Intervertebral disc implants and tooling
a technology of intervertebral discs and tooling, which is applied in the field of cervical intervertebral disc implants, can solve the problems of undesirable progressive fusion of a long sequence of vertebrae, significant pain to the individual suffering from the condition, etc., and achieve the effect of facilitating insertion into the disc spa
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
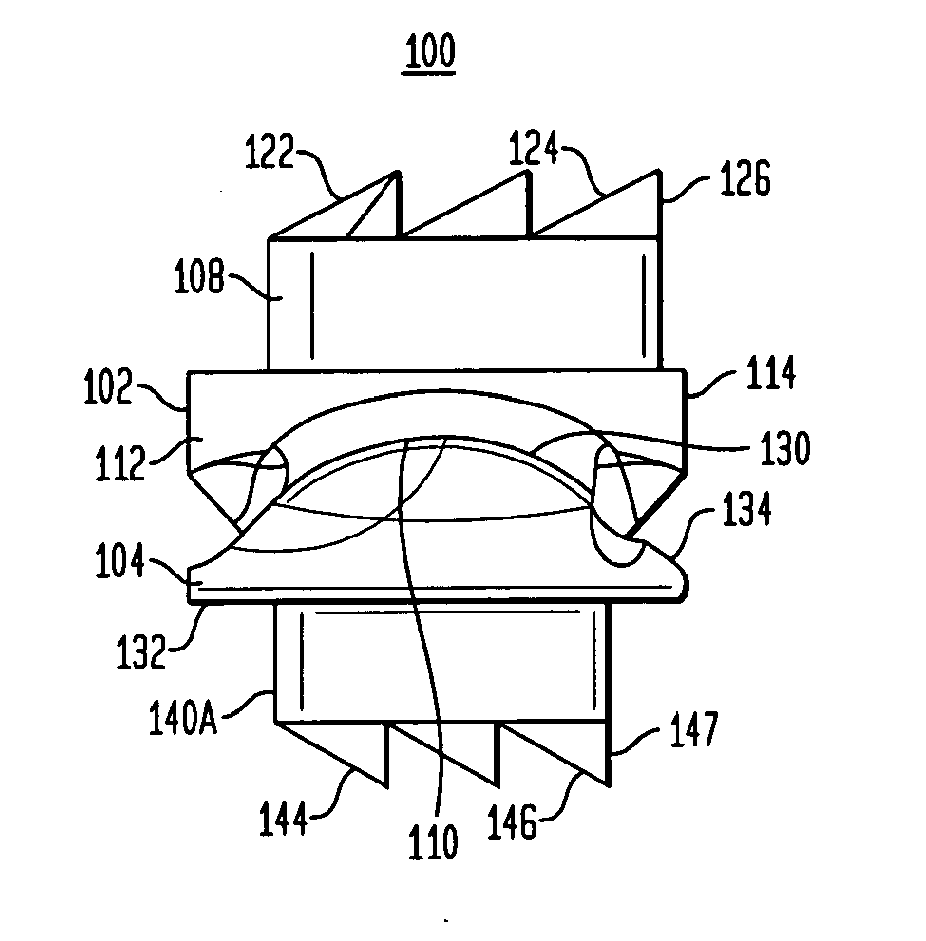
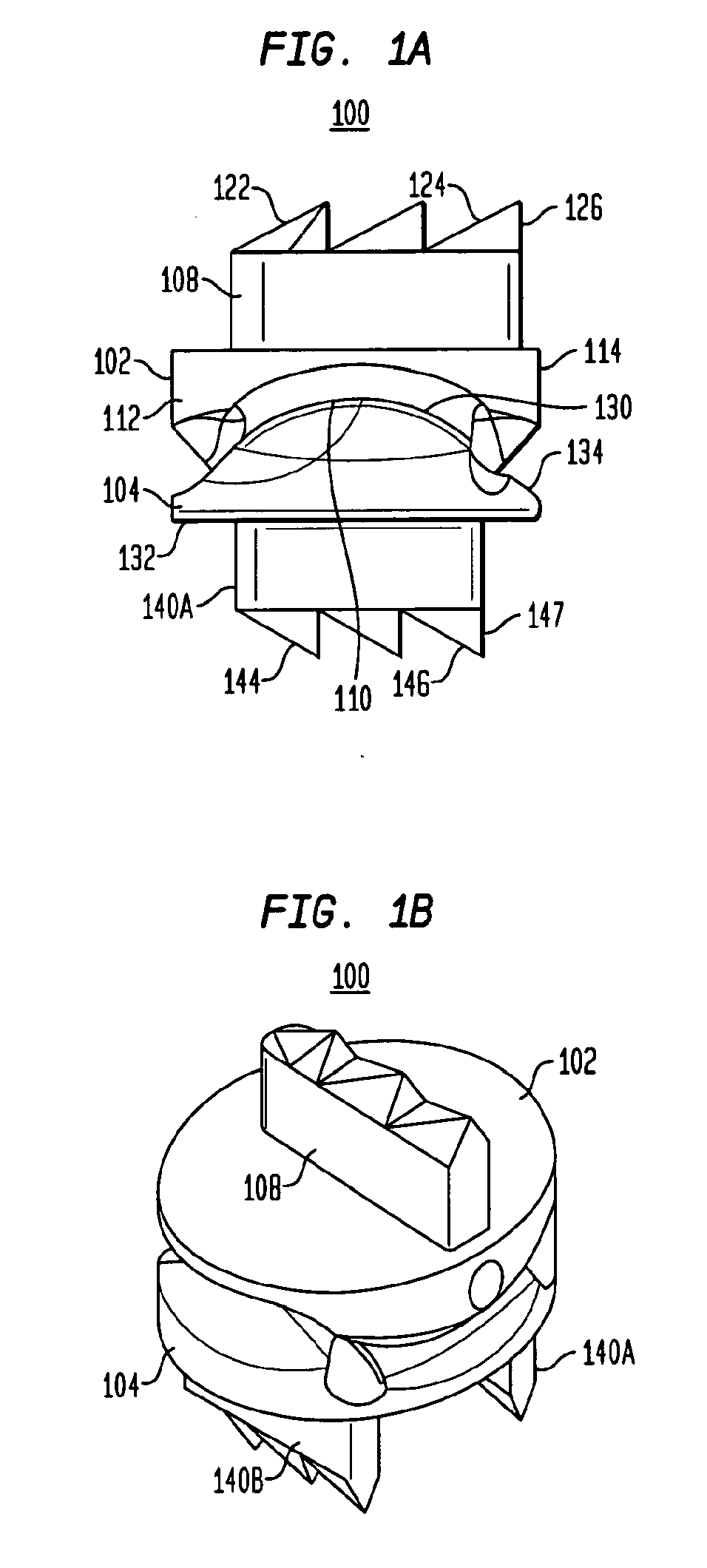
[0062]Referring to FIGS. 1A and 1B, in certain preferred embodiments of the present invention, an intervertebral disc implant 100 includes a top element 102 and a bottom element 104. As will be described in more detail below, the top and bottom elements 102, 104 have opposing articulating surfaces that engage one another. The intervertebral disc implant is adapted to be inserted into a disc space between adjacent vertebrae. In certain preferred embodiments, two or more disc implants can be stacked over one another in two or more successive disc spaces. In still other preferred embodiments, the disc implants are cervical implants.
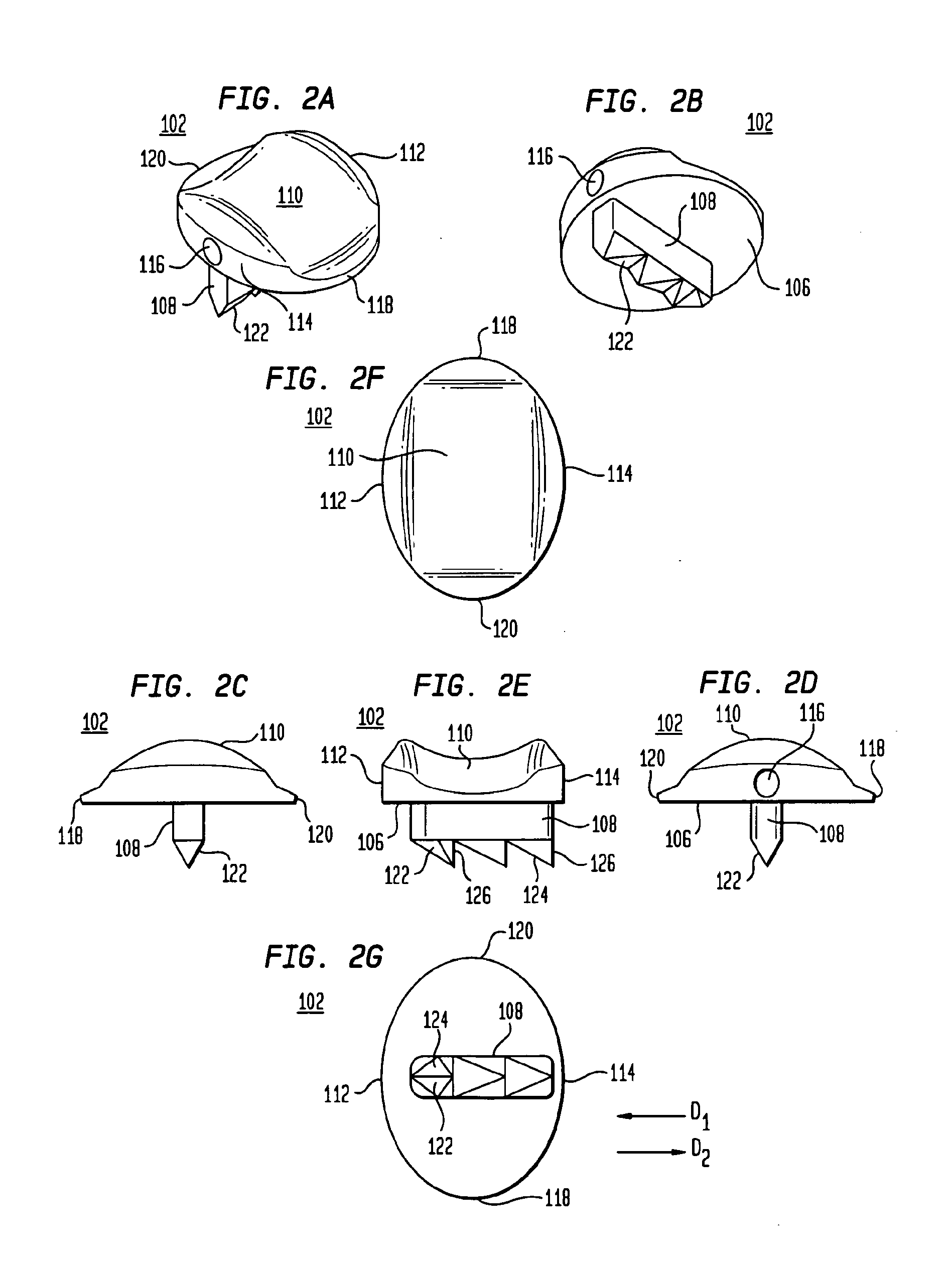
[0063]Referring to FIGS. 2A-2E, the top element 102 includes a first bone engaging surface 106 having a protrusion 108 and a second articulating surface 110. Referring to FIGS. 2E-2G, the top element 102 has a posterior end 112 and an anterior end 114. As shown in FIGS. 2A-2B and 2D, the top element 102 has an opening 116 at the anterior end 114 thereof that...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com