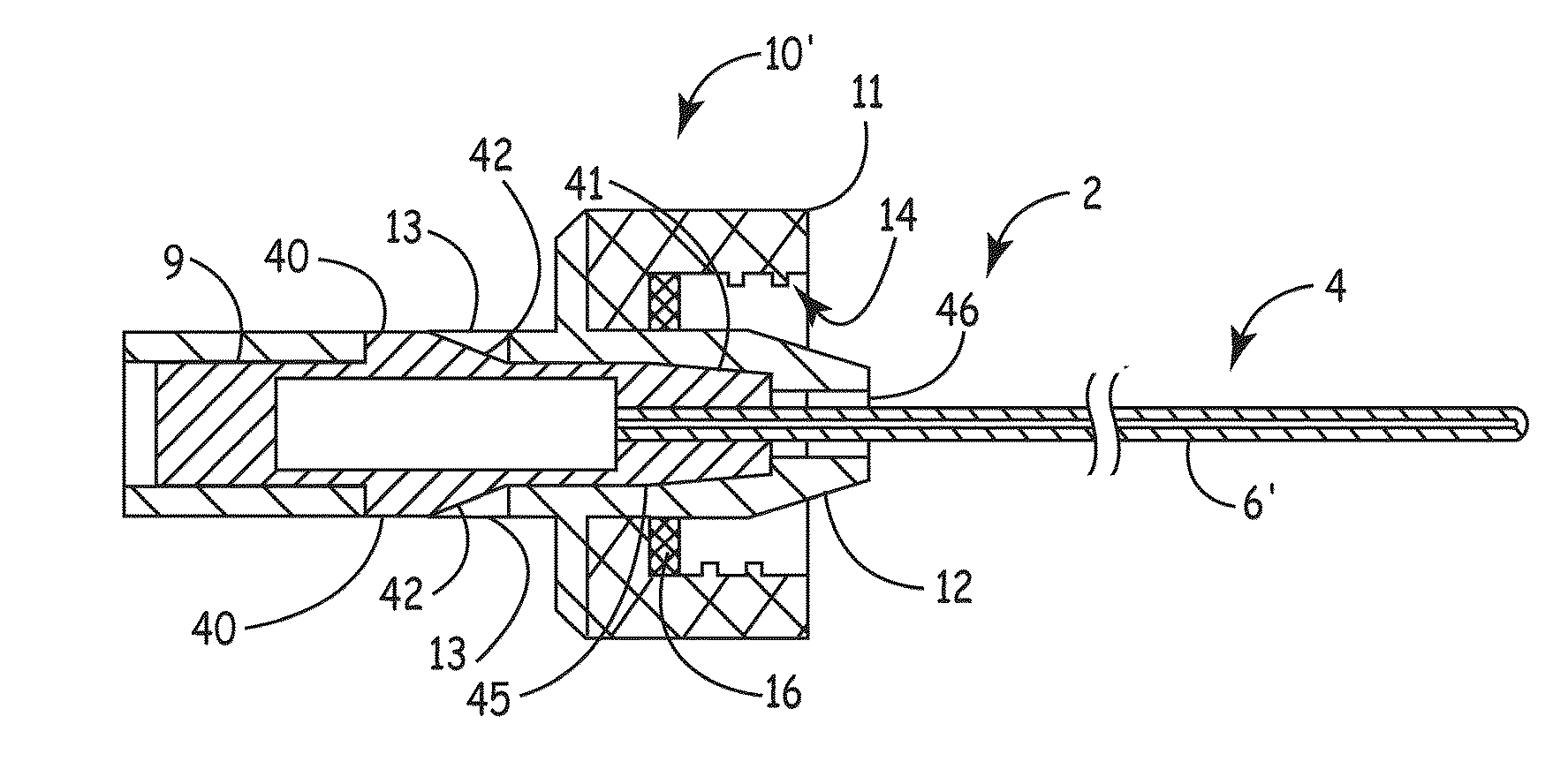
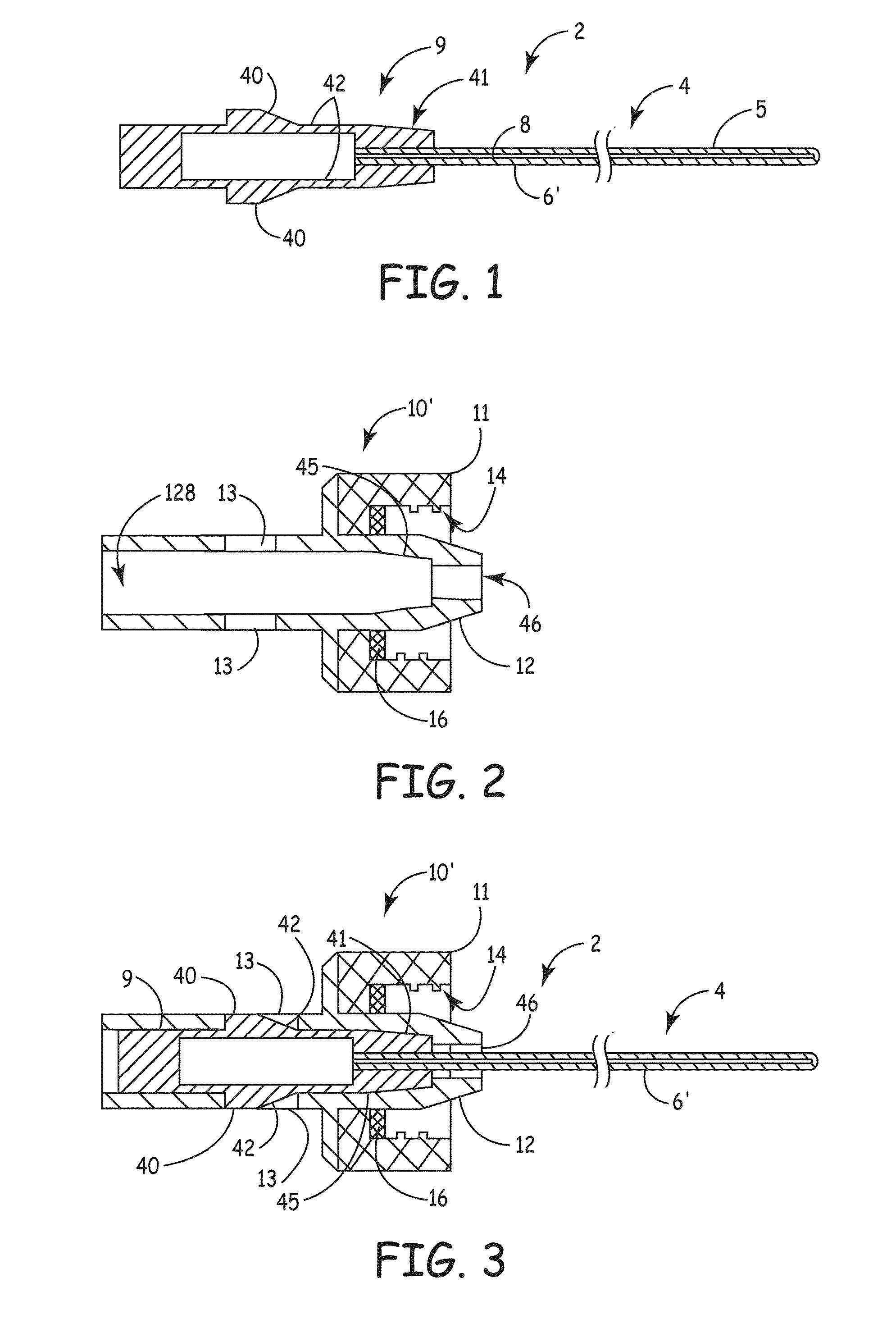
[0007]An embodiment of the invention, herein referred to as “the Device”, is an elongate member that can be inserted into a
medical device, such as a catheter or a drainage tube, for the prevention and treatment of infectious organisms within the
medical device and in proximity to the elongate member, and further prevents the migration of infectious organisms into the body by providing a
physical barrier. For the sake of simplicity, the term “catheter” is used for all medical devices in which the present invention can be inserted and used to treat, prevent, and eliminate infectious organisms.
[0009]The present invention prevents and treats infectious organisms in the lumen of in-dwelling medical devices, such as long-term, trans-dermal catheters. The invention also prevents the formation of
thrombus within the lumen of
indwelling catheters by physically blocking blood from entering the catheter in the proximity of the Device, and, in some embodiments, by the incorporation of an
antithrombotic agent.
[0010]One useful application of the invention is in preventing infections in people with
hemodialysis catheters. The present invention prevents or eliminates infectious organisms on the luminal wall of a catheter by providing a means for the prolonged presence of an
antimicrobial agent and / or providing a means for periodically scrubbing the luminal wall of the catheter to remove the
biofilm in which infectious organisms proliferate.
[0011]Competing methods for preventing, eliminating, and treating infectious organisms in the lumen of a catheter are in limited use. One method uses an
antimicrobial coating on or in the internal wall of the catheter. The issues that have precluded widespread use include the antimicrobial
coating eventually wearing off, losing
potency, or becoming covered with blood products, rendering the
coating ineffective. When
antibiotics are used as the antimicrobial agent, there is an additional concern regarding the emergence of resistant organisms to
antibiotics and the risk of
anaphylaxis to the
antibiotics. Another method for treating infectious organisms in the lumen is the use of an antibiotic or antimicrobial liquid, known as a locking agent or locking solution. In this method, an antimicrobial fluid is injected into the catheter, and a cap is attached to the hub of the catheter to prevent the fluid from leaking out of the catheter and to prevent infectious organisms from entering into the lumen.
[0013]In the case of using the Device with
dialysis catheters, the present invention is designed to be replaced regularly after each
dialysis session, approximately three times per week. This replenishes the antimicrobial agent with each replacement, resulting in a consistent and
high concentration of antimicrobial agent present within the catheter on an ongoing basis resulting in decreased
risk of infection.
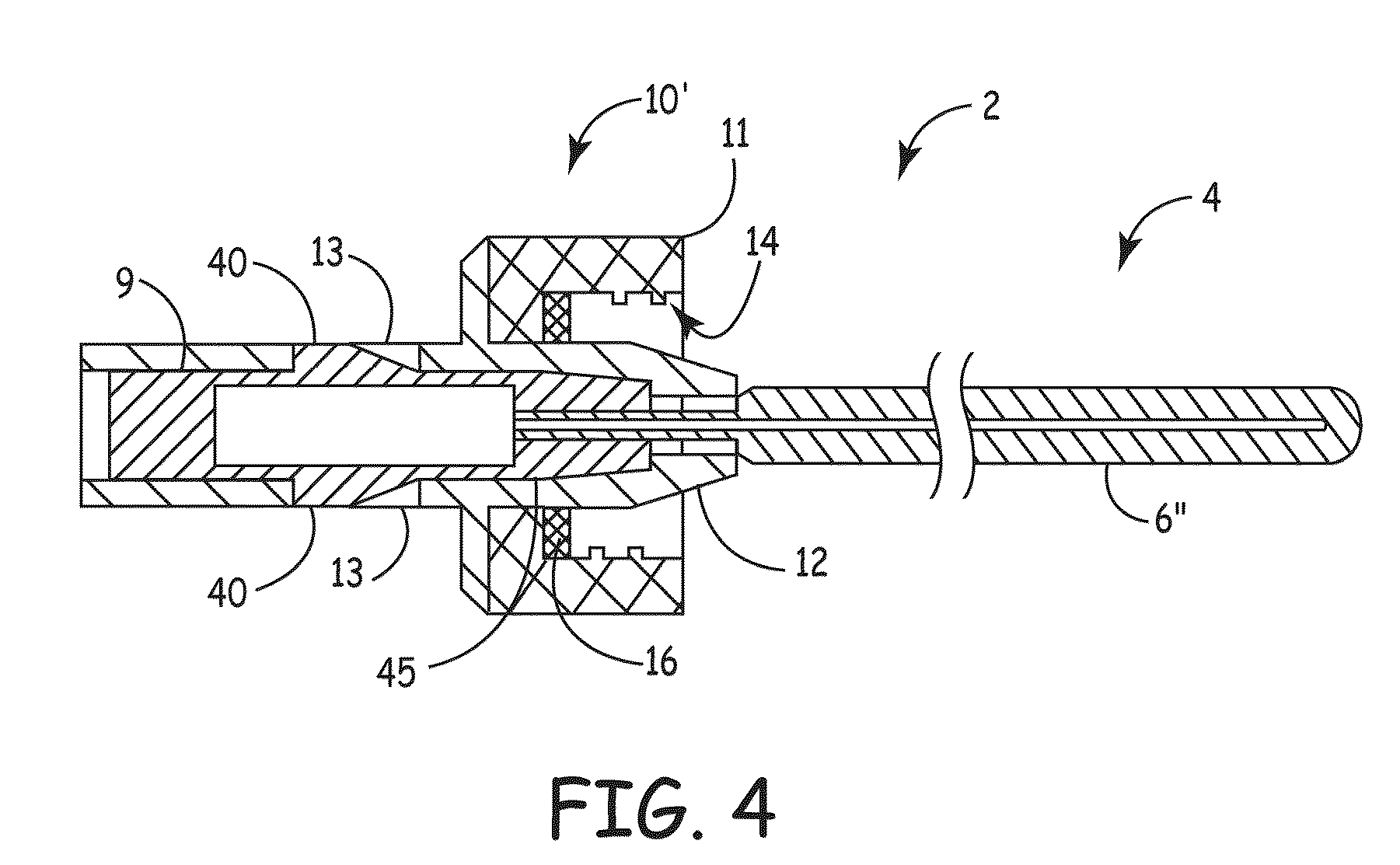
[0014]In addition, separation between the antimicrobial agent and blood can result in lower
infection rate, fewer side effects, and less risk of developing
resistant bacteria because a non-antibiotic antimicrobial is used. In certain embodiments, the present invention creates a
physical barrier between the blood and the antimicrobial agent. The barrier greatly reduces the exchange of antimicrobial agent with
blood circulating in the body, resulting in fewer side effects from the antimicrobial agent. This can result in a more consistent level of antimicrobial agent along the length of the catheter adjacent to the Device. Additionally, the barrier reduces the amount of antimicrobial agent entering the bloodstream, thus reducing the risk of an adverse reaction to the agent or developing organisms resistant to the antimicrobial agent. In comparison, it is well-known that liquid locking agents can and do migrate into the bloodstream, and the blood can migrate into the catheter, thus reducing the effectiveness of the antimicrobial agent, increasing the possibility of
bacteria entering the bloodstream and increasing the rate of
thrombosis in the catheter. The act of flushing the catheter lumen with a fluid agent and / or inserting a plug into the lumen will result in the removal of blood from the lumen and thus reduce the risk of
thrombosis. If the liquid agent is an anti-thrombotic lock, such as heparinized
saline, the risk of
thrombosis is further reduced. The use of a plug, as described in the present invention, prevents the blood from reentering the lumen and results in a
lower risk of thrombosis in the lumen.
 Login to View More
Login to View More  Login to View More
Login to View More