Condensate Glucose Analyzer
a glucose analyzer and condensate technology, applied in the field of blood glucose concentration monitoring, can solve the problems of confusion, loss of consciousness or seizure, blurred vision, etc., and achieve the effect of convenient use and simple operation
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
Selection of Sensors
[0272]The following are examples of various sensor technologies that may be utilized in practicing the method of the present invention:
Microgravimetric Sensors
[0273]Microgravimentric sensors are based on the preparation of polymeric- or biomolecule-based sorbents that are selective for a particular analyte, such as glucose. A direct measurement of mass changes induced by binding of a sorbent with glucose can be observed by the propagation of acoustic shear waves in the substrate of the sensor. Phase and velocity of the acoustic wave are influenced by the specific adsorption of glucose onto the sensor surface. Piezoelectric materials, such as quartz (SiO2) or zinc oxide (ZnO), resonate mechanically at a specific ultrasonic frequency when excited in an oscillating field. Electromagnetic energy is converted into acoustic energy, whereby piezoelectricity is associated with the electrical polarization of materials with anisotropic crystal structure. Generally, the osc...
example 2
Detection of glucose in exhaled breath
[0310]Persons with diabetes presently check their blood glucose levels between 1 and 6-8 times each day. Knowledge of blood glucose levels is an absolute necessity for guiding proper administration and dosing of insulin and other medications used to control hyperglycemia. Presently the person must draw blood samples, usually from a finger using a lancet device, and place the sample on a “test strip” which is inserted into a glucose monitor that gives the blood glucose concentration. This process requires considerable skill, time and subjects the person with diabetes to immediate recognition as a diabetic and thus results in the potential for embarrassment and even prejudice and / or discrimination when applying for employment.
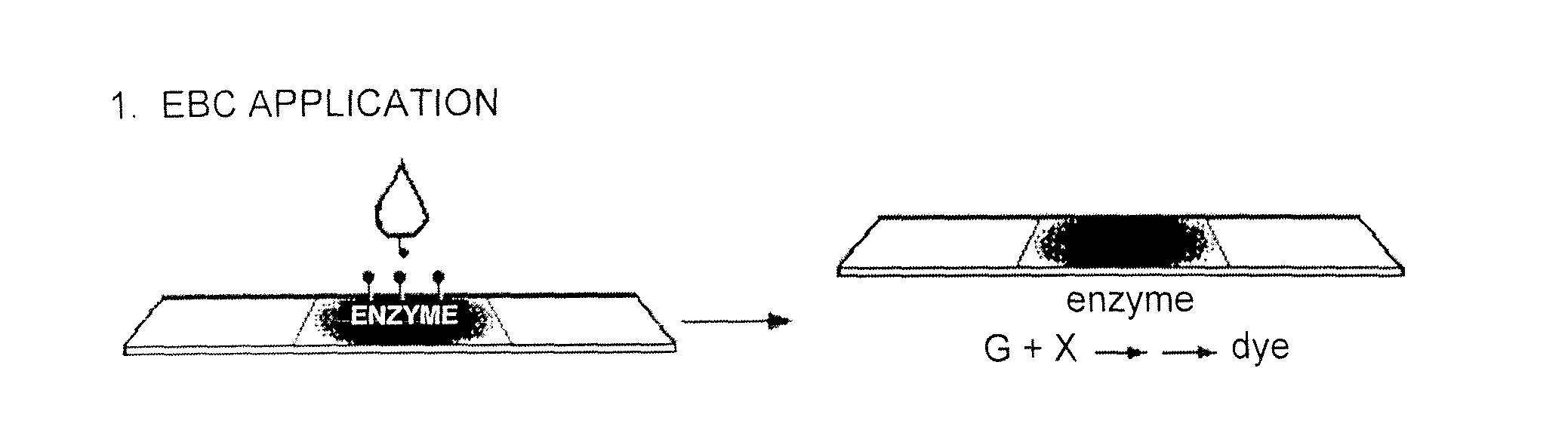
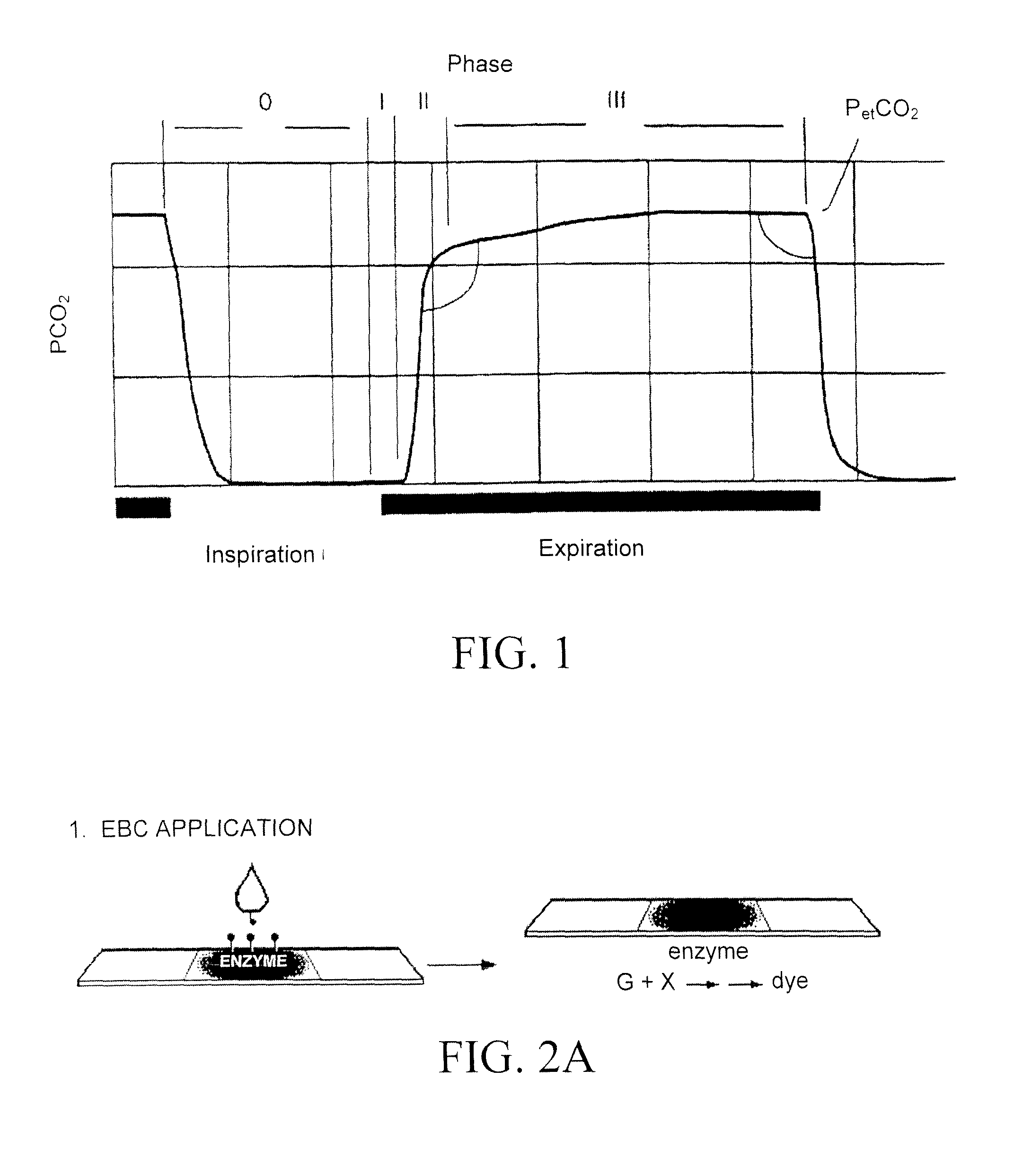
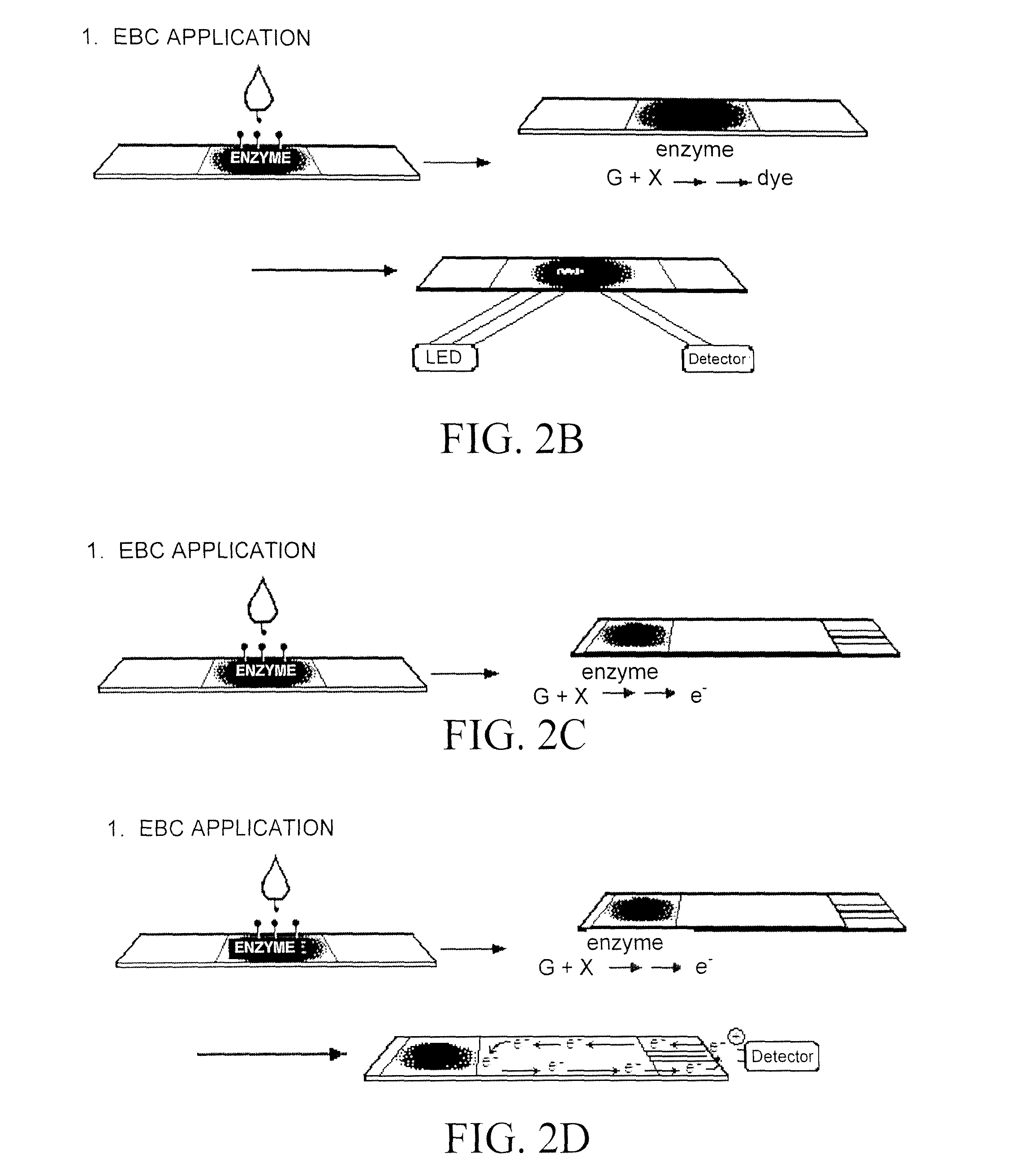
[0311]An attractive alternative is to use a sensor system that collects a sample of exhaled breath which for compounds such as glucose, which are extremely hydrophilic, condenses the sample into a “condensate” which is then p...
example 3
Correlation of Glucose in Exhaled Breath with Glucose in Blood
[0312]A non-diabetic subject ingested a 100 gm glucose solution. Both exhaled breath and blood samples were taken from the subject at 40 and 20 minutes before ingestion of the glucose solution and for 10 minutes interval every 15 minutes, see FIGS. 3A and 3B, after ingestion of the glucose solution. Glucose was readily detectable in the exhaled breath, which was condensed into a liquid. The concentration of both the breath and blood glucose rose and fell at the same rates (see FIGS. 3A and 3B).
[0313]According to the subject invention, the ratio of exhaled breath to blood glucose concentration is 3 to 5 magnitudes lower and that this ratio is predictable and reproducible. By analyzing glucose present in EBC, a more predictive, non-invasive, and simpler method is provided to monitor glucose concentration in a subject by monitoring breath rather than blood.
PUM
| Property | Measurement | Unit |
|---|---|---|
| temperature | aaaaa | aaaaa |
| temperature | aaaaa | aaaaa |
| temperature | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com