System using a helical retainer in the direct plication annuloplasty treatment of mitral valve regurgitation
a technology of mitral valve and helical retainer, which is applied in the field of direct plication annuloplasty can solve the problems of imperfect valve closure, problem of mitral valve gap, and no commercially successful device for the treatment of mitral valve regurgitation in such a manner currently exists, so as to reduce the possibility of clot development, reduce interference with leaflet motion or
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
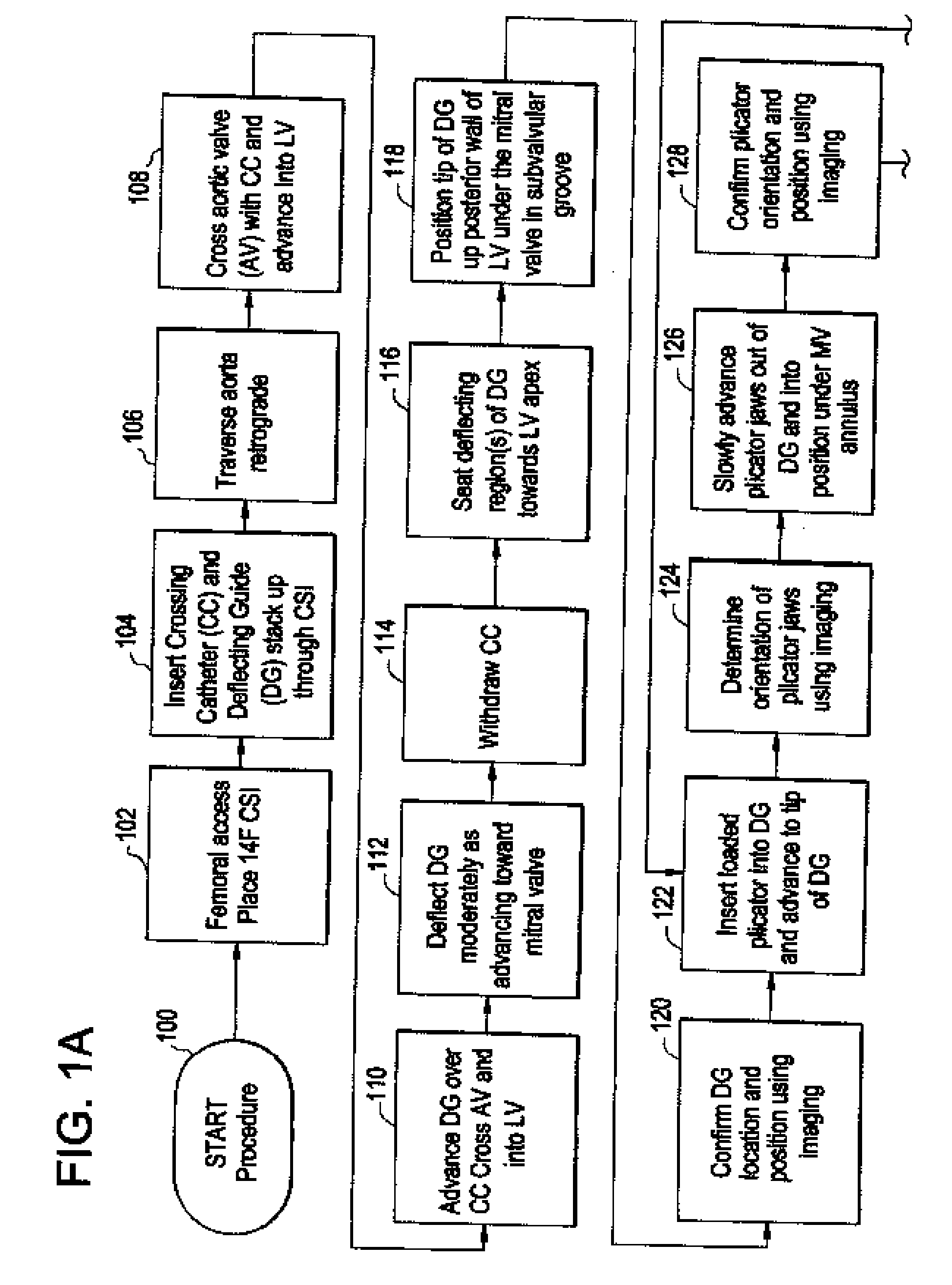
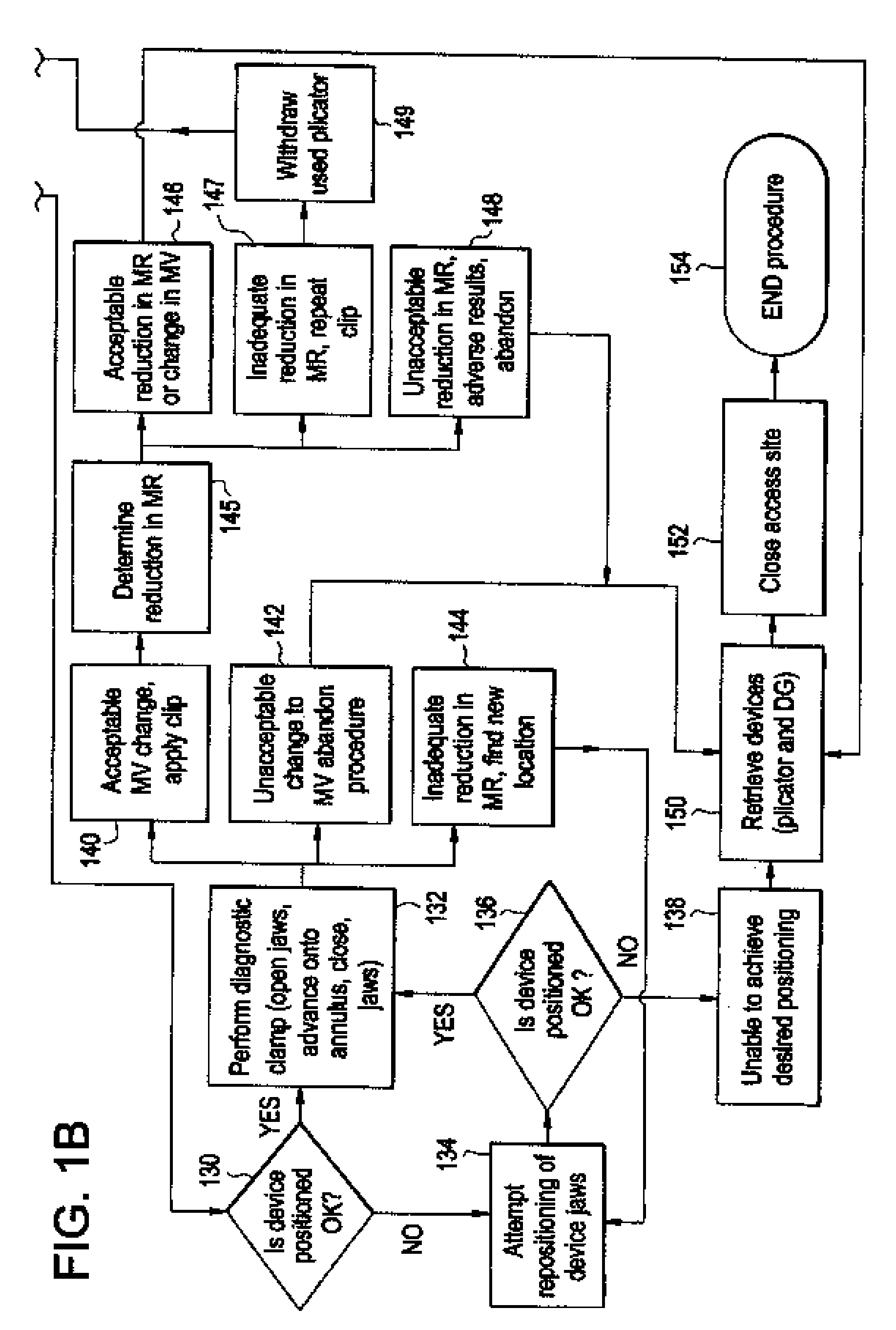
[0056]FIG. 1 is a flow diagram depicting a method of providing direct plication annuloplasty to the mitral valve in a heart such as that depicted in FIG. 2A in accordance with the present invention. At step 100 the procedure begins with a puncture for access to the femoral artery using standard techniques. At step 102 the physician or other practitioner places a catheter sheath introducer (CSI) into the femoral access point using standard techniques. Any known CSI may be used in the procedure with the preferable size being approximately 14 french. At step 104 a crossing catheter, preferably prolapseable or having a curved tip, and a deflecting guide catheter are inserted together in a “stack” formation through the CSI. Alternatively, the deflecting guide catheter is inserted through the CSI without a crossing catheter although the use of a crossing catheter is the preferred method. The crossing catheter is described herein in greater detail with respect to FIGS. 4 and 5 below and th...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com