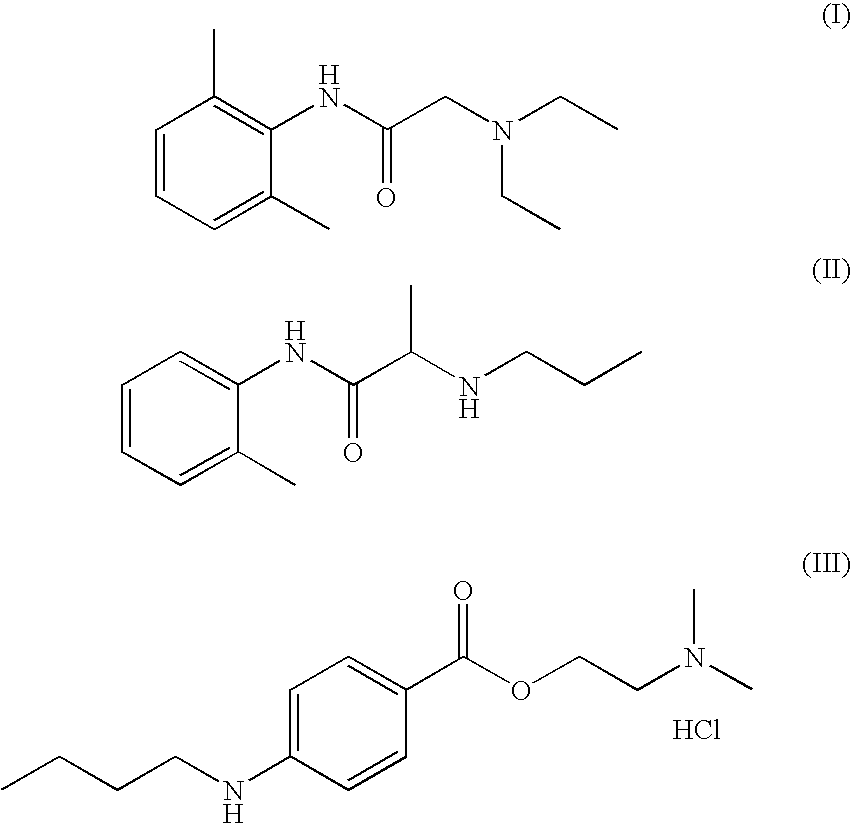
Anesthetic composition for topical administration comprising lidocaine, prilocaine and tetracaine
a technology of tetracaine and lidocaine, which is applied in the direction of biocide, plant growth regulator, pharmaceutical non-active ingredients, etc., can solve the problems of only performing surgical techniques, stinging at the wound site, and often problematic use of transdermal anesthetics (i.e. through the skin) to achieve the effect of increasing tim
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
Preparation of the Composition
[0030] Tubes of 30 g were prepared with the composition per tube described in the following table:
Component% (w / w)Dissolution ADistilled water31.82% Nipagin M-Ac0.08%Nipasol M-Ac0.02%Tween-201.00%Guar gum1.50%Dissolution BTetracaine HCl4.00%Distilled water45.00% Dissolution CLidocaine base 1.5%Prilocaine base 1.5%Dissolution DDistilled water1.00%Topical hyaluronidase0.08%Dissolution ETween 800.50%Dissolution FMethylpyrrolidone 10%Dissolution GDMSO2.00%
[0031] Lidocaine base and prilocaine base were weighed and sieved through a 2 mm mesh. Components of dissolutions A, B, D, E, F and G were weighed separately. The amounts of required distilled water for each dissolution were also prepared in 100 mL recipients. Distilled water for dissolution A was heated in an appropriate recipient and Nipagin and Nipasol were added until dissolved. The mixture was left to cool. Then, Tween-20 was added and the mixture was shacked with a stripping knife without lather...
PUM
| Property | Measurement | Unit |
|---|---|---|
| w/w percentages | aaaaa | aaaaa |
| melting point | aaaaa | aaaaa |
| melting point | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com