Inspiratory resistor valve system with expiratory port
a resistor valve and inspiratory technology, applied in the field of inspiratory resistor valve systems with expiratory ports, can solve the problems of less effective or ineffective, and achieve the effects of reducing intrathoracic pressure, preventing respiratory, and increasing blood volum
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
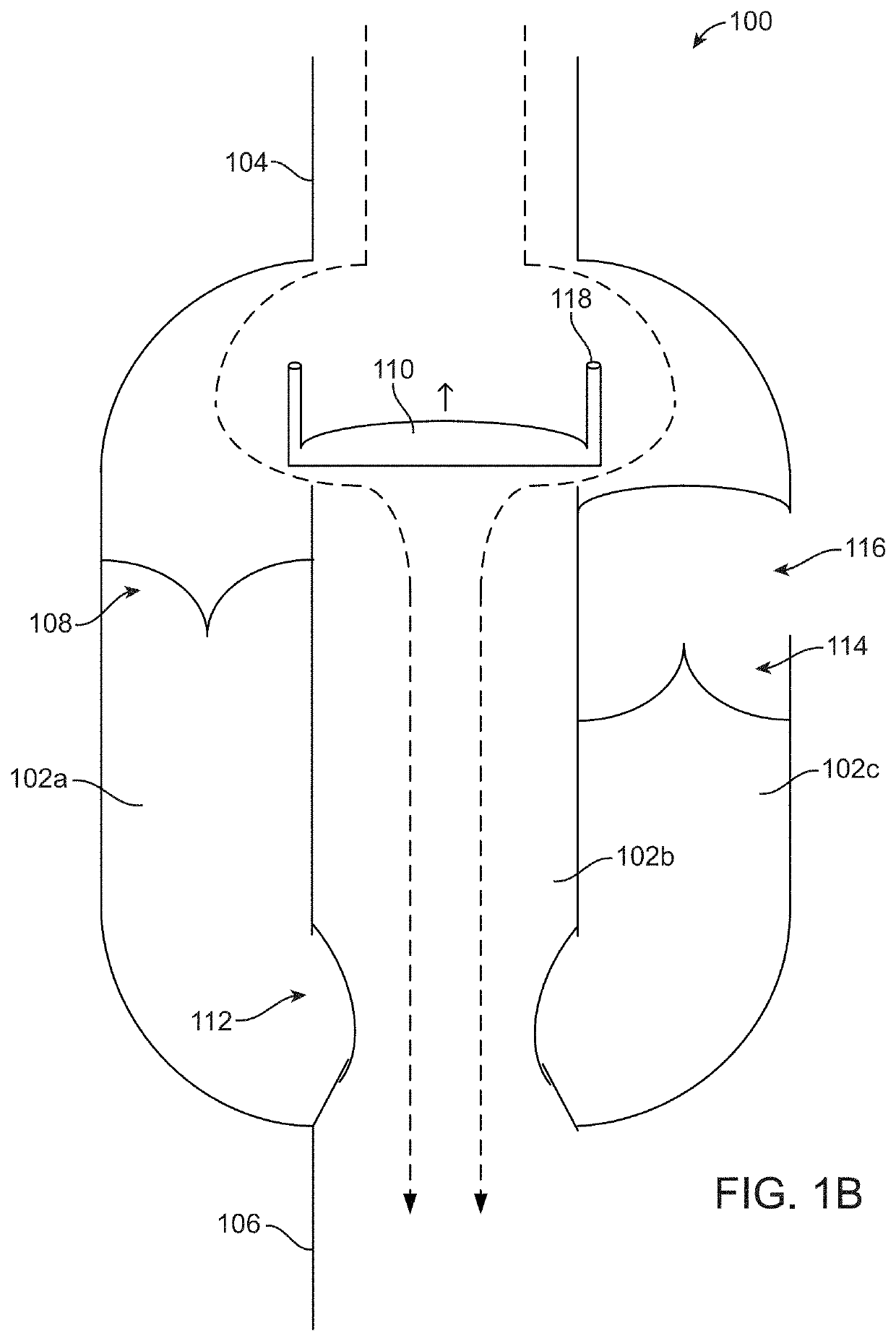
Image
Examples
example
[0078]In an anesthetized pig, CPR was performed with an automated device that provides for compression and active decompression. A functional IRV, as described in this patent, that includes an inspiratory port and a separate expiratory port (similar to IRV 300), was attached to the endotracheal tube and pressures were measured with a pressure transducer at the level of the patient port. With each positive pressure breath airway pressures increased to approximately 20 mmHg and during each decompression phase they decreased to approximately −5 mmHg as illustrated in FIG. 6.
[0079]The IRVs described herein may be used in conjunction with physiological sensors, air flow sensors, pressure transducers, timing and / or status lights, impedance sensors to detect air / blood ratio in the thorax, and / or a controller or other interface of a CPR device, ventilator, and / or AED to provide feedback related to how to perform CPR, deliver positive pressure ventilations, and / or deliver shocks to a patient...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com