SARS Vaccine Compositions and Methods of Making and Using Them
a composition and vaccine technology, applied in the field of delipidation methods, can solve the problems of severe damage to the body, extreme suffering, morbidity and mortality, and enormous economic burden on society, and achieve the effects of simple, effective and efficient methods, and positive immunologic responses
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
Development of a Modified Coronavirus Viral Particle for Use as a Vaccine
[0134]Solvent treatment technology was used to develop a modified coronavirus viral particle to use as a prophylactic vaccine against the SARS virus. In addition, solvent-treated virus that was subsequently subjected to chemical inactivation was tested for the ability to raise neutralizing antibodies and produce a cellular immune response in mice. In the following text and elsewhere in the application, the coronavirus that produces SARS is also referred to as SARS.
[0135]The SARS stocks used in the experiments were propagated at the Lovelace Respiratory Research Institute (LRRI), Albuquerque, N. Mex., in the laboratory of Dr. Kevin Harrod, Director of the Infectious Disease Program. The initial SARS seed stock was provided by the Centers for Disease Control (CDC). Supernatants from SARS infected VERO cells were then sent to Dr. Erdman at the CDC for inactivation by gamma irradiation.
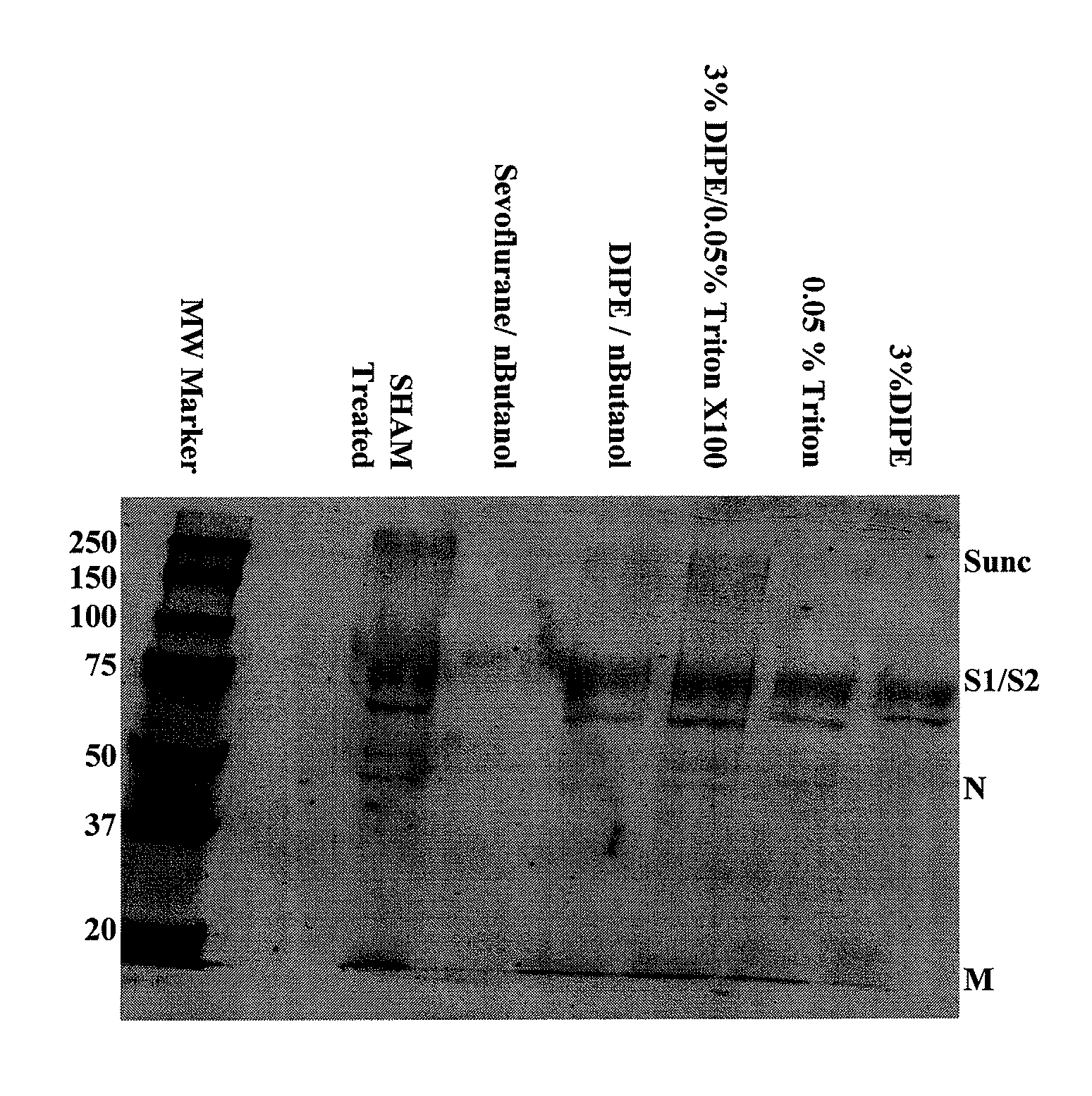
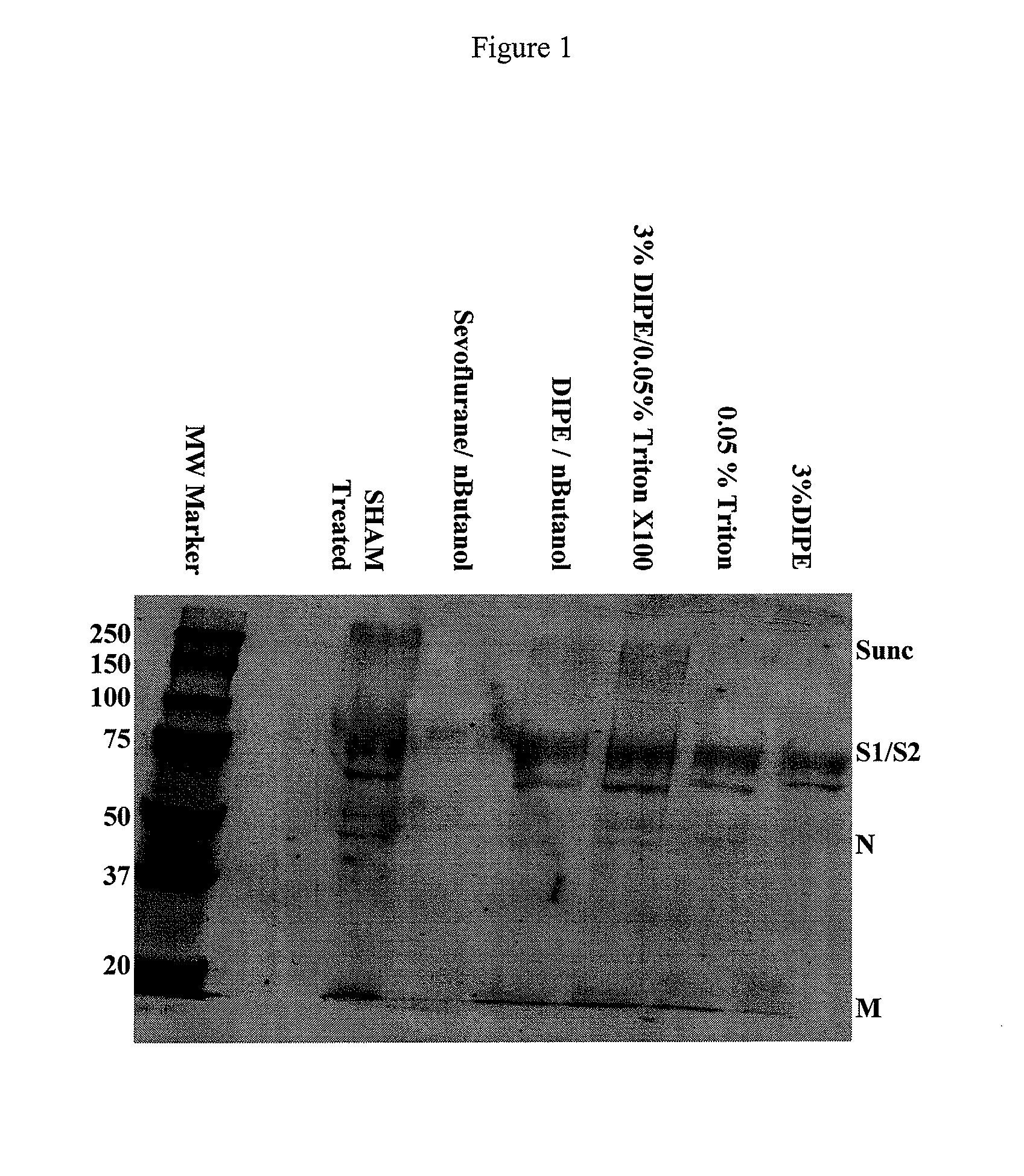
[0136]The delipidation proces...
experiment # 1
Experiment #1 Evaluation of Three Different Delipidation Methods for SARS
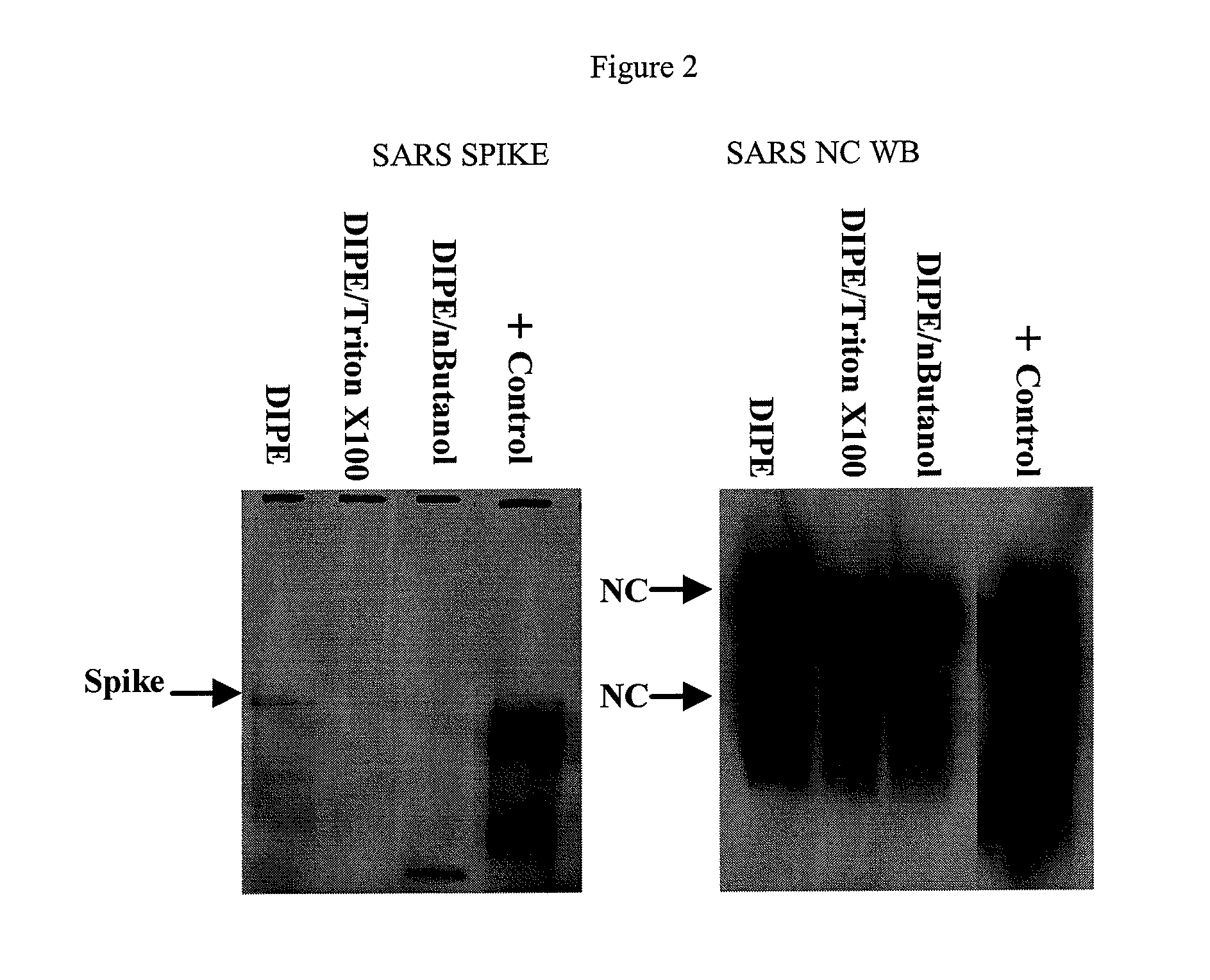
[0180]The particles obtained by three delipidation processes were tested with respect to generating an immune response. The experiment was designed with three mice per group testing the following three groups:
A. Inactivated SARS treated with 3% DIPE;
B. Inactivated SARS treated with DIPE / n-BuOH (95:5); and,
C. Inactivated SARS treated with 3% DIPE / 0.05% Triton X-100.
[0181]Mice were vaccinated sc with 50 μg of inactivated delipidated SARS in 50 μl in one footpad. At three weeks post vaccination, mice were sacrificed, and serum was harvested.
[0182]Serum aliquots were sent to the laboratory of Dr. Michael W. Cho (Case Western Reserve University), where SARS neutralization titers were evaluated using a neutralization assay for SARS using pseudotyped murine leukemia virus (MuLV) with the Spike protein of SARS-CoV (or VSV-G as a negative control) as previously described (Han et al., 2004 Virology. 326:140-149). SARS NC...
experiment # 2
Experiment #2 SARS-Dose Escalation Study of Optimally Delipidated SARS Vaccine
[0192]The objective of this study was to test three different concentrations of delipidated inactivated purified SARS with inactivated purified SARS only, at 0.1 μg, 1 μg, and 10 μg boosts. Mice (3 mice / group) were primed with SARS supernatant (virus was unpurified) obtained from LRRI that was γ-irradiated by Dr. Erdman at the CDC and had a protein concentration of 4 mg / ml. Mice were primed using Incomplete Freunds Adjuvant sc with 100 μg total protein in a volume of 500 μl. Two weeks later, mice were boosted with the appropriate concentration of delipidated SARS, or inactivated SARS in a volume of 500 μl administered sc. Four weeks after the booster injection, mice were sacrificed and serum collected and sent to Dr. Cho for neutralizing antibody titers. Serum IgG titers to SARS NC and Spike were performed at Lipid Sciences, Inc.
Results
[0193]FIG. 6 illustrates the Spike Ab titers from Experiment #2, compar...
PUM
| Property | Measurement | Unit |
|---|---|---|
| pressures | aaaaa | aaaaa |
| temperatures | aaaaa | aaaaa |
| temperature | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com