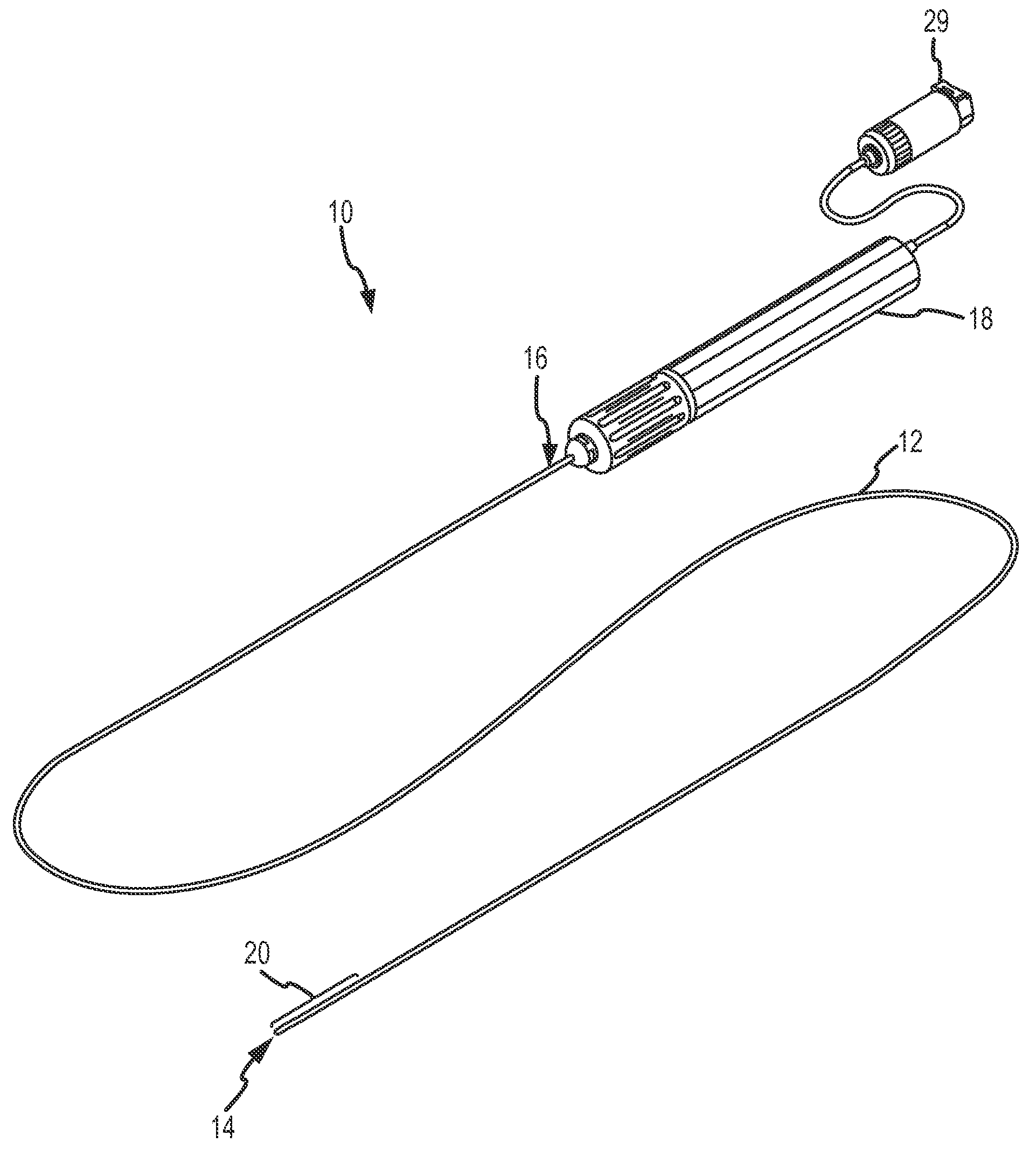
Fiber optic tissue ablation
A catheter tip for delivering laser light energy to create lesions extending to a depth of several millimeters in tissue includes an elongated, flexible housing. A reflector is oriented longitudinally in a channel the housing. A side emitting optical fiber diffuser, extending the length of the reflector, is held at a fixed separation from the reflector. The reflector and the side emitting diffuser are configured and spaced to provide a convergent beam directed through the tissue under treatment. Reflector curvature may be circular or elliptical in cross section, or other selected shape. The diffuser and reflector relative positioning being selected to place the beam focal point (or image) at a predetermined lateral distance from the reflector preferably not closer than the far wall of the tissue under treatment. Temperature probes are provided to monitor the temperature gradient through the tissue thickness. Optionally cooling and / or irrigation fluid are provided. Optionally, the fiber terminates at a retro-reflector.
Owner:OPTECH VENTURES
Coated hypodermic needle
A needle for a medical procedure includes a shaft with an inner surface, an outer surface, a proximal section, and a distal section. The distal section has a conductive tip configured to be a first electrode for voltage measurement. The needle further includes a first electrically insulative outer layer over a portion of the outer surface of the shaft. The conductive tip is adapted for insertion through tissue into, for example, a pericardial space of a patient. A system for determining the location of a needle during a medical procedure includes the needle and an anatomical mapping and localization system electrically coupled to the needle and adapted to measure voltage at the conductive tip. A system for determining tissue thickness during a medical procedure includes the needle, an anatomical mapping and localization system electrically coupled to the needle, and an electrocardiograph operatively coupled to the needle and adapted to monitor electrical activity at the conductive tip and at the second electrode. The needle may include a second electrode.
Owner:ST JUDE MEDICAL ATRIAL FIBRILLATION DIV
Surgical fastening apparatus
ActiveUS20110095069A1Provide flexibilitySuture equipmentsStapling toolsPosition dependentEngineering
A surgical fastening apparatus including a fastener receiving frame including a plurality of spaced apart openings formed therein and a fastener supporting member containing a plurality of surgical fasteners extending therefrom. The surgical fasteners are engagable with the plurality of openings to mate with the fastener receiving frame to fasten tissue therebetween. The fasteners are engageable with the openings in a plurality of positions dependent on a tissue thickness between the fastener receiving frame and the fastener supporting member.
Owner:TYCO HEALTHCARE GRP LP
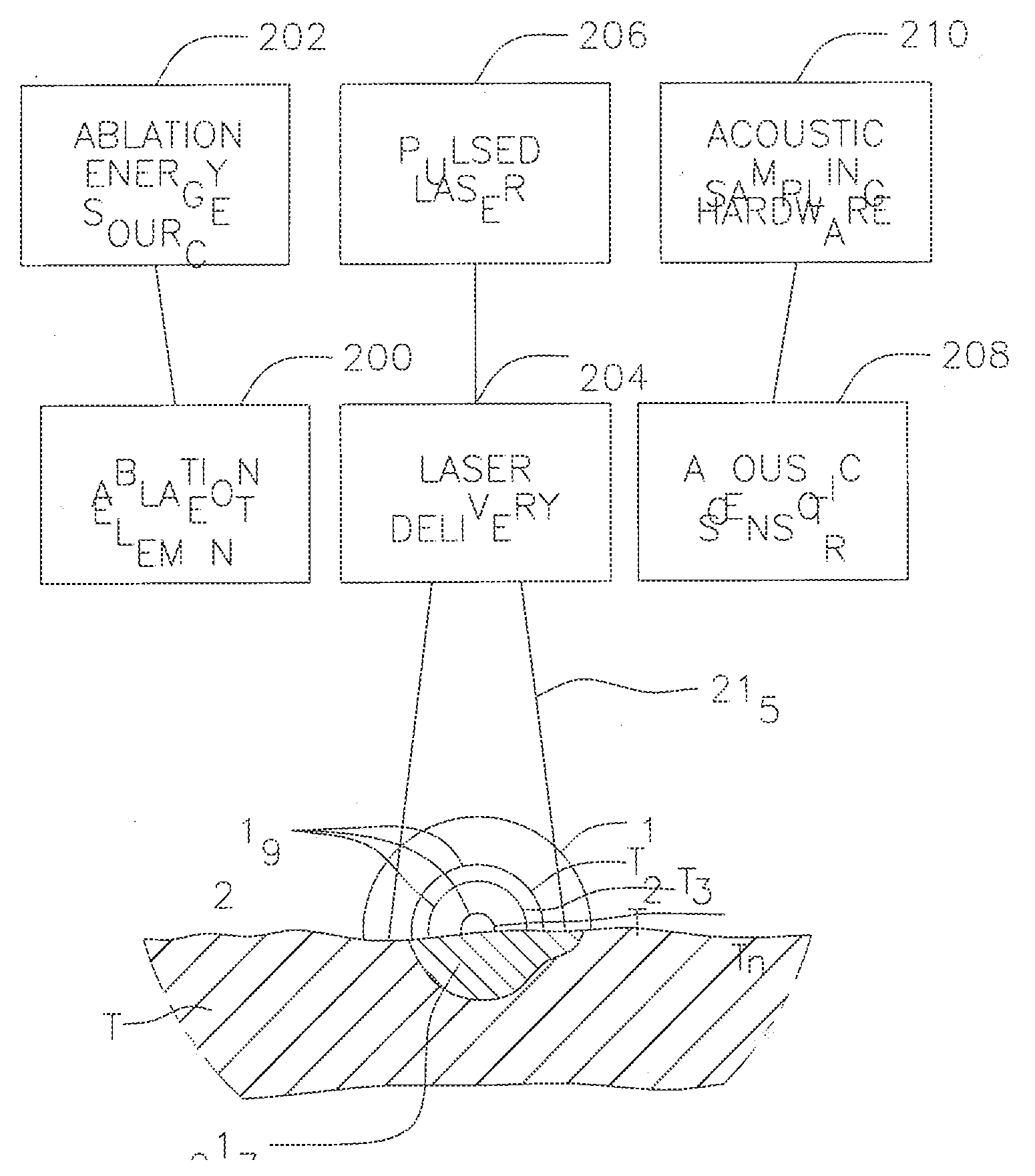
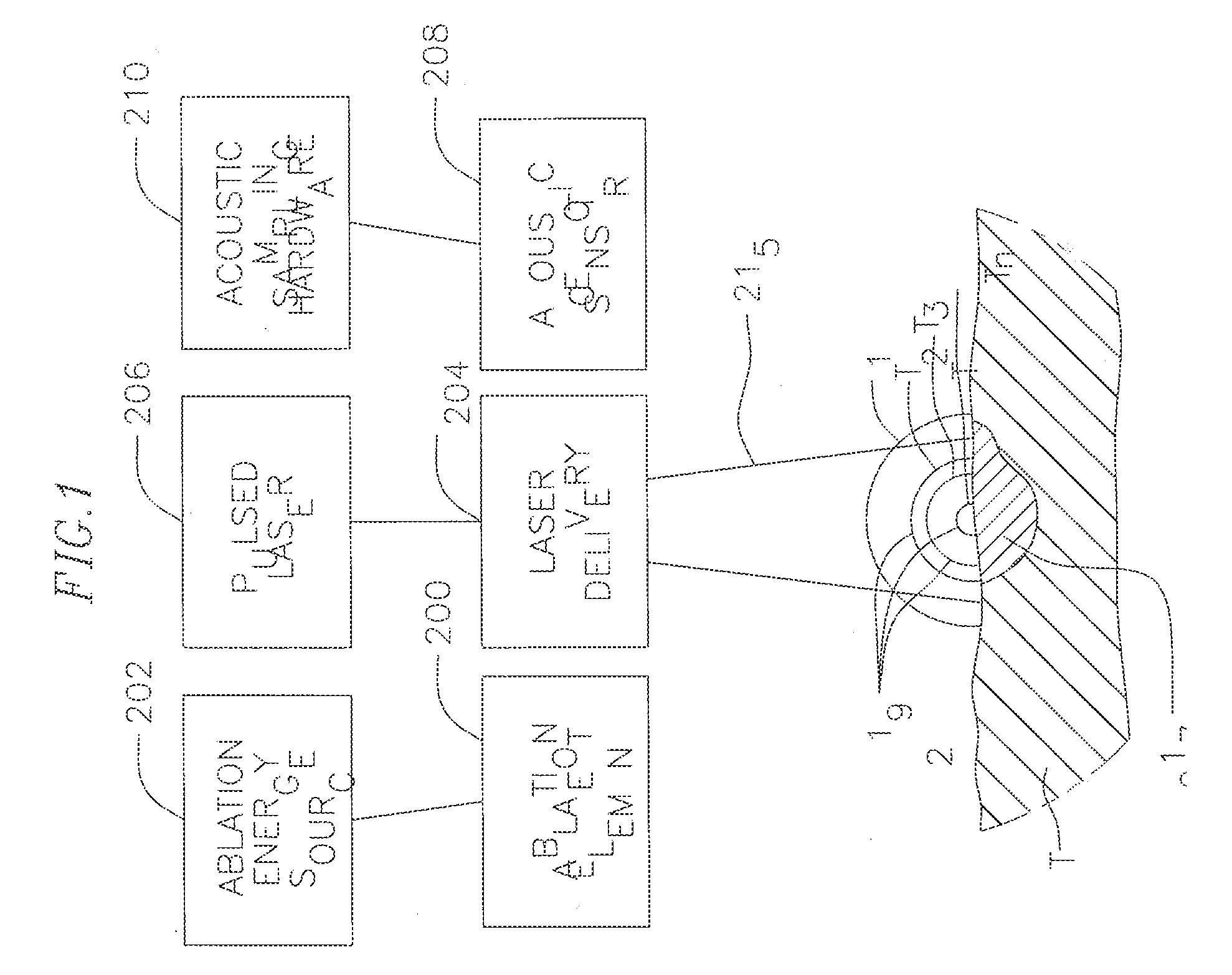
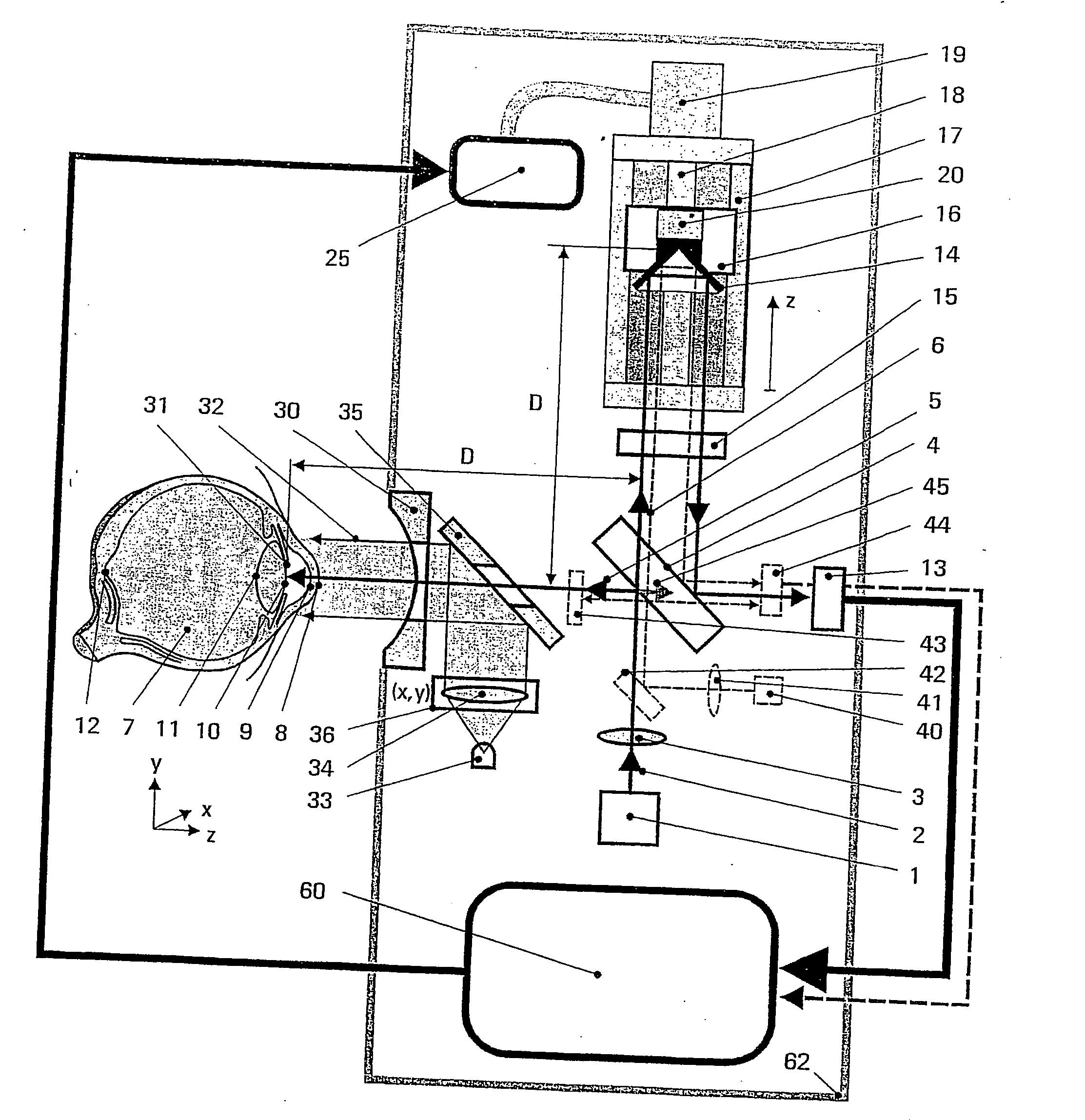
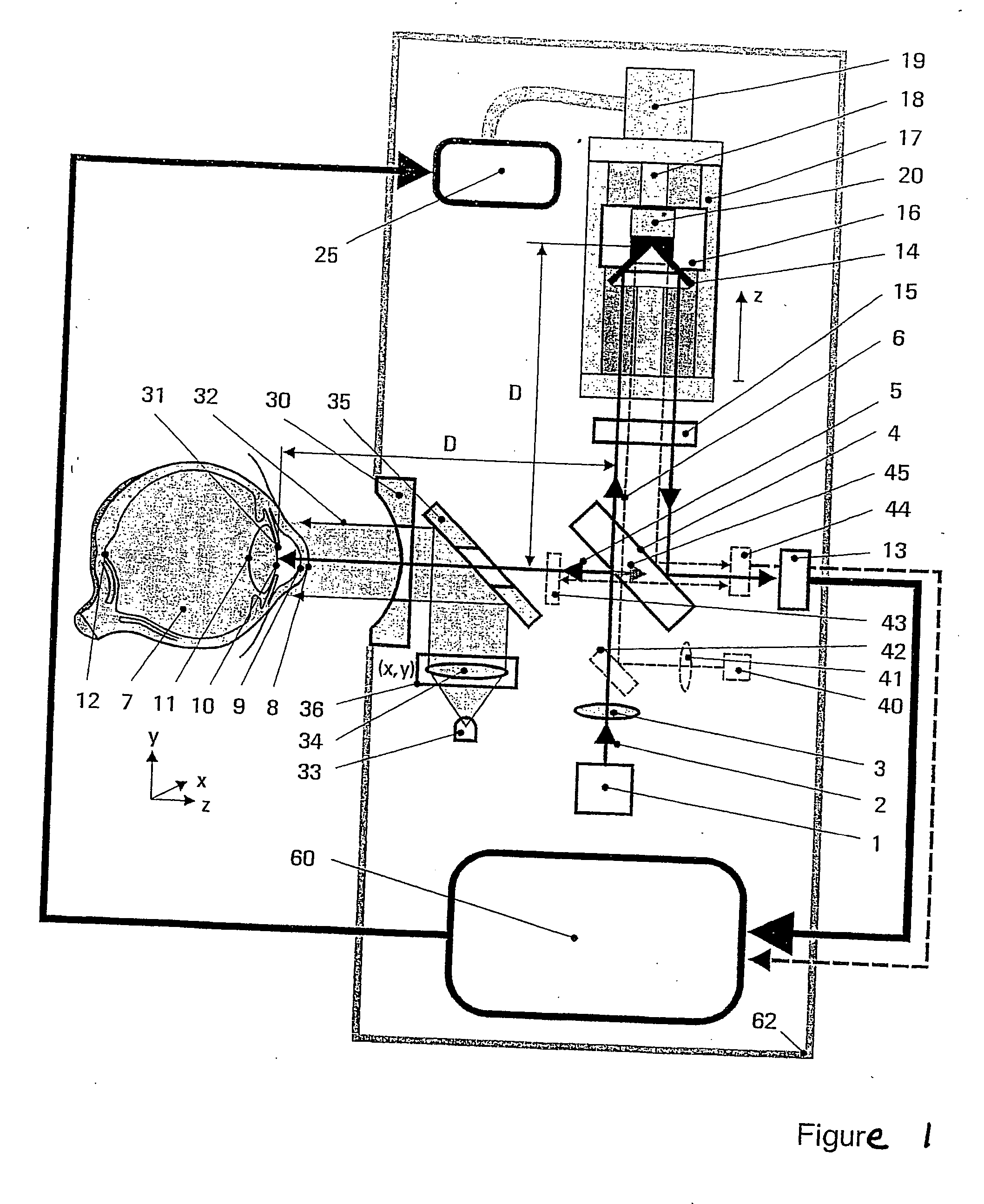
Real-time optoacoustic monitoring with electophysiologic catheters
InactiveUS20080154257A1High sensitivityHigh resolutionCatheterSurgical instrument detailsRf ablationLesion progression
A system and method for opto-acoustic tissue and lesion assessment in real time on one or more of the following tissue characteristics: tissue thickness, lesion progression, lesion width, steam pop, and char formation, system includes an ablation element, laser delivery means, and an acoustic sensor. The invention involves irradiating tissue undergoing ablation treatment to create acoustic waves that have a temporal profile which can be recorded and analyzed by acoustic sampling hardware for reconstructing a cross-sectional aspect of the irradiated tissue. The ablation element (e.g., RF ablation), laser delivery means and acoustic sensor are configured to interact with a tissue surface from a common orientation; that is, these components are each generally facing the tissue surface such that the direction of irradiation and the direction of acoustic detection are generally opposite to each other, where the stress waves induced by the laser-induced heating of the tissue below the surface are reflected back to the tissue surface.
Owner:BIOSENSE WEBSTER INC
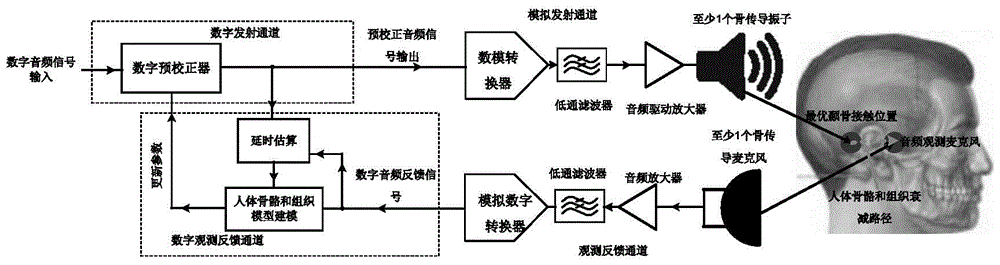
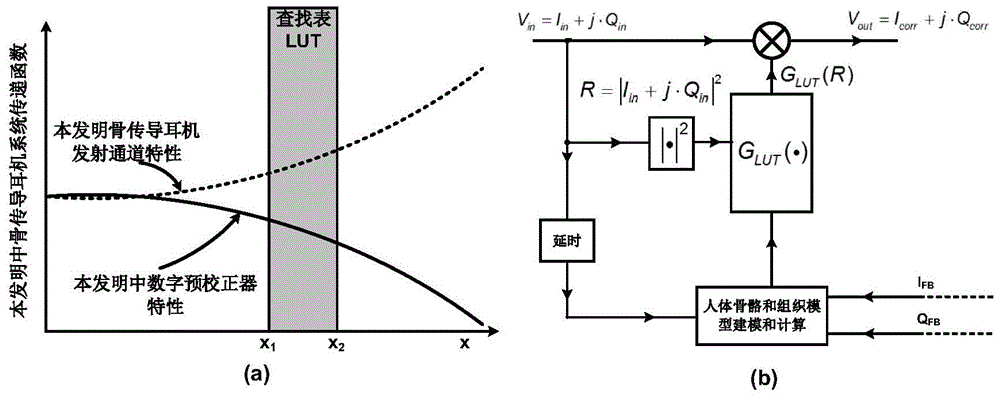
Bone conduction headset and audio processing method thereof
InactiveCN105721973ASimplify complexityReduce production processBone conduction transducer hearing devicesEarpiece/earphone attachmentsLow-pass filterBone conduction hearing
The invention discloses an audio processing method for a bone conduction headset, the bone conduction headset and an audio playback device based on the bone conduction headset. The bone conduction headset comprises a human bone and tissue model modeling module, a digital pre-corrector, a delay estimation unit, a digital-to-analog converter, an analog-digital converter, a first low-pass filter, a second low-pass filter, an audio amplifier, an audio driving amplifier, at least one bone conduction microphone, and at least one bone conduction vibrator. In the method, human bone and tissue attenuation effect information of different users is detected in real time; a compensating transfer function is generated based on the attenuation effect information; and an input audio signal is subjected to digital pre-correction via the compensating transfer function, and then the processed input audio signal is transmitted in human bones and tissues. Through adoption of the method, a problem that experience of the bone conduction headset is different caused by different tissue thickness of the different users is solved.
Owner:王泽玲
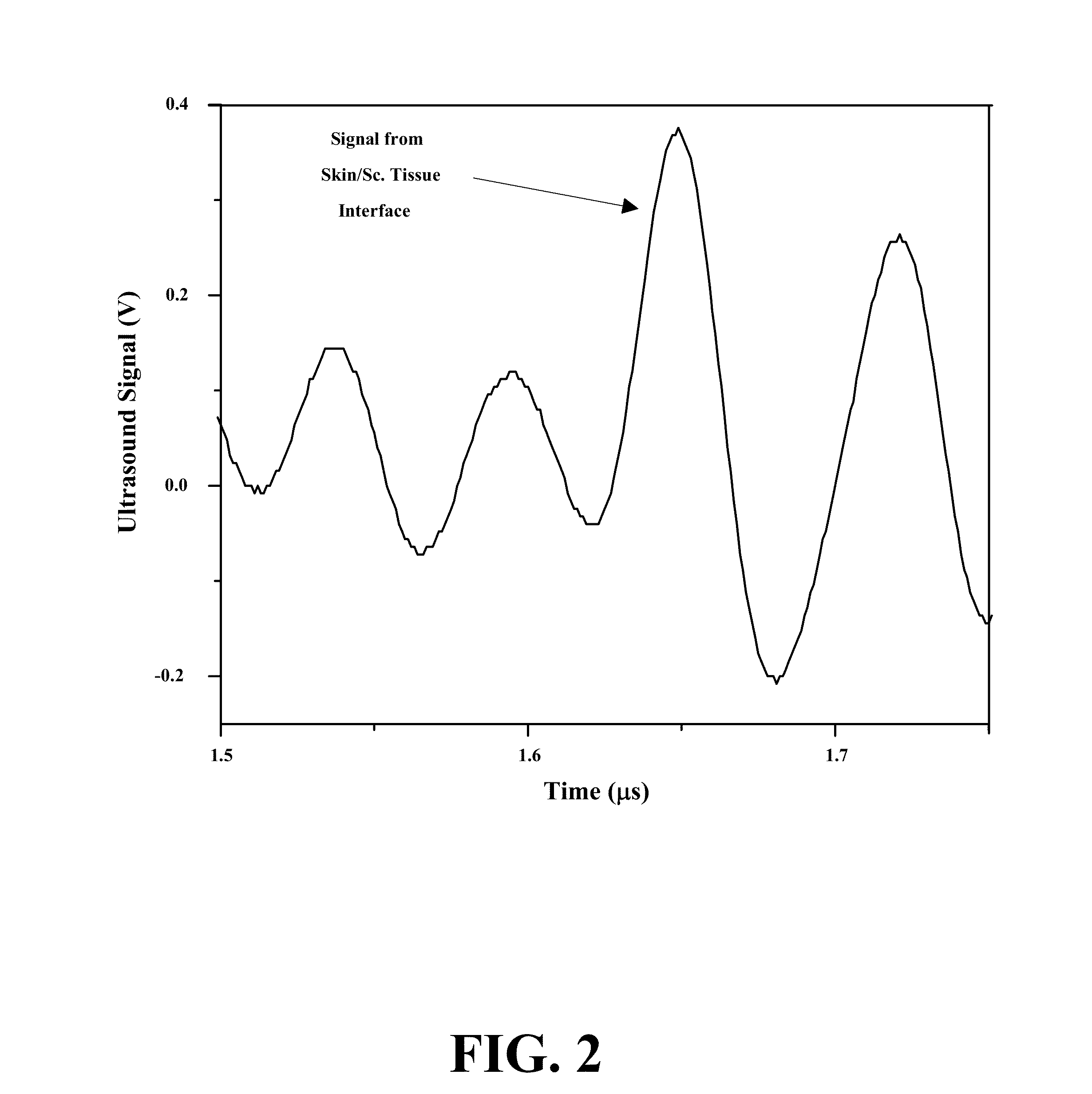
Tissue thickness measurement device
InactiveUS20060184024A1Accurate measurementAccurate distributionUltrasonic/sonic/infrasonic diagnosticsInfrasonic diagnosticsMeasurement deviceUltrasonic sensor
A device is described that can be easily used to accurately measure and monitor tissue thickness using ultrasound. The device comprises a remote control and data processing unit, a handheld ultrasound transducer, a display monitor and means for effectively coupling ultrasound to tissue.
Owner:INTELAMETRIX
Volume rendering of medical images
Certain embodiments provide a photo-realistic rendering apparatus and method. An illumination model is used that includes placing a synthetic or virtual light source adjacent a region of tissue of interest in order to visualize the thickness of the tissue by modeling how light from the virtual light source interacts with the tissue of interest, through effects including absorption and scattering, as light emitted from the light source travels through the tissue of interest to a view point of view plane. It is simulated how some light is absorbed making tissue regions that are thicker darker (since more of the light is absorbed and the intensity reduces) and more red (since tissue tends to absorb blue and green wavelengths more strongly than red wavelengths and this chromatic effect is incorporated in the illumination model). A 2D image can thus be provided in which the color and intensity of light propagating through the tissue provides visual feedback on the tissue thickness.
Owner:TOSHIBA MEDICAL SYST CORP
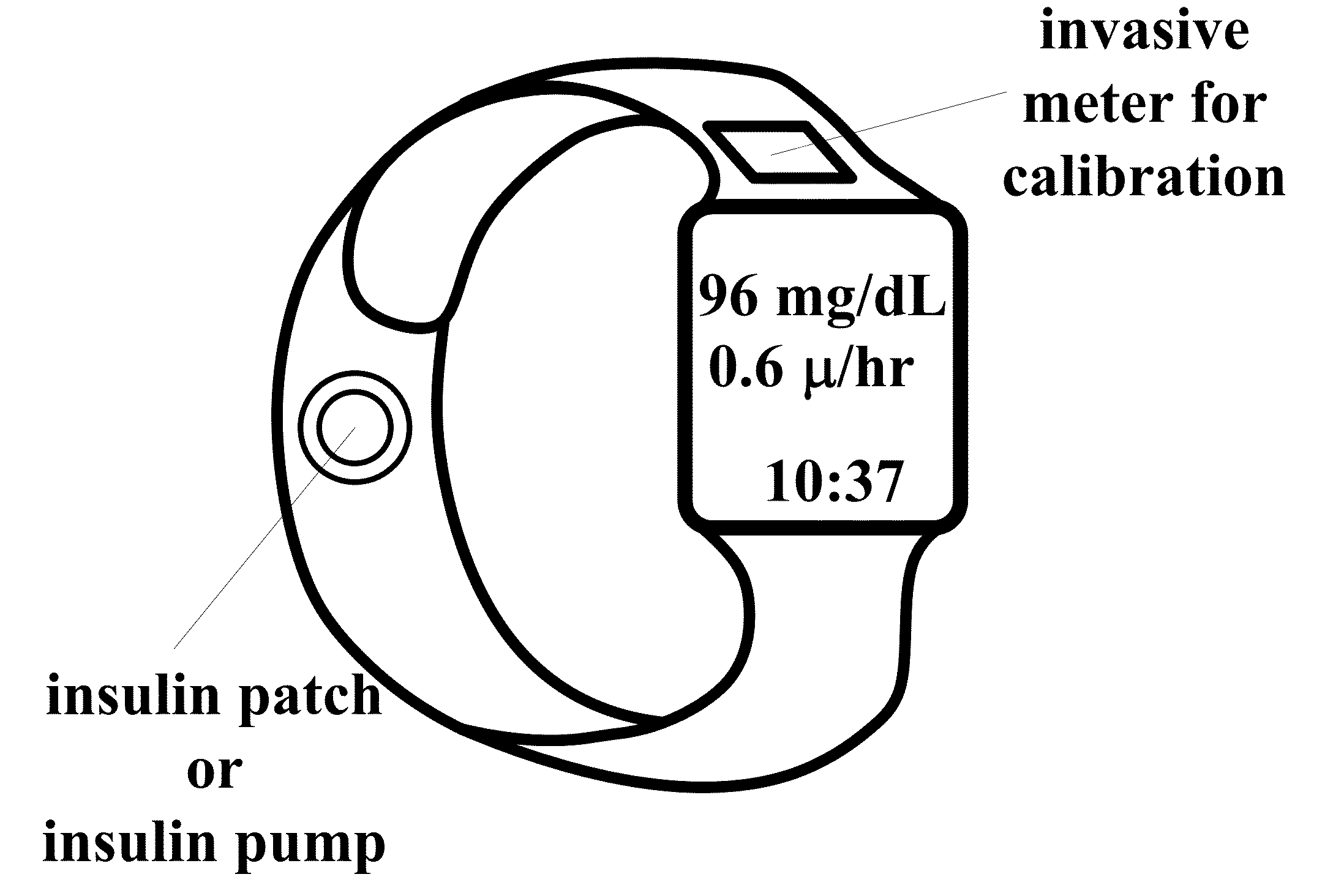
Wearable, noninvasive glucose sensing methods and systems
ActiveUS20160192867A1Improve ease and safetyReduce morbidityDiagnostics using lightHealth-index calculationGlucose polymersUltrasonic testing
New wearable systems for noninvasive glucose sensing include an ultrasound generator, an ultrasound detector and a feedback unit. Methods for noninvasive glucose sensing using a wearable device include measuring a thickness (geometrical and / or optical) of a target tissue or a time of flight of ultrasound or optical pulses in the target tissue and determining a glucose value from the thickness of the target tissue or the time of flight in the target tissue in accordance with a target tissue thickness (geometrical and / or optical) or time of flight versus glucose calibration curve.
Owner:ESENALIEV RINAT O
Acoustic transducer for pulse-echo monitoring and control of thermally ablative lesioning in layered and nonlayered tissues, catheter contact monitoring, tissue thickness measurement and pre-pop warning
InactiveUS20120265069A1Reduce manufacturing costSmall in French diameterUltrasonic/sonic/infrasonic diagnosticsUltrasound therapyMedicineTransducer
An ablation catheter with acoustic monitoring comprises an elongated catheter body; a distal member disposed adjacent a distal end and including an ablation element to ablate a biological member at a target region outside the catheter body; and one or more acoustic transducers each configured to direct an acoustic beam toward a respective target ablation region and receive reflection echoes therefrom. The distal member includes a transducer housing in which the acoustic transducers are disposed, the transducer housing including at least one transducer window which is the only portion in the distal member through which the acoustic beam passes, at least the at least one transducer window portion of the distal member being made of a material comprising at least 50% carbon by volume, the transducer window material having an acoustic impedance between that of the acoustic transducers and that of the biological member.
Owner:ST JUDE MEDICAL
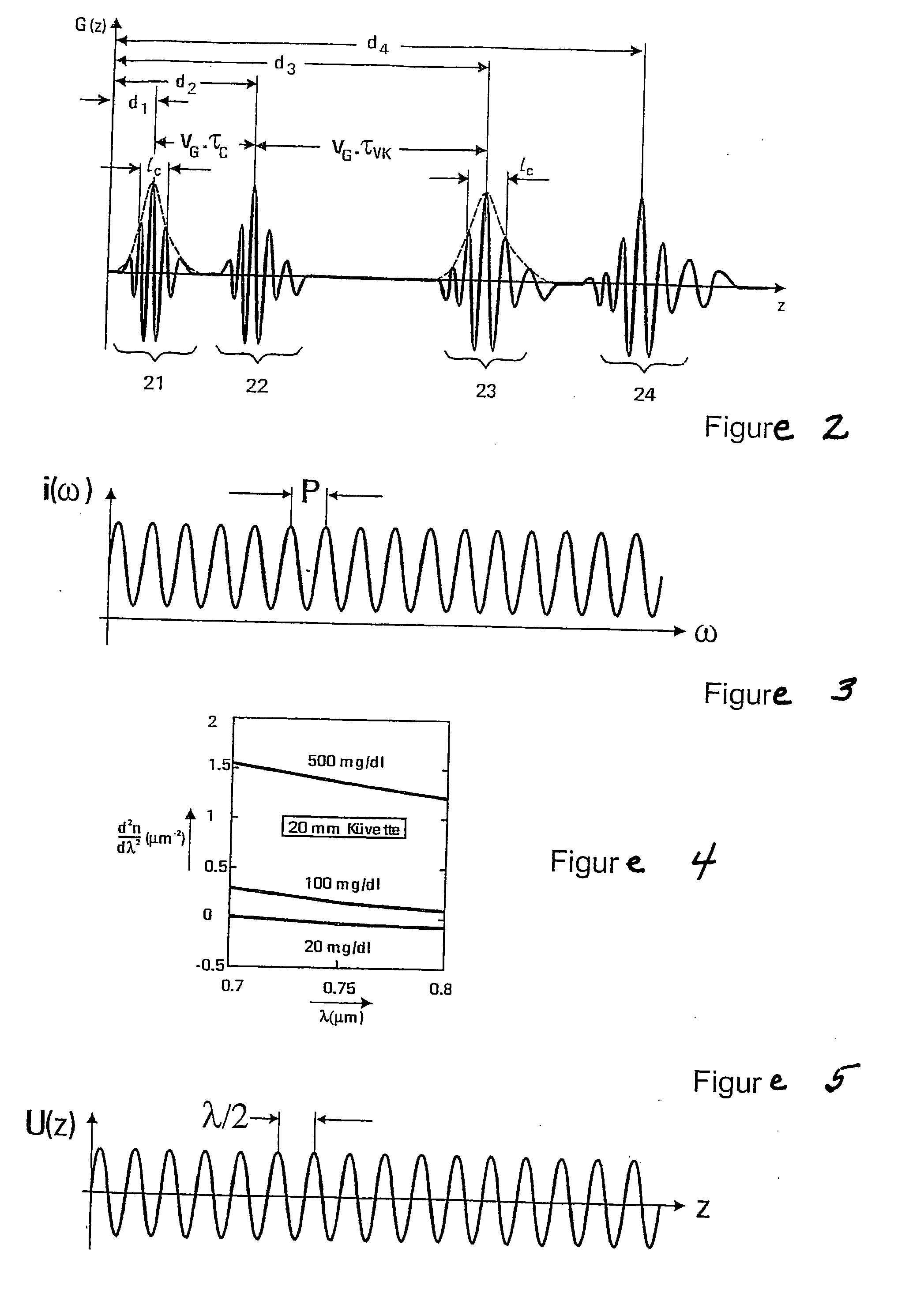
Method and assembly for measuring a dispersion in transparent media
InactiveUS20060244972A1Reliable and accurate measurementEasy to useDiagnostic recording/measuringSensorsBeam splitterGlucose Measurement
Spatially localized dispersion measurement and glucose measurement by means of optical short-coherence interference refractometry. This application is directed to methods and arrangements for the measurement of the dispersion and of the glucose content in transparent and partially transparent tissues and body fluids. Methods of short-coherence interferometry and spectral interferometry are modified for the measurement of tissue thickness and for the measurement of local dispersion. In the technique based on short-coherence interferometry, partial interferograms from the short-coherence interferogram G(τ) are used for the dispersion measurement. In the technique based on spectral interferometry, partial areas from the ω-spectrum of the spectral interferogram are used for the dispersion measurement. FIG. 6 shows an arrangement based on spectral interferometry. A temporally short-coherence light source illuminates the modified Michelson interferometer. The beam splitter splits the illuminating beam into a measurement beam and a reference beam. The light waves and reflected from the interferometer impinges on the spectrometer at the interferometer output. The registered spectral interferogram i(ω) forms the basis for the calculation of the dispersion of different orders. The viewing direction of the eye of the subject is fixated by means of a target beam.
Owner:CARL ZEISS MEDITEC AG
Coated hypodermic needle
ActiveUS20090171304A1Surgical needlesSurgical instrument detailsHypodermic needleLocalization system
A needle for a medical procedure includes a shaft with an inner surface, an outer surface, a proximal section, and a distal section. The distal section has a conductive tip configured to be a first electrode for voltage measurement. The needle further includes a first electrically insulative outer layer over a portion of the outer surface of the shaft. The conductive tip is adapted for insertion through tissue into, for example, a pericardial space of a patient. A system for determining the location of a needle during a medical procedure includes the needle and an anatomical mapping and localization system electrically coupled to the needle and adapted to measure voltage at the conductive tip. A system for determining tissue thickness during a medical procedure includes the needle, an anatomical mapping and localization system electrically coupled to the needle, and an electrocardiograph operatively coupled to the needle and adapted to monitor electrical activity at the conductive tip and at the second electrode. The needle may include a second electrode.
Owner:ST JUDE MEDICAL ATRIAL FIBRILLATION DIV
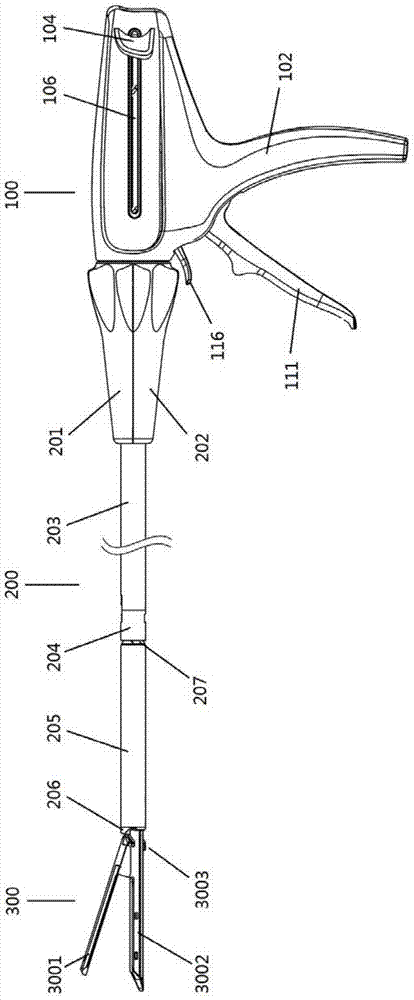
Surgical instrument capable of being operated by signal hand
ActiveCN103767751AIt has the advantage that the surgical instrument has an automatic reset functionWith automatic reset functionSurgical staplesSurgical forcepsEngineeringActuator
The invention provides a surgical instrument capable of being operated by a single hand. The surgical instrument comprises an actuator, a middle connecting body and a controller. The actuator, the middle connecting body and the controller are sequentially connected. The actuator comprises a nail bin assembly, a nail anvil assembly and a driving assembly. The controller comprises a firing trigger mechanism, a firing safety mechanism and an automatic reset mechanism. The surgical instrument has an automatic reset function; when the firing safety mechanism is not started and a doctor operates a firing trigger, the actuator of the surgical instrument can clamp tissue; when the doctor release the firing trigger, the actuator of the surgical instrument can automatically reset and release the clamped tissue. Due to the function, the surgical instrument enables the doctor to adjust the position, clamped by an anastomat, of the tissue conveniently through a single handle, also enables the doctor to improve the uniformity of the tissue thickness when thick tissue is clamped finally in the mode of repeatedly clamping the same part of the tissue, reduces tissue damage, and accordingly the meshing and cutting effects are improved.
Owner:SHANGHAI YISI MEDICAL TECH CO LTD +1
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com