Stent coated with a sustained-release drug delivery and method for use thereof
a drug delivery and stent technology, applied in the direction of packaging foodstuffs, blood vessels, immunological disorders, etc., can solve the problems of reducing the recurrence rate of obstruction, and dilating the vessel and relieving the obstruction, so as to improve the structure and function of tissue, improve the function and/or life of the device, and reduce the effect of recurrence ra
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
example 1
[0103]To 20 gm of 10% (w / v) aqueous poly(vinyl alcohol) (PVA) solution, 80.5 mg of agent TC-112 was dispersed. 5 pieces of glass plates were then dipping coated with this TC-112 / PVA suspension and followed by air-drying. The coating and air-drying was repeated four more times. At the end about 100 mg of TC-12 / PVA was coated on each glass plates. The coated glass plates were then heat treated at 135° C. for 5 hours. After cooling to room temperature, the glass plates were individually placed in 20 ml of 0.1 M mol phosphate buffer (pH 7.4, 37° C.) for release test. Sample was taken daily and entire release media were replaced with fresh one at each sampling time. The drugs and TC-112 released in the media were determined by reverse-phase HPLC. The half-life for TC-112 in pH 7.4 buffer is 456 min, in serum is 14 min.
[0104]The results are shown in FIG. 3, which shows the total cumulative release of TC-112 from PVA coated glass plates. The slope of the curve demonstrates that TC-112 is r...
example 2
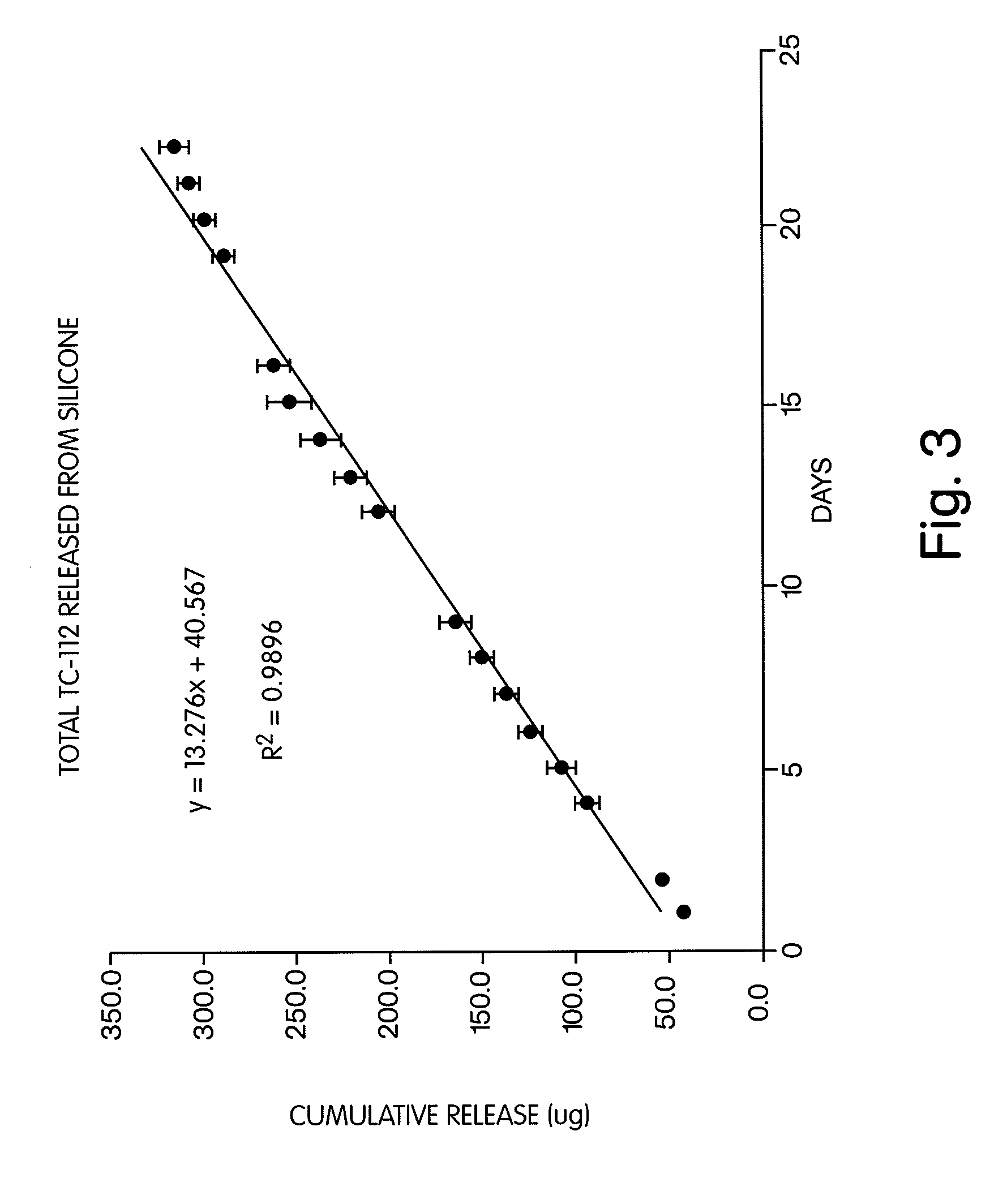
[0105]12.0 gm of silicone part A (Med-6810A) were mixed with 1.2 gm of silicone part B (Med-6810B), and degassed in sonicator for 10 min, followed by water aspirator. 41.2 mg of (TC-112) were dispersed in this degassed silicone, and degassed again. 0.2 gm of the mixture was spread on one surface of a glass plate. The glass plates (total 5) were then placed in oven and heated at 105° C. for 20 min. to cure. After removing from the oven and cooled to room temperature, 0.2 gm of the mixture was spread on the other uncoated surface of each glass plate. The coated glass plates were then heat treated again at 105° C. for 20 min. After cooling to room temperature, the glass plates were individually placed in 20 ml of 0.1 M phosphate buffer (pH 7.4, 37° C.) for release test. Samples were taken daily, and the entire release media was replaced with fresh media at each sampling time. The drugs (5-fluorouracil and naproxen) and TC-112 released in the media were determined by HPLC.
[0106]The tota...
example 3
[0108]A mixture of 3.3 gm Chronoflex C(65D) (Lot# CTB-G25B-1234) dispersion containing 0.3 gm of Chronoflex C(65D) and 2.2 gm Chronoflex C(55D) (Lot# CTB-121B-1265) dispersion containing 0.2 gm of Chronoflex C (55D), both in dimethyl acetamide (DMAC) (1:10, w / w) was prepared by mixing the two dispersions together. To this mixture, 6.0 gm of tetrahydrofurane (HPLC grade) were added and mixed. The final mixture was not a clear solution. Then 101.5 mg of TC-32 was added and dissolved into the polymer solution.
[0109]Ten (10) HPLC inserts were then coated with the polymer / TC-32 solution by dipping, which was then followed by air-drying under ambient temperature. The coating and air-drying process was repeated four (4) times (5 times total) until a total of about 10 mg of polymer / CT-32 was applied to each insert. The inserts were then placed in an oven at 80° C. for two hour to remove the residue of the solvent.
[0110]The inserts were placed individually in 20 ml of 0.1 m phosphate buffer,...
PUM
| Property | Measurement | Unit |
|---|---|---|
| solubility | aaaaa | aaaaa |
| solubility | aaaaa | aaaaa |
| logP | aaaaa | aaaaa |
Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com