Devices and methods to conform and treat body cavities
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
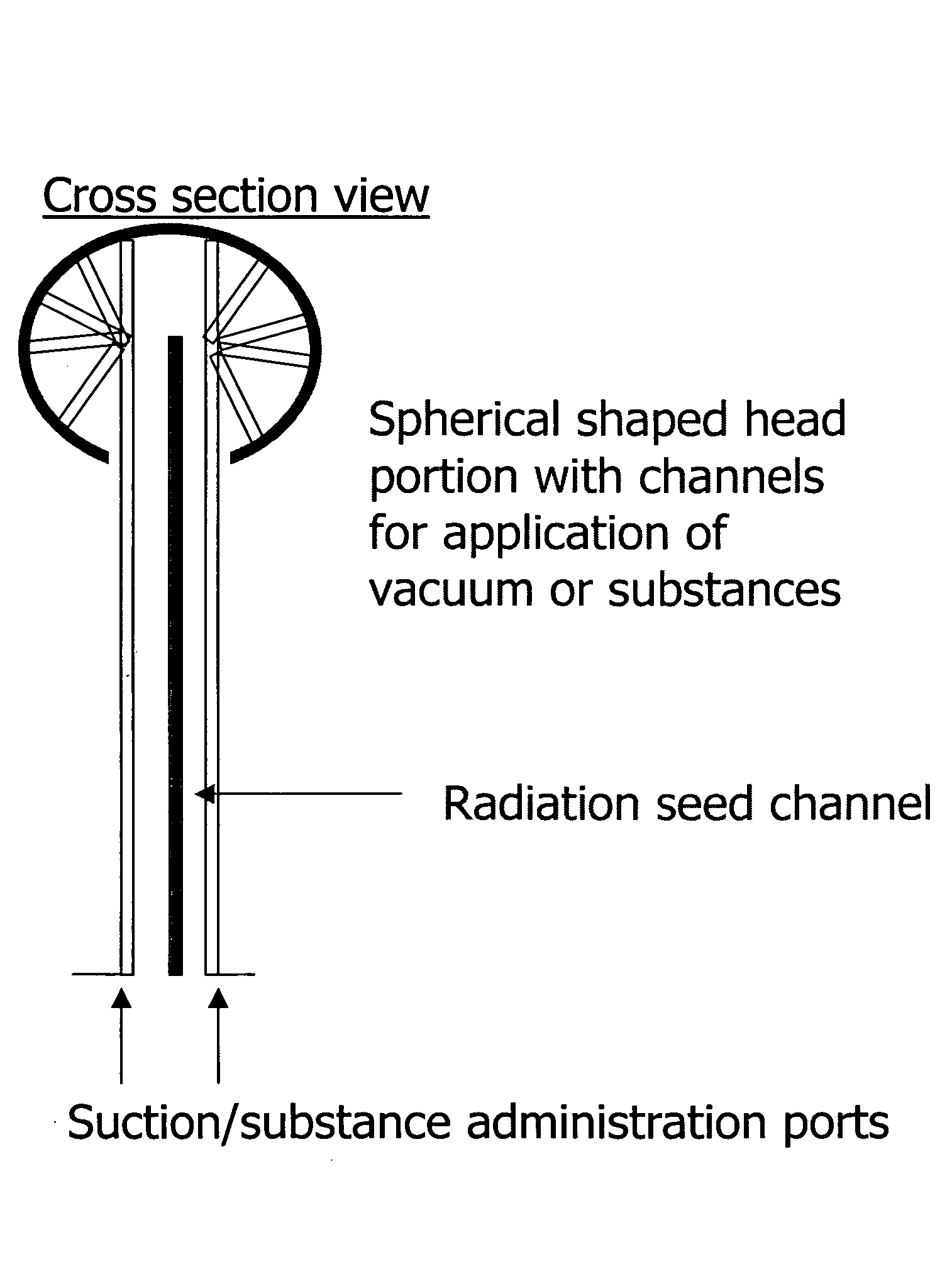
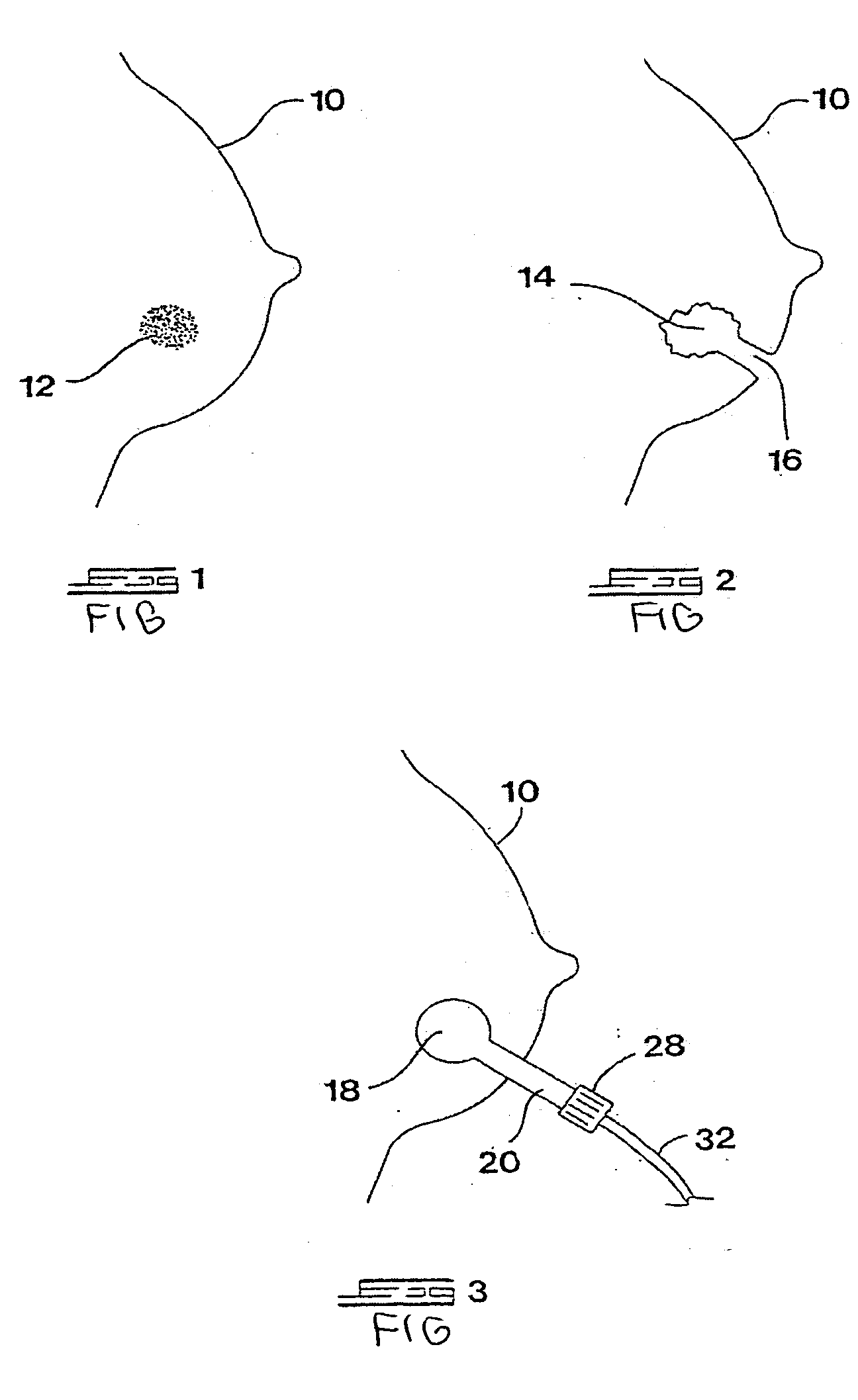
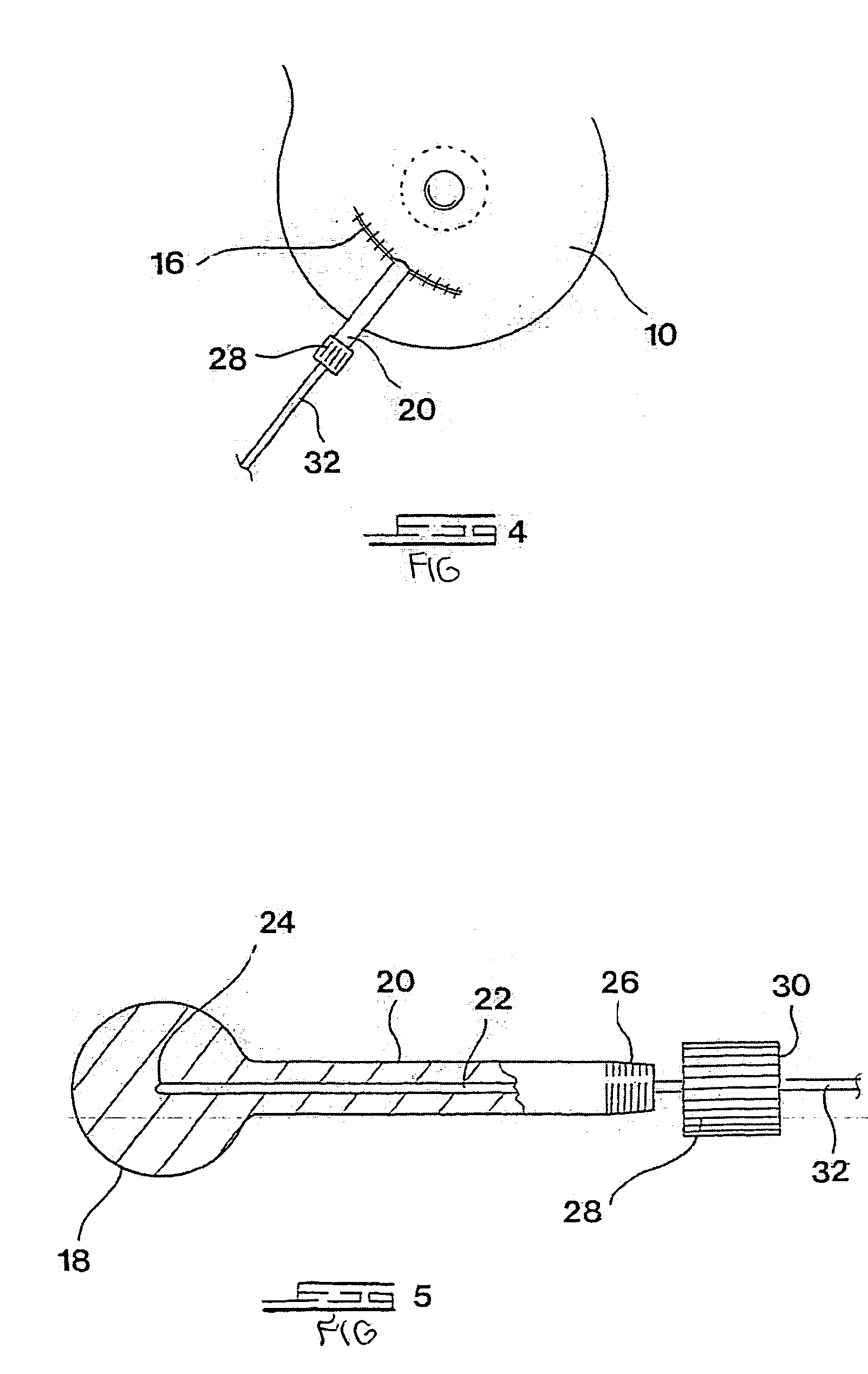
Method used
Image
Examples
example 1
[0059]
TABLE 1Calculation of the volumes treated in example 1 of the presentinvention and comparison to traditional treatment:VolumeBiologically effective dose to:irradiated:1.The whole breast = 64.4 GyApproximately850 cc2.Whole breast plus tumor bed: 77.16 Gy600 cc3.Shell of breast tissue from the surface of the114 ccapplicator of diameter 5 cm: the dose drops from21 Gy surface dose to 26.9 Gy at a radius of 3.5 cmand the volume of this irradiated shell of tissue is
[0060] Therefore volume of breast tissue spared from irradiation: (850−114)cc=736 cc.
[0061] The volumes are exemplary and relate to an “average” sized breast. The volume in each case may vary, of course, according to the size of the breast.
example 2
[0062]
TABLE 2Variation of the radiation dose from the surface of a 5 cm diameterspherical applicator:Table 2 shows how the dose drops from 21 Gy at the surface of theembodiment of the present invention to the radii indicated, as wellas the volumes of tissue irradiated to the corresponding dose levels:Radius (cm)Dose (Gy)BED(7) (Gy)Volume irradiated (cc)2.5218402.7186482.5 − 65.5 = 172.816.85792.0 − 65.5 = 26.53.014.547.5113 − 65.5 = 47.53.510.827.4179.7 − 65.5 = 114.2
[0063] Generally, the method of invention can be used to deliver a radiation dose at the surface of the applicator in the range 5-30 Gy.
[0064] Similar considerations are valid for the delivery of other physical agents: In the case of heat generated by radiofrequency, the change in tissue density around an applicator can be observed and measured under real-time ultrasound to indicate the thickness of the shell treated around the applicator of the present invention. The same holds true for cold administered for example b...
example 3
[0066]
TABLE 3The volumes of surgically removed breast tissue plus the valuesterilized in principle by the local administration of a physical agent,in this example radiation:TumorVolume surgicallydiameterVolume ofVolume of surgicallyremoved plus(cm)tumor (cc)removed shellirradiated shell10.565.5182.51.51.887.2201.22.04.2113.1227.12.58.2143.8257.8
[0067] Generally, the method of the invention would be suitable to treat a layer of tissue surrounding an embodiment of the present invention of between 0 and 20 millimeters thickness.
[0068] Treatment using the method and an embodiment of the present invention can as much as treble the volume of tissue rendered “safe” surgically, yet the irradiated volume is only about 25% of the volume of breast tissue irradiated by the standard current method.
[0069] In one embodiment of the present invention, the treatment time comprises the time required to insert the applicator and deliver, for example, a radiation dose of 21 Gy. This should take approx...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com