Device and method for reconstruction of osseous skeletal defects
a technology for osseous skeletal defects and medical devices, applied in the direction of prosthesis, ligaments, shoulder joints, etc., can solve the problem of not providing means for reconstituting normal bony structures, and achieve the effect of immediate stabilization of the extremity
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
Femoral Resection
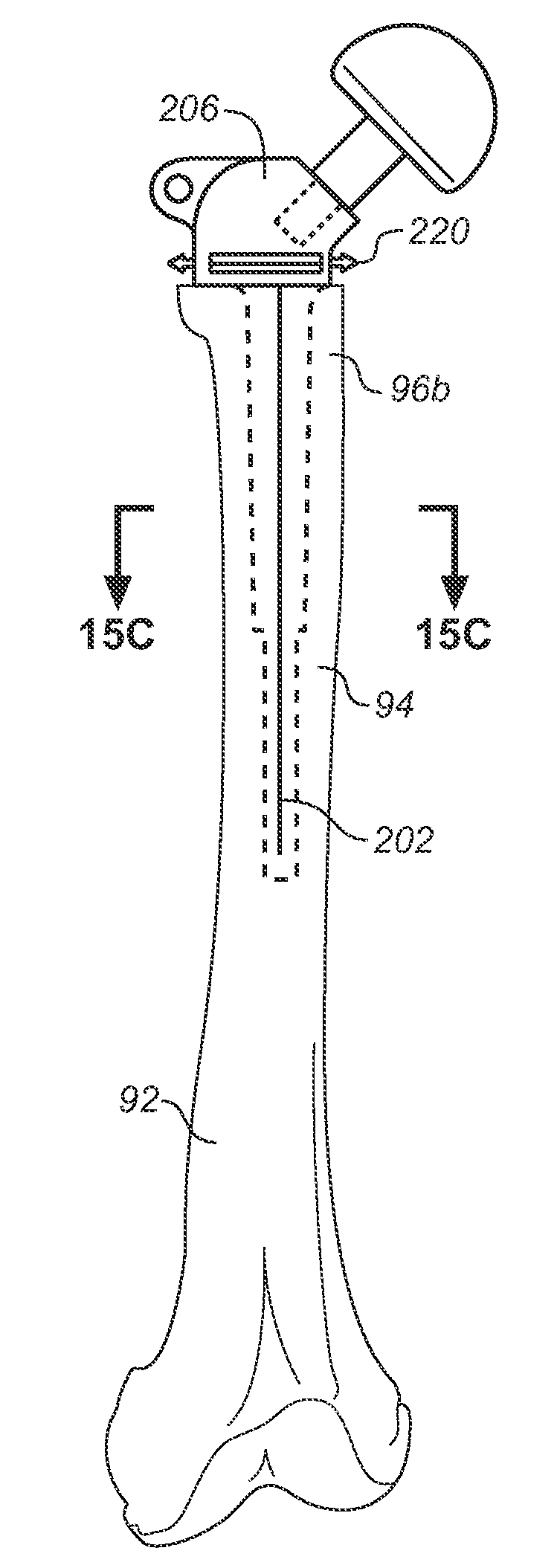
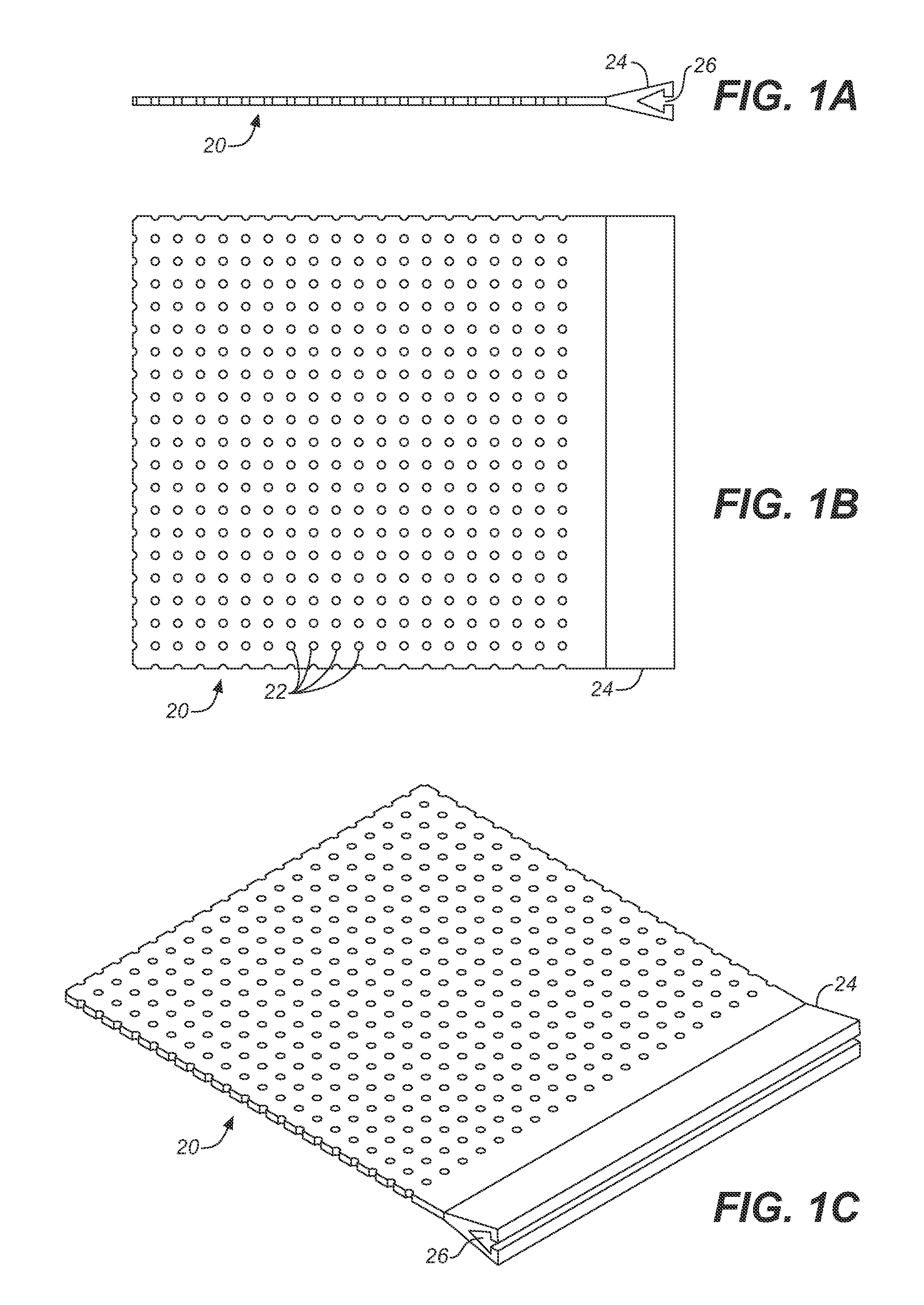
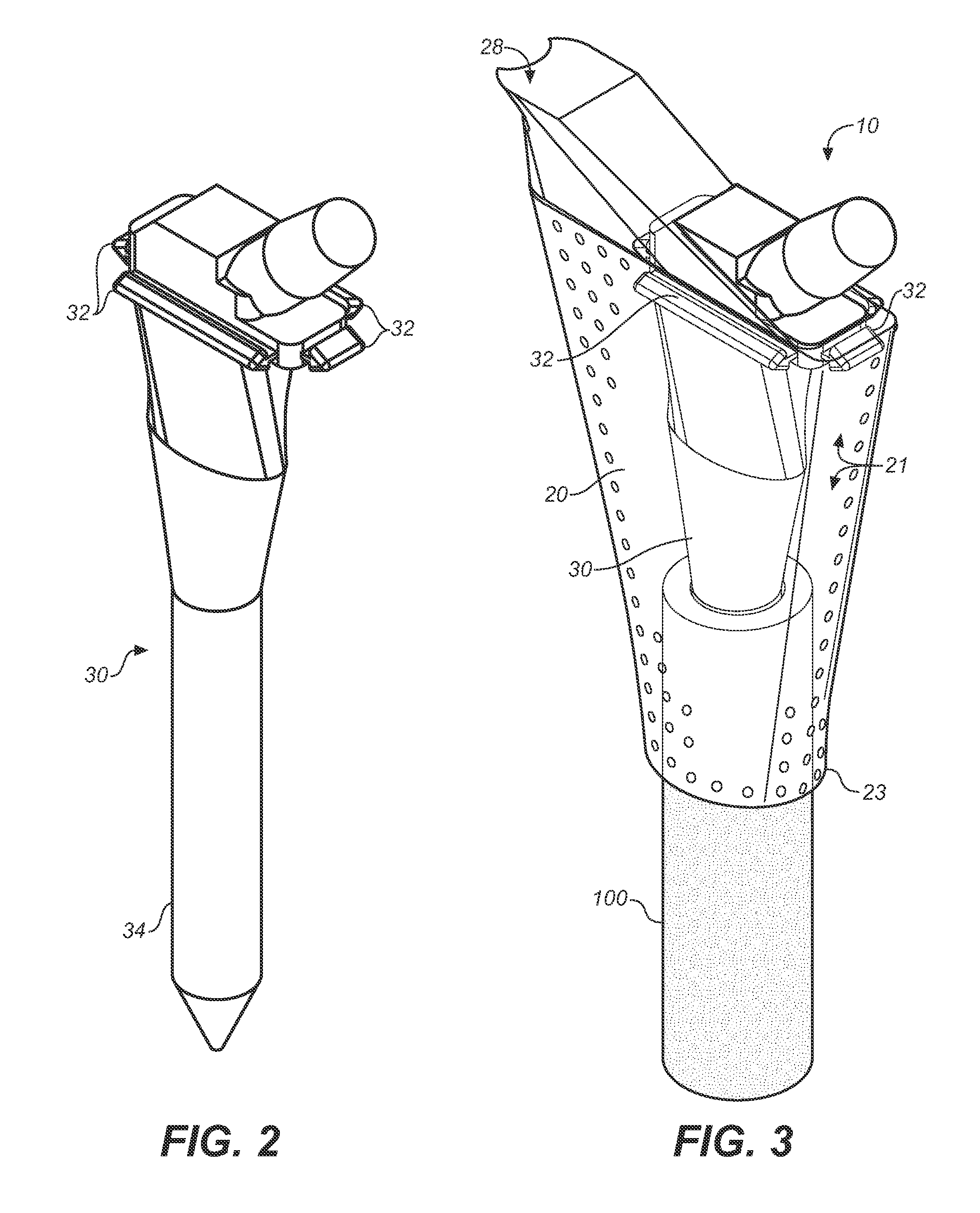
[0067]Referring next to FIGS. 2 and 3, the present invention is utilized in resection of a proximal femoral osteosarcoma in a 15 year old male. FIG. 2 illustrates a femoral prosthesis 30 of the present invention, and FIG. 3 illustrates an implantable device 10 comprising the femoral prosthesis 30 surrounded by a flexible member 20. The implantable device 10 is used to reconstruct the proximal femur of a patient (not shown) in a five-step process. This process is adaptable for use, as will be evident to those of skill in the art, within any of the large joints including the hip, knee, shoulder, elbow, and ankle.
[0068]First, a prosthesis 30 is selected for use, with consideration given to the appropriate height and diameter of the stem 34 in order to achieve adequate fixation, leg length restoration, and soft tissue tension in the extremity. The prosthesis 30 is provided with one or more attachment members 32. In this instance, rails are placed circumferentially aroun...
example 2
Acetabular Reconstruction
[0073]With reference next to FIGS. 4A-4D, the present invention may be used to treat a large superior defect of the acetabulum 112 in the case of hip dysplasia or in the revision setting. FIG. 4A shows the porous surface of an uncemented acetabular cup prosthesis 40 with peripheral attachment members 42 disposed proximate the rim of the hemispherical prosthesis. FIG. 4B depicts a patient's iliac wing 110 and acetabulum 112, the latter having a large superior dome defect. As shown in FIG. 4C, the cup 40 is placed in the acetabulum and can be fixed to the residual acetabulum using a combination of press-fit with available bone, or with acetabular screws, or using a combination of modular cup attachments and screws placed into the ilium, ischium, and pubis.
[0074]The residual bone loss is reconstituted by attachment of the flexible member 20 to the margins 42 of the cup 40 with attachment members 44, as shown in FIG. 4D, and by filling the resultant cavitary spa...
example 3
[0075]With reference next to FIGS. 5A through 8, a total knee arthroplasty with a comminuted supracondylar fracture with major bone loss is treated with a long press-fit intramedullary revision femoral component embedded in the residual femoral diaphysis. FIGS. 5A through 5C illustrate a femoral prosthesis 50 of the present invention, and FIG. 6 illustrates an implantable device 12 comprising the femoral prosthesis 50 surrounded by a flexible member 20. The implantable device 12 is used to reconstruct the distal femur of a patient (not shown) in a multi-step process.
[0076]The process described in Example 1 is adapted for use on the distal femur, wherein first a prosthesis 50 is selected for use, with consideration given to the appropriate height and circumference of the stem 52. The prosthesis 50 is provided with rounded artificial articular surfaces 56, 58, simulating the medial epicondyle and medial condyle of the femur and the lateral epicondyle and lateral...
PUM
| Property | Measurement | Unit |
|---|---|---|
| diameter | aaaaa | aaaaa |
| diameter | aaaaa | aaaaa |
| pore sizes | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com