Preparation method for acellular biological tissue material heparin coating
A biological tissue and decellularization technology, applied in the direction of coating, packaging item types, special packaging items, etc., can solve the problems of low heparin binding, promotion of monocyte adhesion, easy tissue calcification, etc., and achieve low immunogenicity. , beneficial to tissue reconstruction and host endothelial cell regeneration, good biocompatibility
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Problems solved by technology
Method used
Image
Examples
Embodiment 1
[0037] Preparation of heparin-coated bovine jugular vein (BJV) material and determination of heparin binding
[0038] Methods: (1) 20 local BJVs were collected, and each root was divided into two sections, one section was used for decellularized photooxidized BJV (DP-BJV), and the other section was used for heparin-coated BJV after decellularized photooxidized (LBL-BJV). Decellularized photooxidation is prepared by CN100443064C patented method: 300-500 kg of healthy buffaloes are taken, the jugular vein is taken out within 30 minutes of warm ischemia time, and the fascia tissue is removed under aseptic conditions. Soak in PBS (pH 7.4) solution of 0.5% Trinaton X-100 for 48 hours, then soak in PBS solution of 0.025% trypsin and 0.02% EDTA for 30 minutes, rinse with PBS for 3 times, and then put in 20 μg / ml DNase·I and 0.2 mg / ml RNase·A in PBS solution for 24 hours, and washed with PBS solution 3 times. The above treatment was performed on a shaker with a shaking frequency of 7...
Embodiment 2
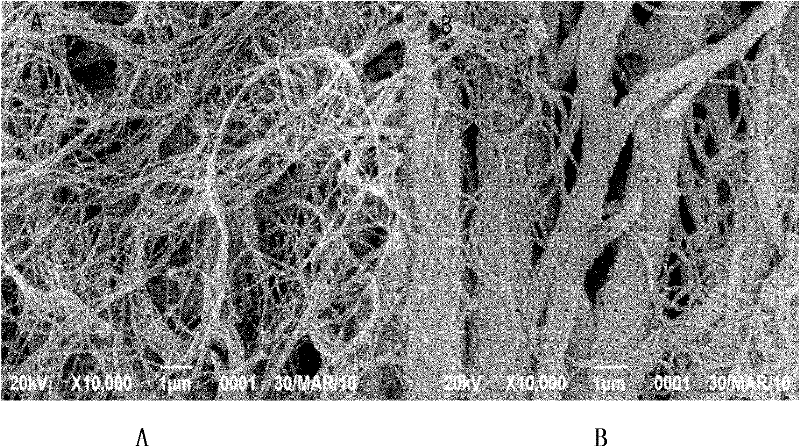
[0046] Electron microscope inspection and toluidine blue staining inspection of heparin-coated BJV materials
[0047] Methods: 10 local BJVs were collected, each root was divided into 2 sections, and randomly divided into the decellularized photooxidized group and the decellularized photooxidized heparin-coated group. All BJVs used in the experiment were cut into vascular slices (1cm×1cm) at a distance of 1cm from the valve sinus. . The decellularized photooxidation method is the same as that in Example 1. Preparation of heparin-coated BJV: immerse the decellularized photooxidized BJV in 5% heparin (containing 2% sodium chloride), and soak for 24 hours at 0-4°C. After rinsing with normal saline for 3 times, soak in 5% dihydroxy iron (Ⅲ) solution for 5 minutes; wash with normal saline for 3 times, 5 minutes each time, soak with 5% heparin (containing 2% sodium chloride) for 5 minutes, wash with normal saline for 3 minutes times, 5 min each time; repeat the above steps 4 times...
Embodiment 3
[0054] Detection of biomechanical properties of heparin-coated bovine jugular vein (BJV) material
[0055] Methods: 20 local BJVs were collected, each BJV was cut into two slices (4cm×1cm) of blood vessel strips (4cm×1cm) at a distance of 1cm from the valve sinus, and divided into decellularized photooxidation group and heparin-coated group. 20 tablets (decellularized photooxidation and heparin coating method are the same as in Example 2). The biomechanical properties of the two groups of blood vessel strips were detected by INSTRON tensile machine.
[0056] Results: The test results are shown in Table 1. The tensile strength of heparin-coated BJV was increased, and the elastic modulus, maximum load, and maximum tensile stress were significantly improved compared with decellularized photooxidized BJV.
[0057] Table 1 Pull test results
[0058]
[0059] There is a statistically significant difference between the two groups (P<0.05).
[0060] Conclusion: After heparin co...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com