Methods for Treating Hematopoietic Neoplasms
a hematopoietic neoplasm and neoplasm technology, applied in the direction of biocide, drug composition, active ingredients of phosphorous compounds, etc., can solve the problems of reducing affecting the survival rate of hematopoietic neoplasms, and vla4 expression by leukemic cells, etc., to achieve the effect of reducing
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
A. Example 1
Combretastatin A4 Phosphate (CA4P) Inhibits Leukemic Cell Proliferation
[0065]Leukemic cells were seeded at 1×105 cells / ml in X-vivo medium (Bio-Whittaker, MA) with 5% FBS and CA4P or pre-incubated with the PARP-inhibitor DPQ or caspase-inhibitors Z-VAD-fmk and Q-VD-OPh (R&D, Minneapolis, Minn.). A panel of leukemic cells was incubated with CA4P at the different concentrations indicated in FIG. 1, and viable cells were counted after 48 hours using trypan blue exclusion. Results of four experiments in duplicate are expressed as the ratio of the percentage of viable cells / control±SEM (*p50 ranging from 2.5 to 5 nM (FIG. 1). The majority of the AML cell lines tested was sensitive to CA4P at a concentration of 2.5 nM or less. All leukemic cell lines, as well as a recently established primary leukemic cell line (R81) 16 were sensitive at low doses of CA4P (<10 nM).
example 2
B. Example 2
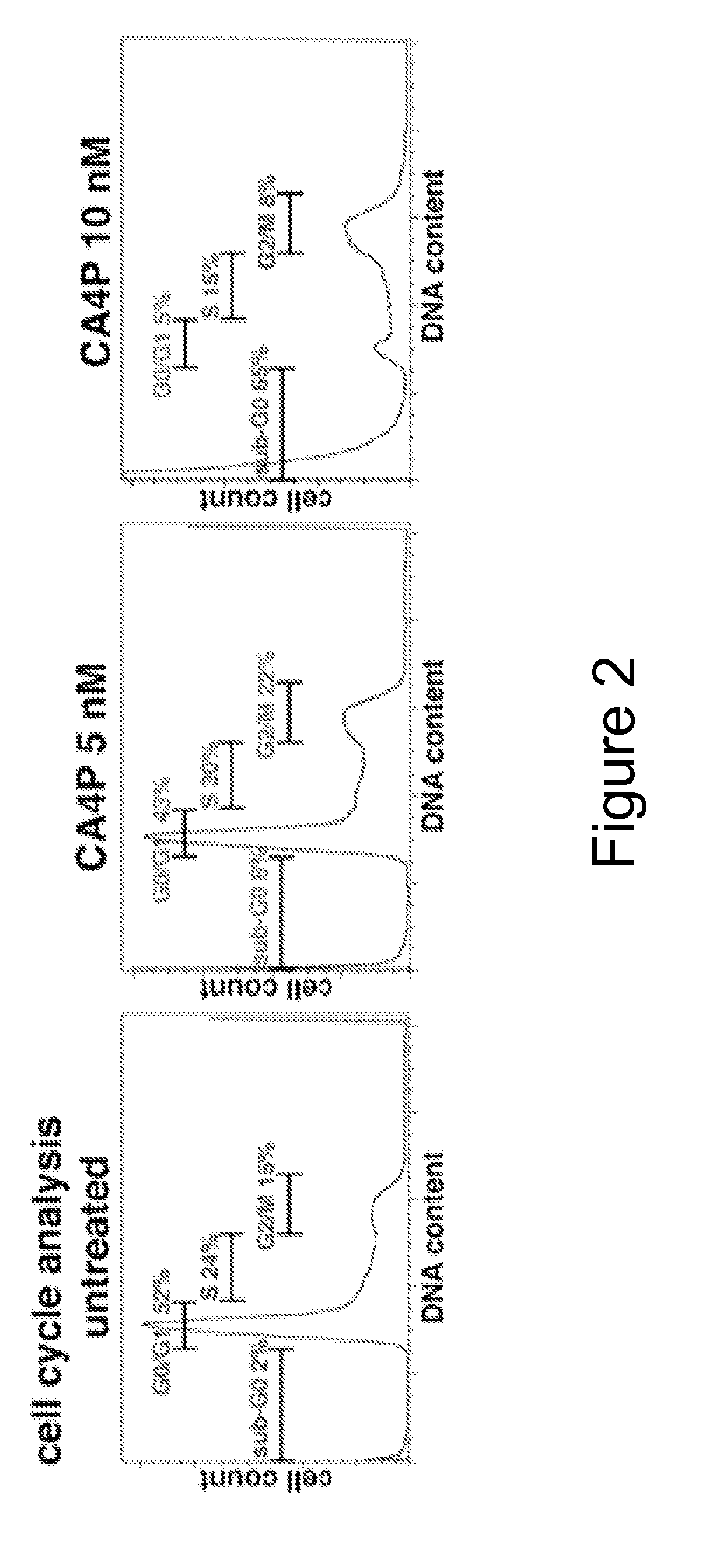
CA4P Causes Cell Cycle Arrest in G2 / M Phase
[0066]CA4P induces G2 / M arrest and cell death, as evidenced by increase in the sub-G0 / G1 peak (FIG. 2). Leukemic cells were seeded at 105 per ml in X-vivo supplemented with 5% FBS and then incubated with CA4P. KG1a leukemic cells were treated with CA4P at 0, 5 and 10 nM concentrations. After incubation for 48 hours, apoptotic cells were quantified by ApoAlert Annexin-V-fluorescine isothiocyanate (FITC) propidium iodide (PI) Apoptosis Kit (BD) using a Coulter Elite flow cytometer. In CA4P-treated cells, cell cycle analysis with propidium iodine (PI) showed G2 / M arrest and evidence of DNA fragmentation (sub G0-phase) at 48 hours.
example 3
C. Example 3
Combretastatin A-4 Phosphate Causes DNA Fragmentation and Morphological Evidence of Mitotic Catastrophe
[0067]DNA damage in CA4P-incubated leukemic cells was assessed by comet assay. The concept behind this assay is based upon the ability of denatured, cleaved DNA fragments to migrate out of the cell under the influence of an electric field, whereas undamaged DNA migrates more slowly and remains within the confines of the nucleus. Evaluation of the DNA “comet” tail shape and migration pattern allows for assessment of DNA damage. Results were expressed as the percentage of cells with a comet tail in 100 randomly selected, non-overlapping cells visualized by standard light microscopy. Quantification of the number of leukemic cells displaying a comet tail strongly increased after CA4P treatment (FIG. 3), consistent with CA4P-induced DNA damage. Results of three experiments in duplicate are expressed as the mean of the number of cells with a comet tail (%)±SEM (*p<0.05 as com...
PUM
| Property | Measurement | Unit |
|---|---|---|
| concentrations | aaaaa | aaaaa |
| refractory | aaaaa | aaaaa |
| Adhesion | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com