Valve prosthesis for implantation in body channels
a valve prosthesis and valve technology, applied in the direction of prosthesis, catheter, blood vessel, etc., can solve the problems of mainly difficulty in breathing, patients can have syncope, and difficulty in breathing, and the evolution of such a disease is disastrous
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
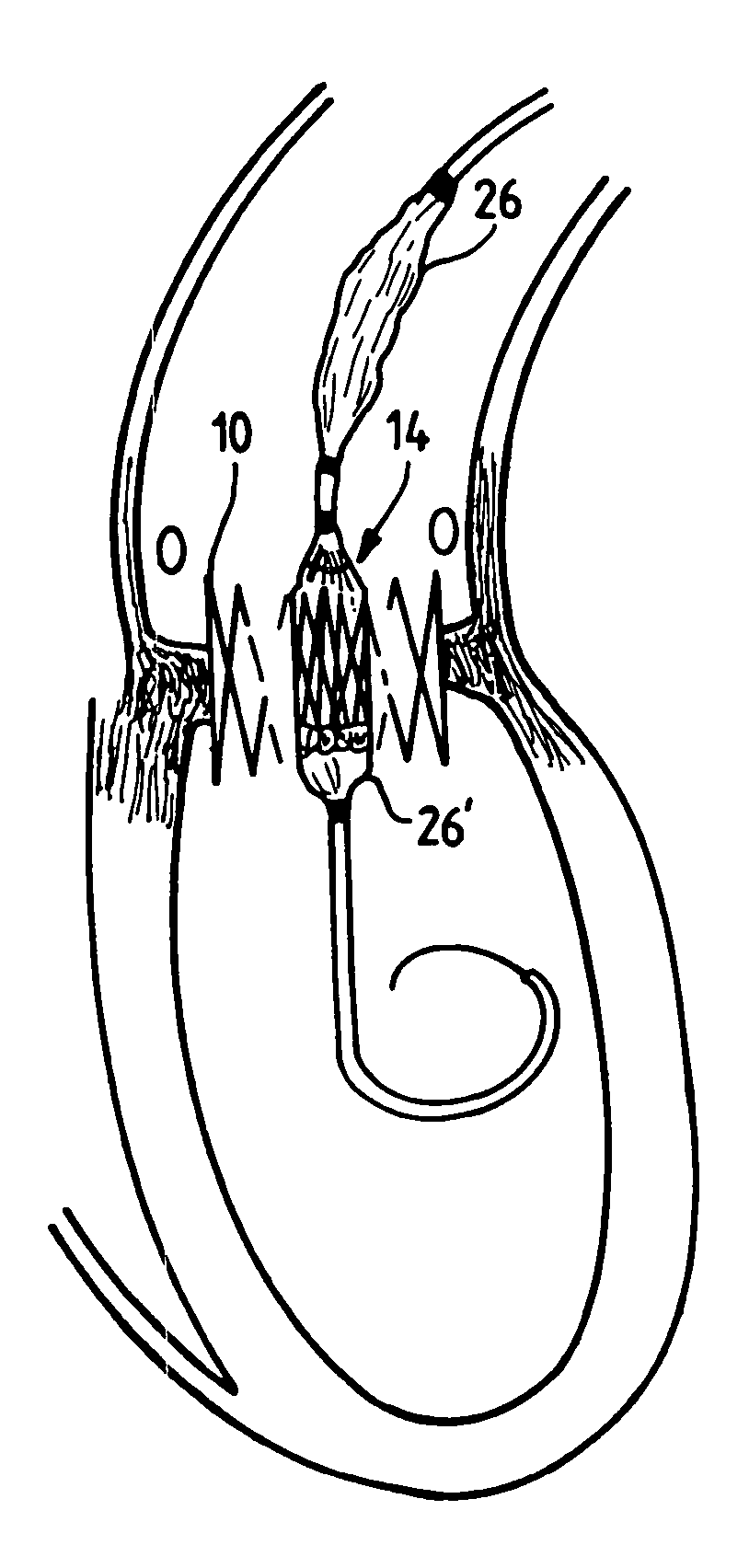
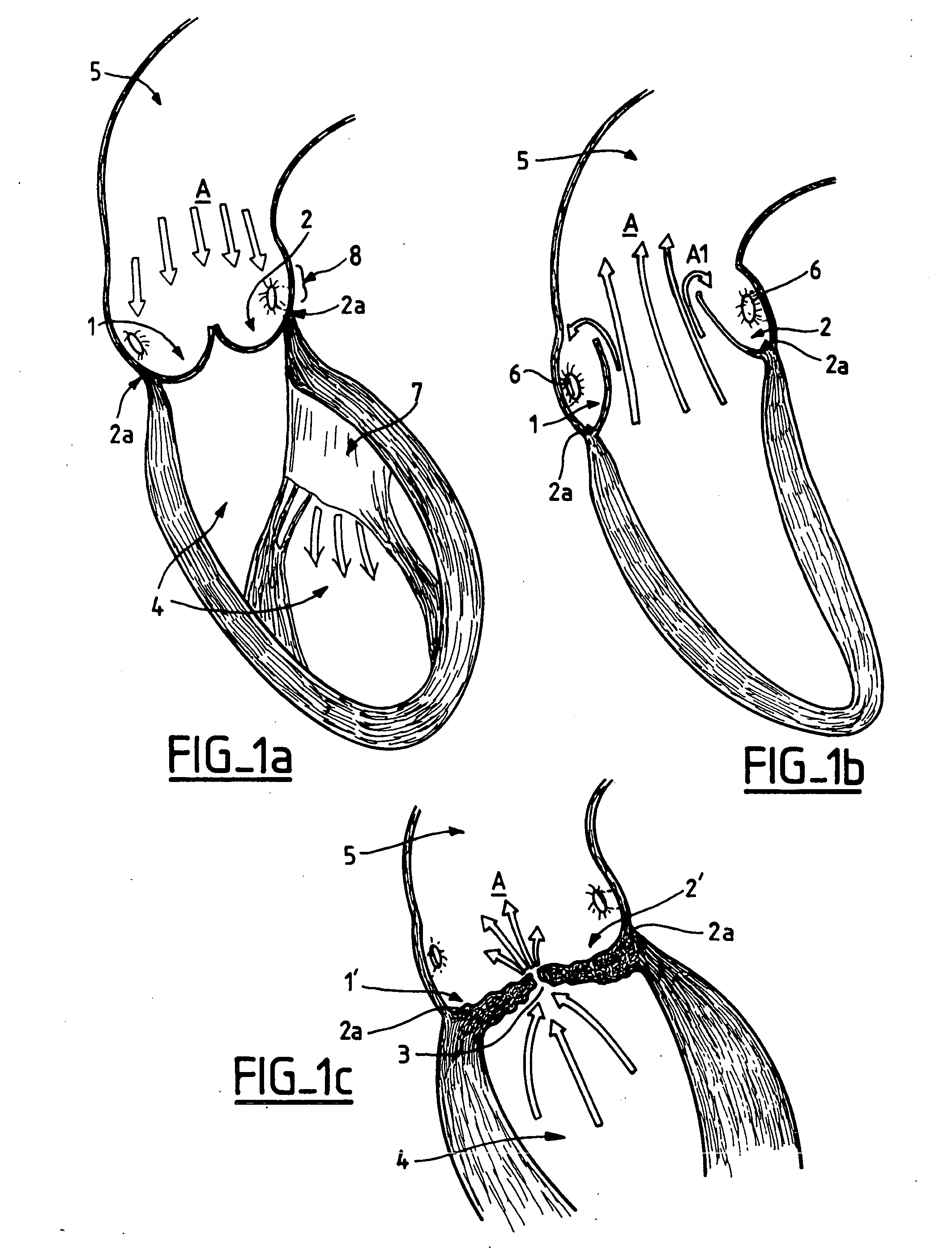
[0068] In the diastole and systole illustrations of section views of FIGS. 1a and 1b, the arrows A indicates the general direction of the blood flow. The semi-lunar leaflets 1 and 2 of a native aortic valve (with only two out of three shown here) are thin, supple and move easily from the completely open position (systole) to the closed position (diastole). The leaflets originate from an aortic annulus 2a.
[0069] The leaflets 1′ and 2′ of a stenosed valve as illustrated in FIG. 1c, are thickened, distorted, calcified and more or less fused, leaving only a small hole or a narrow slit 3, which makes the ejection of blood from the left ventricle cavity 4 into the aorta 5 difficult and limited. FIGS. 1a to 1c show also the coronary artery ostium 6a and 6b and FIG. 1 a shows, in particular, the mitral valve 7 of the left ventricle cavity 4.
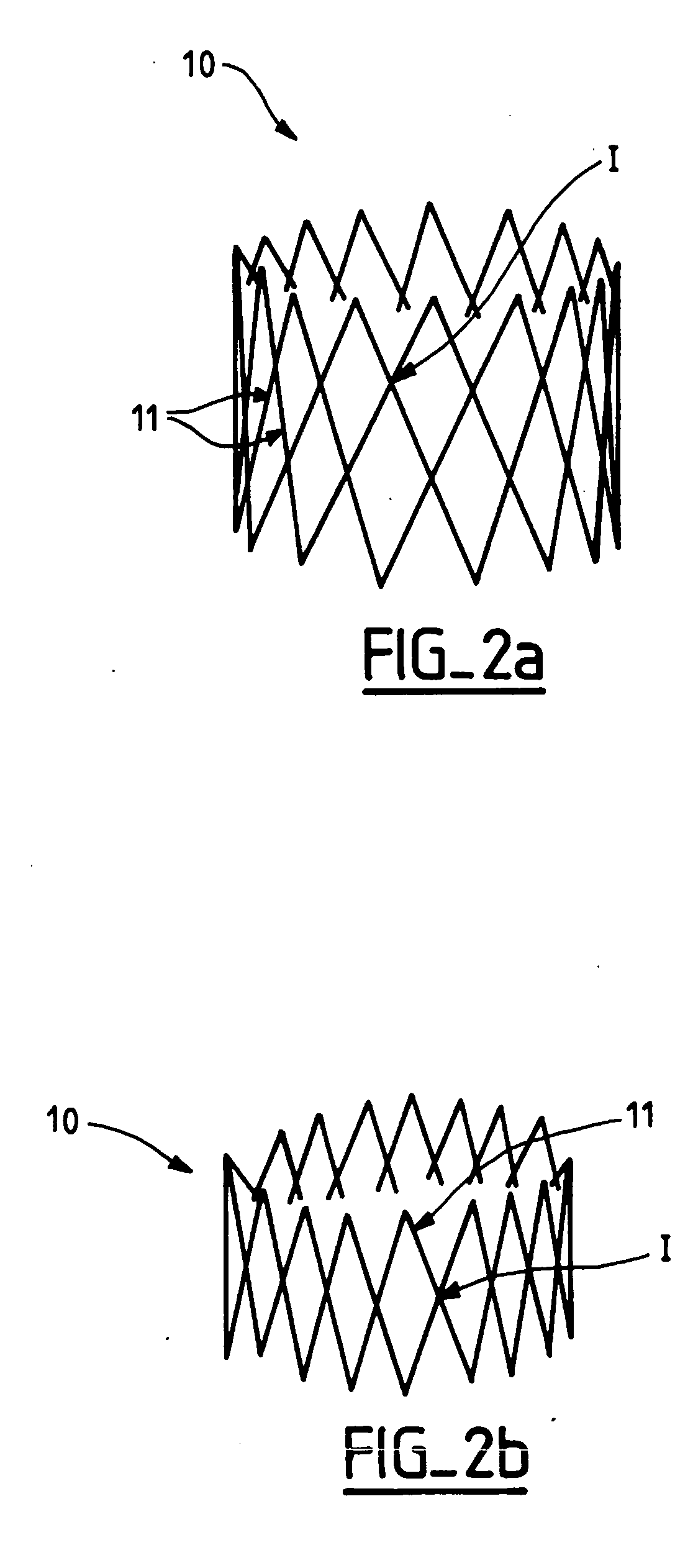
[0070] An implantable valve according to the invention essentially comprises a supple valvular structure supported by a strong frame. The positioning ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com