Treatment of circulating tumor cells using an extracorporeal device
a technology of circulating tumor cells and extracorporeal devices, which is applied in the direction of blood circulation devices, cardiovascular disorders, drug compositions, etc., can solve the problems of rare ctcs shed from solid tumors into blood stream that cannot be separated and concentrated in blood effectively in the online, and the current treatment methods for solid tumors are not effective at eliminating ctcs. , to achieve the effect of effective inducing apoptosis, necrosis and/or autophagy
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
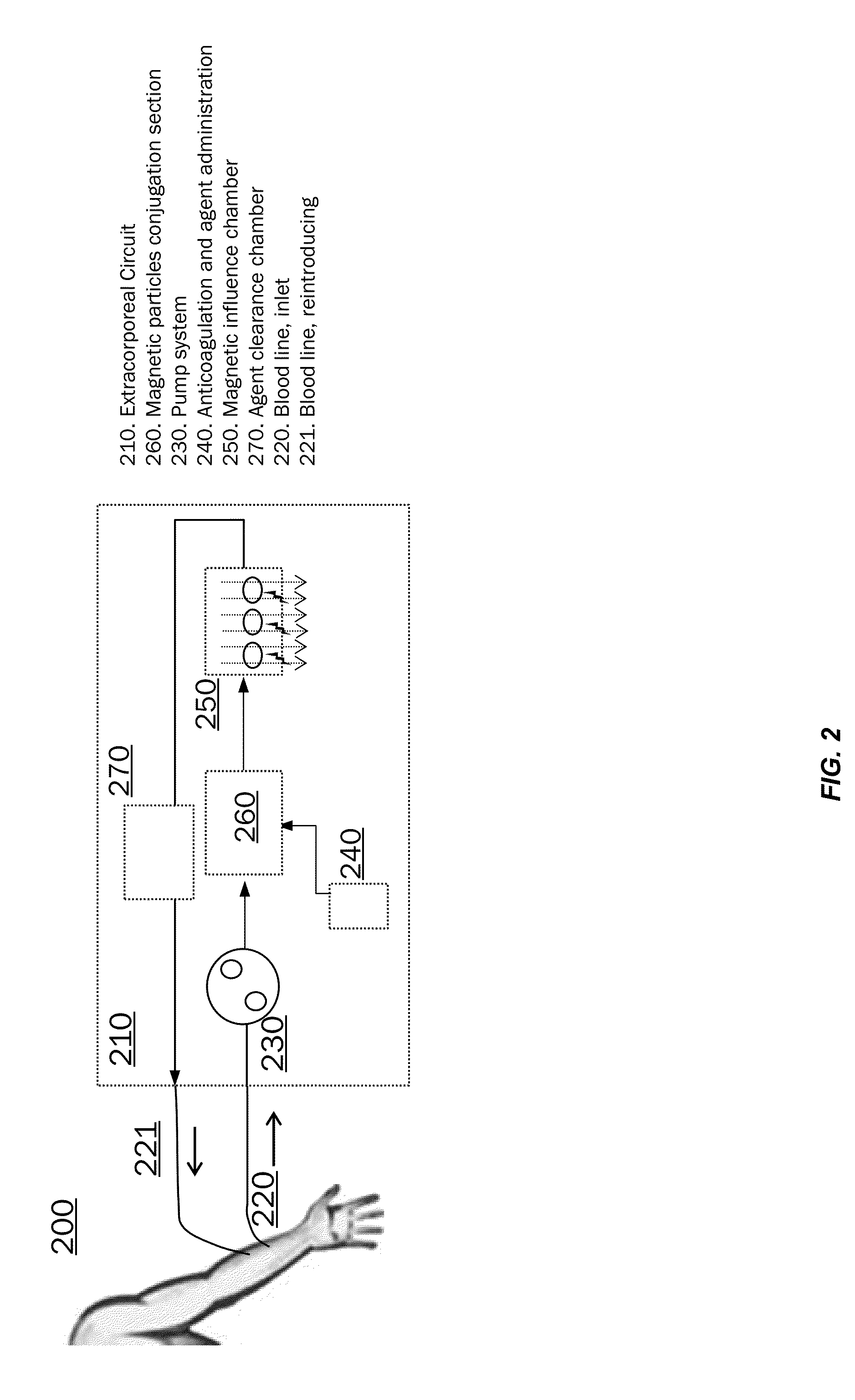
Image
Examples
example 1
Using IRDye® 700DX-EGF Probe and Photoactivating Light to Kill Cancer Cells Overexpressing the EGF Receptor
[0086]This example illustrates the application of photodynamic therapy using an IRDye® 700DX-targeting agent (e.g., EGF-700DX) and photoactivating light to kill targeted cells.
[0087]Cancer cells that overexpress the EGF receptor (e.g., A431 cells) were seeded in an in vitro culture system. The cells were incubated with the targeting agent EGF-700DX and exposed to irradiating light at a wavelength of 690 nm and at 8 J / cm2 or 16 J / cm2.
[0088]FIG. 3 shows a reduction in the number of targeted cells after exposure to irradiating light at 8 J / cm2 or 16 J / cm2. FIGS. 3A-E show a reduction in the number of targeted cancer cells after exposure to irradiating light at 8 J / cm2 or 16 J / cm2. FIGS. 3A-C are control data and FIGS. 3D-E show exposure to 8 J / cm2 or 16 J / cm2, respectively. In addition, FIG. 3E shows significant morphology changes in cells treated with EGF-700DX and irradiating li...
example 2
Methods for Inducing Apoptosis, Necrosis or Autophagy in Cancer Cells Using an IRDye® 700DX-EGF Probe and Photoactivating Light
[0094]A study was performed to optimize the conditions for IRDye®700DX-EGF based photodynamic therapy. In the experiment factors (e.g., parameters and variables) that contribute to the level of apoptosis and / or necrosis are tested. In particular, three factors with two conditions for each were evaluated in a 2×2×2 factorial design of experiments. The factors included: A) probe concentration at 0.5 μM and 2.0 μM, B) irradiation of 4 J / cm2 or 16 J / cm2, and C) probe incubation time of 5 minutes or 10 minutes. All possible treatment conditions were tested. Representative images of the treated cells are provided in FIGS. 6A-6D and 7A-7D.
[0095]Briefly, cancer cells that overexpress EGF (e.g., A431 cells) were plated and incubated with the IRDye® 700DX-EGF probe at the test concentration and at a flow rate of 1.36 mL / min. After the incubation, the cells were washed...
example 3
Methods for Inducing Apoptosis, Necrosis or Autophagy in Cancer Cells Using an IRDye® 700DX-EGF Probe or an IRDye® 700DX-Panitumumab Probe
[0100]This example illustrates that the IRDye® 700DX-EGF probe and the IRDye® 700DX-panitumumab probe can induce cell death in A431 cells which are human epithelial cancer cells that overexpress the EGF receptor. EGF is the ligand for the EGF receptor and panitumumab is a fully human monoclonal antibody specific to the receptor.
[0101]A431 cells were plated and incubated with either probe for 5 minutes, 10 minutes or 20 minutes prior to washing and irradiation at 24 J / cm2. The IRDye® 700DX-EGF probe was used at a concentration of 0.5 μM in complete media and the IRDye® 700DX-panitumumab probe was used at a concentration of 0.1 μM. After irradiation, the cells were cultured at 37° C., 5% CO2 for approximately 24 hours. The NucleoCounter® NC-3000™ cell vitality assay (Chemometec, Allerød, Denmark) was performed. Table 1 provides cell numbers. Table 2...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D Engineer
- R&D Manager
- IP Professional
- Industry Leading Data Capabilities
- Powerful AI technology
- Patent DNA Extraction
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2024 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com