Patents
Literature
Hiro is an intelligent assistant for R&D personnel, combined with Patent DNA, to facilitate innovative research.
379 results about "Light therapy" patented technology
Efficacy Topic
Property
Owner
Technical Advancement
Application Domain
Technology Topic
Technology Field Word
Patent Country/Region
Patent Type
Patent Status
Application Year
Inventor
Light therapy—or phototherapy, classically referred to as heliotherapy—consists of exposure to daylight or to specific wavelengths of light using polychromatic polarised light, lasers, light-emitting diodes, fluorescent lamps, dichroic lamps or very bright, full-spectrum light. The light is administered for a prescribed amount of time and, in some cases, at a specific time of day.
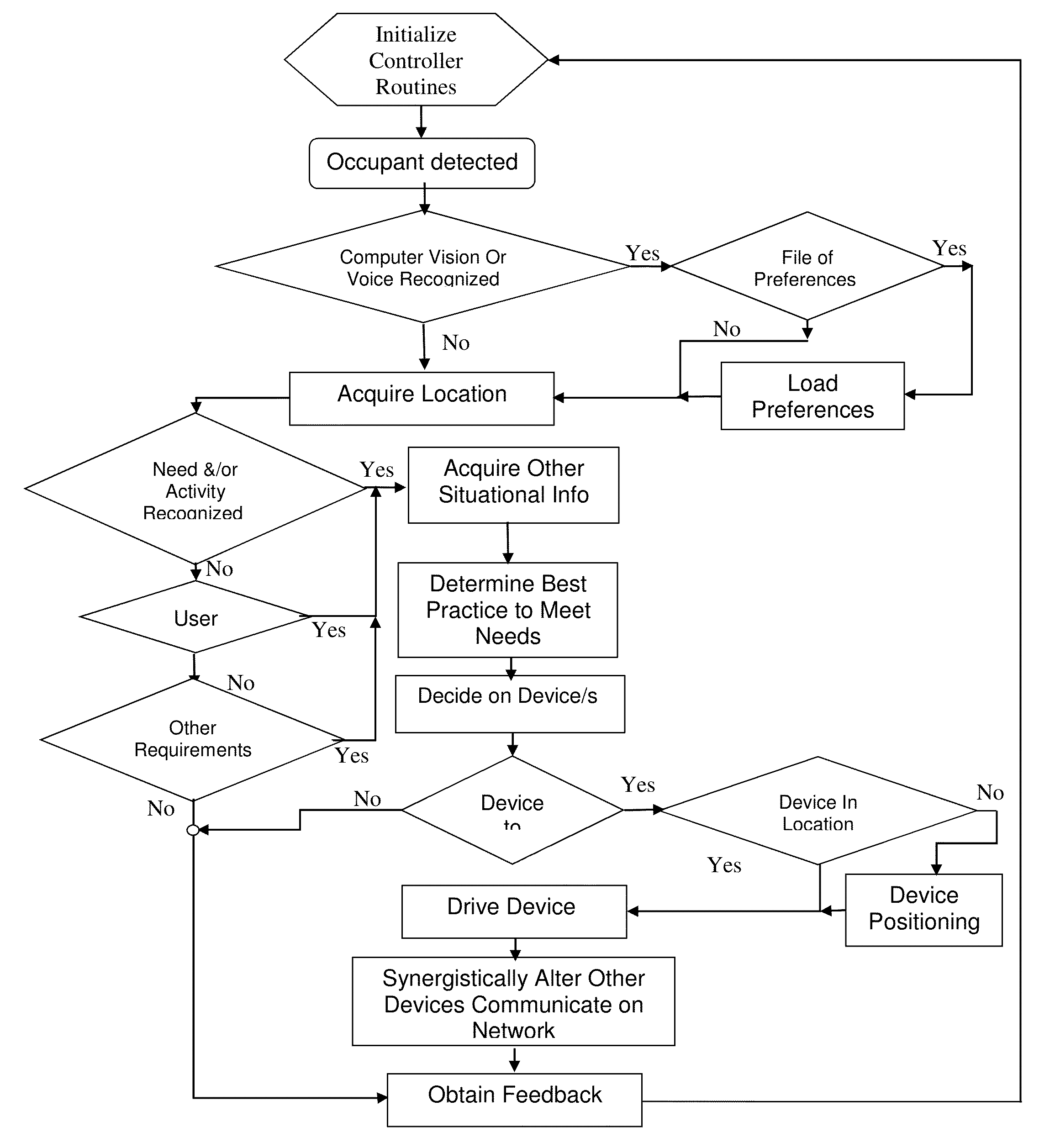
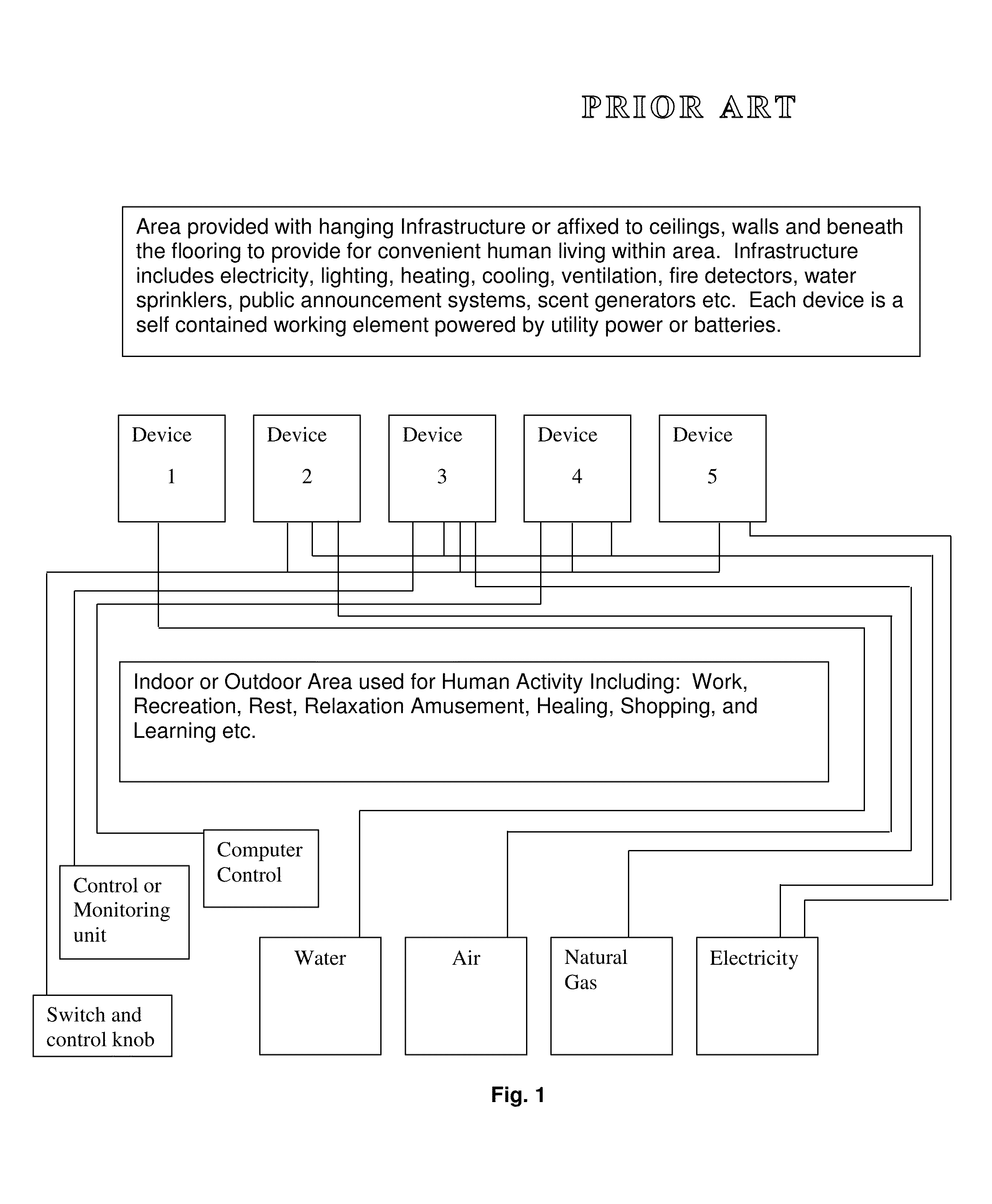
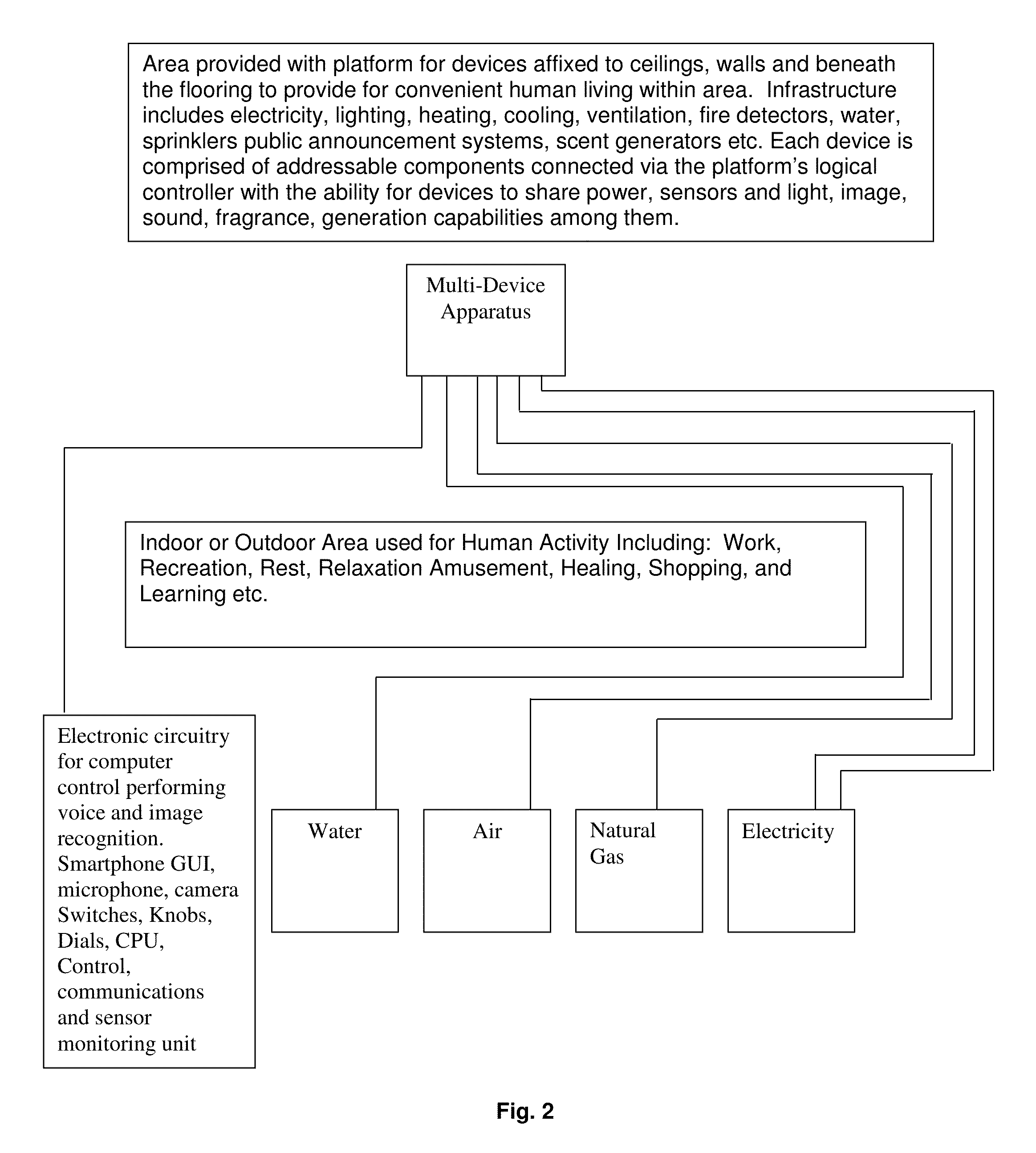
Integrated Docking System for Intelligent Devices
An integrating device 200 for supporting one or more devices 207 capable of delivering mass, energy and / or information to occupants localized to a sub-area of a room is combined with sensors 212 capable of detecting occupants within one sub-area or another and processor 206 which correlates the coordinates of the occupants to those of the delivery devices 207 and a controller 206 that drives the specific sub-area device to provide a localized delivery of services such as lighting, heating, cooling, sound and video, intercom, noise cancellation systems, information, entertainment content, connectivity to the internet or social media, and light therapy in an automatic process based on the detected instantaneous needs of the occupant for services.
Owner:SPERO YECHEZKAL EVAN
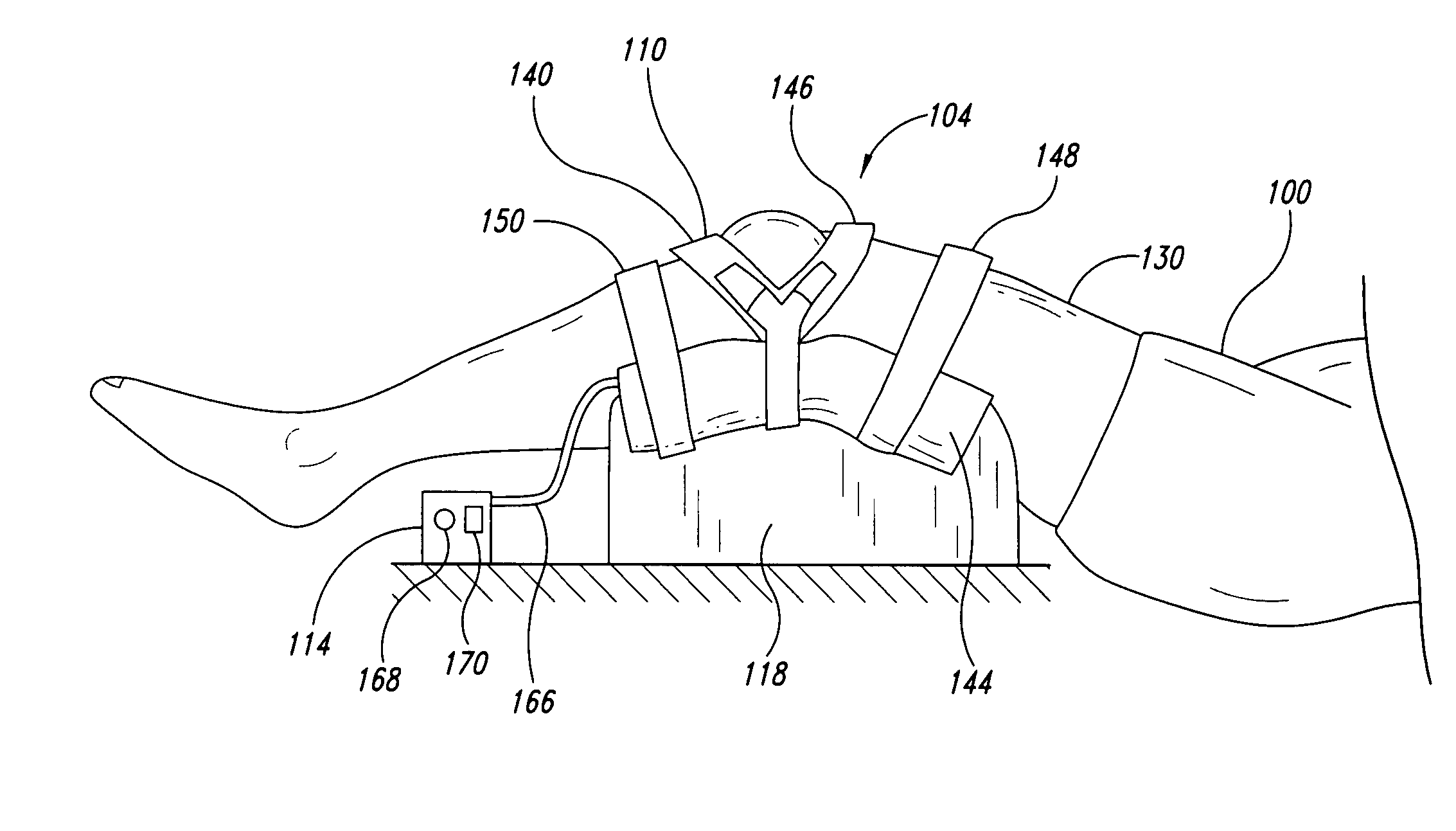
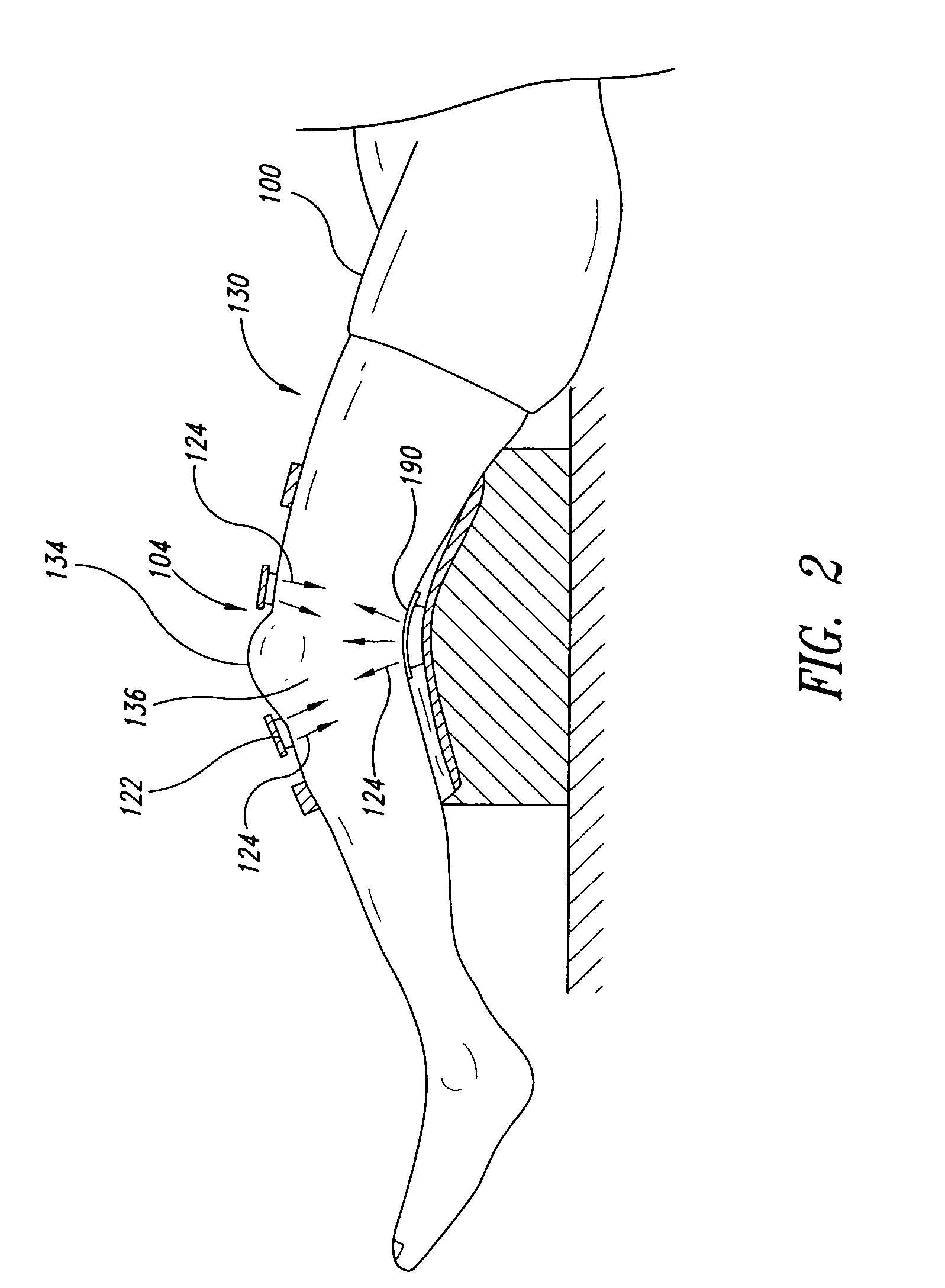
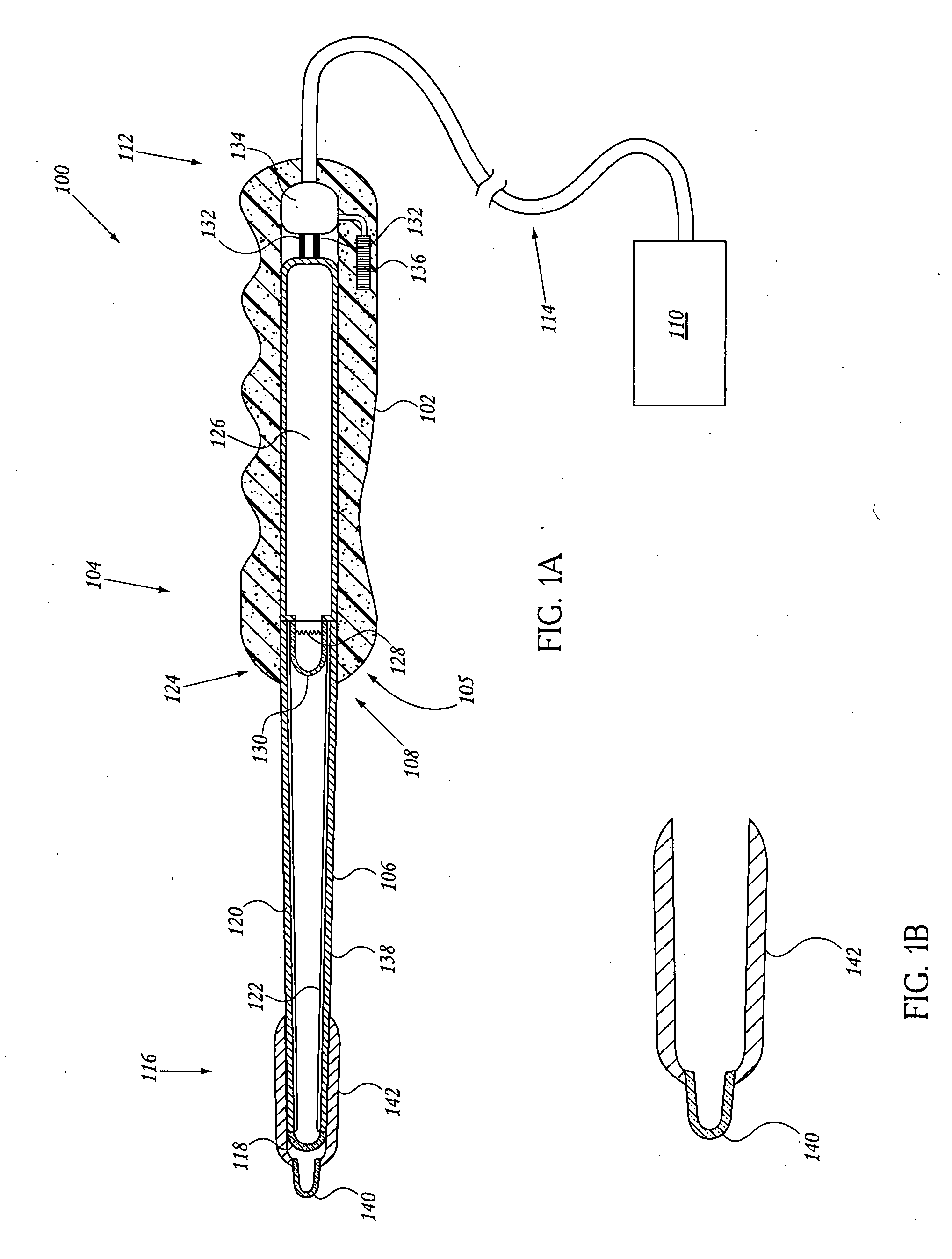
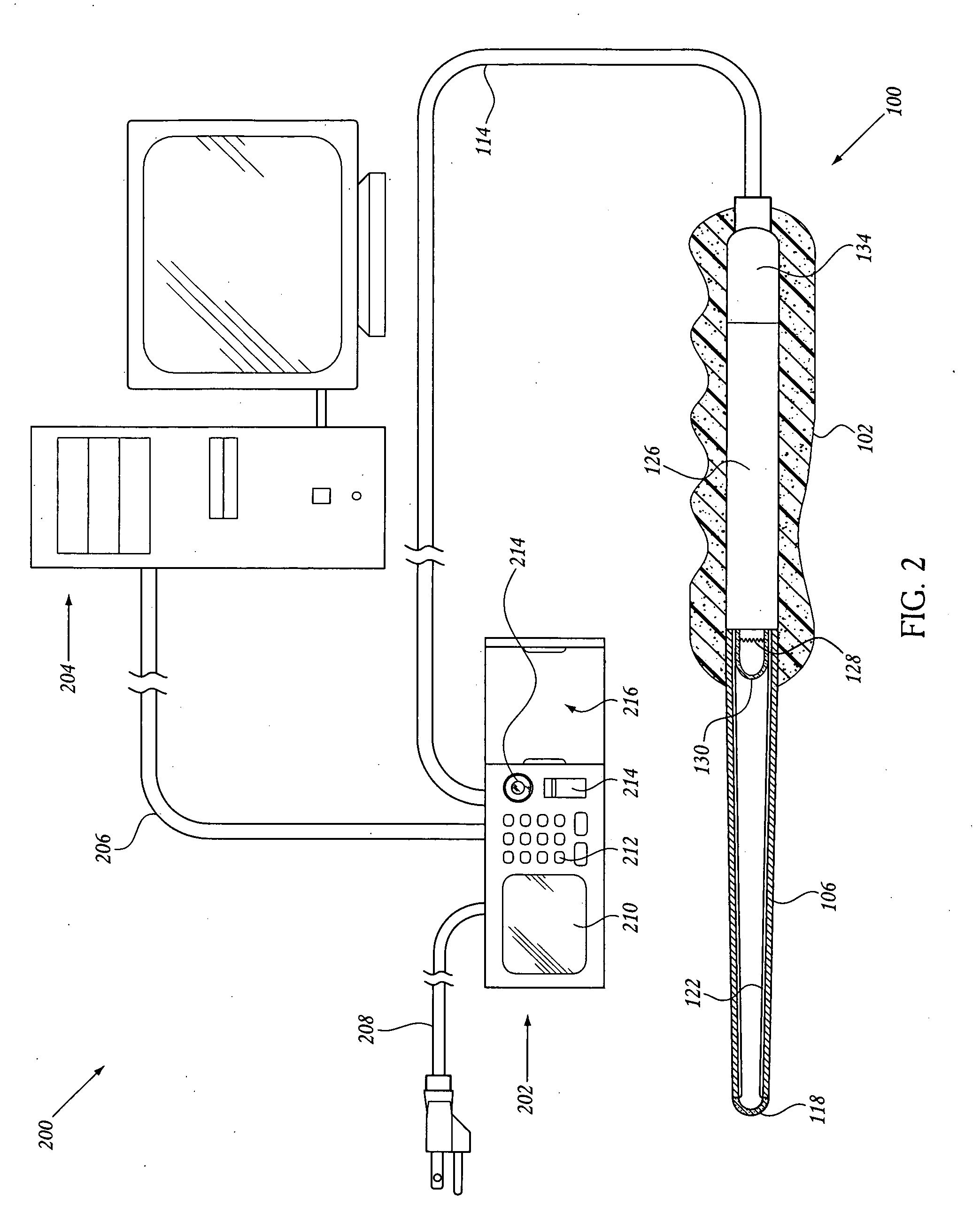
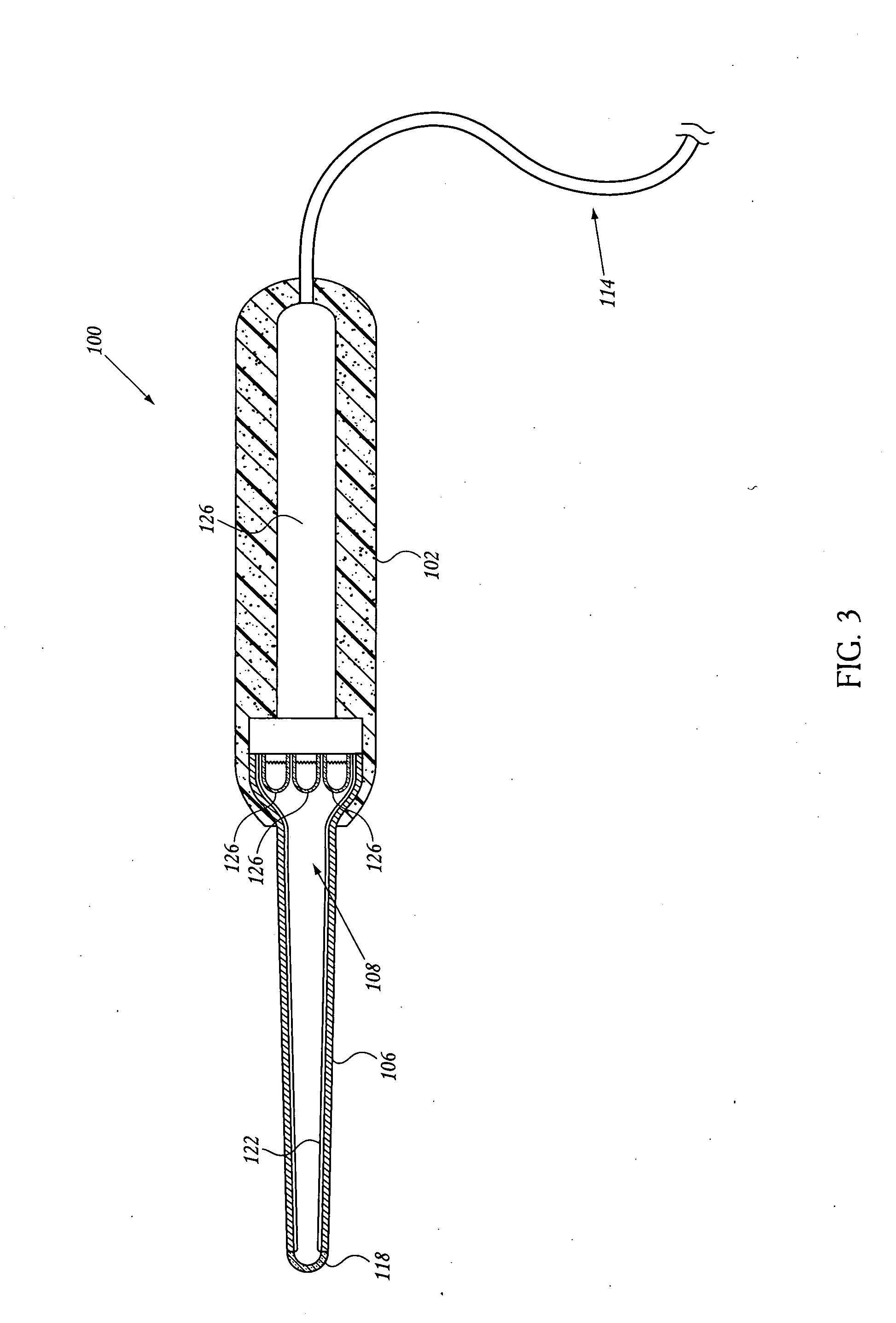
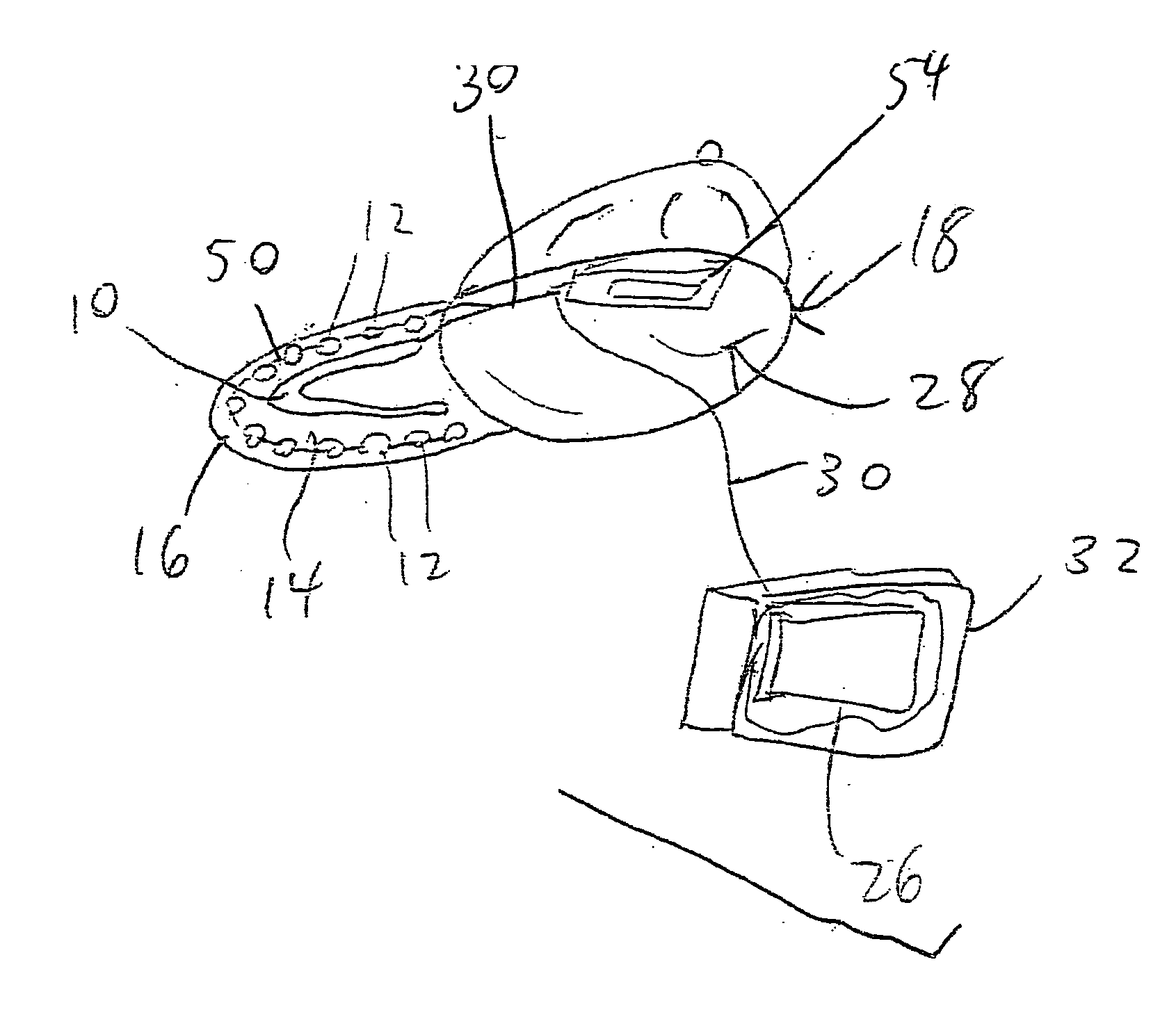
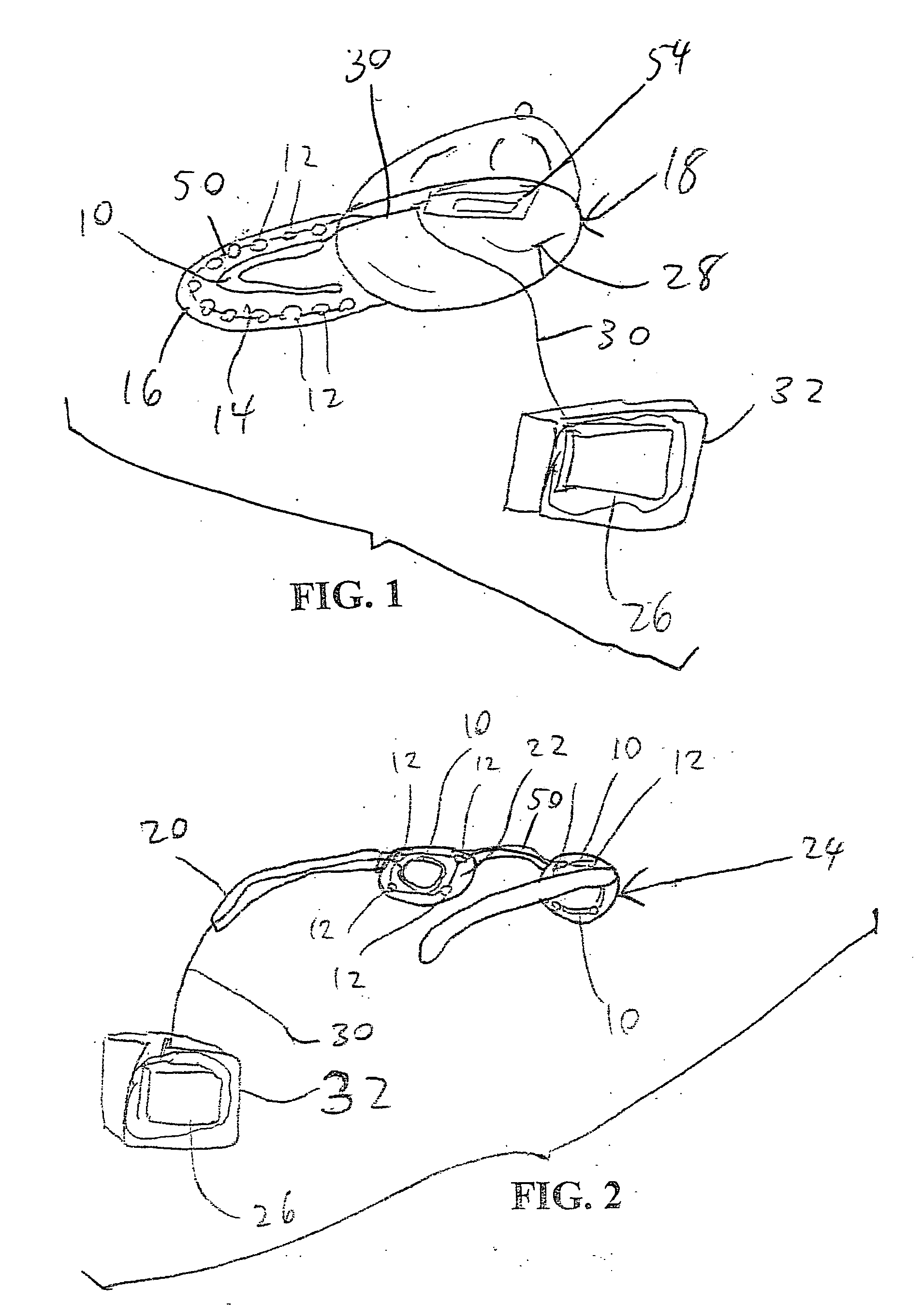
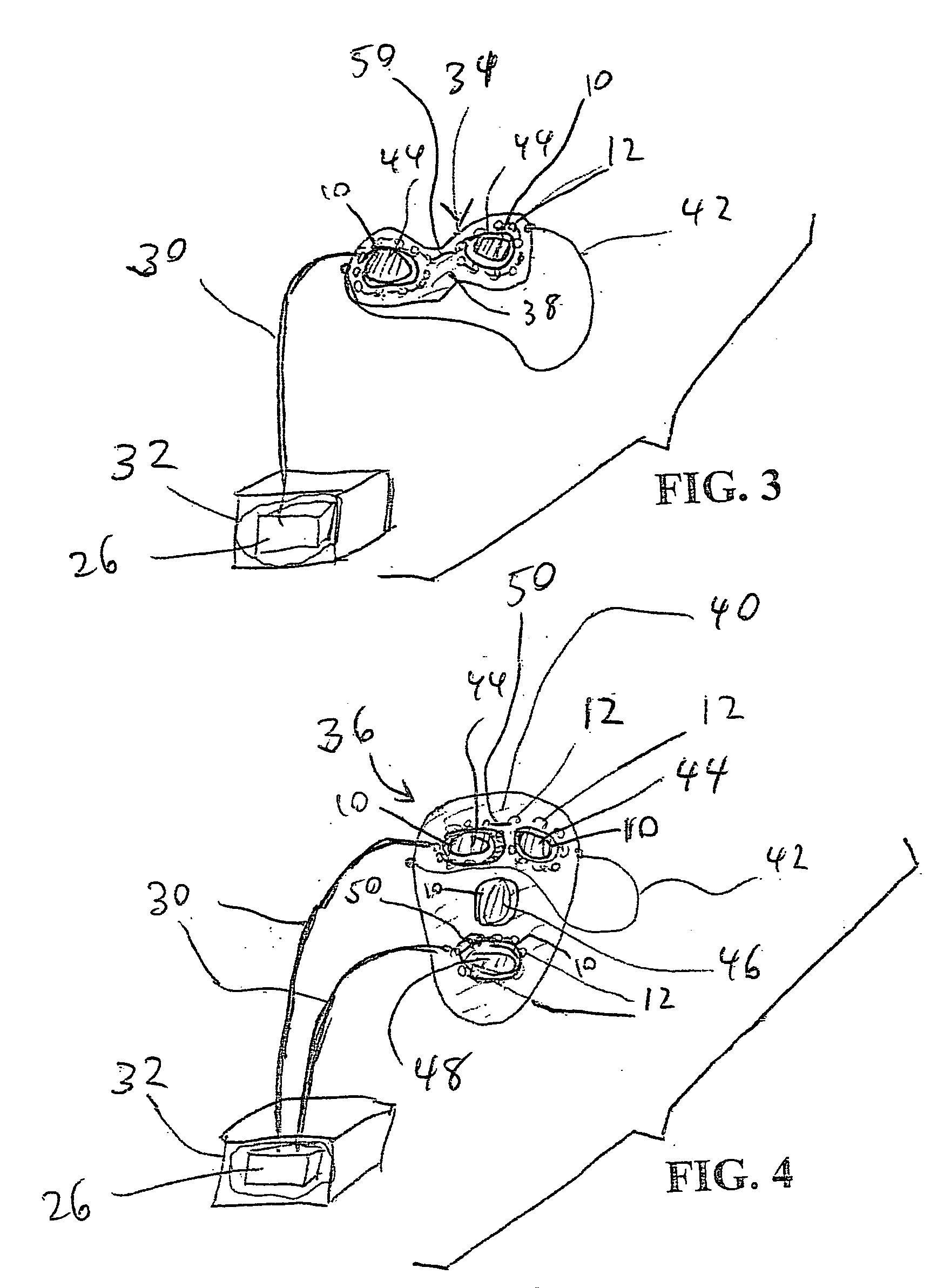
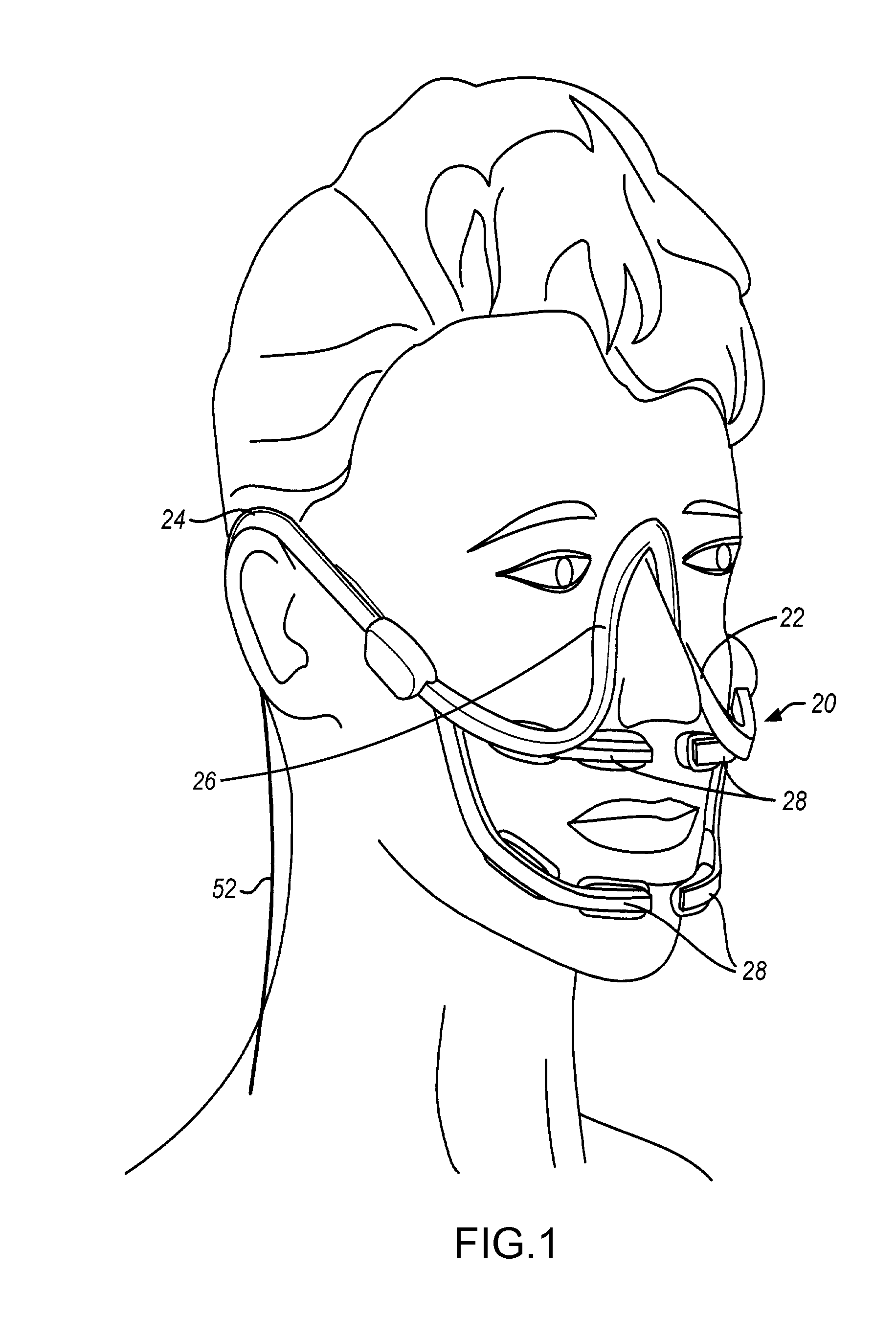
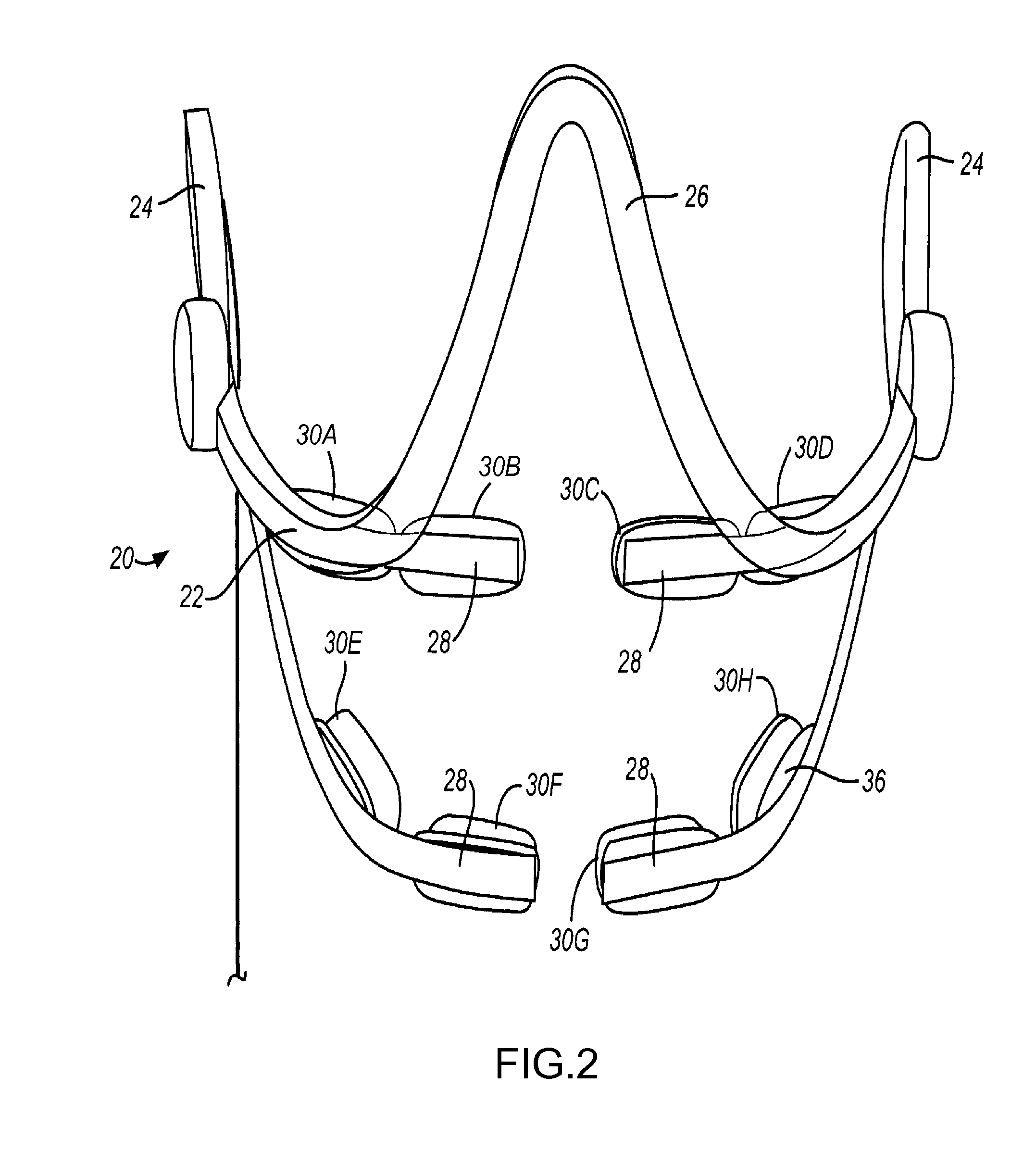
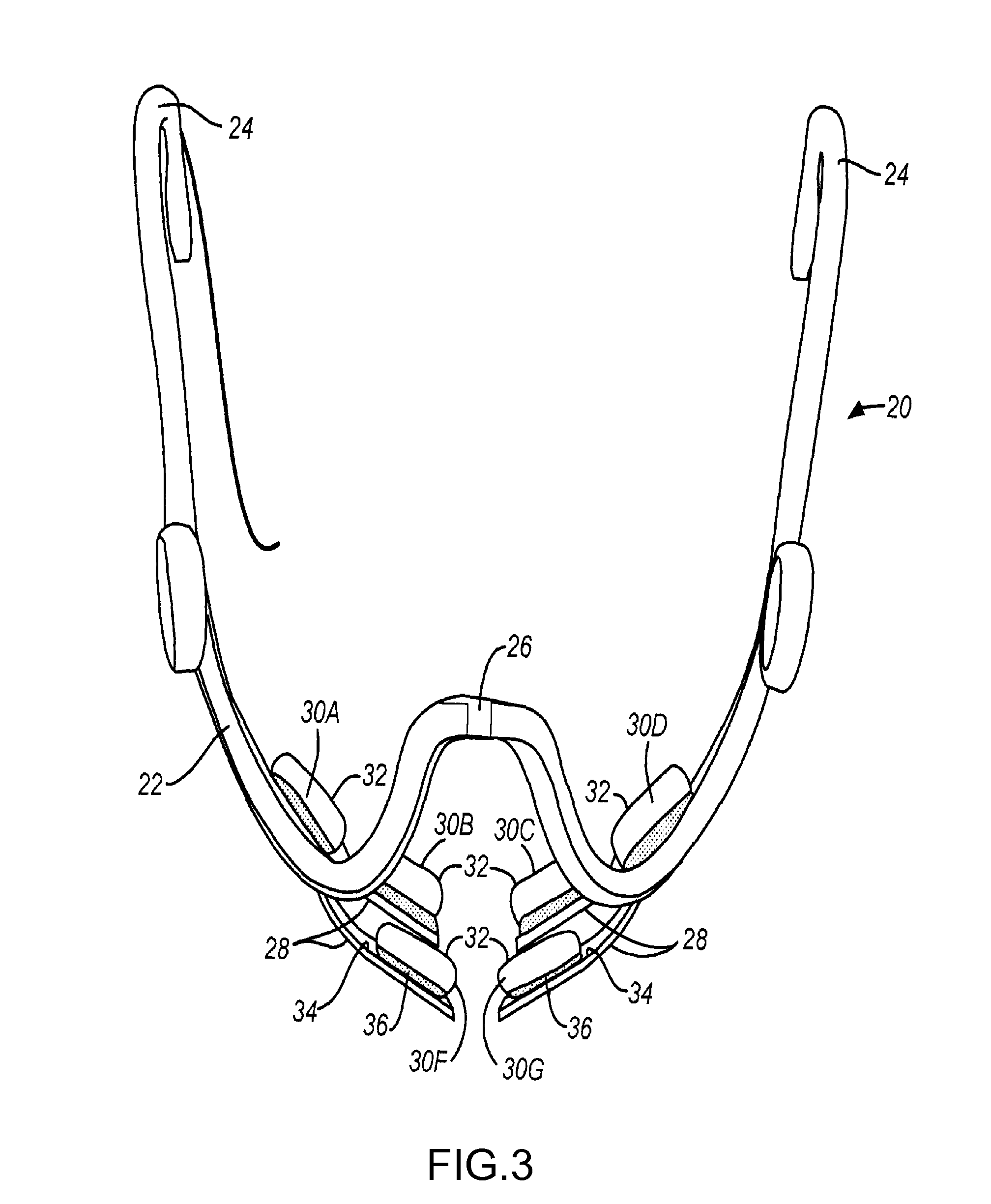
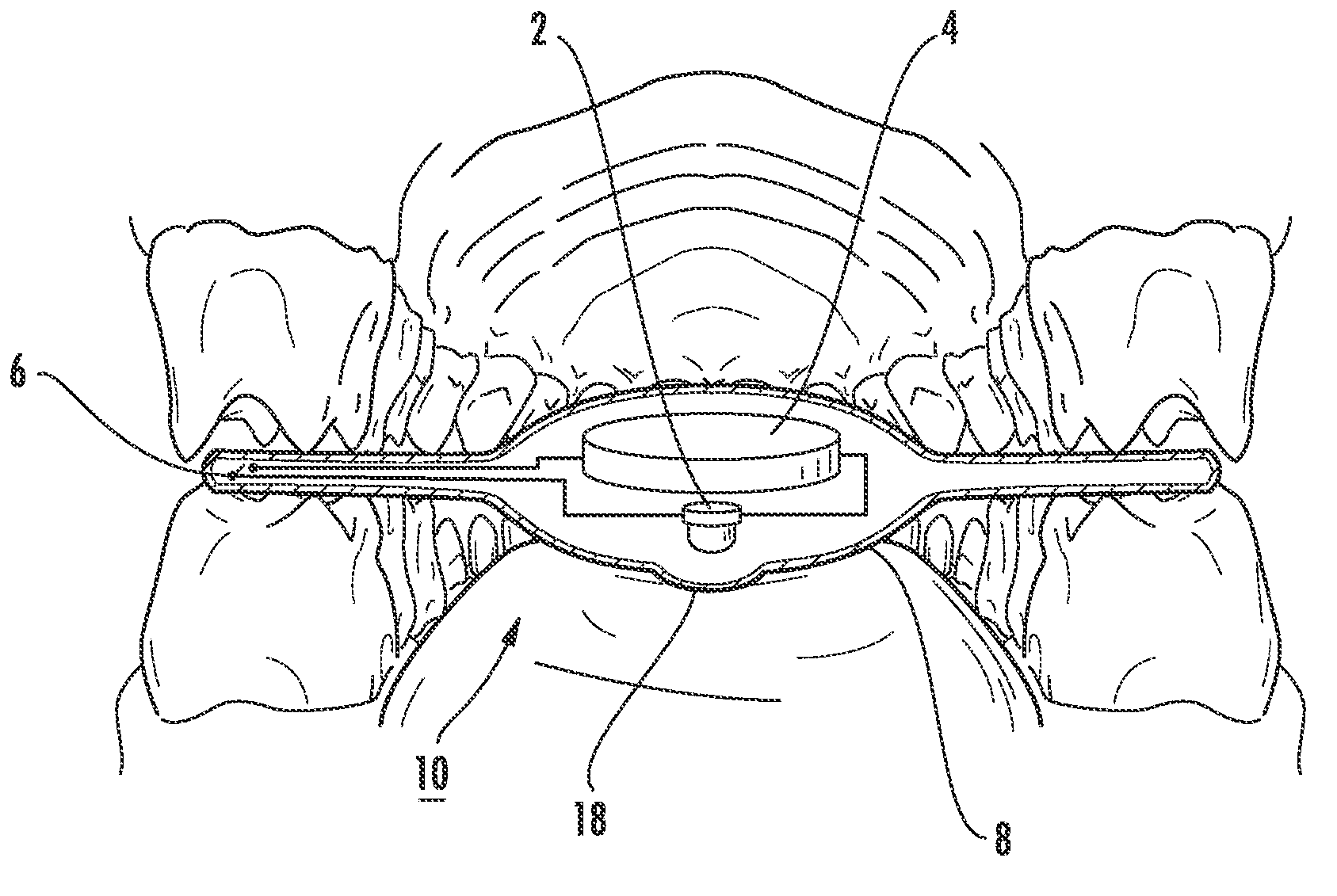
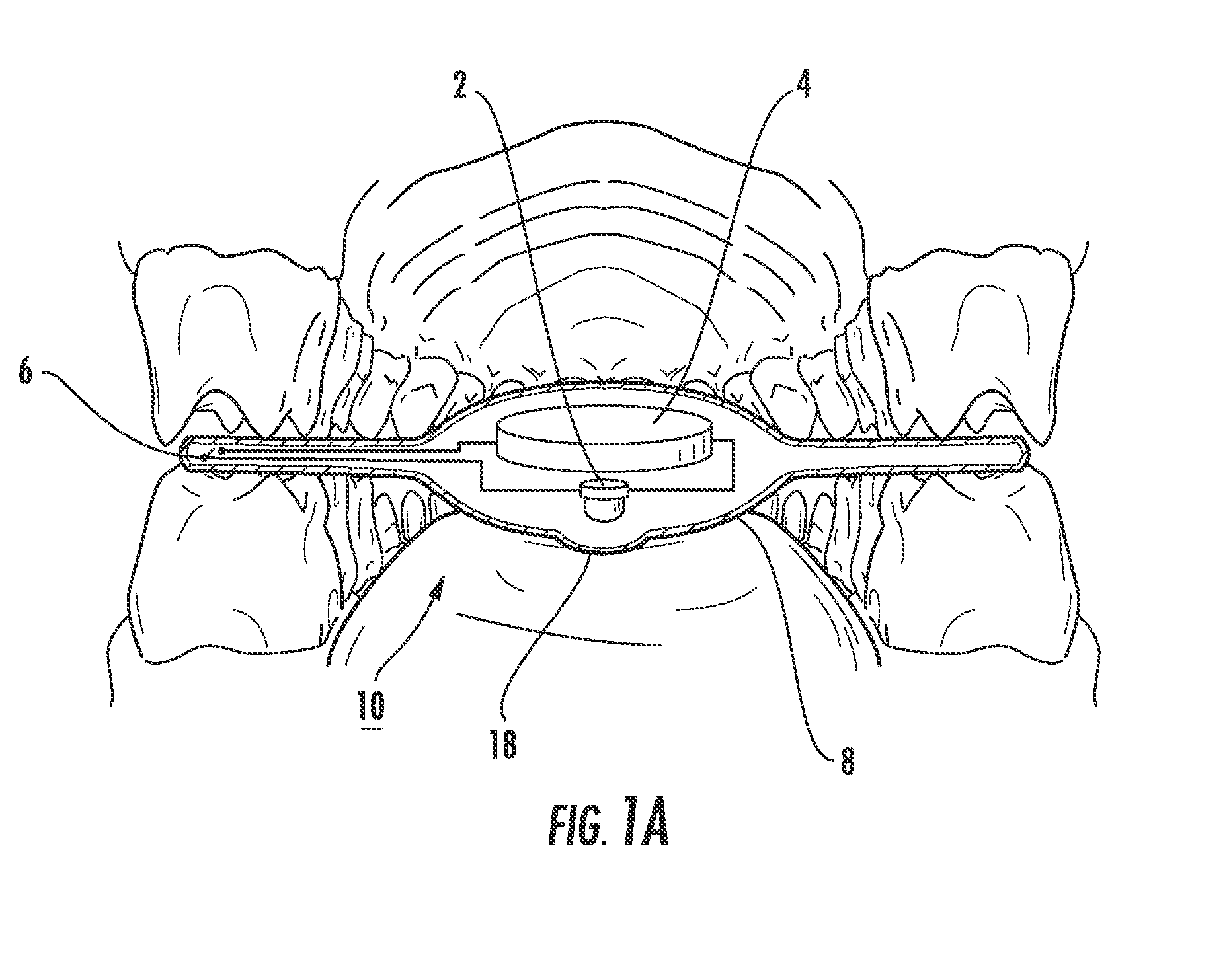
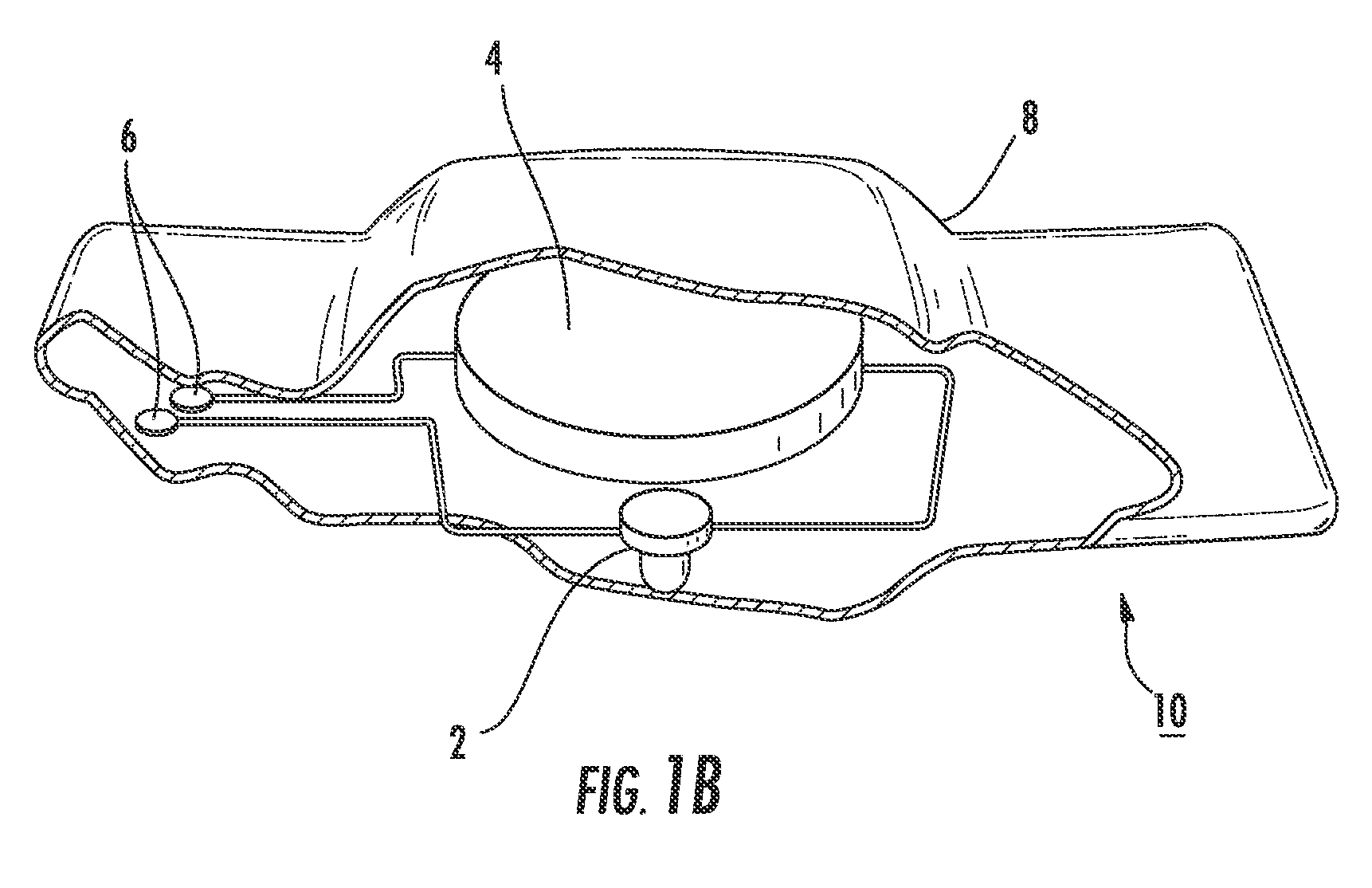
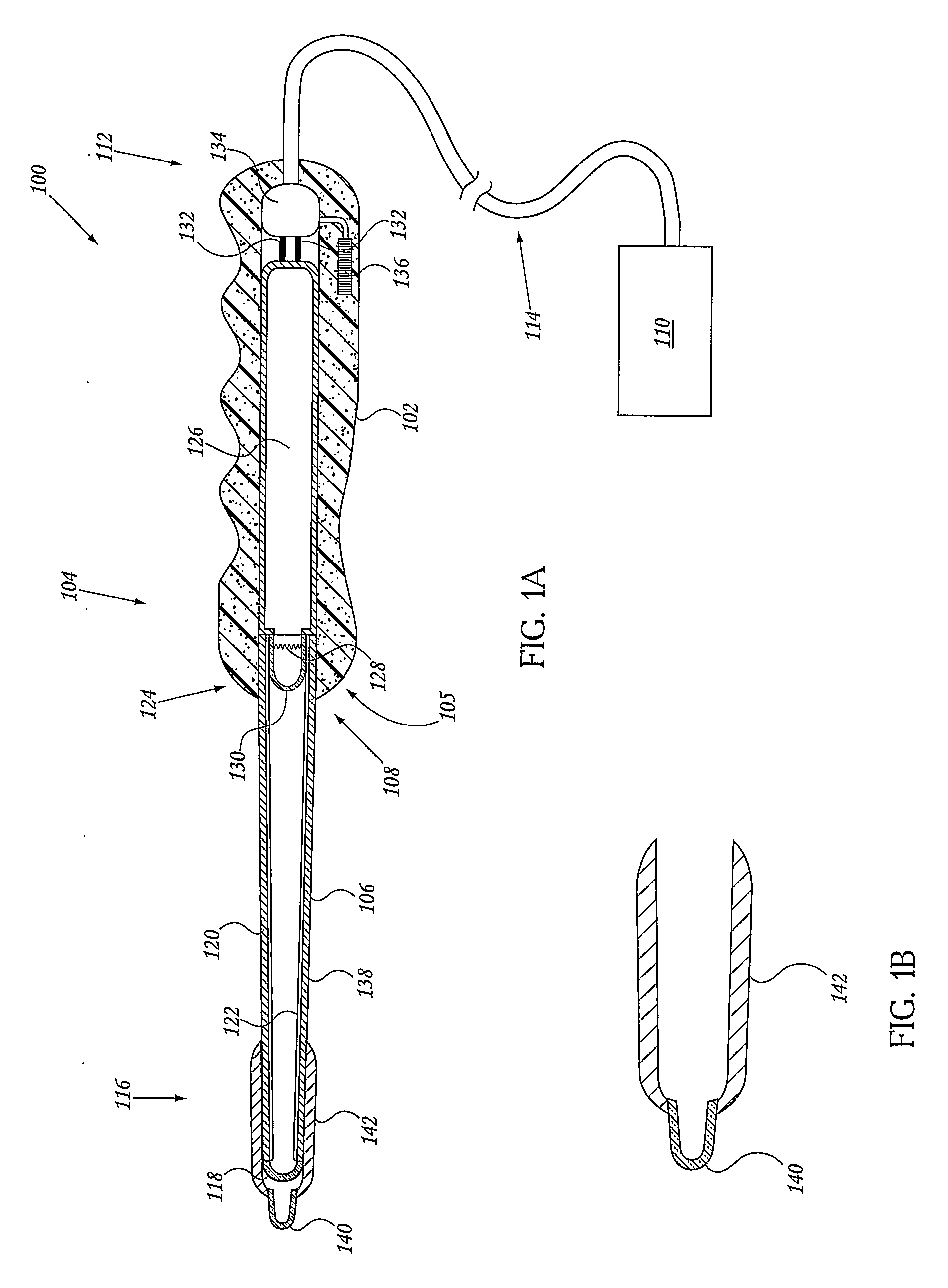
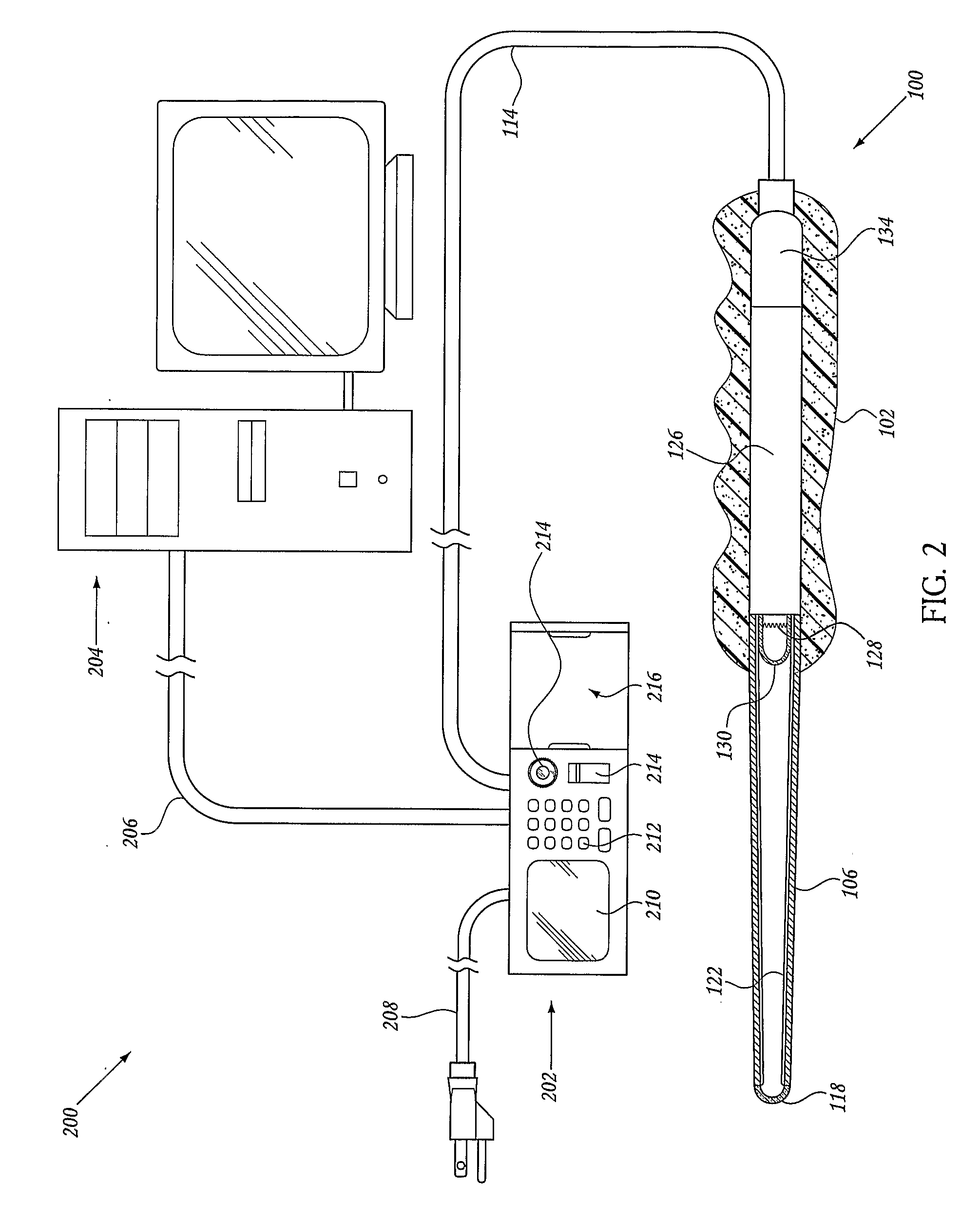
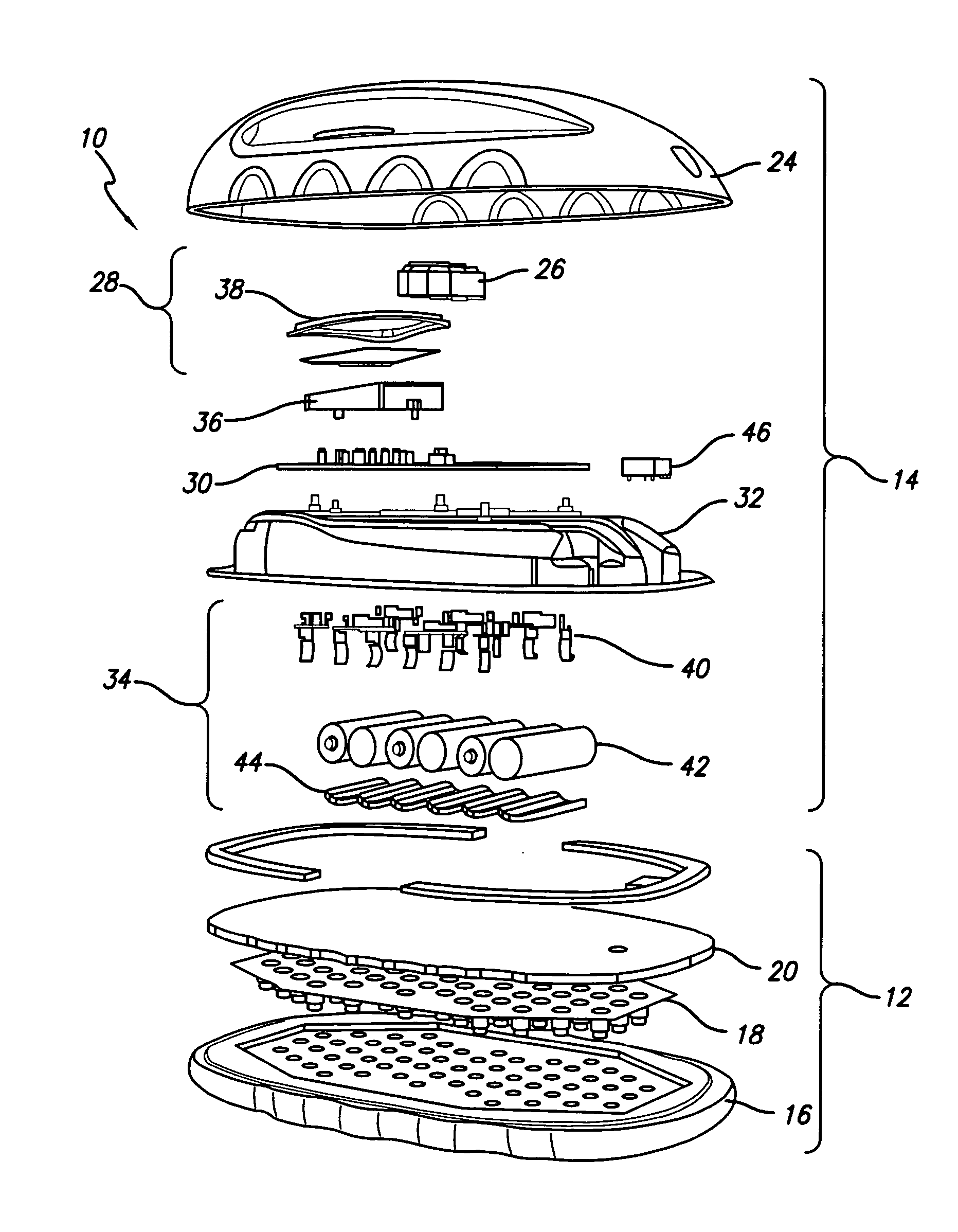
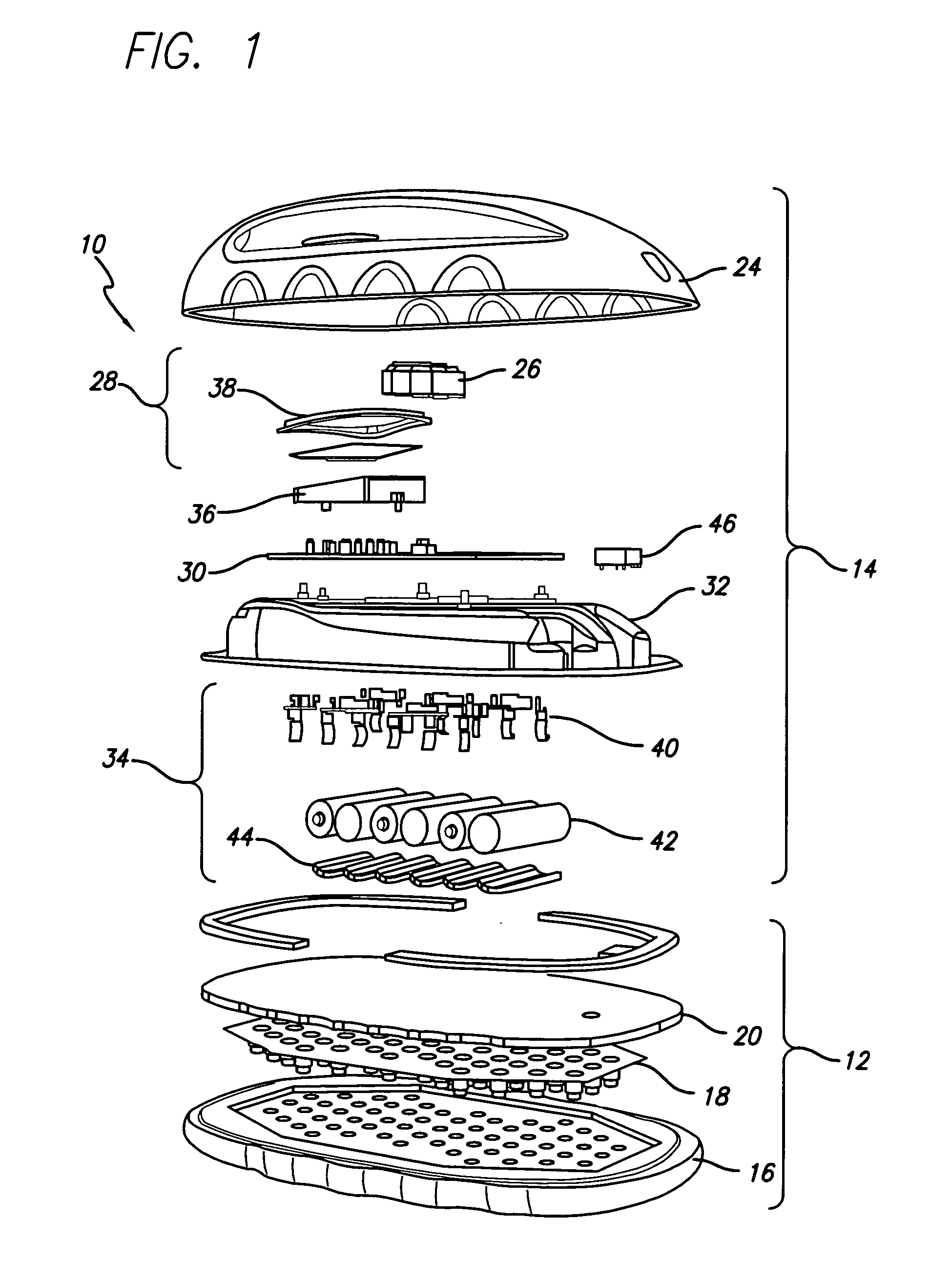
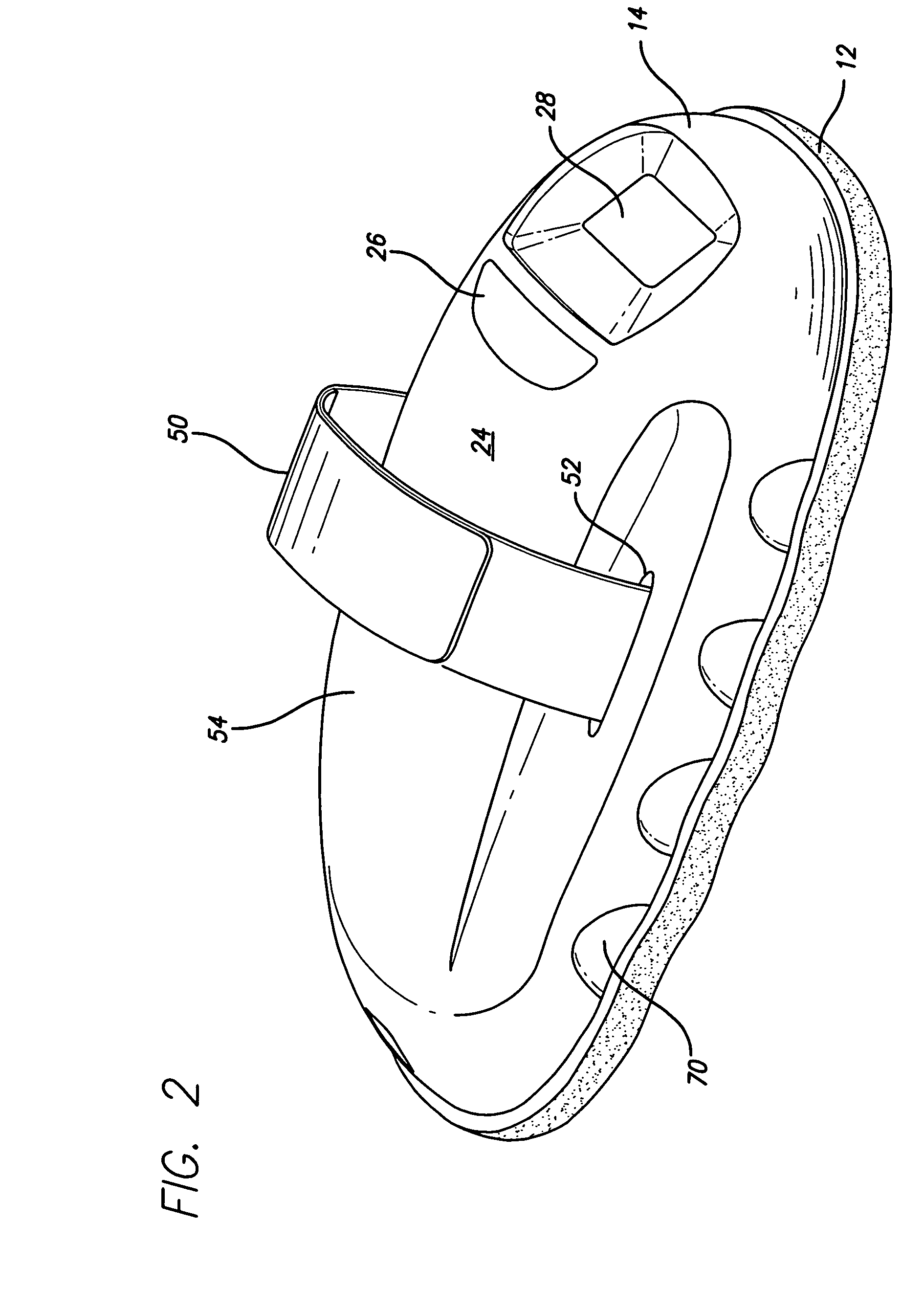
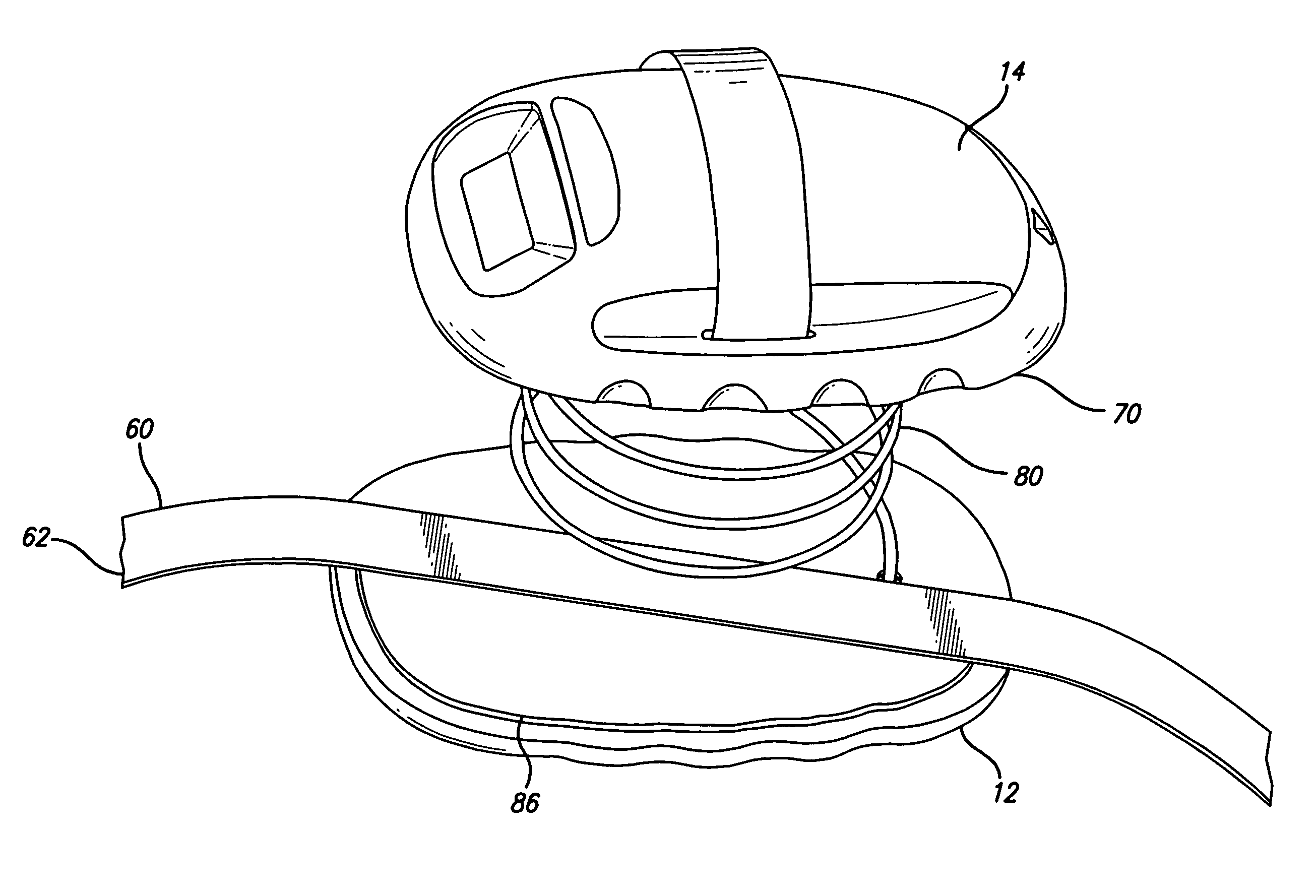
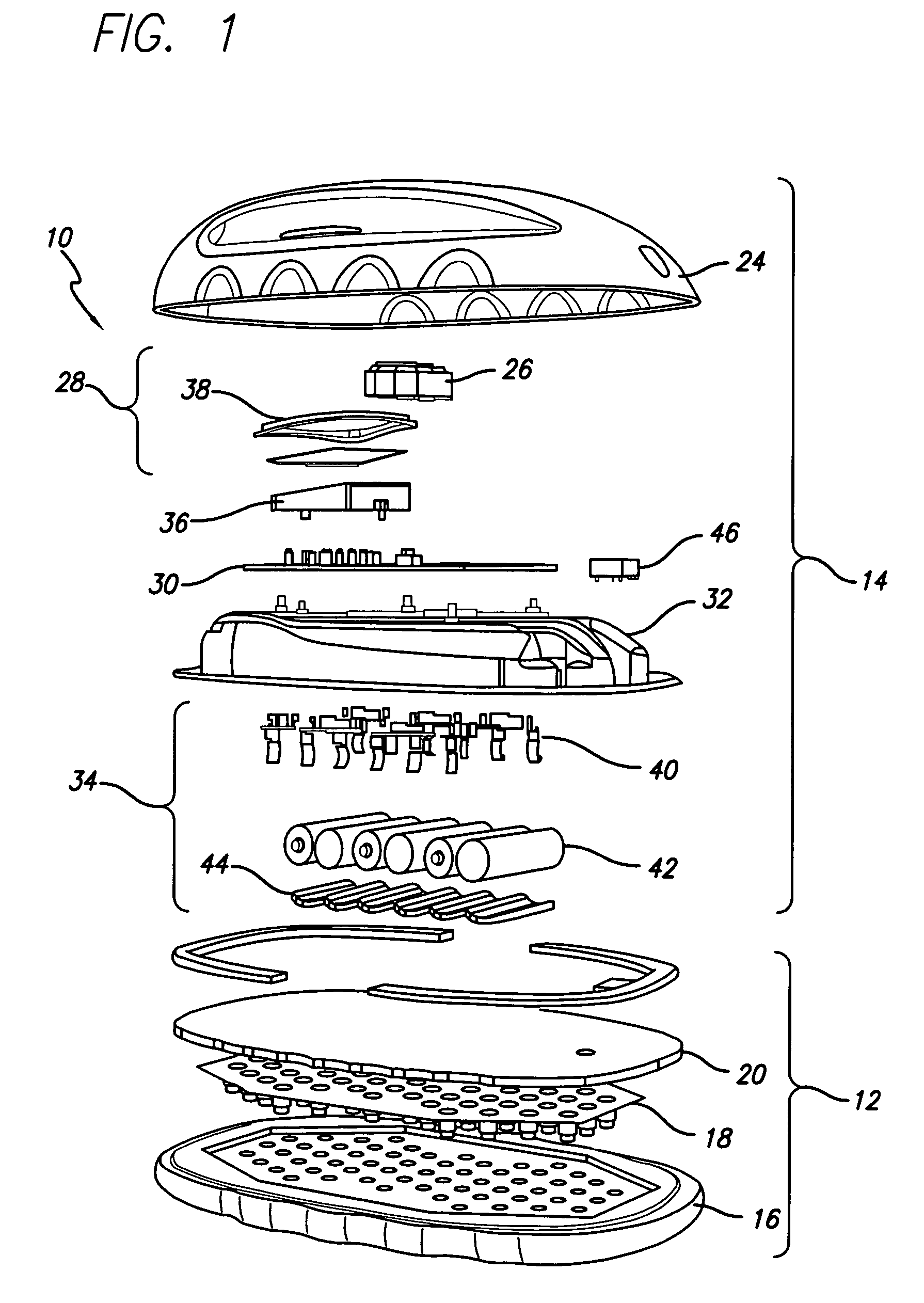
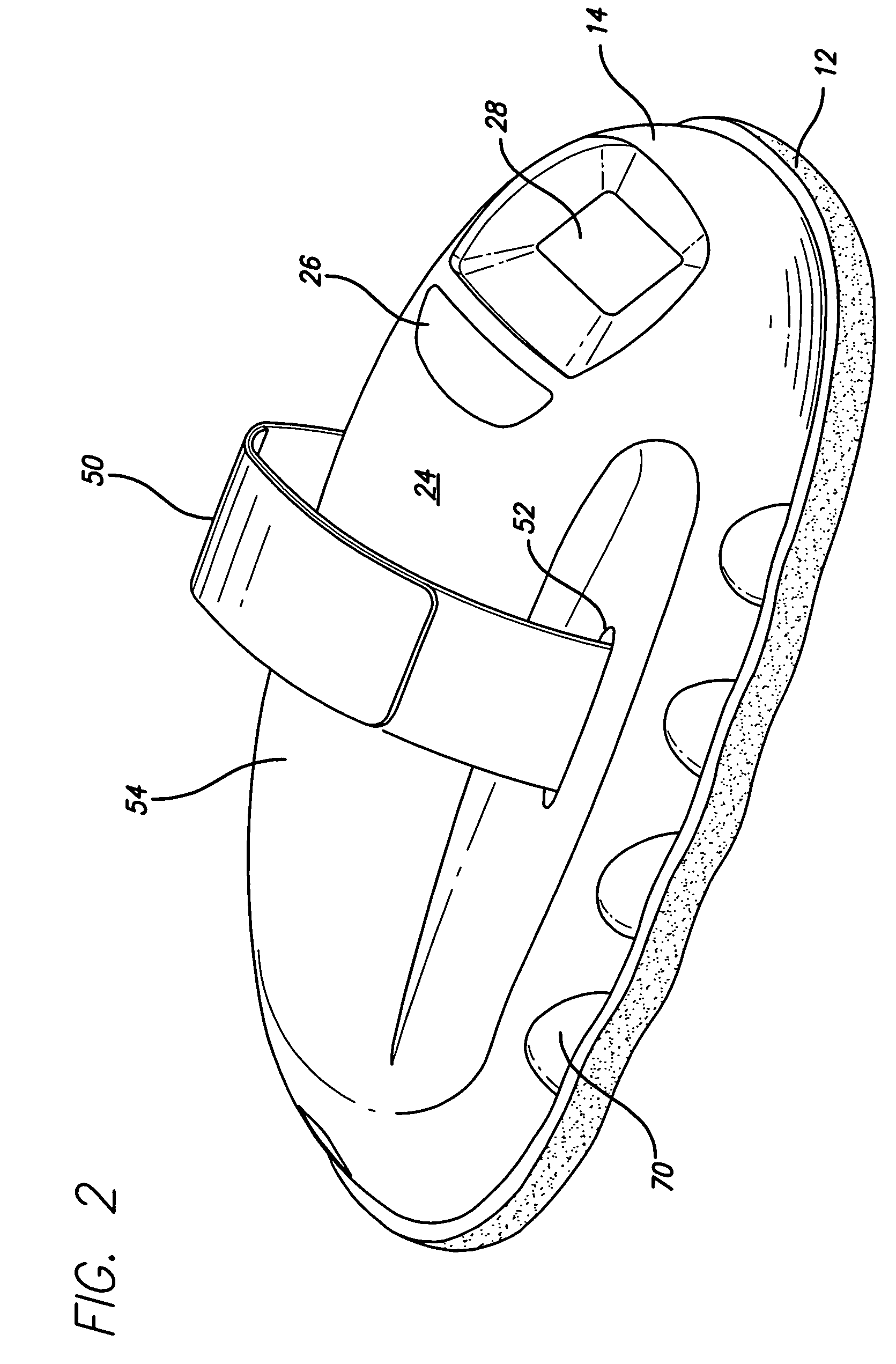
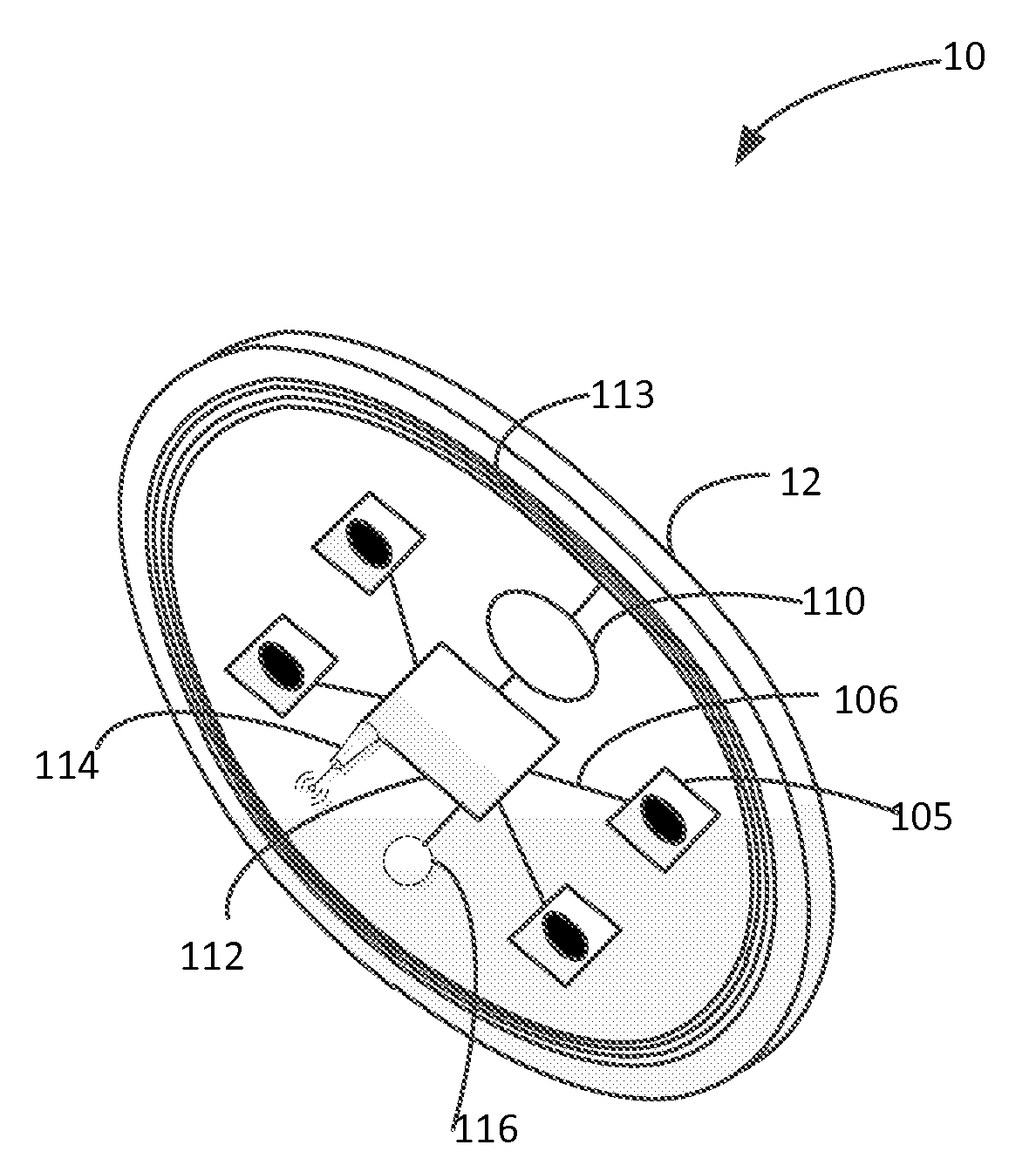
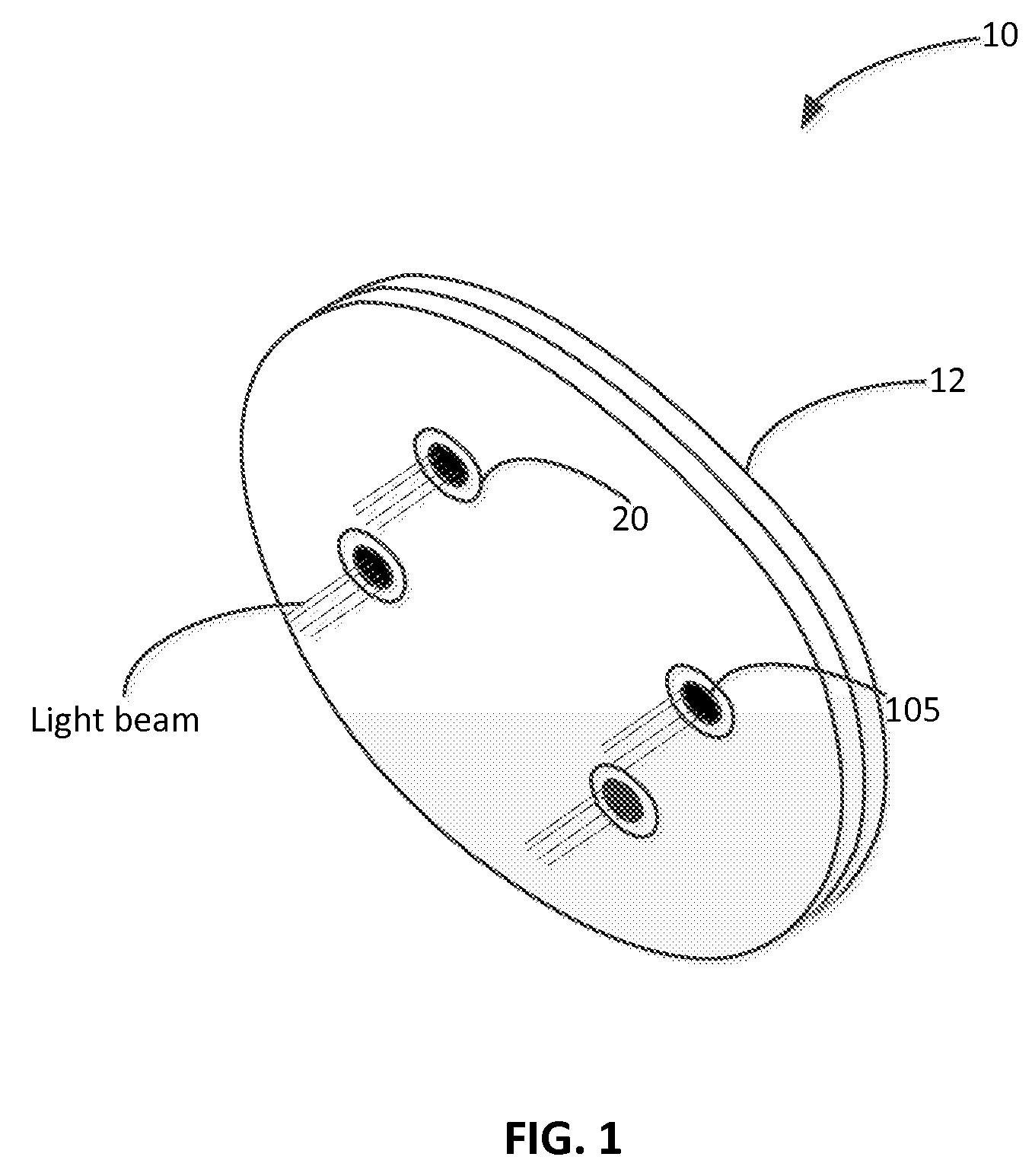
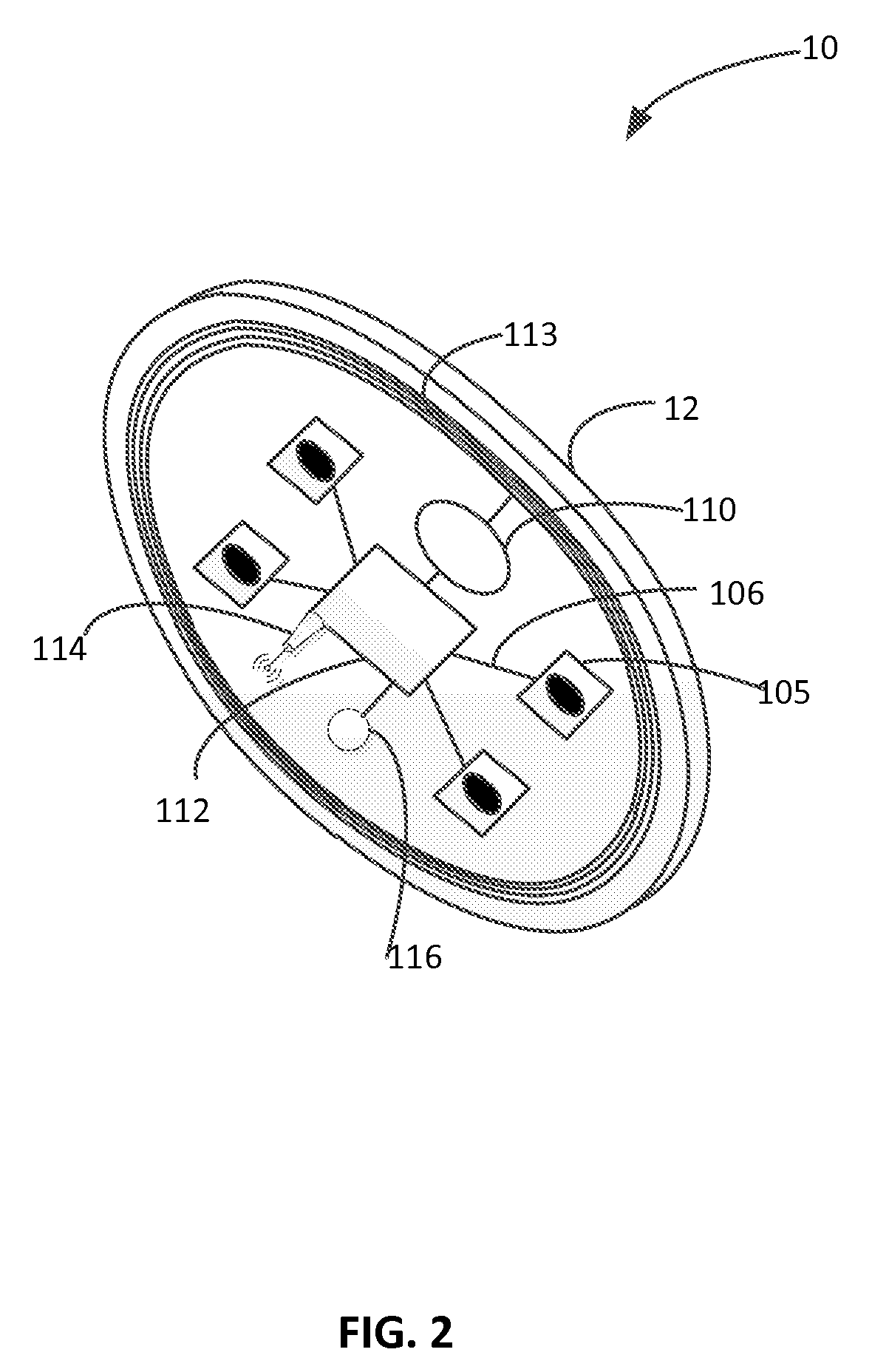
External wearable light therapy treatment systems
InactiveUS20070129776A1Reinforced jointsImprove abilitiesDiagnosticsSurgeryLight therapyLight energy
A light therapy system provides for self-alignment or positioning with respect to a joint of a subject. The light therapy system can provide light therapy to a body part of a subject. The therapy system has a main body configured to be placed adjacent a target site and an activatable light emitting system is coupled to the main body. The light emitting system is capable of delivering a therapeutic amount of light energy to the target site when the main body is placed adjacent the target site.
Owner:LIGHT SCI ONCOLOGY
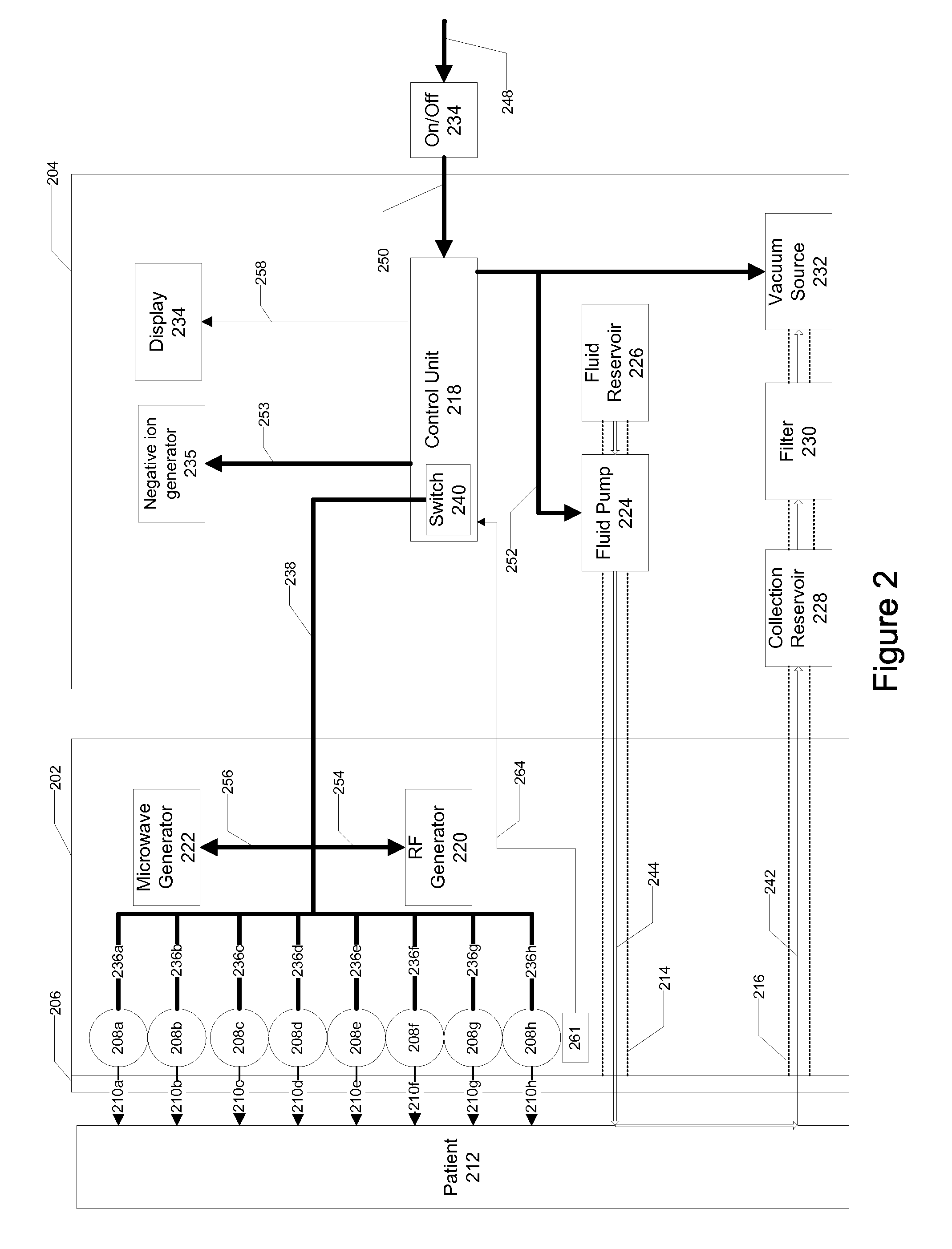
Microdermabrasion System with Combination Skin Therapies
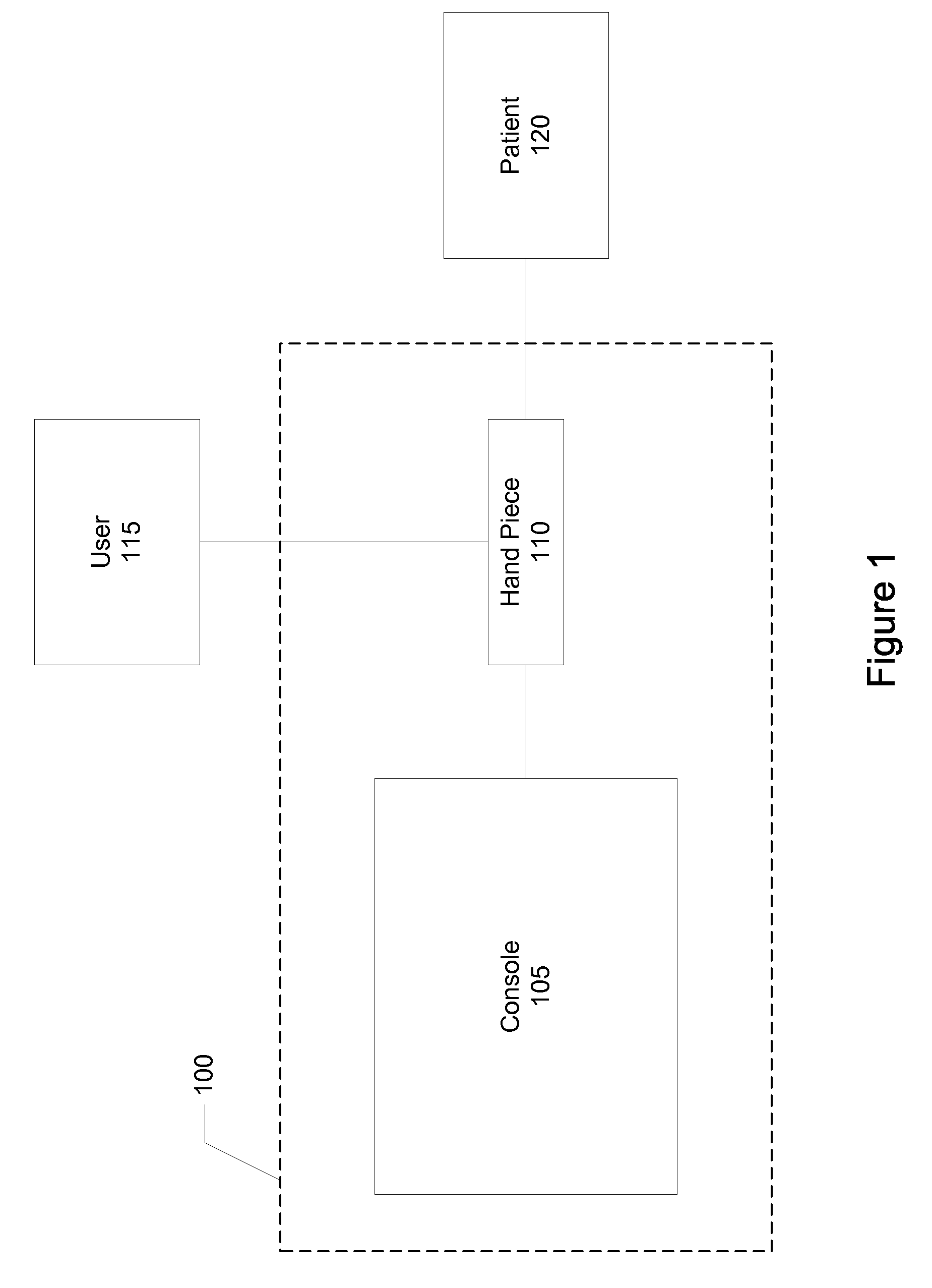
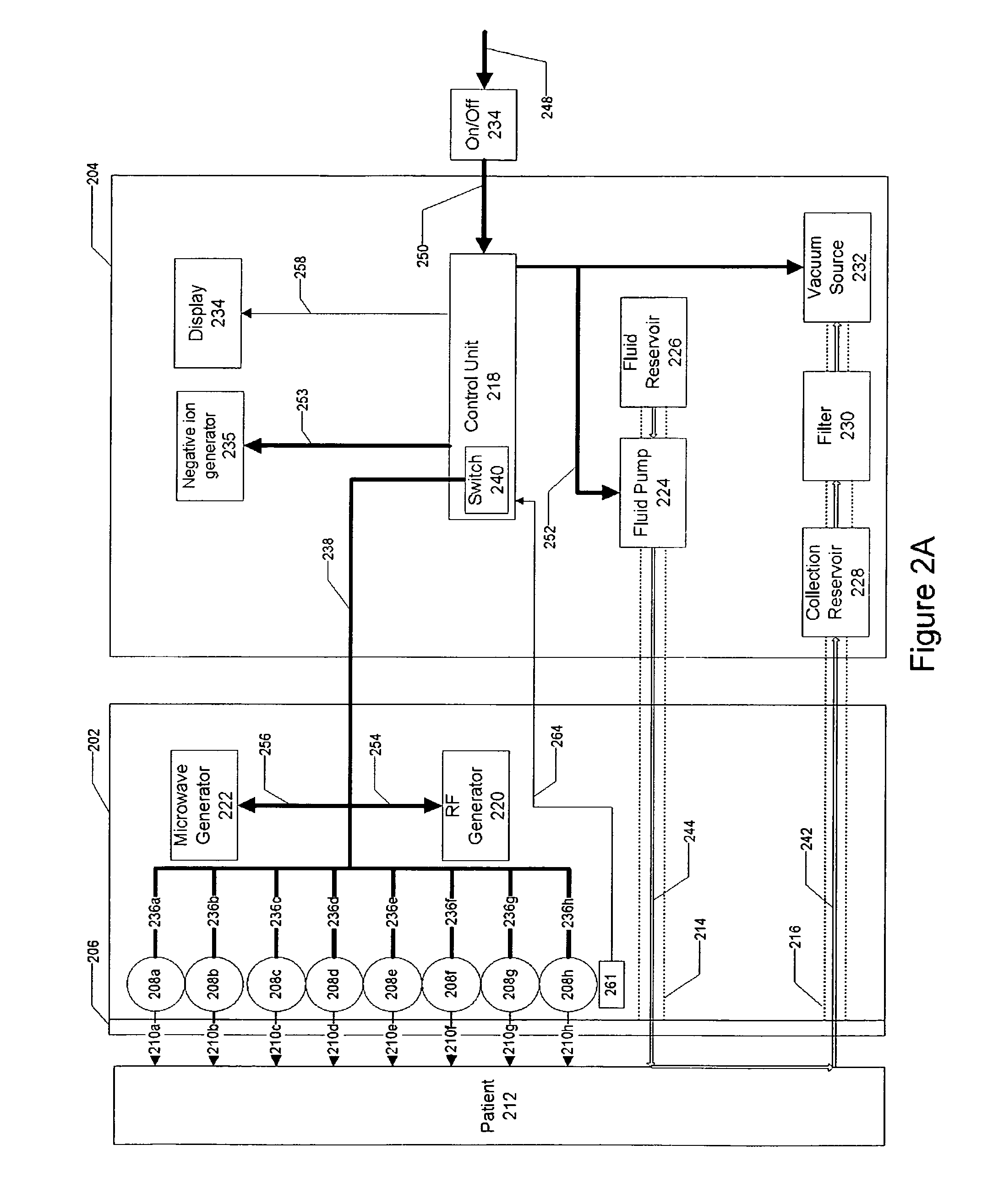
A microdermabrasion system offers a combination of other skin therapies in conjunction with microdermabrasion. In an implementation, the system applies light therapy, photodynamic therapy, radio frequency and microwave energy therapy, massage therapy, or combinations of these while exfoliating the skin.
Owner:ENVY MEDICAL
Intra-oral light therapy apparatuses and methods for their use
In some embodiments, an apparatus comprises a housing, an emitter, and an electronic circuit. The housing is configured to fit within a patient's mouth. The emitter is at least partially encased within the housing. The emitter is configured to emit an effective amount of light to the alveolar soft tissue when the housing is disposed within the mouth. The electronic circuit is operatively coupled to the emitter. The electronic circuit is configured to control the emitter when the housing is disposed within the mouth and the apparatus is in use during orthodontic treatment. The apparatus and its use for regulating tooth movement or maintaining or improving oral tissue health are disclosed herein.
Owner:BIOLUX RES HLDG INC
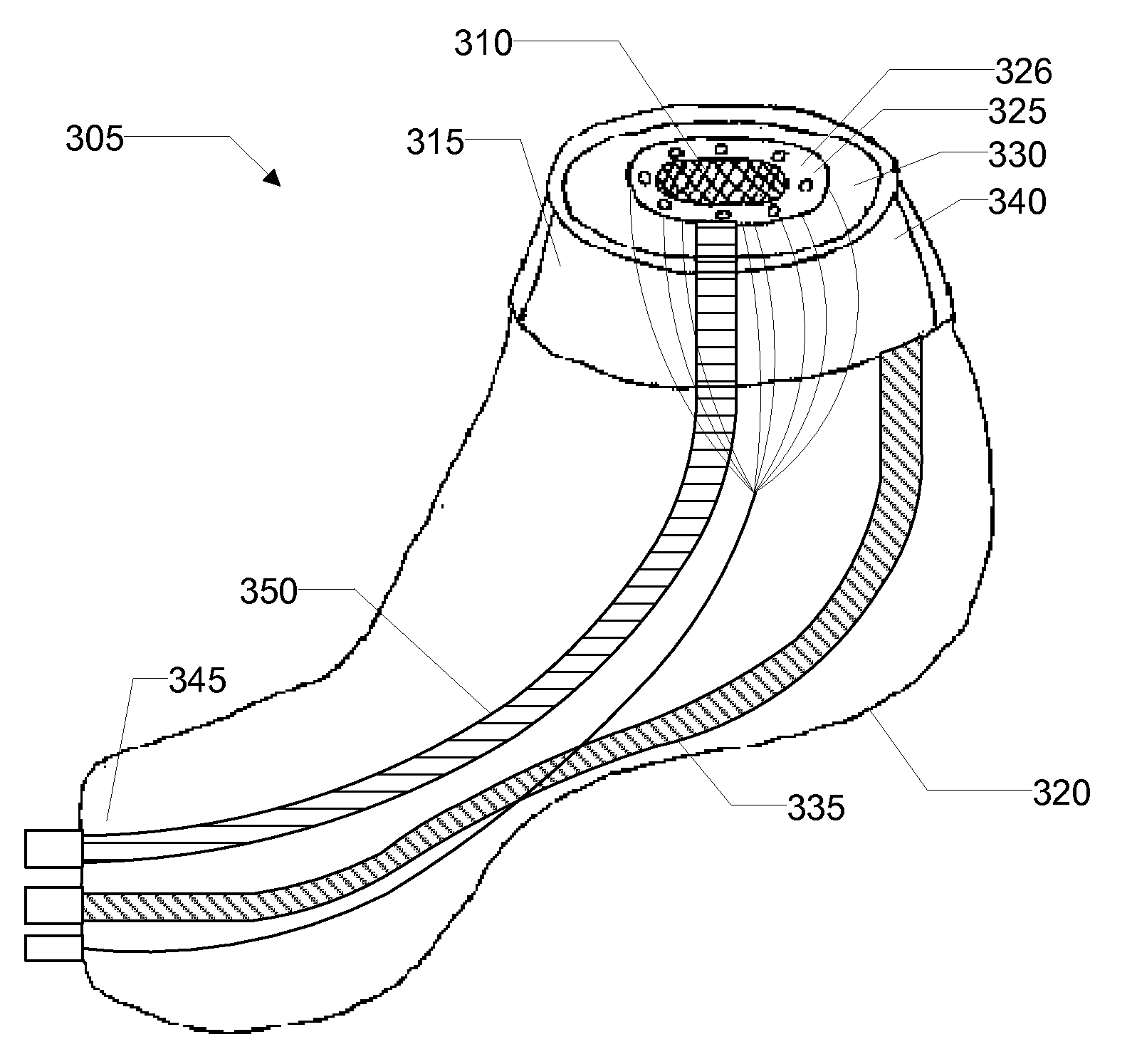
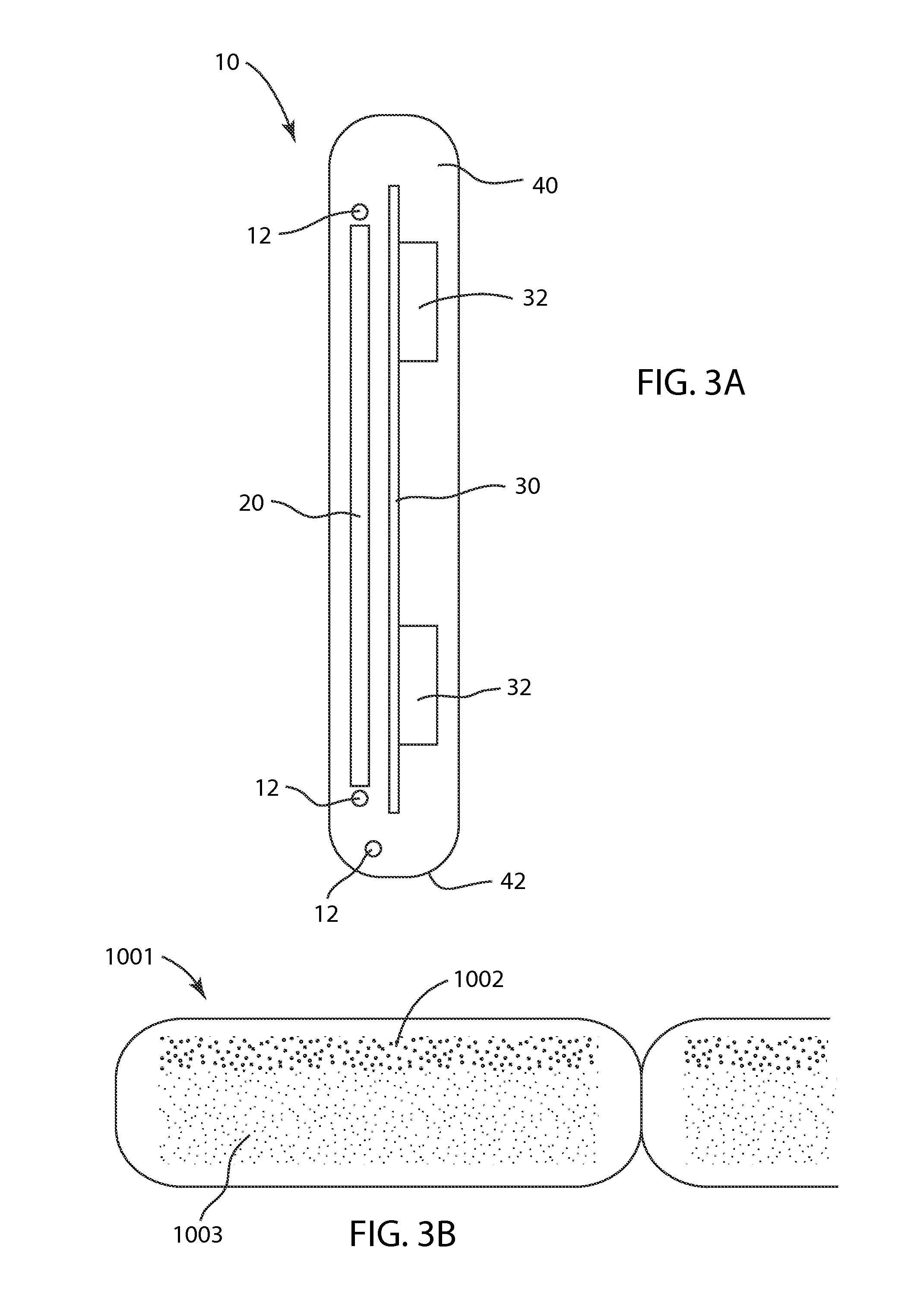
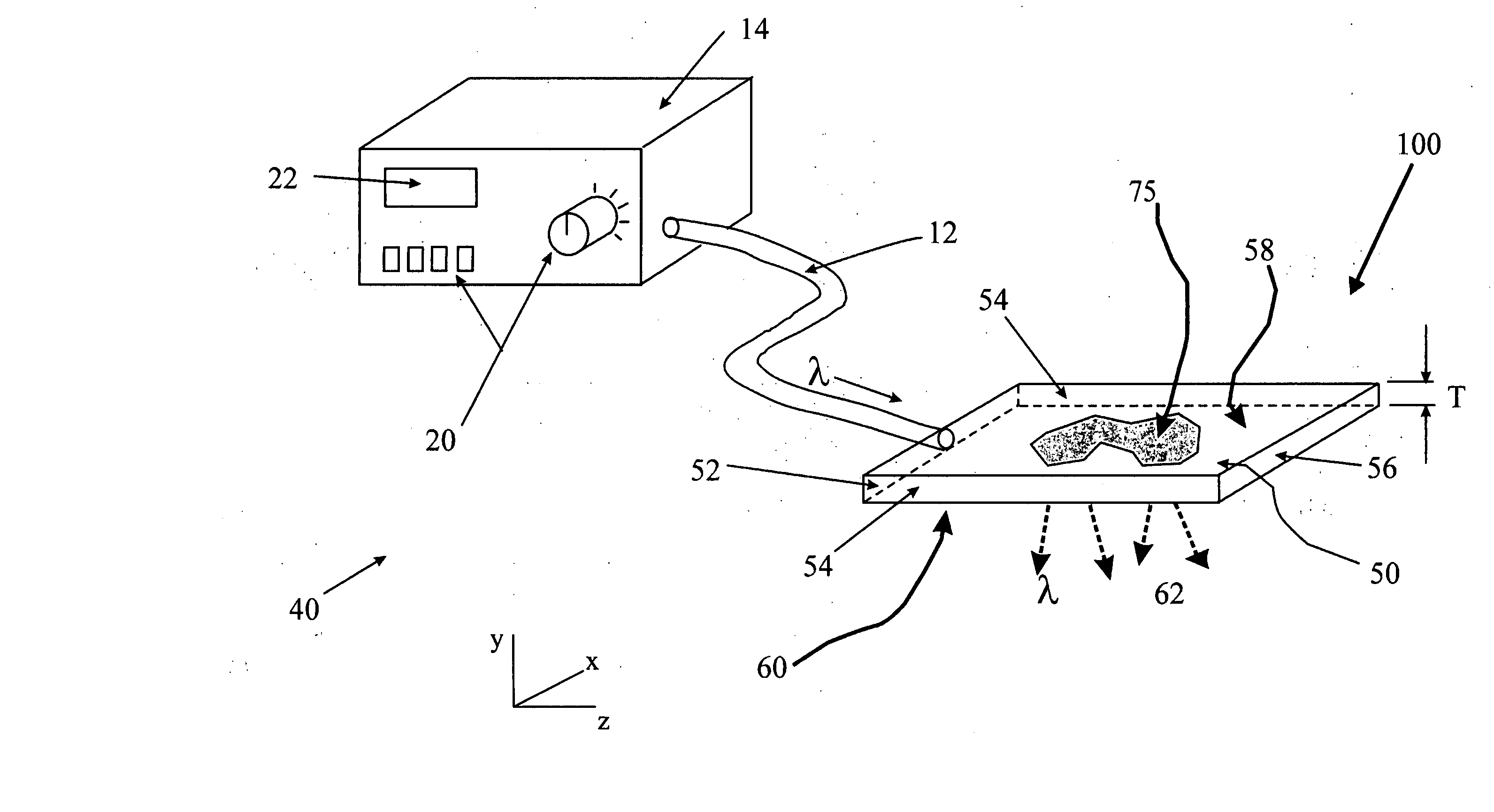
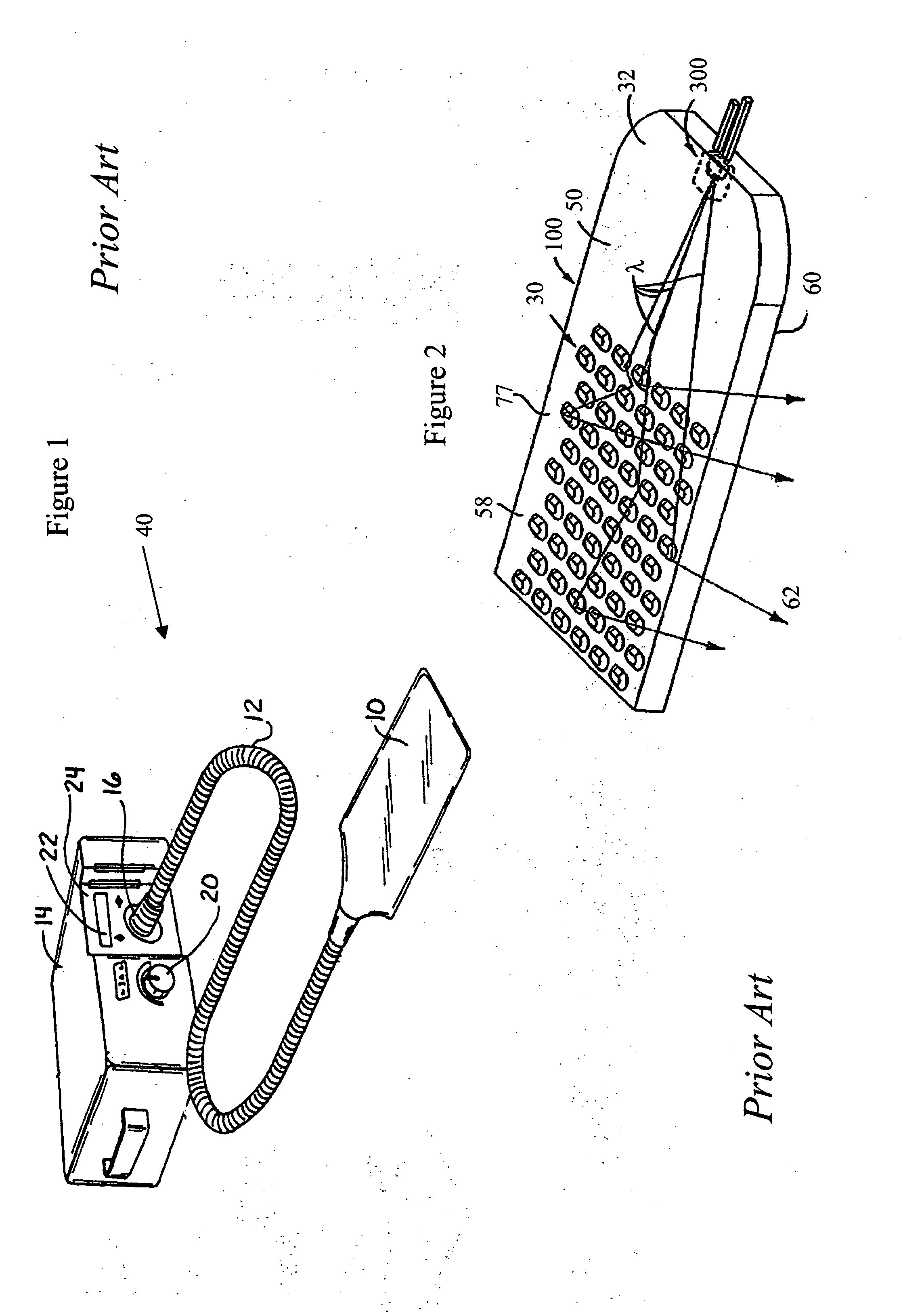
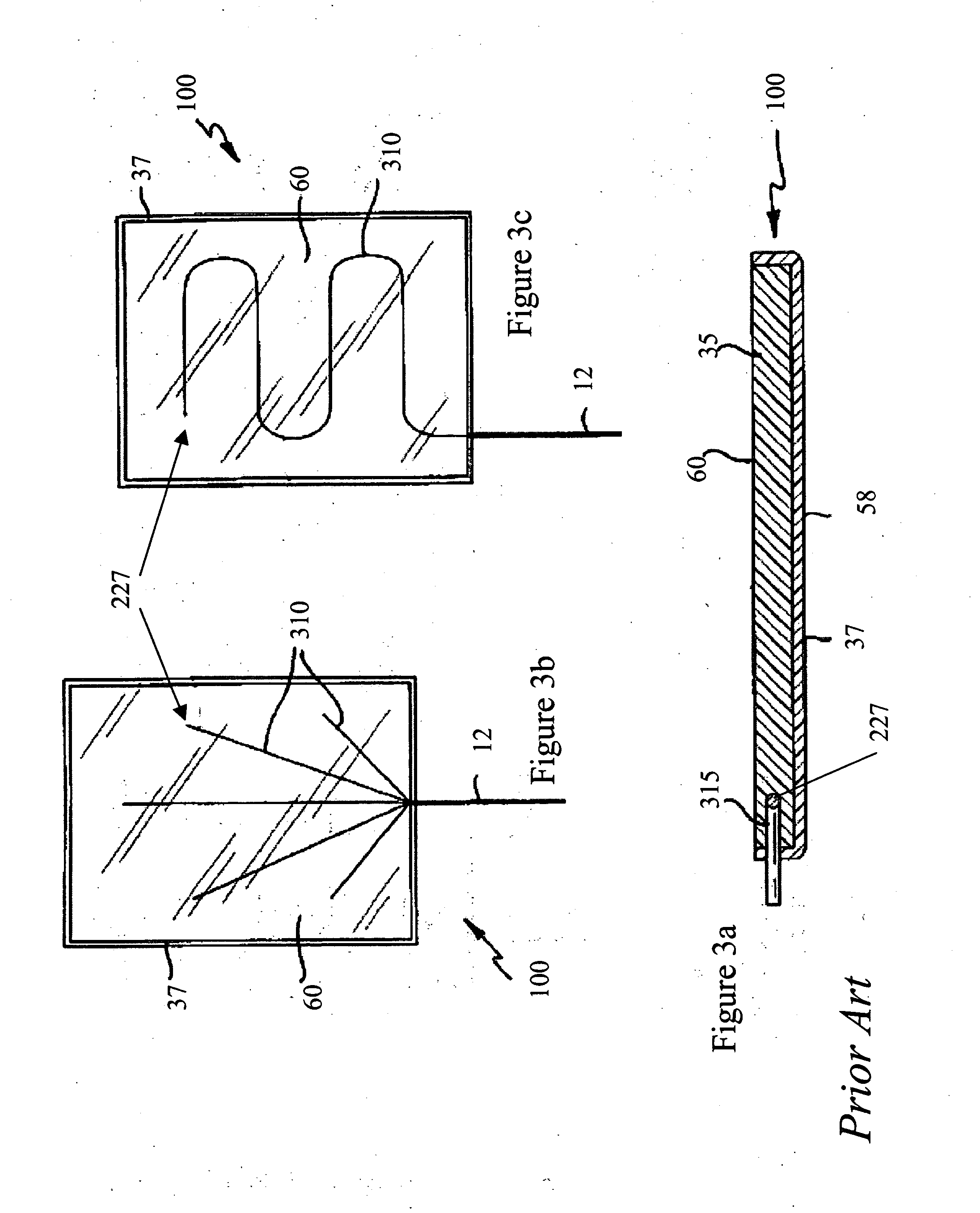
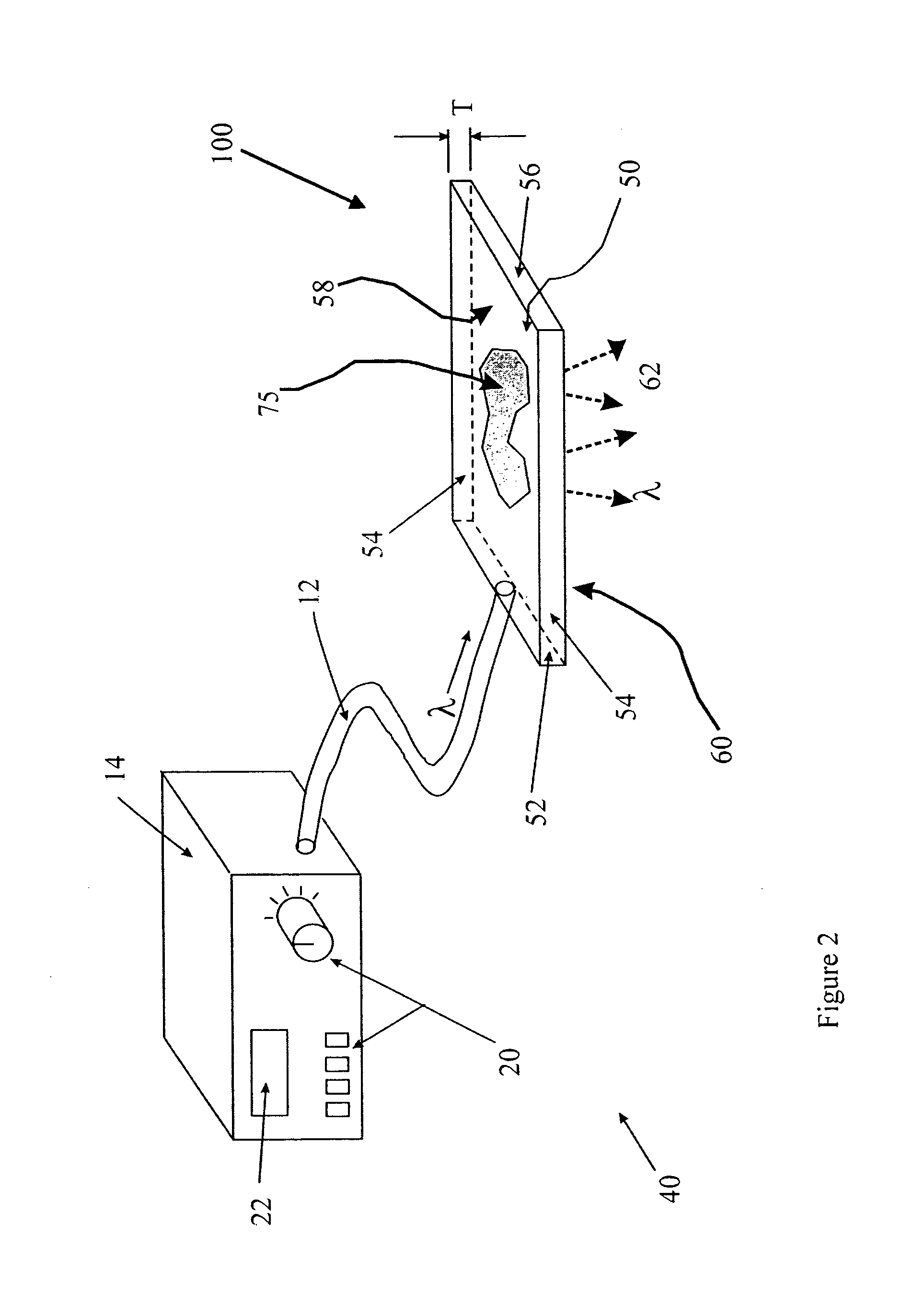
Light guide based light therapy device
A light therapy device (40) for delivering light energy to treat medical conditions in tissues (200) includes a light source (300) with one or more light emitters, which provides input light (305). A light coupling means comprised of one or more optical fibers (310) for coupling the input light into a bandage portion (100) comprising a flexible optical substrate (50). A light extraction means (30) directs a portion of the input light out of the bandage and towards one or more localized areas of the tissues. A semi-permeable transparent membrane (400), attached directly or indirectly to the substrate, controls a flow of moisture and moisture vapor to and from the tissues. A controller (16) means controls a light dosage emitted from the light therapy device.
Owner:CARESTREAM HEALTH INC
Optical therapy devices, systems, kits and methods for providing therapy to a body cavity
An optical therapy device is disclosed. The optical therapy device provides therapeutic light therapy to a body cavity. The device includes a housing adapted to be hand held, a UV light source positioned in or on the housing, and an insertion member having a distal end configured to be inserted into the body cavity to illuminate tissue in the body cavity with light from the light source.
Owner:VALAM CORP
Light therapy device
A light therapy device (40) for delivering light energy to a portion of a patient's body comprises a light source (115). The light source comprises one or more light emitters (122) for providing input light. A light coupling means (80) directs the input light into a light guide (140). A flexible optically transparent light guide material comprises the light guide. A light extraction means (75) is applied to a surface of the light guide material. The light extraction means is positioned to provide light therapy treatment to one or more localized areas of the patient's body. A control means controls a light dosage relative to intensity, wavelength, modulation frequency, repetition, and timing of treatments.
Owner:CARESTREAM HEALTH INC
Heat and light therapy treatment device and method
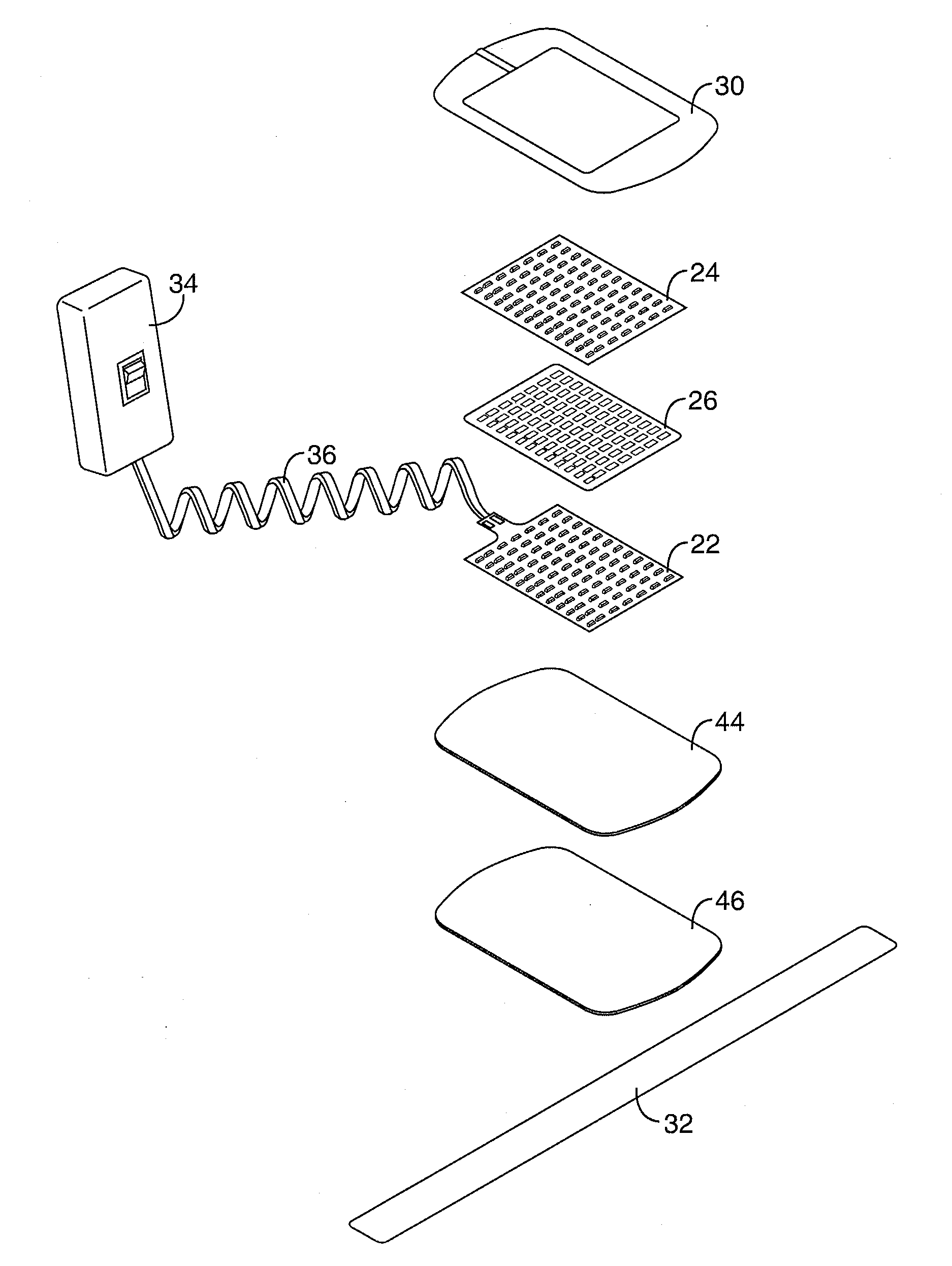
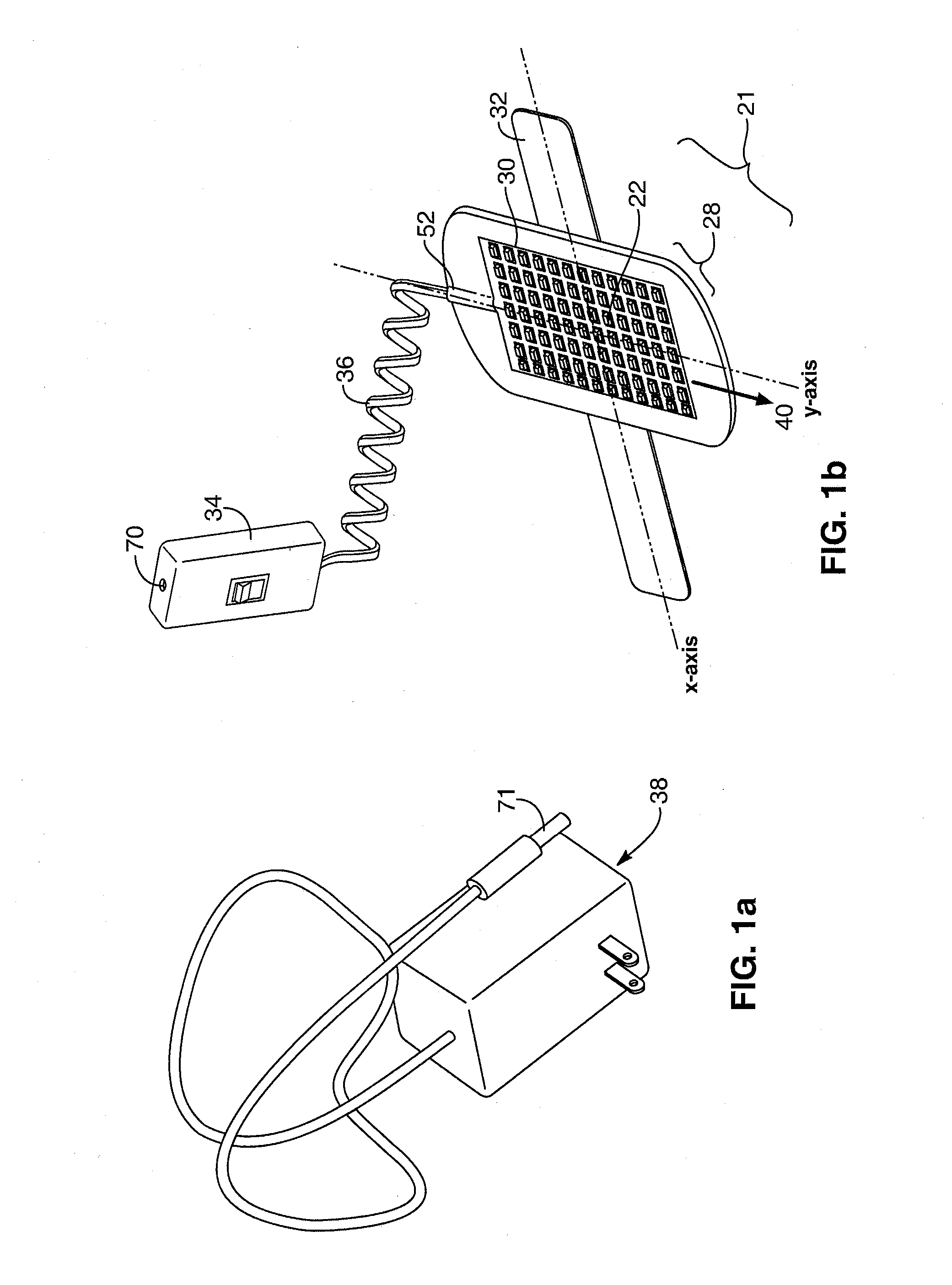
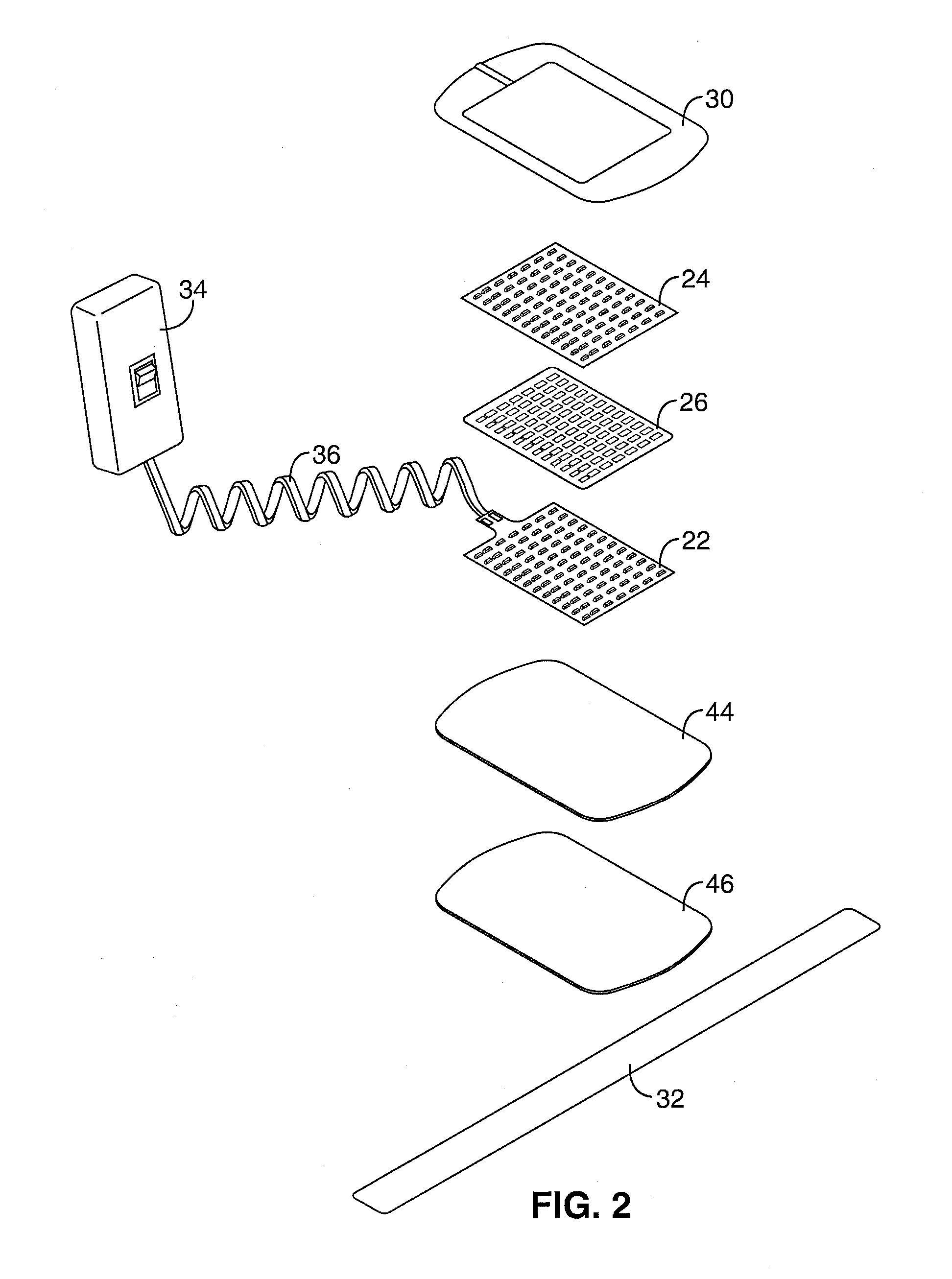
InactiveUS20060287696A1Function increaseFacilitates convenient and straightforward and effective useElectrotherapyLight therapyLight therapyLight energy
Heat and light is generated and applied to the skin of a user with multiple arrays of light emitting devices. The amount of heat and light energy delivered from each array is separately controlled relative to a predetermined dose of light energy and a temperature of the skin adjacent to each array. The arrays may be flexibly connected to conform to the contours of a significant area the user's anatomy.
Owner:BIOCARE SYST
Electroluminescent light therapy devices
InactiveUS20050278003A1Eliminate wrinklesElectrotherapySurgical instrument detailsWrinkle skinOphthalmology
Wearable devices including a hat or cap, eyeglasses, an eye mask, or a face mask deliver light from light-emitting diodes or deliver electroluminescent light from a light source including an electroluminescent wire or flat panel powered by an inverter connected to the hat or cap, the eyeglasses, the eye mask, or the face mask. The delivery of the light is for entertainment or therapeutic purposes. Delivery of therapeutic light to the retinal area or to the skin of the user by a wearable device, without the use of the hands of the user, applies consistent levels of the therapeutic light to relax the user, to remove wrinkles in the skin, and to impart other healing effects. A sufficient amount of lux at appropriate optical wavelengths is generated to be incident for long periods upon the retina of the user or upon the skin of the user for healing effect.
Owner:LIVE WIRE ENTERPRISES
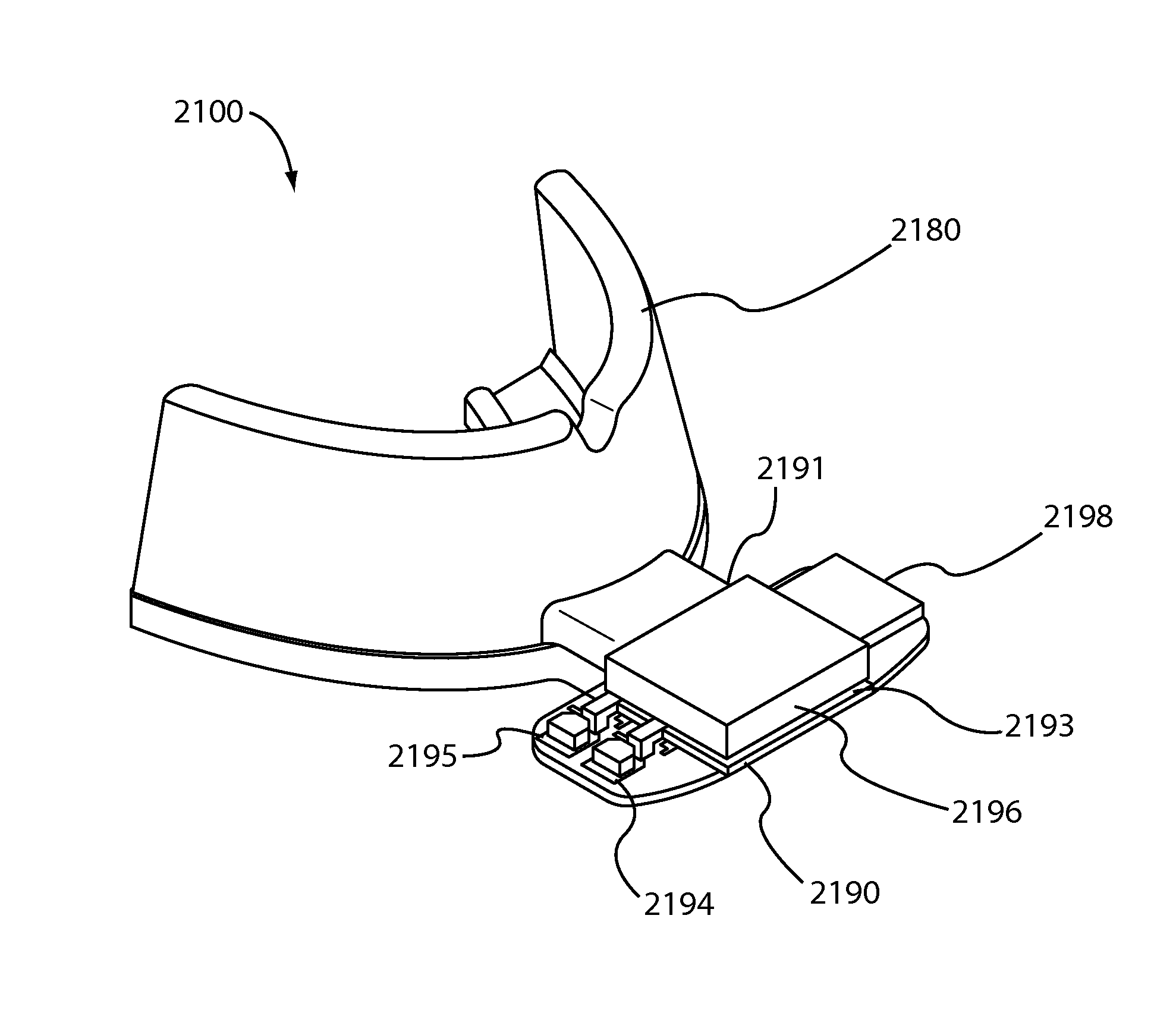
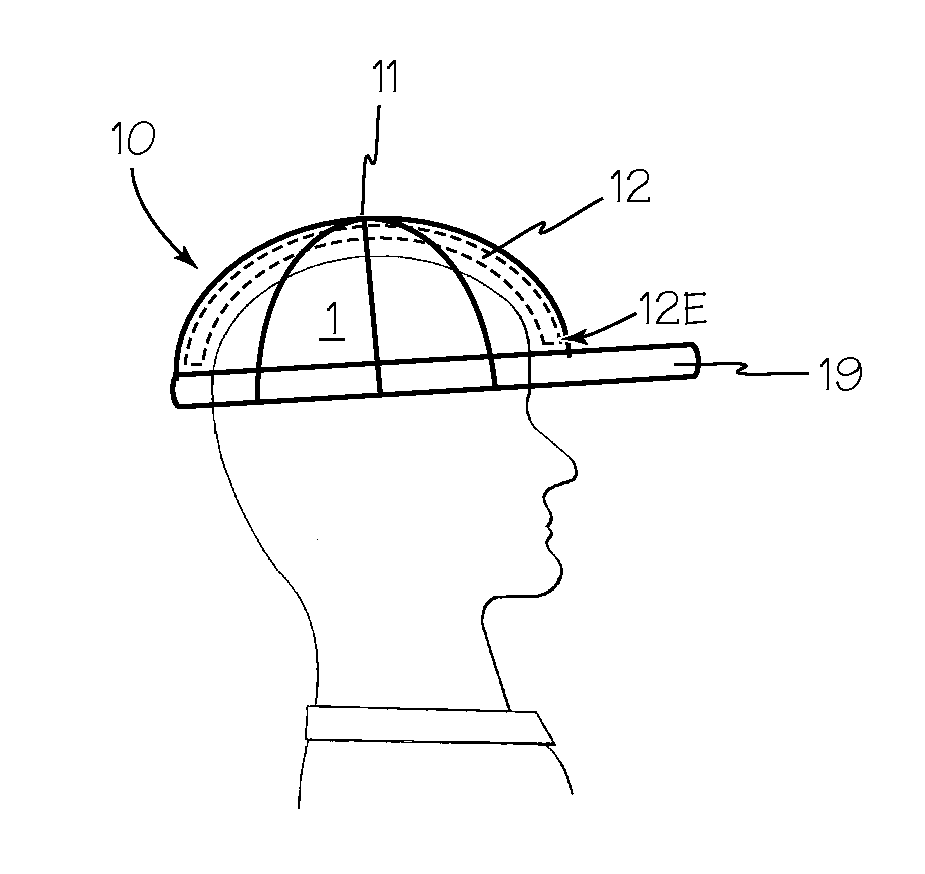
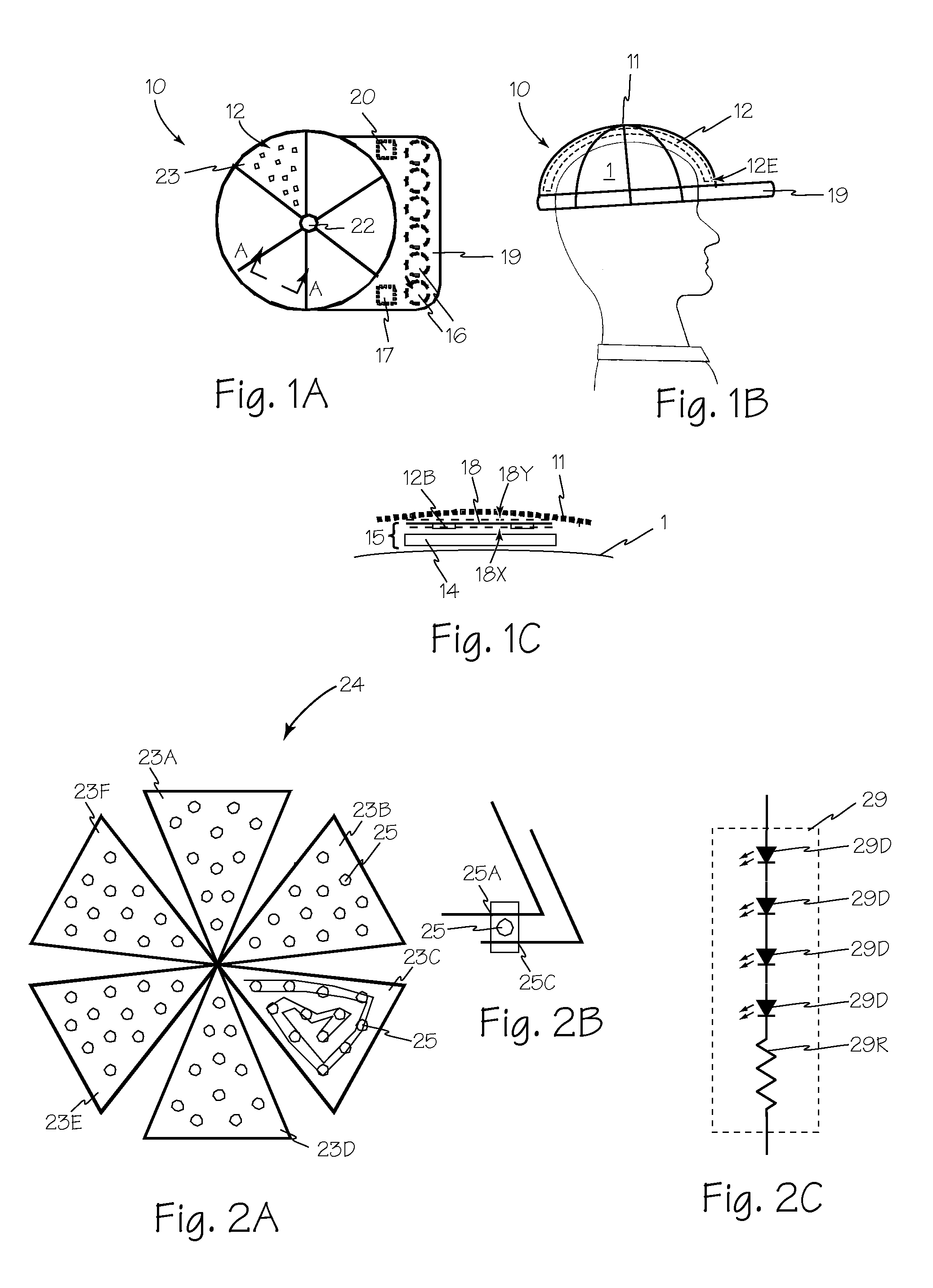
Methods, Compositions and Apparatus for Treating a Scalp
InactiveUS20100106077A1Efficient use ofSimple processElectrotherapyMedical applicatorsDocking stationLight therapy
A phototherapy light cap is a flexible, generally hemispherical cap having a light source to supply suitable dosage requirements of current and future light therapies. The phototherapy light cap may also include a rechargeable battery source, a light source or an array of light sources, a light diffuser and an interface to a recharging source that may be a docking station. A phototherapy light cap may alternatively be an insert for any commercial head dressing, preferably adapted for convenient recharging. Combining the use of a phototherapy light cap with gelatinized therapeutic agents provides a suitable treatment technique for a scalp utilizing phototherapy, heat and any suitable combination of active ingredients such as minoxidil.
Owner:TRANSDERMAL CAP
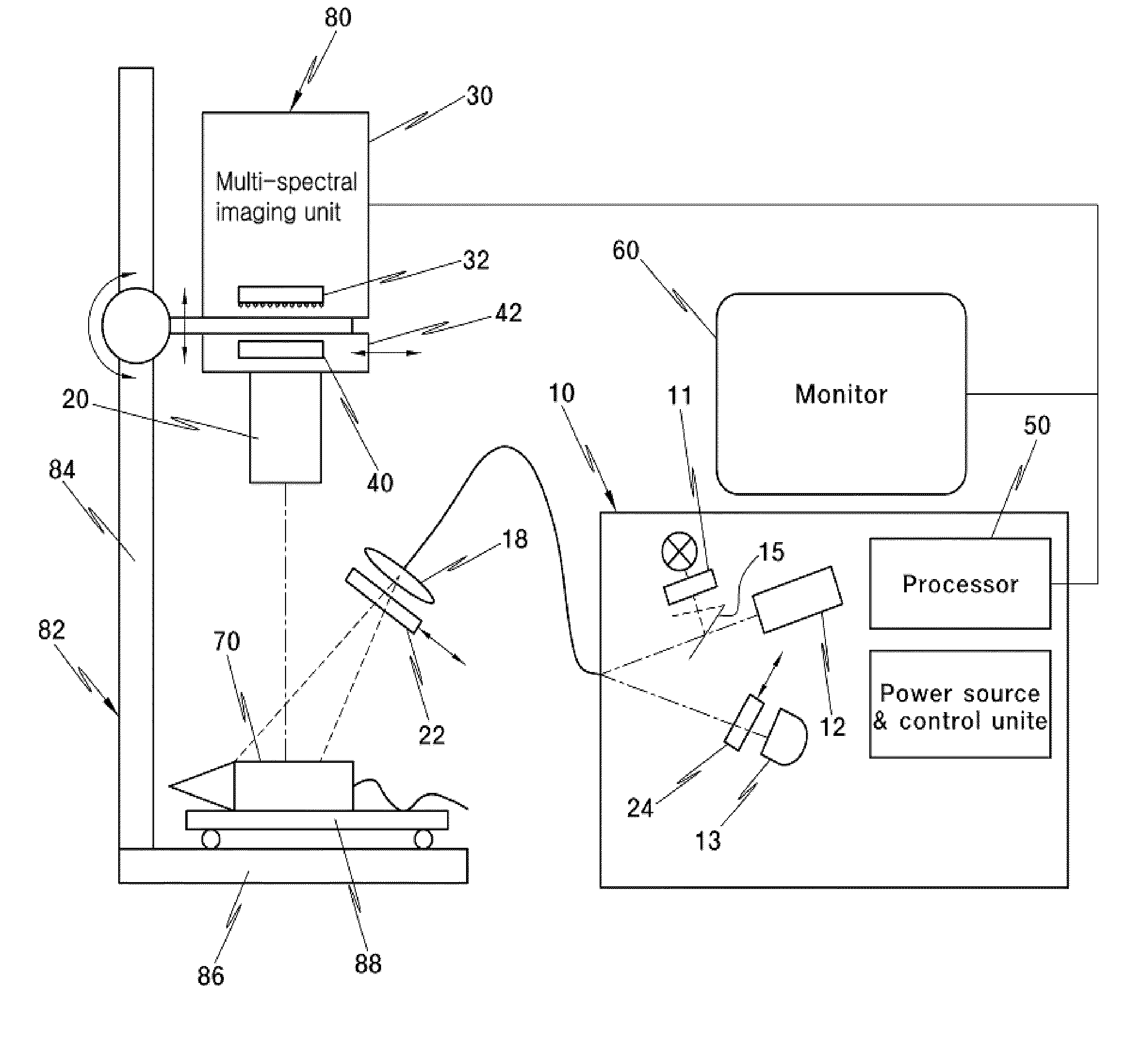
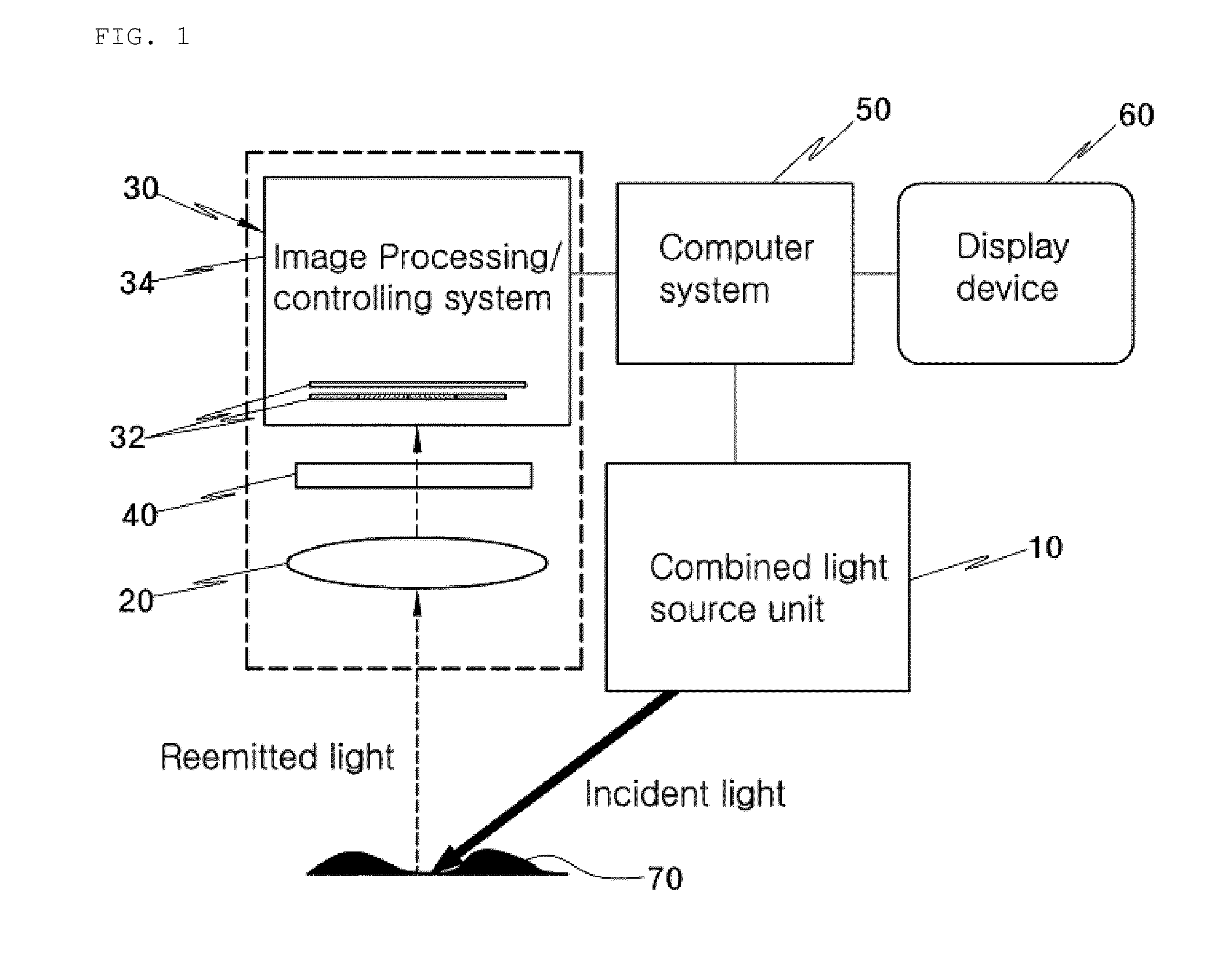
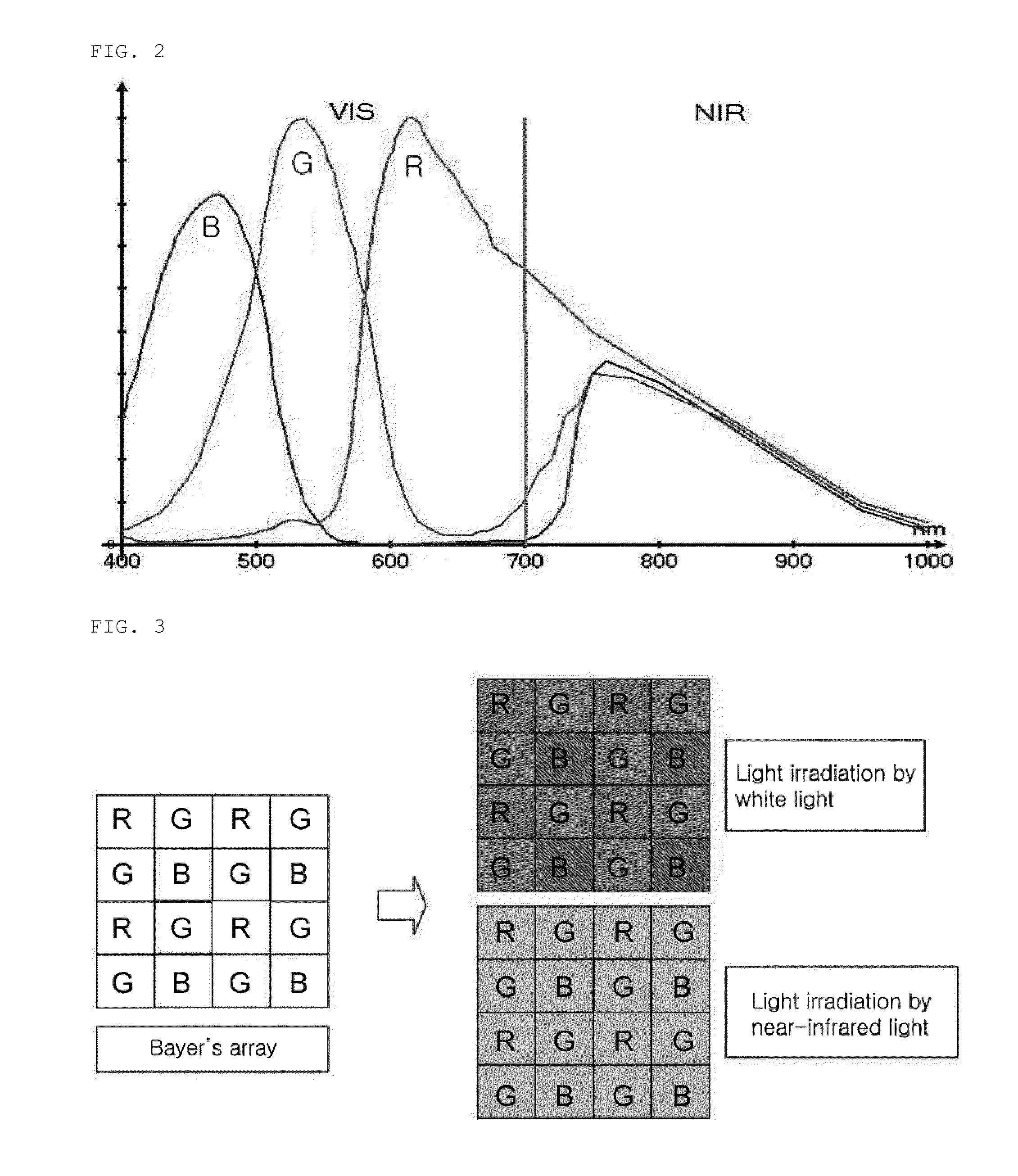
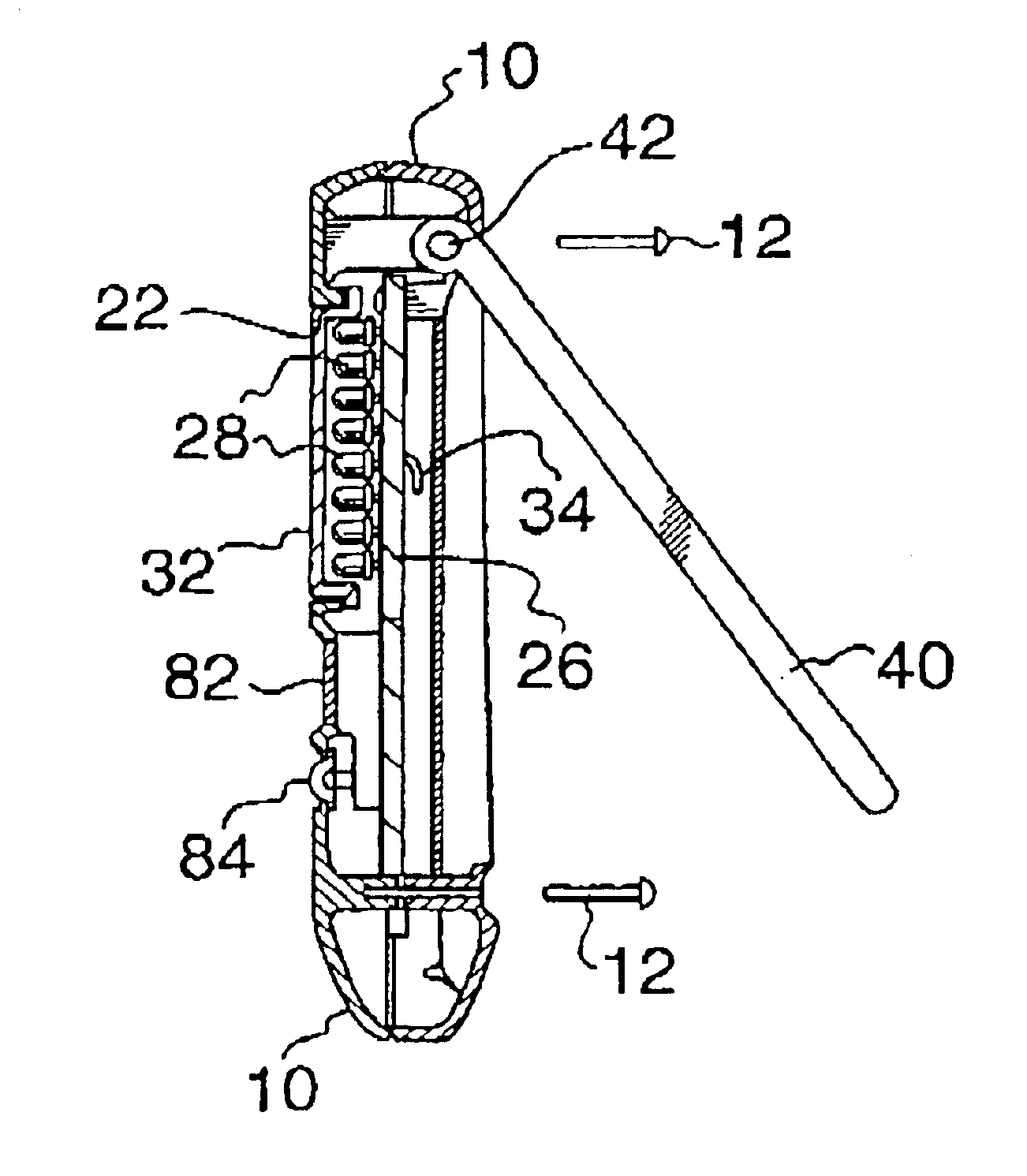
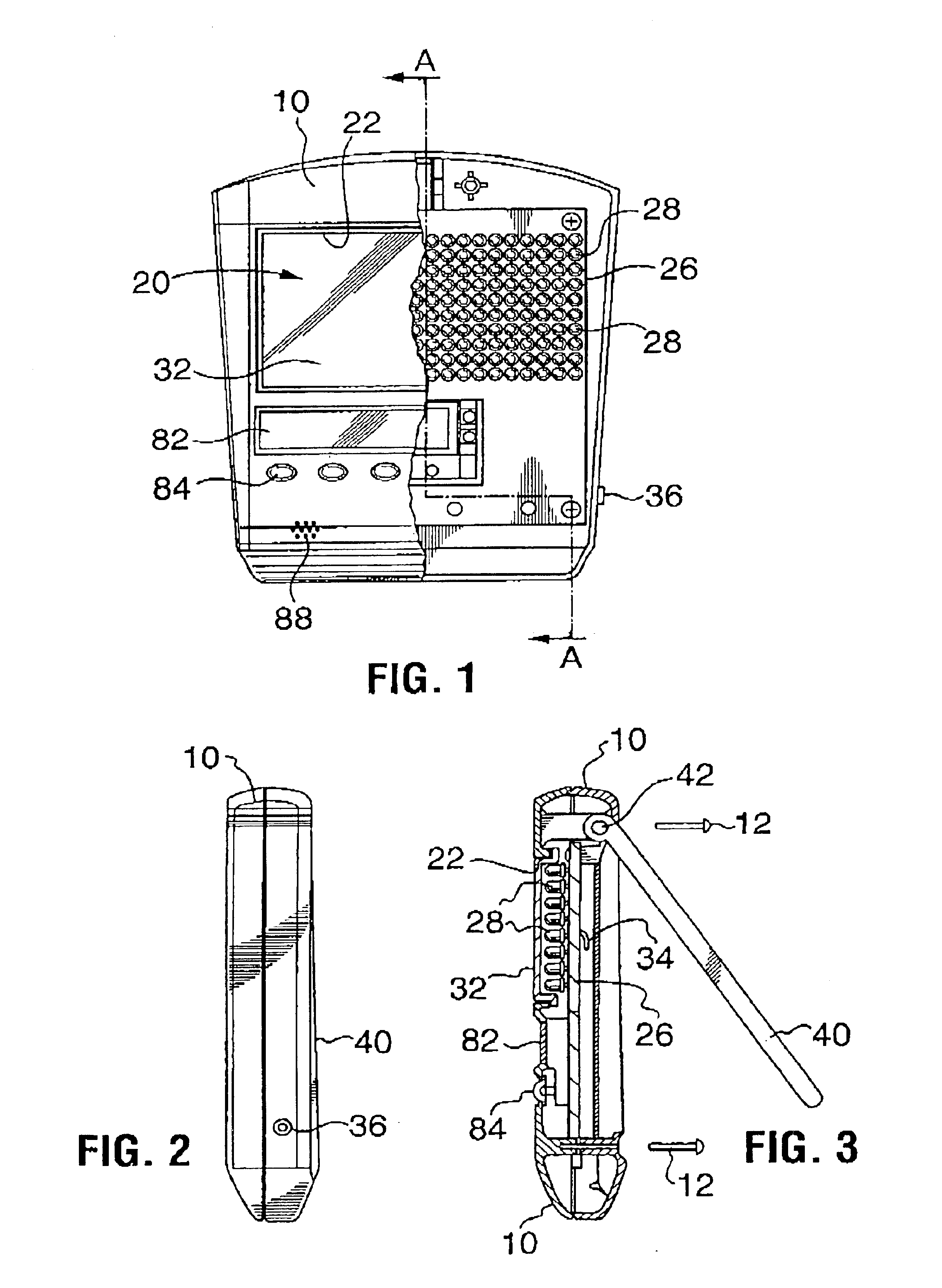
Combined apparatus for detection of multispectral optical image emitted from living body and for light therapy
InactiveUS20110270092A1Simple structureRaman/scattering spectroscopyDiagnostics using fluorescence emissionFluorescenceDisplay device
The present invention provides a fluorescence detection and photodynamic therapy apparatus including: a combined light source unit 10 including a plurality of coherent and non-coherent light sources 11, 12 and 13 configured to irradiate light onto a to-be-observed object while performing continuous illumination; an optical imaging unit 20 configured to form an image of the to-be-observed object 70 and project the image to an image processing / controlling system 34; a multispectral imaging unit 30 including a one-chip multispectral sensor and the image processing / controlling system 34; a blocking filter 40 installed between the to-be-observed object 70 and the one-chip multispectral sensor 32, the blocking filter being configured to block some light reflected off from the to-be-observed object 70 while allowing some light and fluorescent light to pass therethrough; a computer system 50 configured to process, analyze, reproduce and store the image acquired from the multispectral imaging unit 30, and transfer the image to a display device 60 and control the overall operation of all the related elements; and the display device 60 configured to display a processing result of the image by the computer system 50.
Owner:KOREA ELECTROTECH RES INST
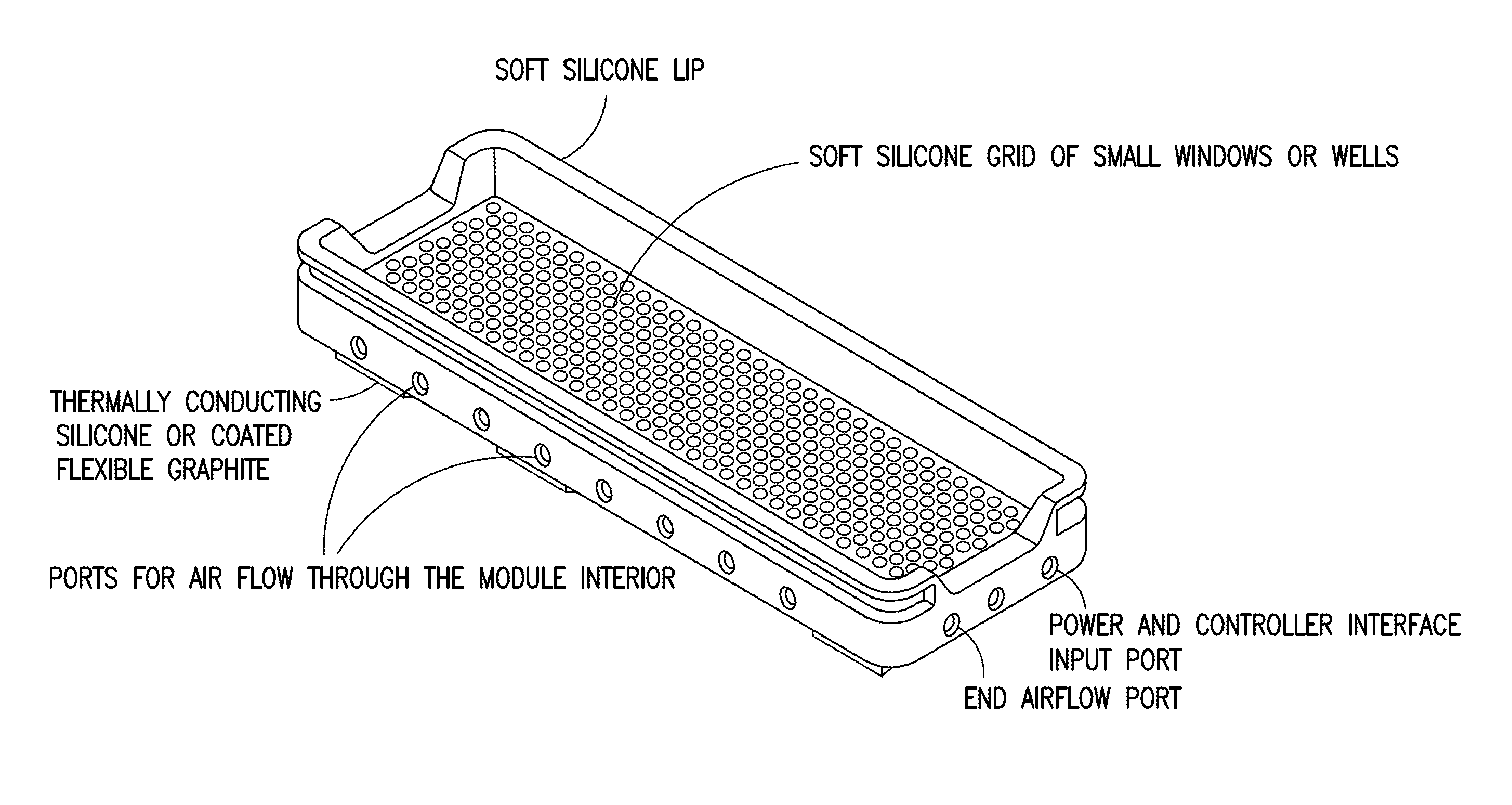
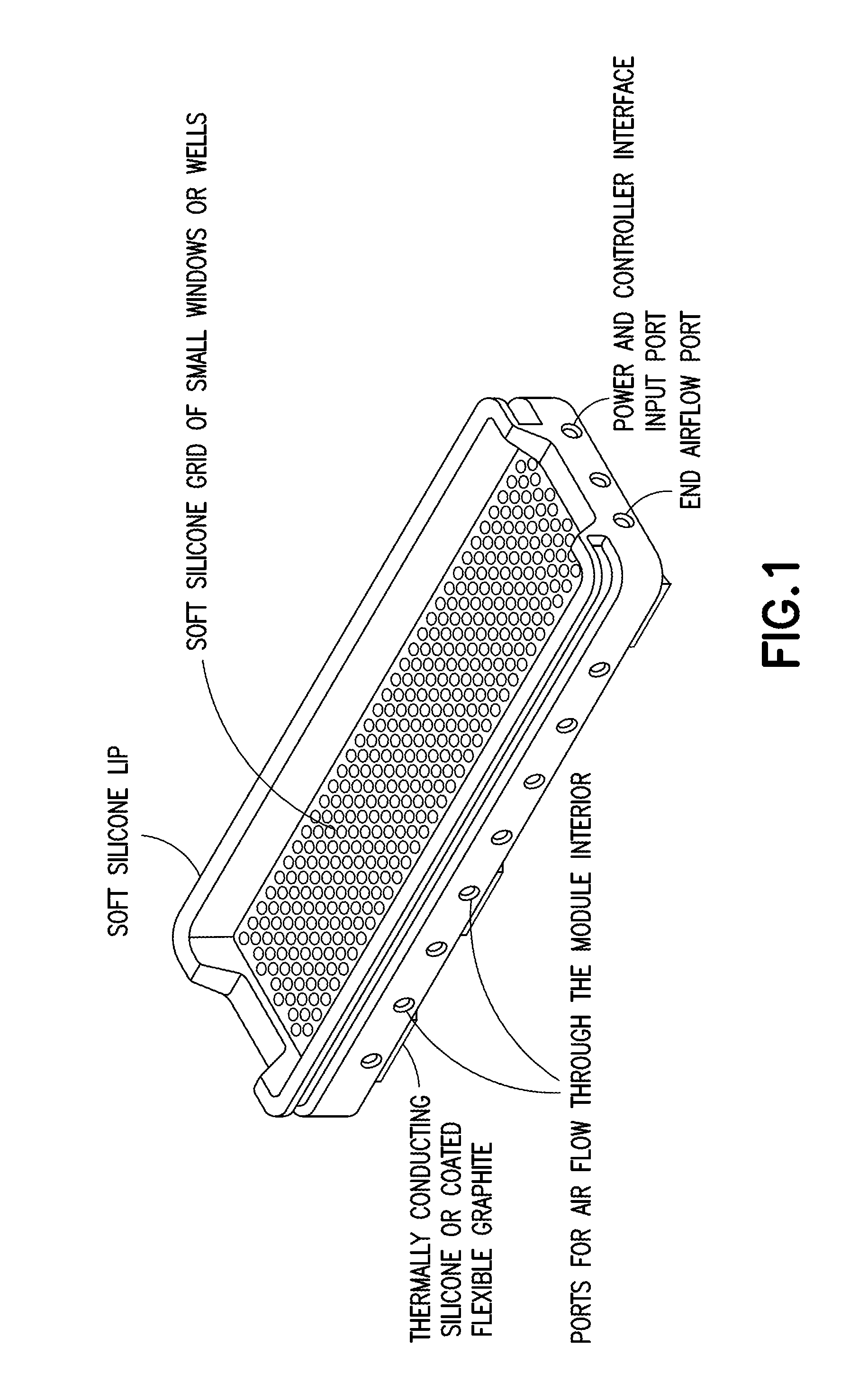
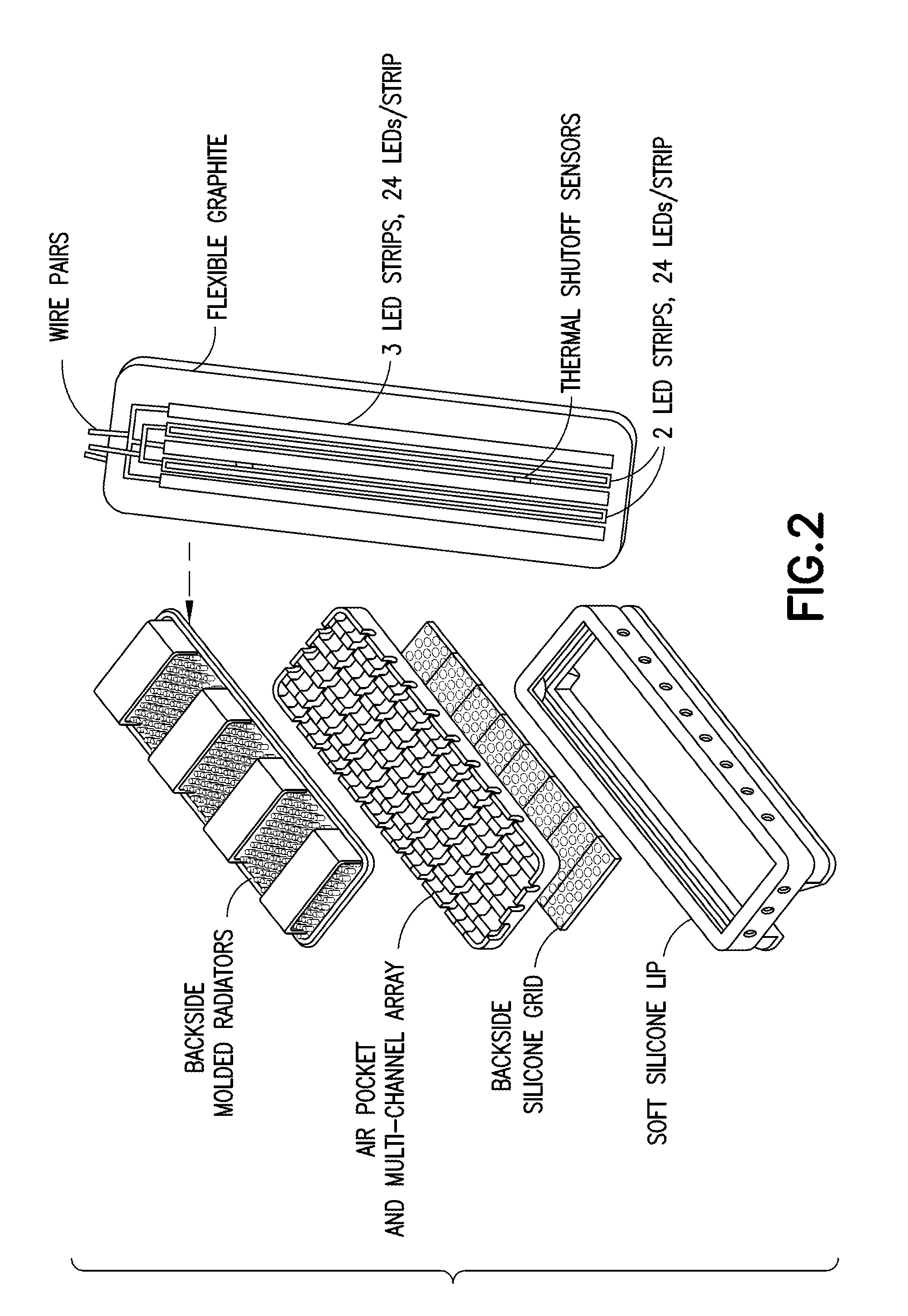
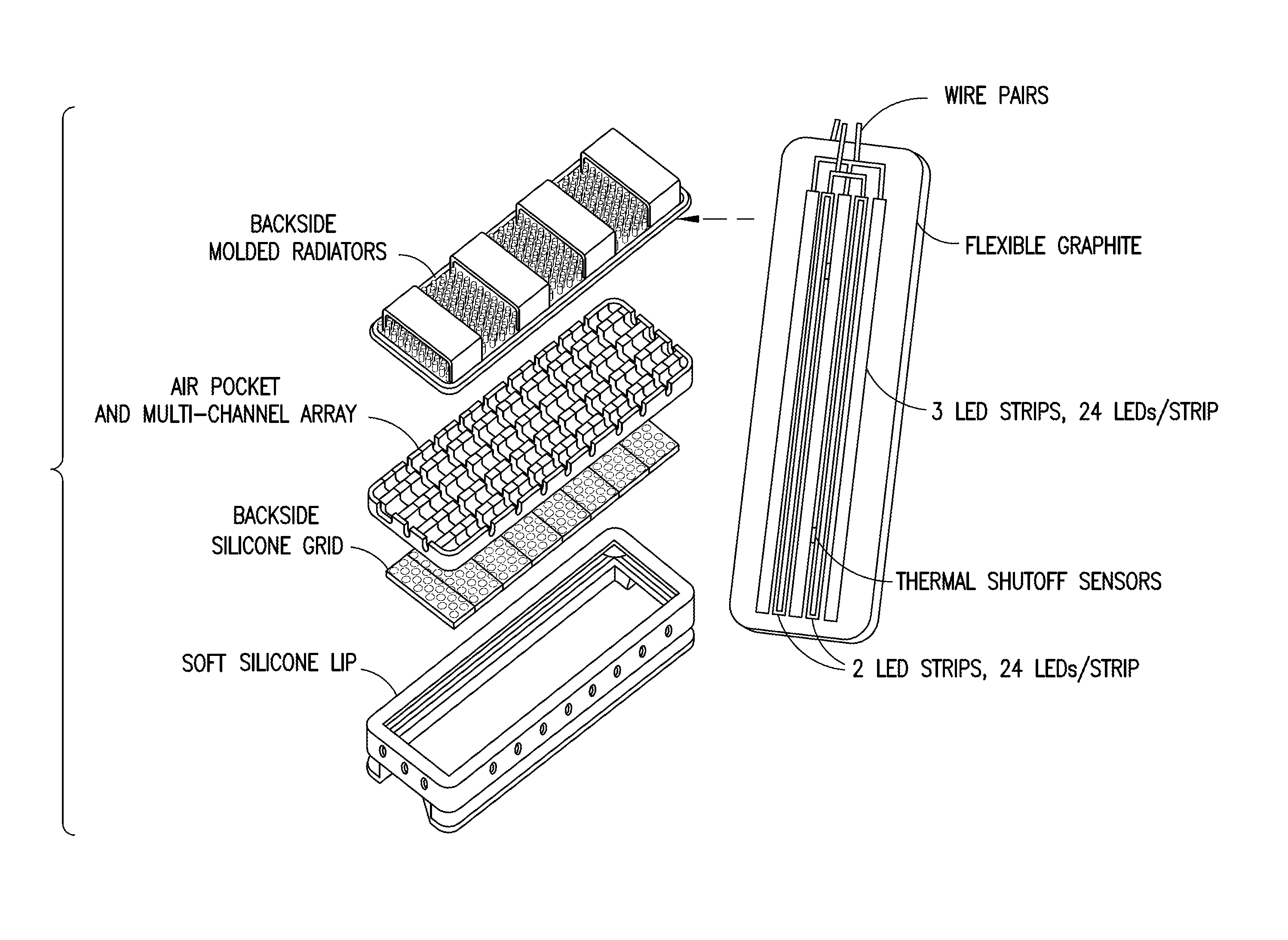
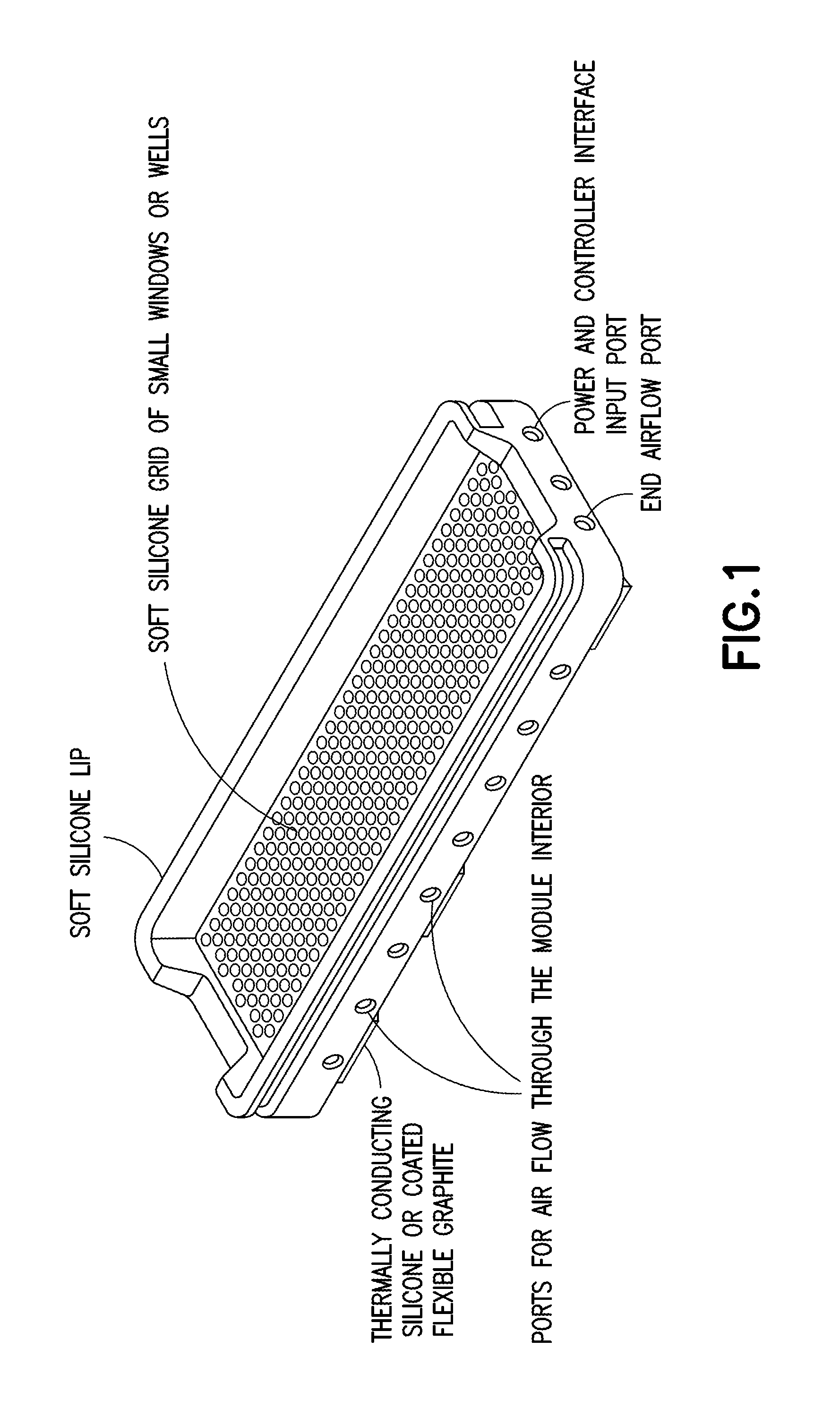
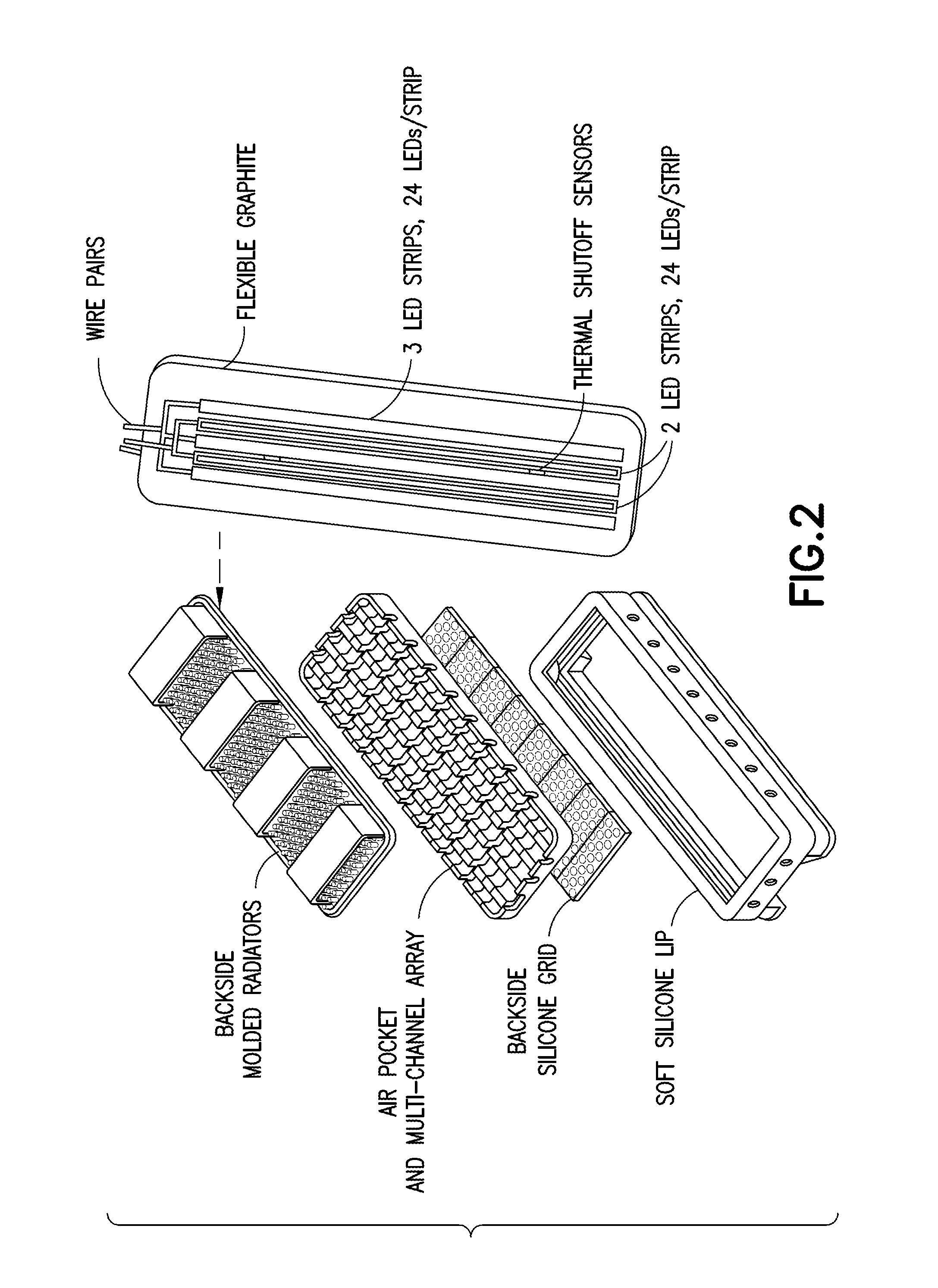
Multispectral therapeutic light source
ActiveUS20140288351A1High cost-effectiveHigh quantum-efficiencyElectrotherapySurgeryUltravioletPeak value
A light source apparatus including light spectrum-converting materials that emit light primarily over large portions of the 360 nm-480 nm and the 590-860 nm spectral range is provided. This apparatus provides a cooled, high-luminance, high-efficiency light source that can provide a broader spectrum of light within these spectral ranges than has been cost-practical by using many different dominant peak emission LEDs. Up to 15% of the output radiant power may be in the spectral range 350-480 nm in one embodiment of this device, unless a specific separate source and lamp operating mode is provided for the violet and UV. Control methods for light exposure dose based on monitoring and controlling reflected or backscattered light from the illuminated surface and new heat management methods are also provided. This flexible or rigid light source may be designed into a wide range of sizes or shapes that can be adjusted to fit over or around portions of the bodies of humans or animals being treated, or mounted in such a way as to provide the special spectrum light to other materials or biological processes. This new light source can be designed to provide a cost-effective therapeutic light source for photodynamic therapy, intense pulsed light, for low light level therapy, diagnostics, medical and other biological applications as well as certain non-organic applications.
Owner:JONES GARY W
Methods useful for remodeling maxillofacial bone using light therapy and a functional appliance
Methods are provided for regulating bone remodeling or tooth movement, comprising allowing a functional appliance to exert a force on oral or maxillofacial bone, muscle, or soft tissue, or one or more teeth of a patient in need thereof; and administering an effective amount of light to the oral or maxillofacial bone, muscle, or soft tissue, or one or more teeth, wherein the light is administered before, during, or after the force is exerted. Methods are also provided for regulating bone remodeling, comprising administering an effective amount of vitamin D to an oral or maxillofacial bone, muscle, or soft tissue, or to one or more teeth of a patient in need thereof; and administering an effective amount of light to the oral or maxillofacial bone, muscle, or soft tissue, or to the one or more teeth. Apparatuses useful for providing light therapy and / or vitamin D is also provided.
Owner:BIOLUX RES HLDG INC +1
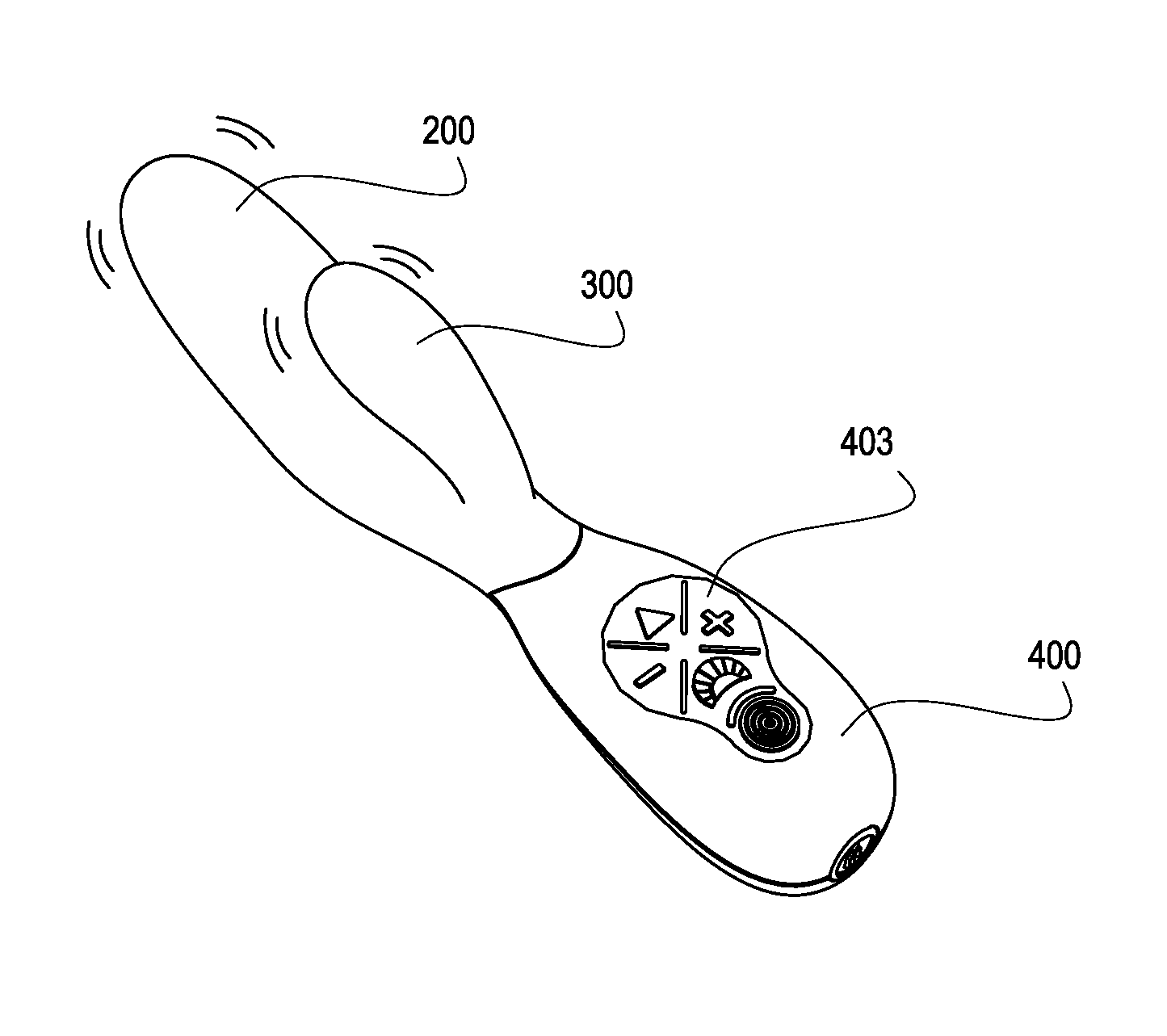
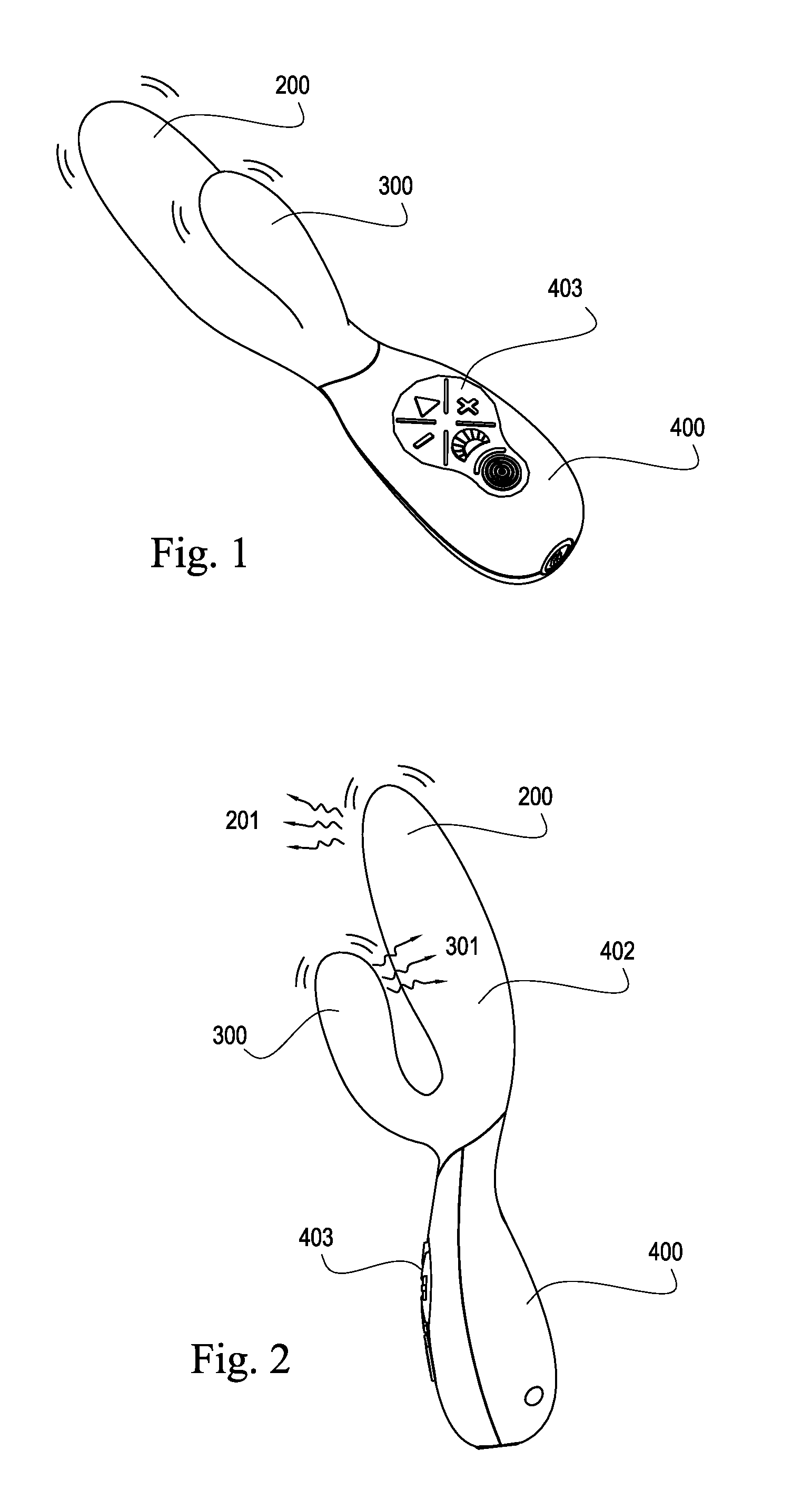
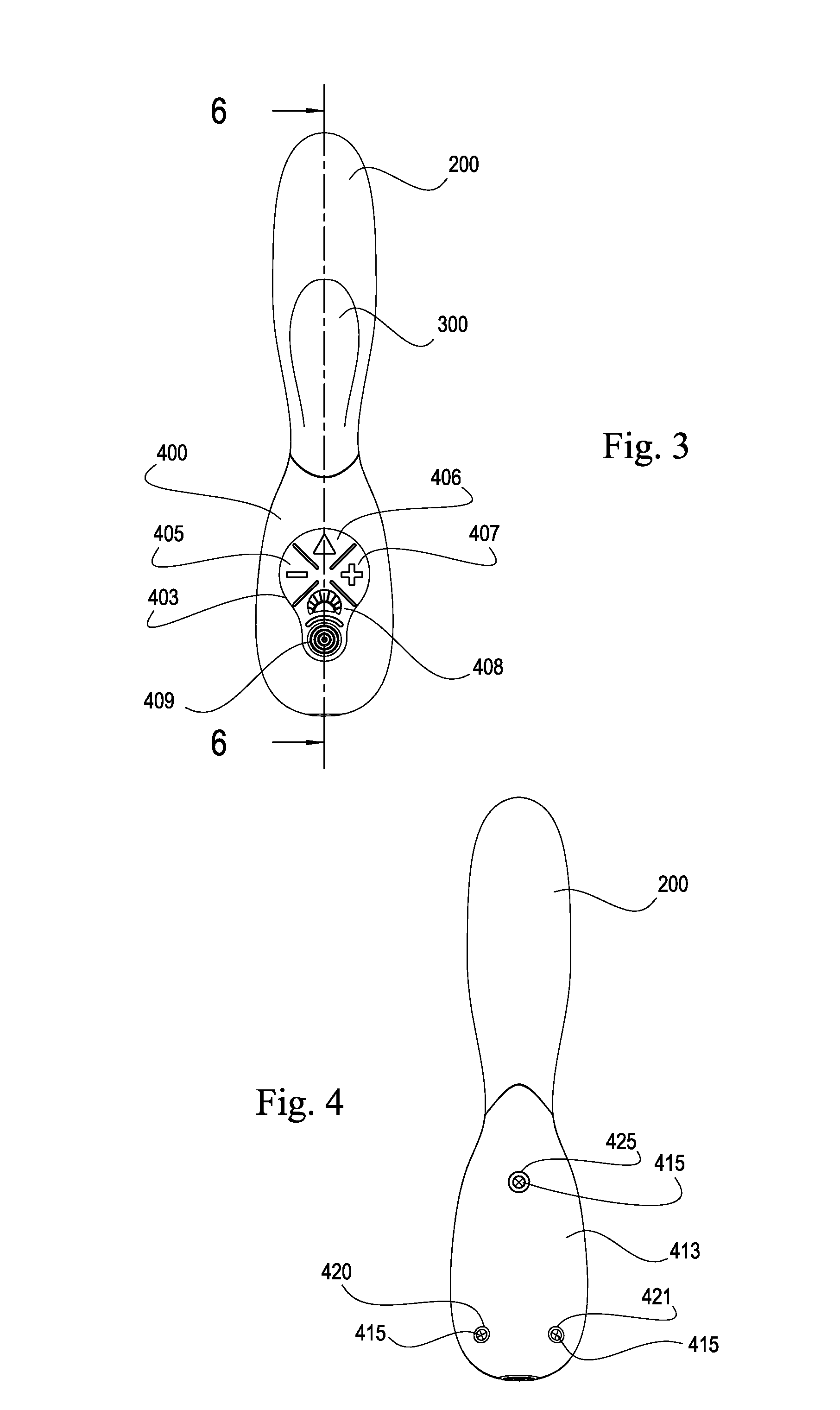
Sexual stimulation device using light therapy
ActiveUS20130261385A1Improve performance experienceImprove stimulation effectChiropractic devicesVibration massageMechanical irritationLight therapy
A sexual stimulation apparatus which may comprise a plurality of light sources for photostimulation and microbe reduction of the vagina, clitoris, or both; a plurality of vibrators for mechanical stimulation of the vagina, clitoris, or both; a plurality of modes of operation for achieving improved sexual stimulation in a user; a handle for ease of operation; a controller and programmable memory for containing modes of operation and driving the light sources and vibrators of the invention; a vaginal finger; a clitoral finger; a handle for ease of use; a keypad for user entry of commands; a charging and programming port; and a power source which may be a rechargeable battery which may be rechargeable by direct, inductive or other means; and a handle for ease of operation. The invention also comprises a flexible covering that provides smooth sliding engagement with the vagina and clitoris of a user.
Owner:ZIPPER RALPH
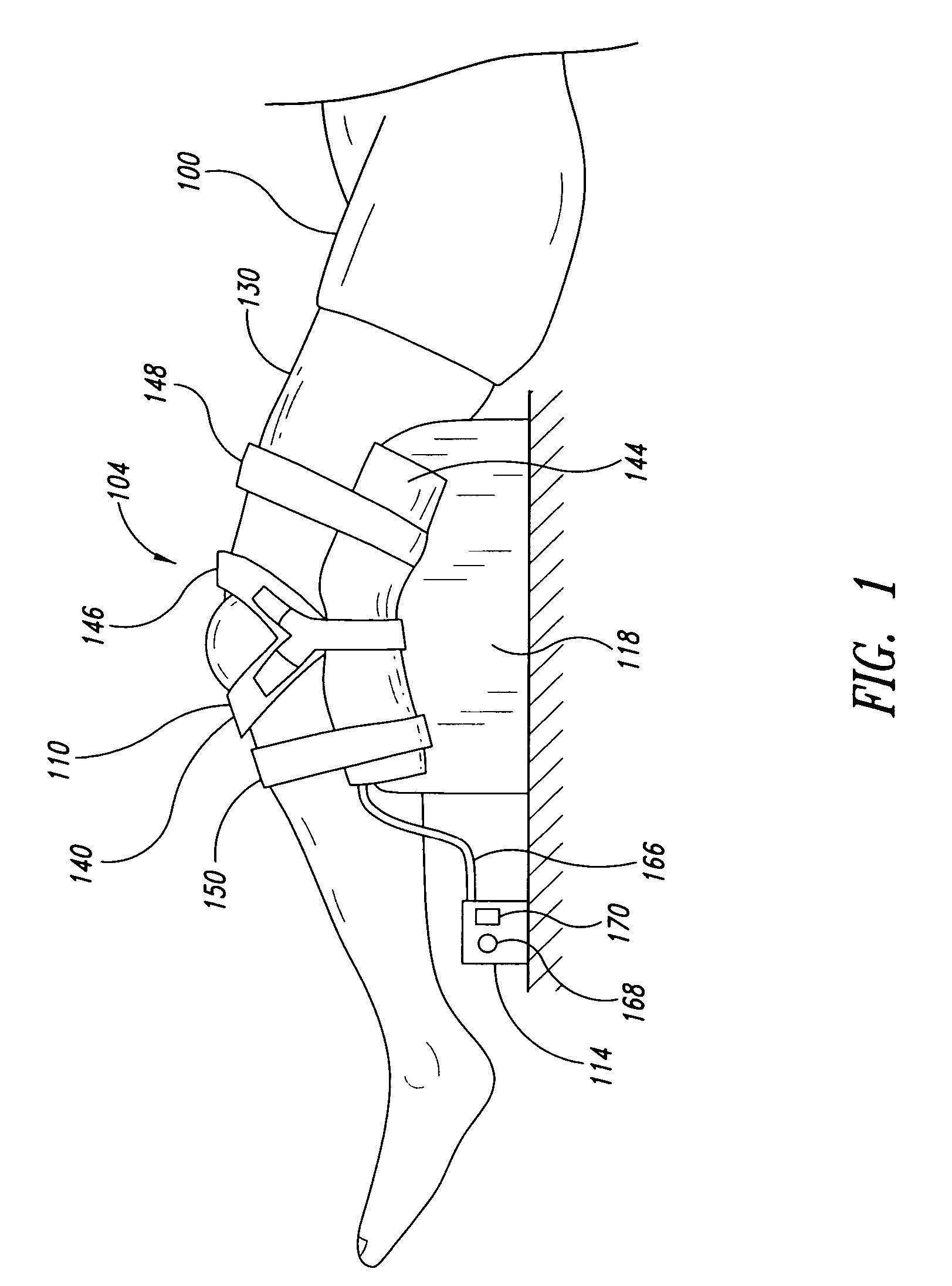
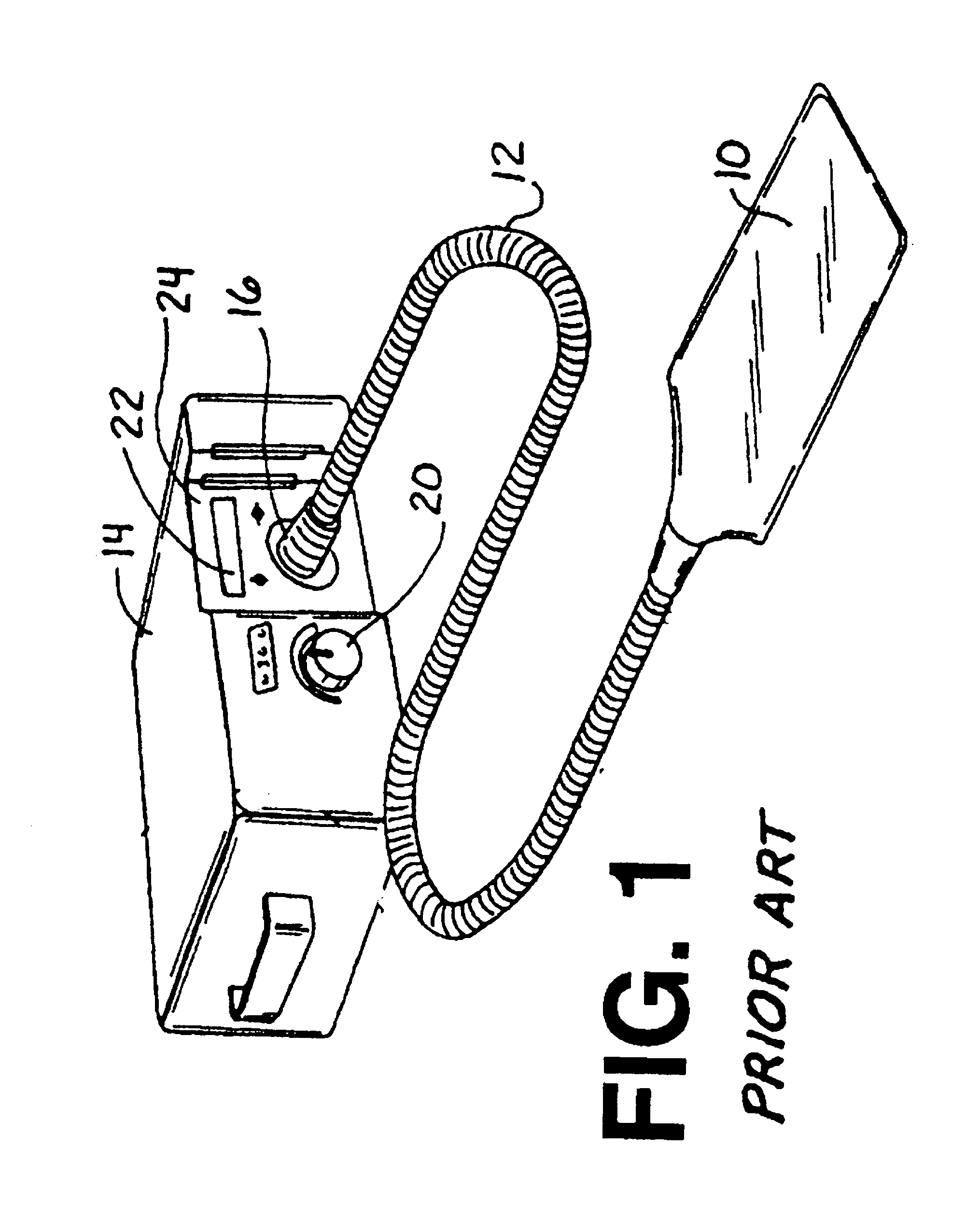
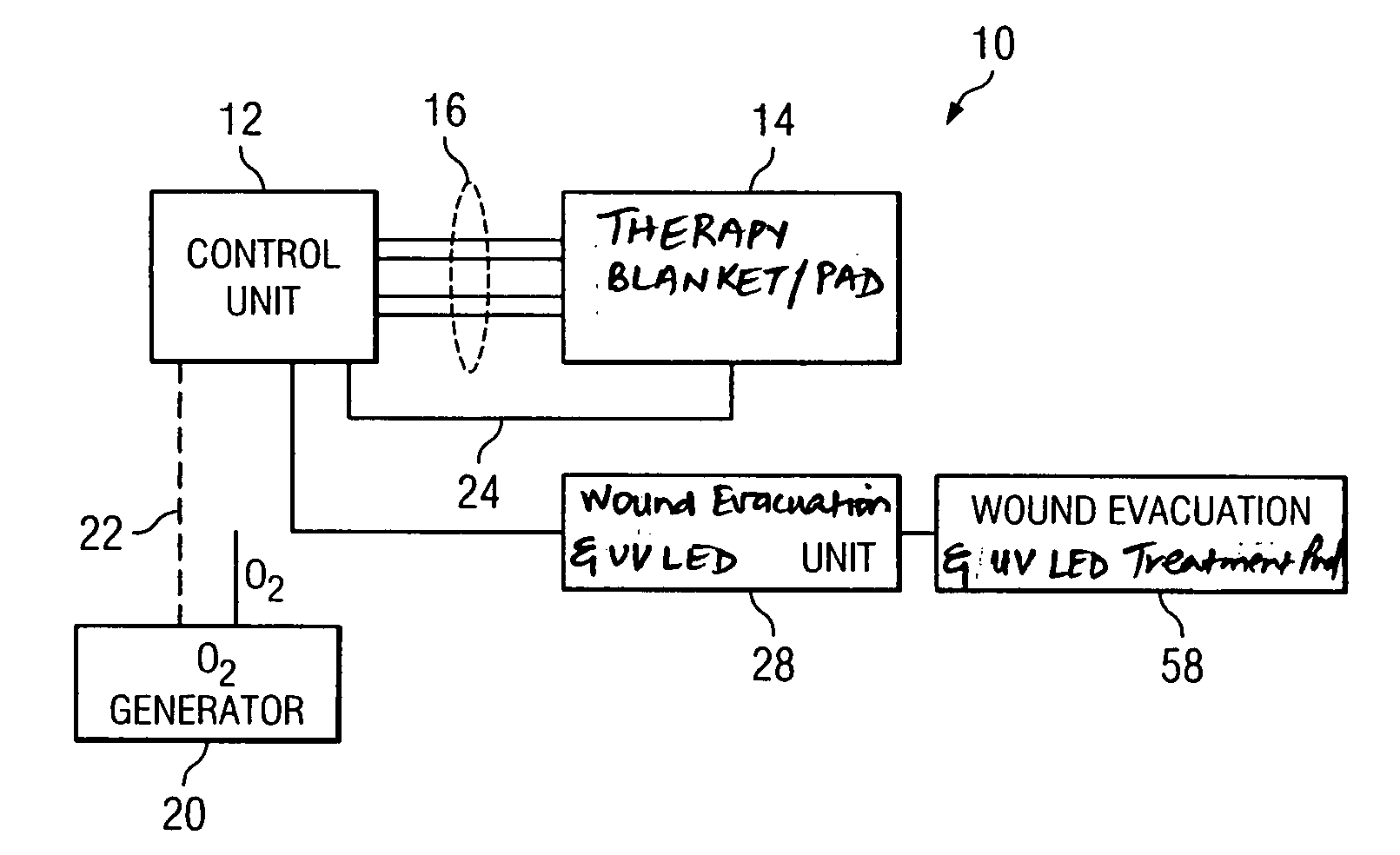
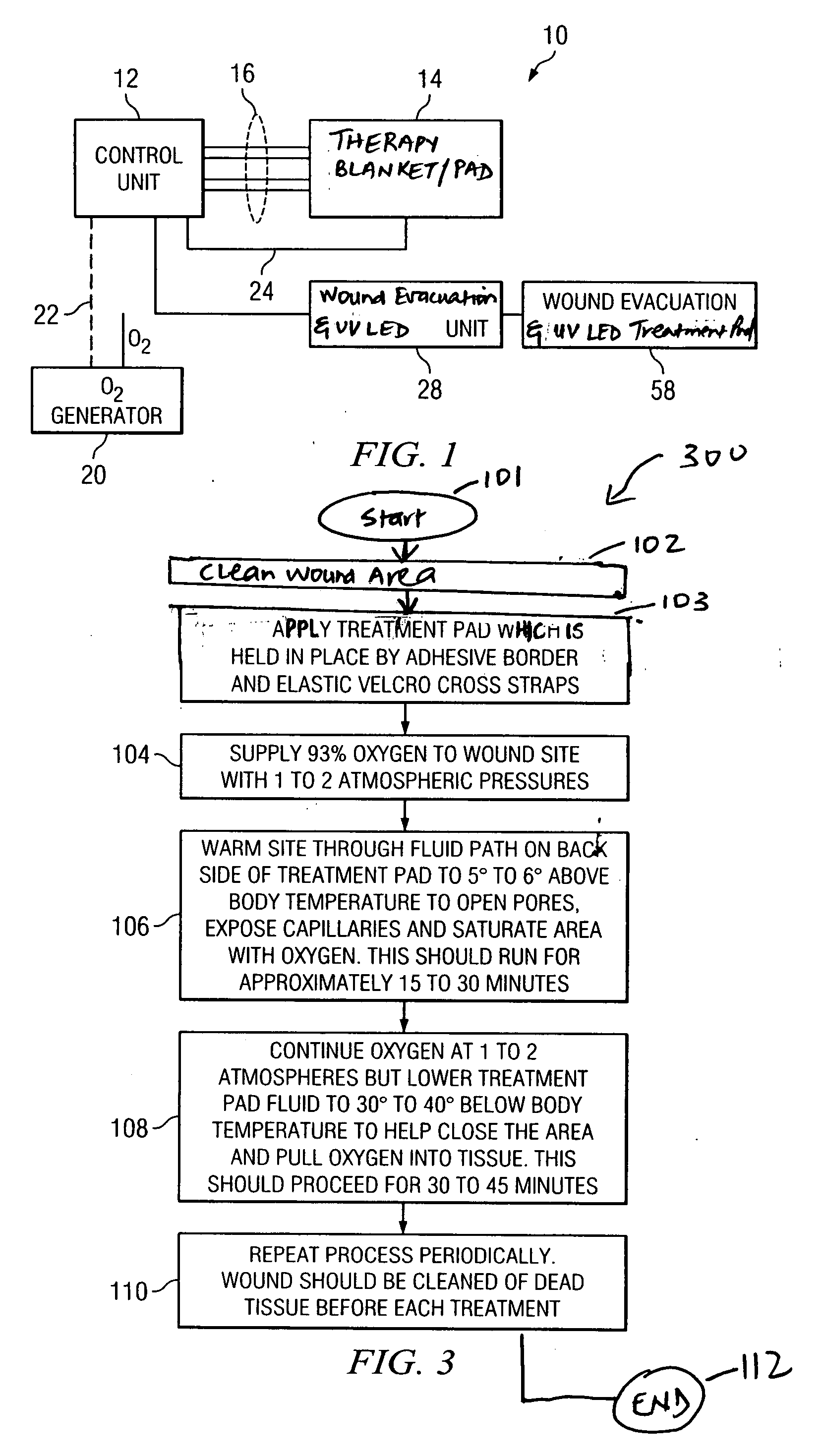
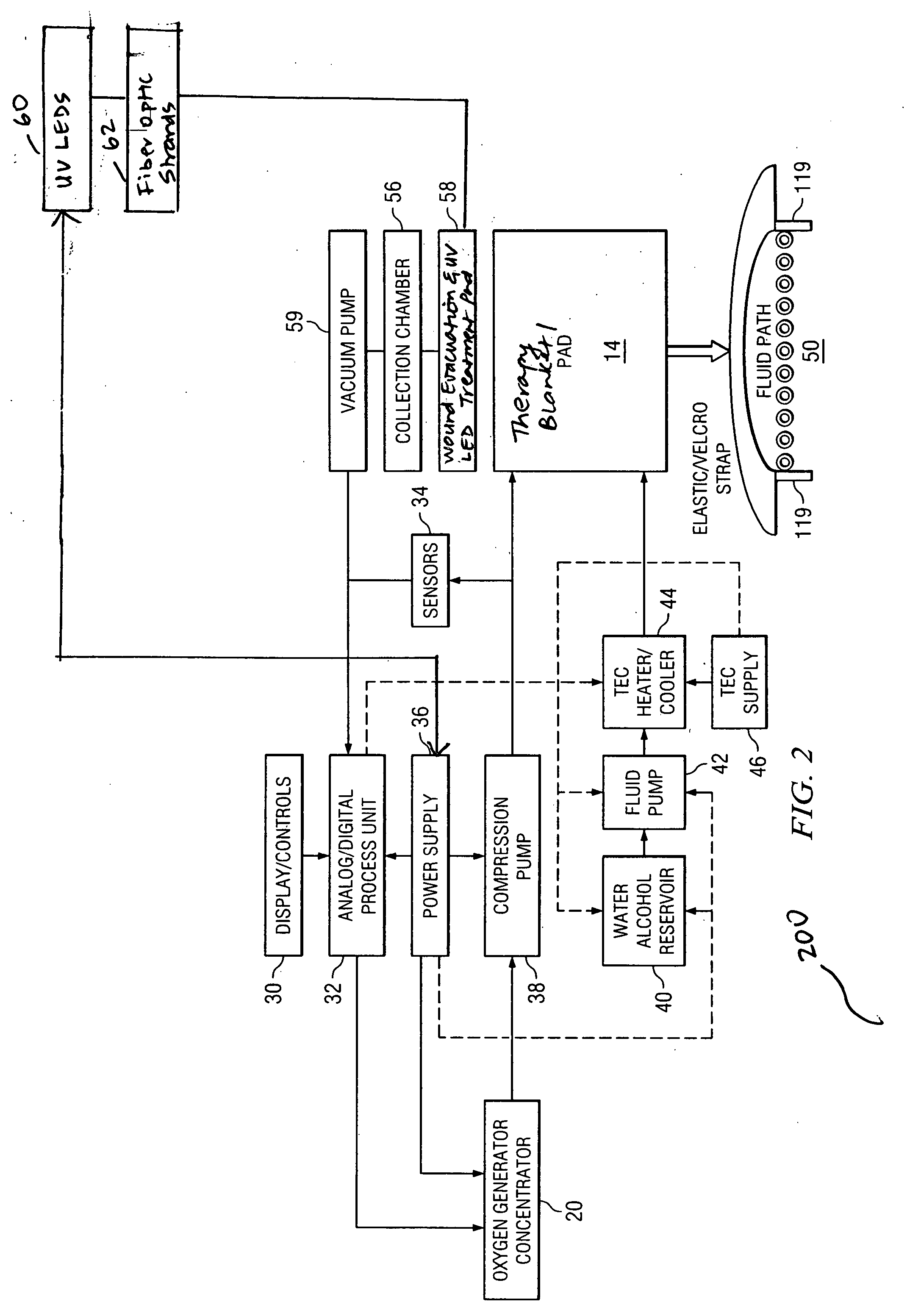
Wound care method and system with one or both of vacuum-light therapy and thermally augmented oxygenation
ActiveUS20080071330A1High saturationEasy to receivePneumatic massageDiagnosticsLight therapyWound care
A system for treatment of a wound area of a patient including a first treatment pad comprising a plurality of Light Emitting Diodes (LEDs) for cleaning and exposing a wound area to ultraviolet light, a second treatment pad comprising removal ports for exposing the wound area to a negative pressure, and a control unit interoperably connected to the first and second treatment pads for providing a negative pressure and the ultraviolet light to the wound area.
Owner:THERMOTEK
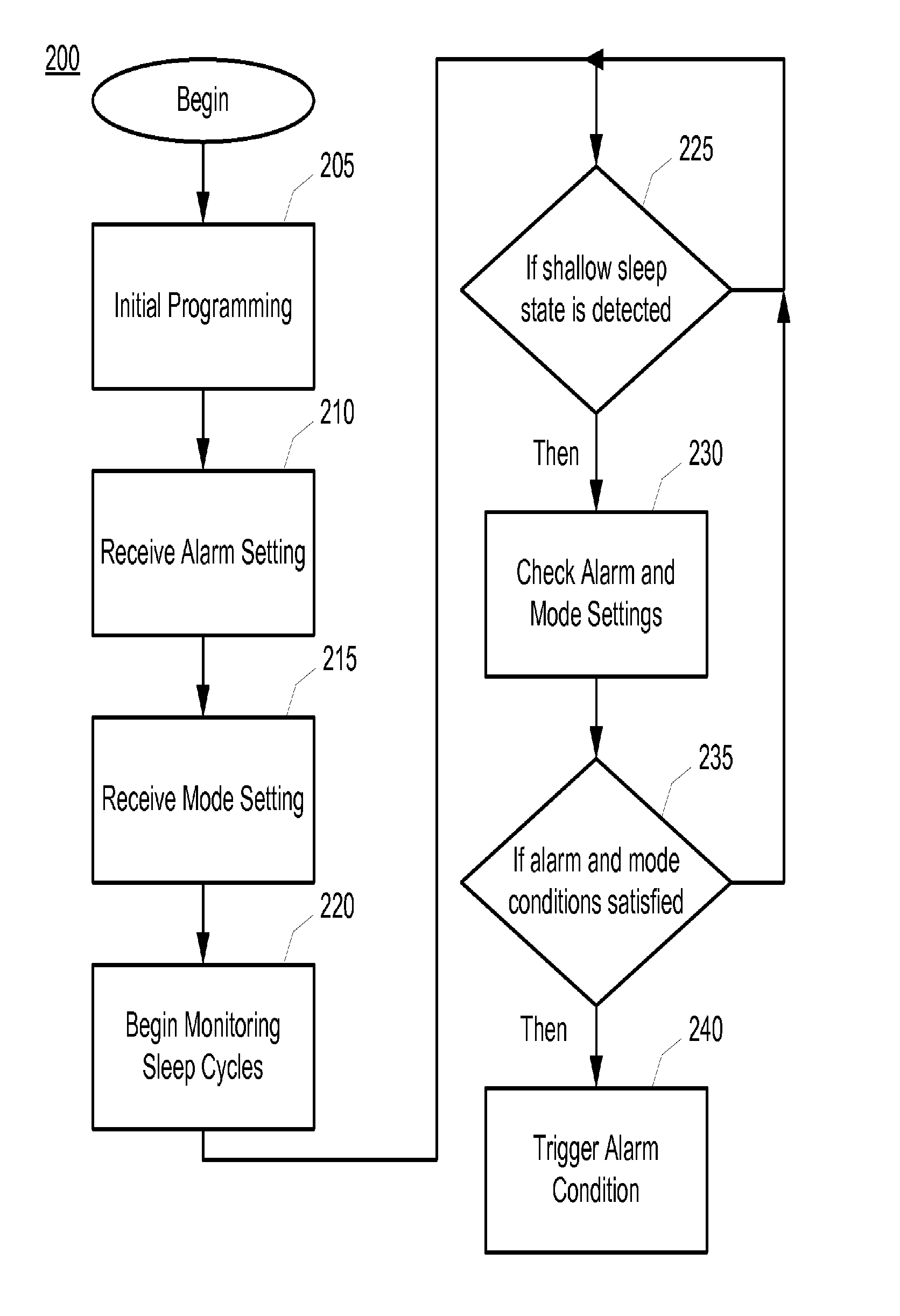
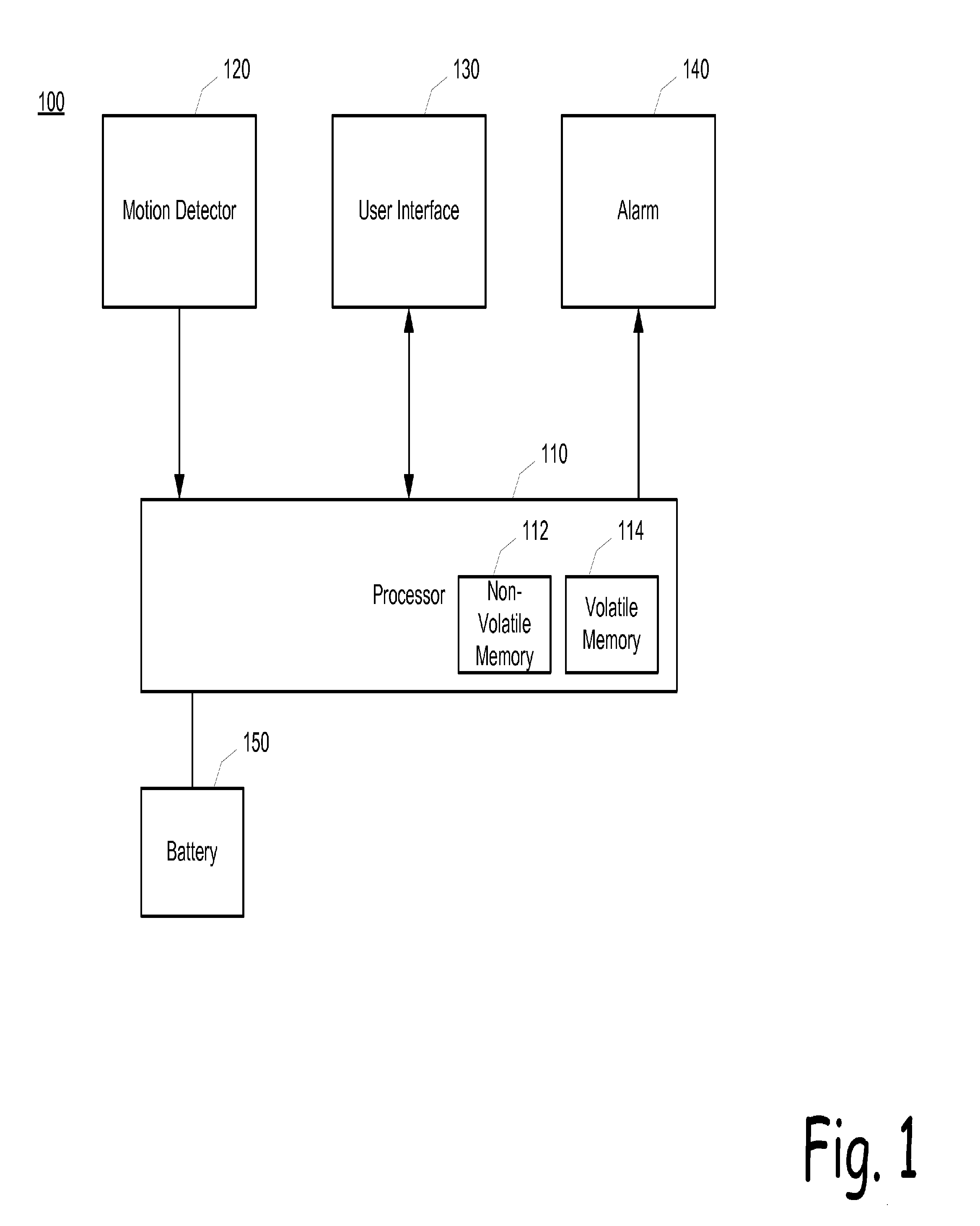
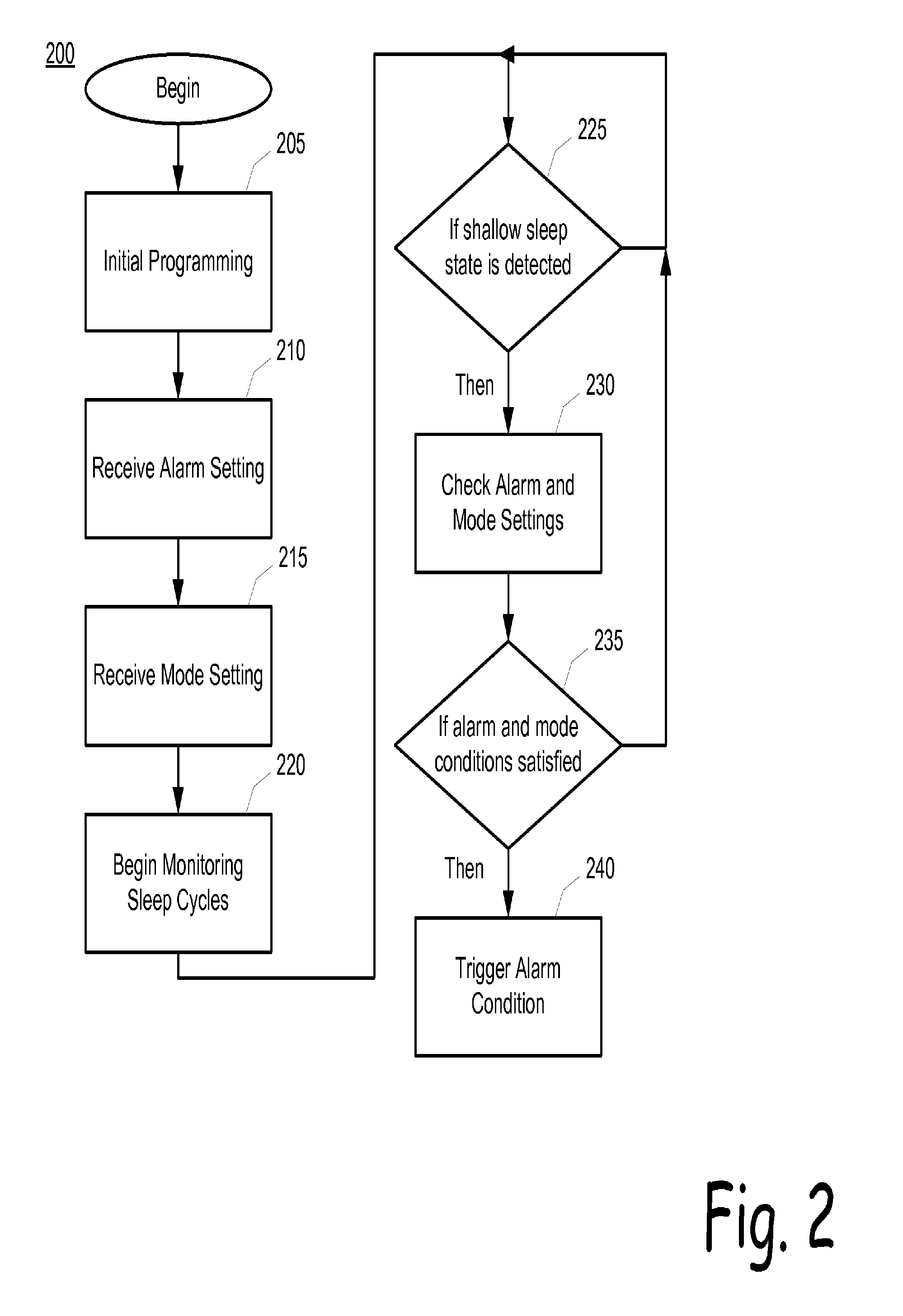
Easy wake device
A device that monitors a user's sleep cycles and operates to sound an alarm to awaken the user at an optimal point within a sleep cycle. Once an alarm time is set and the alarm is activated, the device begins to monitor a wearer's sleep cycles by identifying the points in time at which the wearer moves his or her body limbs. As the alarm time is approached, the device can trigger the alarm earlier if the wearer is at an optimal point in the sleep cycle or, even retard the triggering of the alarm if the optimal point in the sleep cycle is expected to occur shortly. The device can be used to assist children in waking up to prevent bed wetting, or in a patient for obtaining light therapy.
Owner:DP TECH
Intraoral light-emitting device
ActiveUS20070259310A1Improve expectationsIncreases safety of oral cavity light exposureDental toolsLight therapyWhitening AgentsCleansing Agents
The present invention relates to methods, systems, kits and devices that emit light to the oral cavity. The device includes a light source; a power source in electrical communication with the light source; and a bite actuated switch in electrical communication with the power source and the light source. The device is a size or shape that fits within an oral cavity of an individual. Since the device along with the light and power source are self contained, the user have their hands-free and can perform other activities while using the device. The device, methods, systems, and kits, further include the use of an agent (e.g., antibacterial agents, tooth whitening agents, cleaning agents) that assists or enhances the efficacy of the light therapy.
Owner:FORSYTH DENTAL INFARY FOR CHILDREN
Optical Therapy Devices, Systems, Kits and Methods for Providing Therapy to a body Cavity
An optical therapy device is disclosed. The optical therapy device provides therapeutic light therapy to a body cavity. The device includes a housing adapted to be hand held, a UV light source positioned in or on the housing, and an insertion member having a distal end configured to be inserted into the body cavity to illuminate tissue in the body cavity with light from the light source.
Owner:ALLUX MEDICAL INC
Light therapy device
InactiveUS6875225B1Small sizeSimple and durableLight therapySemiconductor devices for light sourcesLight therapyLight treatment
A light therapy device is taught including a light emitting assembly having light emitting diodes (LEDs) as a light source. The light emitting assembly capable of generating 2,500 lux to 7,500 lux at 12 inches.
Owner:THE LITEBOOK
Light therapy device
Owner:IDEAL LIVING HLDG
Method and Apparatus for Bi-Axial Light Treatment
A method and apparatus for providing light therapy using a biaxial flexible circuit substrate with infrared light-emitting diodes dispersed throughout the substrate, which is housed within a housing unit and has a transparent cover, a reflective layer and a means for connecting to a power source, is disclosed.
Owner:HAVELL DAVID +1
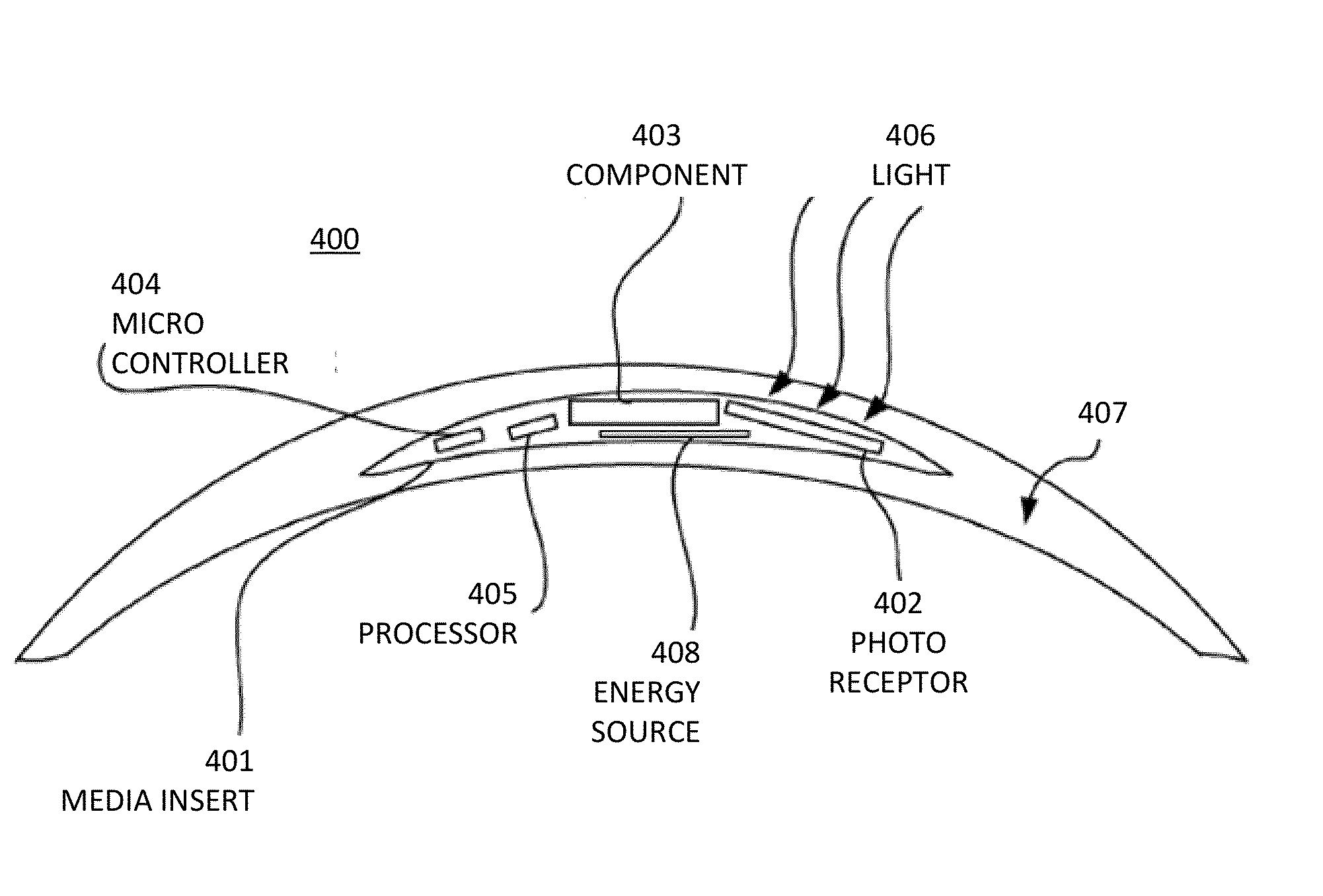
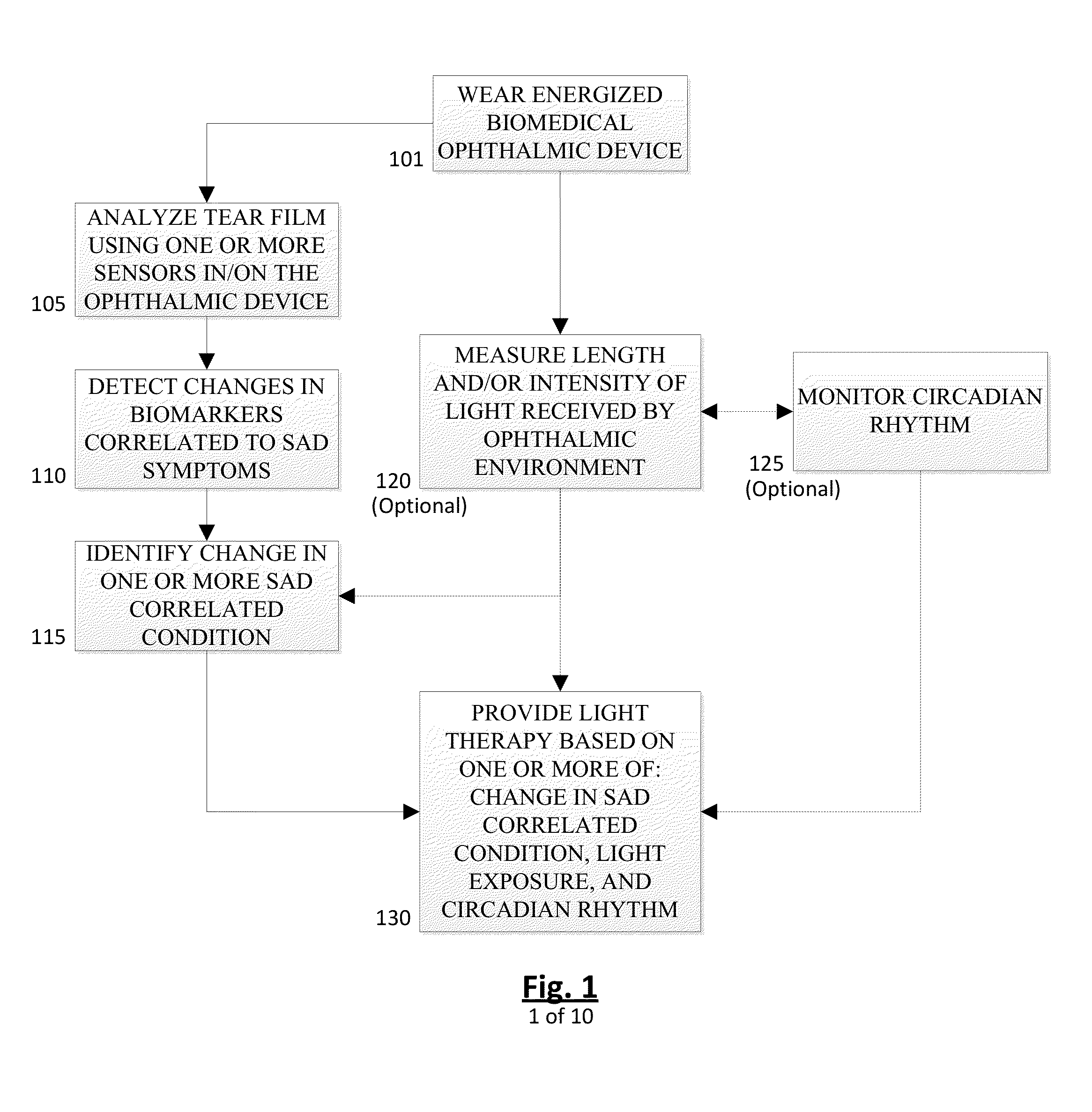
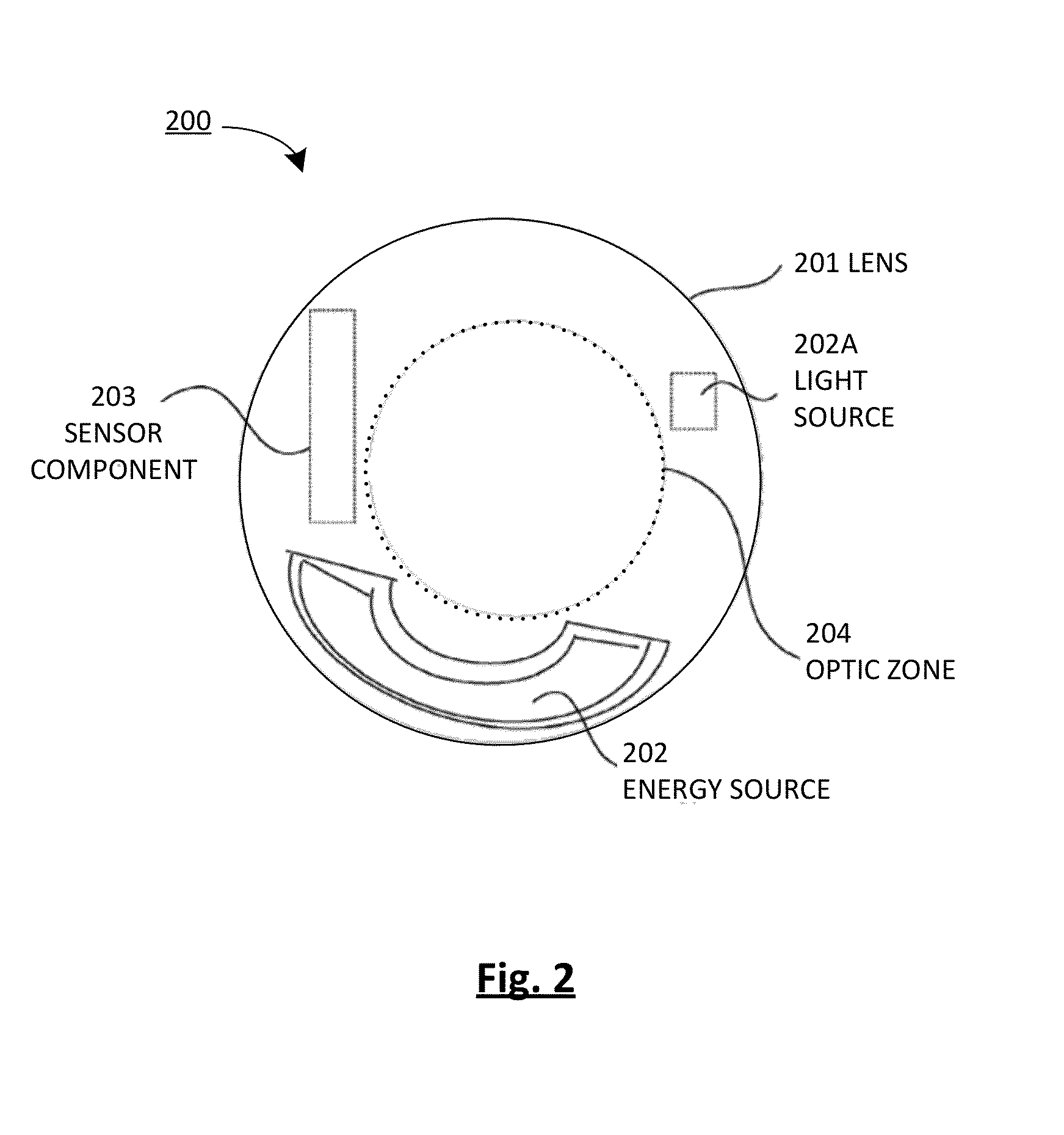
Method and device for monitoring and treatment of seasonal affective disorder
ActiveUS20140277291A1Effective treatmentPositive experienceSensorsLight therapyLight therapySeasonal Affective Disorders
This invention provides for an energized biomedical ophthalmic device and associated method of measuring changes in biomarkers contained in tear film to generate data related to a light therapy regimen used to treat symptoms associated with seasonal affective disorder. In some embodiments, the energized biomedical ophthalmic device can include an energized contact lens with a light source in communication with a processor controlling said light source according to the light therapy regimen. The light therapy regimen may be generated or modified by the processor from the measured changes and sometimes from user's preferences, and / or additional measurements, including for example, light exposure and / or circadian rhythm of the user.
Owner:JOHNSON & JOHNSON VISION CARE INC
Light therapy device
Owner:IDEAL LIVING HLDG
Multispectral therapeutic light source
ActiveUS8858607B1High cost-effectiveHigh quantum-efficiencyElectrotherapySurgical instrument detailsUltravioletPeak value
Owner:JONES GARY W
Light Therapy for Treating or Managing Diabetes and Metabolic Syndrome
Techniques for managing diabetes and pre-diabetes using light are disclosed herein. In one example, a light generating device is positioned to a body part of a diabetic or pre-diabetic patient, and a beam of light generated by the light generating device is directed to the body part of the patient to control blood sugar level of the patient. In various embodiments, the beam of light directed to the patient can also help to control the blood lipid level such as triglyceride level, blood liver enzyme of the patient, and various other symptoms of diabetes and pre-diabetes. In various embodiments, the body part includes body area rich in adipose tissue, such as the abdominal area, thigh, buttocks, and upper arms of the patient.
Owner:PRESCOTT MARVIN A
Microdermabrasion system with combination skin therapies
A microdermabrasion system offers a combination of other skin therapies in conjunction with microdermabrasion. In an implementation, the system applies light therapy, photodynamic therapy, radio frequency and microwave energy therapy, massage therapy, or combinations of these while exfoliating the skin.
Owner:ENVY MEDICAL
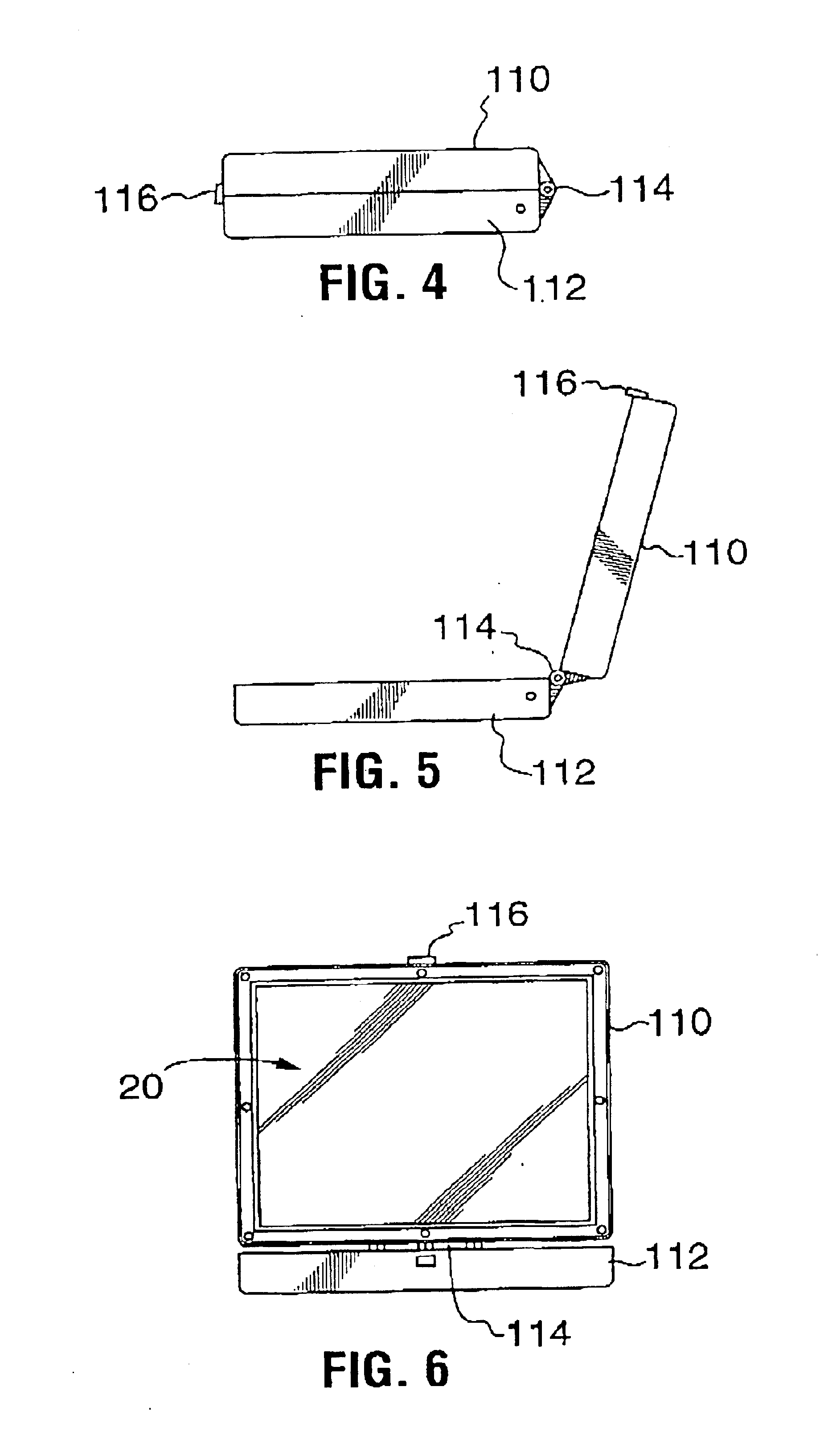
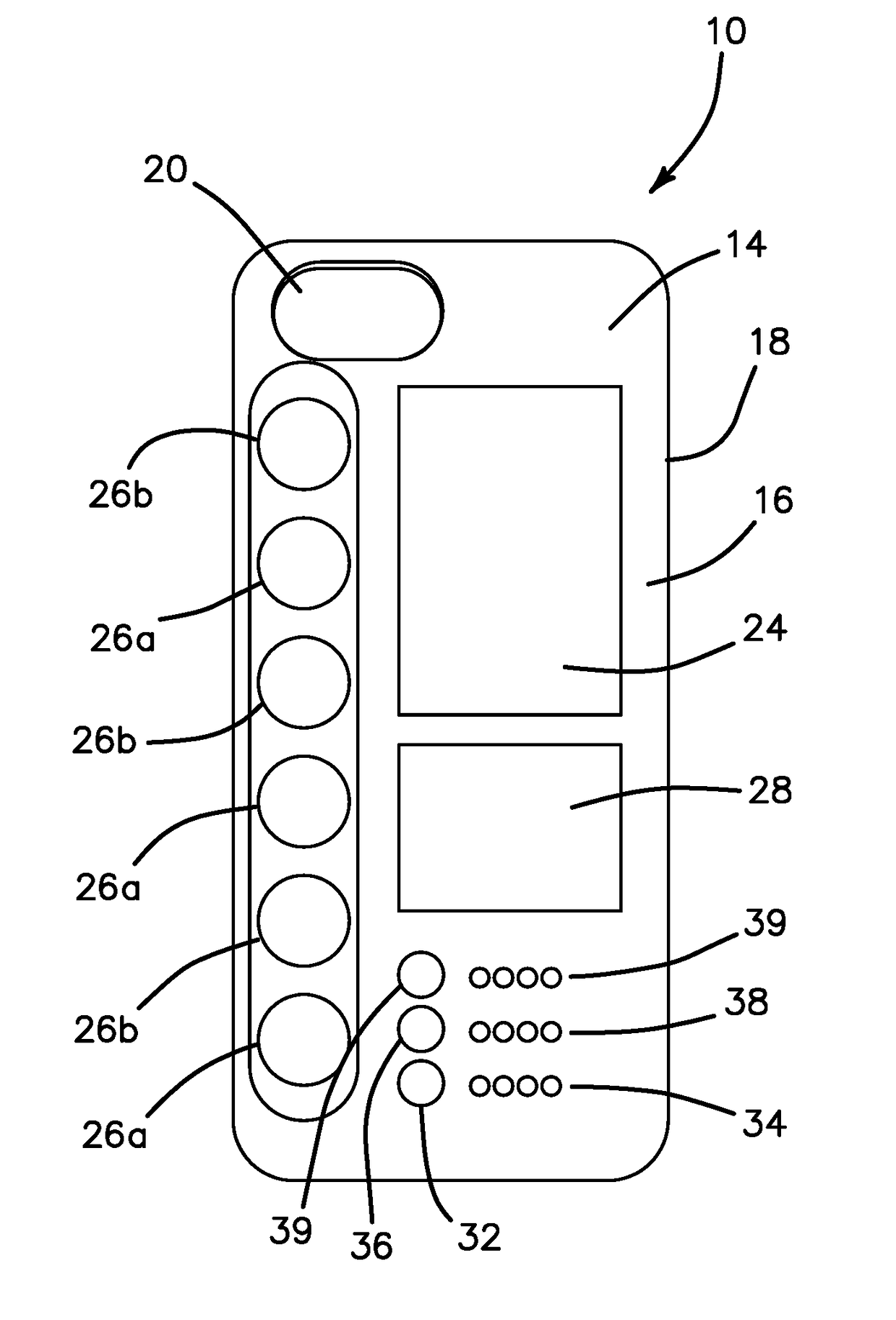
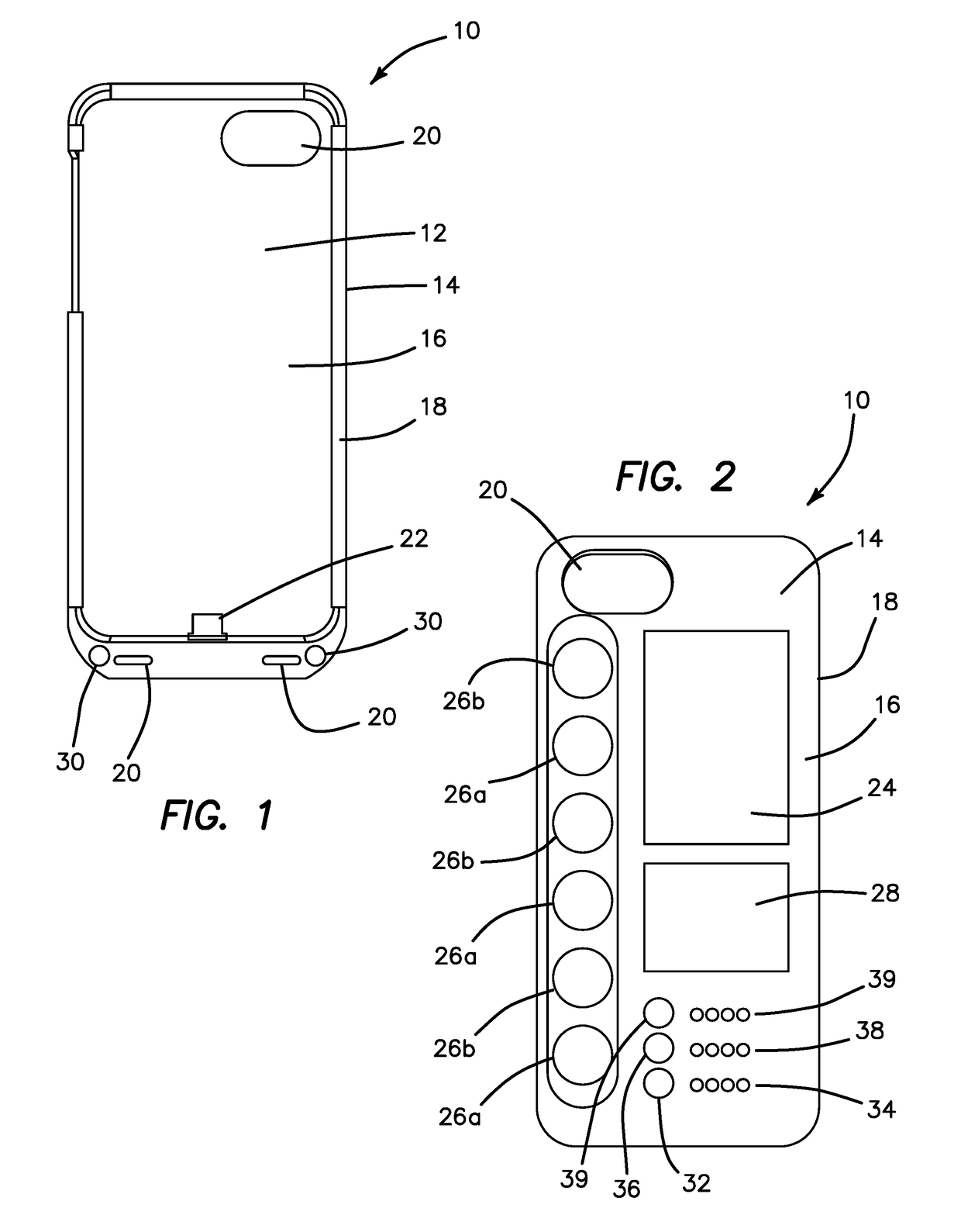
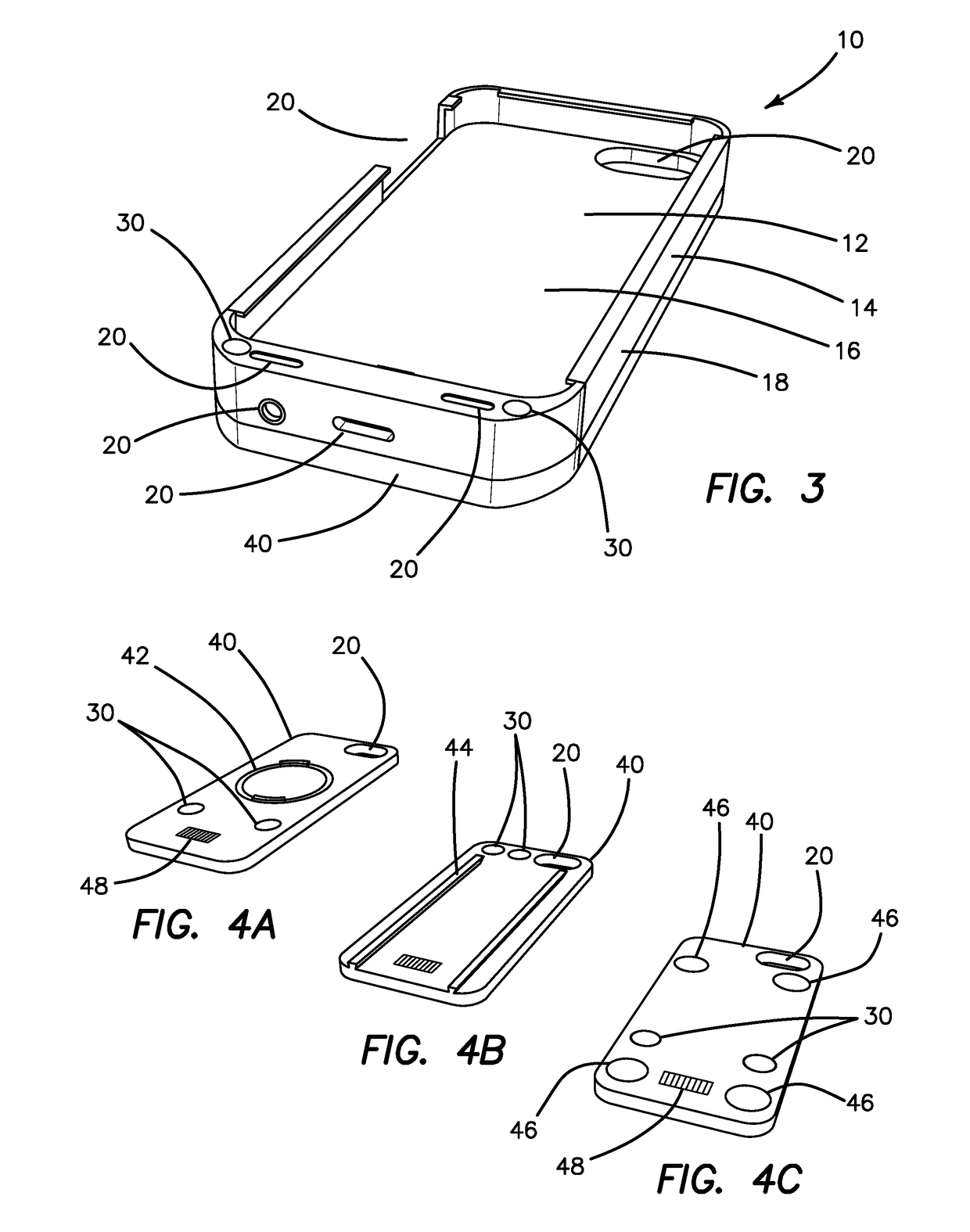
Mobile device case with ultraviolet light sanitizer and light therapy
A protective case for a mobile electronic device is provided. The case includes at least one light emitting diode that emits electromagnetic radiation in the range of UV-C light for sanitizing contaminated surfaces. The case also includes additional LEDs that emit light at wavelengths known to have a therapeutic effect such as a blue light for treating seasonal affective disorder. The LEDs are provided in a separate encasement that is detachable from the protective cover configured to receive and protect the mobile electronic device. A short-range wireless receiver is included to communicate with an application installed on the mobile electronic device for controlling the activation, intensity, duration and mode of the LEDs including predetermined treatment or sanitization protocols.
Owner:ETS TECH LLC
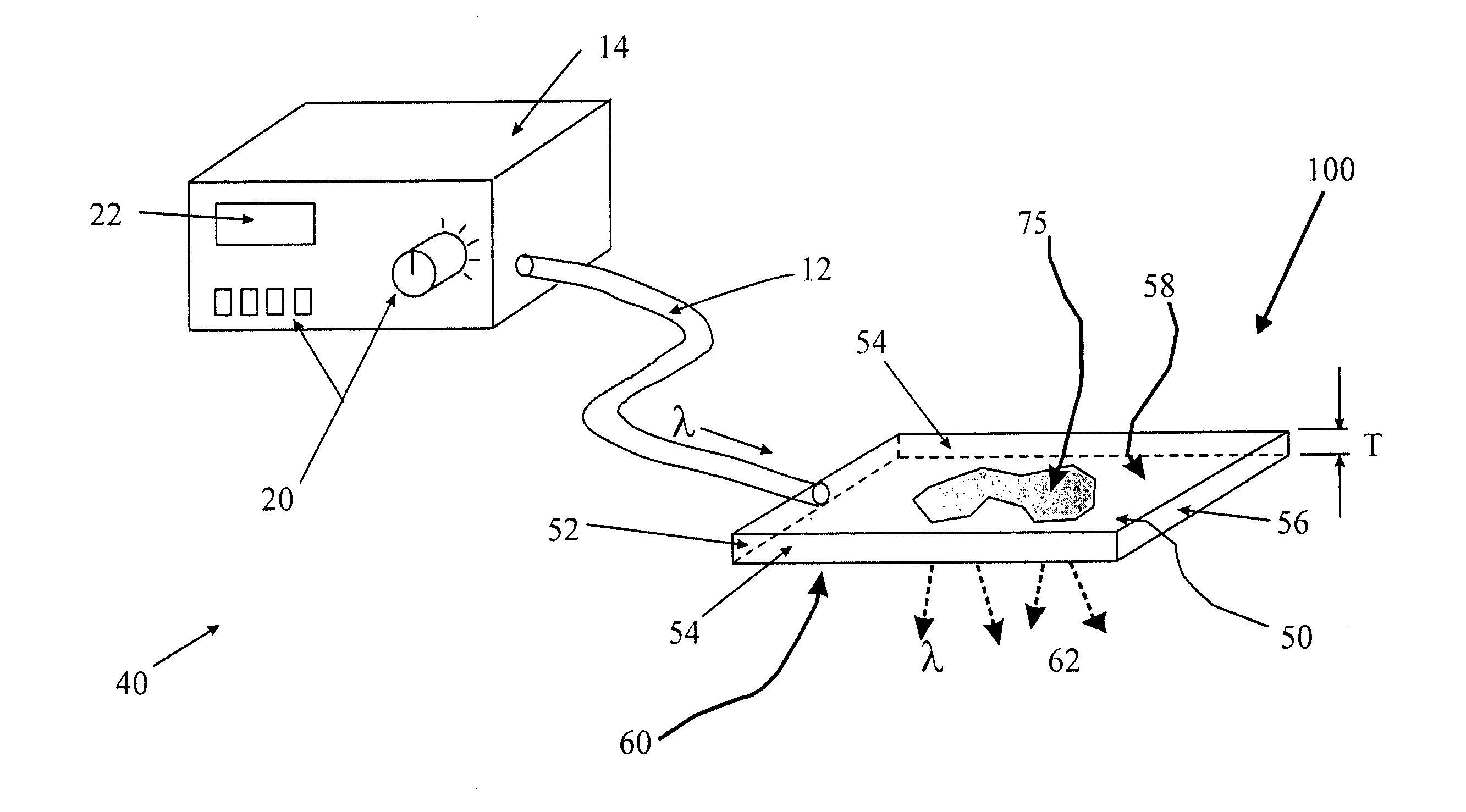
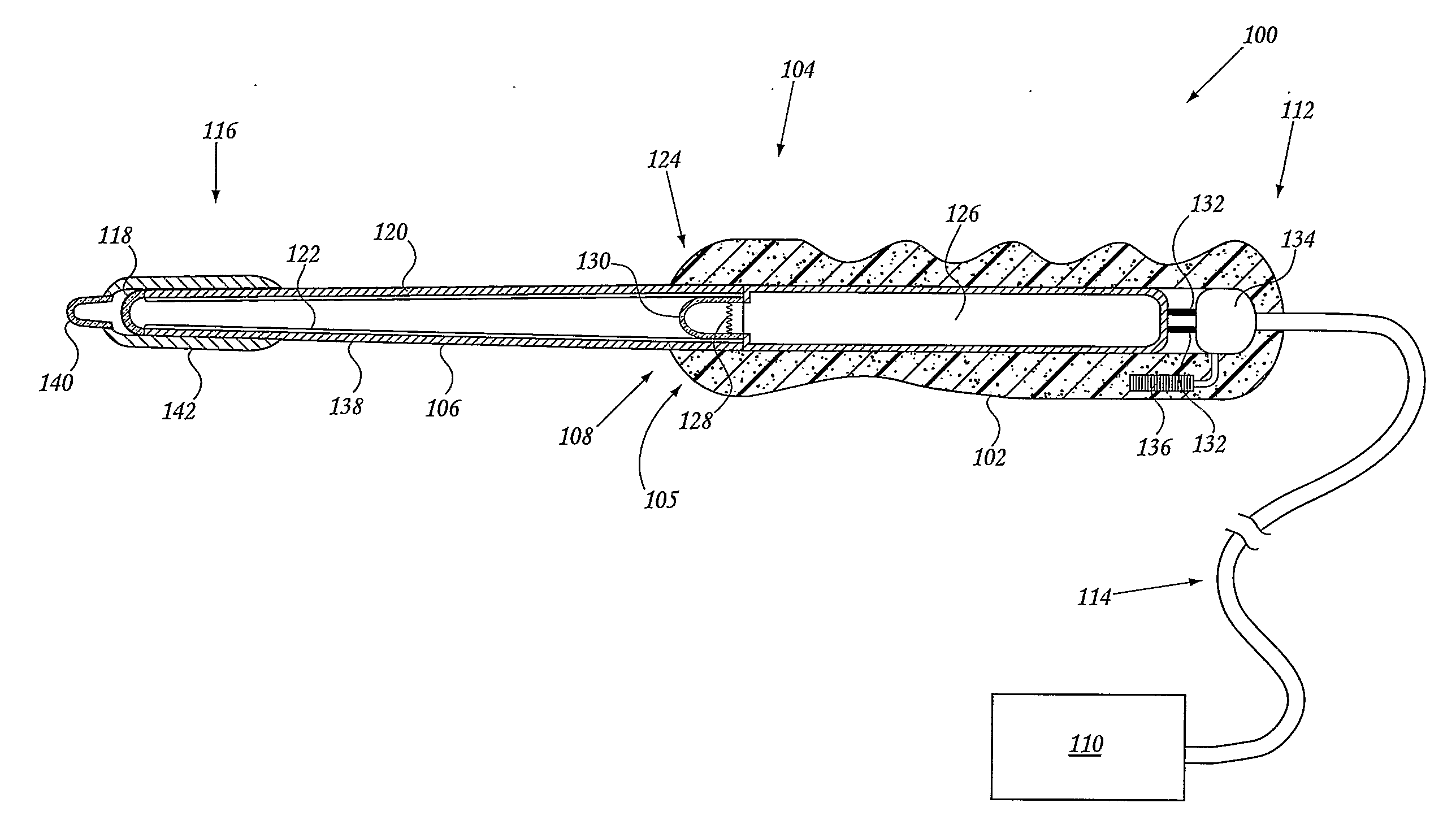
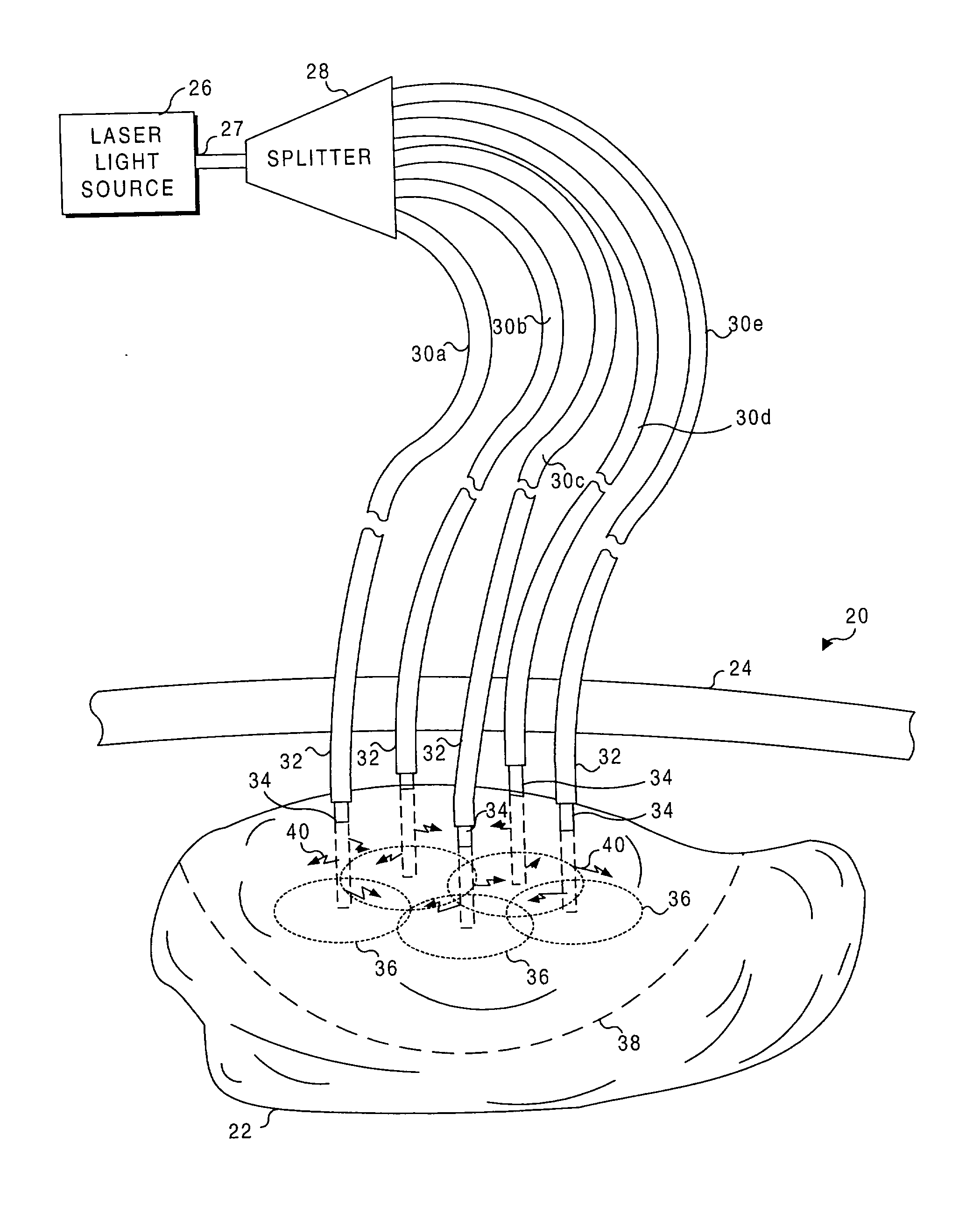
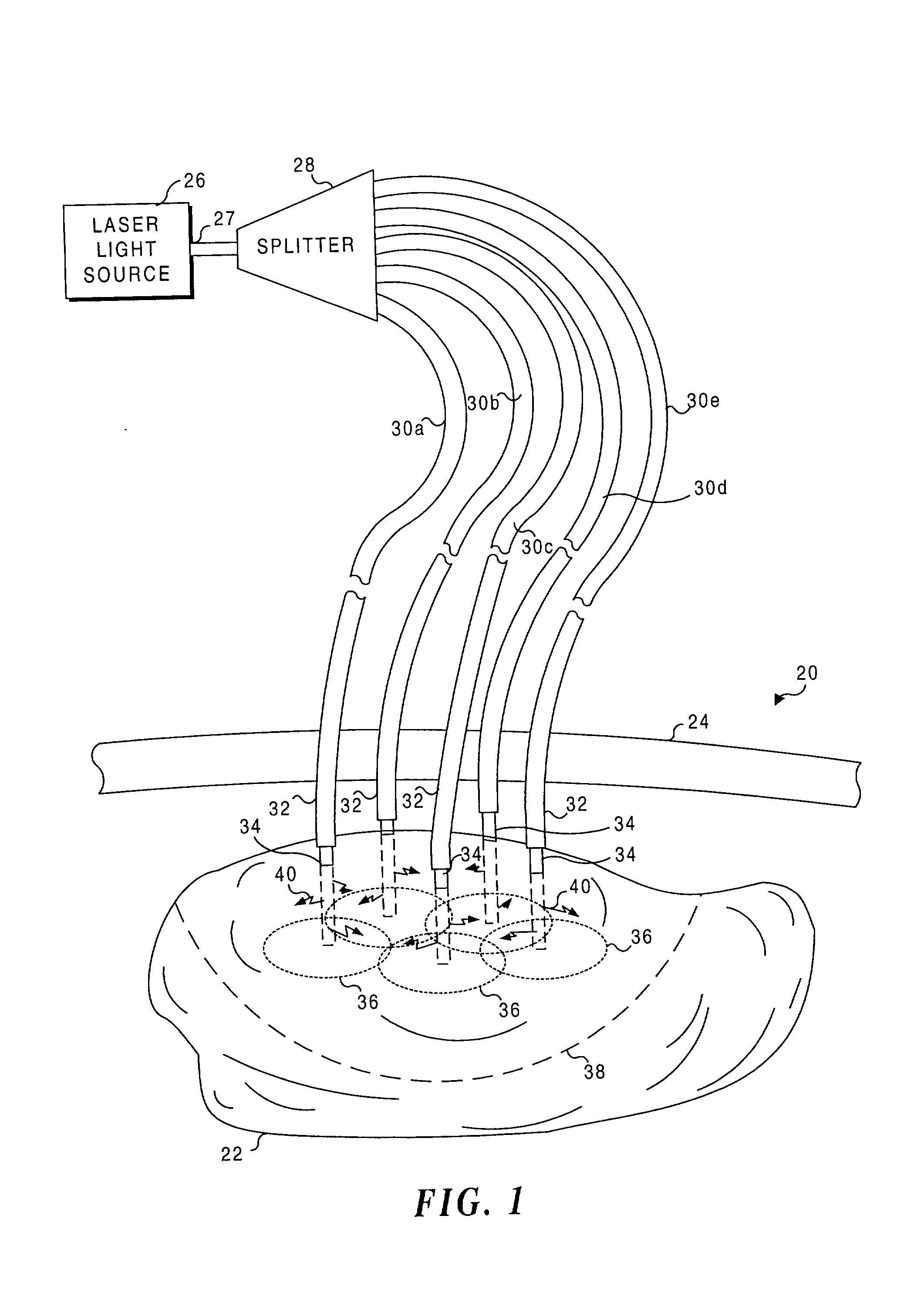
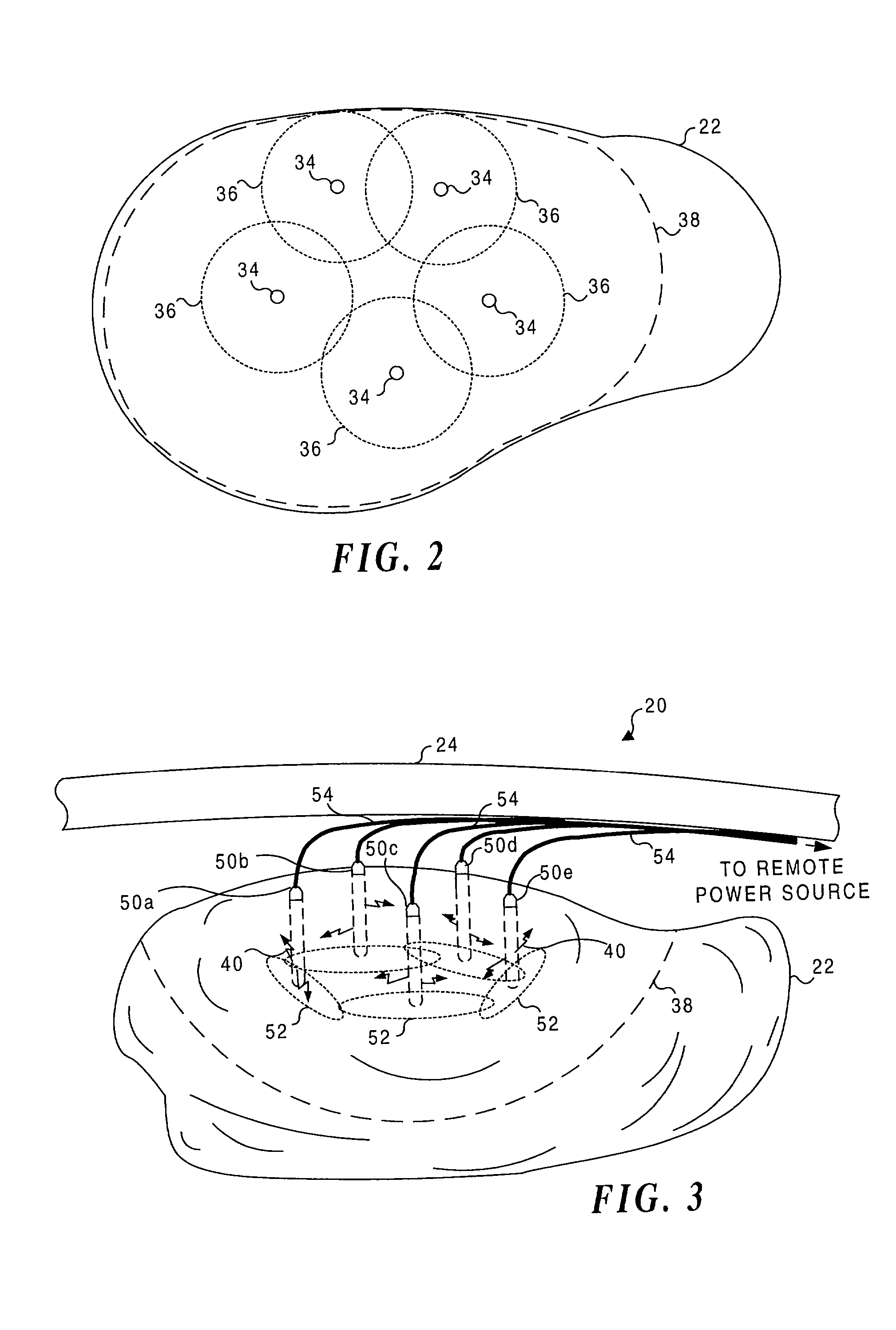
Application of light at plural treatment sites within a tumor to increase the efficacy of light therapy
Light is administered during photodynamic therapy (PDT) for an extended period of time at a plurality of sites distributed within the abnormal tissue of a tumor. A clinical study has shown that a substantially greater volume of abnormal tissue in a tumor is destroyed by the extended administration of light therapy from a plurality of probes than would have been expected based upon the teaching of the prior art. In this process, a plurality of light emitting optical fibers or probes are deployed in a spaced-apart array. After a photoreactive agent is absorbed by the abnormal tissue, the light therapy is administered for at least three hours. The greater volume of necrosis in the tumor is achieved due to one or more concomitant effects, including: the inflammation of damaged abnormal tissue and resultant immunological response of the patient's body; the diffusion and circulation of activated photoreactive agent outside the expected fluence zone, which is believed to destroy the abnormal tissue; a retrograde thrombosis or vascular occlusion outside of the expected fluence zone; and, the collapse of the vascular system that provides oxygenated blood to portions of the tumor outside the expected fluence zone. In addition, is possible that molecular oxygen diffusing and circulating into the expected fluence zone is converted to singlet oxygen during the extended light therapy, causing a gradient of hypoxia and anoxia that destroys the abnormal tissue outside the expected fluence zone.
Owner:LIGHT SCI ONCOLOGY
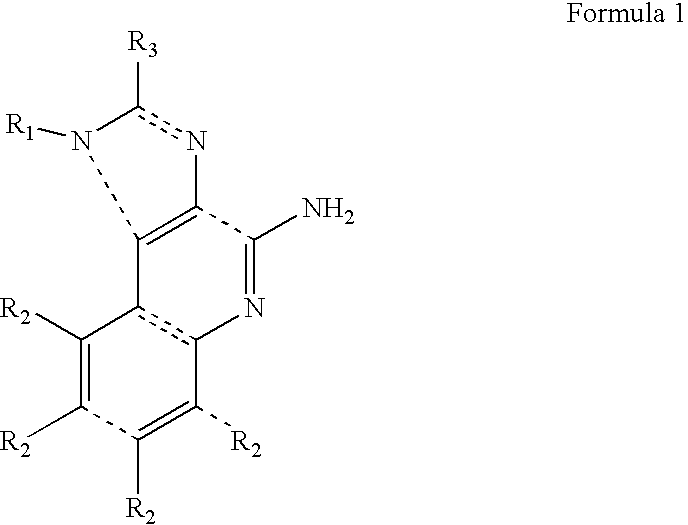
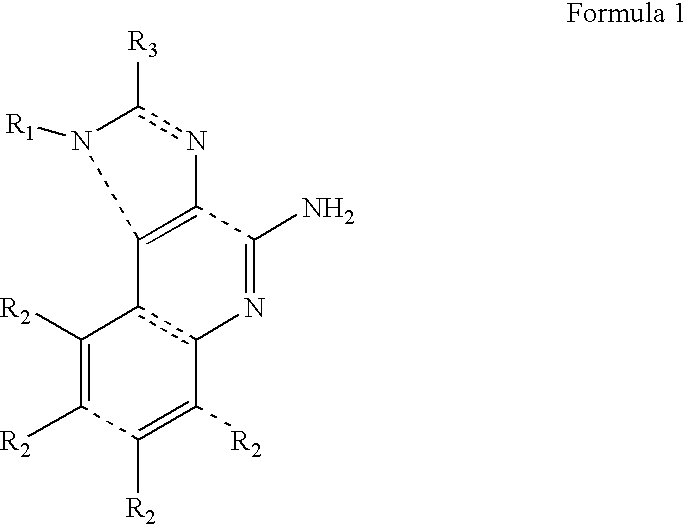
Combination therapies for treating photodamaged skin
Combination therapies for reducing the appearance of fine lines and wrinkles on aged skin or non-precancerous, normal photodamaged section of skin, in a patient not being treated for viral infection or skin cancer comprising (i) topical application of an imidazoquinoline amine derivative in a dermatologically-acceptable carrier in further combination with one or more cosmetic treatments selected from the group consisting of: (i) Light Emitting Diode (L.E.D.) Light Therapy; (ii) Intense Pulsed Light (I.P.L.) Therapy; (iii) laser skin resurfacing; (iv) mechanical exfoliation; (v) superficial, medium depth or deep chemical peels; (vi) radiofrequency treatment; (vii) ultrasound treatment; (viii) intradermal and intraepidermal injections with hyaluronic acid and derivatives thereof; and (ix) cryosurgery.
Owner:BAUMANN LESLIE
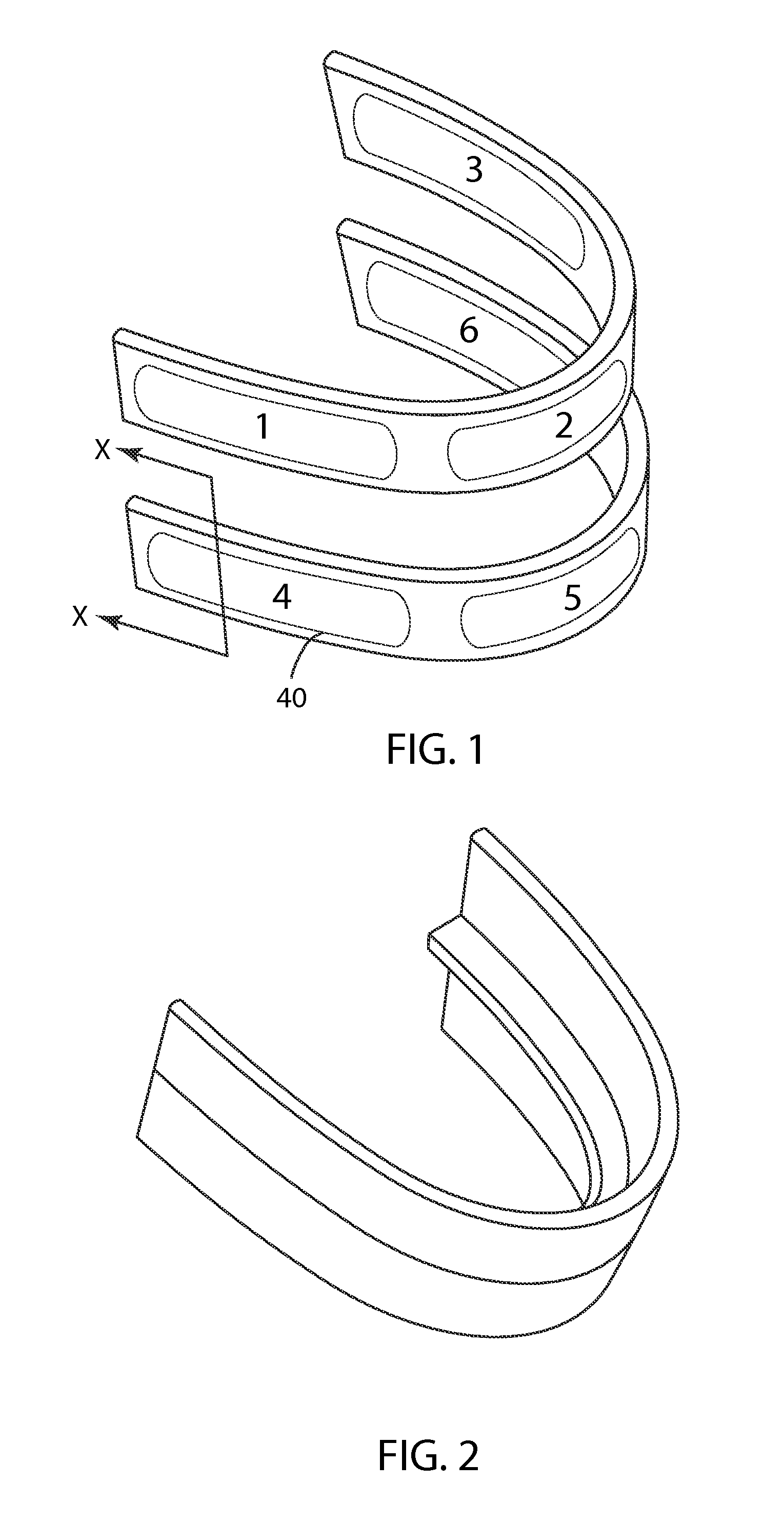
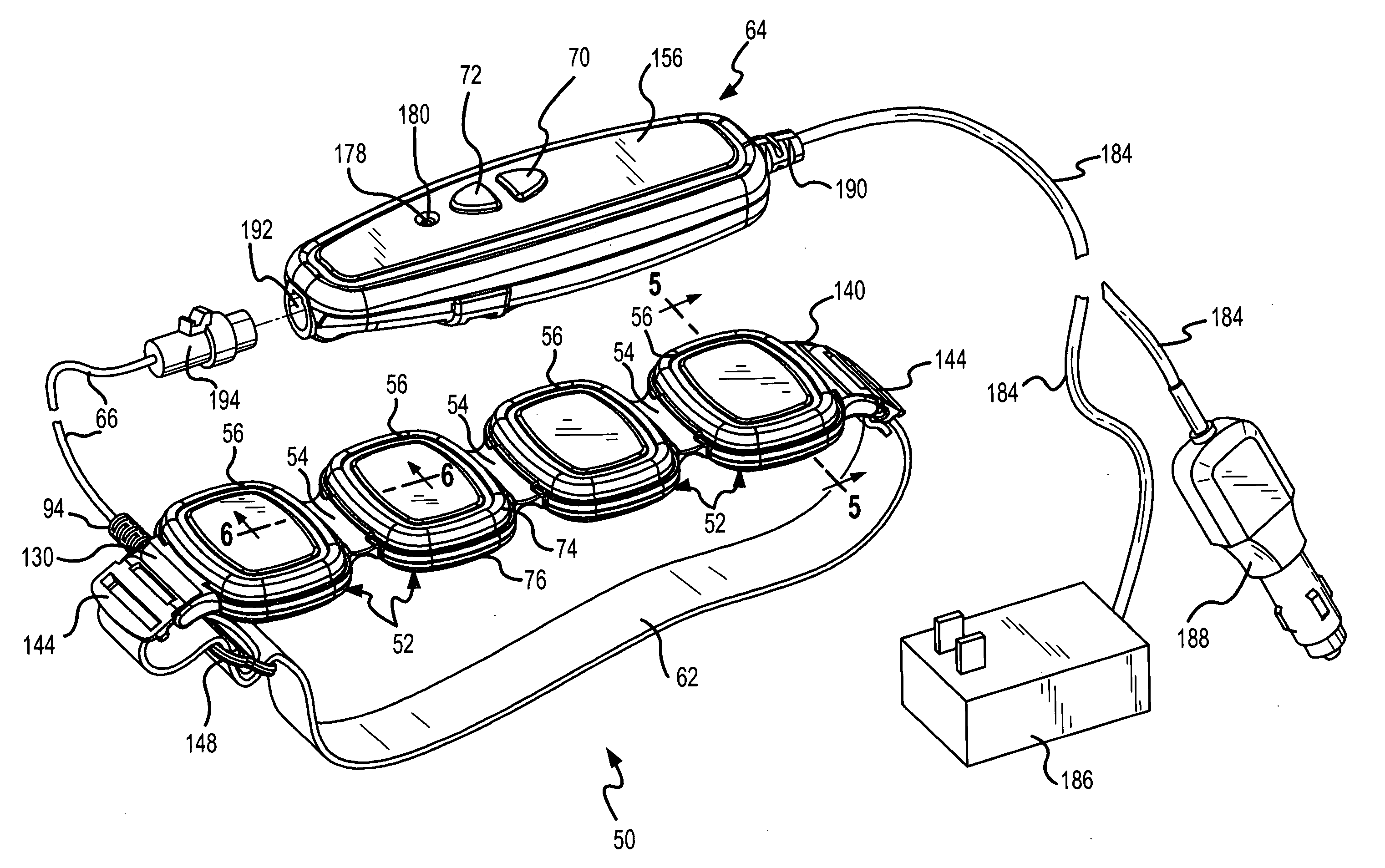
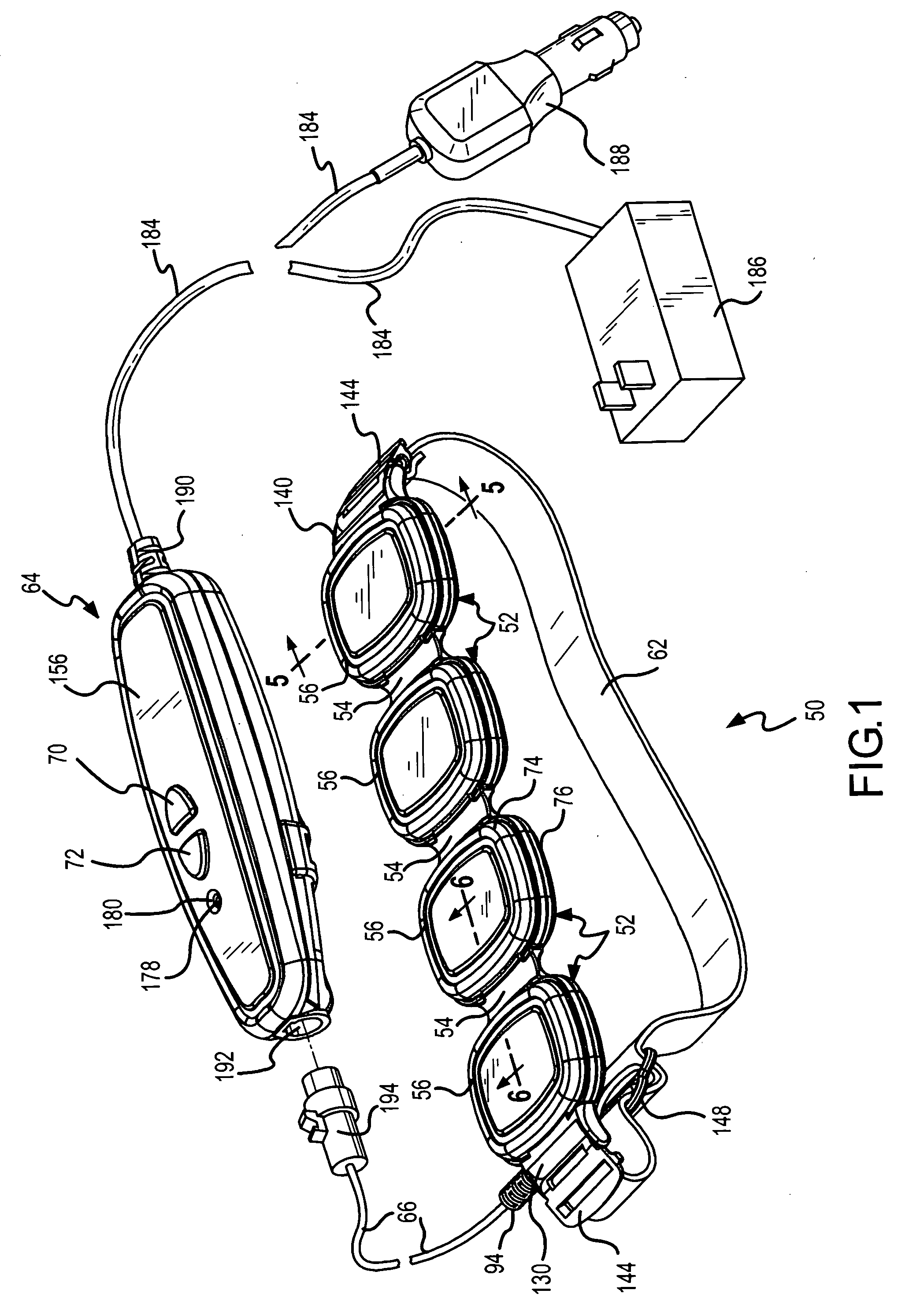
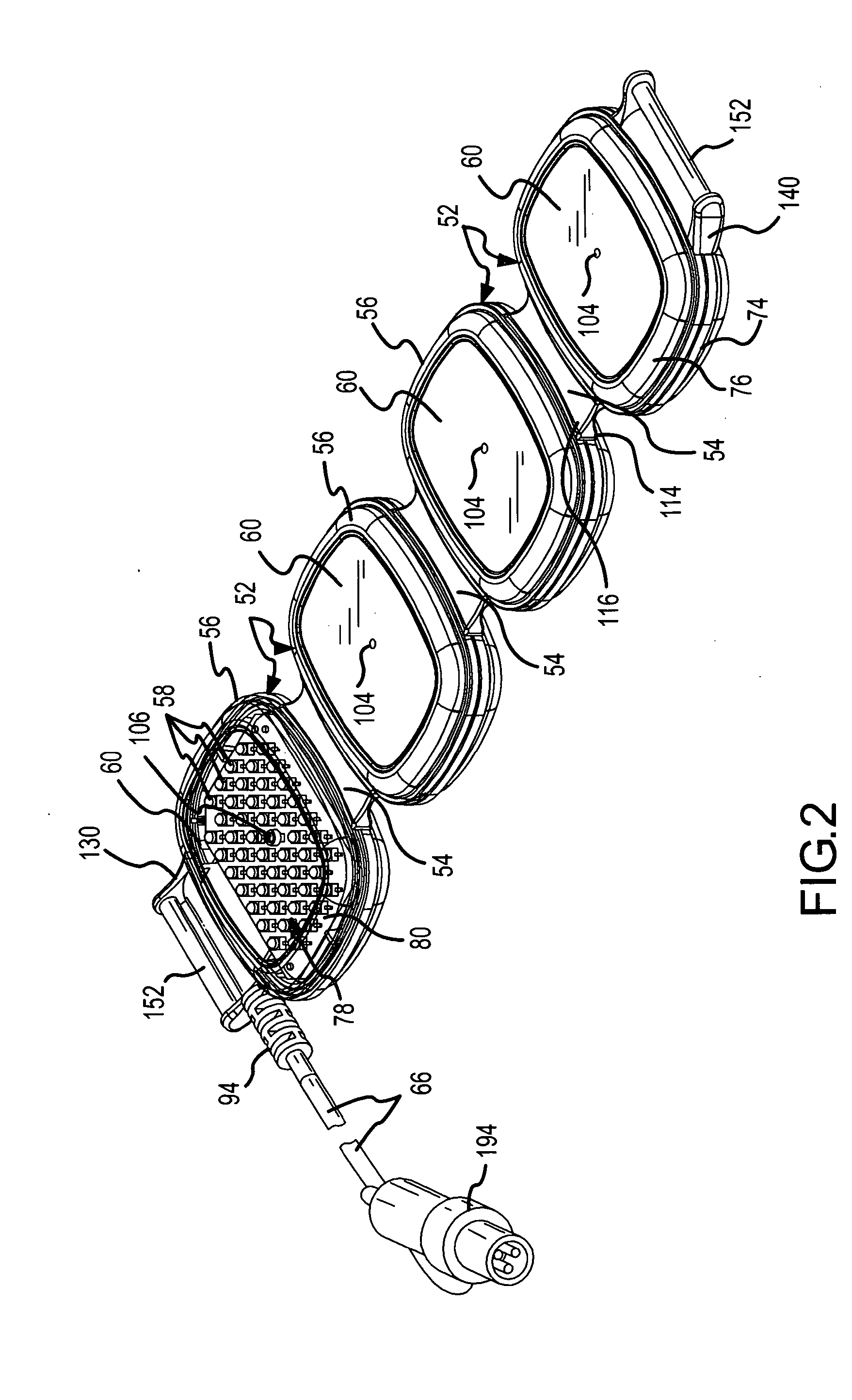
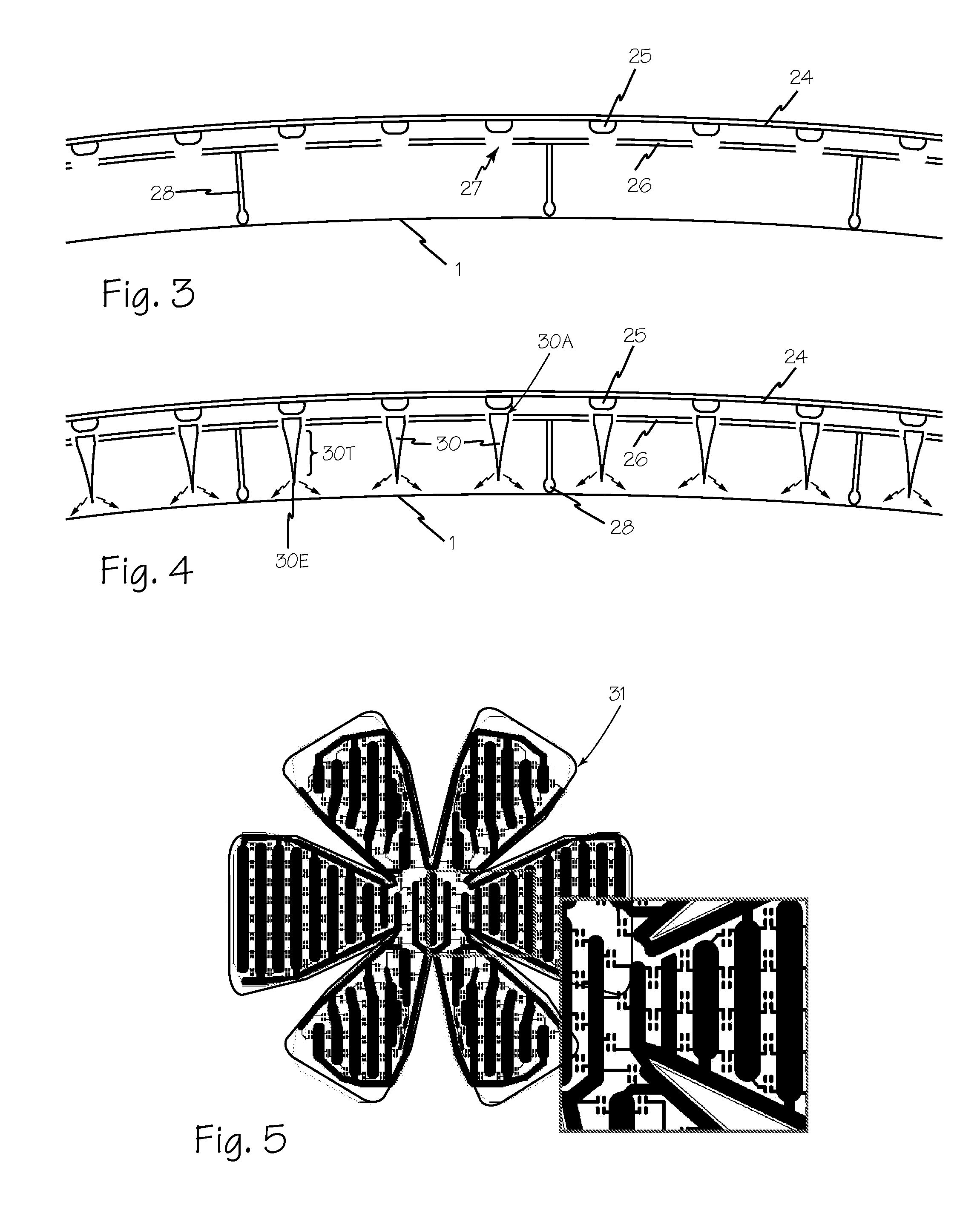
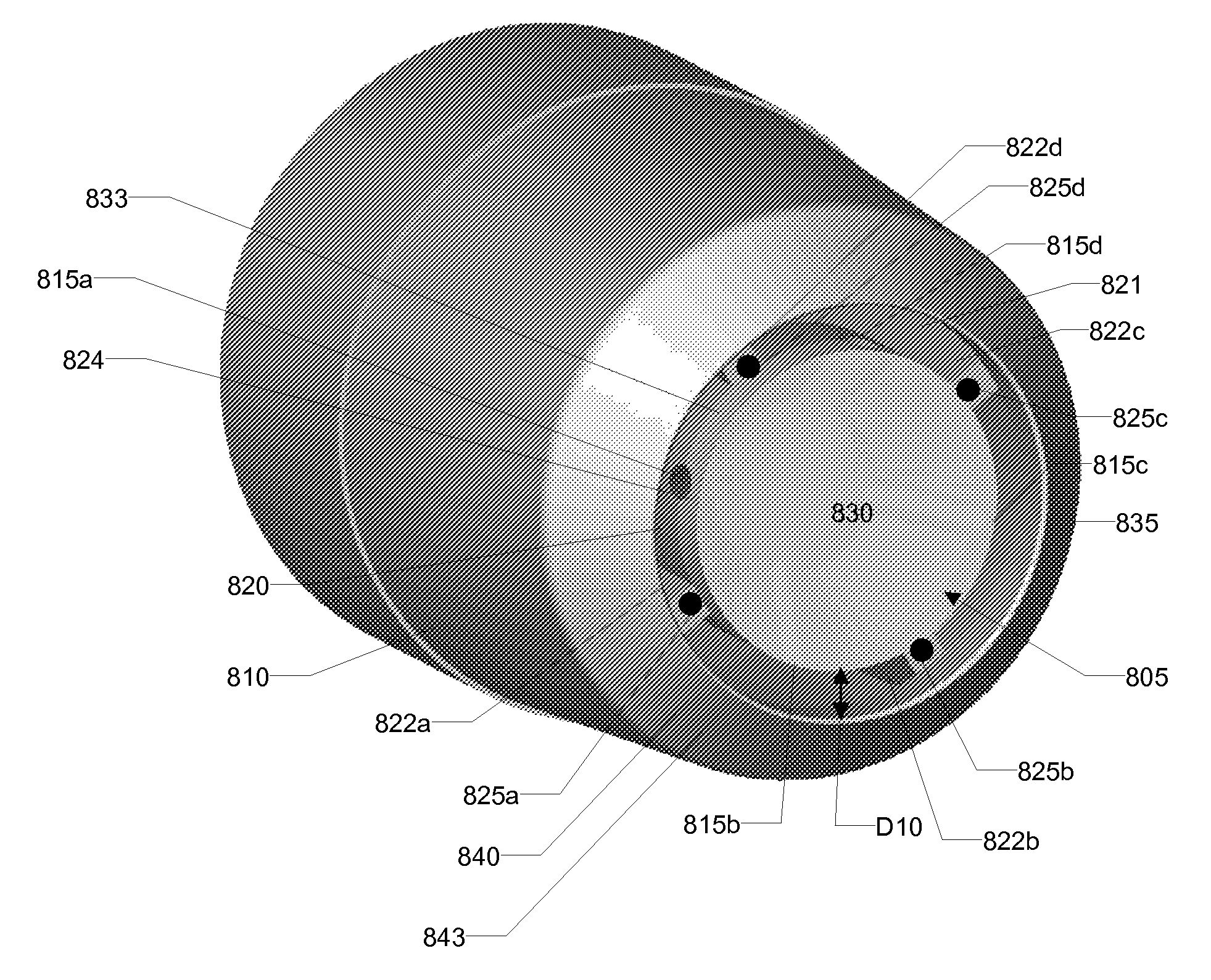
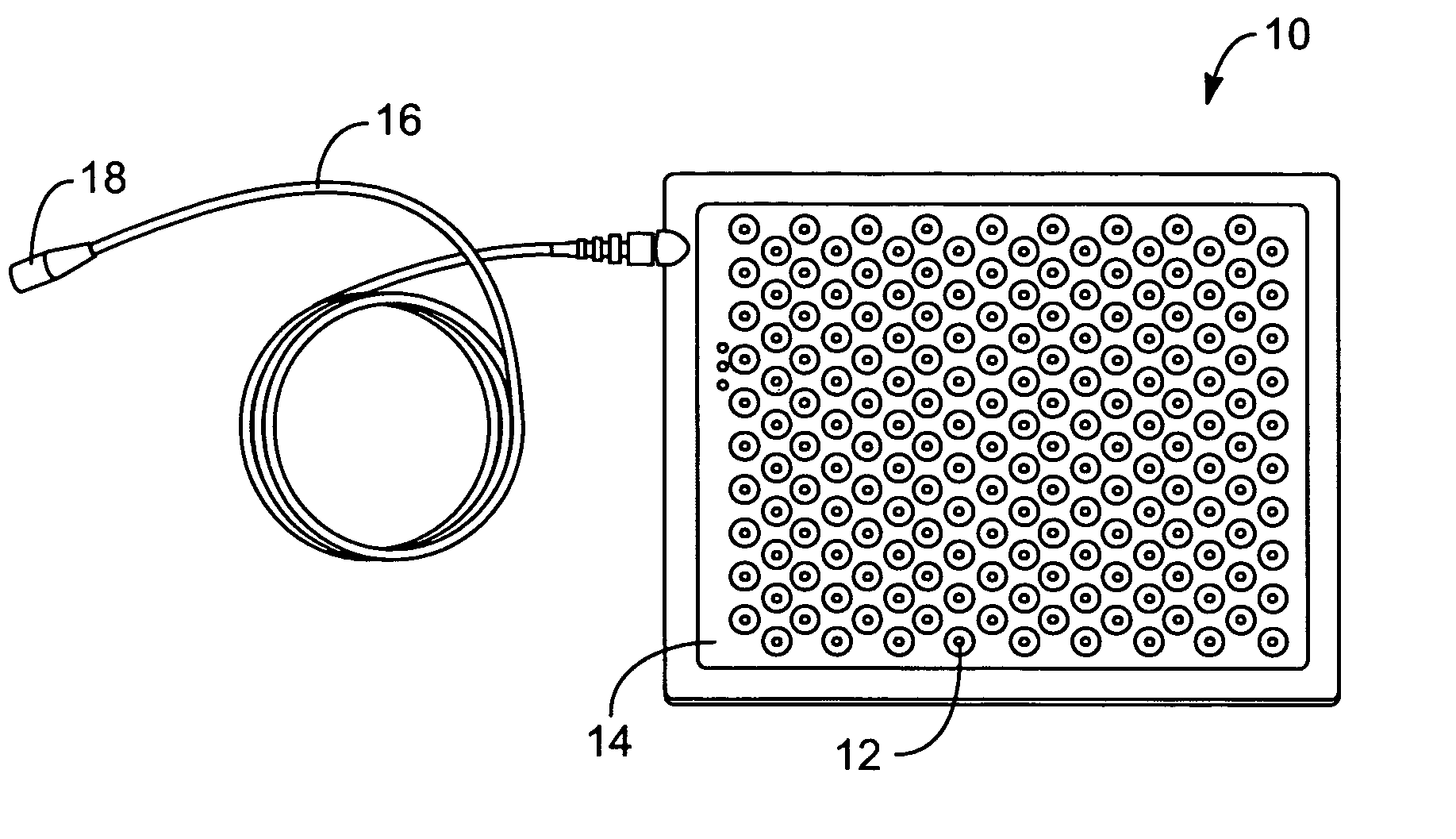
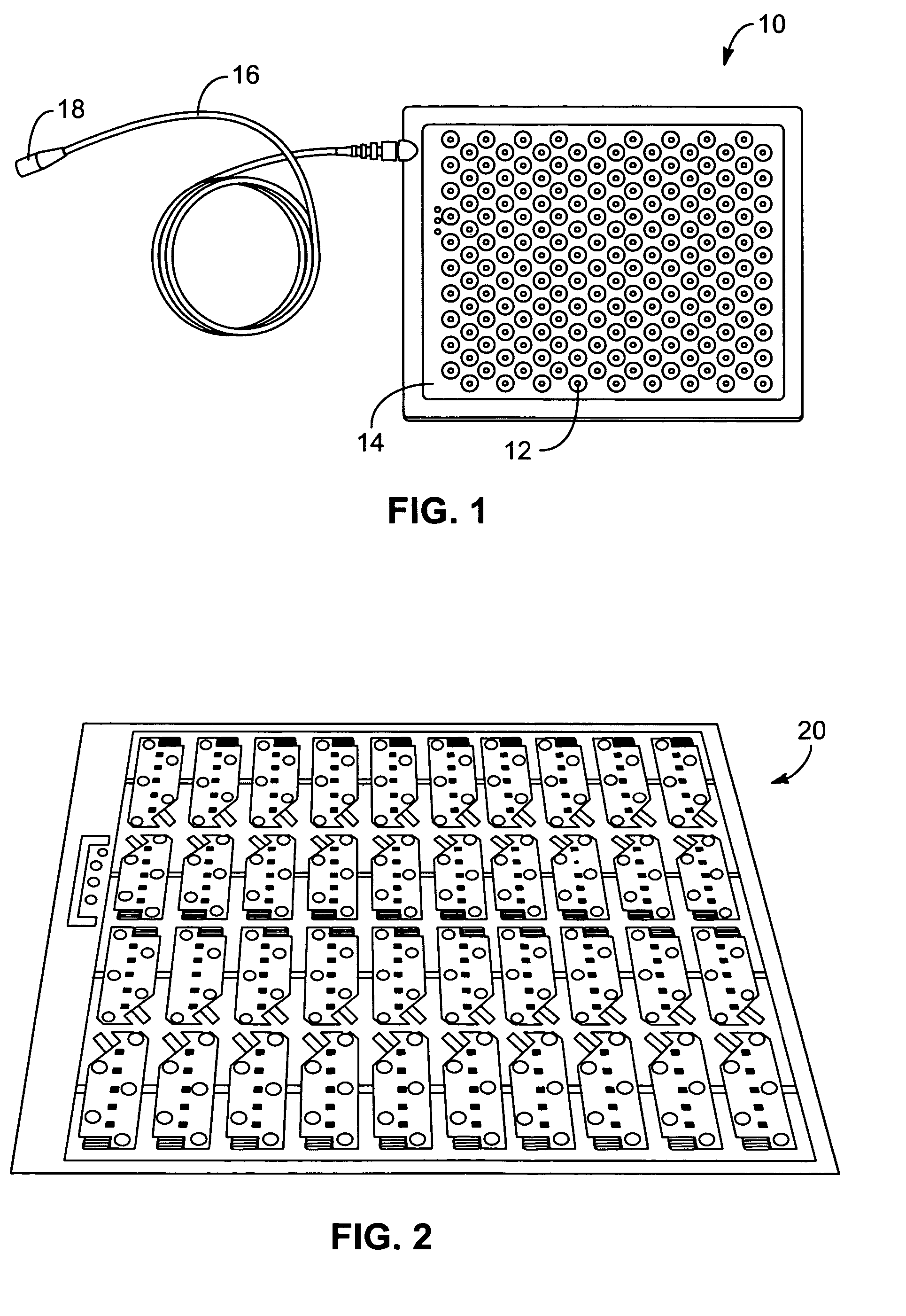
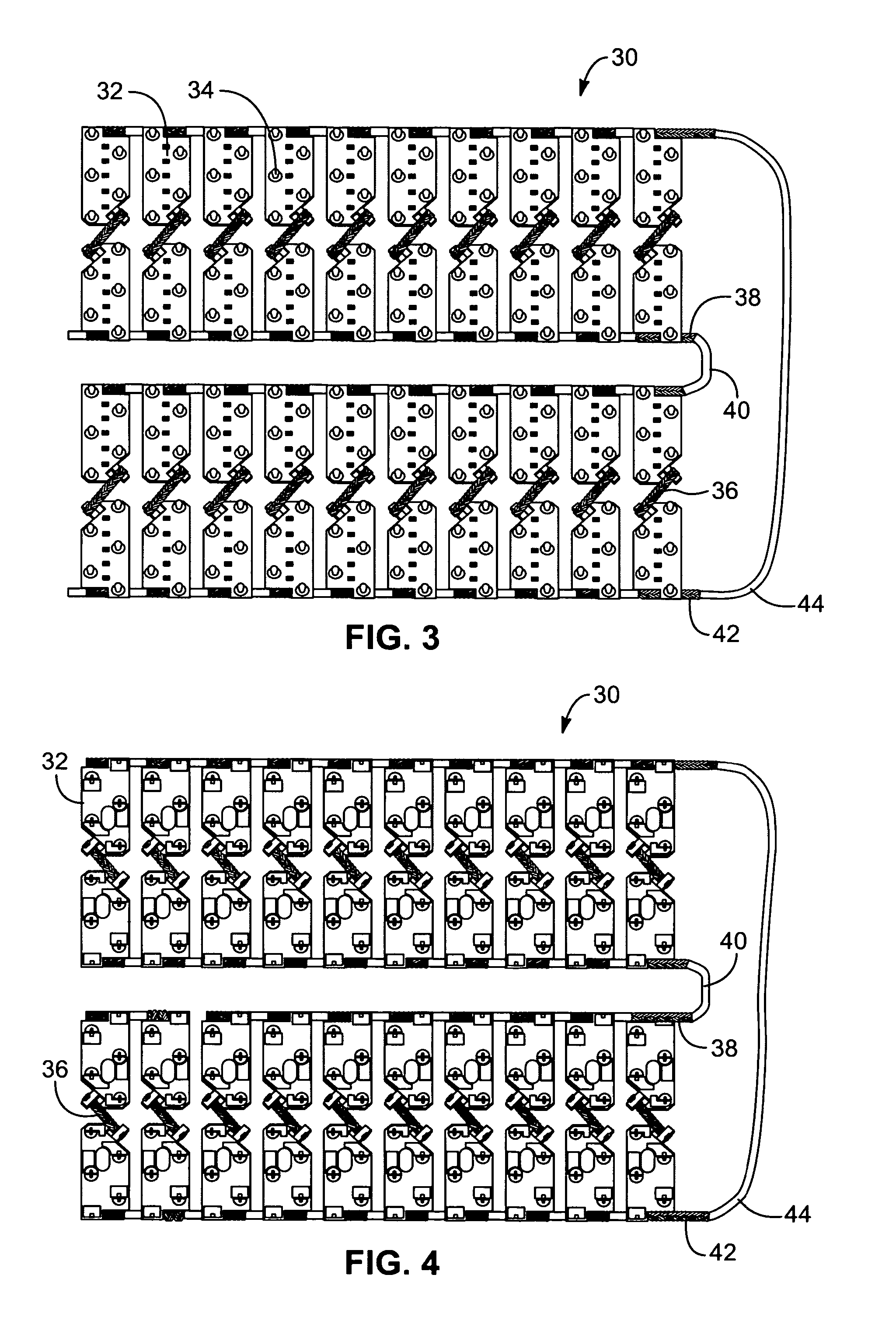
Systems and methods for providing a dynamic light pad
Systems and methods for providing a light pad configured for light therapy, wherein the light pad is dynamically flexible to conform to curvatures of the human body. The light pad includes a flexible, electrical circuit board configuration, a plurality of light sources coupled to the flexible, electrical circuit board configuration, wherein the plurality of light sources are configured to provide light therapy to a patient, and an electrical circuit comprising the plurality of light sources and electrical interconnections of the flexible, electrical circuit board configuration. In at least some embodiments, the flexible, electrical circuit board configuration comprises a plurality of circuit boards that are interconnected by one or more braided cords. The circuit boards provide increased flexibility of the light pad as bending is allowed between the boards, while the braided cord provides a resilient, long-lasting, electrical connection between the independent boards.
Owner:DYNATRONICS CORP
Features
- R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
Why Patsnap Eureka
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Social media
Patsnap Eureka Blog
Learn More Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com