Devices for maintaining patency of surgically created channels in tissue
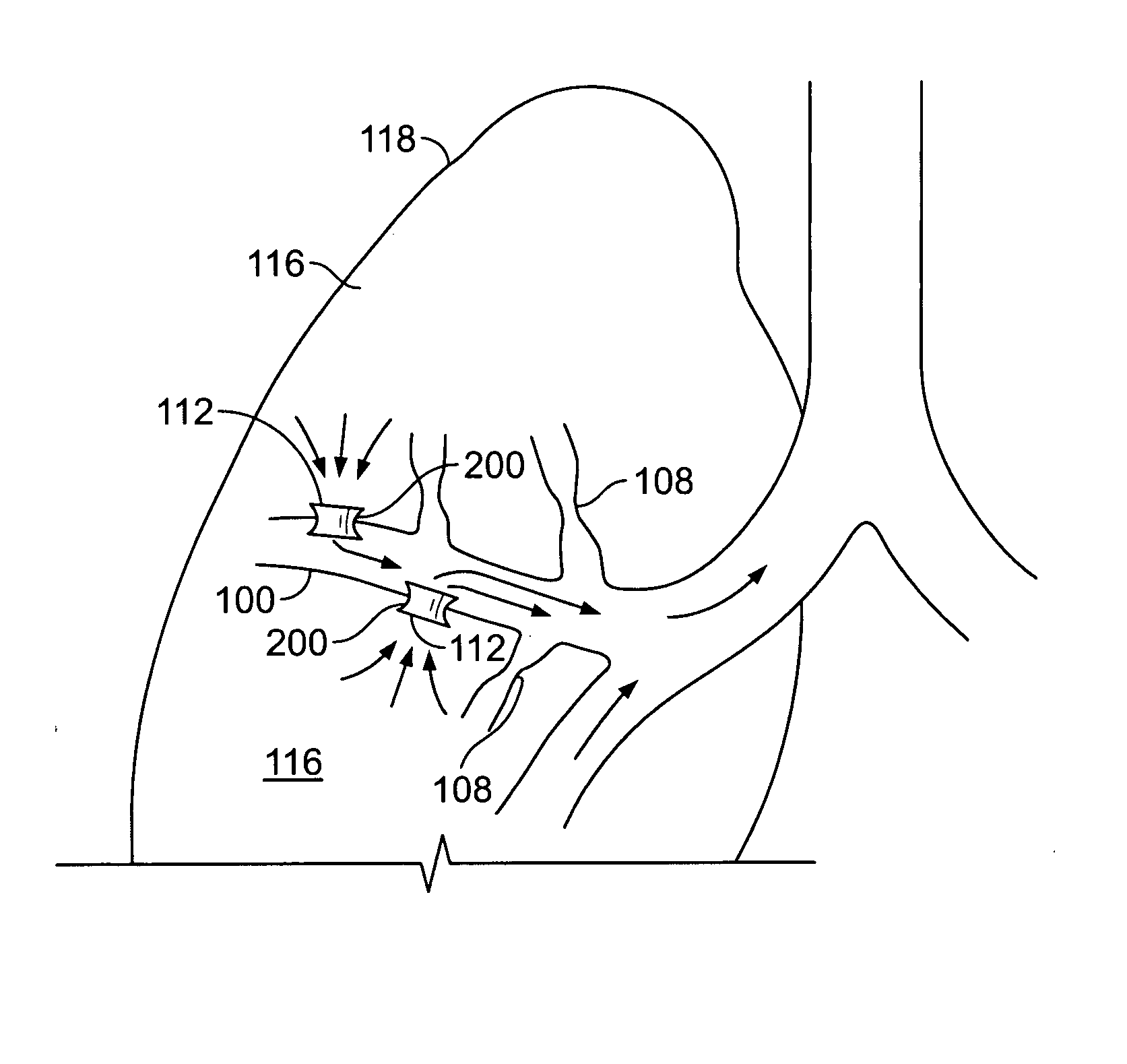
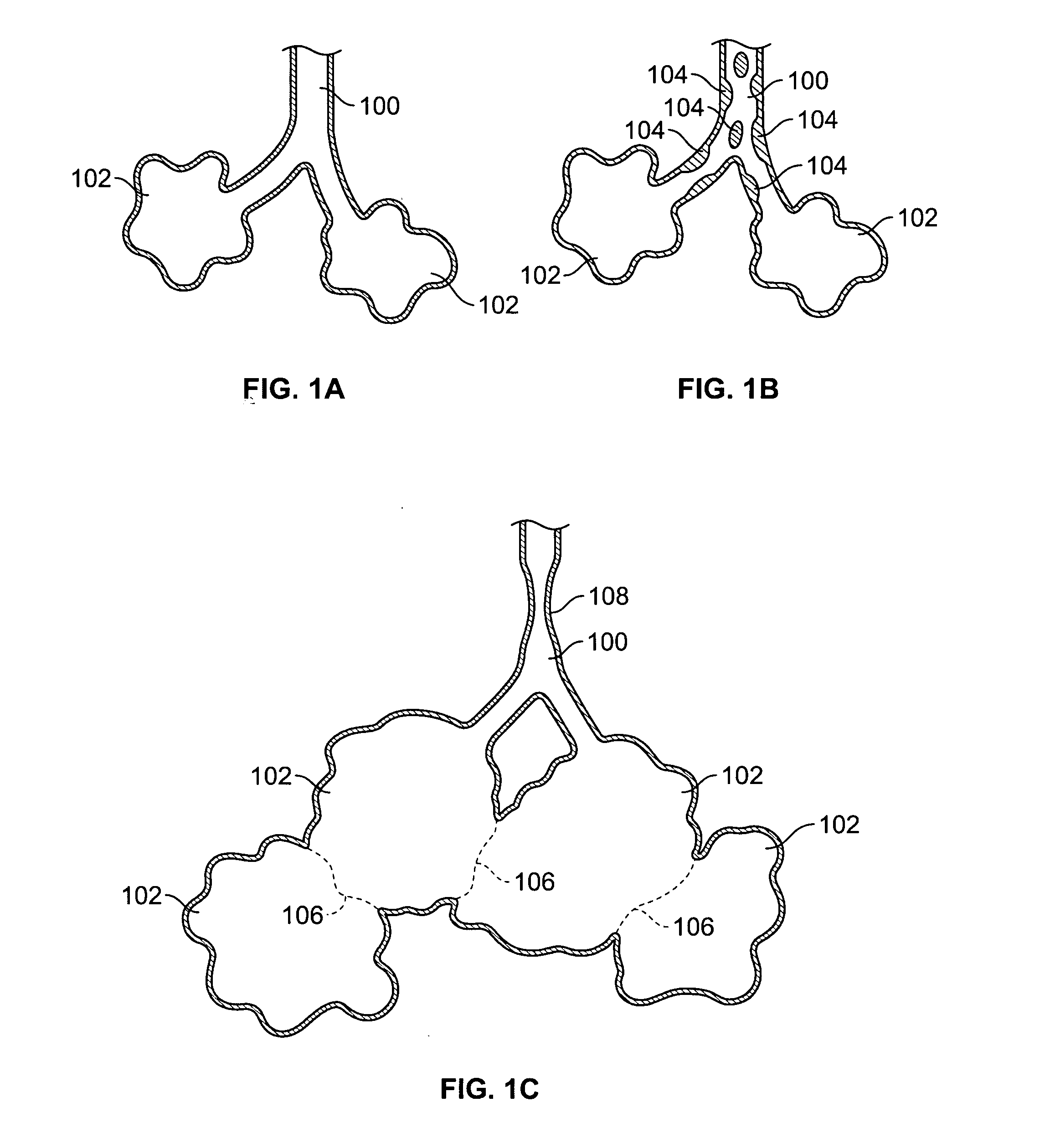
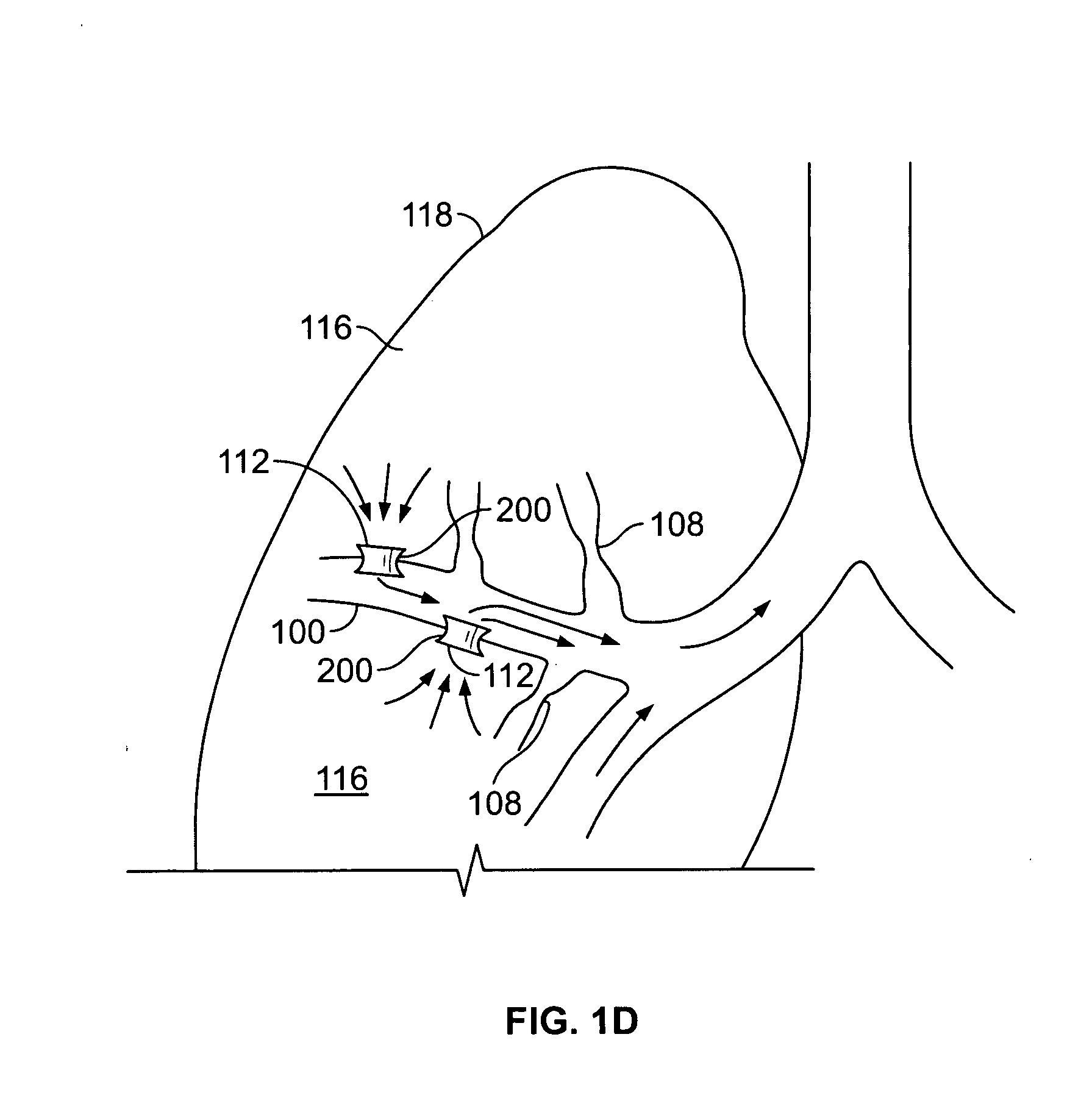
a technology of surgical creation and tissue, applied in the direction of surgical staples, surgical forceps, therapy, etc., can solve the problems of copd-related muscle weakness, inability to perform common daily activities, and little hope of recovery, so as to increase the duration of patency of the channels and/or implants
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example
[0199] Implants comprising stainless steel mesh frame fully encapsulated with a composition comprising silicone (as described below) and paclitaxel were implanted in several canine models. Visual observation indicated that, on average, the passage through the implants of the present invention remained unobstructed and were associated with significantly reduced fibrotic and inflammatory responses, in canine models, at a considerably higher rate than an implant without any drug adjunct or coronary drug eluting stents (as shown in FIG. 12).
[0200] The composition comprised approximately a 9% paclitaxel to silicone ratio with approximately 400 micrograms of paclitaxel per implant. Measurements found that approximately 30% of the paclitaxel released after 60 days. In general, for implants with the paclitaxel / silicone composition, observations of chronic inflammation, epithelial metaplasia and fibrosis were all very mild.
[0201] For paclitaxel as the bioactive substance, polymers ...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com