Multi-lumen vascular grafts having improved self-sealing properties
a multi-lumen, vascular graft technology, applied in the direction of prosthesis, blood vessels, coatings, etc., can solve the problems of affecting the healing effect of the graft, so as to achieve the effect of improving healing effect, and reducing the risk of recurren
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
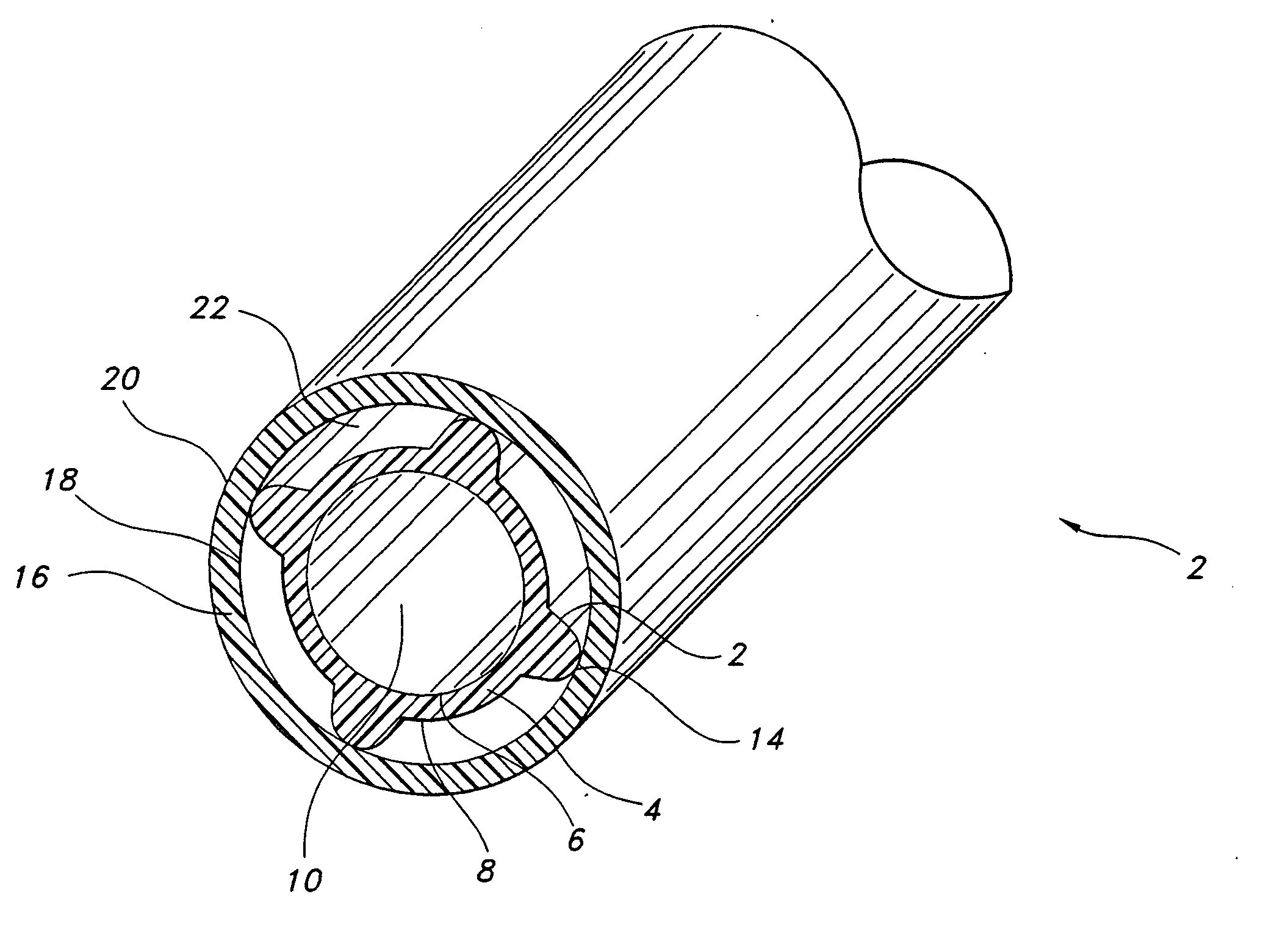
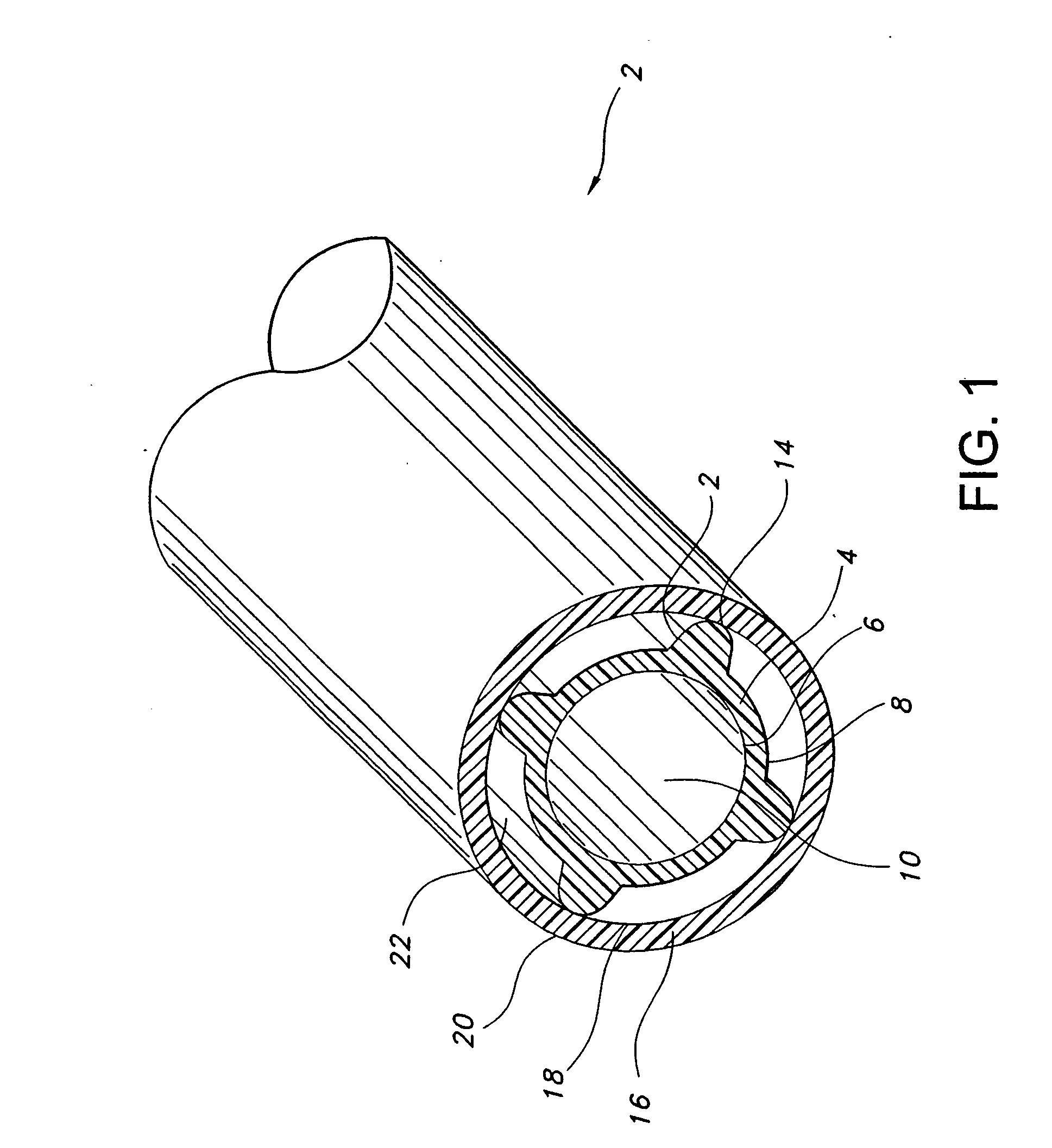
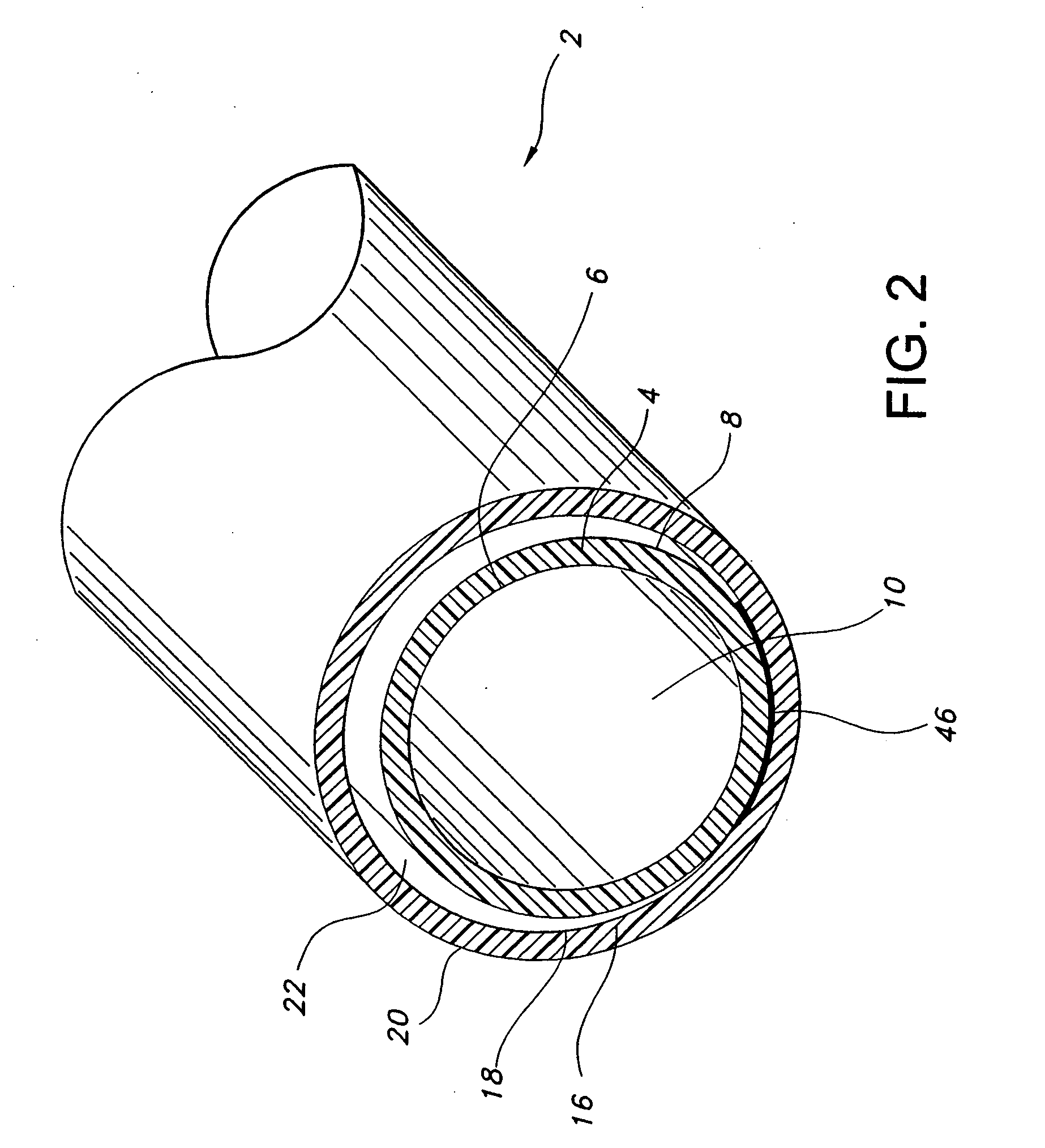
[0036] The prosthesis of the present invention includes an implantable self-sealing tubular structure having a plurality of secondary lumens between a primary and a secondary tubular structure. Desirably, the prosthesis is formed from extruded PTFE or other similar material which exhibits superior biocompatibility.
[0037] In the present invention, a primary tubular body is formed which defines a blood contacting lumen. A secondary tubular structure is formed about and integral with the first tubular structure at an outer wall of the primary tubular body. A portion of an inner wall of the secondary tubular body and a portion of an outer wall of the primary tubular body defines at least one secondary lumen between the tubular bodies. The secondary lumen may contain a non-biodegradable self-sealing elastomeric material. Optionally, a pharmacologically or physiologically active agent may be supplied in the graft for delivery to the patient.
[0038] In an advantageous aspect of the invent...
PUM
| Property | Measurement | Unit |
|---|---|---|
| intemodal distance | aaaaa | aaaaa |
| internodal distance | aaaaa | aaaaa |
| intemodal distance | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com