Method and device for monitoring and improving patient-ventilator interaction
a technology of patient-ventilator interaction and monitoring method, which is applied in the direction of medical devices, valve details, operating means/releasing devices, etc., can solve the problems of ineffective effort, effort completely failing to trigger the ventilator, and often marked trigger delay, etc., to achieve the effect of reducing cycling off errors
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
third embodiment
[0183] Certain internal signals need to be displayed to allow the user to adjust the input settings, while others provide the user with the results of monitoring. These signals can be displayed on a monitor 78 included in a freestanding device. Alternatively, if the device is incorporated inside the ventilator, the monitor of the ventilator can be used for this purpose. A third embodiment involves directing the device's outputs to an analog to digital converter and displaying the outputs on a separate computer.
[0184] The following output signals are necessary for adjusting the input settings:
[0185] a) The main signal itself 31.
[0186] b) The output of the integrator 48 in the Tonset circuit (32).
[0187] The use of these two signals for the sake of input adjustment is described below under OPERATION (below).
[0188] Additionally, the signals representing flow 9, pressure 15 and volume 79 may be displayed on the monitor for general monitoring purposes.
[0189] Signals representing the ...
embodiment 103
[0191] In another embodiment of the output processor 103 patient respiratory rate (or TTOT) is inputted to the processor, replacing the “Calculate Patient Rate” function 83. This input is then used to calculate the “Desirable TI”87 and “Flow at Desired TI”90. Patient respiratory rate may be determined by the user from inspection of chest movements or by observing the flow tracing on the monitor, or automatically using computational methods other than the ones described in the above embodiment 103.
Operation
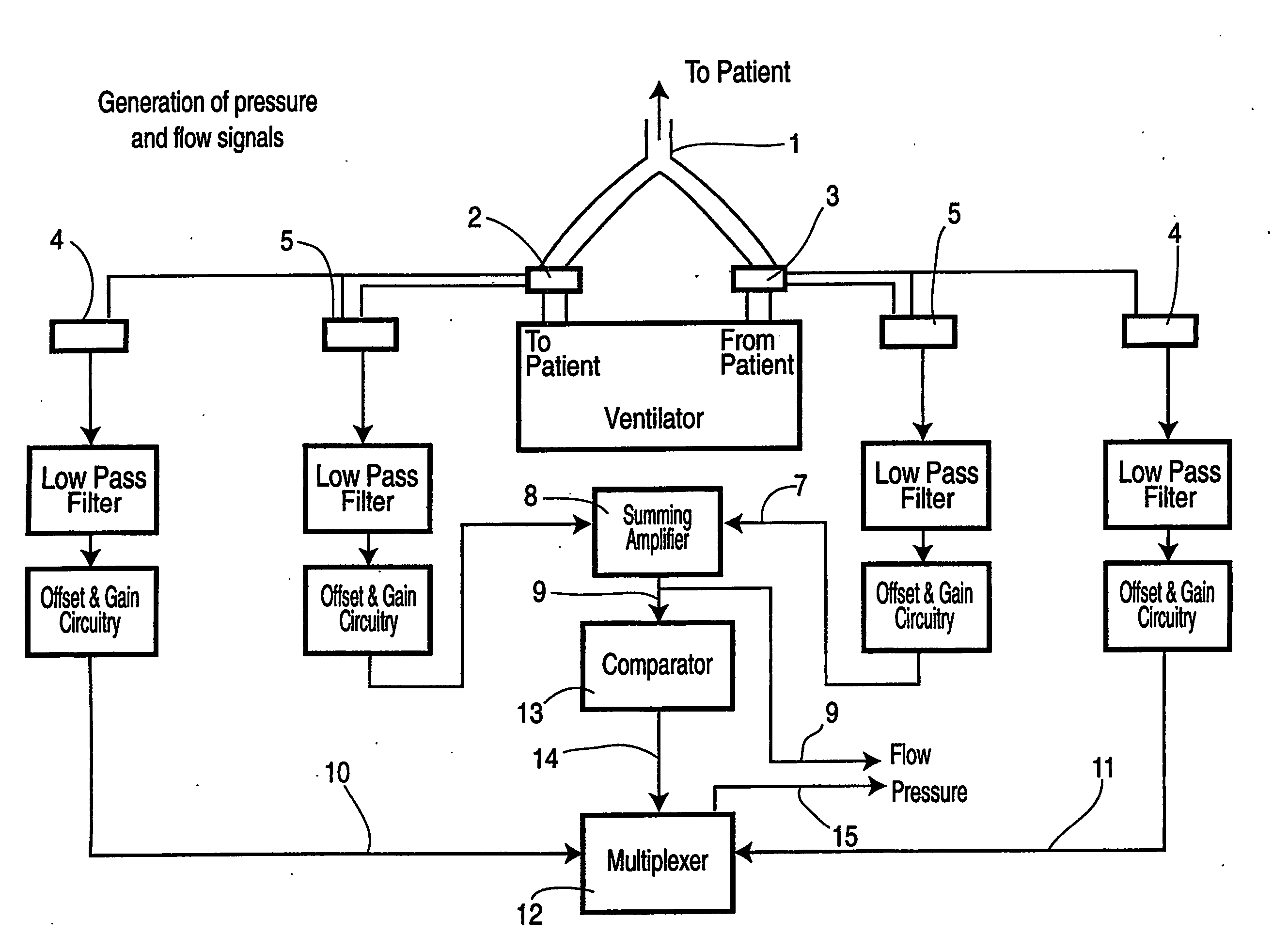
[0192] When the device is built inside the ventilator, the pressure 15 and flow 9 signals are permanently connected to the device. For freestanding systems, the first step is to connect the flow meters and pressure ports to the inspiratory 2 and expiratory 3 lines close to the ventilator (FIG. 7). The device is turned on. Tracing of the Signal 31 appears on the screen (FIG. 10). Subsequent steps depend on what inputs are available on the device and user preference. For the most co...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com