Method for augmenting, reducing, and repairing bone with thermoplastic materials
a technology of thermoplastic materials and bone, applied in the field of methods and materials for augmenting and repairing bone, can solve the problems of inconvenient methods, difficult surgery for surgeons to treat osteoporotic fractures in these areas, and failure of angular stable constructs in osteoporotic bone, etc., and achieve the effect of increasing the discontinuity degree of the first thermoplastic structur
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
PCL Composite Composition
[0089] A PCL / β-TCP composite was produced with the following composition:
[0090] PCL component: Sigma PCL 440744, I.V. 1.59, 20% by weight
[0091]β-TCP component: chronOS granules, 1.4-2.8 mm
[0092] The above components were heated to above 60° C. and kneaded by hand and allowed to cool. A structurally sound, cohesive mass was formed. The composite was reheated and manipulated to simulate manipulation by the surgeon and formed into a ball. It was again allowed to cool.
[0093] The composite material was placed in a solution with Alizarin red S (a red dye selective for calcium). Areas that still had exposed calcium were dyed red and areas encapsulated by polymer were yellow. A significant amount of calcium was free from encapsulation. The same composite was sectioned and the dye had penetrated significant portions of the internal structure demonstrating an interconnected porosity.
example 2
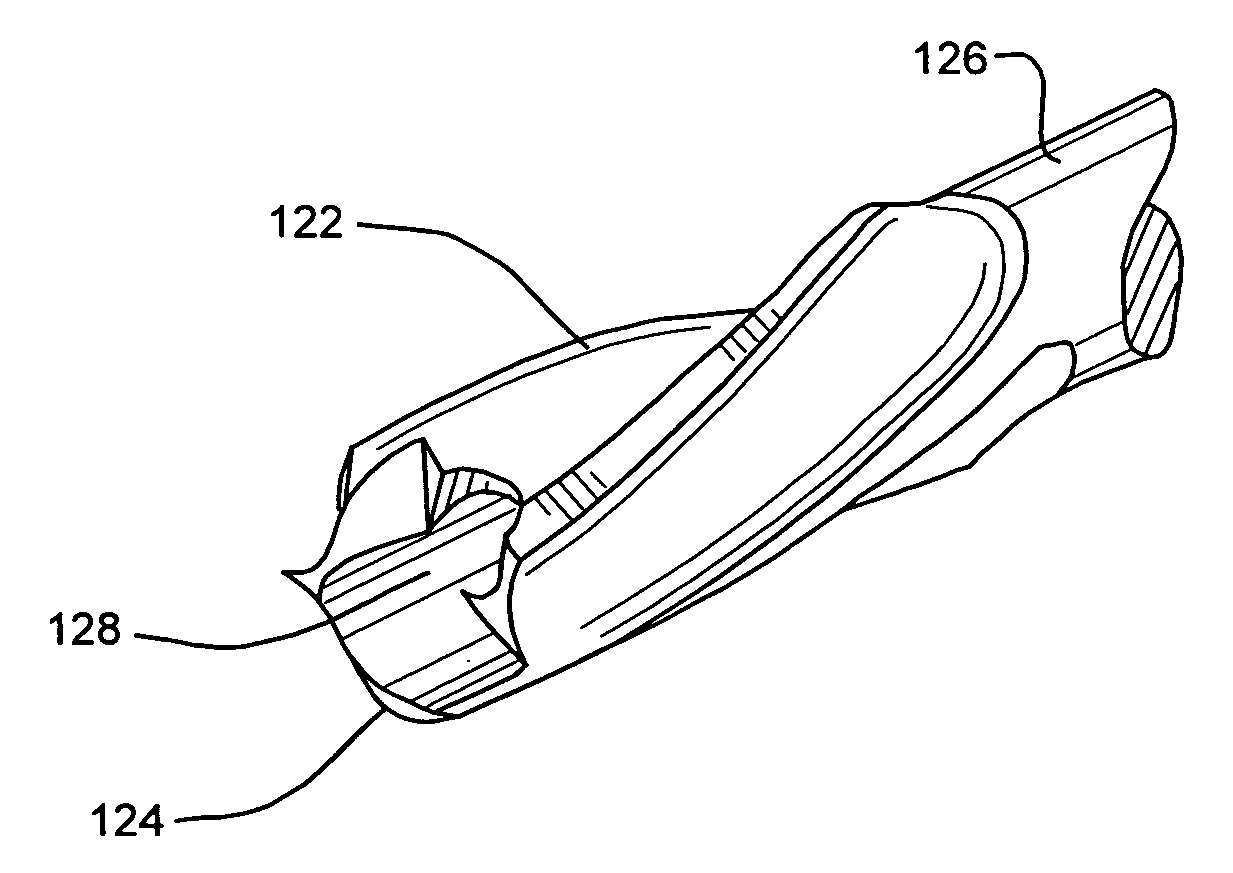
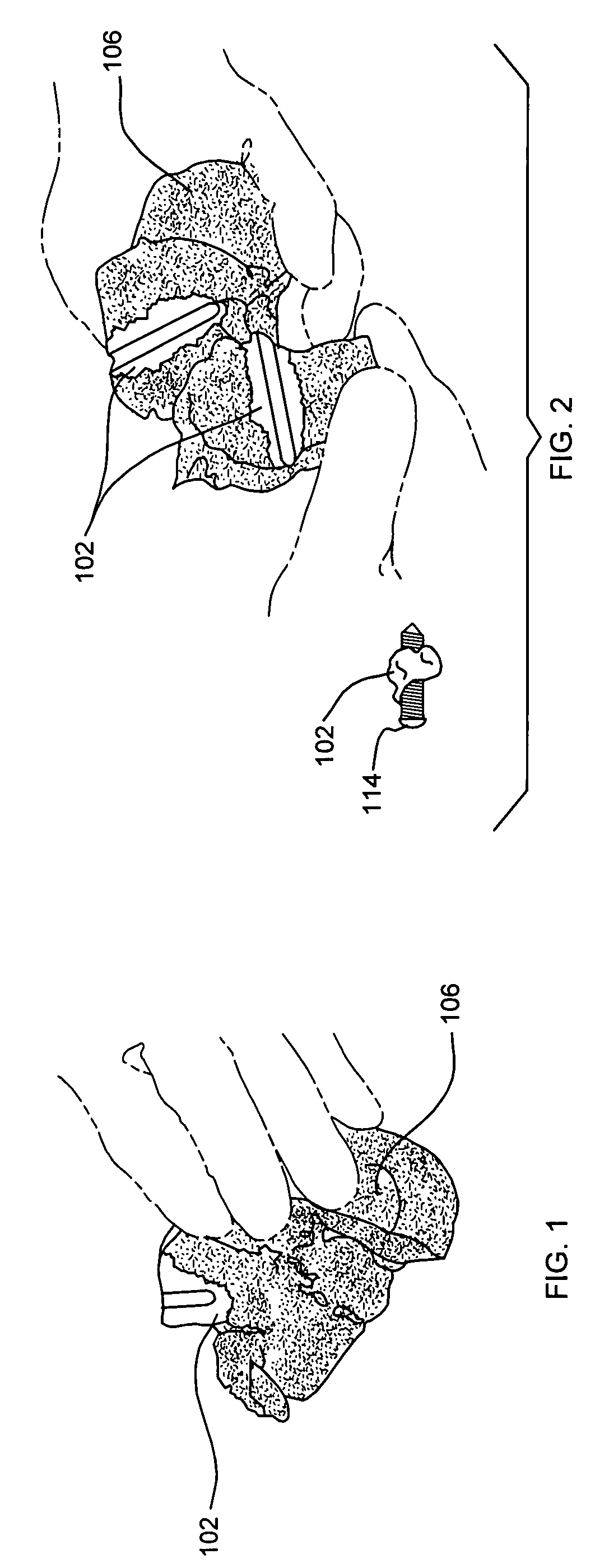
[0094] PCL material was injected into a 4.2 mm drill hole in a cadaver and a 5 mm locking screw was placed therein. The material was injected through an injection device as described above and was used for injection set at 80° C. Good perfusion into the relatively dense cancellous bone can be seen in FIGS. 1 and 2.
example 3
[0095] A finite element analysis (FEA) was performed on a construct simulating a stainless steel screw in cancellous bone with an offset load. The modulus of each of the materials was assigned as reported in Table 1, above. Three conditions were tested in the FEA simulation:
[0096] 1) Ø8 mm stainless steel screw in cancellous bone block without augmentation
[0097] 2) 3 mm of PMMA augmentation around screw
[0098] 3) 3 mm of PCL augmentation around screw
[0099] The screw was rigidly constrained on the proximal end and a unit load was placed on the cancellous bone at the distal end. The maximum stress at the screw to bone interface was assessed with the results shown in FIG. 13.
PUM
| Property | Measurement | Unit |
|---|---|---|
| density | aaaaa | aaaaa |
| resportion time | aaaaa | aaaaa |
| Tm | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com