Patents
Literature
Hiro is an intelligent assistant for R&D personnel, combined with Patent DNA, to facilitate innovative research.
54 results about "Cardiac monitors" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
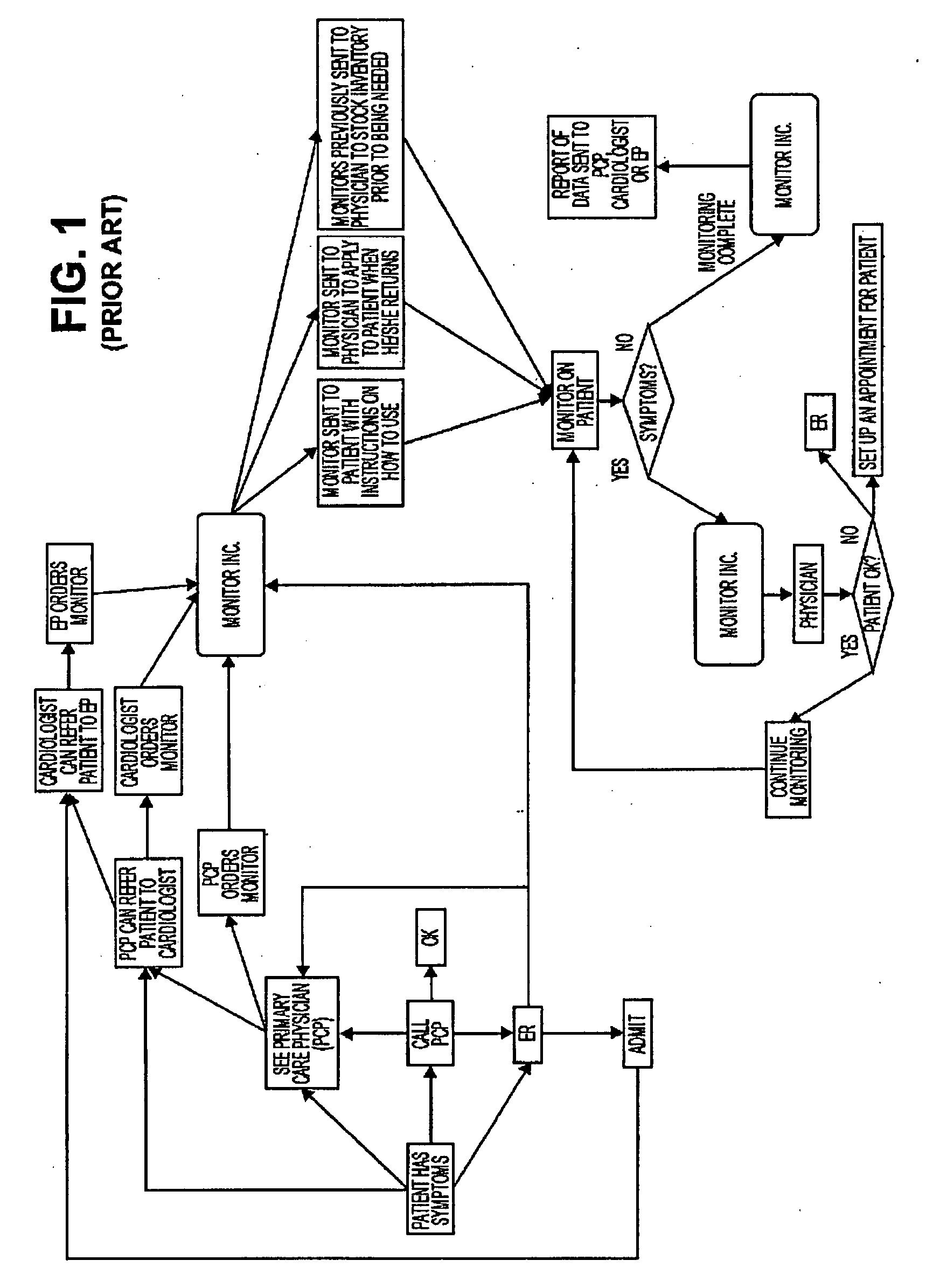
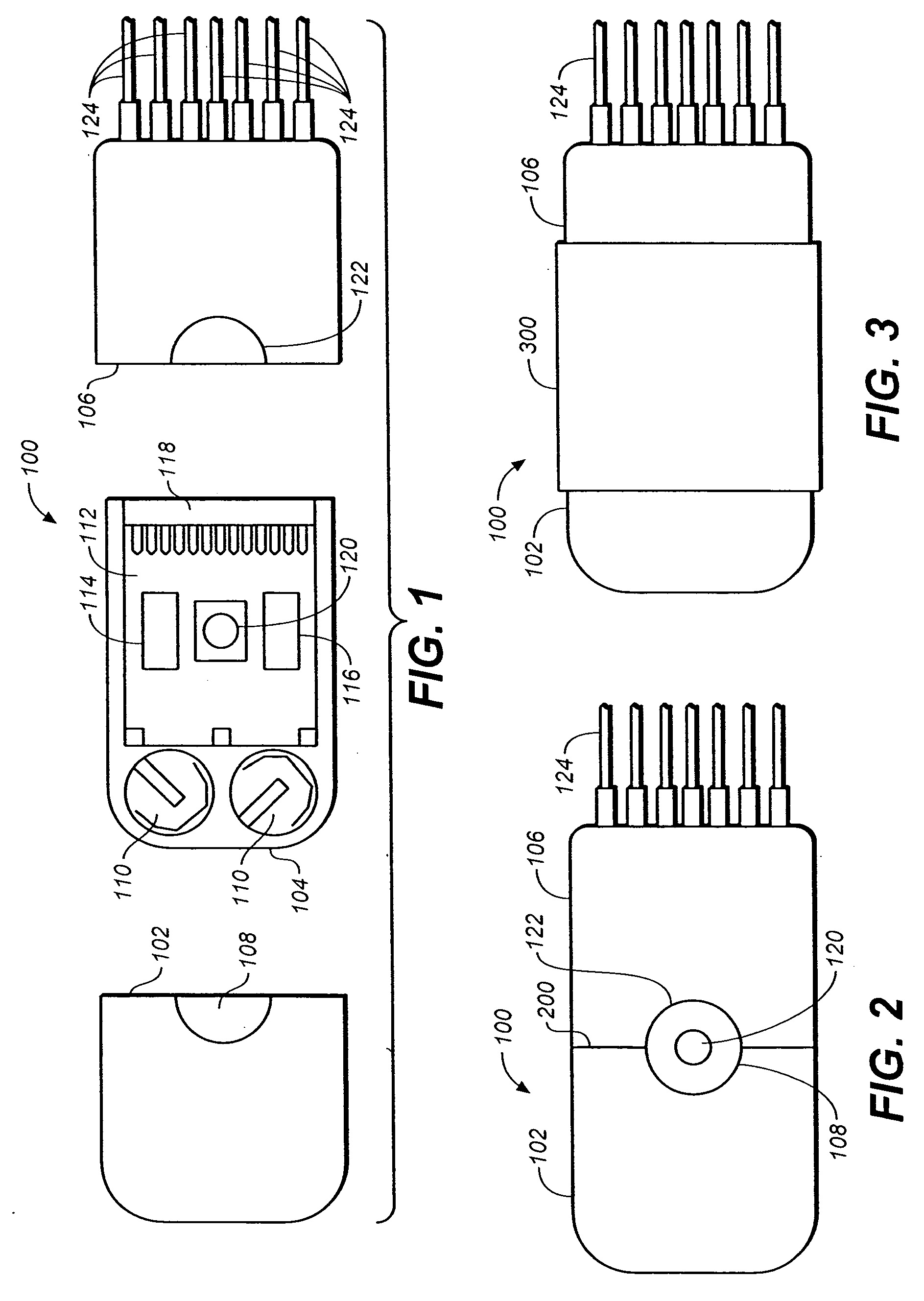
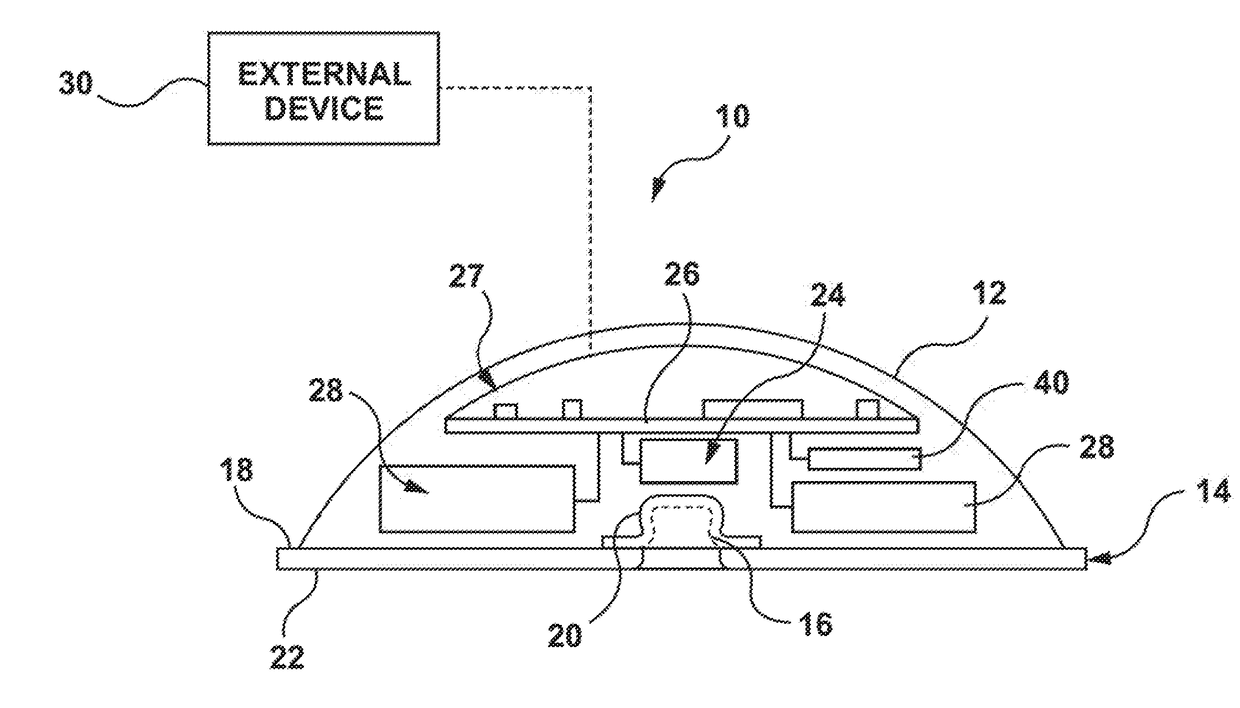
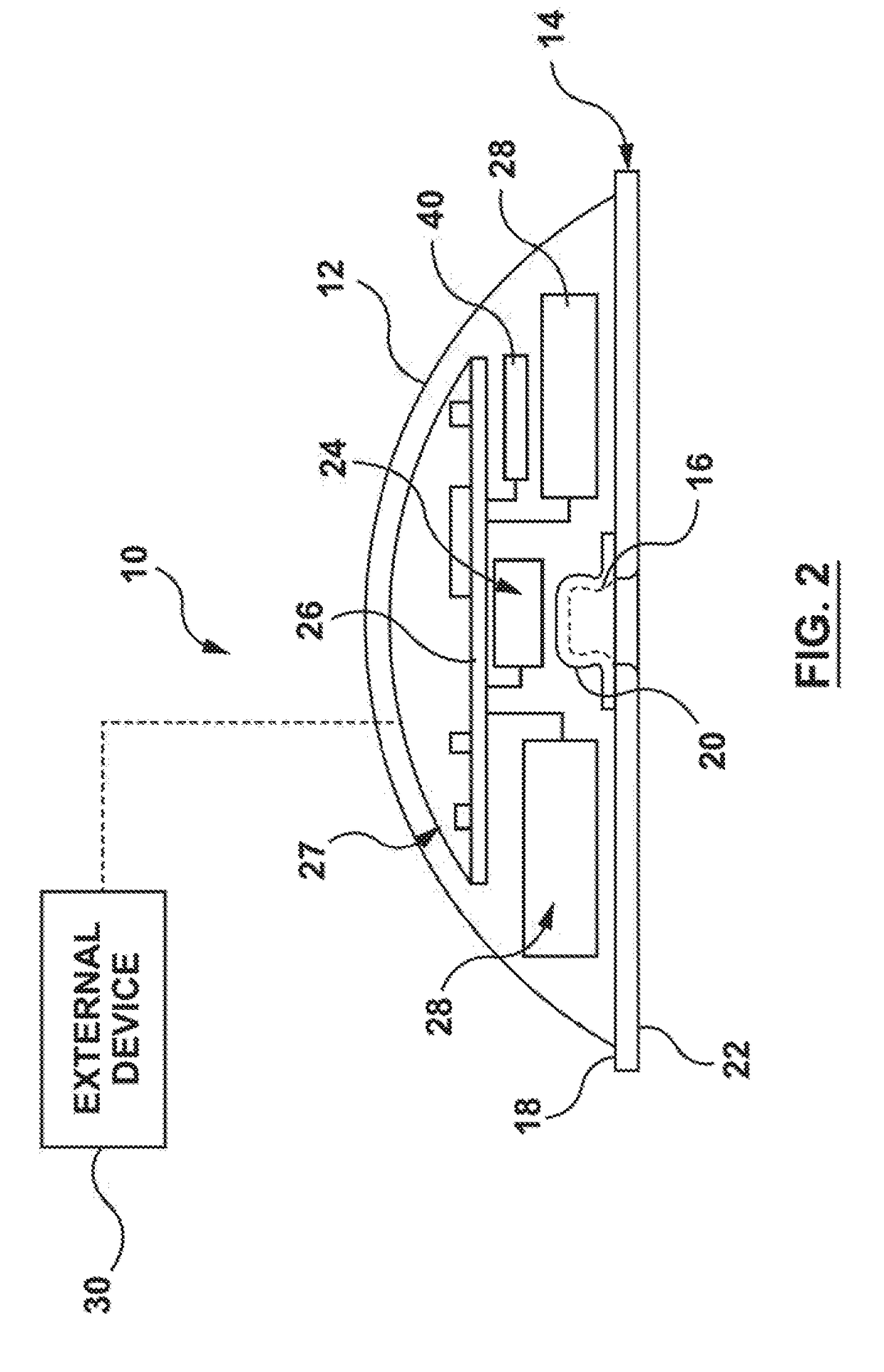
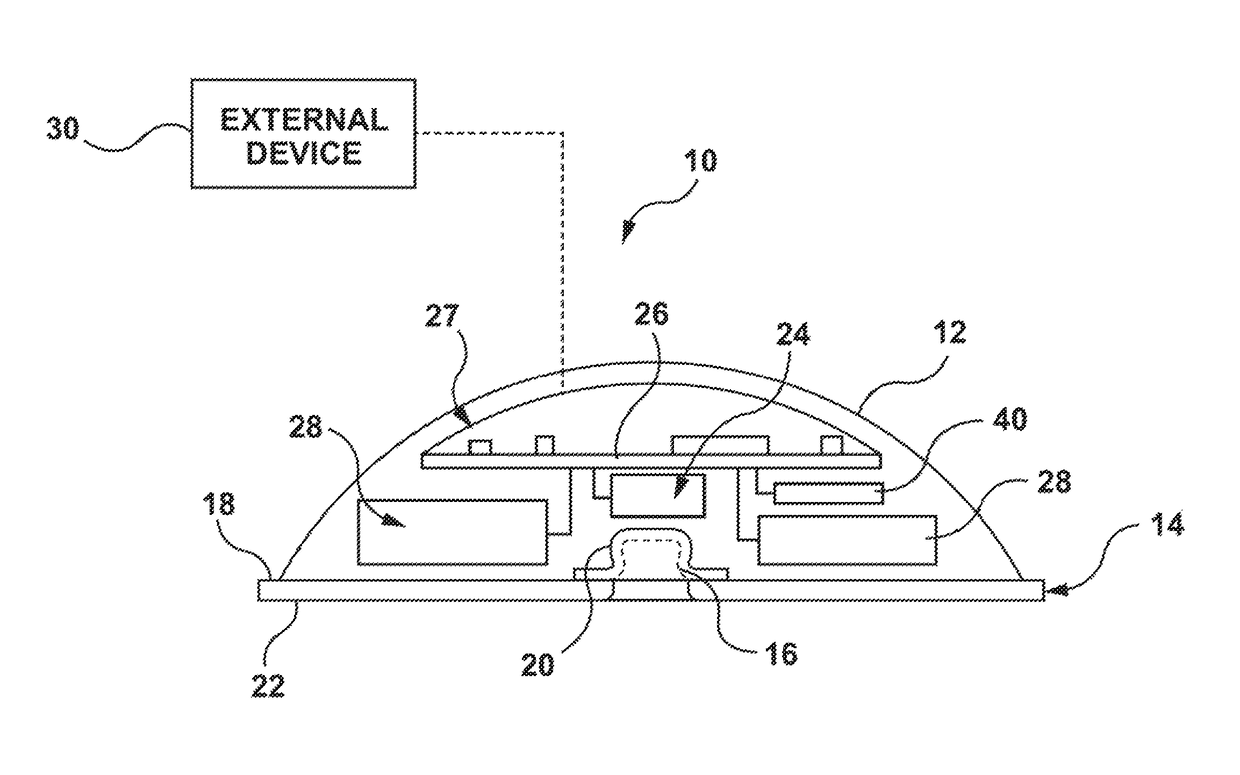
Non-invasive cardiac monitor and methods of using continuously recorded cardiac data
ActiveUS20070249946A1Improve fidelityElectrocardiographyLocal control/monitoringCardiac monitoringNon invasive
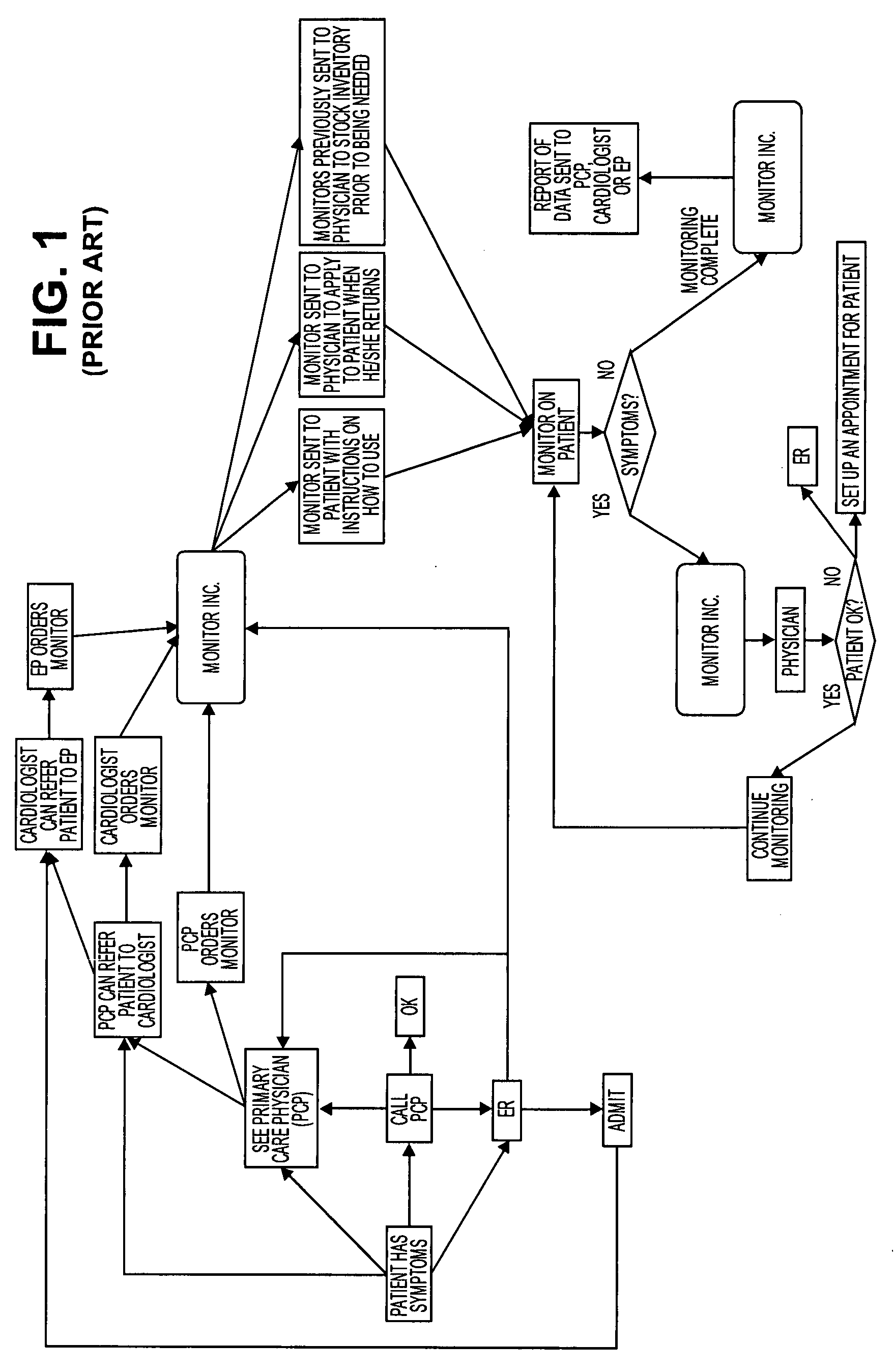
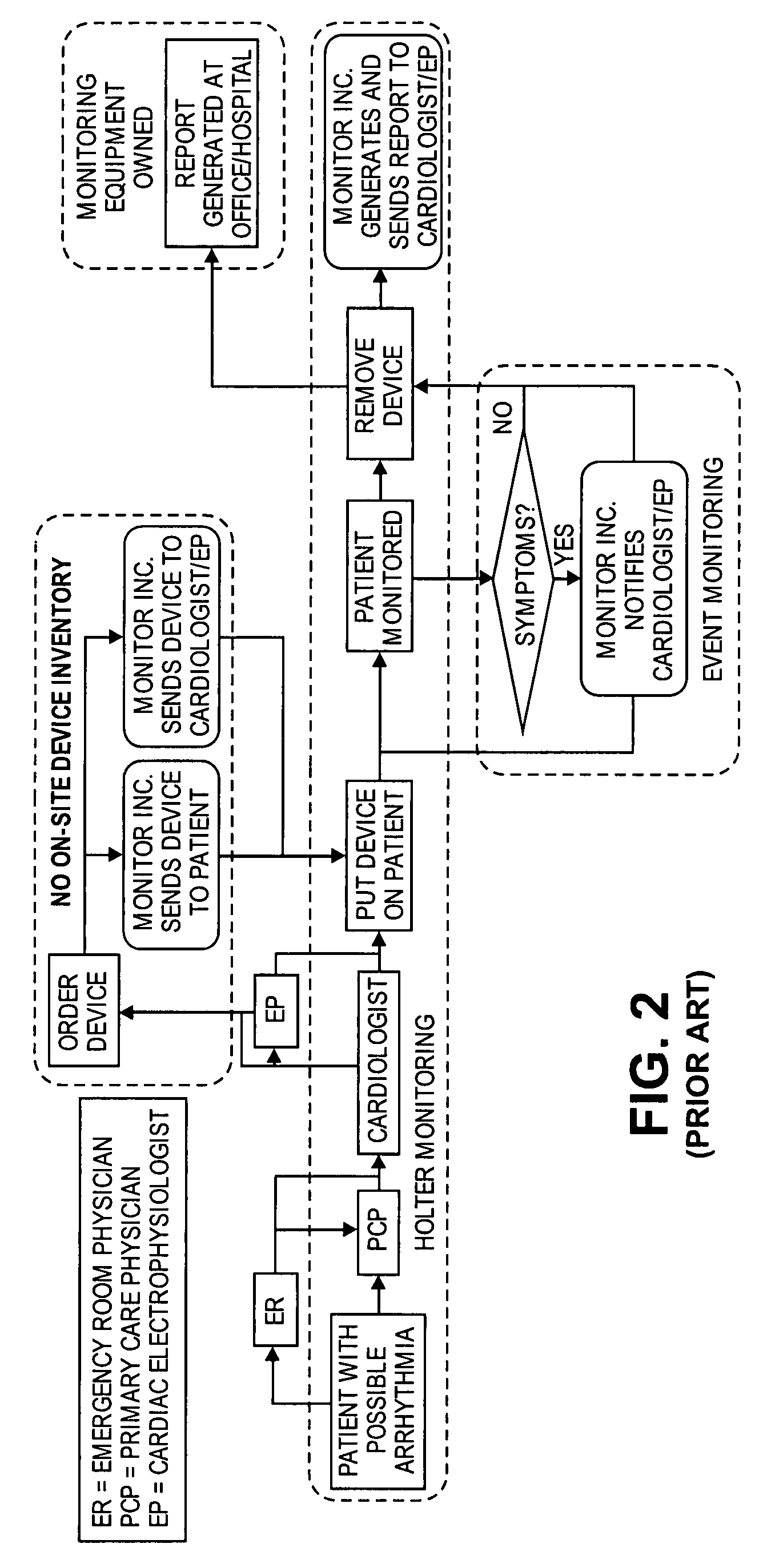
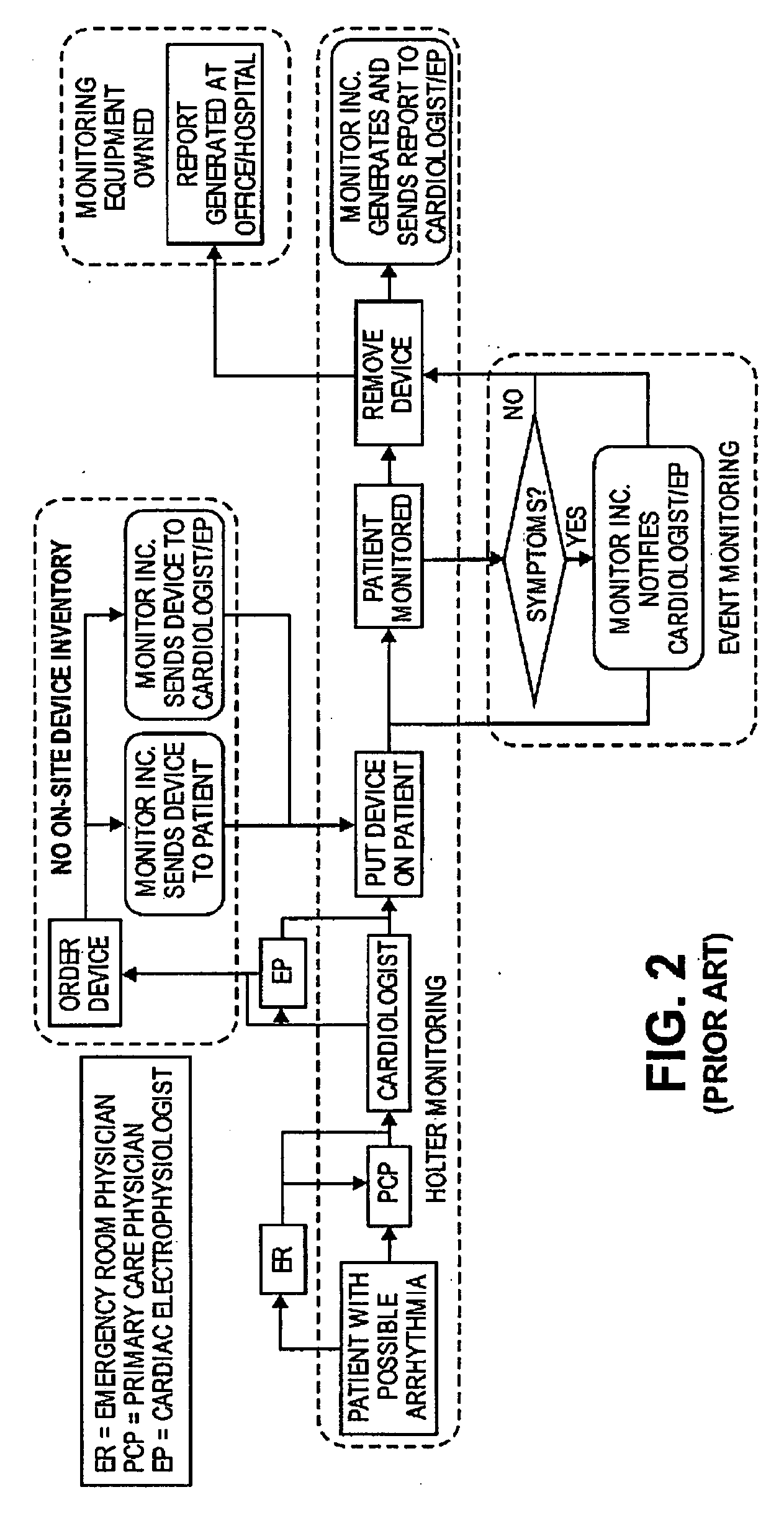
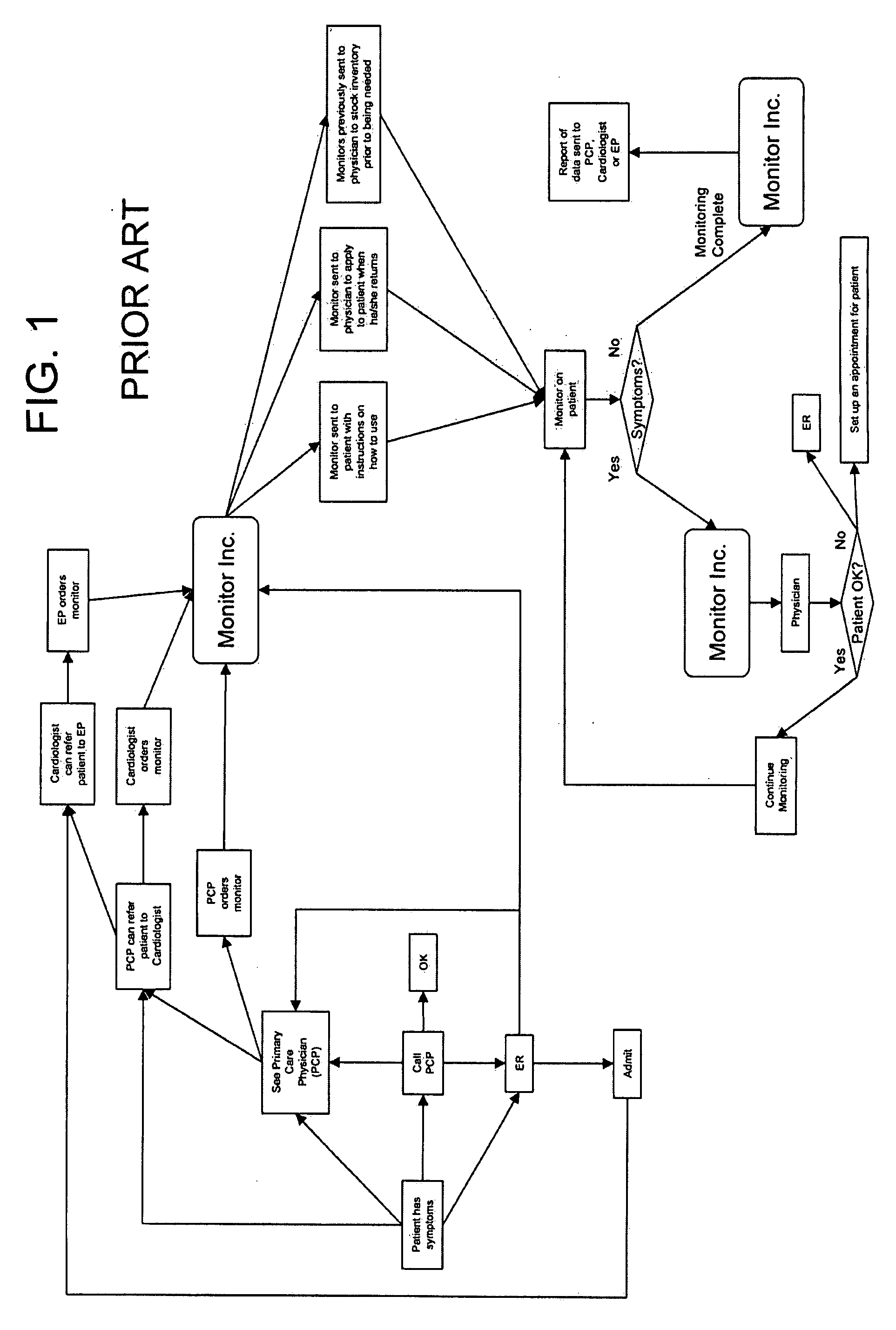
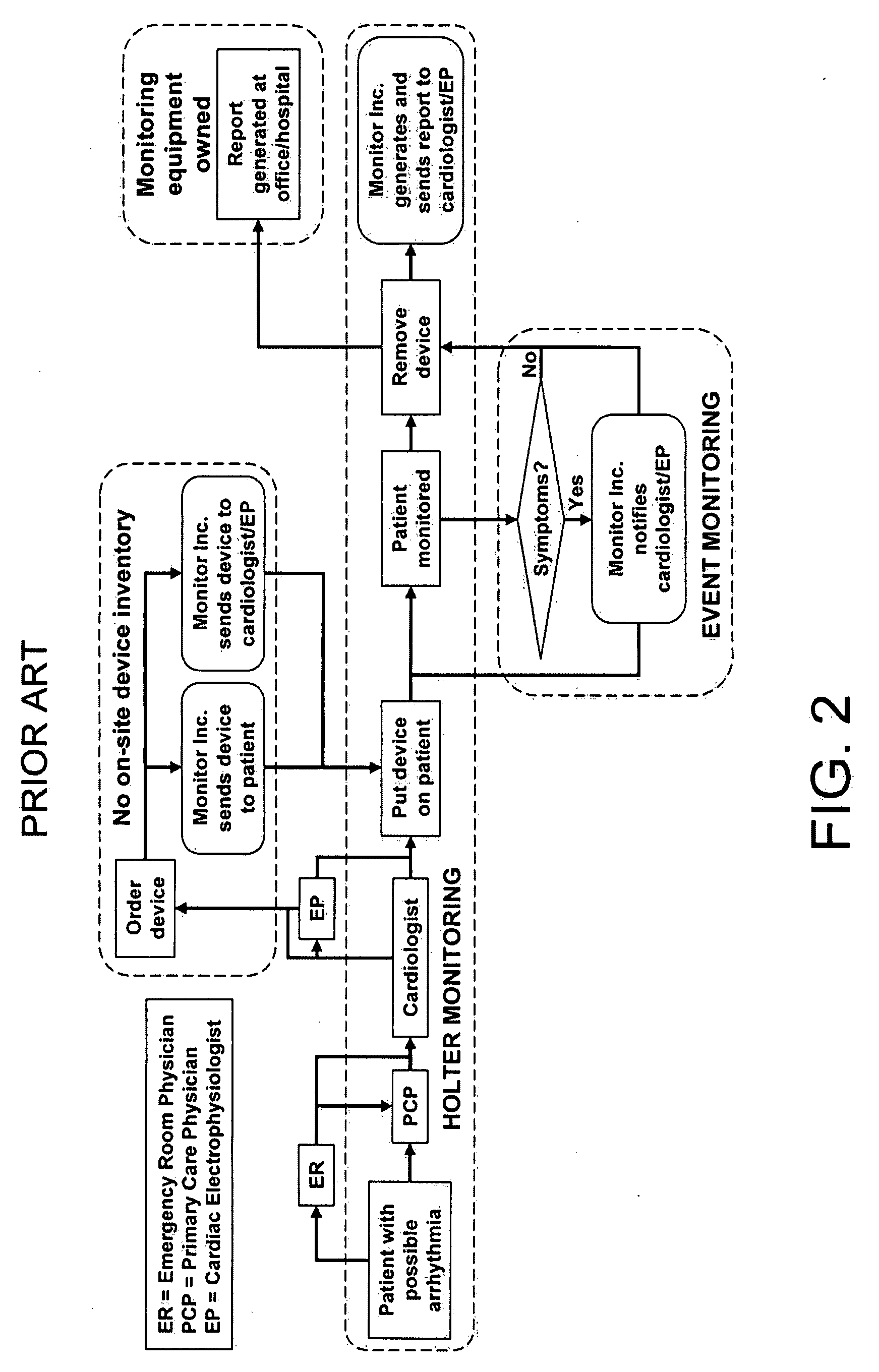
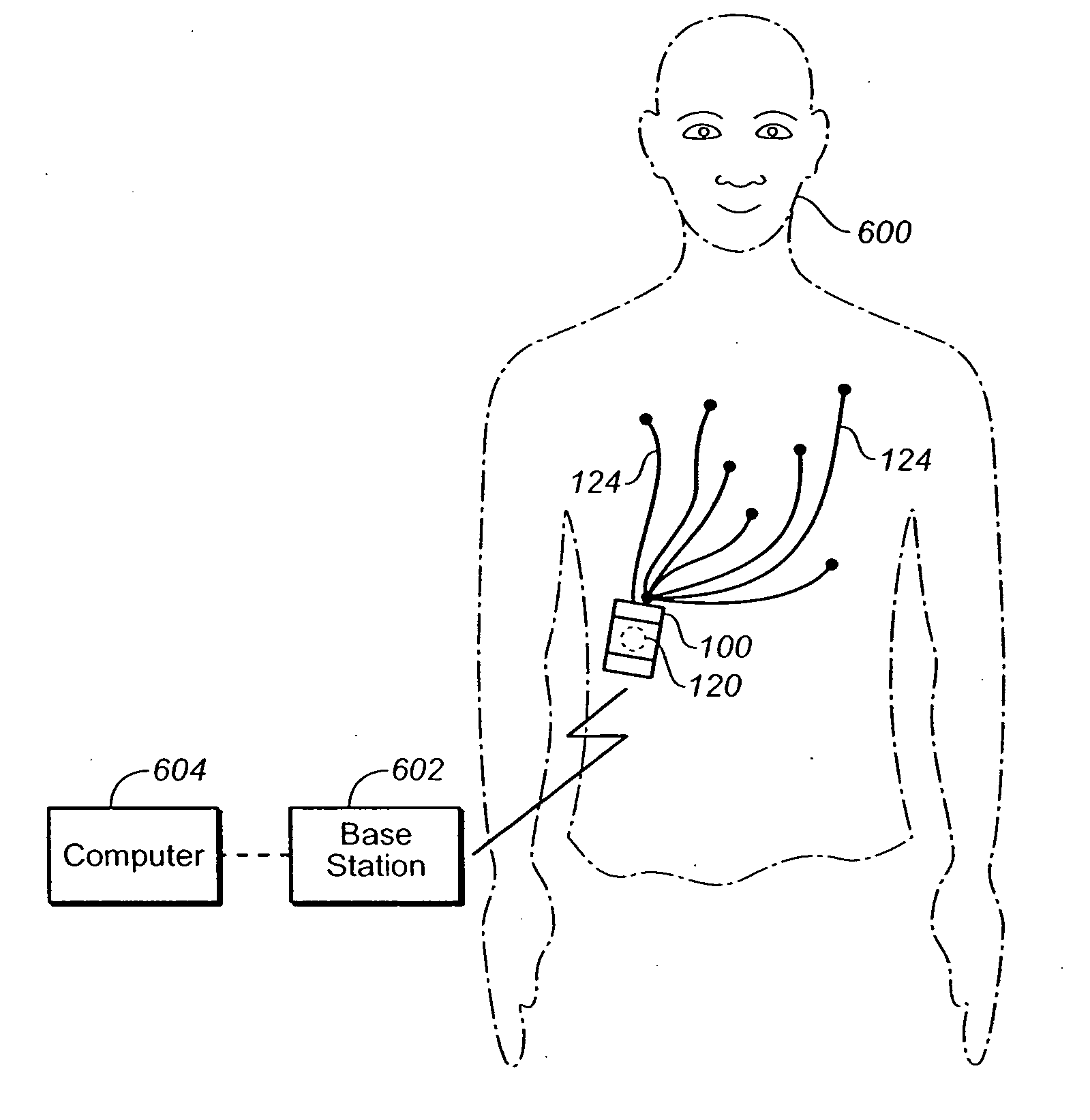
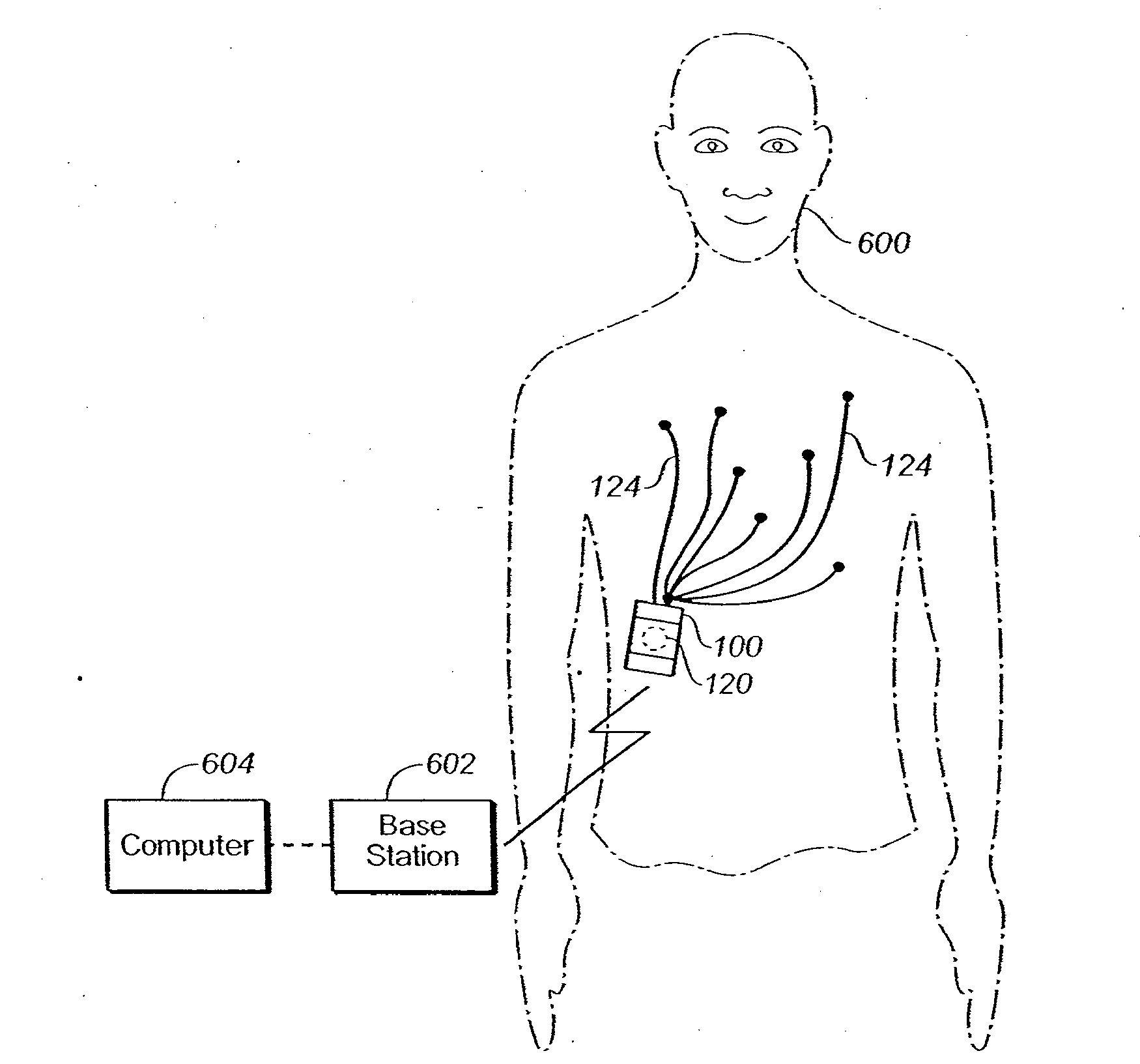
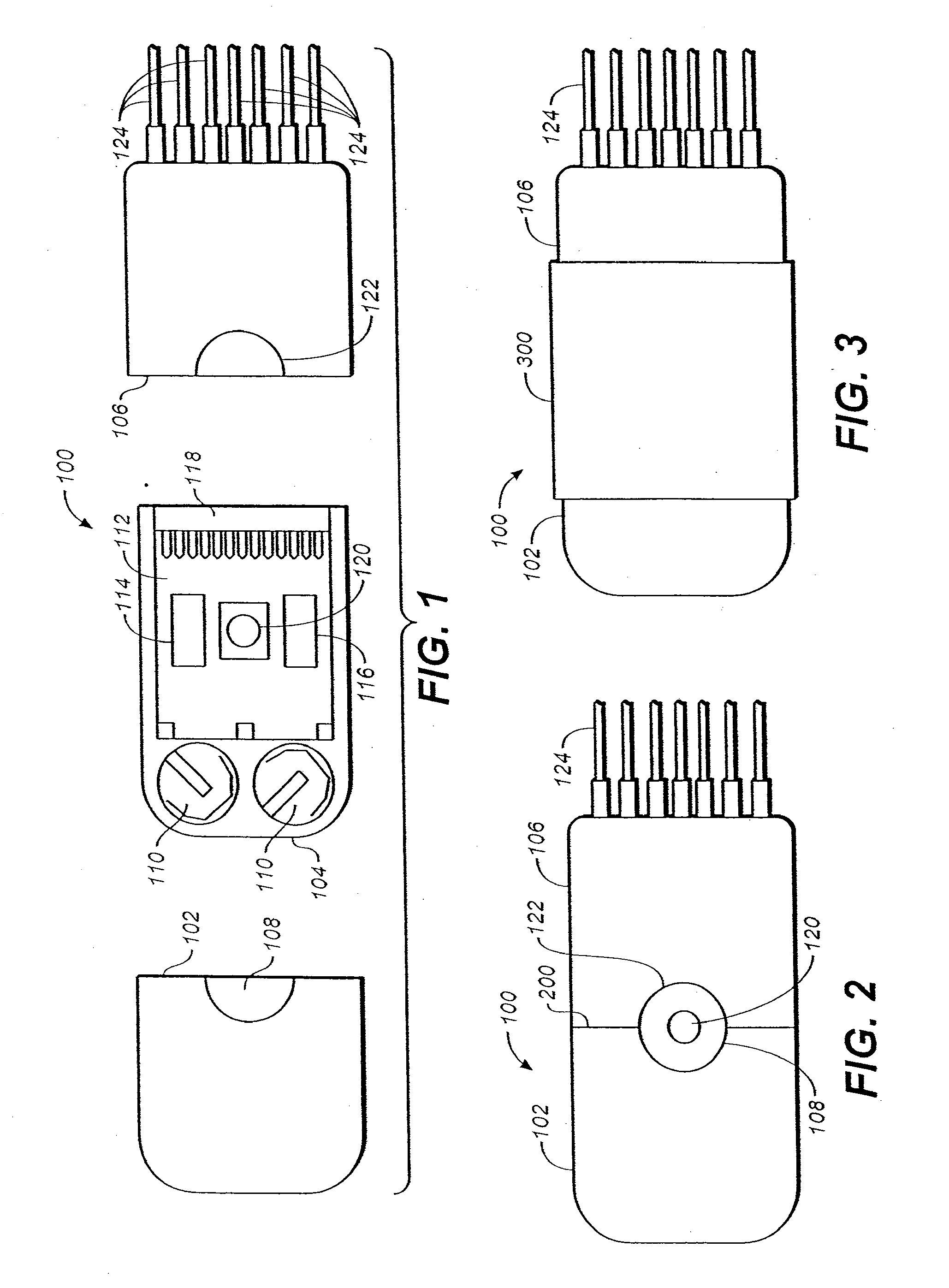
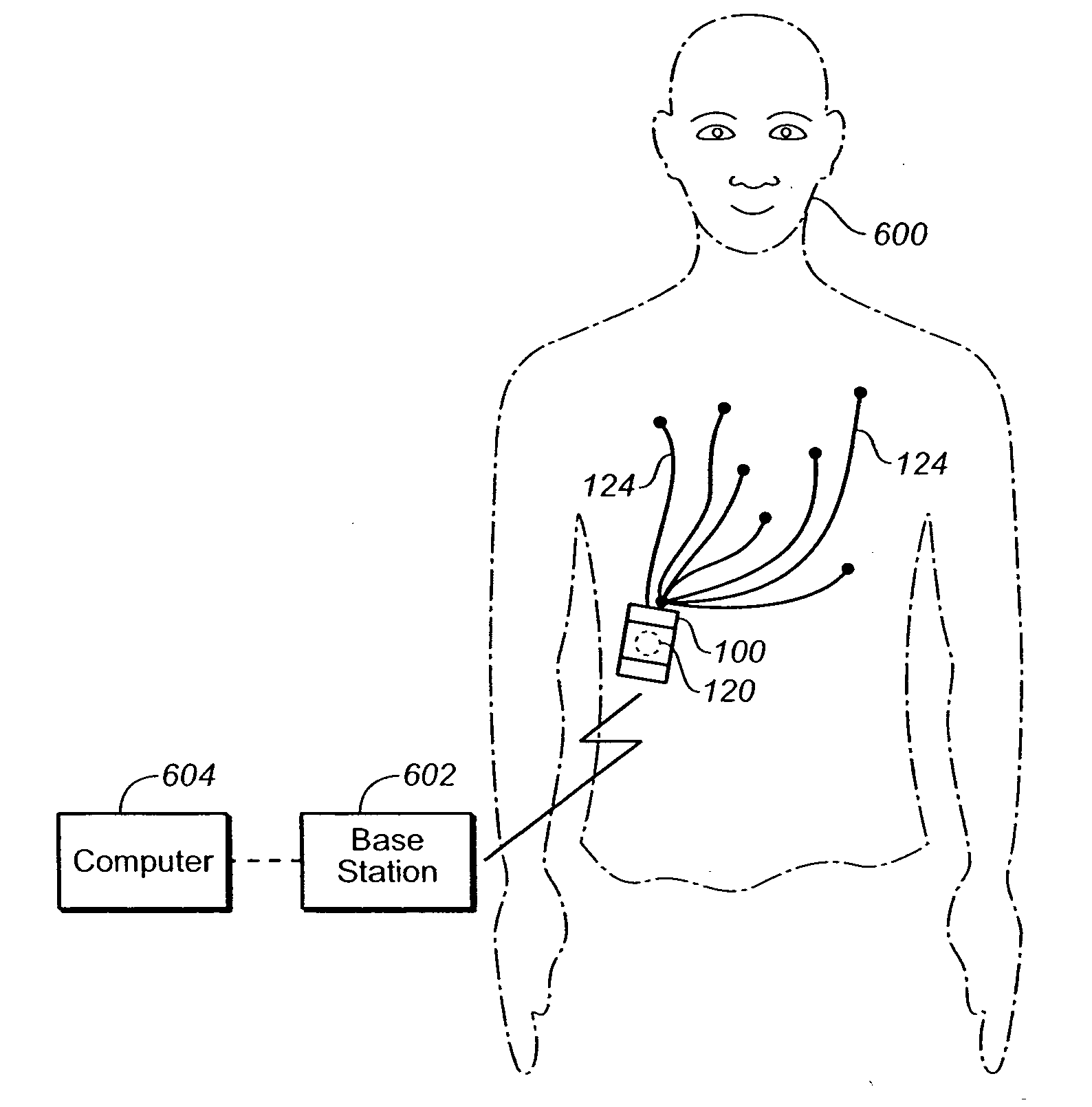
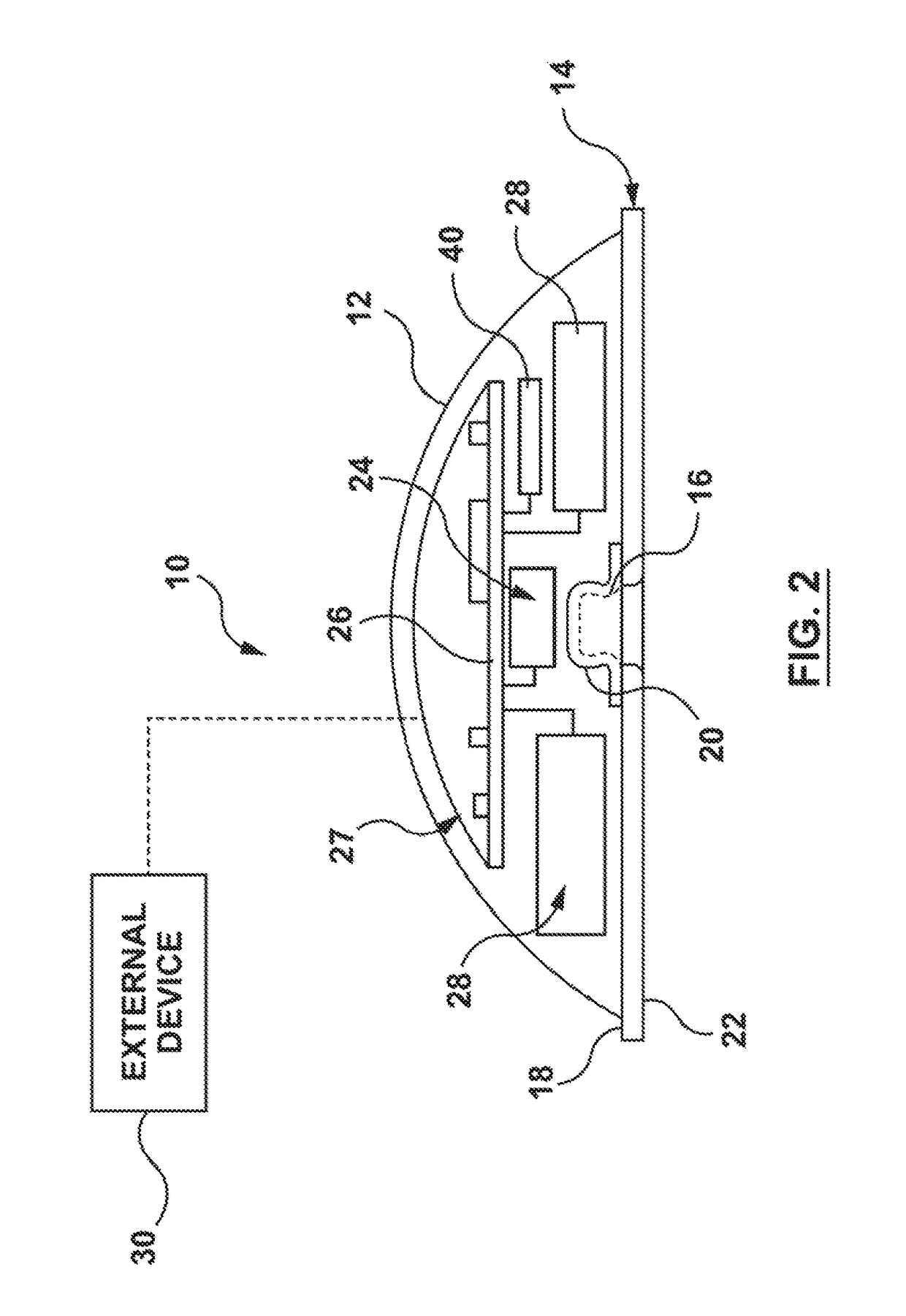
Embodiments of the invention provide methods of obtaining continuous cardiac information from a mammal. First, attach a self-contained, wearable, portable continuous cardiac monitor to the mammal to create a chamber containing electrodes used to detect cardiac signals from the mammal. Next, continuously detect without analyzing the cardiac signals from the mammal for at least 24 hours. Next, store information related to substantially all detected cardiac signals in the cardiac monitor.
Owner:THE BOARD OF TRUSTEES OF THE LELAND STANFORD JUNIOR UNIV
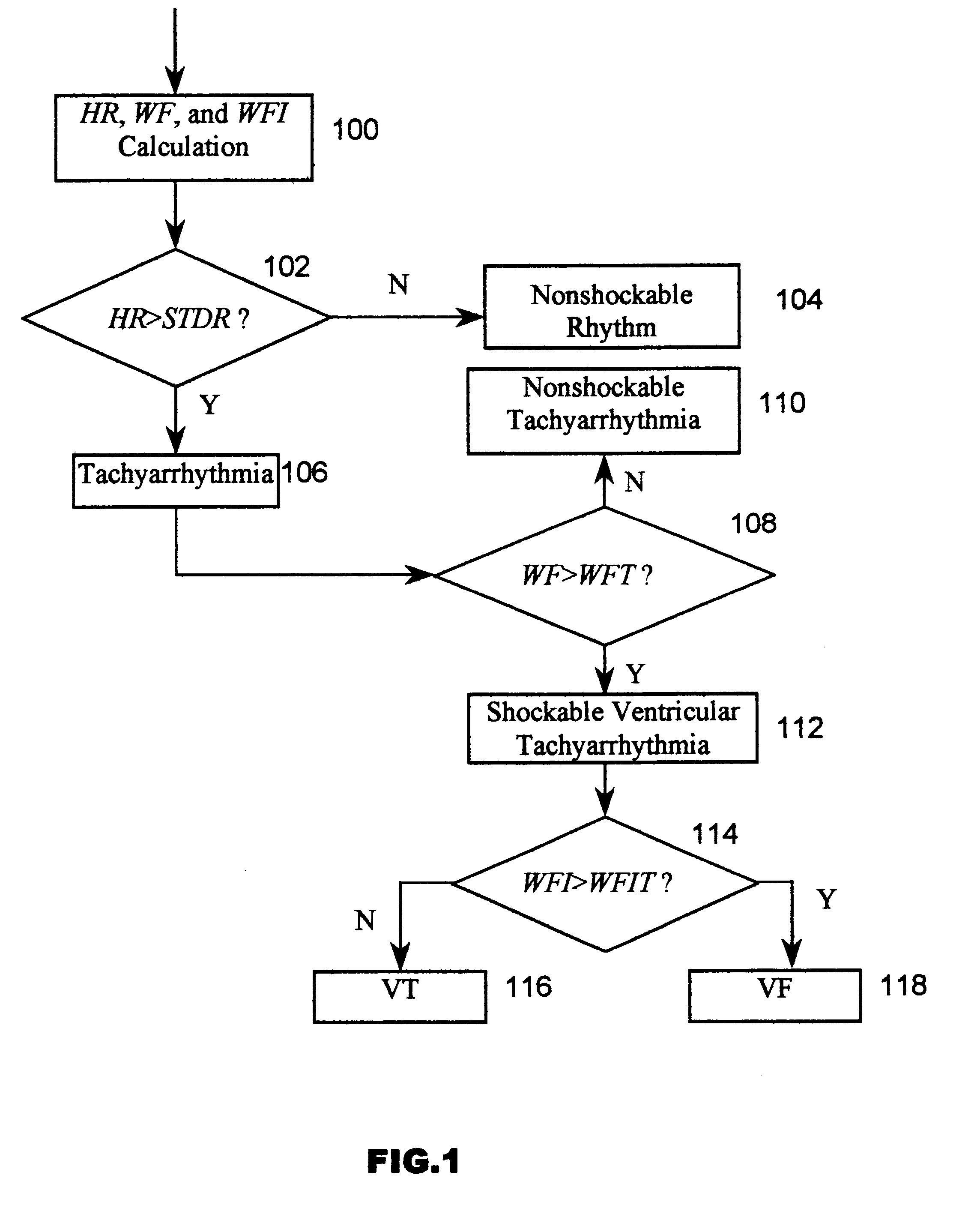
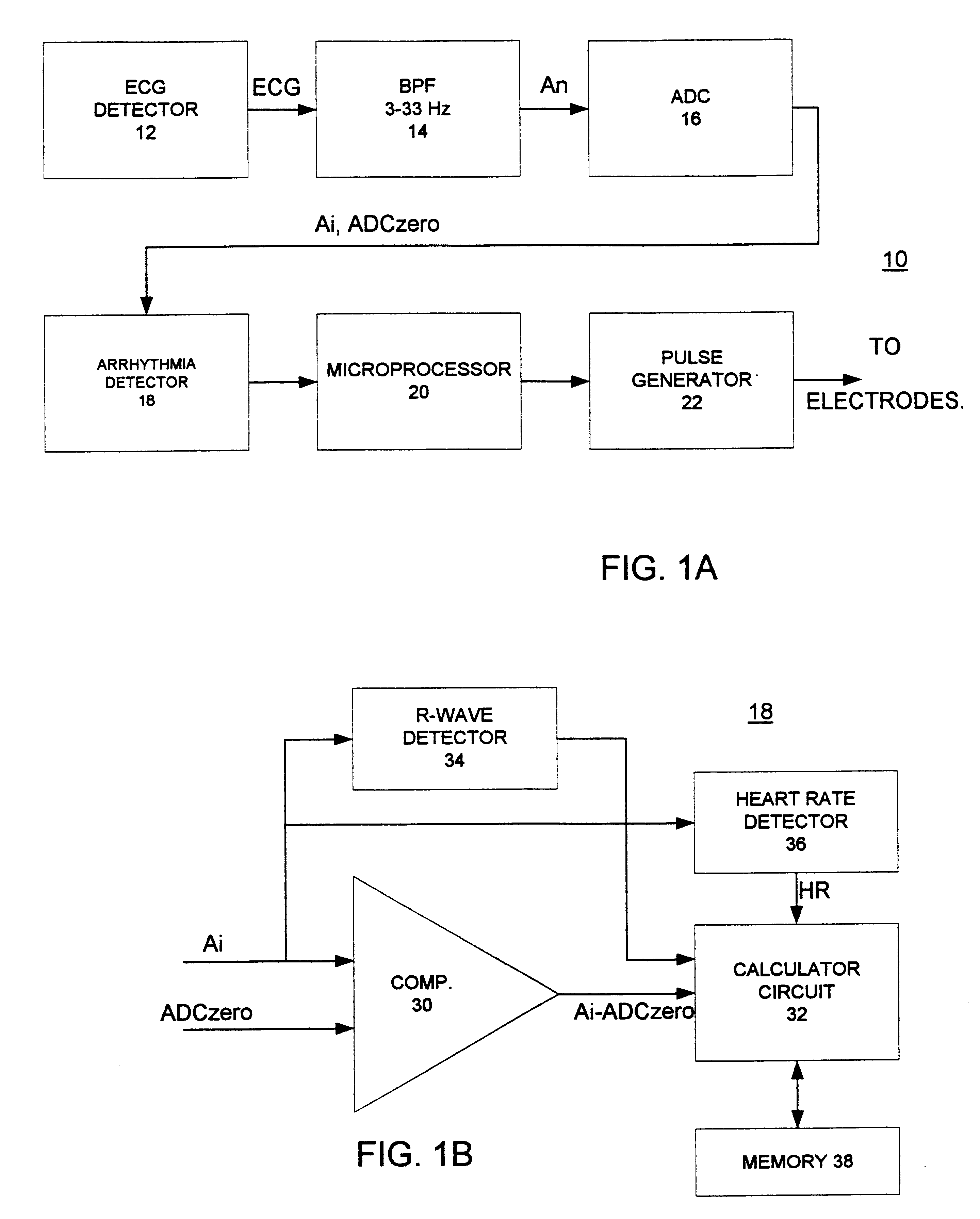
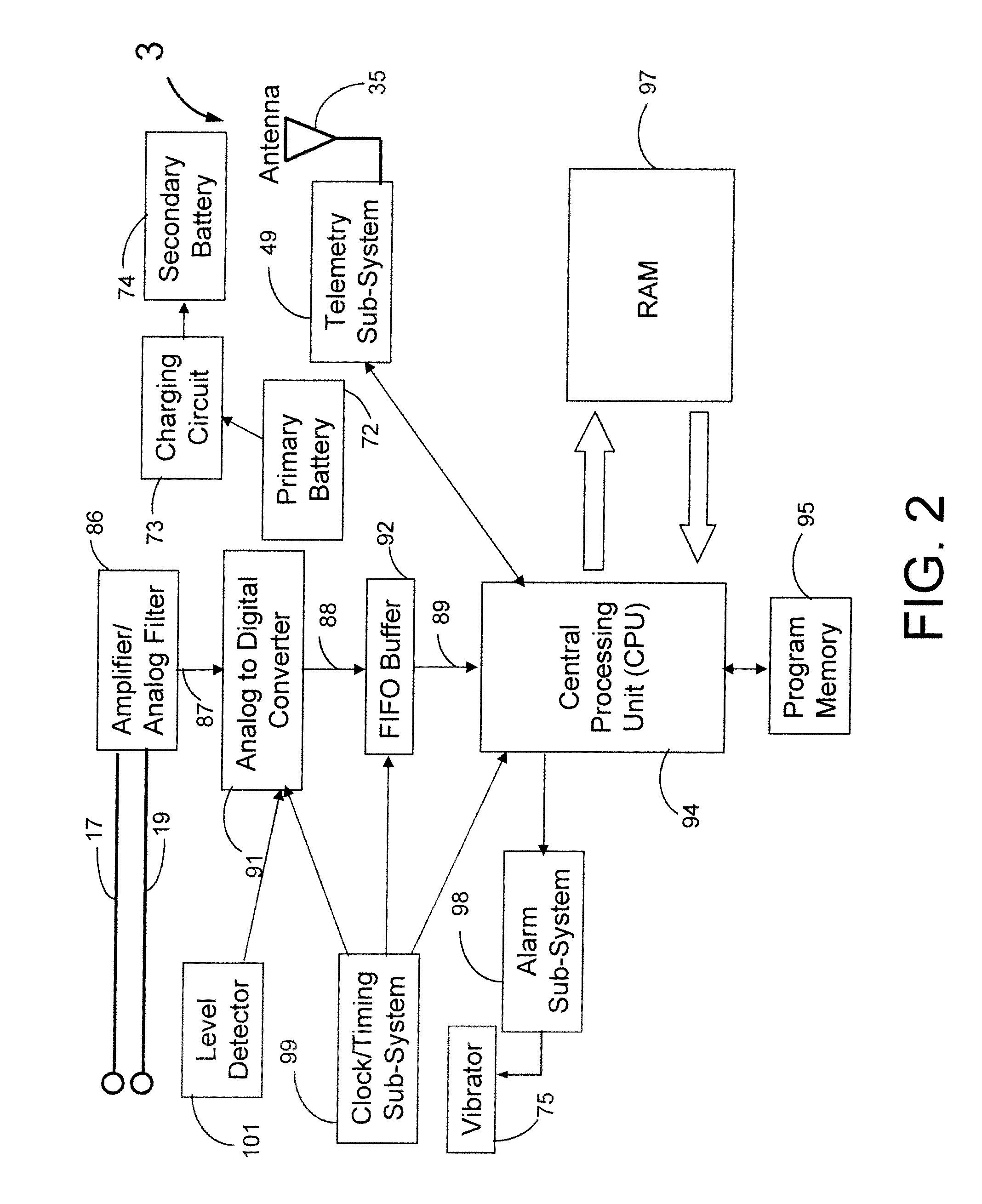
Cardiac arrhythmia detector using ECG waveform-factor and its irregularity
InactiveUS6480734B1Avoiding unnecessary shockSignificant energy savingElectrocardiographyHeart defibrillatorsVentricular tachycardiaCardiac monitoring
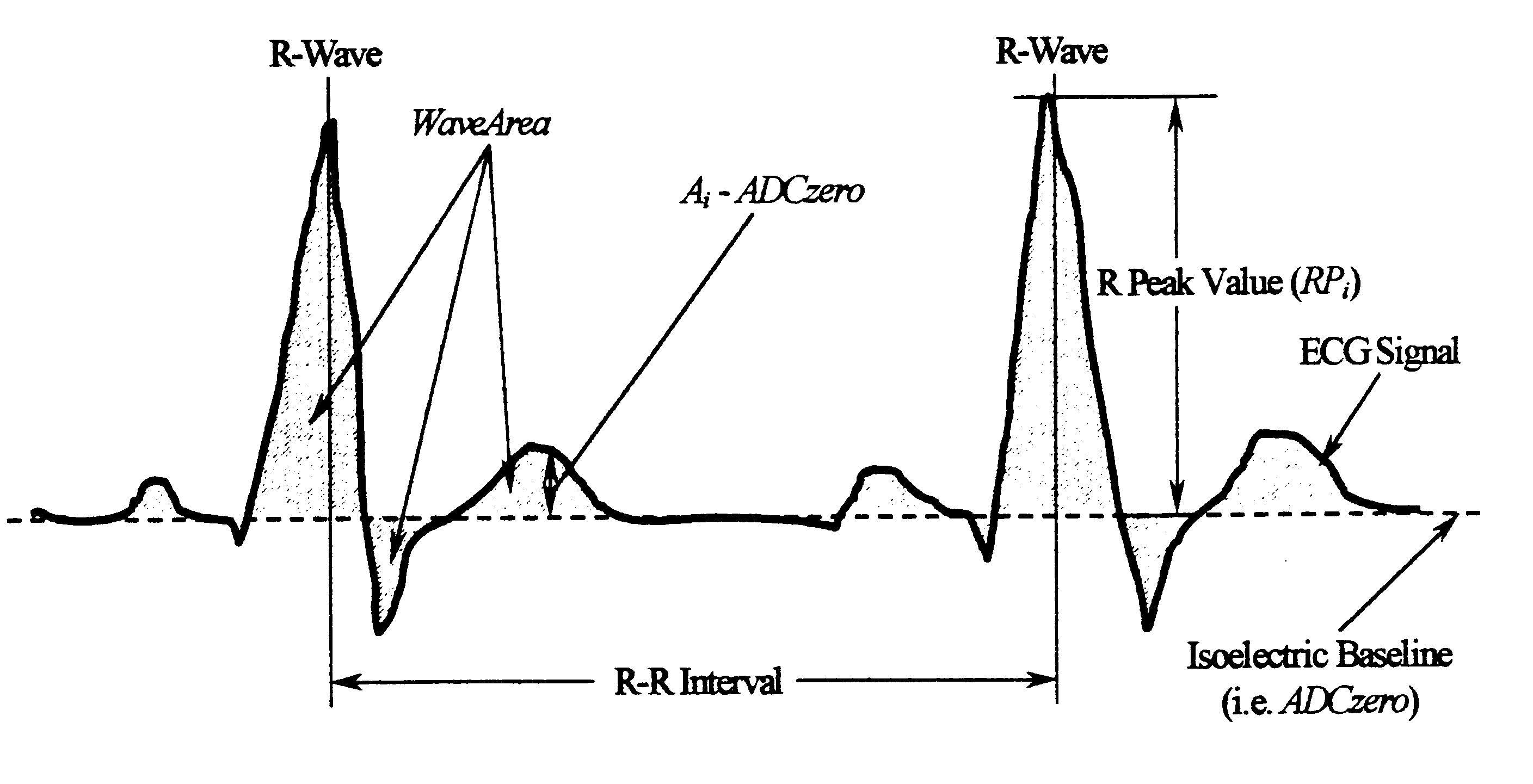
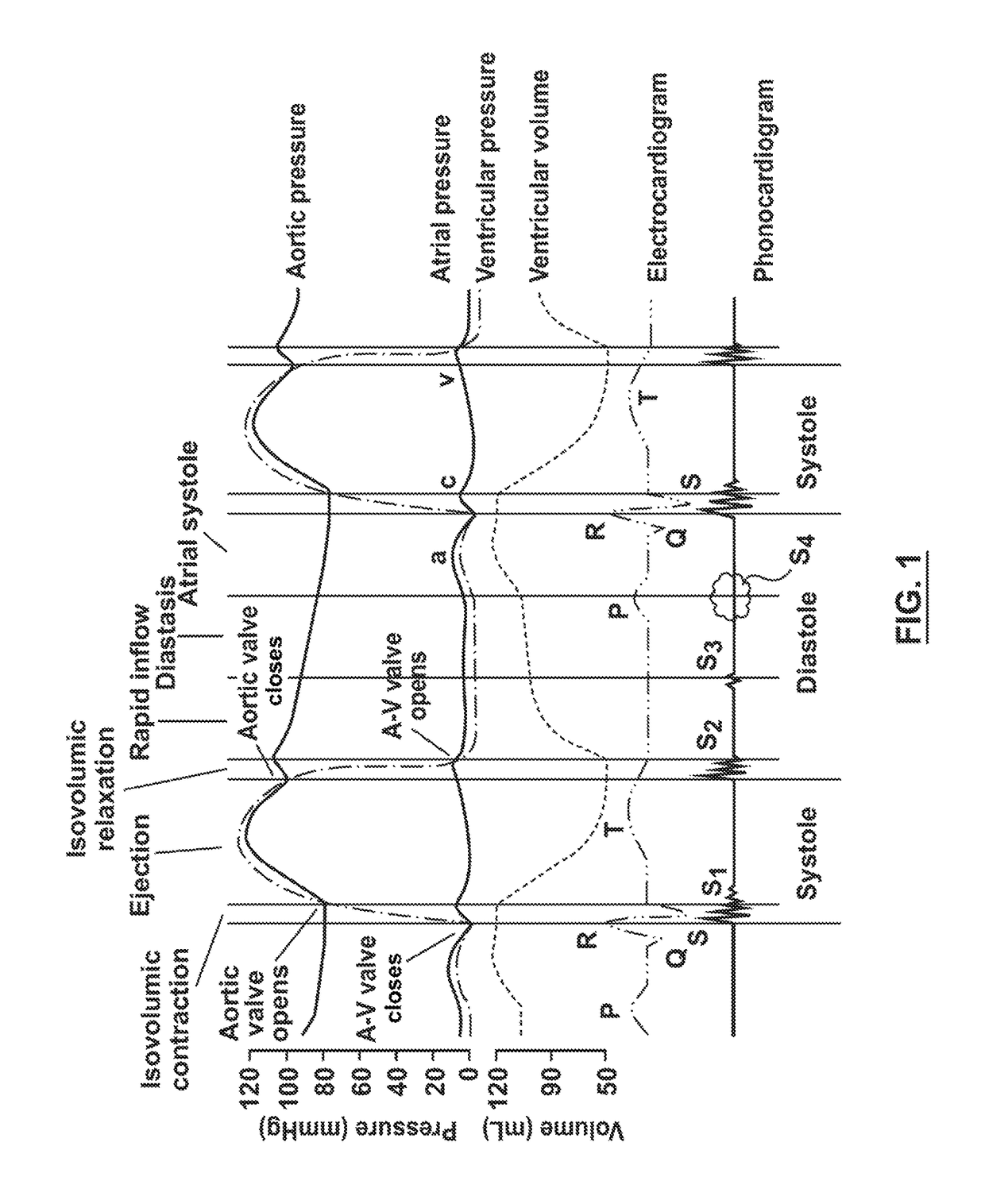
A cardiac monitor is provided that monitors the condition of the heart of a cardiac patient and generates signals indicating one of several conditions, such as supraventricular tachycardia, ventricular tachycardia and ventricular fibrillation. In order to generate these signals, the ECG from the patient is analyzed to determine a cardiac interval and heart rate, as well as a waveform factor and a waveform factor irregularity. The waveform factor is derived from the average of the ECG amplitudes during a cardiac interval and the peak value of the ECG during the same interval. Preferably, a running average is calculated over several intervals. This waveform factor is then used to detect shockable ventricular arrhythmia. The waveform factor irregularity is indicative of the variability of the waveform factor and is used to differentiate between ventricular tachycardia and ventricular defibrillation.
Owner:ZOLL MEDICAL CORPORATION
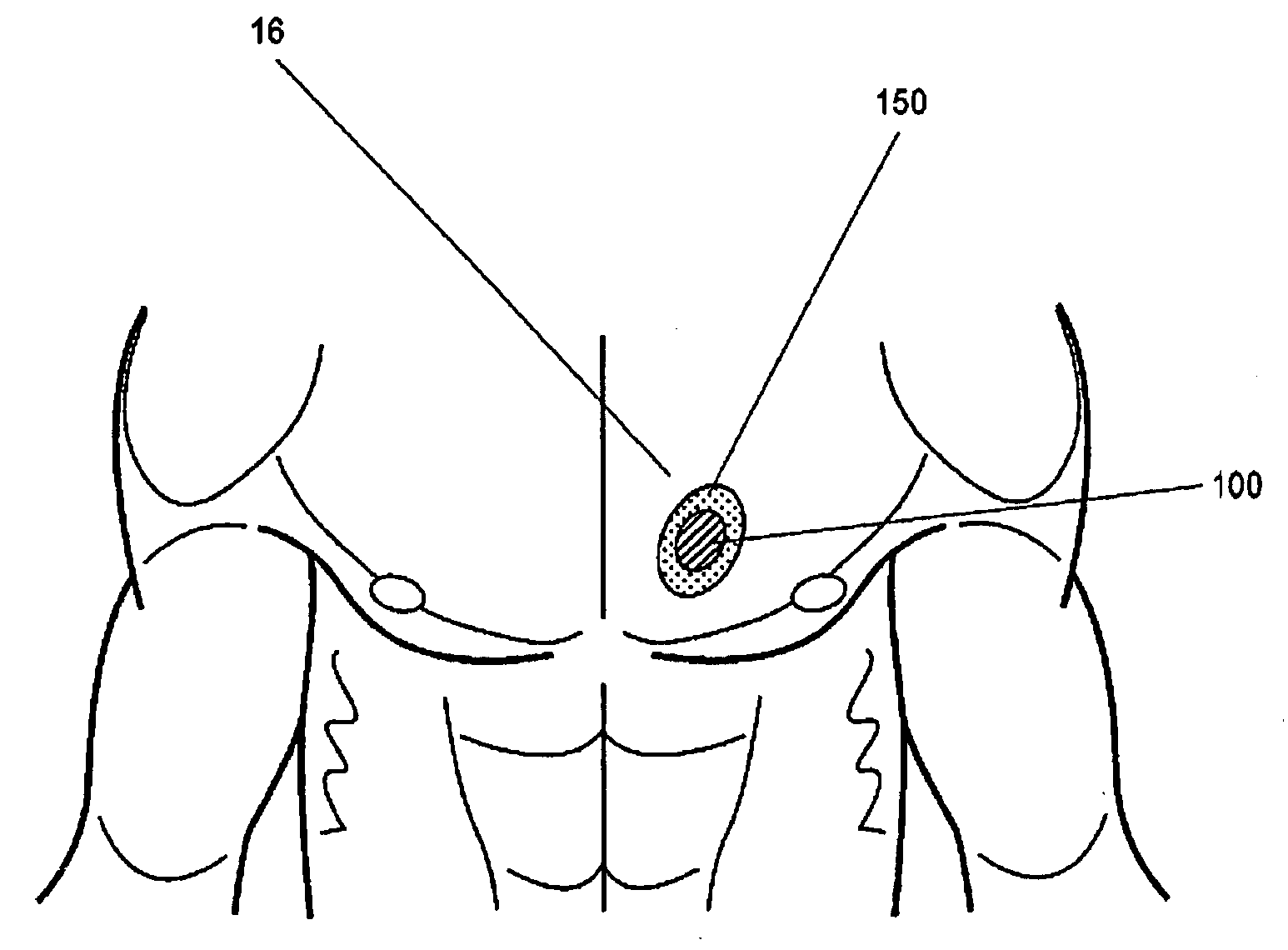
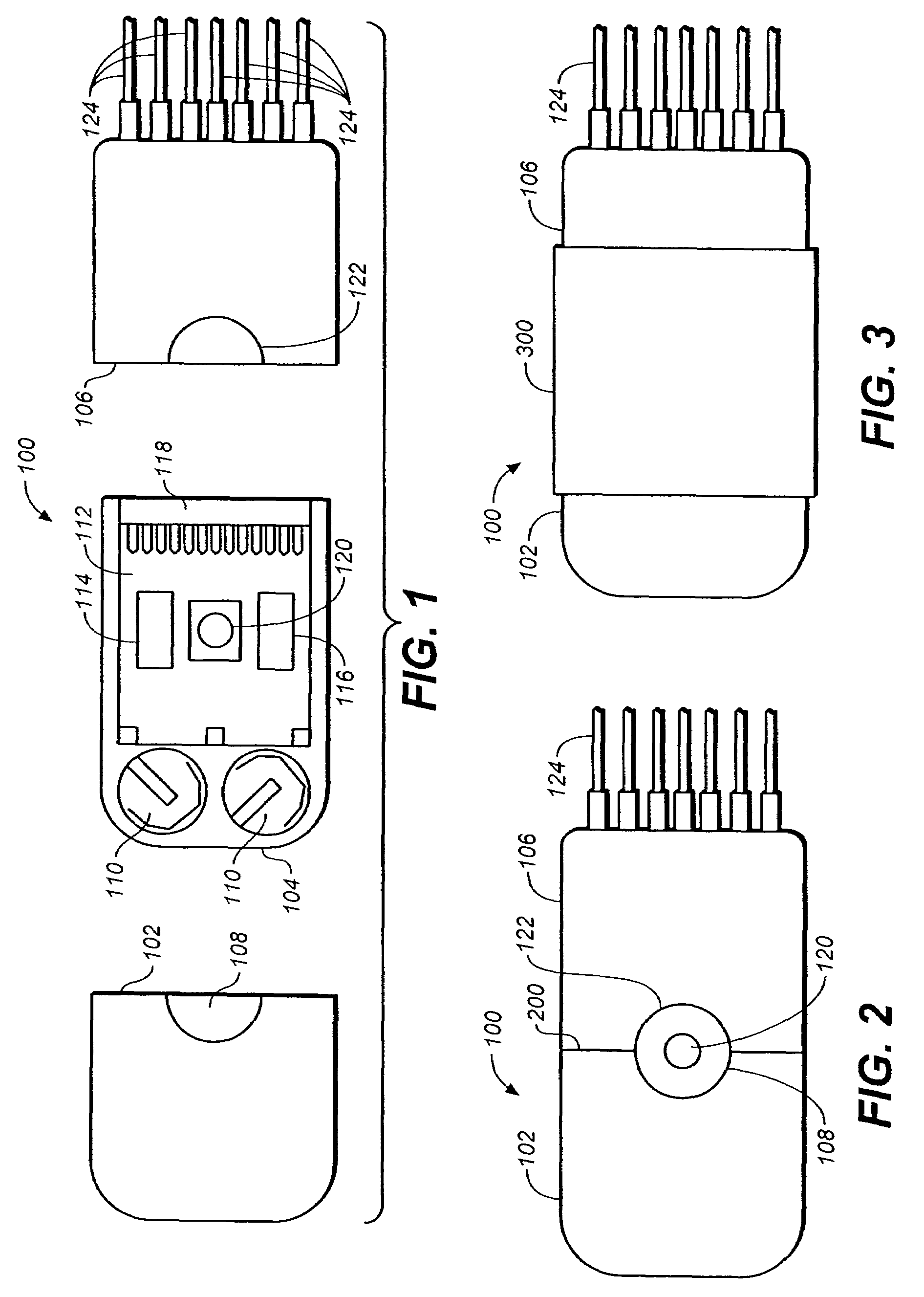
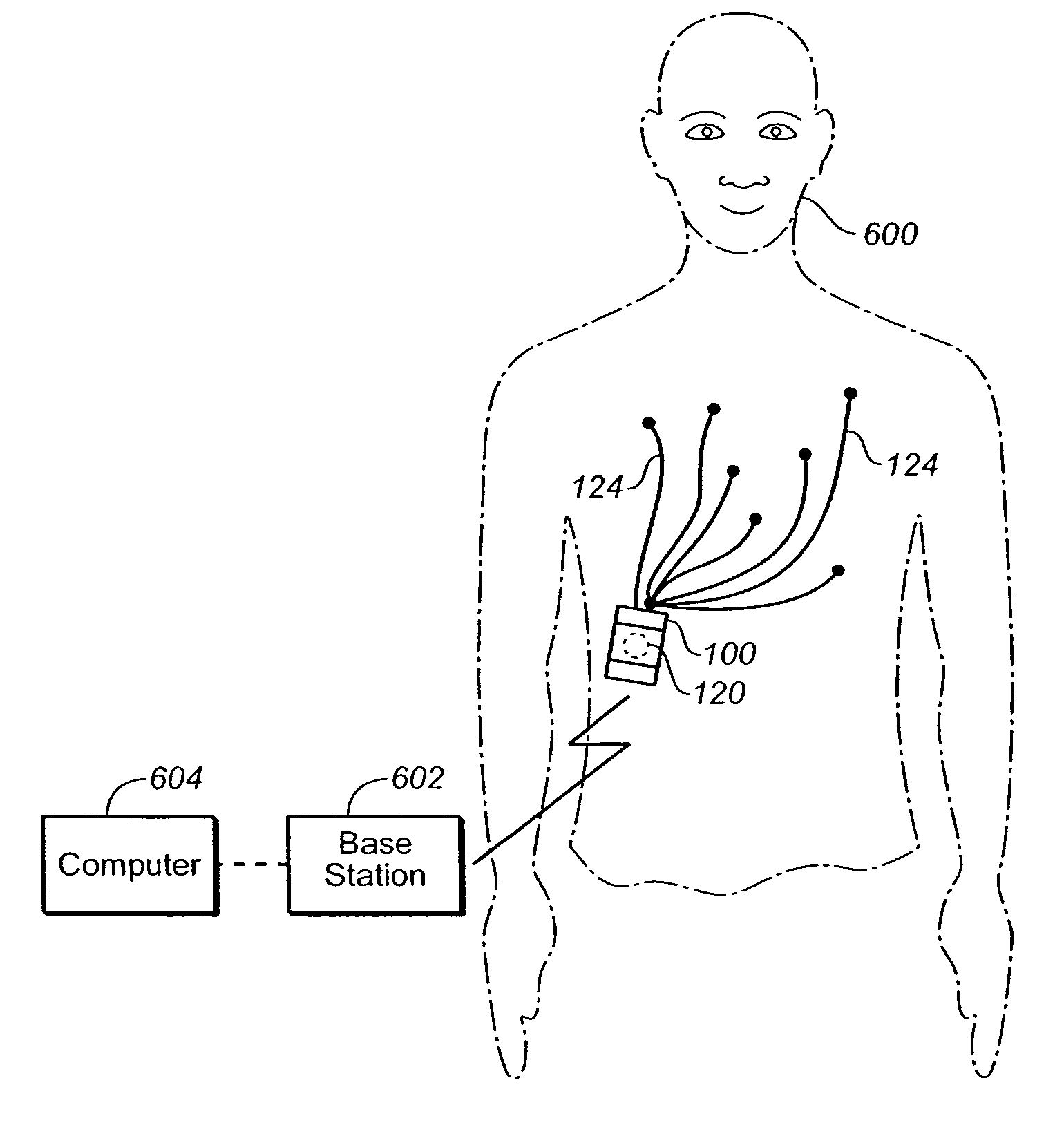
Non-invasive cardiac monitor and methods of using continuously recorded cardiac data
ActiveUS20070255153A1Improve fidelityElectrocardiographyLocal control/monitoringAdhesiveCardiac monitoring
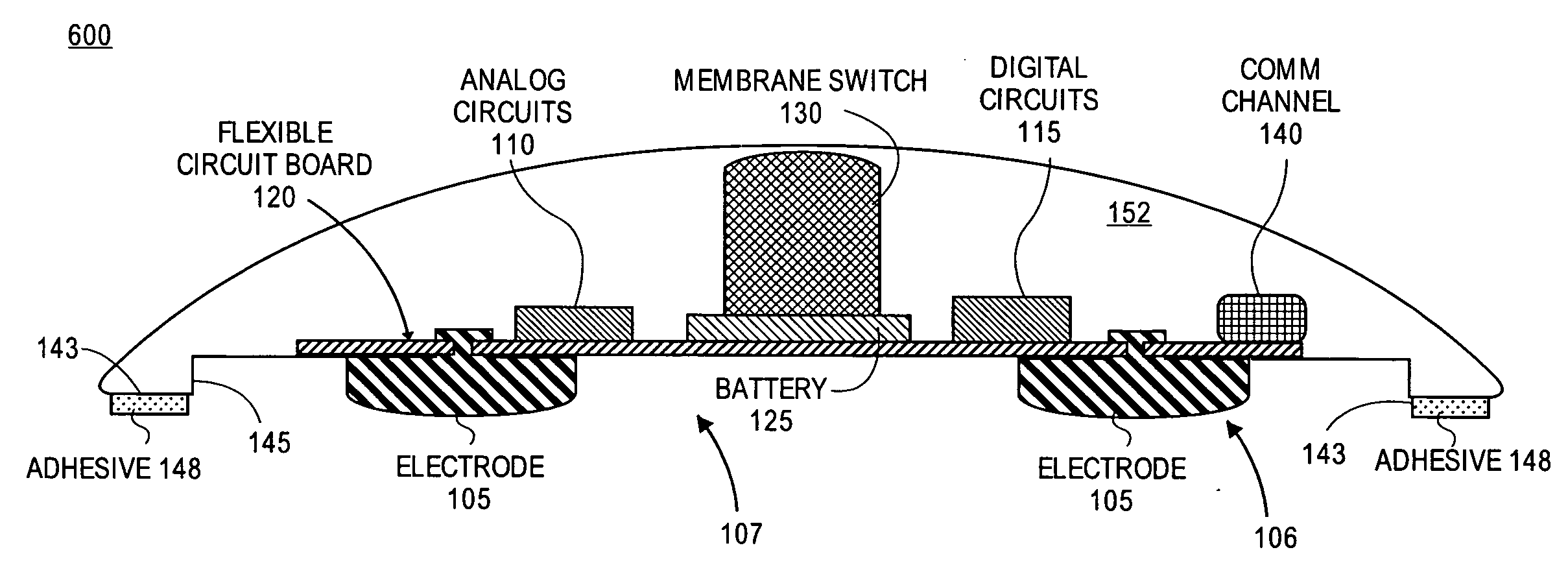
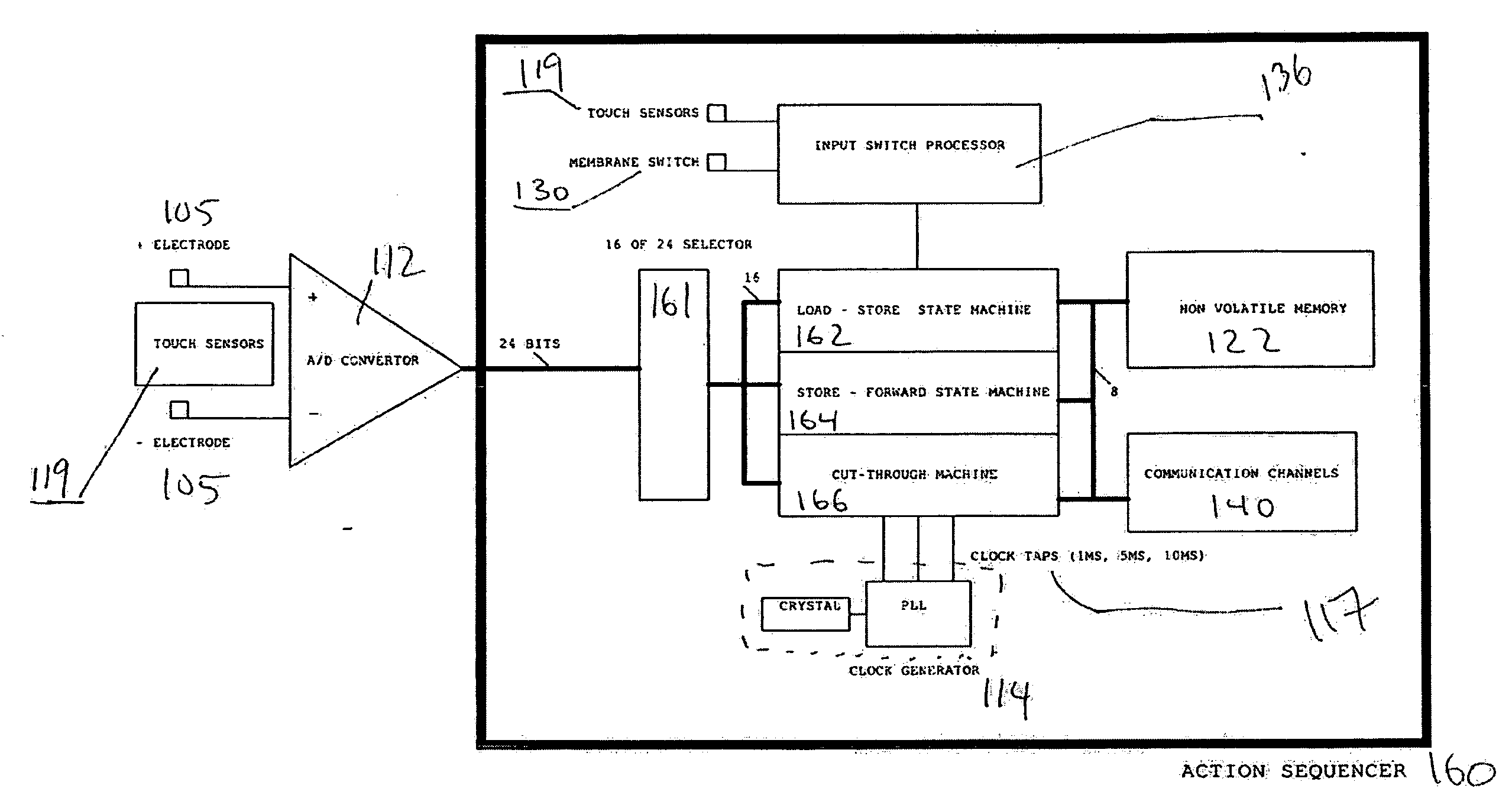
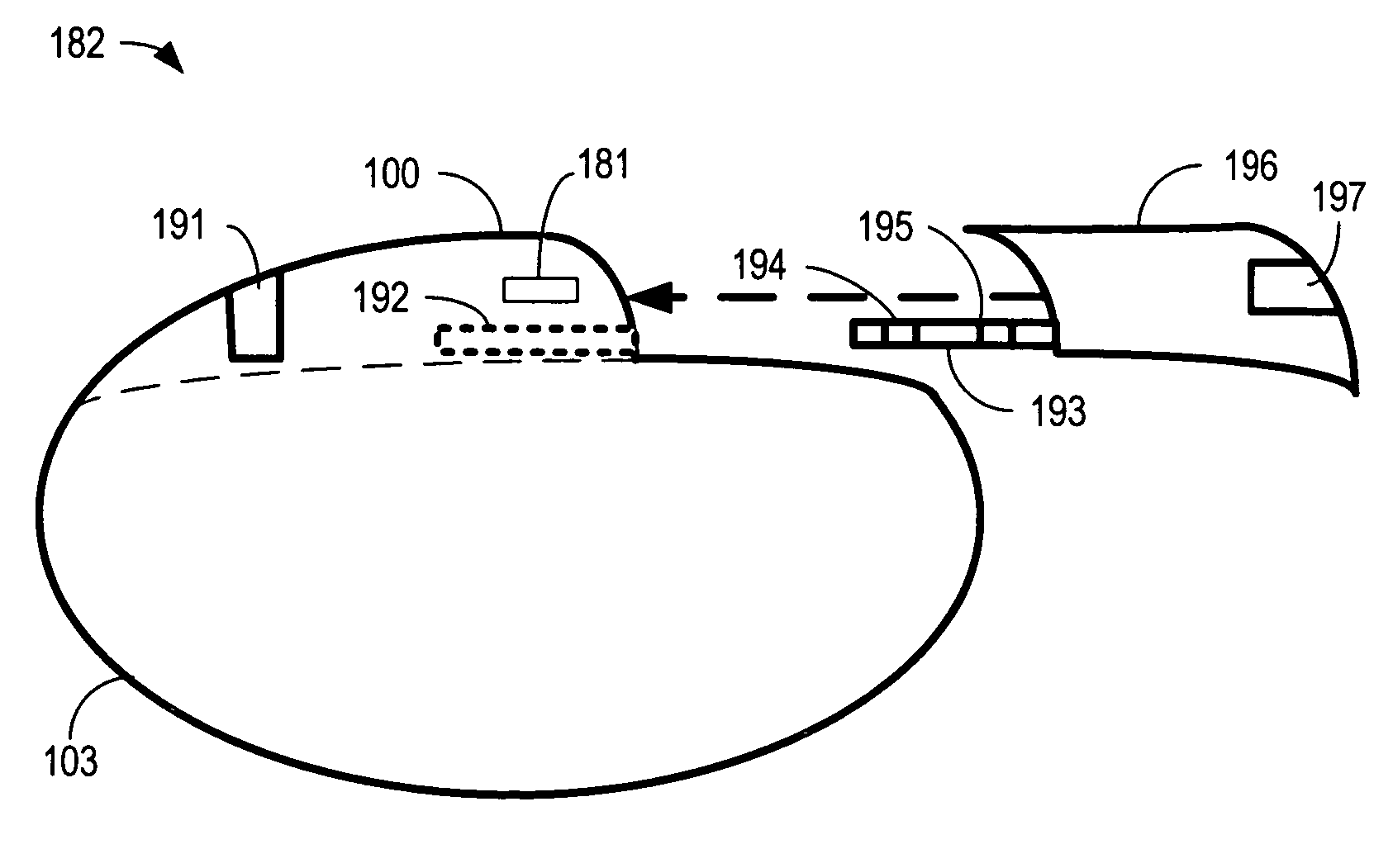
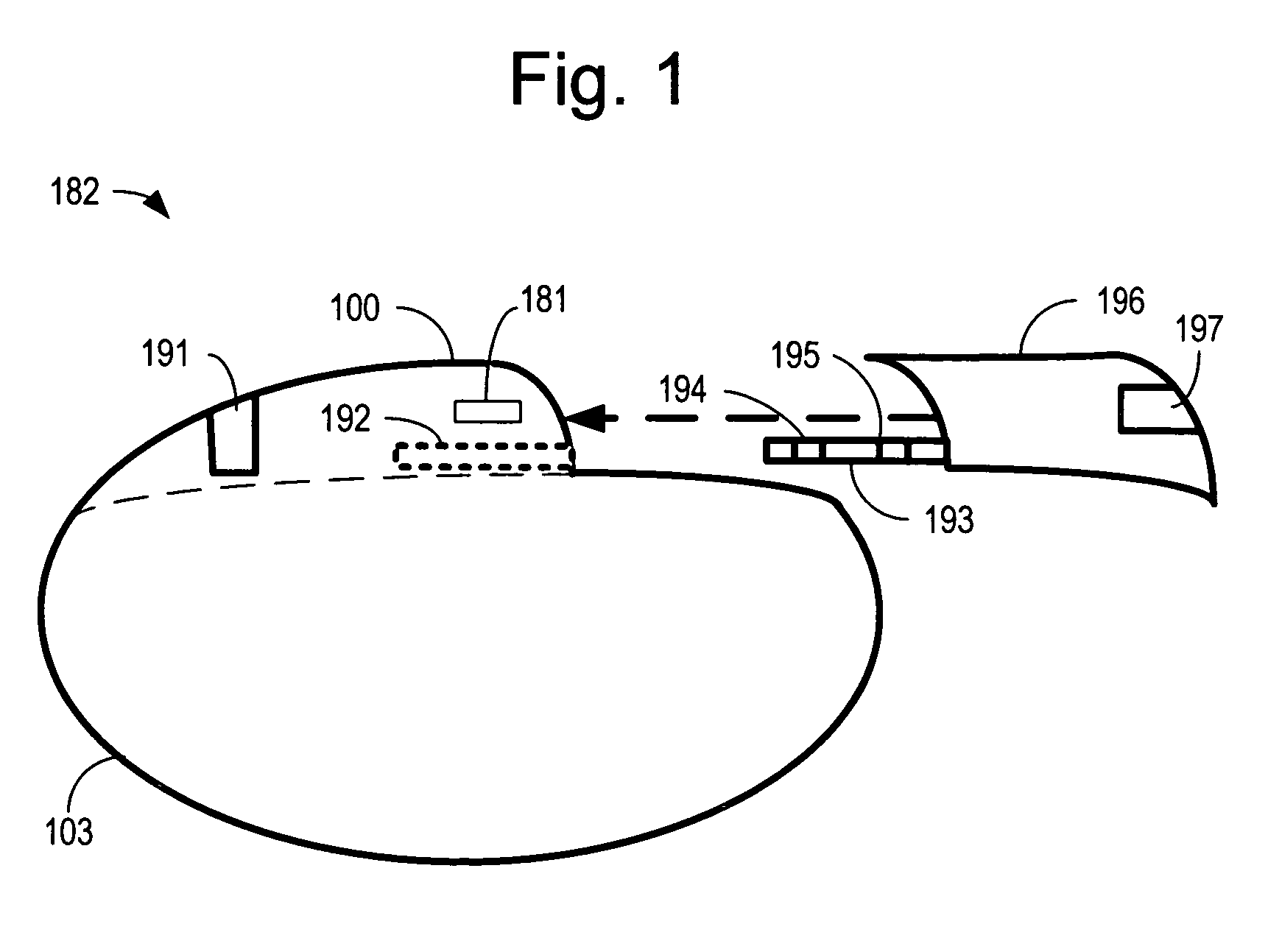
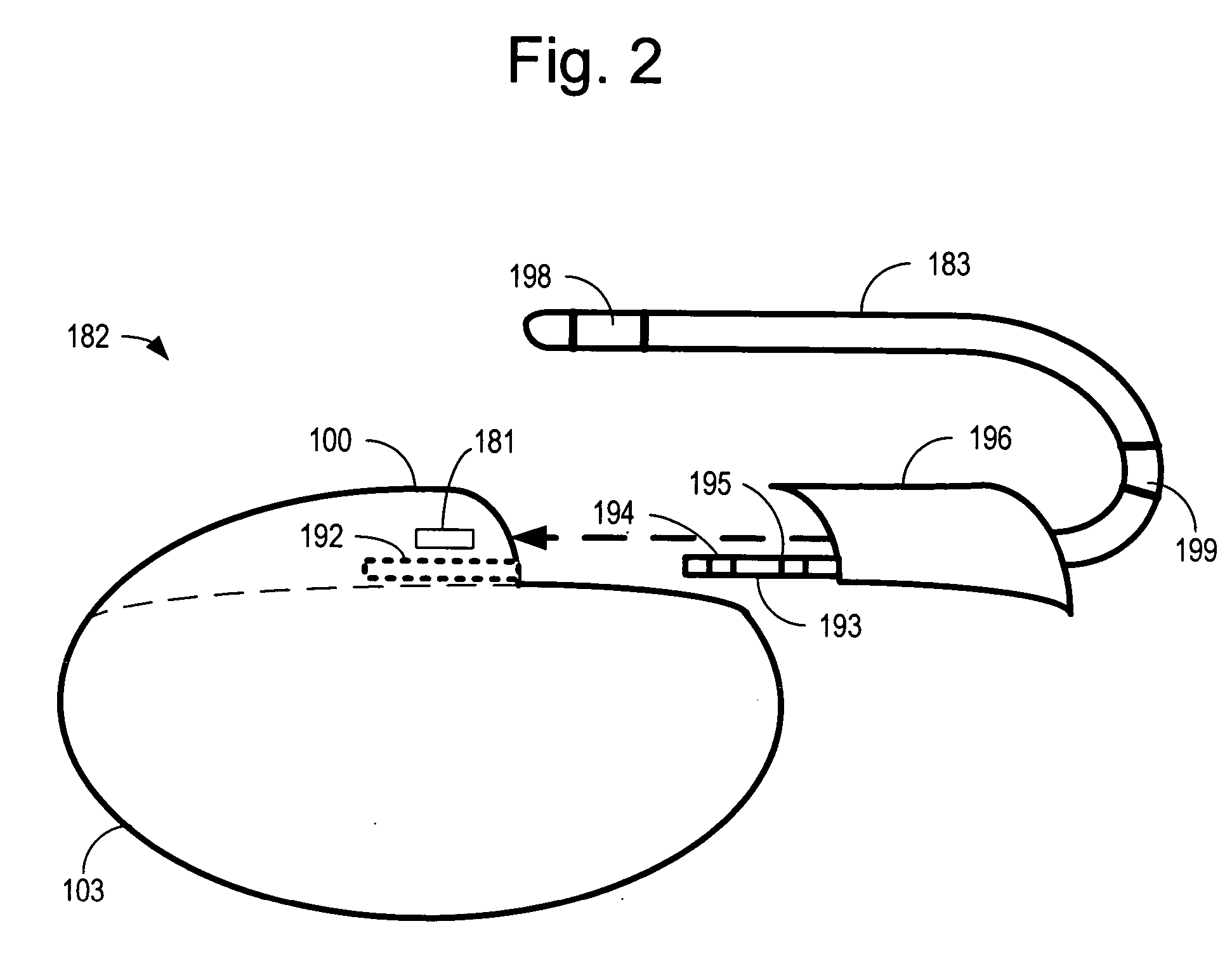
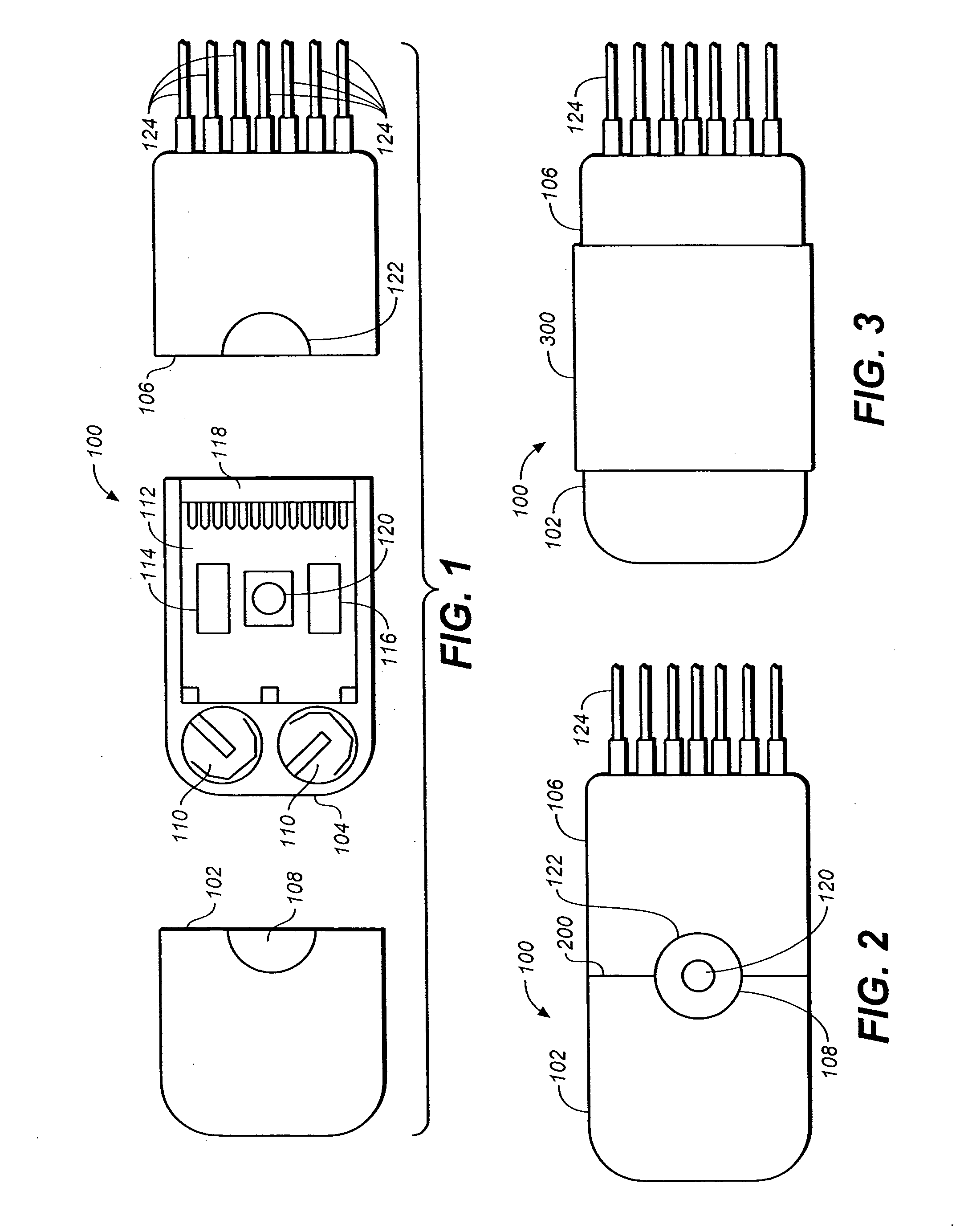
One embodiment of the invention is a cardiac monitor having a housing; a plurality of electrodes within and extending from the housing; a state machine within the housing configured to digitialize and store in memory signals from the plurality of electrodes; a sealing surface and an adhesive on the sealing surface configured to form a watertight perimeter around the plurality of electrodes when the housing is affixed to a mammal. Another embodiment of the invention provides a continuous cardiac monitor having a housing; a surface on the housing adapted to be sealably engaged to a mammal; an adhesive on the surface that is adapted to remain affixed to the mammal for at least 7 days; at least two electrodes within the housing positioned to detect a cardiac information of the mammal while the surface is sealably engaged to the mammal; an electronic memory within the housing wherein, the electronic memory is sized to store at least 24 hours of continuous cardiac information; and wiring within the housing connecting the electronic memory to the electrodes.
Owner:THE BOARD OF TRUSTEES OF THE LELAND STANFORD JUNIOR UNIV
Non-invasive cardiac monitor and methods of using continuously recorded cardiac data
ActiveUS20070225611A1Improve fidelityElectrocardiographyLocal control/monitoringCardiac monitoringNon invasive
Embodiments of the present invention provide a method of analyzing cardiac information by collecting a plurality of self-contained, wearable, portable cardiac monitors each of the cardiac monitors electronically storing at least 24 hours of continuously detected and unanalyzed cardiac signals from a mammal. Next, retrieving cardiac information stored in each of the plurality of self-contained portable cardiac monitors. Next, forwarding retrieved cardiac information.
Owner:THE BOARD OF TRUSTEES OF THE LELAND STANFORD JUNIOR UNIV
Reconfigurable implantable cardiac monitoring and therapy delivery device
Methods and systems for implantable cardiac monitors reconfigurable to cardiac therapy devices. A device includes a housing with electrodes configured for cardiac activity sensing when the device is operated in monitoring mode, and sensing and energy delivery when operated in an energy delivery mode. A header may be configured to receive a cardiac lead, and may be associated with a switch to switch the device between monitoring and therapy modes in response to connecting one or more leads to the header. The device may include a transceiver that transmits the contents of the memory to a patient-external device. A method involves providing an implantable cardiac device configured to operate in a first mode as a loop recorder for monitoring cardiac activity and storing selected cardiac events, and operating in the second mode to monitor cardiac activity and provide cardiac stimulation therapy when the second mode is enabled.
Owner:CARDIAC PACEMAKERS INC
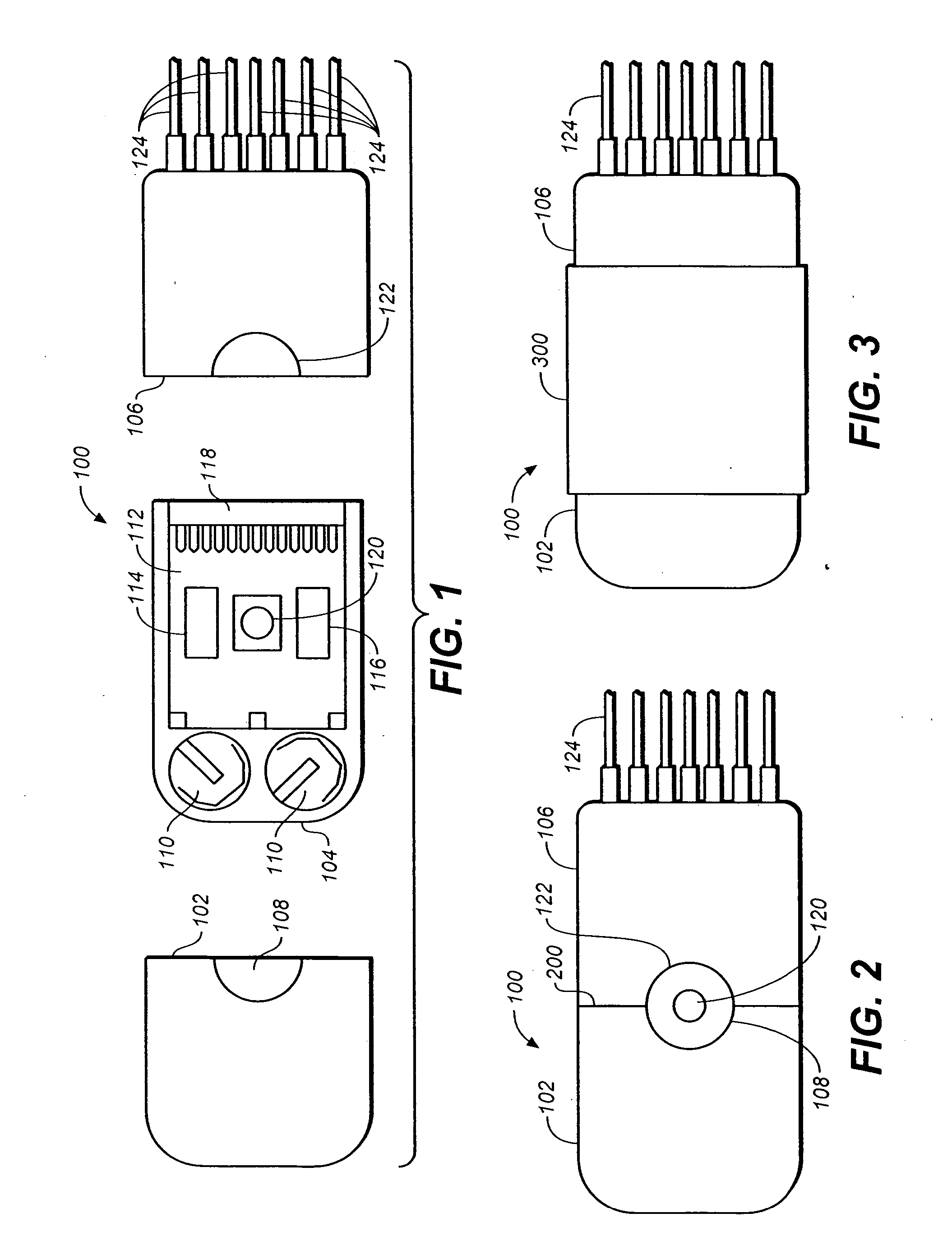
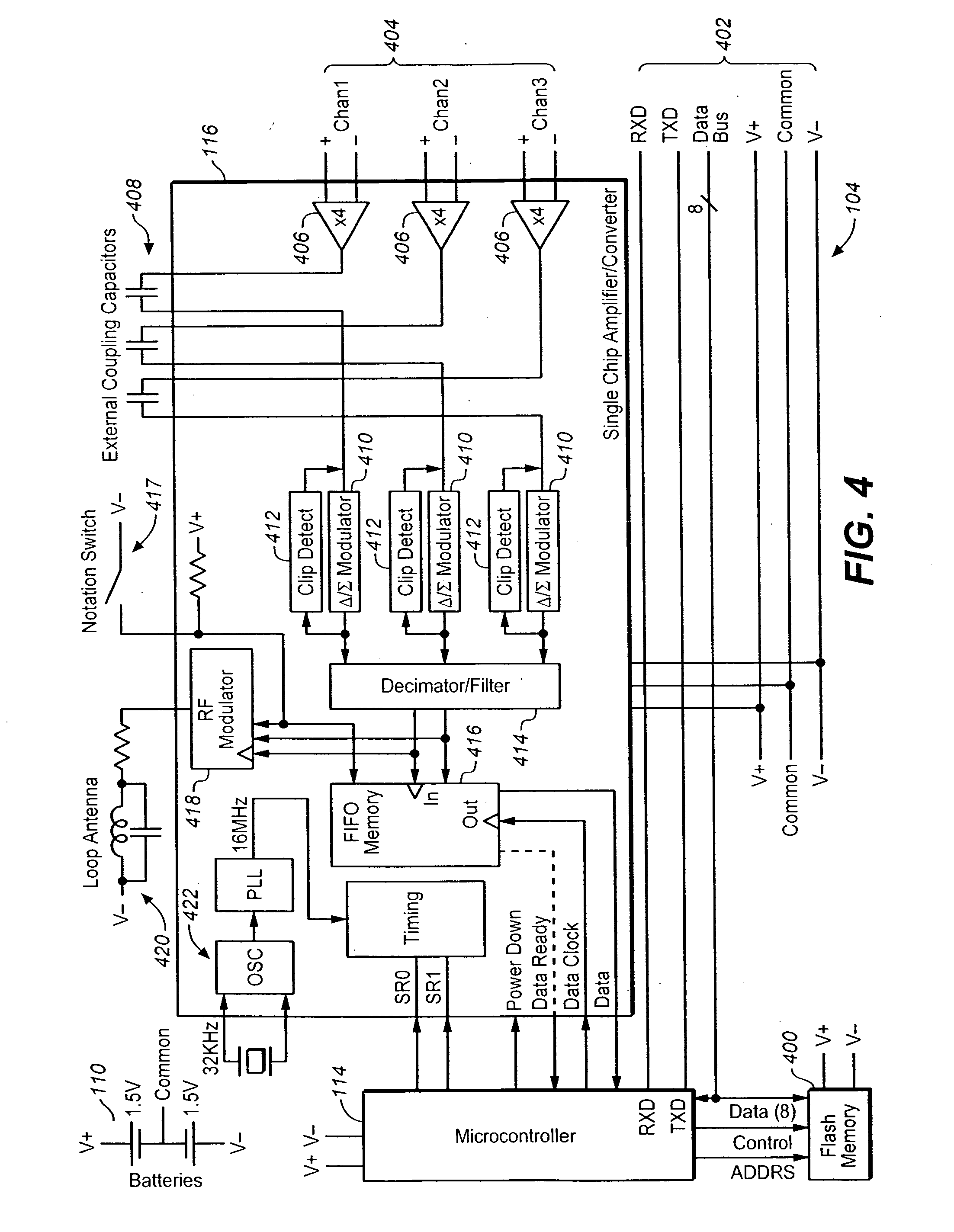
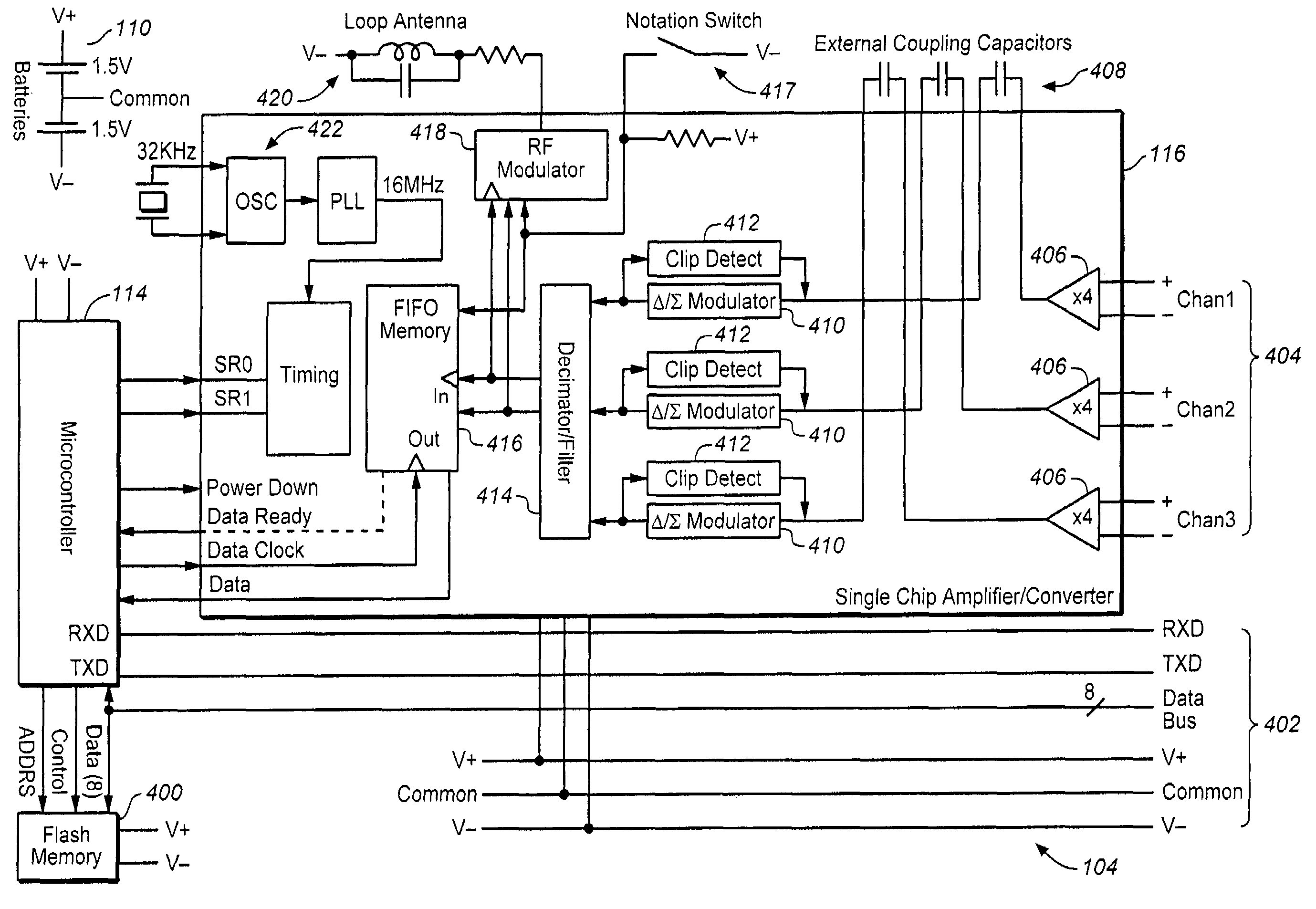
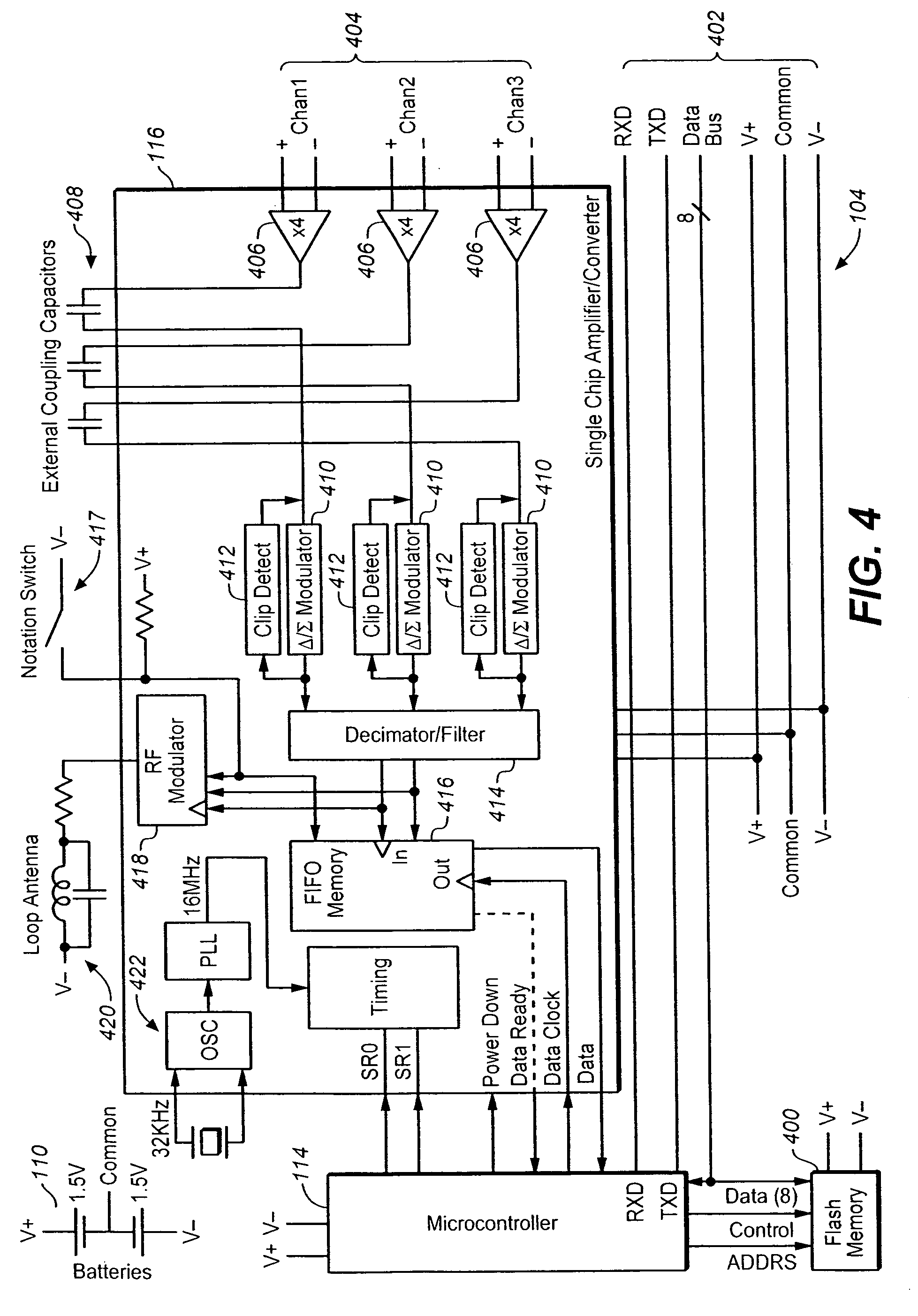
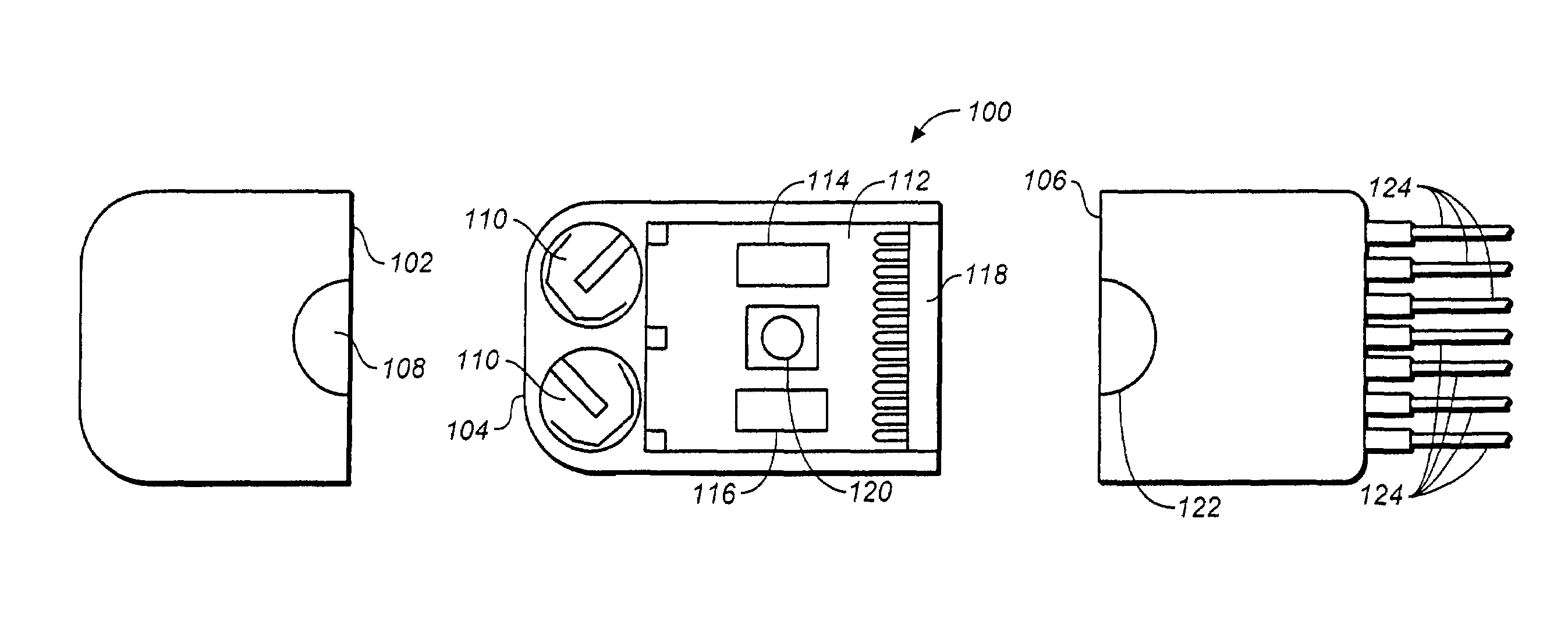
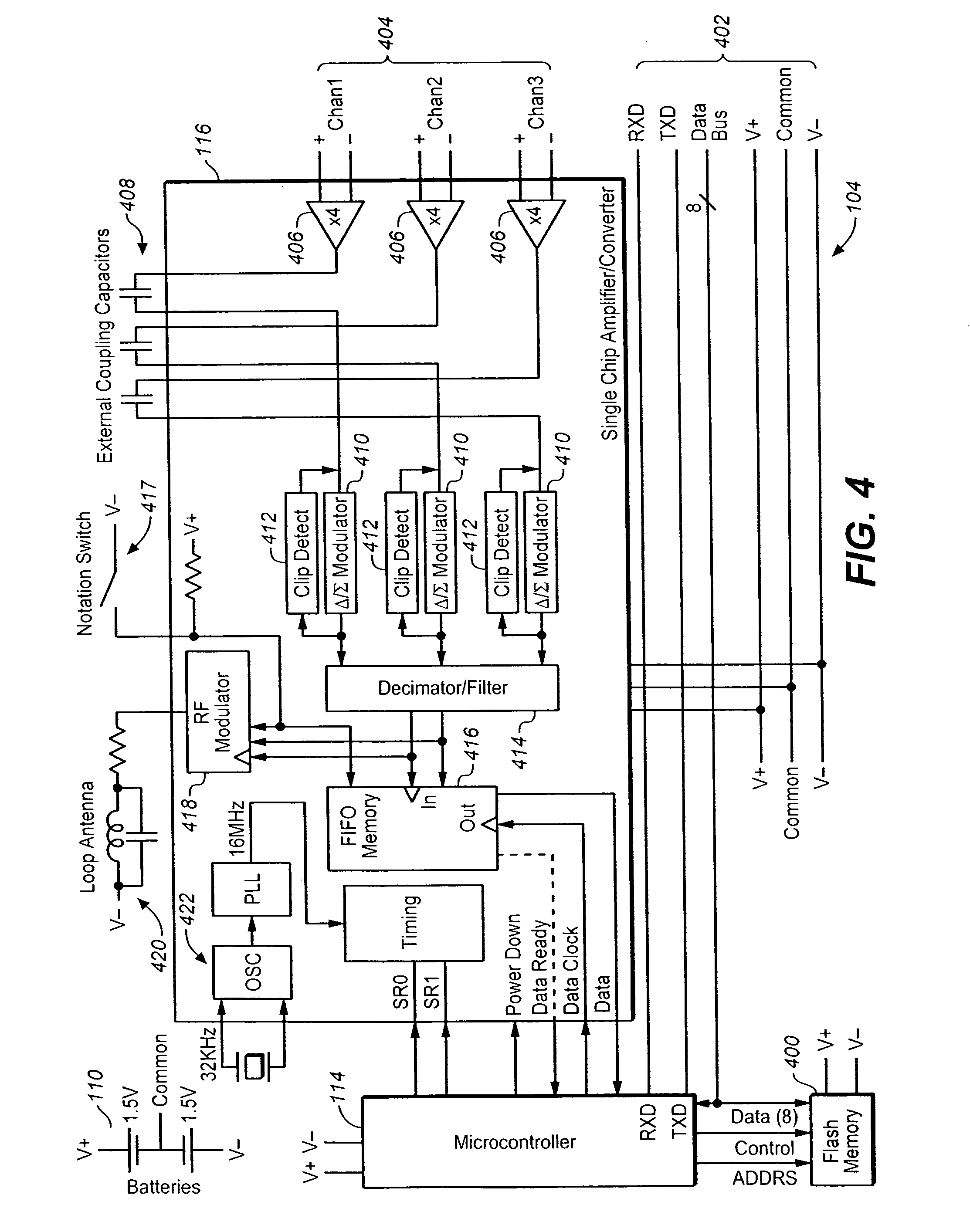
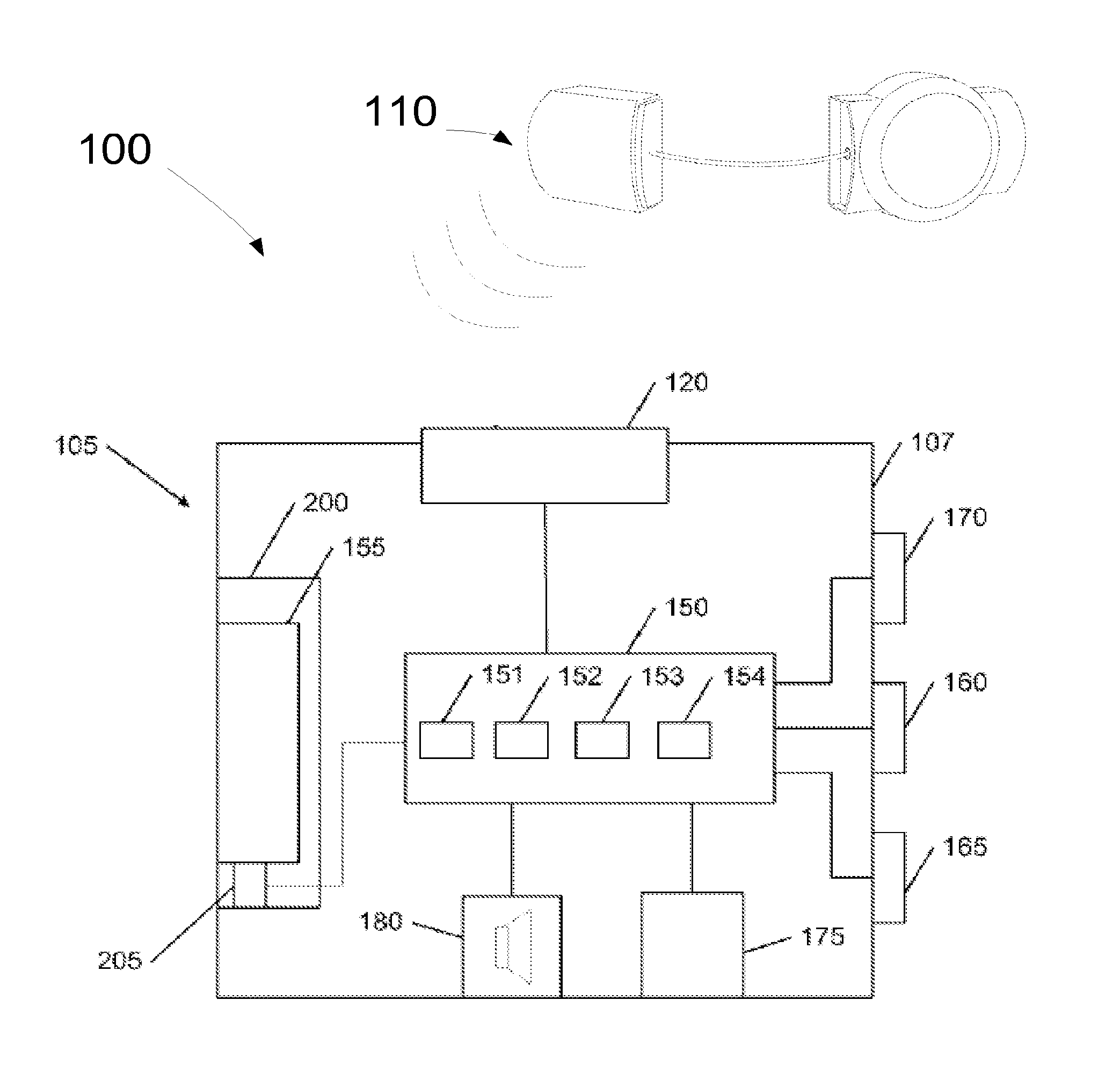
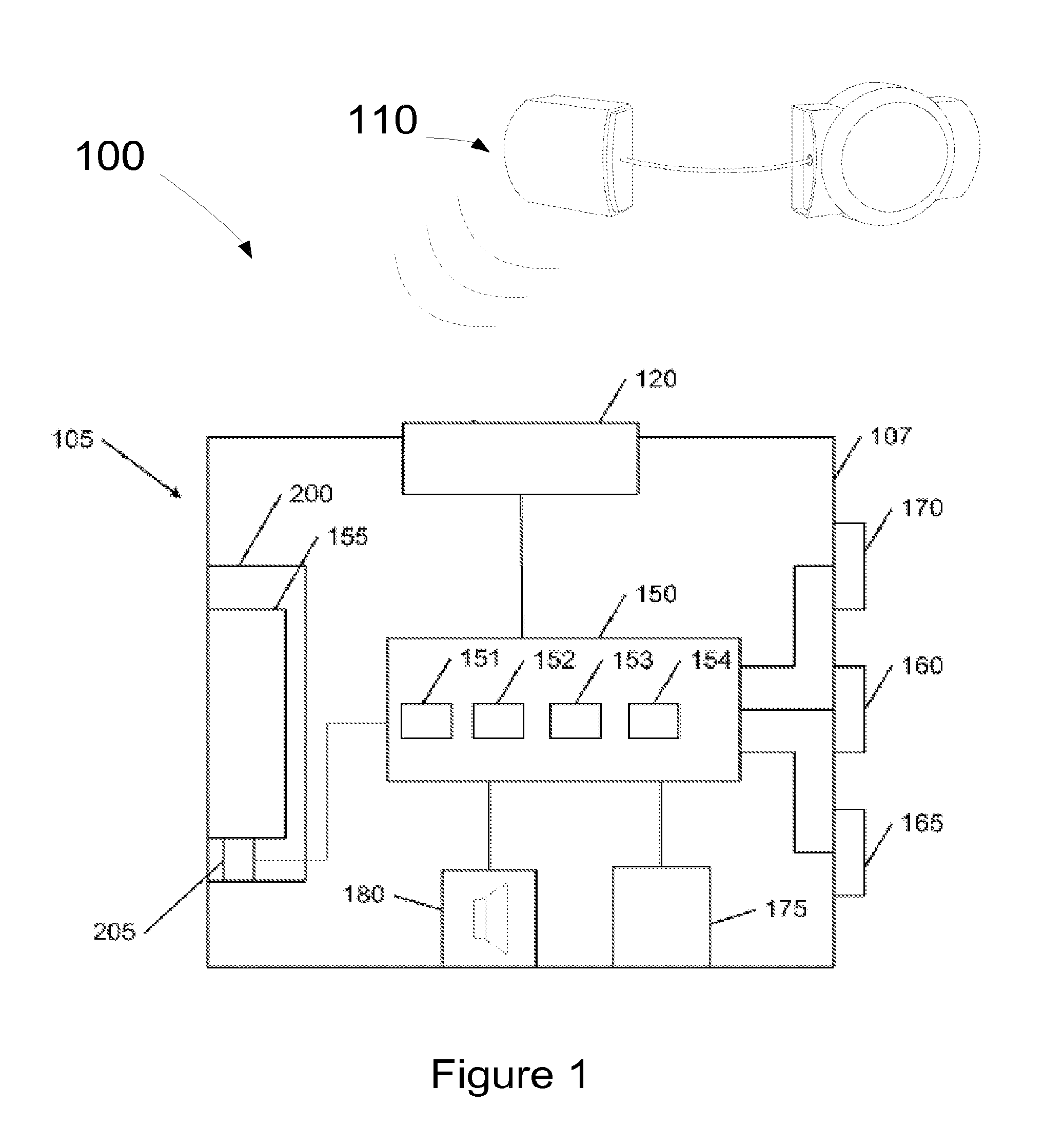
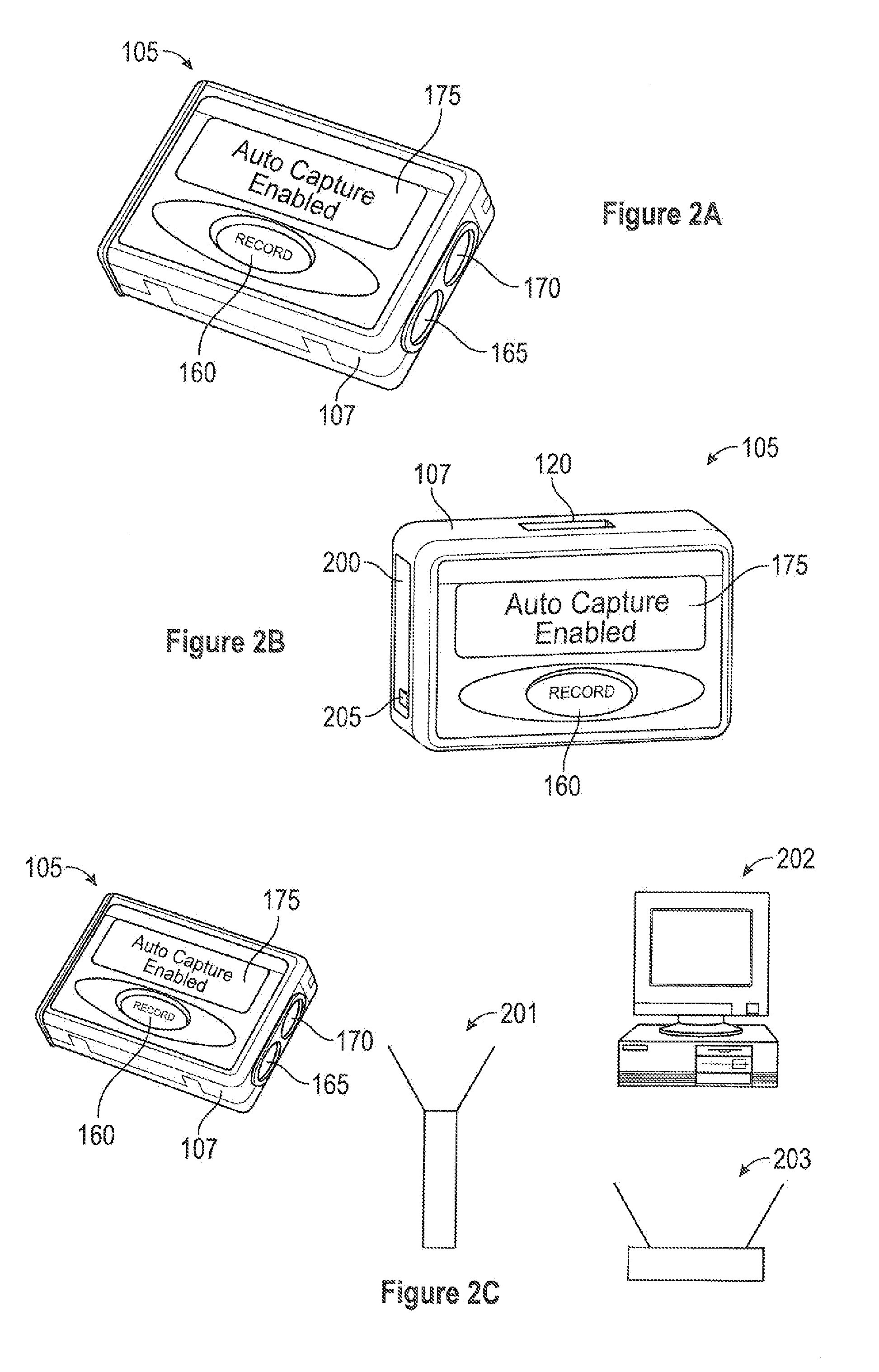
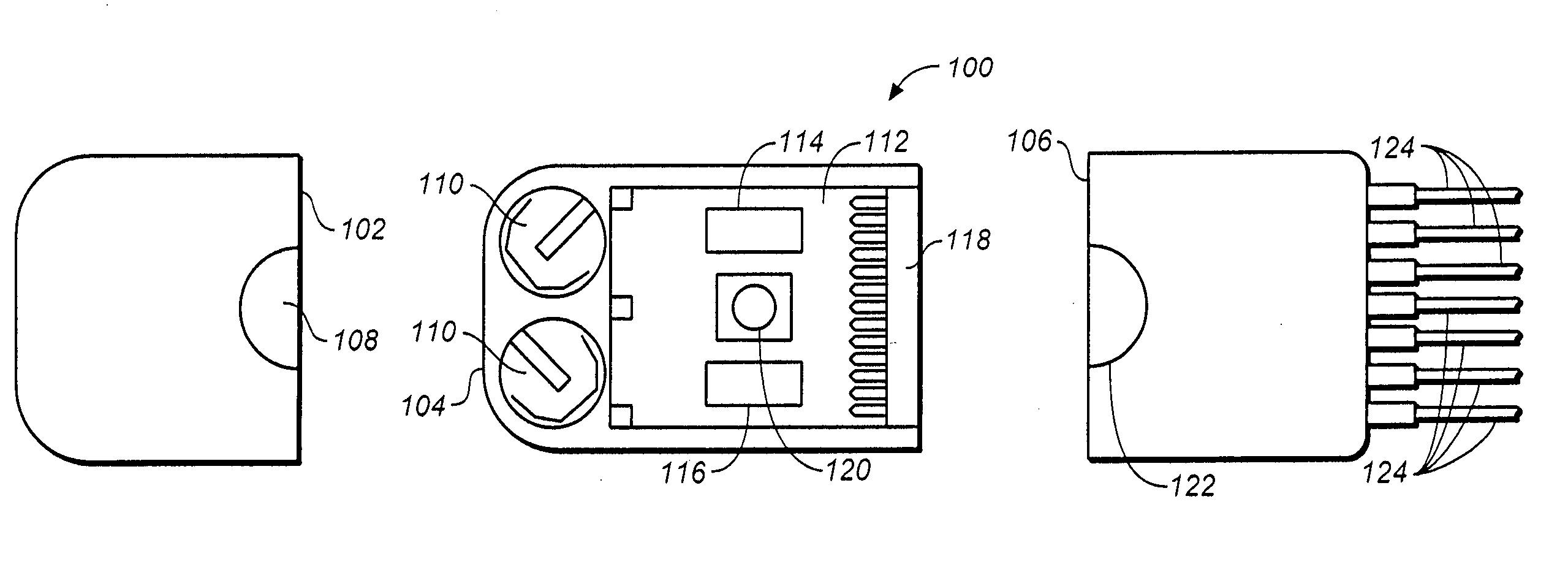
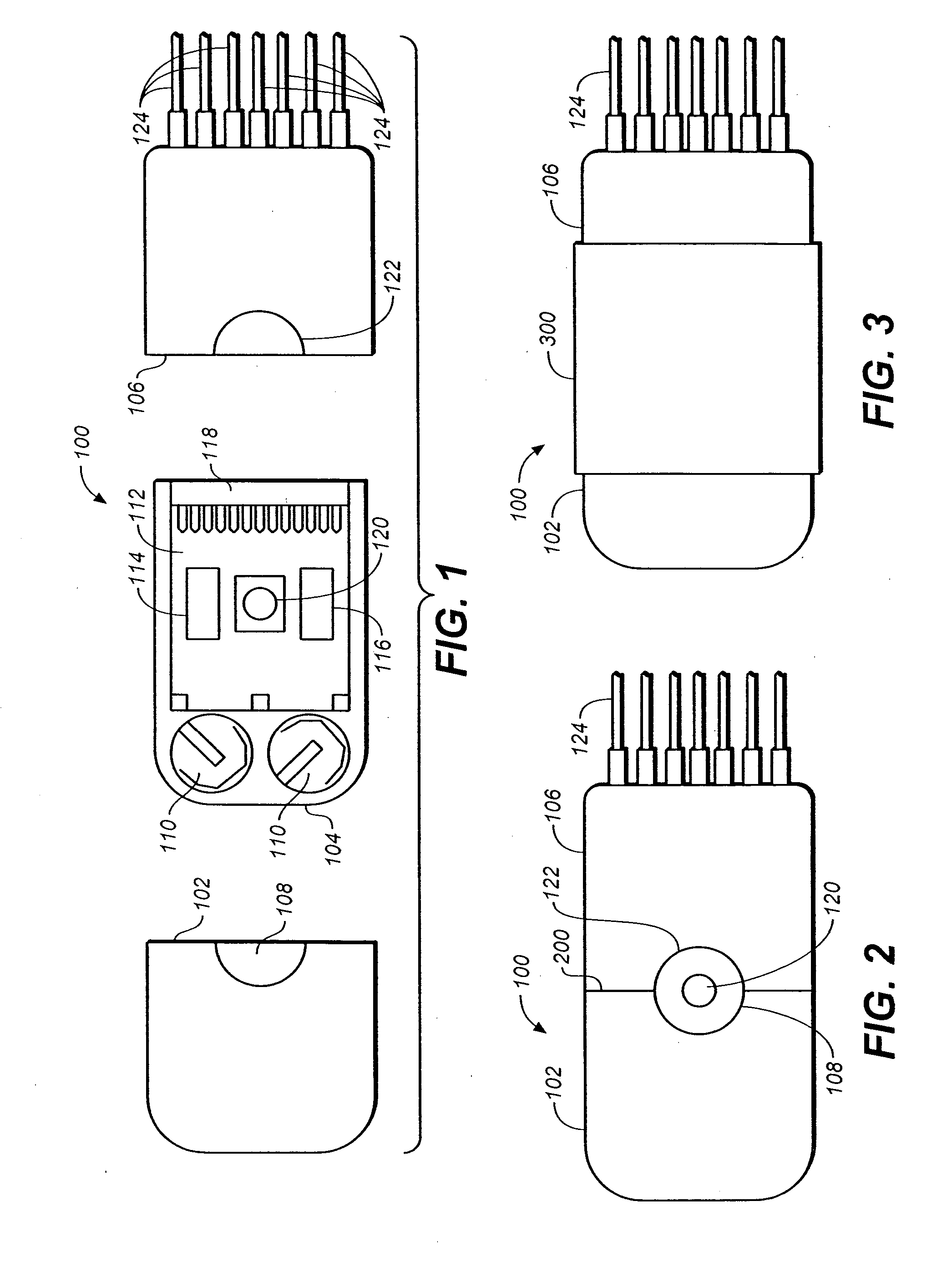
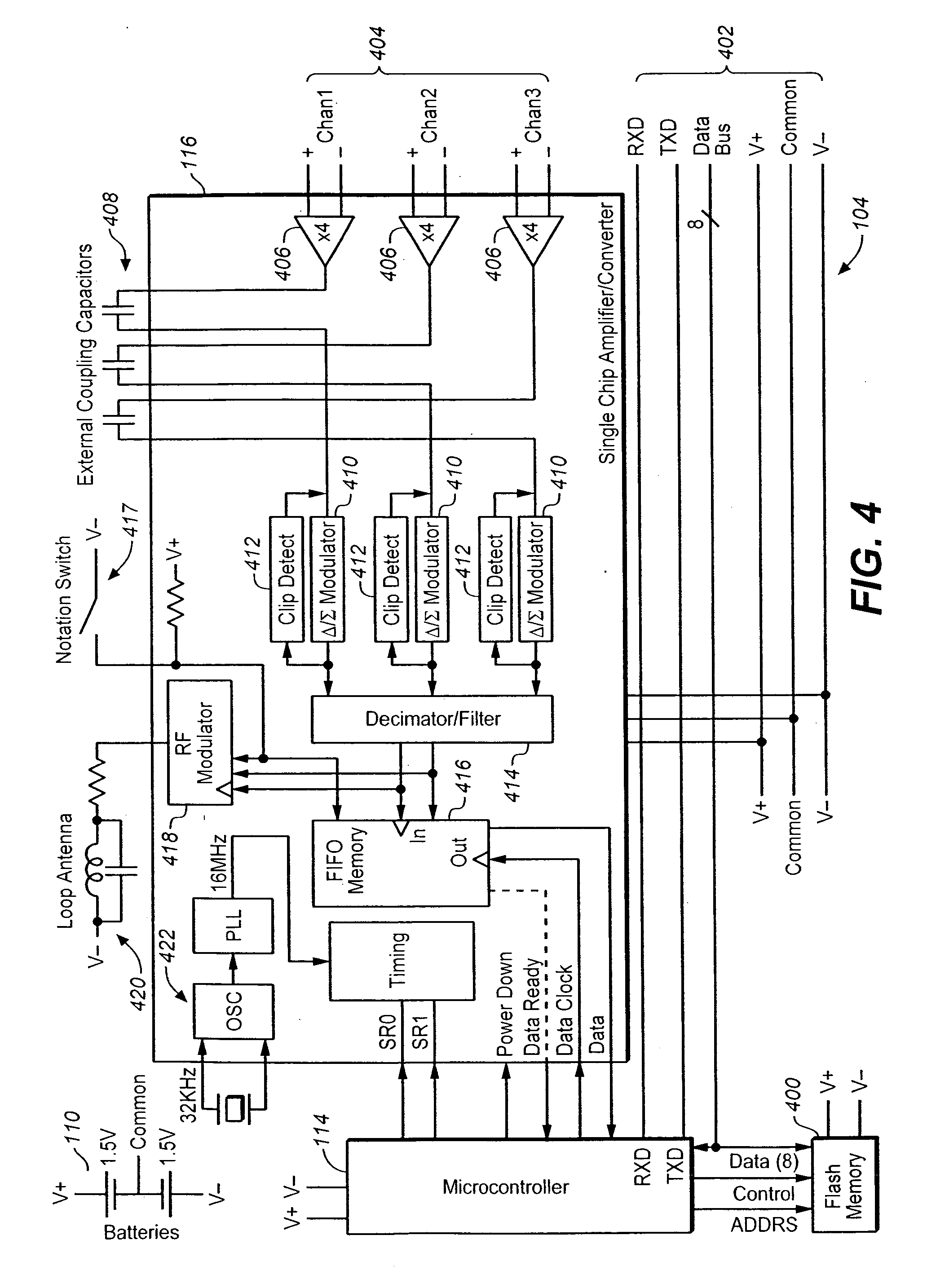
Portable cardiac monitor including RF communication
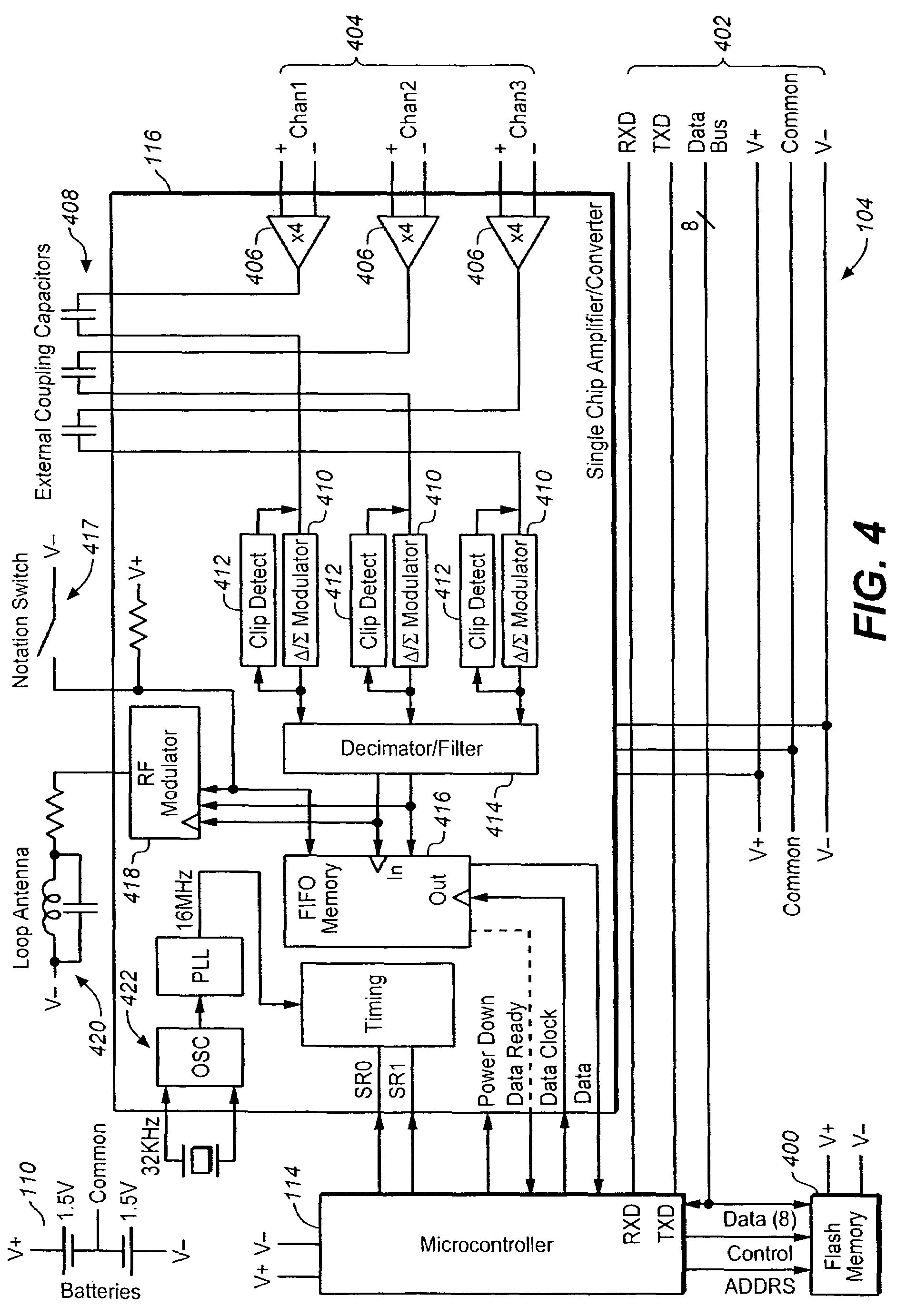
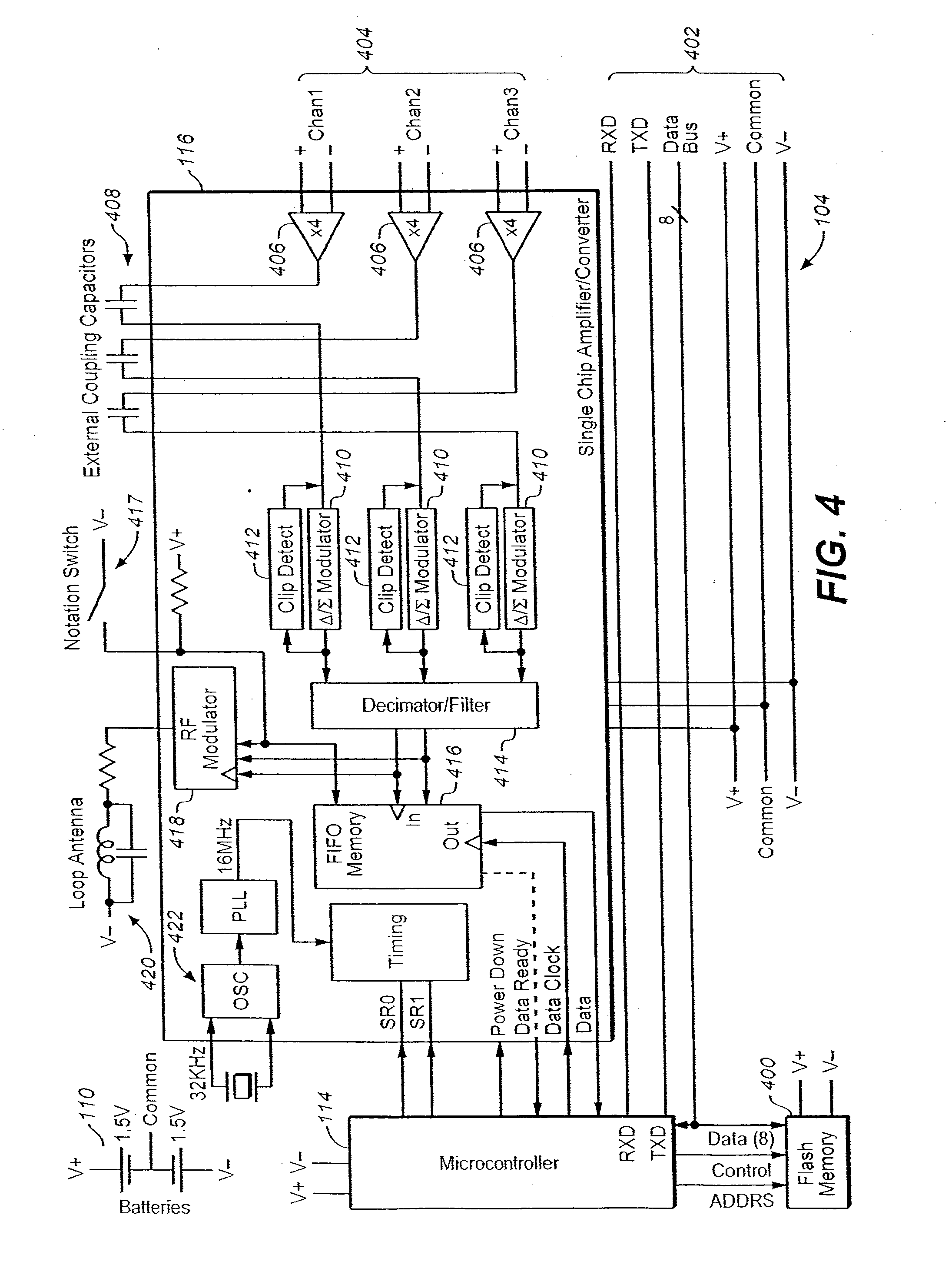
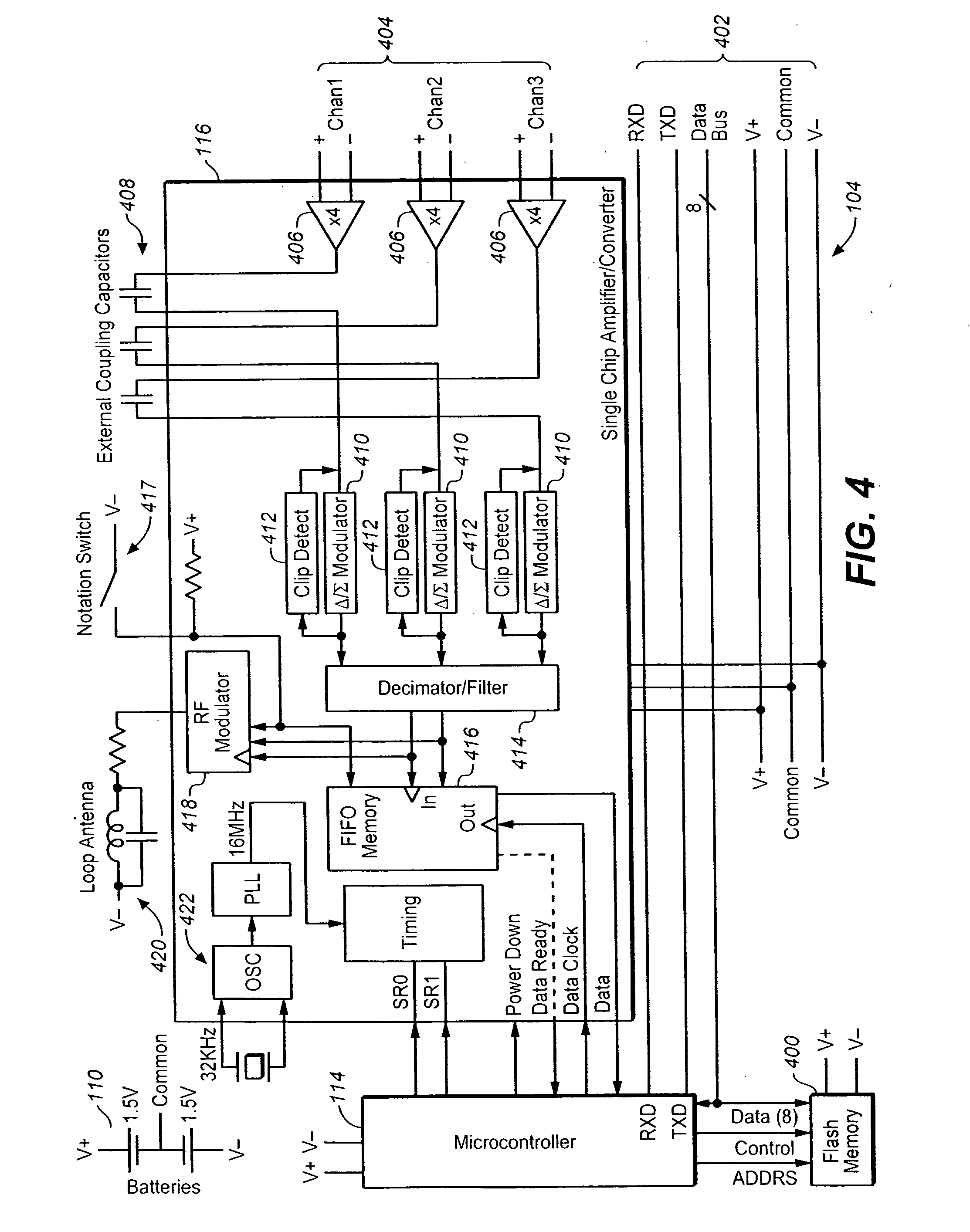
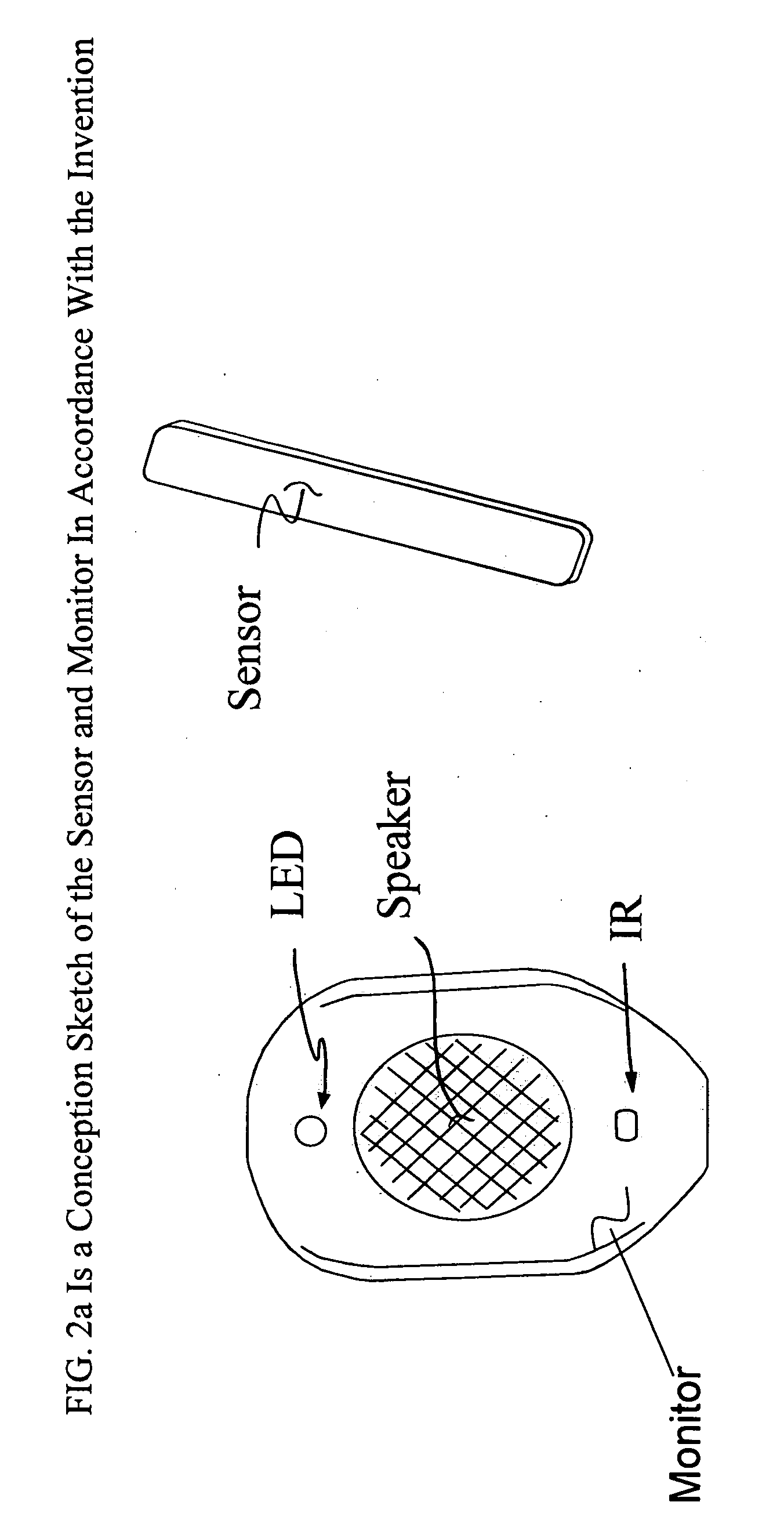
A system and method for obtaining ECG signals from an ambulatory patient are disclosed herein. The system is configured to be inexpensive, small, and robust for outpatient monitoring. The system is configured to be a low power consuming device. The system provides options for a variety of settings and real-time access to the ECG signals being recorded during the recording period.
Owner:EXELYS
Systems and methods for interelectrode distance optimization in a retractable multi-use cardiac monitor
ActiveUS9226679B2Easy and function-enhancing adjustmentElectrocardiographySensorsEcg signalCardiac monitoring
Owner:MEDICOMP
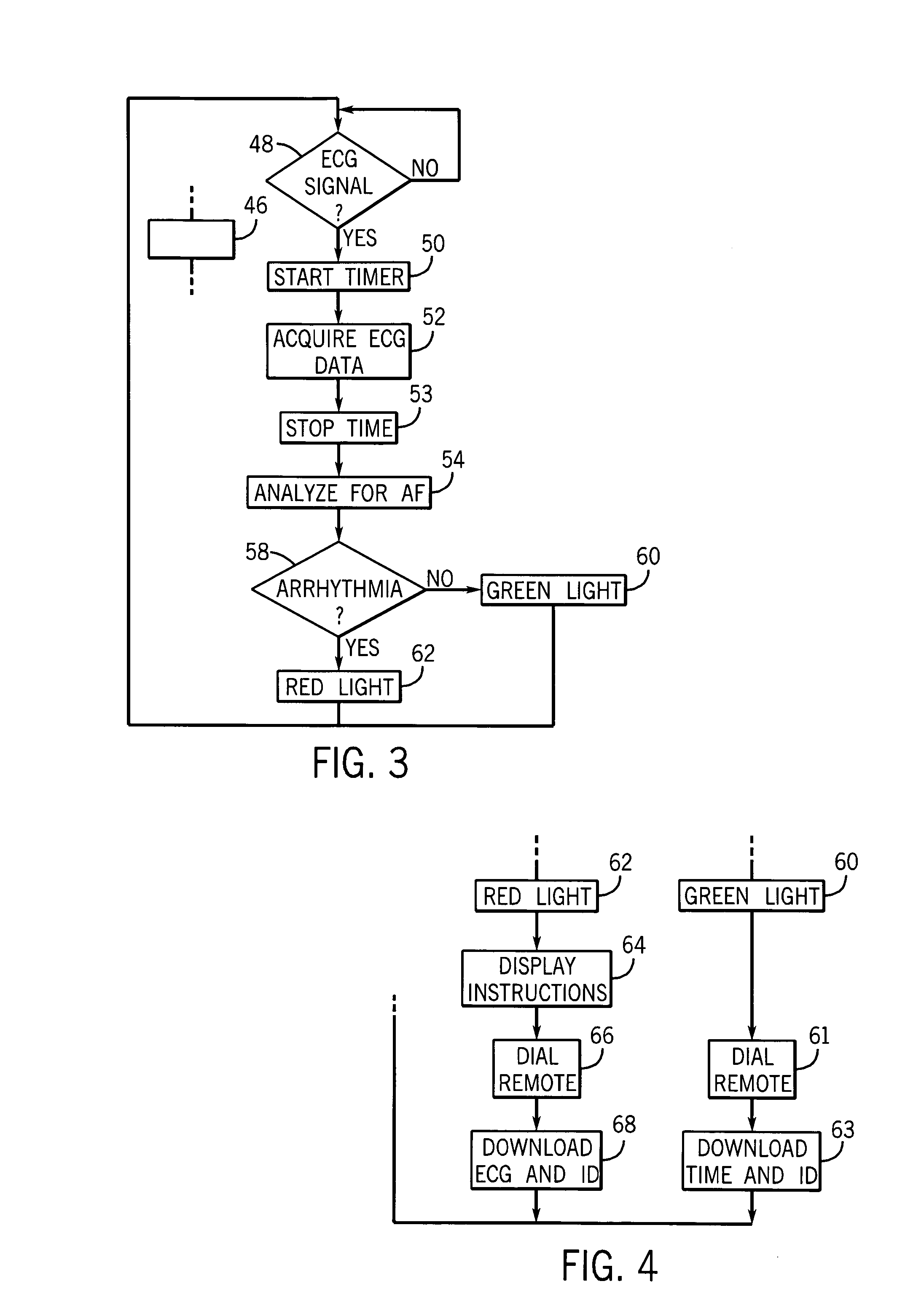
Long term cardiac monitor
InactiveUS7117031B2Reliable detectionLong-term monitoringElectrocardiographyCatheterCardiac arrhythmiaECG Measurement
A cardiac arrhythmia monitor provides electrodes to allow daily ECG measurements of a patient without cumbersome electrode connection to the patient. ECG data may be diagnosed by the monitor to indicate likelihood of an arrhythmia and an indication provided to the patient ECG data based on that indication may be forwarded to a physician or other healthcare professional for a review.
Owner:LOHMAN TECH
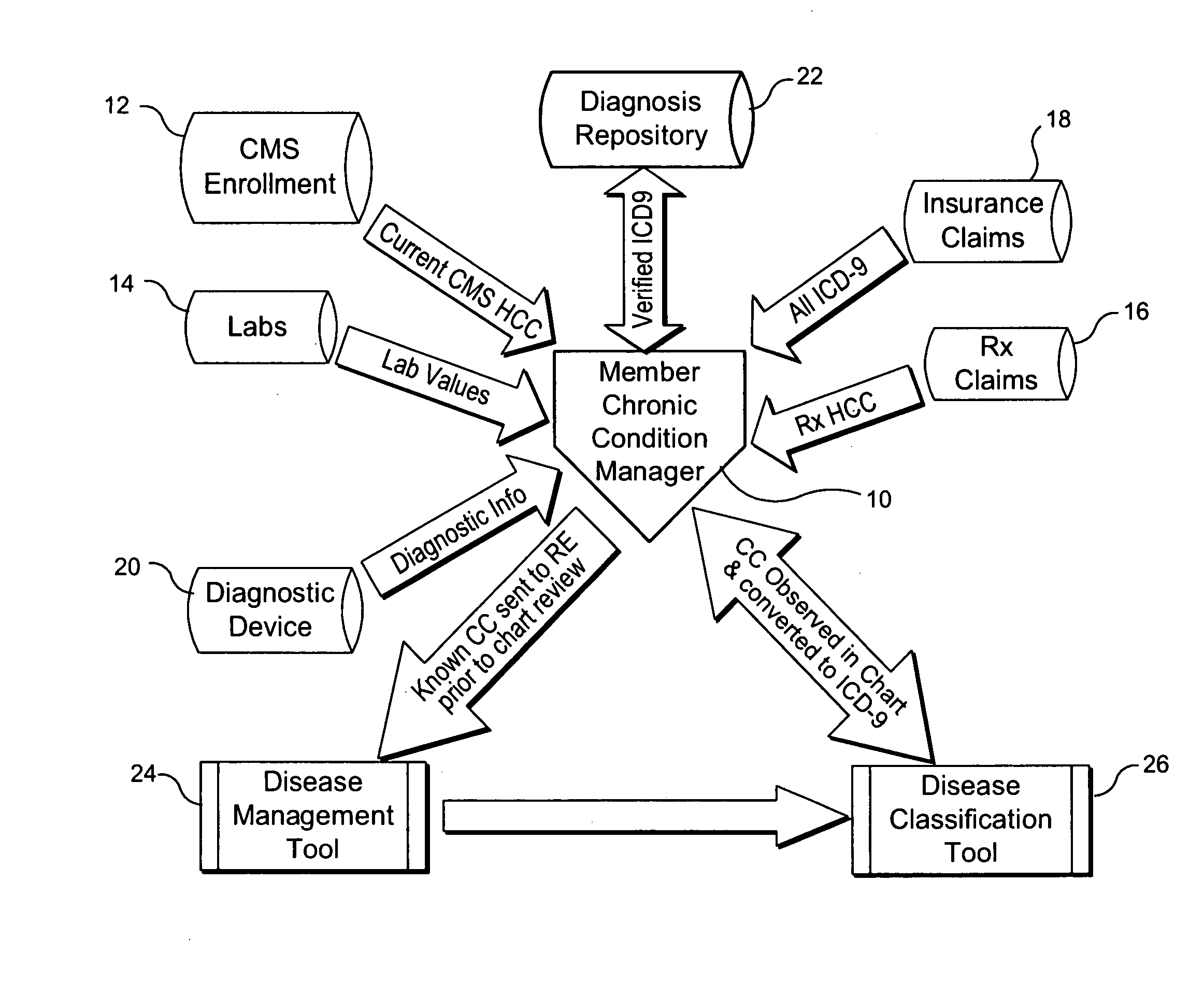
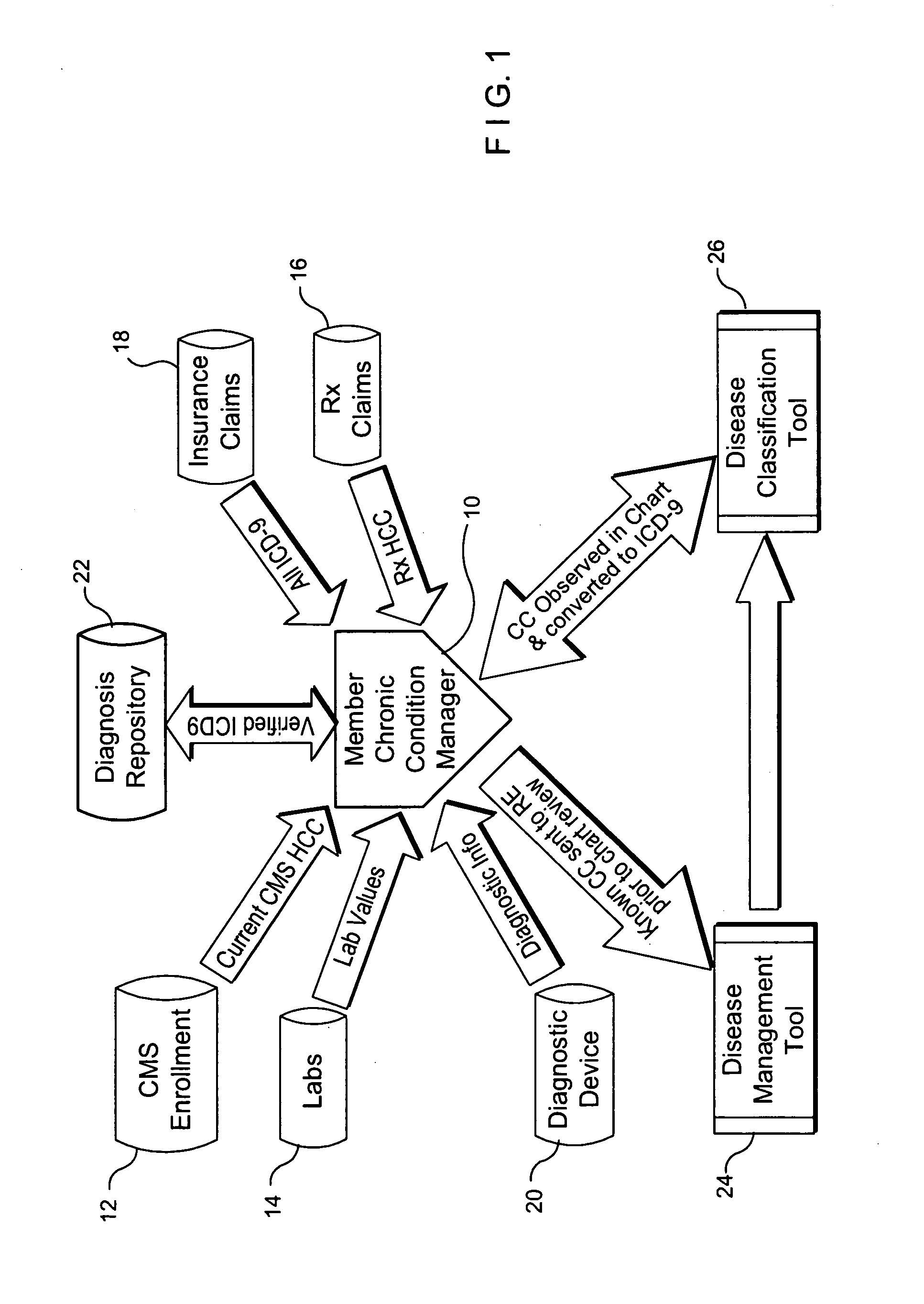
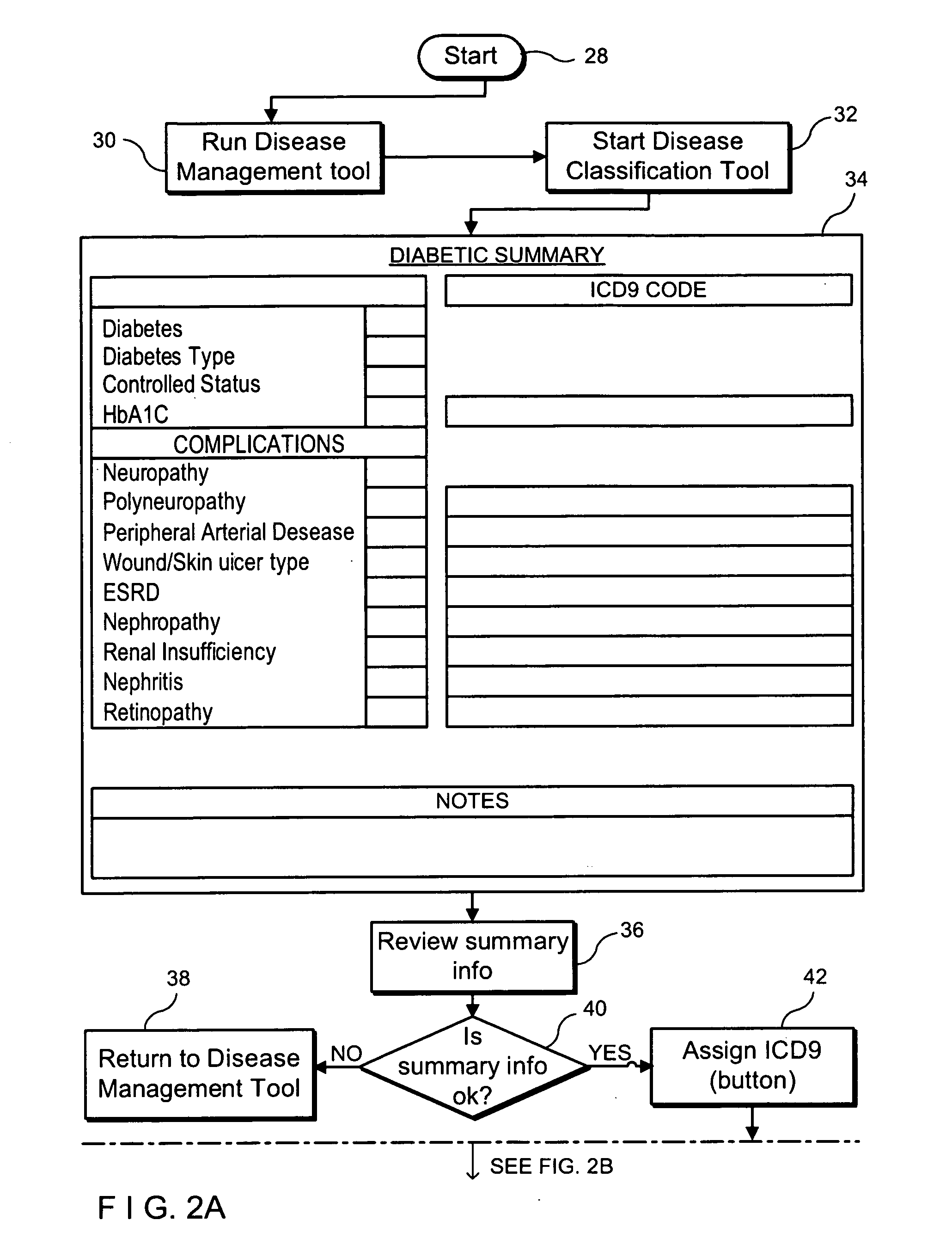
System and method for determining and verifying disease classification codes
InactiveUS20080086327A1Data processing applicationsMedical automated diagnosisChart datumDisease classification
A system and method for determining an updated disease classification code for a patient within a managed care population consisting of (i) a patient condition processing unit for receiving a plurality of patient-related data, (ii) a diagnosis repository database coupled to the patient condition processing unit for storing a preestablished disease classification code for the patient, and (iii) a disease classification code application tool designed to convert medical chart data of the patient into an observed disease classification code for the patient wherein the observed disease classification code is forwarded to the patient condition processing unit and stored in a diagnosis repository database as the updated disease classification code. The updated disease classification code can then be forwarded to the treating physician, reimbursement agency, or any other agency requiring such data. The patient-related data can consist of analog or electronic information relating to patient descriptions, including diagnosis, symptoms, exacerbations and treatment made by the treating physician, patient enrollment data, patient enrollment data, laboratory data, prescription drug data, insurance claims data, data from a diagnostic medial device (such as a heart monitor), etc.
Owner:QMED
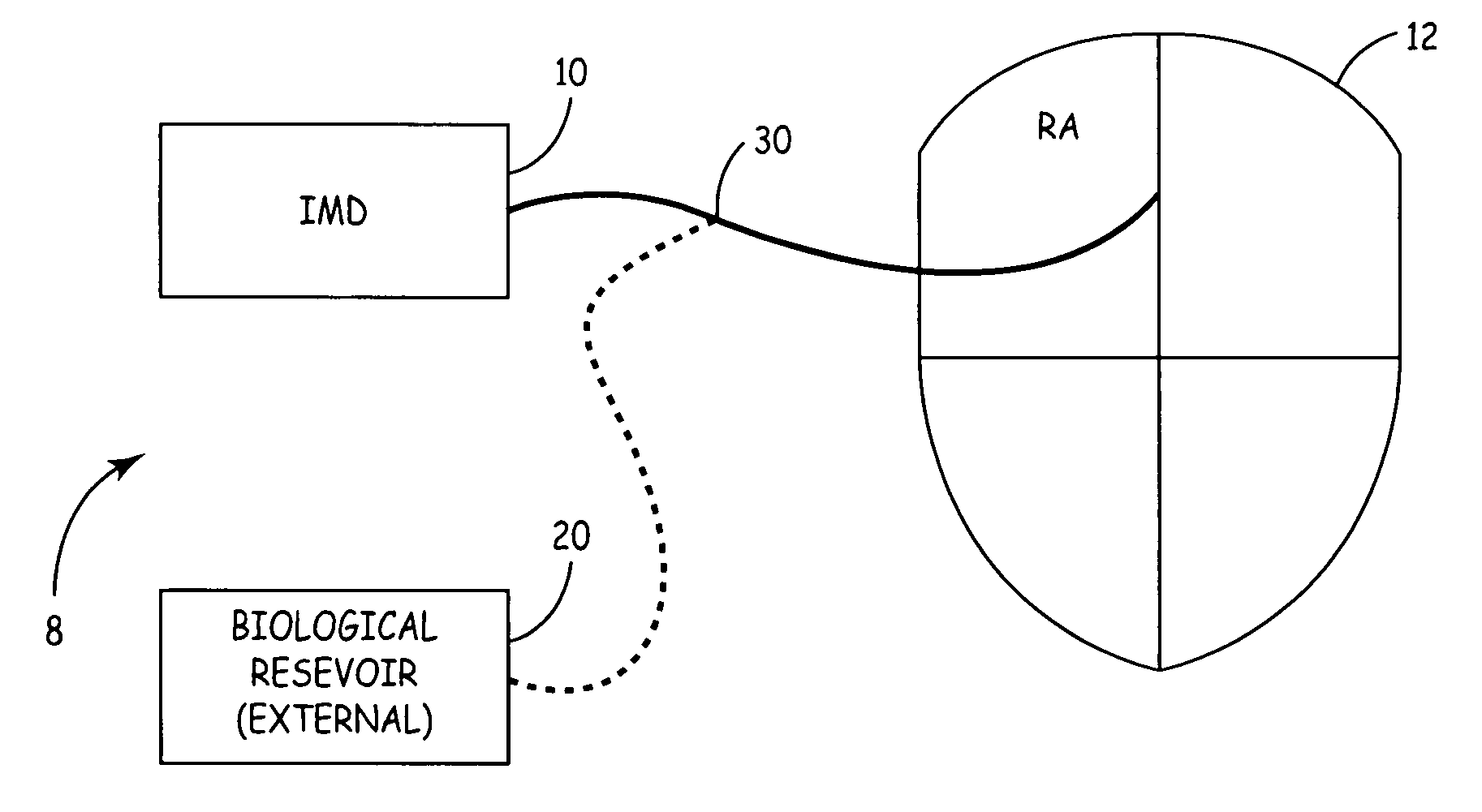
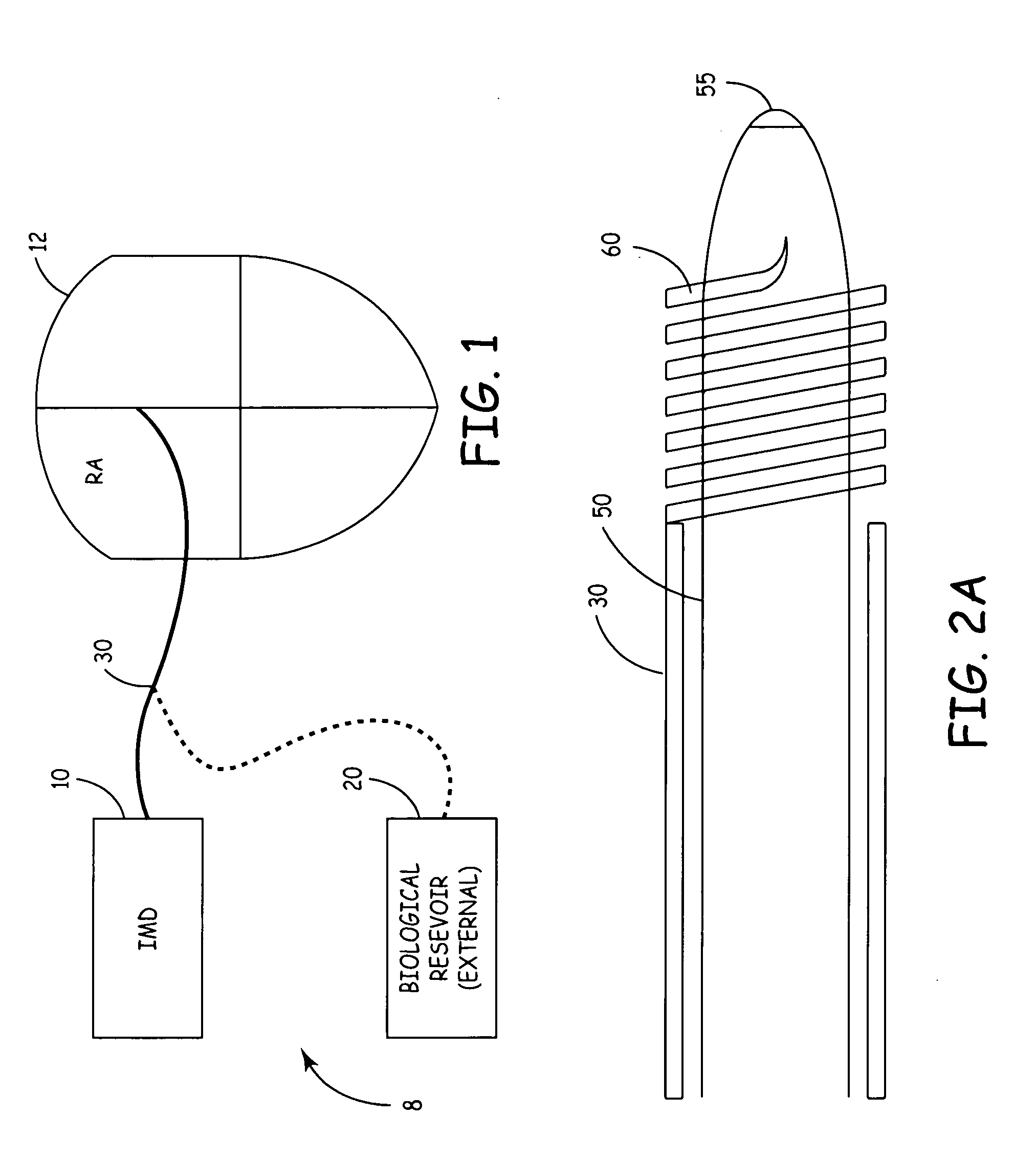
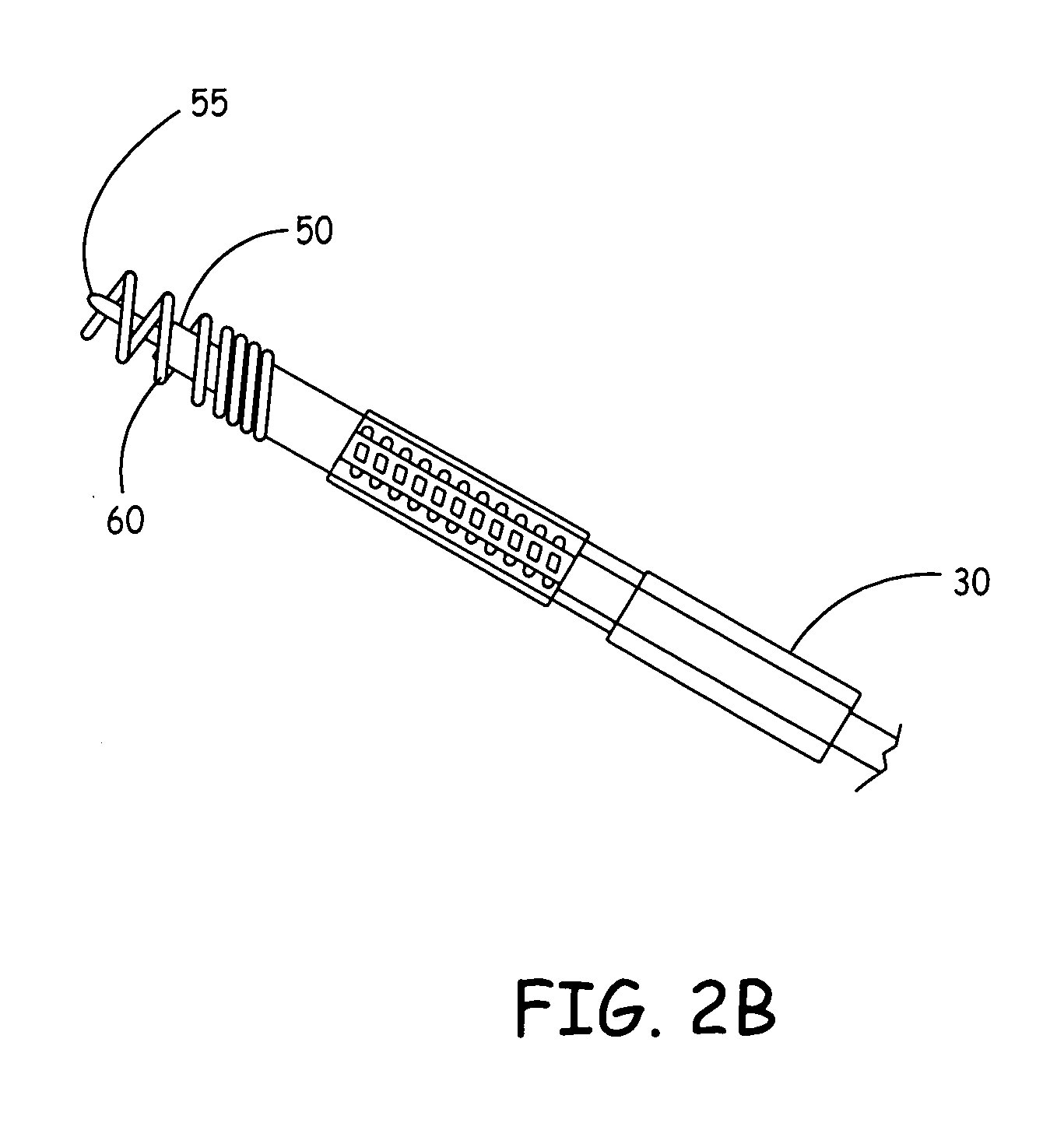
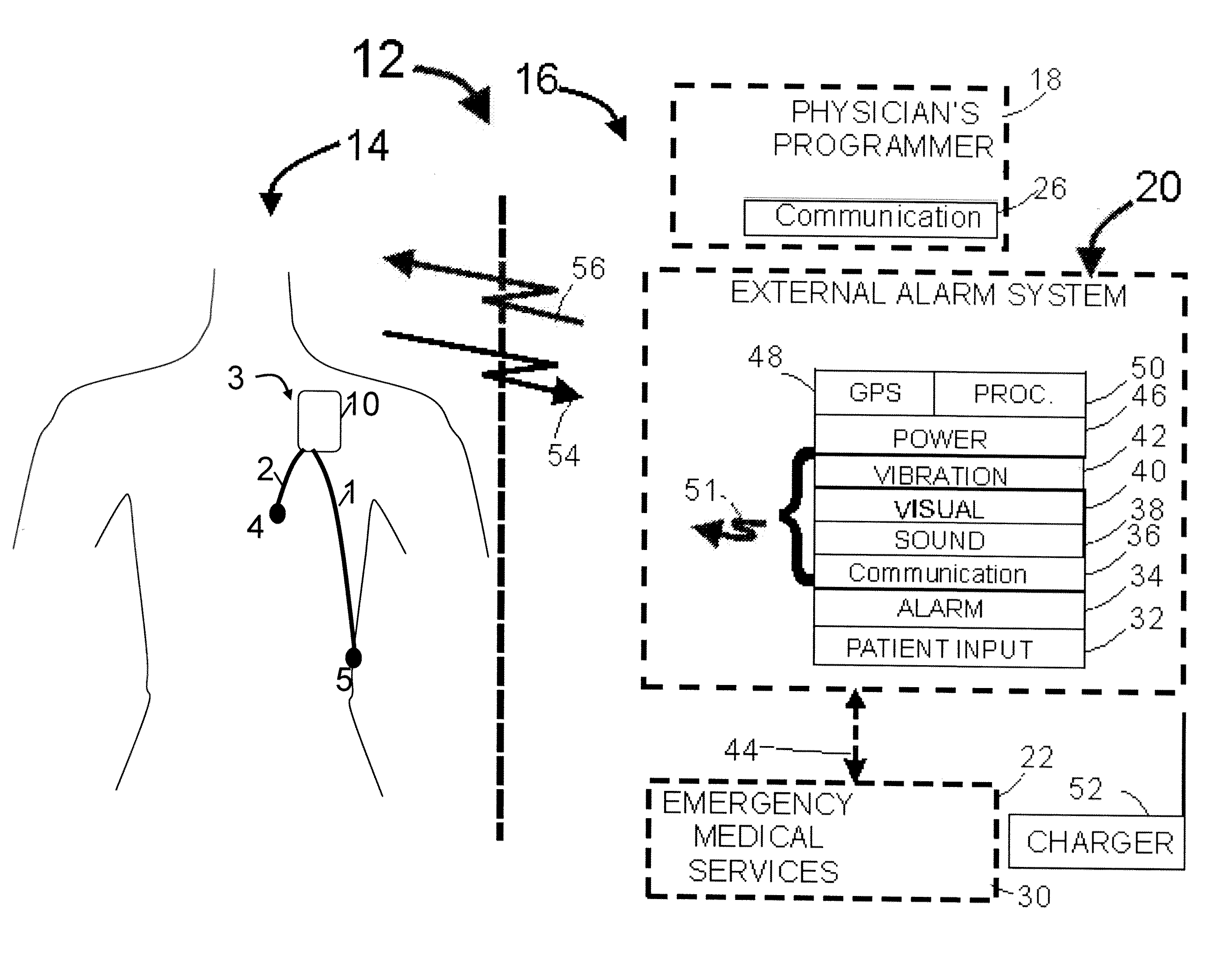
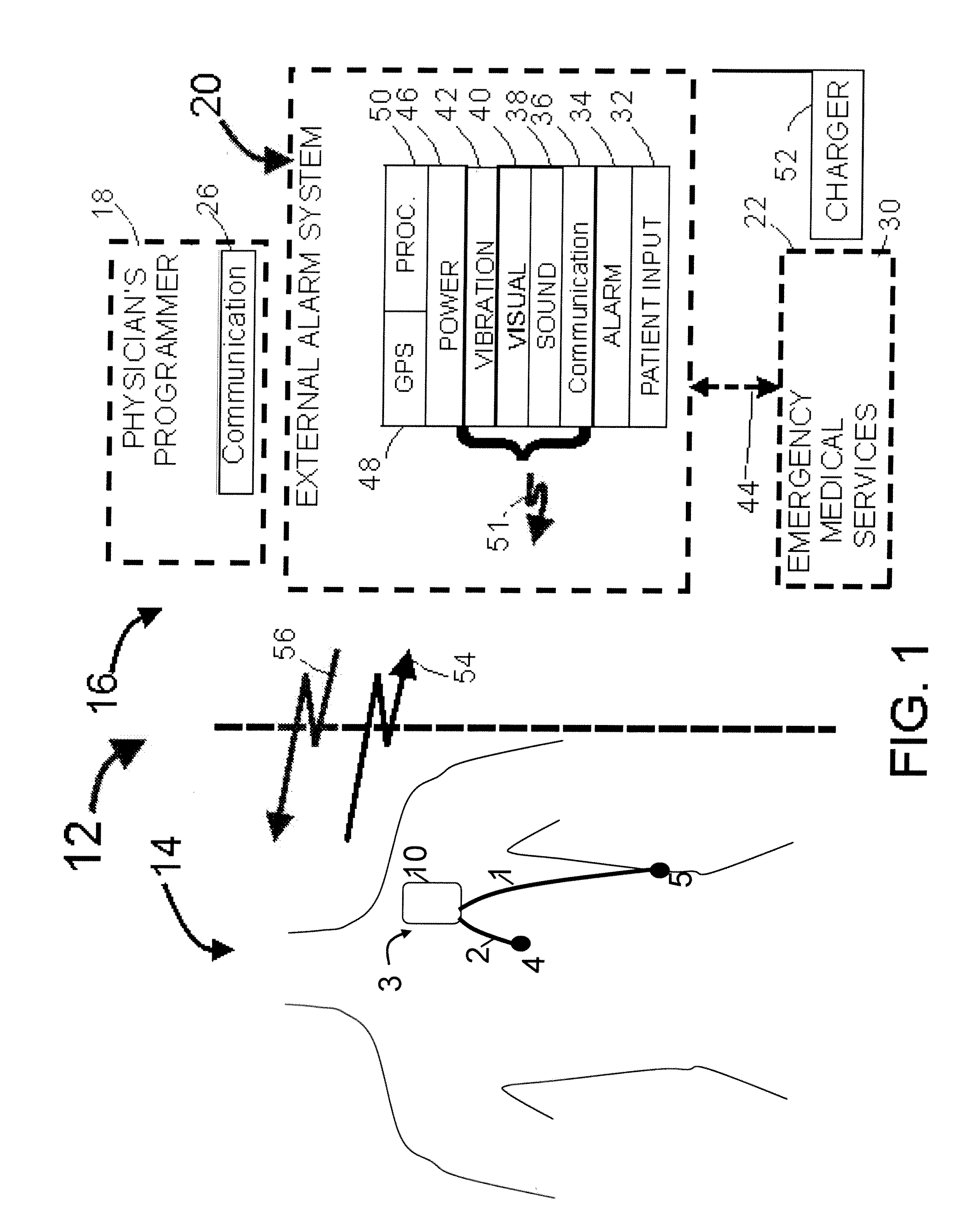
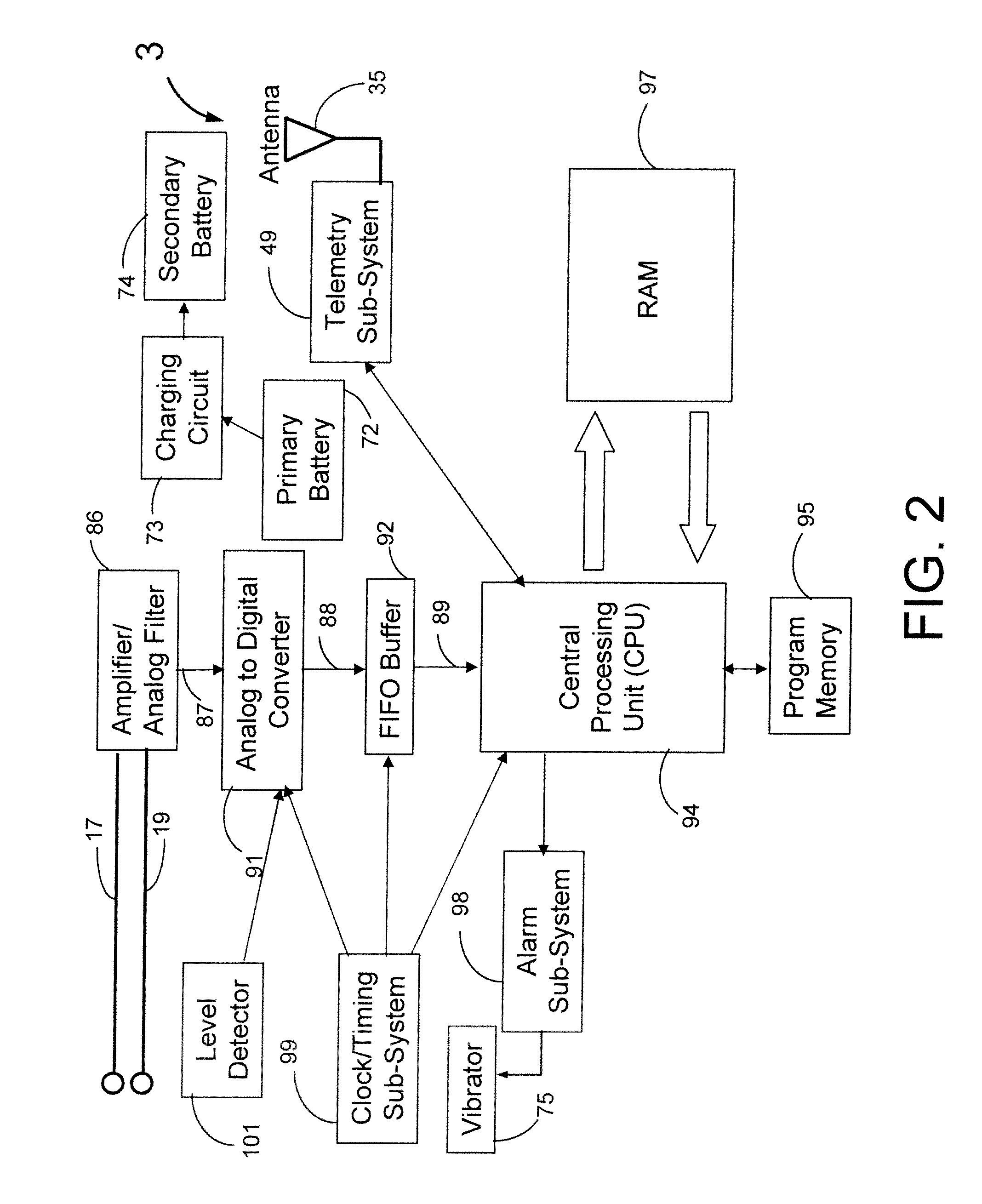
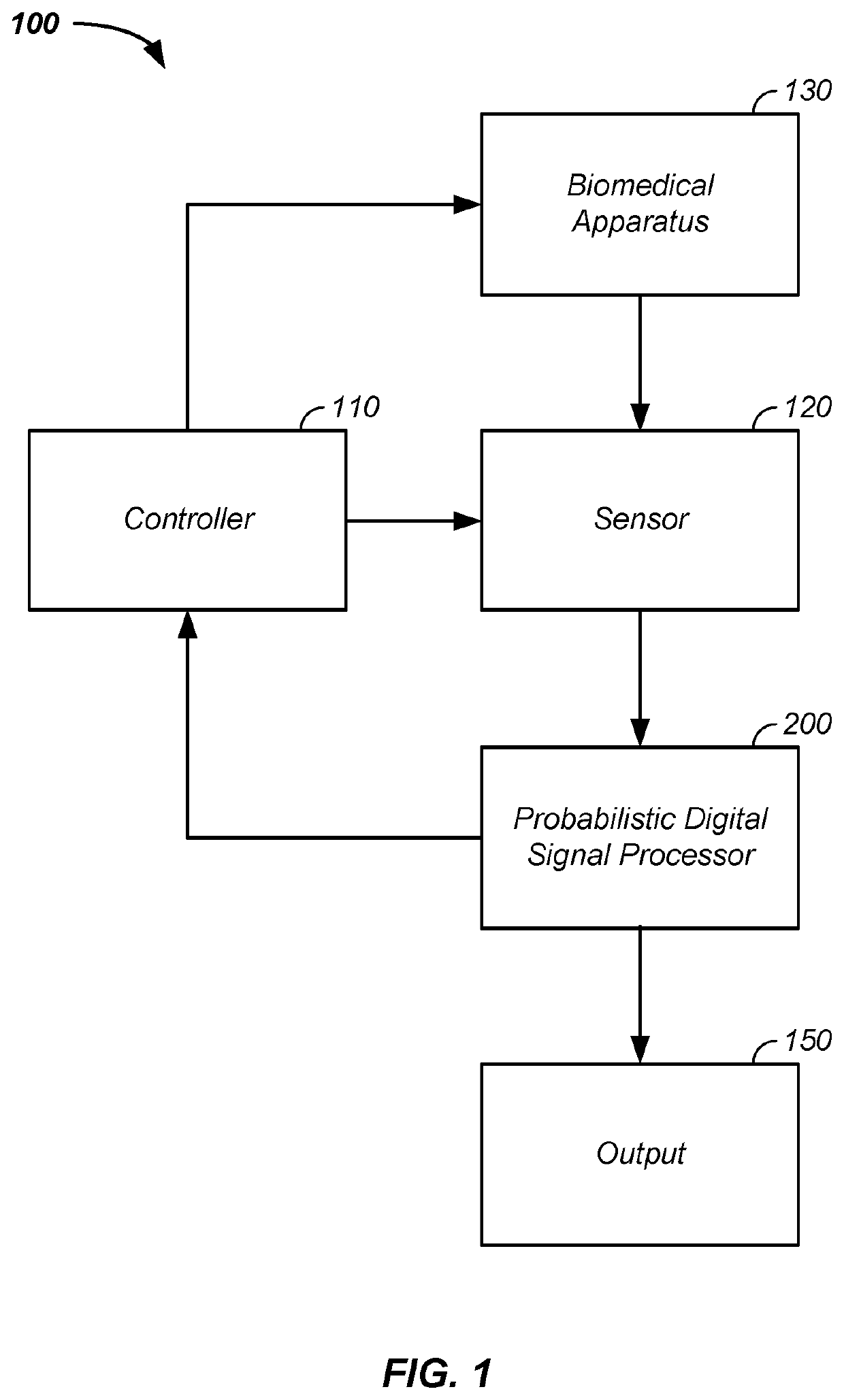
System for the delivery of a biologic therapy with device monitoring and back-up
InactiveUS20050021091A1ElectrocardiographyGenetic material ingredientsCardiac monitoringMedical device
An implantable medical device (IMD), such as a cardiac monitor and / or pulse generator is implanted during a procedure where a biologic is introduced into a targeted area of the heart. The IMD monitors cardiac performance to determine the efficacy of the biologic. Based on the achieved efficacy, the IMD will either take no action, provide device based therapy, and / or ablate the tissue to destroy the biologic and its effects if the biologic proves unsuccessful.
Owner:MEDTRONIC INC
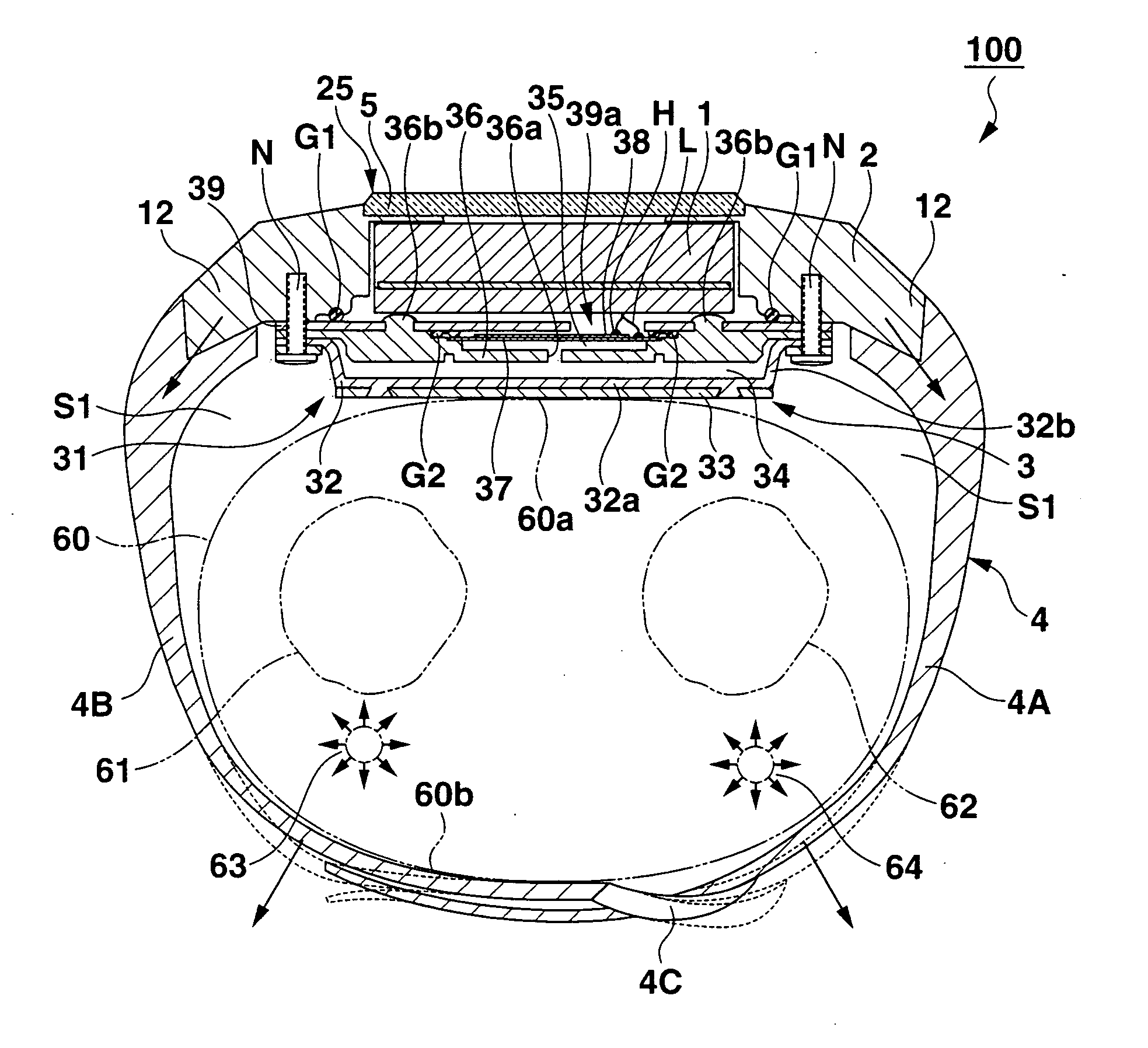
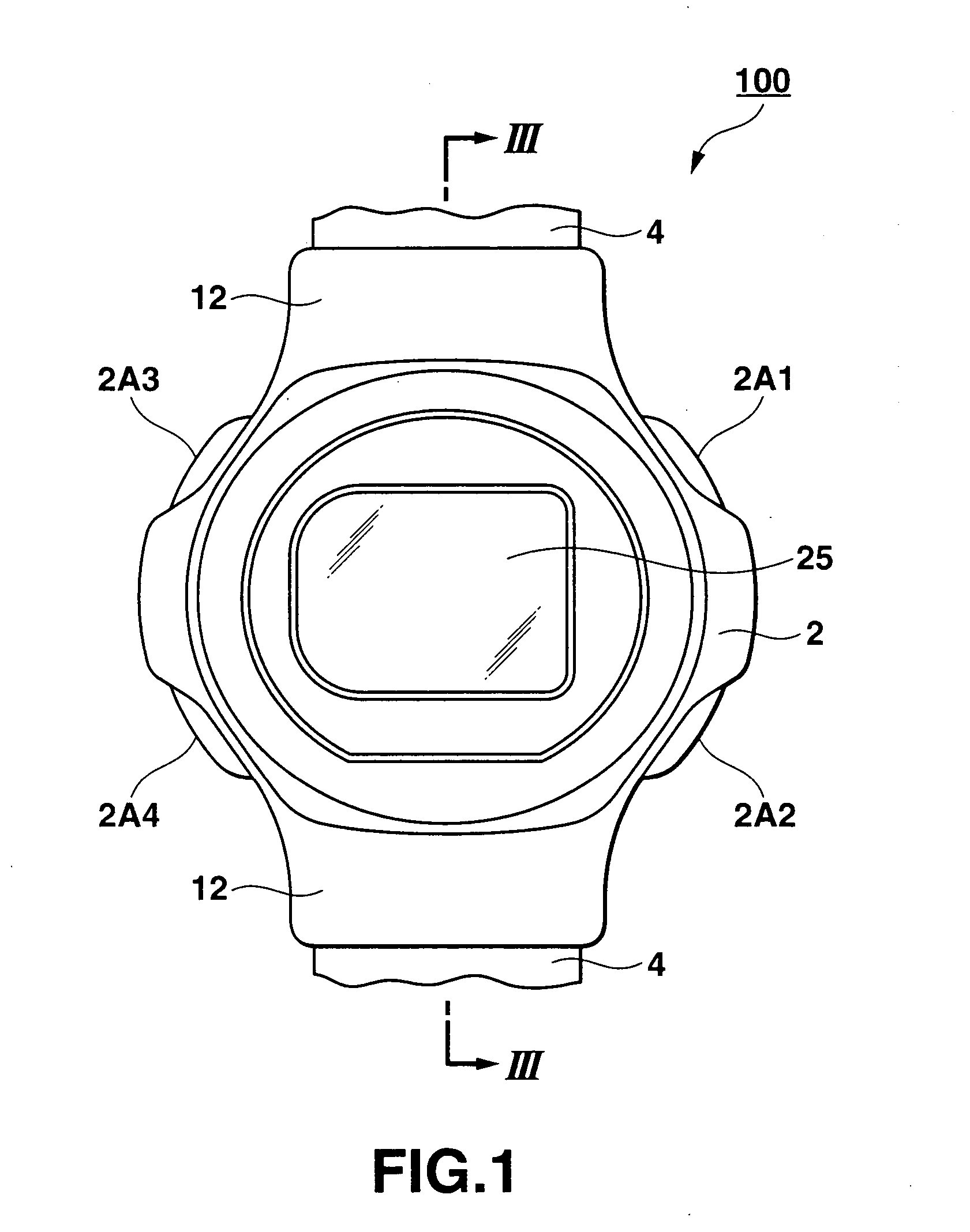
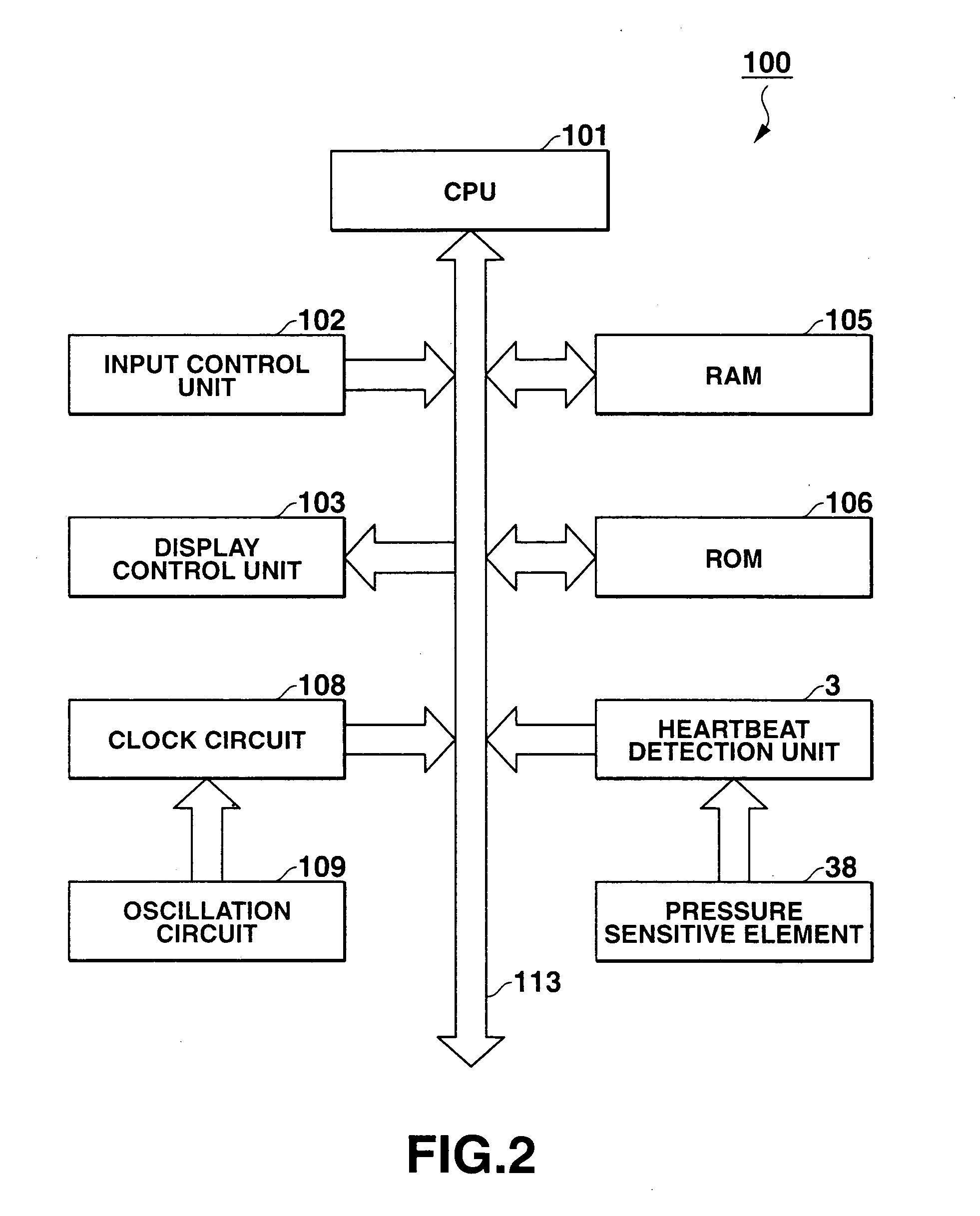
Wearable heartbeat measuring device, system and method
The wearable heartbeat measuring device is accomplished by wearing a wrist-watch-like heart monitor device on the wrist. The heart monitor is worn on the top of the wrist with a strap around the wrist. The strap has an inflexible extending portion that extends from the heart monitor at a predetermined angle and a predetermined width with respect to the wrist so that a predetermined space is maintained between the top portion of the wrist and the strap for promoting the transfer efficiency of the pulsation force that is initially experienced at a part of the strap at the bottom of the wrist. The strap also has a flexible portion. A predetermined angle and a predetermined width of the extended portion also facilitate the flexible portion to form a flat area where the wrist contacts the strap. In the prefer embodiments, the width of the strap exceeds the width of the wrist when it is worn.
Owner:OTAX CO LTD +1
Parameter value rejection for a cardiac monitor
A heart monitor is disclosed. The monitor computes ST segment deviations and stores the results in heart rate based histograms. Periodically, the monitor analyzes the histogram data to determine a median value of ST deviation. Subsequently, beats are excluded from the computation of the time series if their ST deviations both varies too far from the long term median value and varies too far from the then current time series value.
Owner:ANGEL MEDICAL SYST
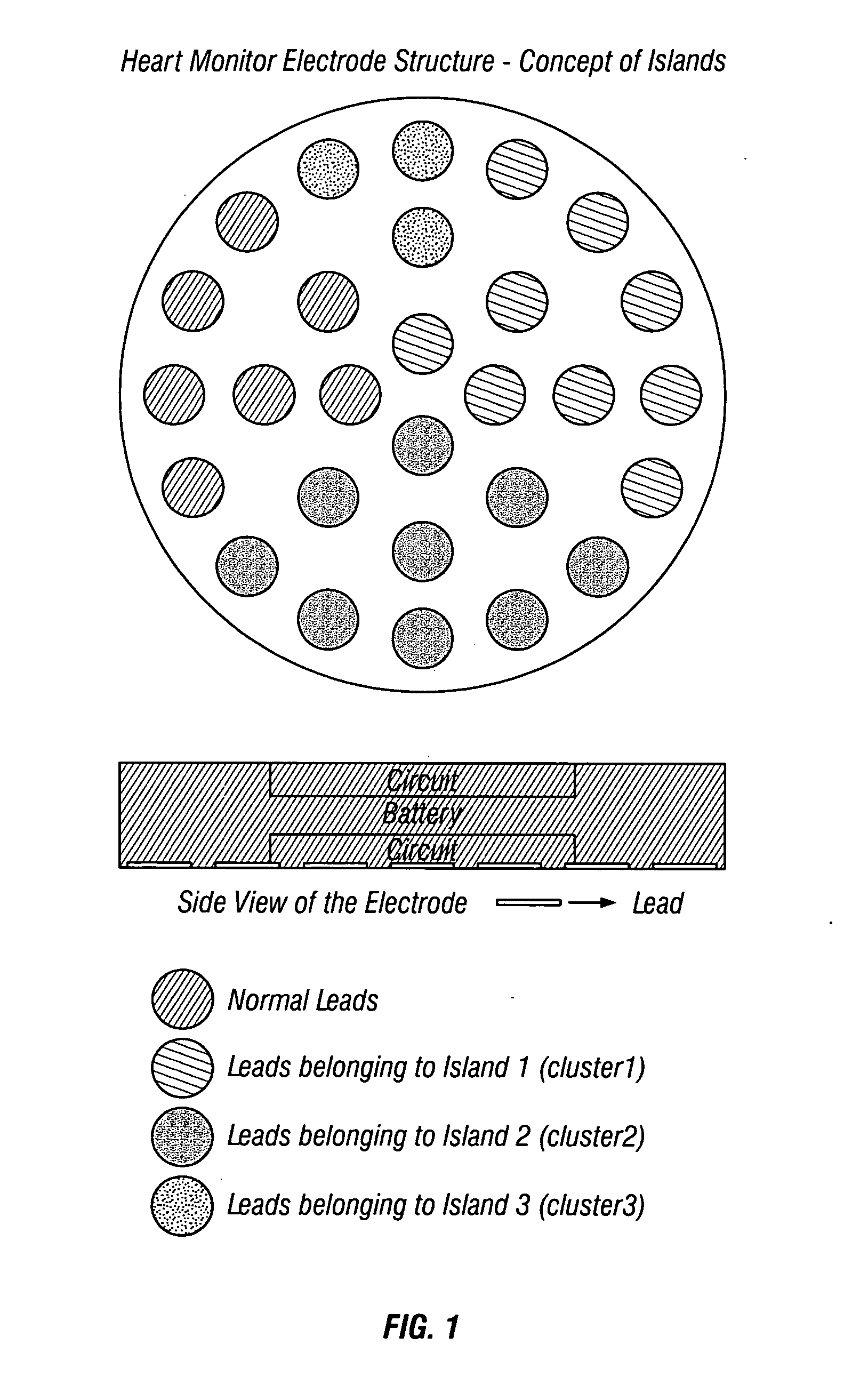
Heart monitor electrode system
A bioelectric interface for monitoring, detection and transmission of detected ECG data is provided comprising a sensory system for detecting bio-physiological measurements utilizing spatially resolved potential profiles obtained from a localized cluster of sub-electrodes to form constituent sets of miniature sensor arrays. Using only a single macro-electrode, two or more sets of sub-electrode arrays are used to measure bipolar spatial gradients obtained from measured cardiac potentials. The sets of sub-electrodes containing the clusters are optimized to attain measurable gradients of diagnostic value. A minimax procedure allows bio-potential sensory acquisition through a bi-directional digital steering process, which essentially comprises monitoring, detection, selection, grouping, recording and transmission of ECG waveform characteristic data.
Owner:GLOBAL CARDIAC MONITORS
Portable cardiac monitor
A system and method for obtaining ECG signals from an ambulatory patient are disclosed herein. The system is configured to be inexpensive, small, and robust for outpatient monitoring. The system is configured to be a low power consuming device. The system provides options for a variety of settings and real-time access to the ECG signals being recorded during the recording period.
Owner:EXELYS
Parameter value rejection for a cardiac monitor
A heart monitor is disclosed. The monitor computes ST segment deviations and stores the results in heart rate based histograms. Periodically, the monitor analyzes the histogram data to determine a median value of ST deviation. Subsequently, beats are excluded from the computation of the time series if their ST deviations both varies too far from the long term median value and varies too far from the then current time series value.
Owner:ANGEL MEDICAL SYST
Portable cardiac monitor
A system and method for obtaining ECG signals from an ambulatory patient are disclosed herein. The system is configured to be inexpensive, small, and robust for outpatient monitoring. The system is configured to be a low power consuming device. The system provides options for a variety of settings and real-time access to the ECG signals being recorded during the recording period.
Owner:EXELYS
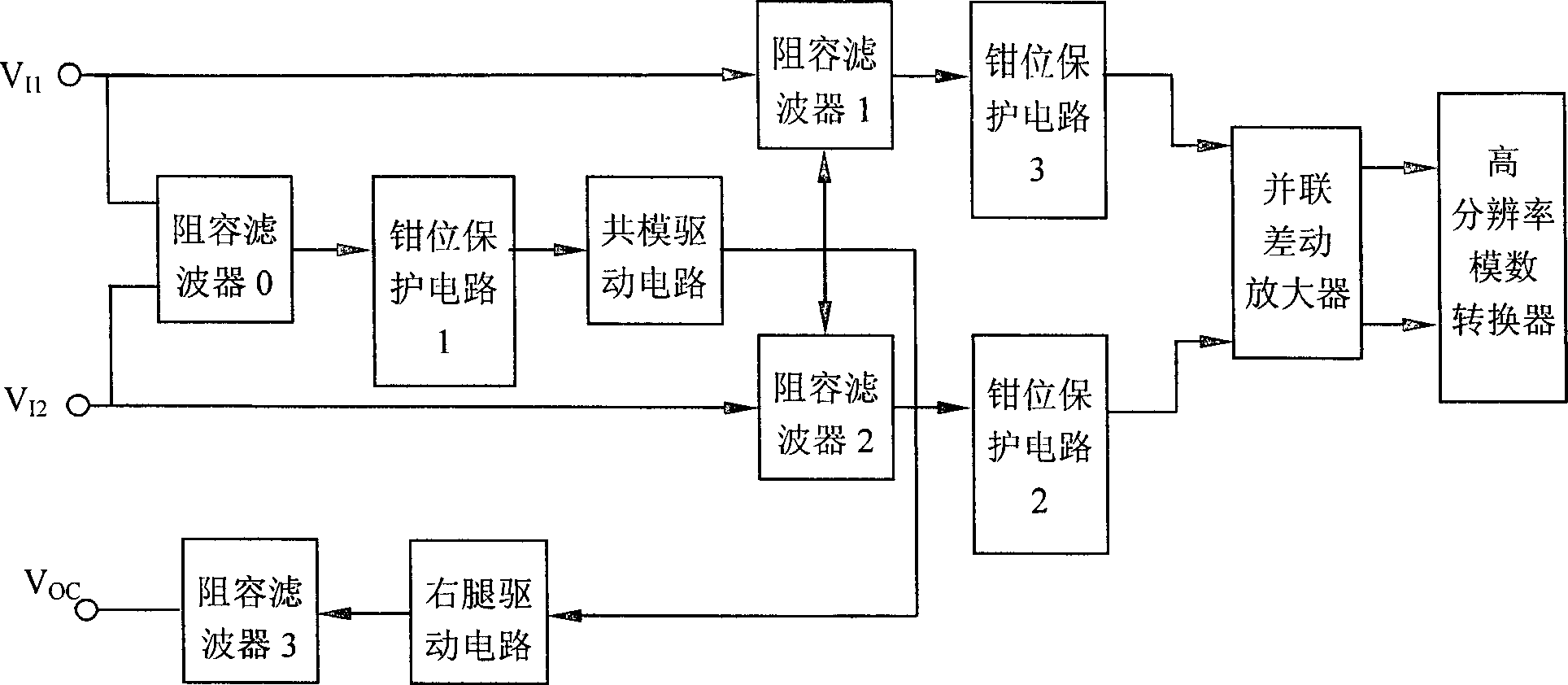
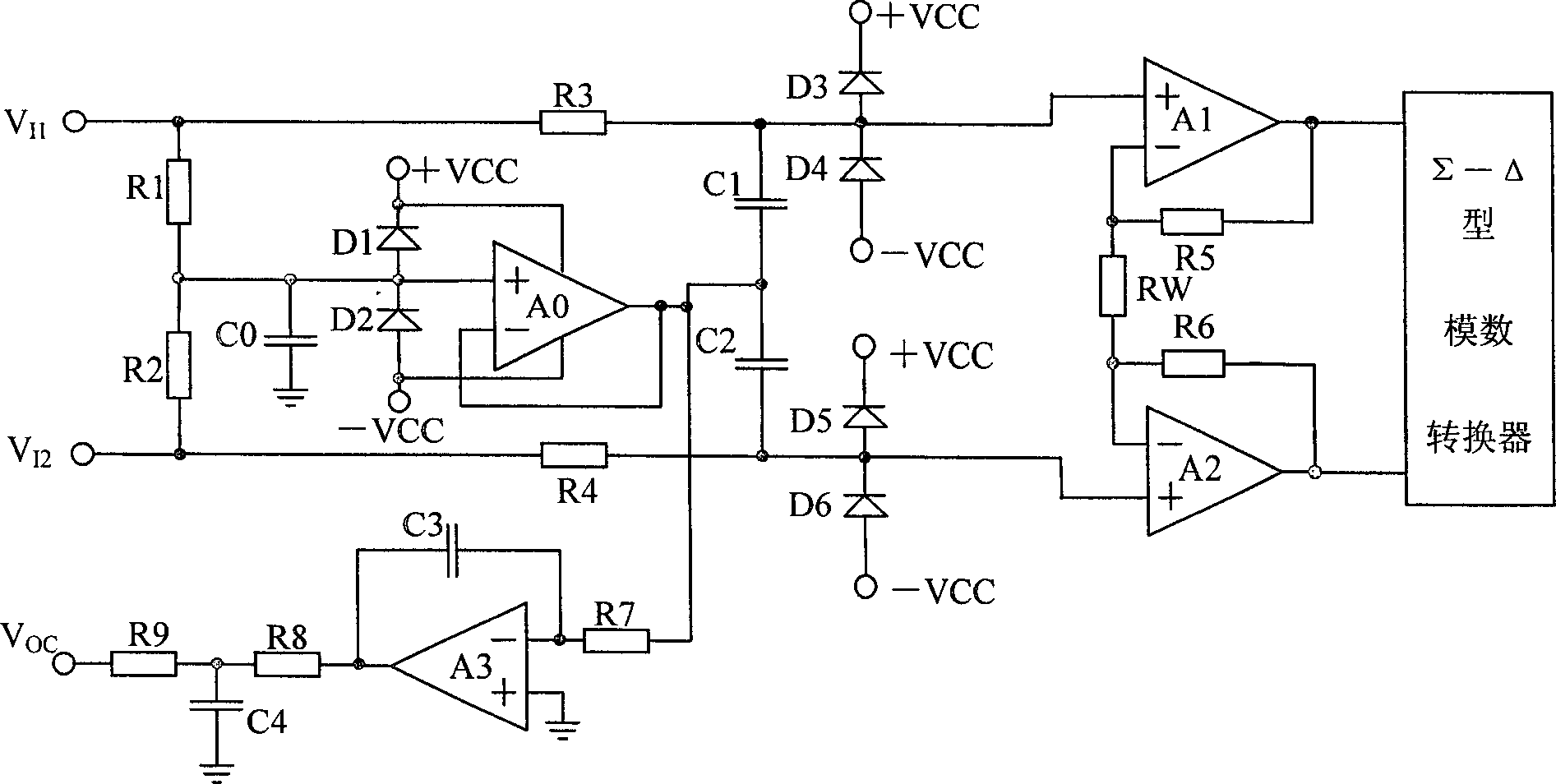
Cardiac monitor module capable of resisting high frequency electric knife interference
InactiveCN1806751AStable outputSuppress interferenceDiagnostic recording/measuringSurgical instruments for heatingCapacitanceEcg signal
The invention relates to physical electrical field, the medical equipment, which in detail relating to an electric knife-resistant cardio-electric monitoring module, technical project of which comprises: the 0 capacitance-resistance filter receiving the two-way electro-cardio signal, the output of the 0 capacitance-resistance filter passing the first protecting clamper, common mode drive circuit, right-leg drive circuit and the third capacitance-resistance filter in turn; one of said two-way electro-cardio signal passing the first capacitance-resistance filter, the third protecting clamper in turn to be input to parallel differential amplifier; the other electro-cardio signal passing the second capacitance-resistance filter, the second protecting clamper in turn to be input to parallel differential amplifier; the output of which is connected to high-resolution cathode analogue / digital converter; the connection of the first and second capacitance-resistance filter is connected to common mode drive circuit. The invention is mainly used in patient monitor for operation.
Owner:TIANJIN UNIV
Portable cardiac monitor including a range limiter
A system and method for obtaining ECG signals from an ambulatory patient are disclosed herein. The system is configured to be inexpensive, small, and robust for outpatient monitoring. The system is configured to be a low power consuming device. The system provides options for a variety of settings and real-time access to the ECG signals being recorded during the recording period.
Owner:EXELYS
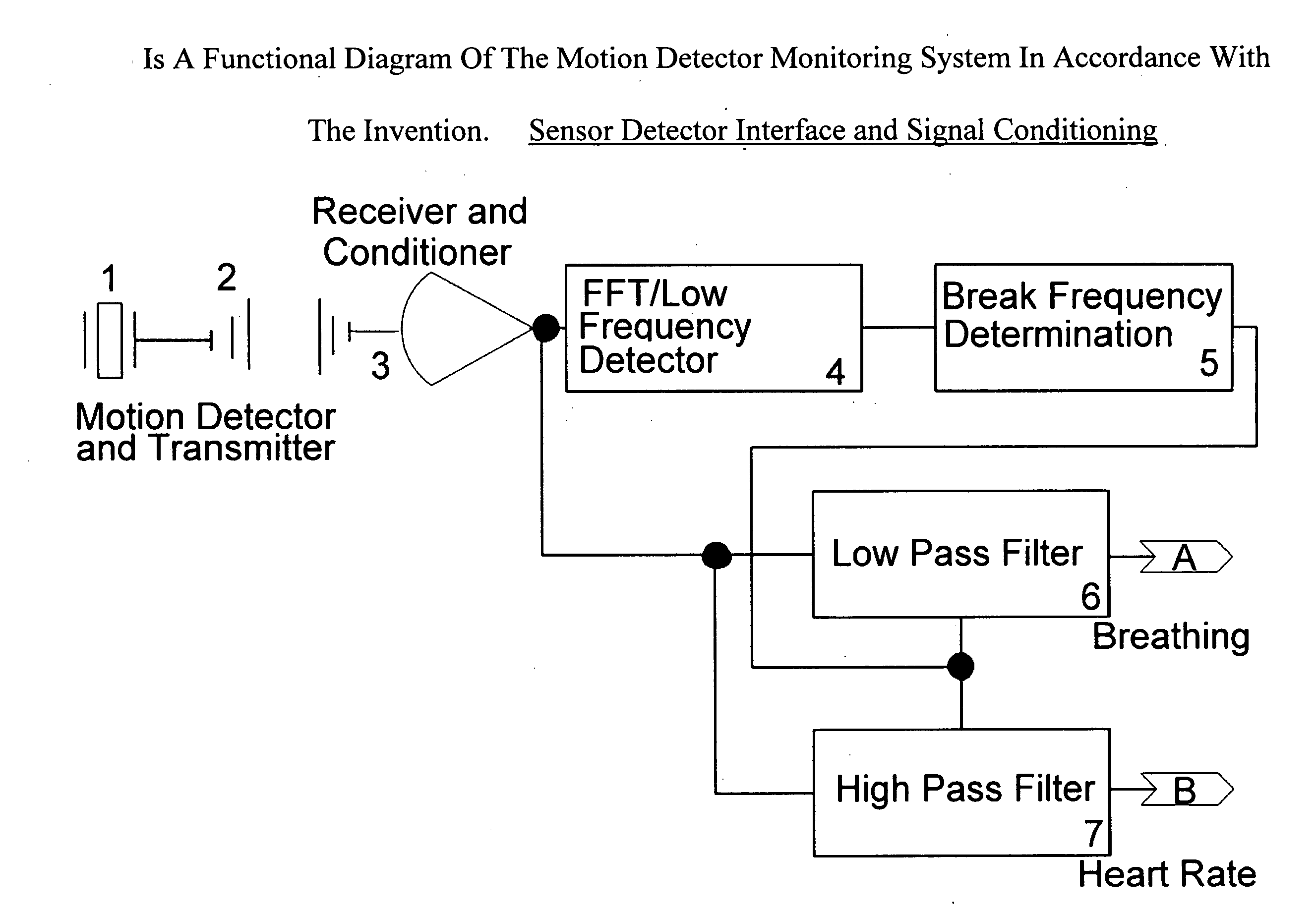
Portable Apnea and Cardiac Monitor
This invention relates to non-invasive monitoring devices, in monitoring minute movements made by the body to report the presence or absence of respiration and normal heart rate. The movements being measured are the pulsations made by the normal operation of both the heart and lungs. This is accomplished by converting the body movements into electrical signals with an adapted polymorph-piezoelectric transducer. The electrical signal that is detected is a mixed signal, a signal composed of a lower frequency (breathing contraction) and the higher frequency (heart pulse). The signals are detected by separating the body motions by an adaptive filter that has a break frequency at twice the frequency of the larger body movement signal (breathing contraction).The separate body movement signals operate with associated logic circuitry to allow each signal to be independently measured, recorded, and acted upon to determine if the individual (patient) is undergoing a life threatening experience. Such an event by either signal will trigger an audio and visual display alarm which is attached on or near the patient. The alarm event trigger is also connected to a low voltage detector circuit to indicate that the supply voltage has dropped below an acceptable level.
Owner:STRUBE RICHARD ELLIS
Method and apparatus for automatic determination of hemodynamically optimal cardiac pacing parameter values
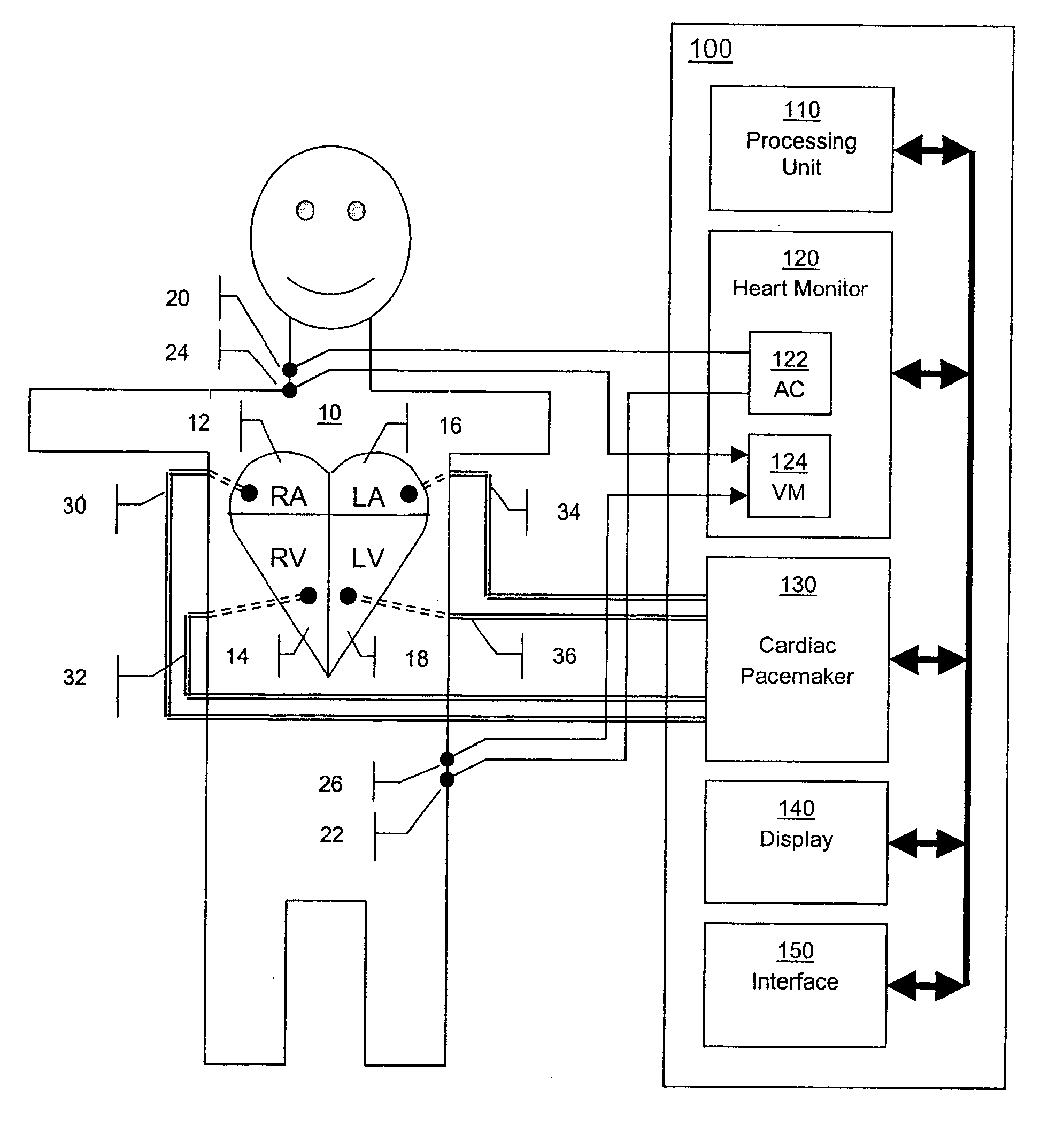
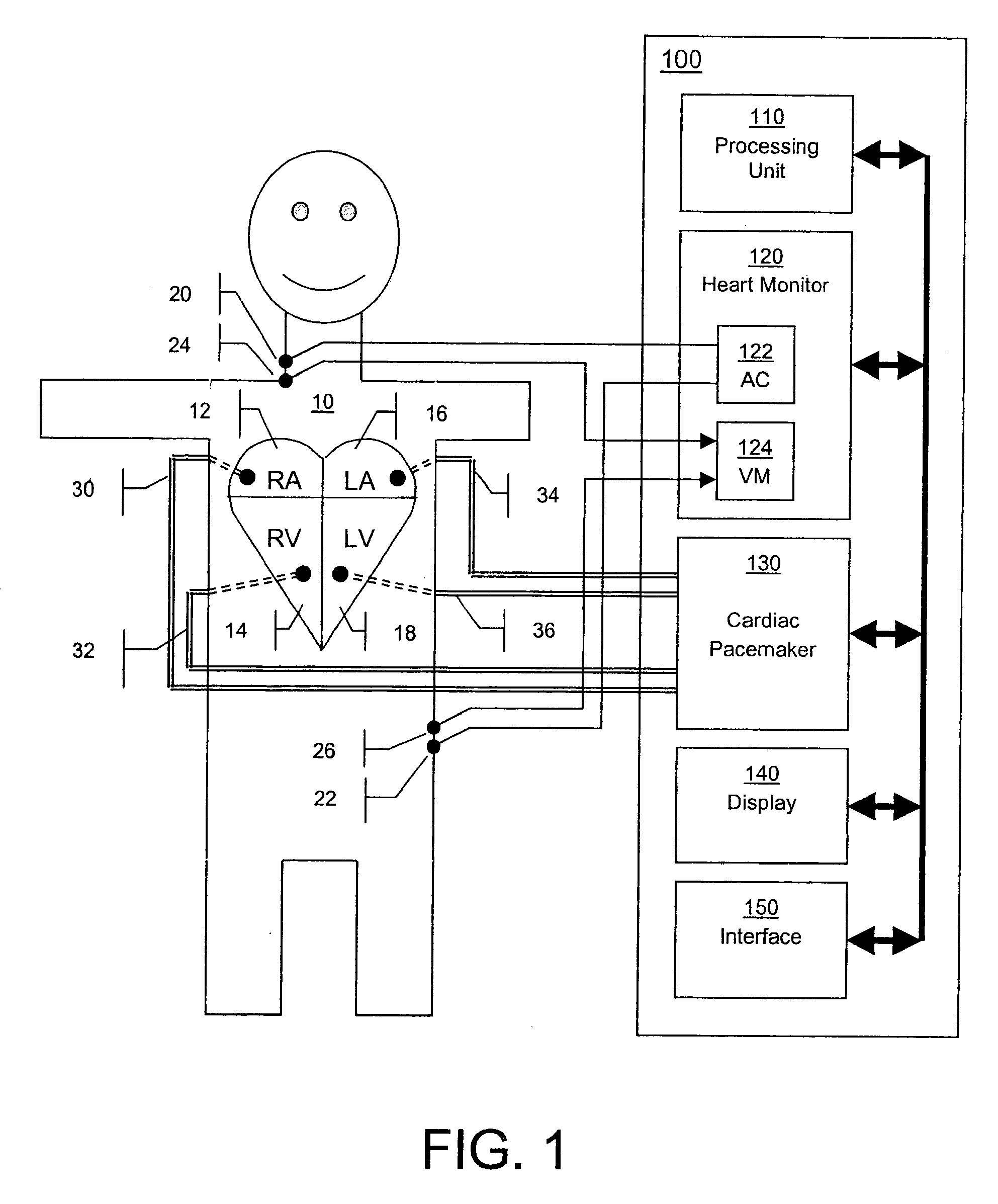
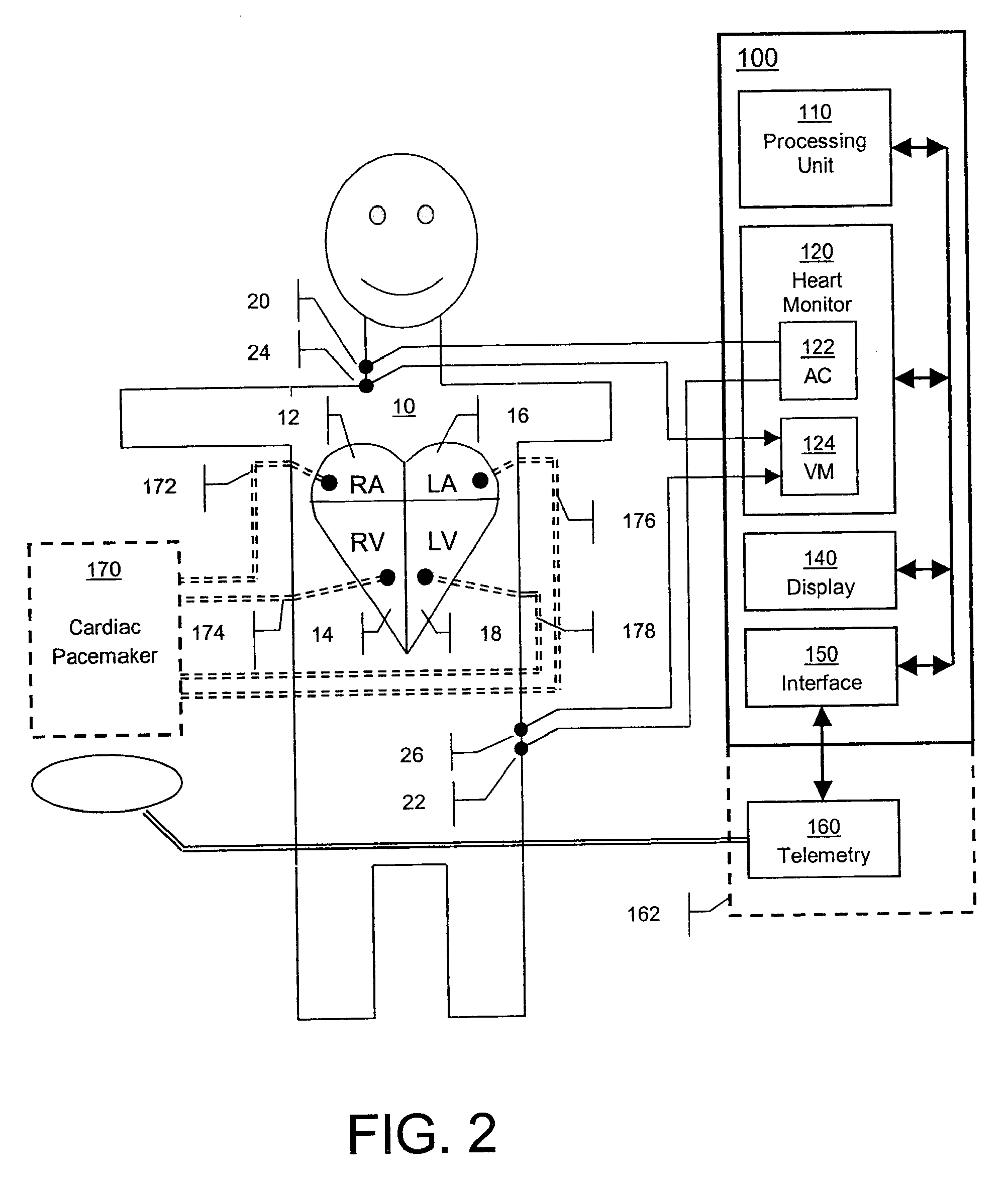
For cardiac rhythm management, a combination of cardiac pacing and a noninvasive heart monitoring is proposed for the determination of a set of programmable pacing parameters hemodynamically beneficial to the patient. The apparatus incorporates a cardiac pacemaker and a thoracic electrical bioimpedance (TEB) heart monitor. This combination allows the creation of a closed-loop system that obtains pacing parameter settings providing hemodynamically beneficial pacing therapy to the patient as determined by measuring and recording of stroke volume (SV), cardiac output (CO), and other indices of ventricular performance by the heart monitor during an optimization cycle automatically employing different permutations of values of pacing parameters such as atrioventricular delays, inter-atrial delay, inter-ventricular delay, or heart rate, that are sequentially programmed to the pacemaker. The hemodynamically beneficial permutation of pacing parameter values is determined from all recordings and programmed to the pacemaker for permanent or temporary pacing therapy.
Owner:OSYPKA MEDICAL
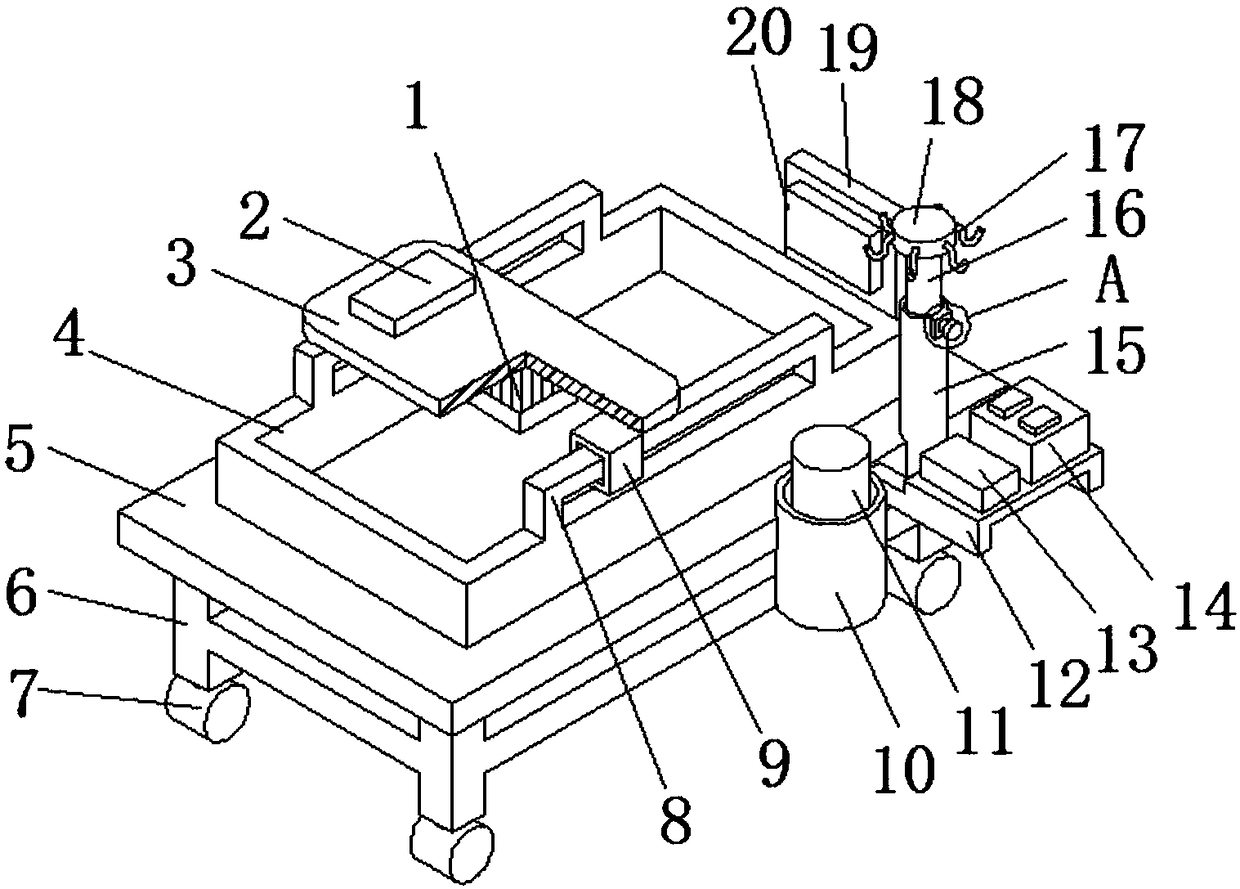
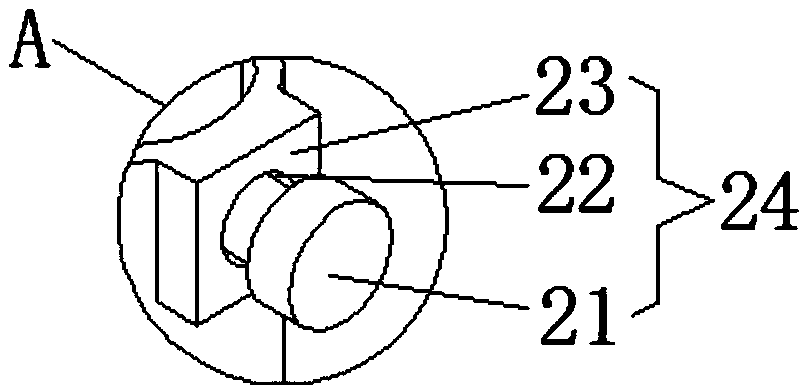
Paediatric clinical integrated type monitoring and rescue device
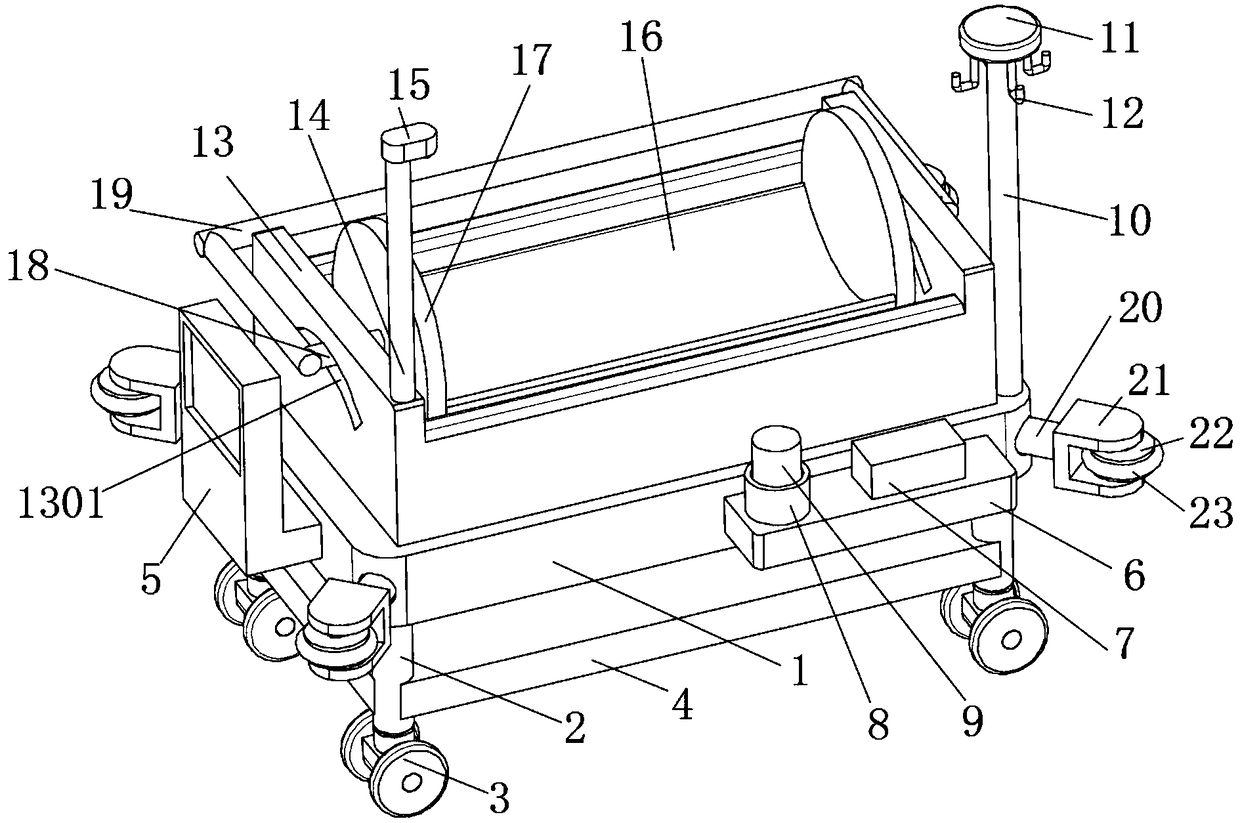
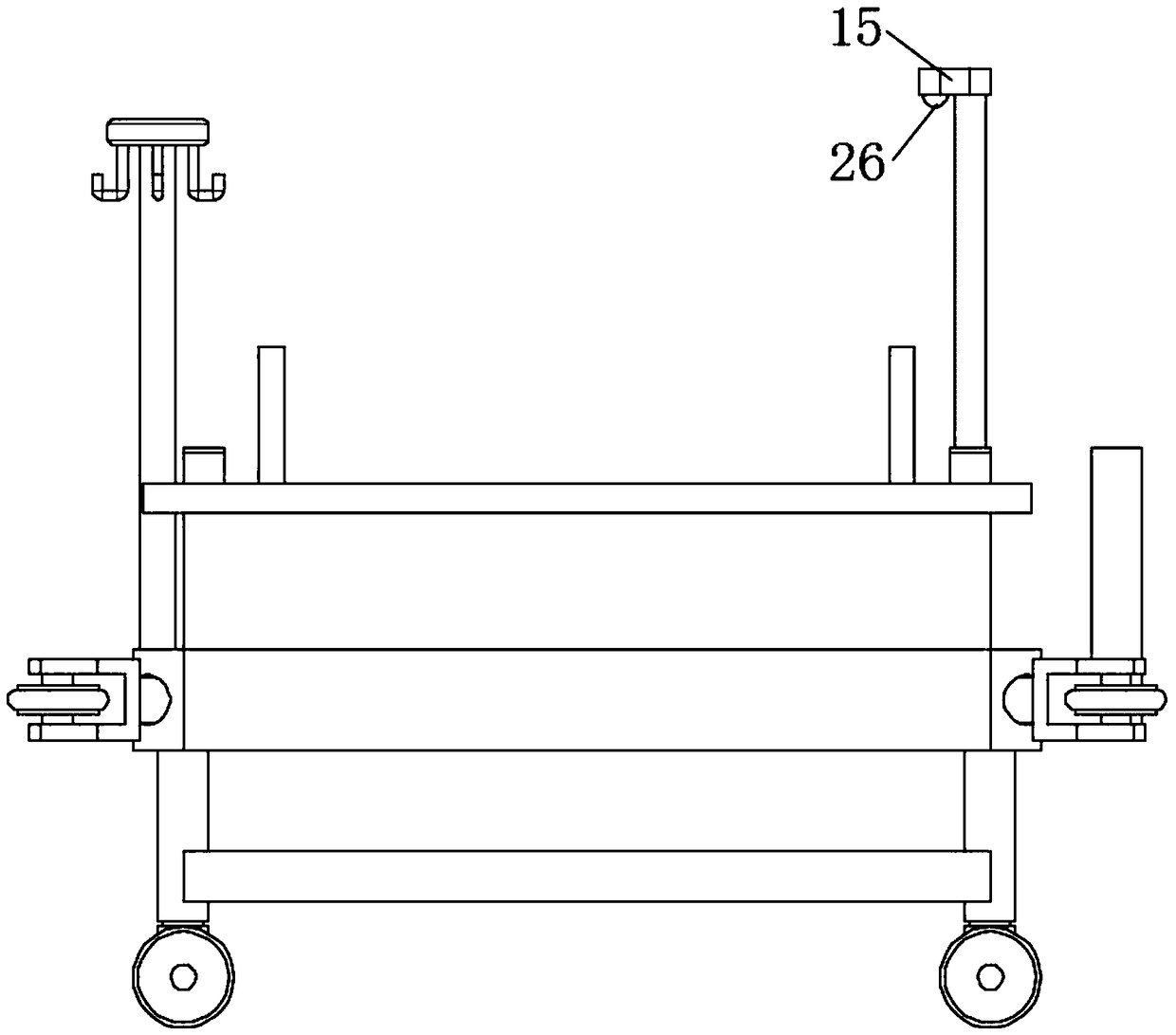
InactiveCN108784662AFunction increaseReal-time monitoring of physiological parametersRespiratorsHeart defibrillatorsEngineeringPaediatric patients
The invention discloses a paediatric clinical integrated type monitoring and rescue device. The device comprises a bed board, wherein the upper surface of the bed board is provided with a frame body,the left side and right side of the frame body are both provided with connecting frames, the outer surfaces of the connecting frames are movably in sleeved connection with connecting sleeves, the upper ends of the two connecting sleeves are provided with a flat plate, one side of the upper surface of the flat plate is provided with a PLC, the rear side face of the bed board is provided with a connecting plate, the side surface of the connecting plate is provided with a heart monitor, one side of the upper surface of the bed plate is provided with a first supporting rod, the inner portion of the upper end of the first supporting rod is in sleeved connection with a second supporting rod, the upper end of the outer surface of the first supporting rod is provided with an adjustment mechanism,the second supporting rod is fixed in the first supporting rod through the adjustment mechanism, the upper end of the second supporting rod is provided with a boss, and hooks are evenly distributed onthe outer surface of the boss. The paediatric clinical integrated type monitoring and rescue device has the advantages that functions are diverse, the pain of a patient is reduced, comprehensive monitoring and rescue facilities are provided for paediatric patients, and the device is used by a medical worker conveniently.
Owner:赵洁
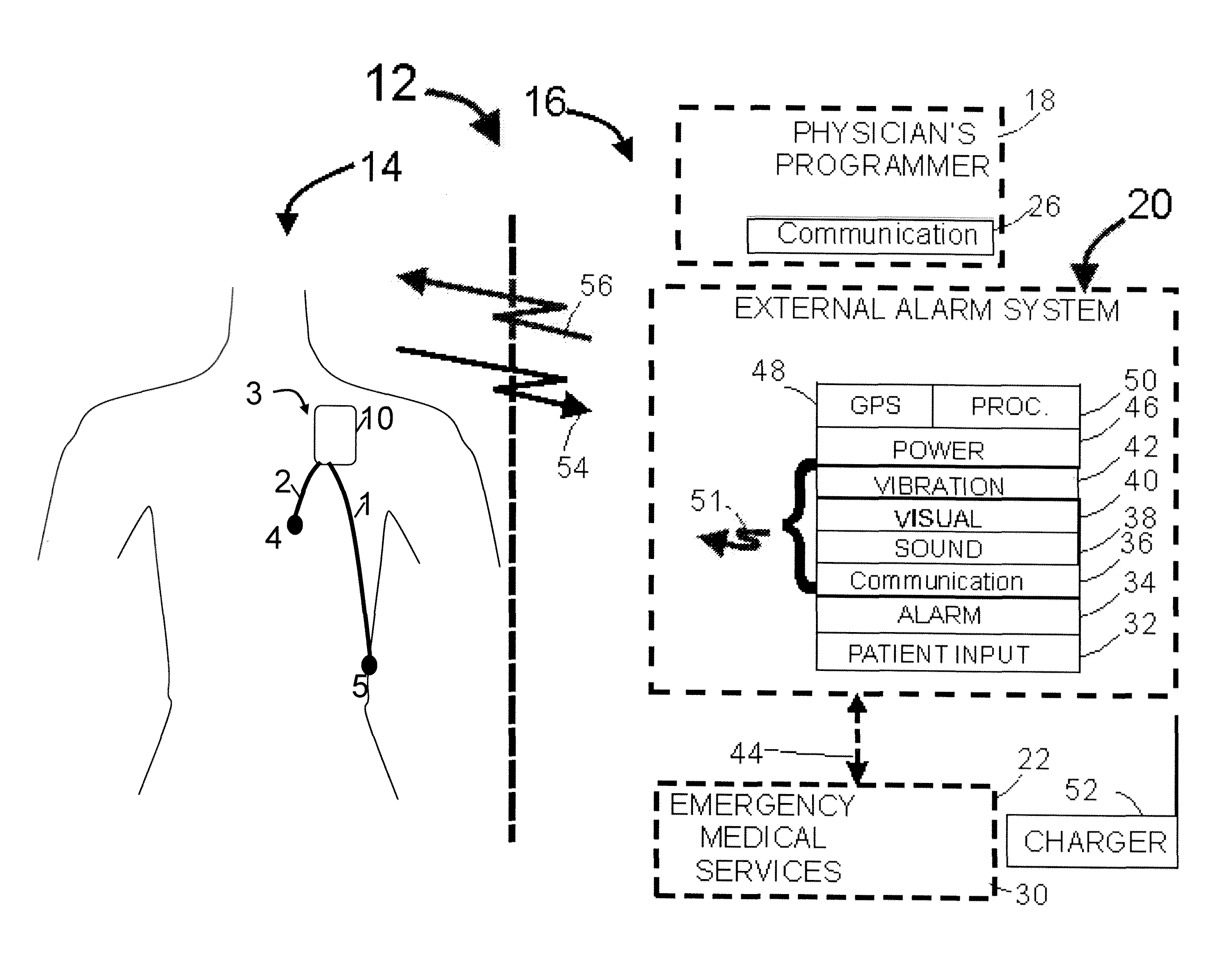
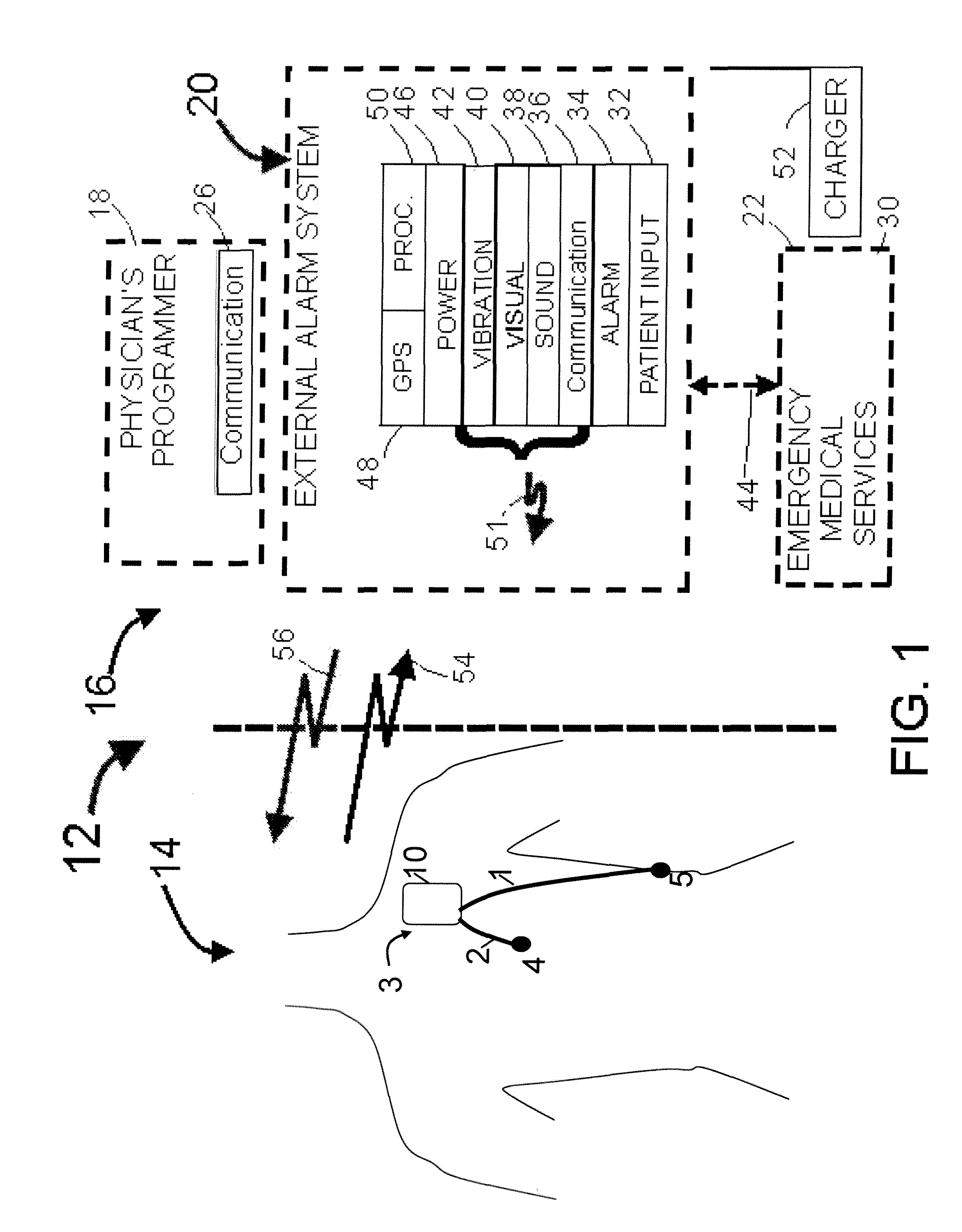
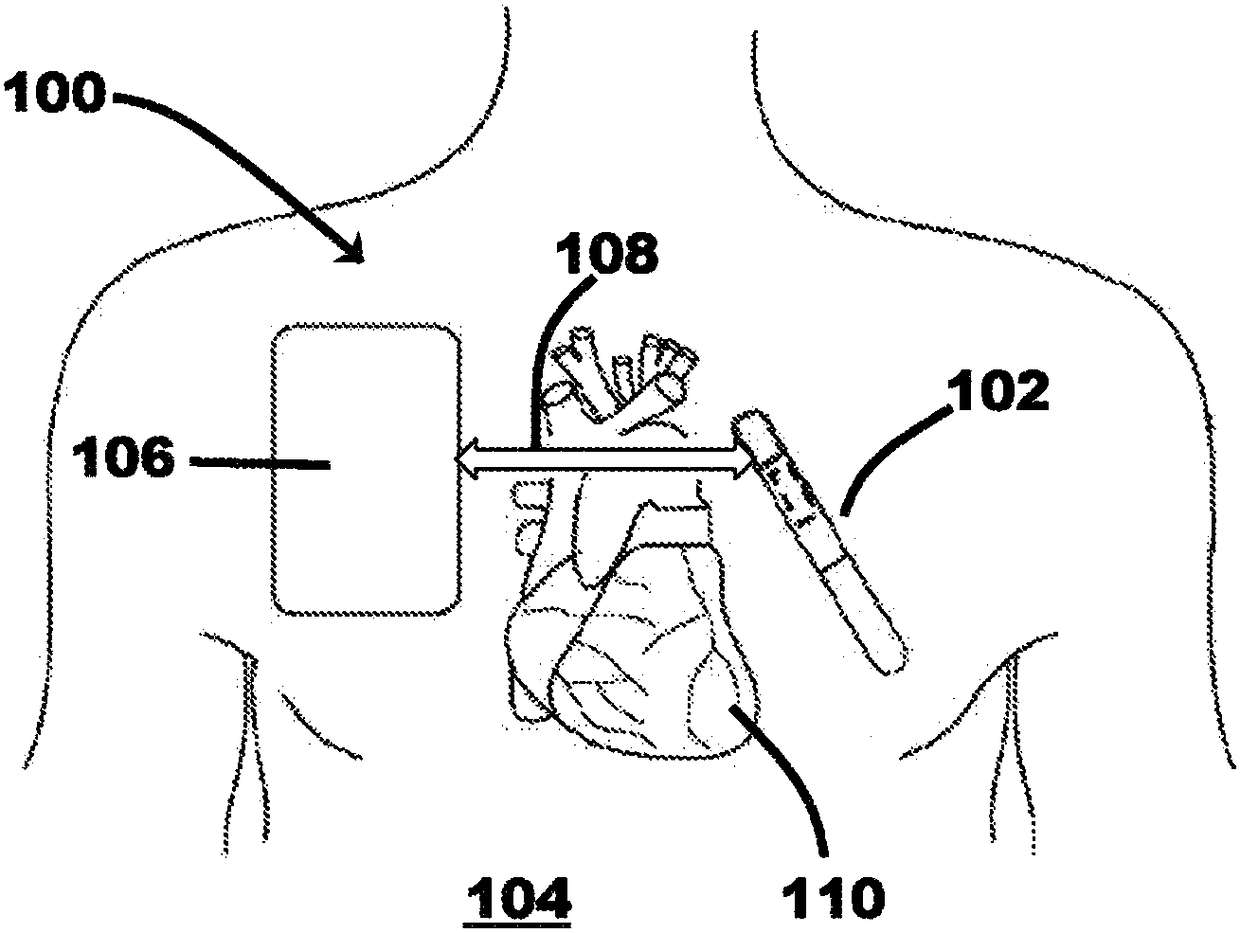
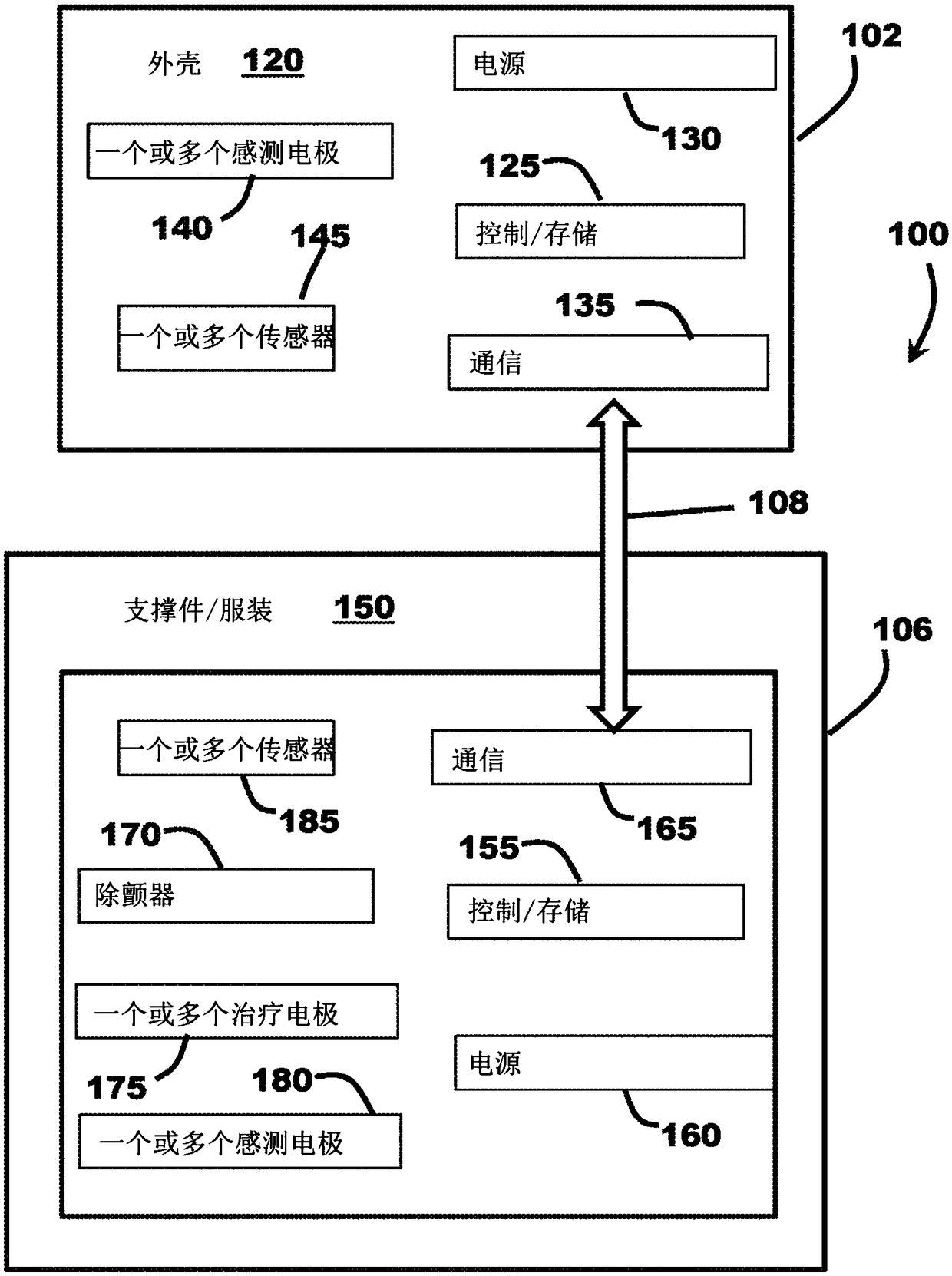
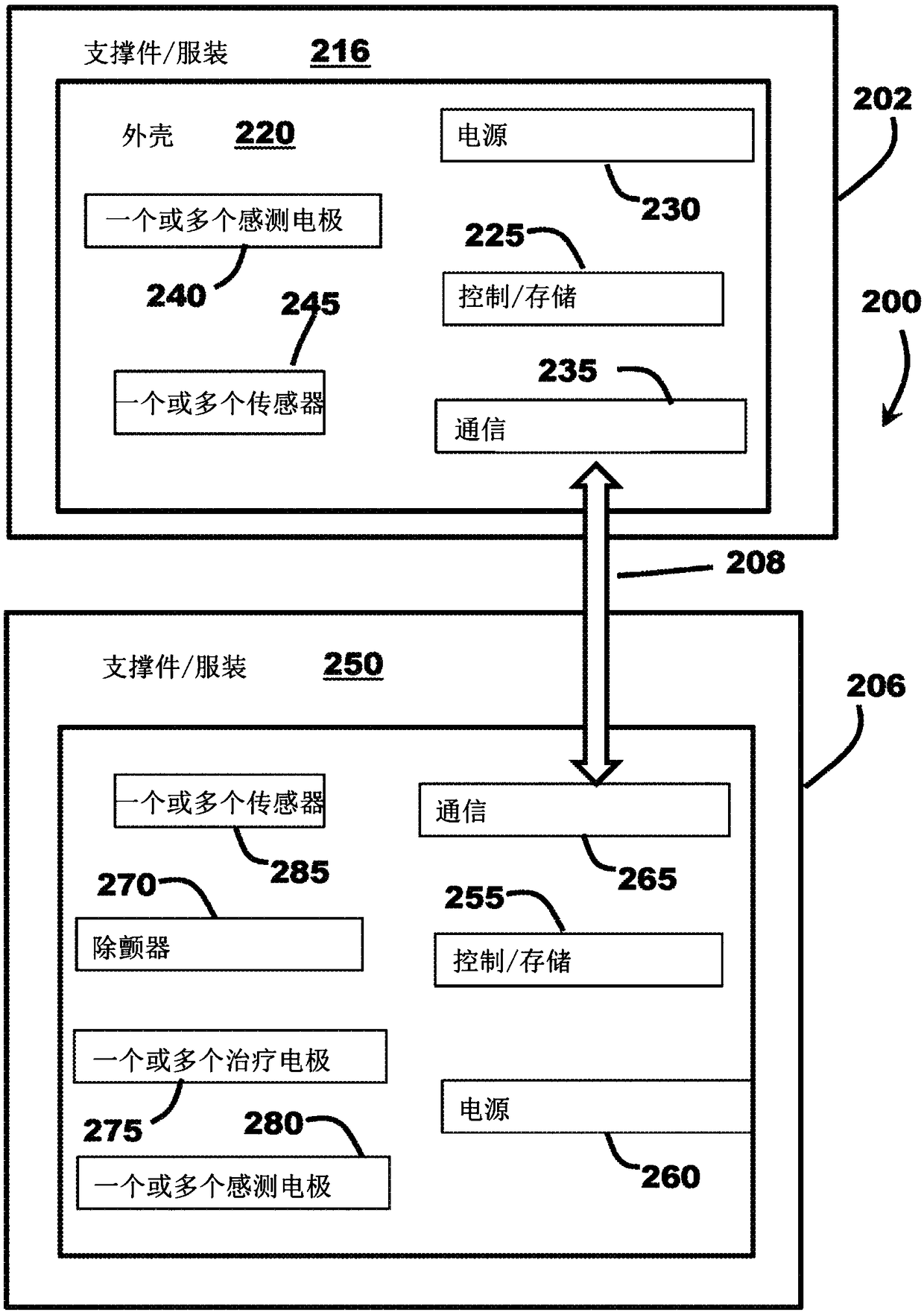
Enhanced wearable therapy device paired with insertable cardiac monitor
A medical system for providing a defibrillation therapy to a patient includes a cardiac monitoring device (CMD) configured to sense and record physiological data indicative of the patient's cardiac function. The CMD includes a communication component. The system also includes an external therapy device configured to deliver defibrillation therapy, and configured to be positioned external to and supported by the patient. The external therapy device includes an external therapy device communication component. The CMD communication component and the external therapy device communication componentare configured to operatively couple the CMD and the external therapy device to one another, so as to work as a system to detect and treat fibrillation.
Owner:CARDIAC PACEMAKERS INC
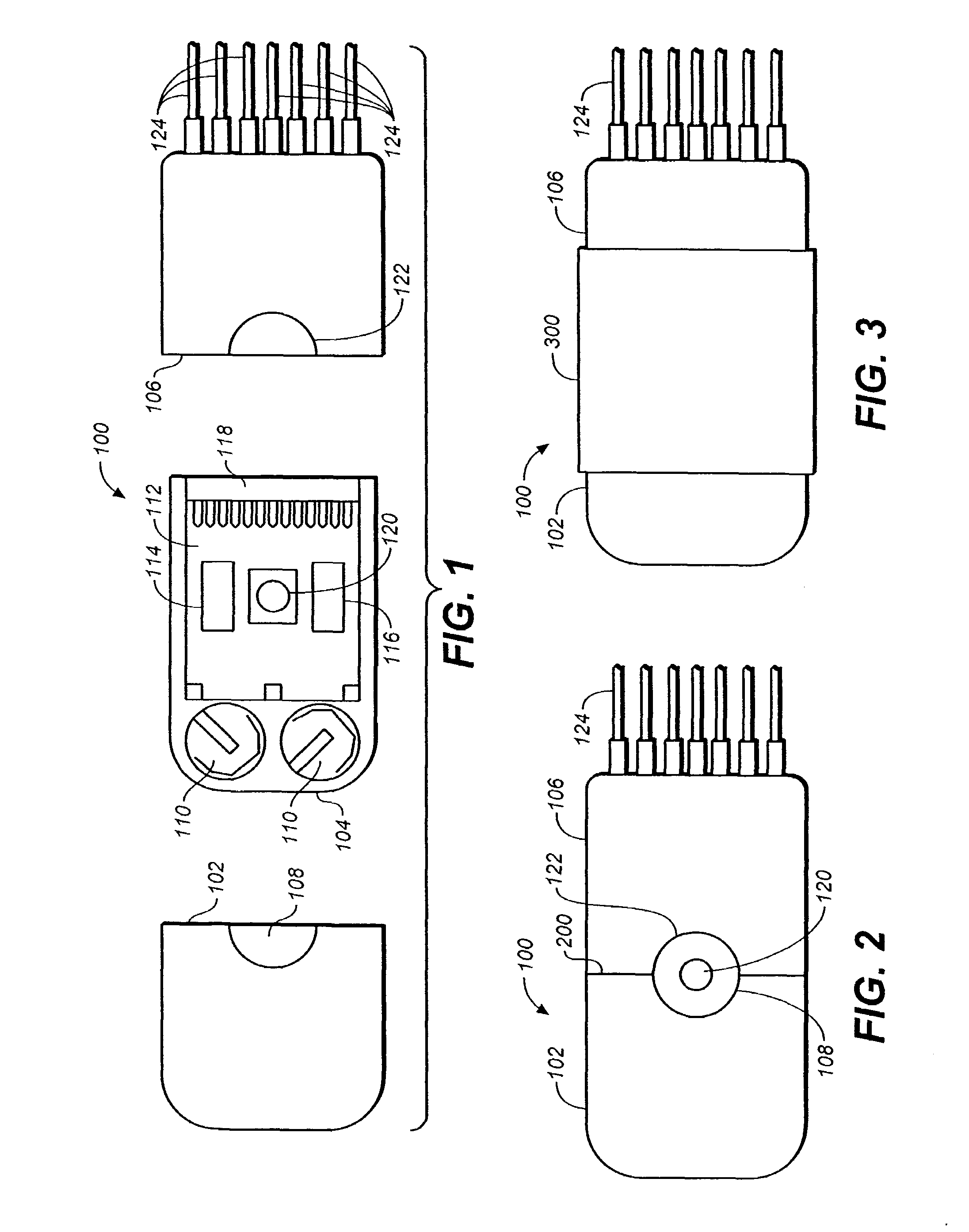
Systems and methods for interelectrode distance optimization in a retractable multi-use cardiac monitor
ActiveUS20150150471A1Easy and function-enhancing adjustmentElectrocardiographySensorsComputer hardwareEcg signal
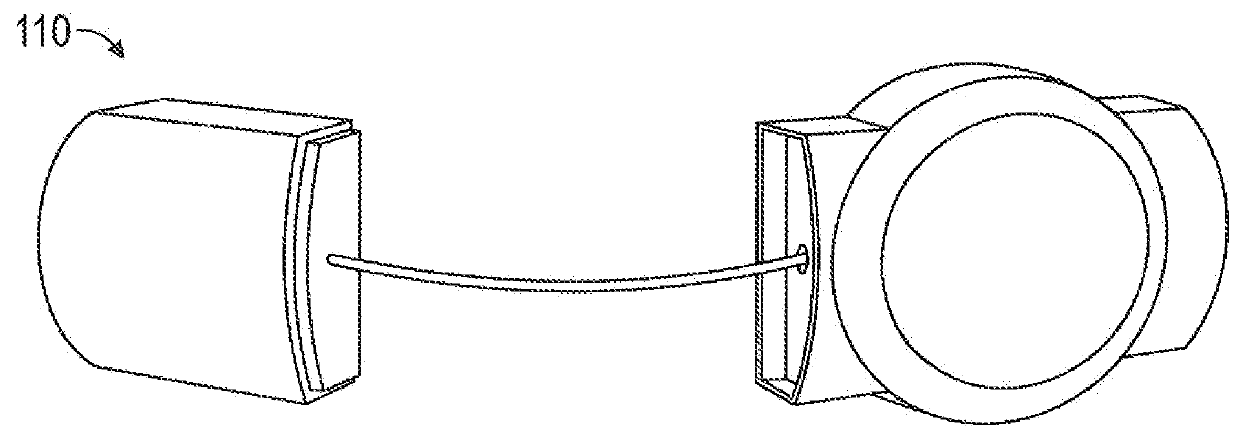
A retractable multi-use cardiac monitor is provided that includes a memory, and first and second sensing connectors positioned on outsides of first and second housings, respectively. The first and second sensing connectors are configured to detect electrocardiogram (ECG) signals that are stored onto the memory as ECG data. The second housing of the retractable multi-use cardiac monitor also includes a wire retractor configured to extend and retract a wire that connects the second and first housings, and that defines an interelectrode distance between the first and second sensing connectors. The retractable multi-use cardiac monitor further includes systems and methods for determining a length for the interelectrode distance that is optimum in terms of strength and fidelity of the detected ECG signals. The retractable multi-use cardiac monitor further includes a wireless radio configured to transmit a portion of the stored ECG data from the memory to a destination.
Owner:MEDICOMP
Cardiac output control apparatus and method of use thereof
The invention comprises an apparatus and a method for operating a cardiac assist pump, comprising the steps of: (1) providing a cardiac monitor comprising: a cardiac output sensor including an activity sensor and at least two of: a pulse oximeter; an electrocardiogram meter; and a blood pressure monitor; (2) receiving time-varying cardiovascular input data, from the cardiac output sensor, related to a transient hemodynamic state of a cardiovascular system; (3) receiving and operating on time-varying activity input data, from the activity sensor, to generate cardiovascular state information; (4) sensing activity with the activity sensor to generate a target cardiovascular state; (5) repeating both the steps of receiving and operating to update the transient cardiovascular state information and the step of sensing to update the target cardiovascular state; and (6) directing the cardiac assist pump to adjust assisted blood flow, yielding the updated transient cardiovascular state, toward the target cardiovascular state.
Owner:REICH ALTON +1
Portable cardiac monitor including pulsed power operation
InactiveUS20060229525A1Easy to identifyElectrocardiographyAmplifier with semiconductor-devices/discharge-tubesEcg signalEngineering
A system and method for obtaining ECG signals from an ambulatory patient are disclosed herein. The system is configured to be inexpensive, small, and robust for outpatient monitoring. The system is configured to be a low power consuming device. The system provides options for a variety of settings and real-time access to the ECG signals being recorded during the recording period.
Owner:EXELYS
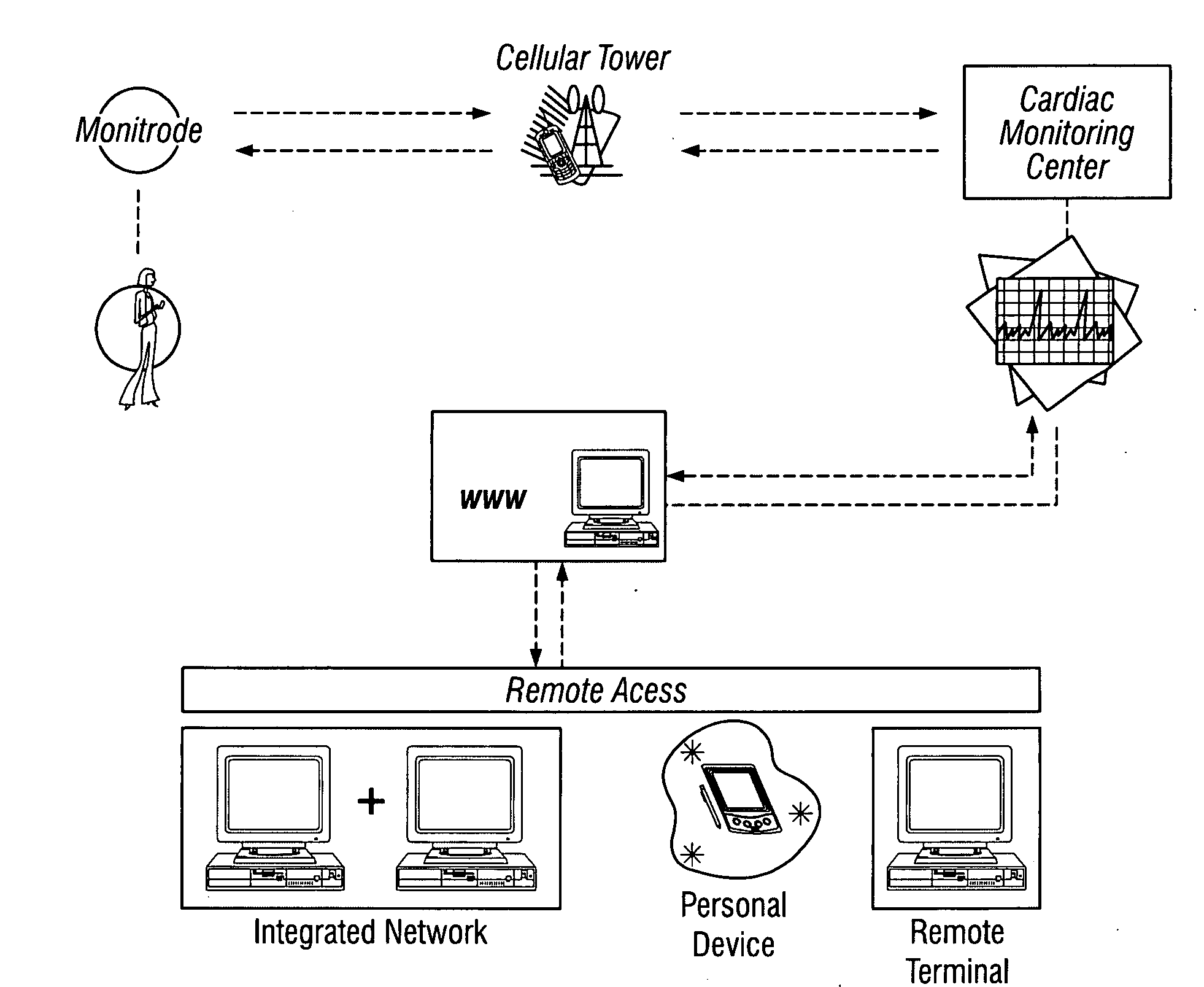
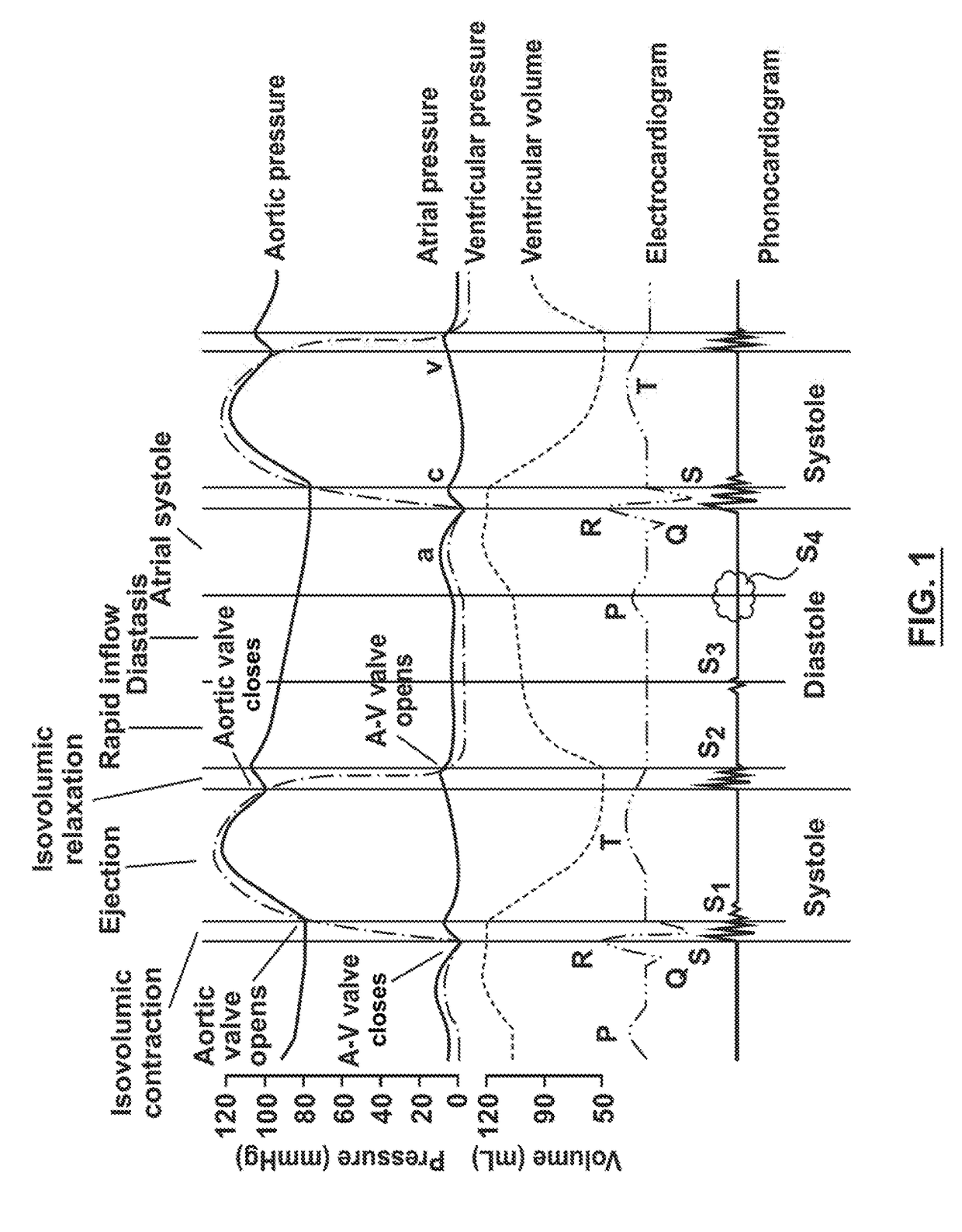
Cardiac monitor system and method for home and telemedicine application
A system for detecting valvular malfunction includes a monitoring device and a processor. The monitoring device includes a heart sound sensor configured to detect heart sounds of the patient, and a signal processor. The processor is configured to receive a signal representative of the detected heart sounds from the signal processor, wherein the processor is configured to compare the signal to a baseline signal stored in memory. The processor may be part of the monitoring device or may be part of an external device, or both.
Owner:MEDTRONIC VASCULAR INC
Cardiac monitor system and method for home and telemedicine application
A system for detecting valvular malfunction includes a monitoring device and a processor. The monitoring device includes a heart sound sensor configured to detect heart sounds of the patient, and a signal processor. The processor is configured to receive a signal representative of the detected heart sounds from the signal processor, wherein the processor is configured to compare the signal to a baseline signal stored in memory. The processor may be part of the monitoring device or may be part of an external device, or both.
Owner:MEDTRONIC VASCULAR INC
Pediatric integrated monitoring and rescue device
InactiveCN109464245ARelieve painSleep aidNursing bedsAmbulance serviceIntegrated monitoringEngineering
The invention relates to the field of pediatric monitoring and rescue equipment, in particular to a pediatric integrated monitoring and rescue device. The device comprises a bottom plate, support columns are symmetrically arranged at four corners of the lower end of the bottom plate, rollers are installed at the bottom ends of the support columns, accommodating plates are fixedly installed at themiddles of the four support columns, the front of the left end of the bottom plate is provided with a heart monitor, a breathing device is arranged on the right side of the front end of the bottom plate, a hanger is fixedly mounted on the front end of the bottom of the bottom plate, a bed is fixedly connected to the top end of the bottom plate, a monitoring device is fixedly mounted on the front end of the left side of the top of the bed, curved sliding grooves are symmetrically formed in the left and right sides of the bed, the top of the bottom plate is connected with a shaking bed body on the inner side of the bed, shaking bed heads are fixedly connected to the left and right sides of the shaking bed body, the outsides of the shaking bed heads are fixedly connected with rolling shafts,the outside end of a buffer shaft is fixedly connected with a rolling bracket, and the rolling bracket is connected to a buffer roller through a rotating shaft. The invention provides the monitoring and rescue device capable of assisting infants to sleep and having an anti-collision buffer function.
Owner:李玉超
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com