Methods for repairing damaged intervertebral discs
a technology of intervertebral discs and methods, applied in the field of medical devices, can solve the problems of reduced disc volume, reduced disc shock absorption ability, back and leg pain, etc., and achieve the effects of minimal collateral damage, reduced disc volume, and enhanced visualization of the sha
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
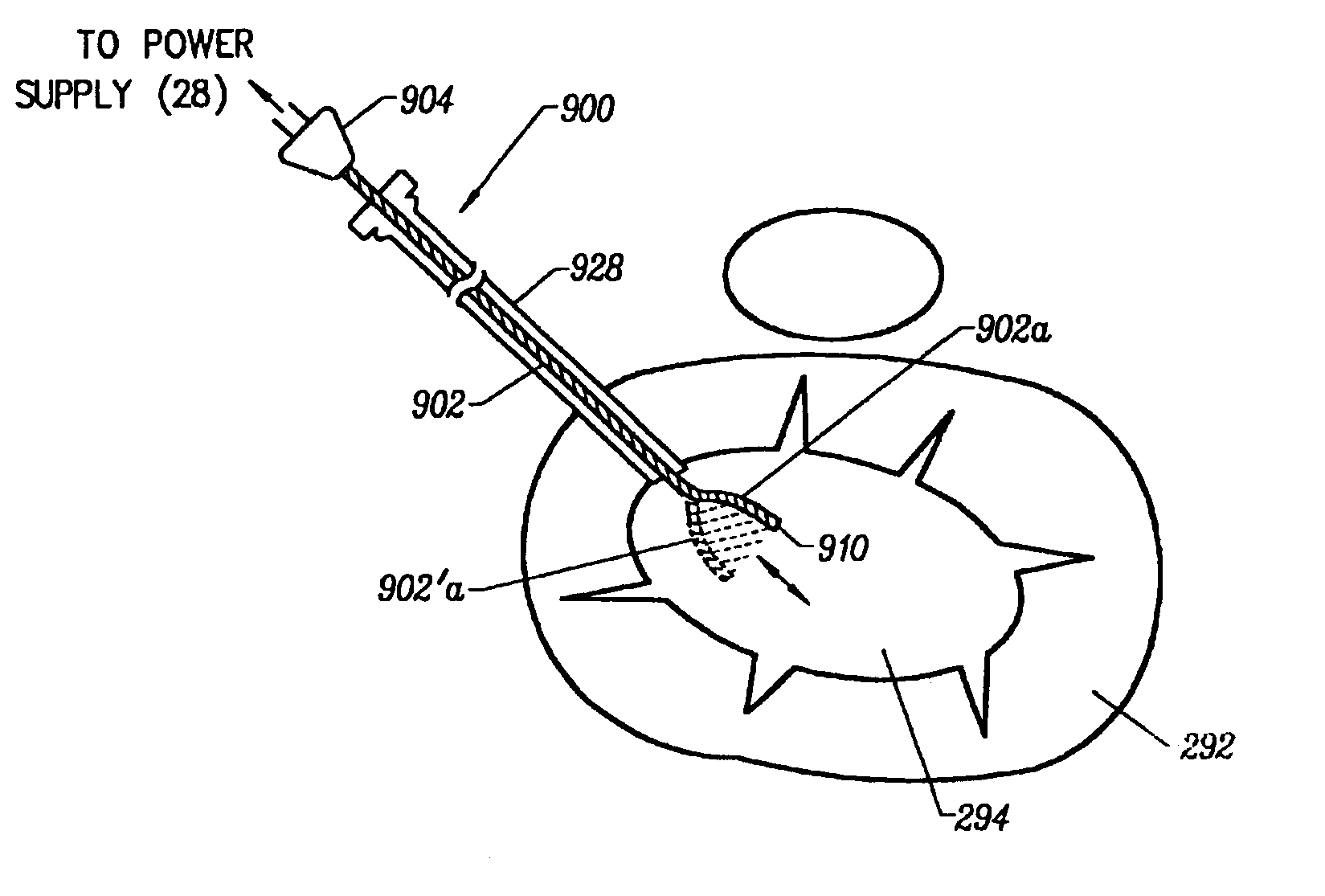
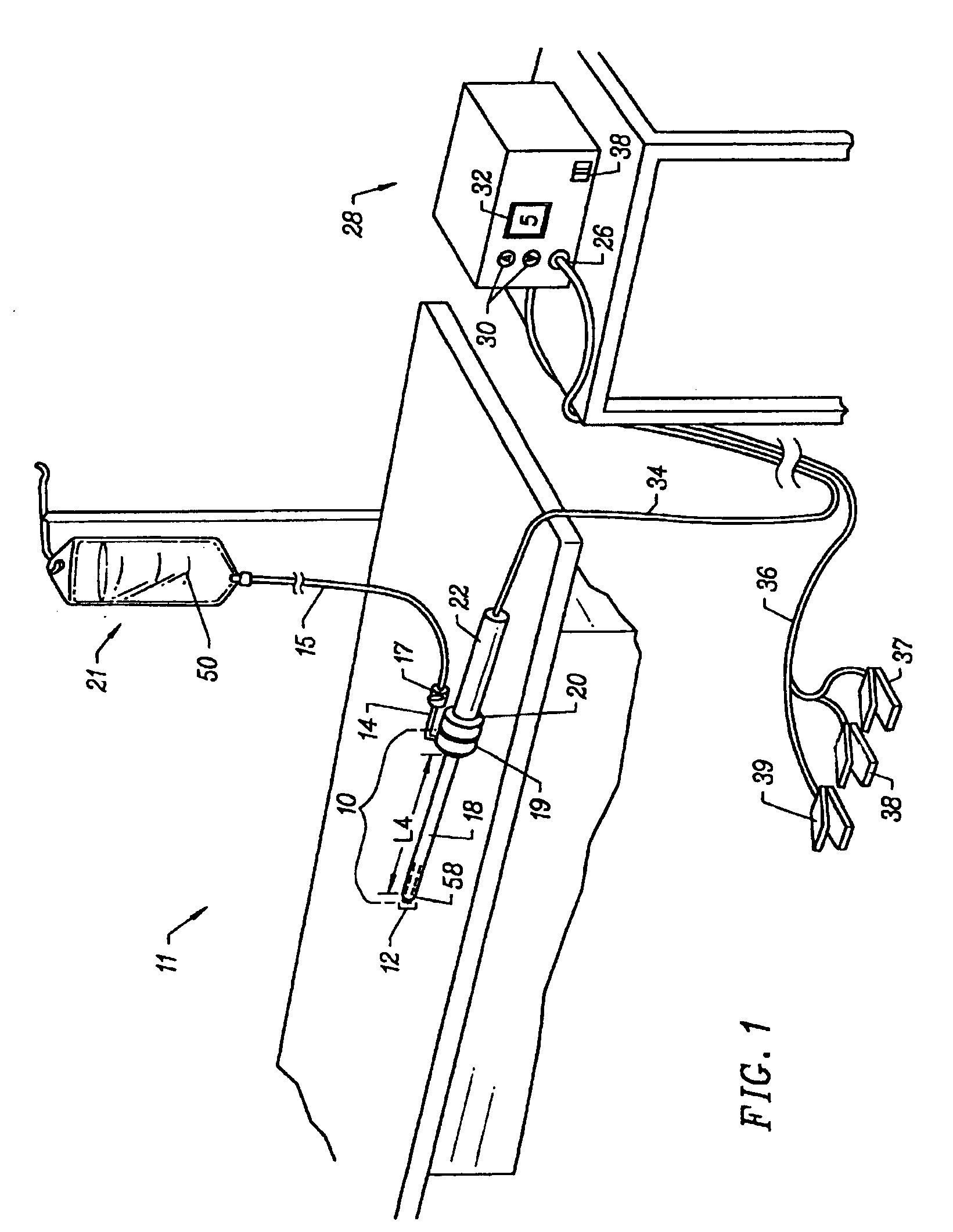
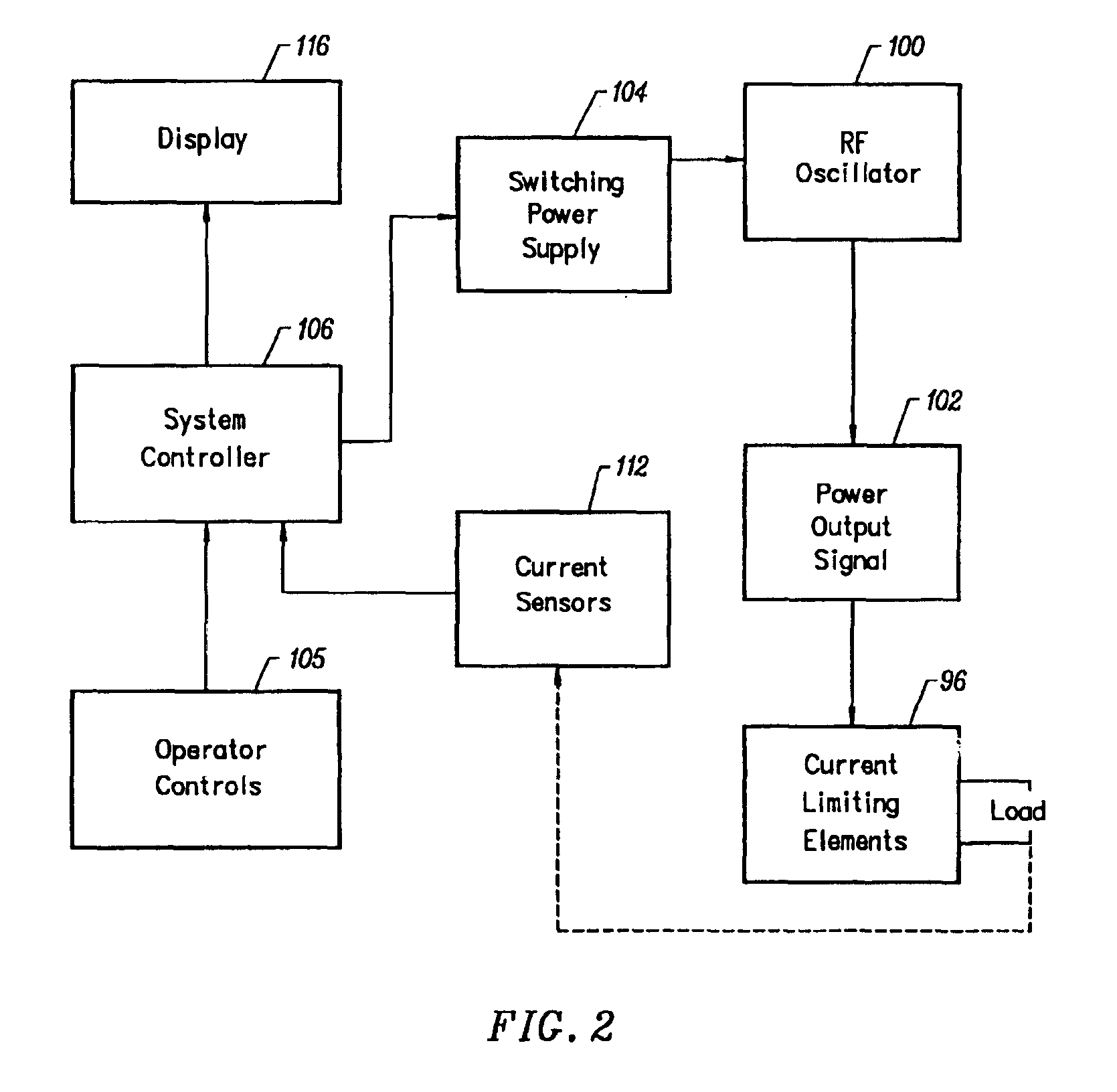
[0074]The present invention provides systems and methods for selectively applying electrical energy to a target location within or on a patient's body, particularly including support tissue or other body structures in the spine. These procedures include treating interspinous tissue, degenerative discs, laminectomy / discectomy procedures for treating herniated discs, decompressive laminectomy for stenosis in the lumbosacral and cervical spine, localized tears or fissures in the annulus, nucleotomy, disc fusion procedures, medial facetectomy, posterior lumbosacral and cervical spine fusions, treatment of scoliosis associated with vertebral disease, foraminotomies to remove the roof of the intervertebral foramina to relieve nerve root compression and anterior cervical and lumbar discectomies. These procedures may be performed through open procedures, or using minimally invasive techniques, such as thoracoscopy, arthroscopy, laparascopy or the like.
[0075]The present invention involves te...
PUM
| Property | Measurement | Unit |
|---|---|---|
| volume | aaaaa | aaaaa |
| volume | aaaaa | aaaaa |
| diameter | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com