Implantable heart assist devices and methods
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
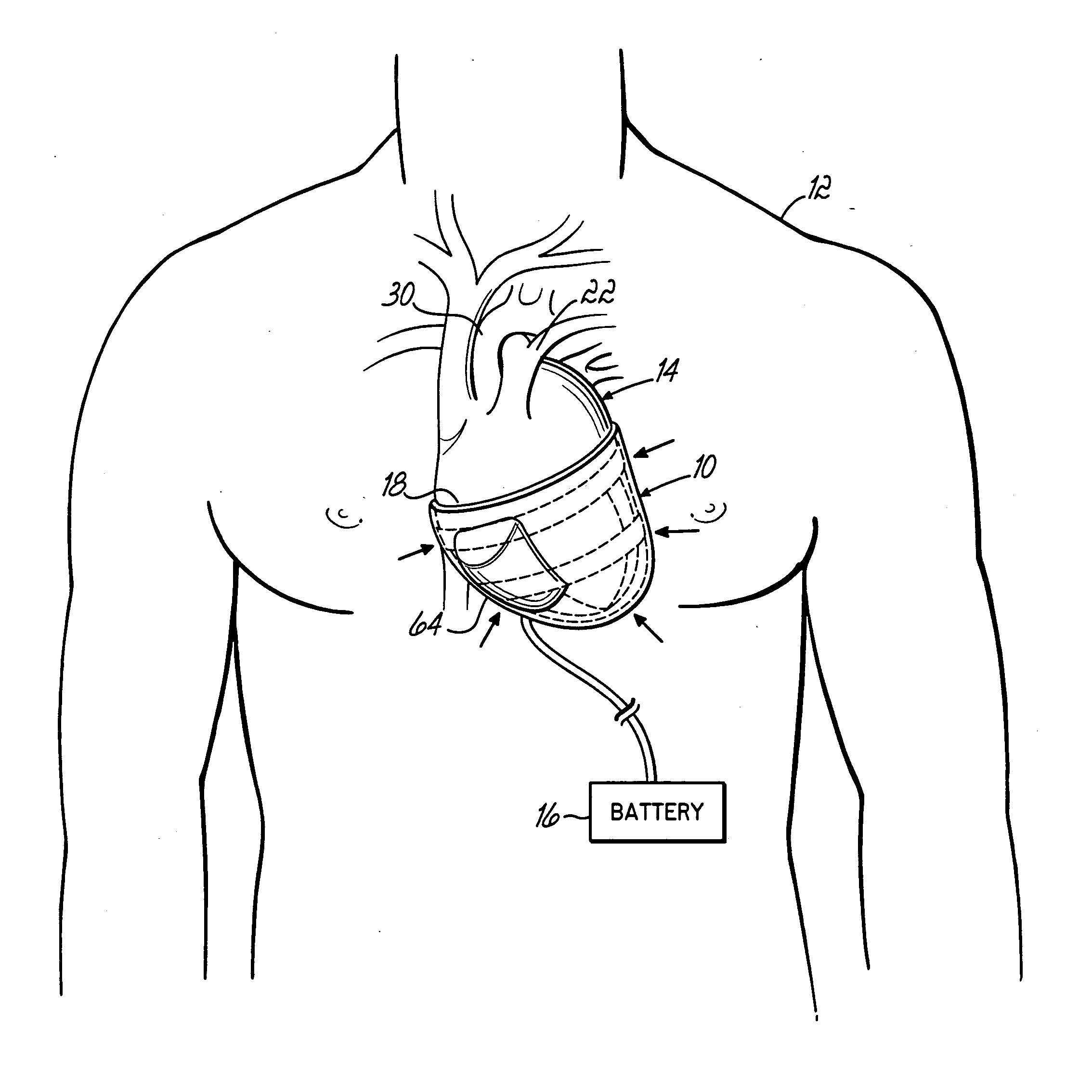
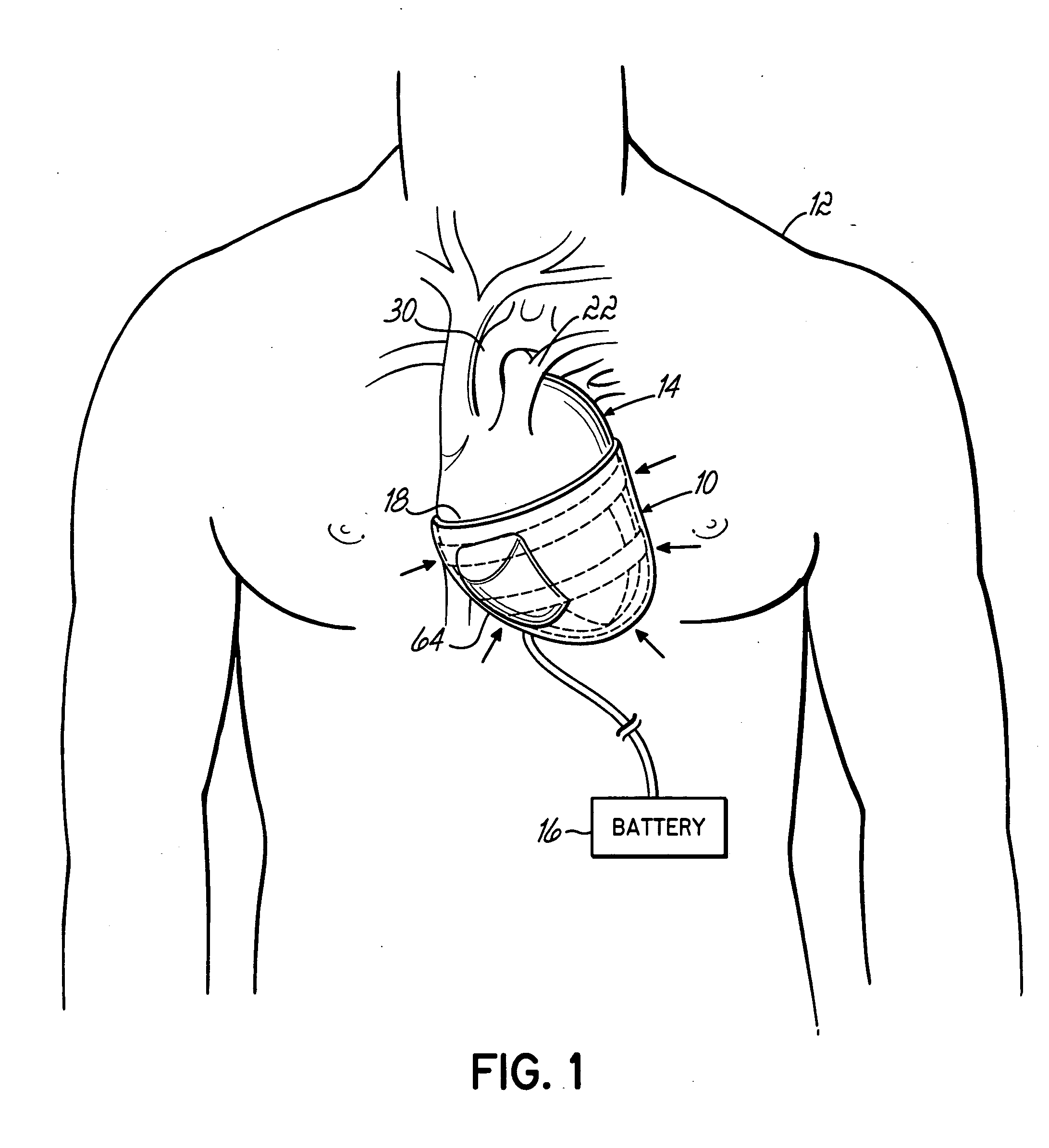
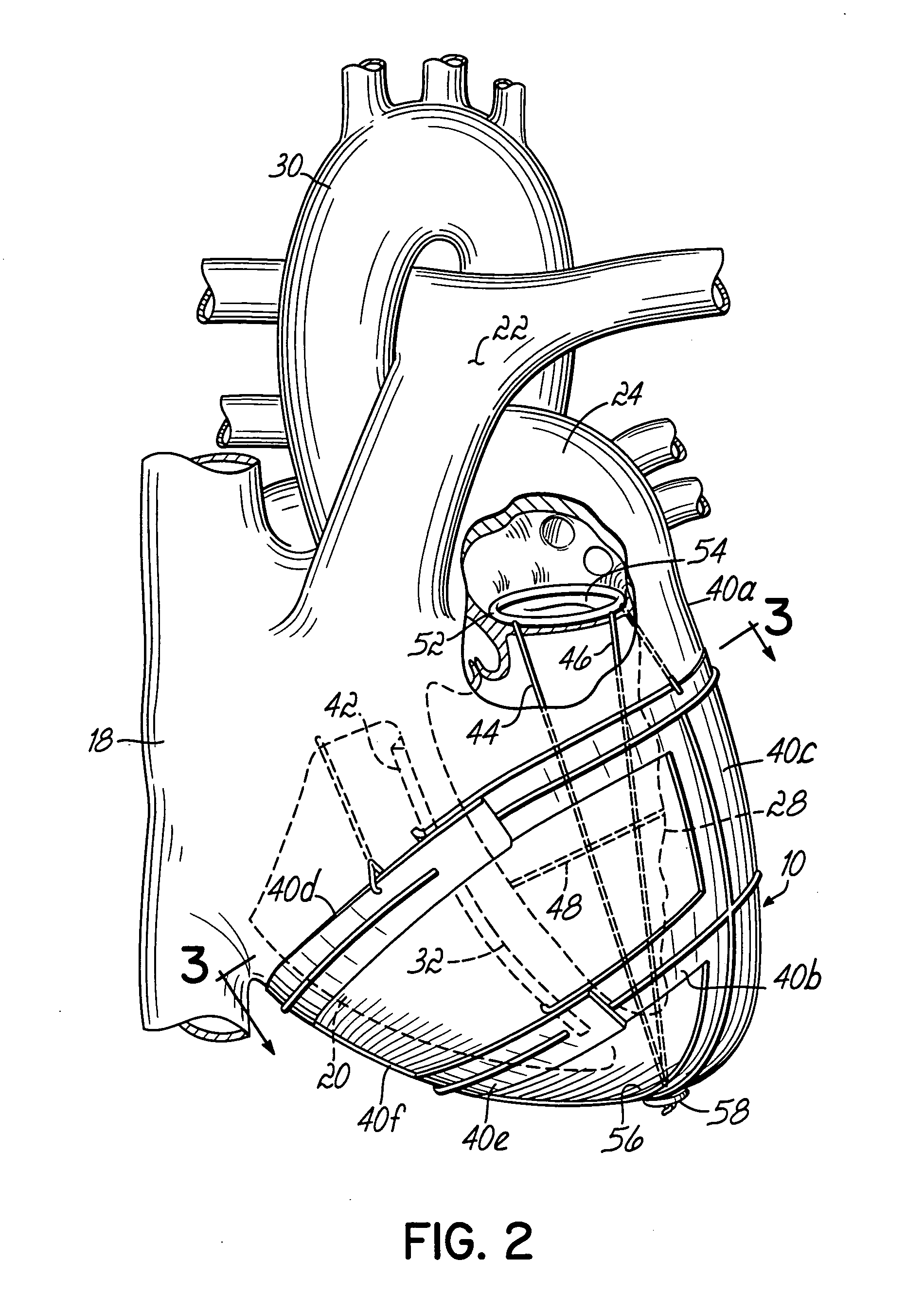
[0048]FIG. 1 illustrates a heart assist device 10 constructed in accordance with the invention and schematically illustrated implanted within a patient 12 in surrounding relation to the patient's heart 14. A power supply 16, such as an electric or pneumatic power supply, is operatively connected to heart assist device 10 for reasons to be discussed below. As generally shown in FIG. 2, heart 14 has four chambers. The right atrium 18 receives blood flowing through veins in the patient's body. The right ventricle 20 pumps the blood to the lungs of the patient through the pulmonary artery 22. The left atrium 24 receives oxygenated blood flowing back from the patient's lungs through the pulmonary vein and the left ventricle 28 pumps this blood out through the aorta 30 to the patient's body. The right and left ventricles 20, 28 compress simultaneously during this pumping action and, in a normal heart, anywhere between about 50% and 80% of the blood in these chambers will be expelled as de...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com