Apparatuses and methods for performing minimally invasive diagnostic and surgical procedures inside of a beating heart
a technology of applied in the field of apparatus and methods for performing minimally invasive diagnostic and surgical procedures inside of the beating heart, can solve the problems of valvular insufficiency, inability to precisely measure, blind dilation, etc., and achieves sufficient intracardial pressure, minimizes the need for cardiopulmonary bypass, and minimizes the risk of air introduction
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
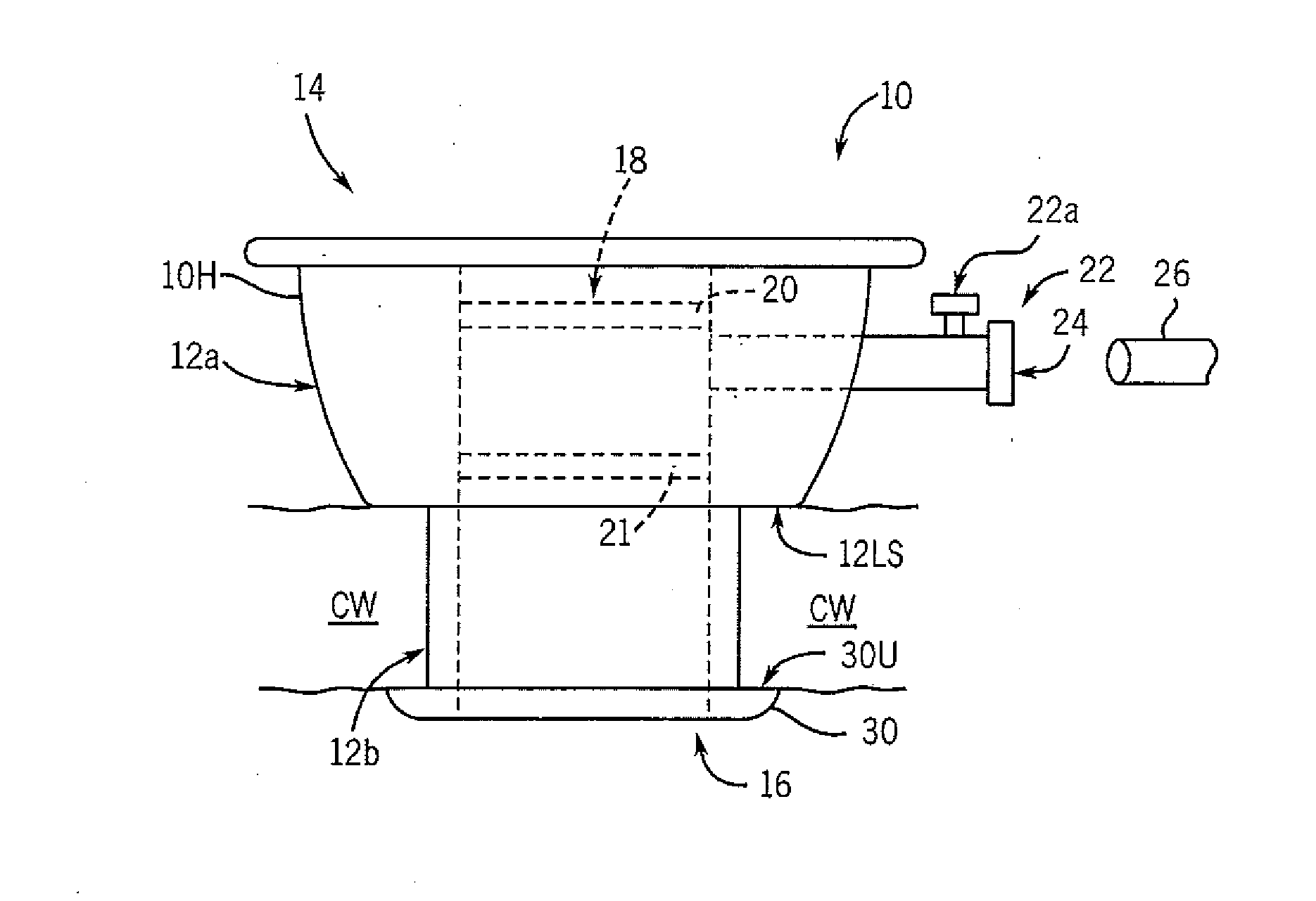
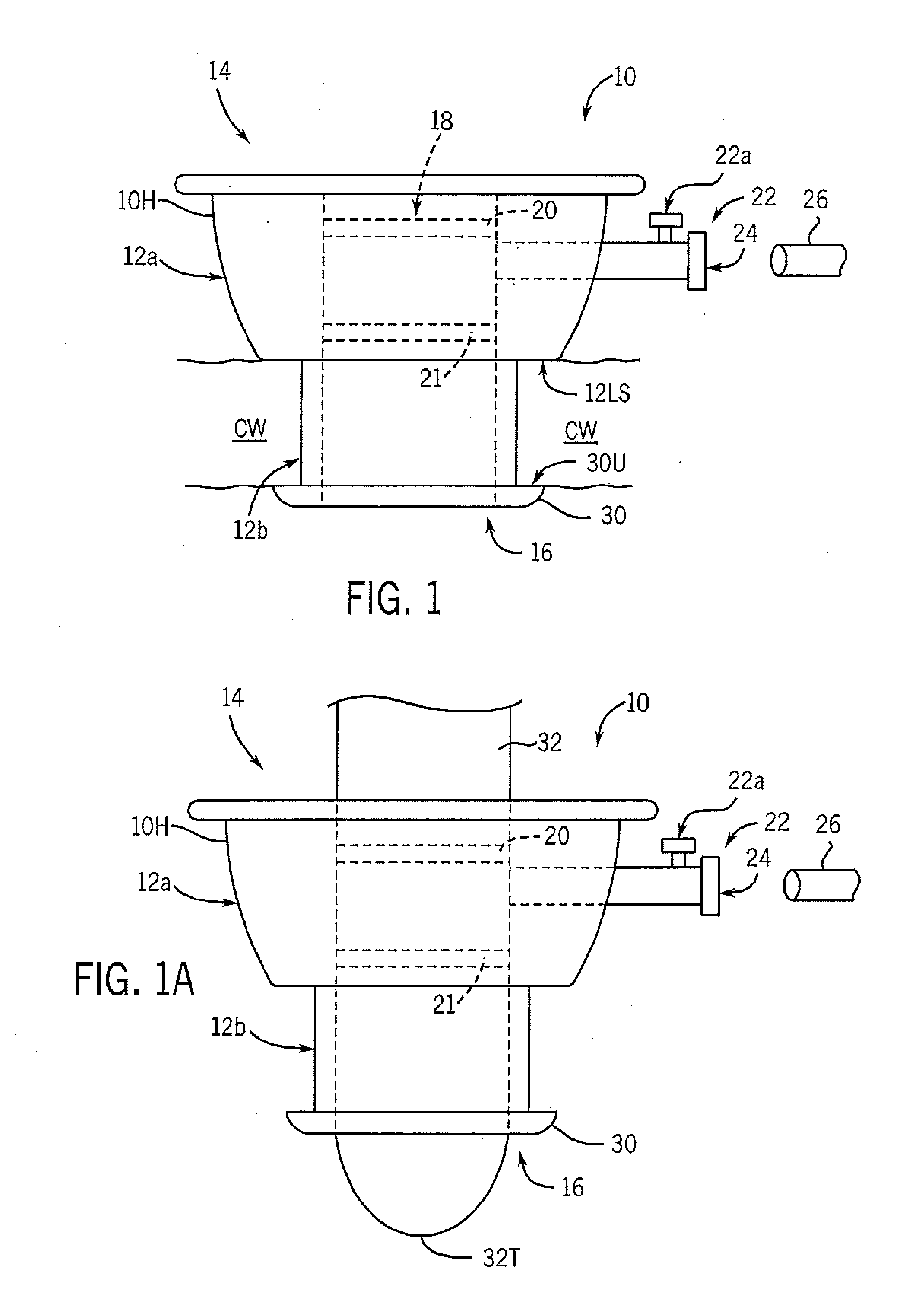
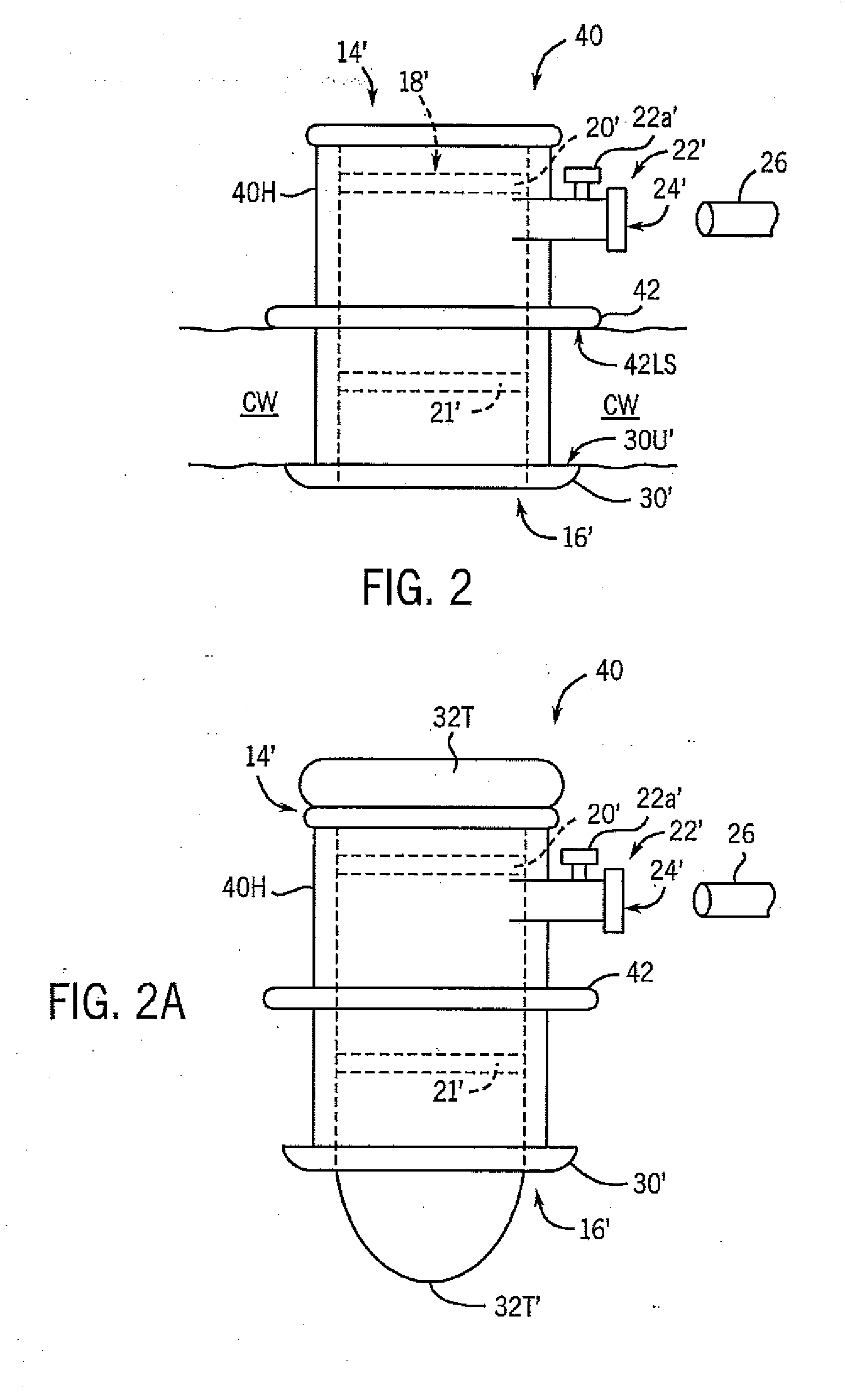
[0066]The present invention provides apparatuses and methods for performing minimally invasive diagnostic and surgical procedures inside of a beating heart, thereby obviating the need for administration of cardioplegia and cardiopulmonary bypass (CPB). Procedures contemplated by the present invention can include mitral and tricuspid valve repair, aortic and pulmonary valve repair, and repair of intracardiac defects, such as atrial and ventricular septal defects. Repair of the mitral valve in turn can include correcting mitral regurgitation (i.e., annular dilation and heart failure, myxomatous degeneration, and chordal rupture) and mitral stenosis. Other procedures include adjuncts to endovascular surgery and access for electrophysiologic studies. One of ordinary skill in the art will recognize other applications for the present apparatuses and methods.
[0067]In this connection, the present invention provides a valved cardiac port that can be temporarily inserted in a chamber wall of ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com