Tissue stabilizer having an articulating lift element
a tissue stabilizer and lift element technology, applied in the field of surgical instruments, can solve the problems of complicated completion of anastomosis, higher likelihood of surgical error in the formation of anastomosis, and forces alone can do little to optimize visualization and presentation of targets, so as to improve the presentation of the arteriotomy and improve the fit against the surface of the hear
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
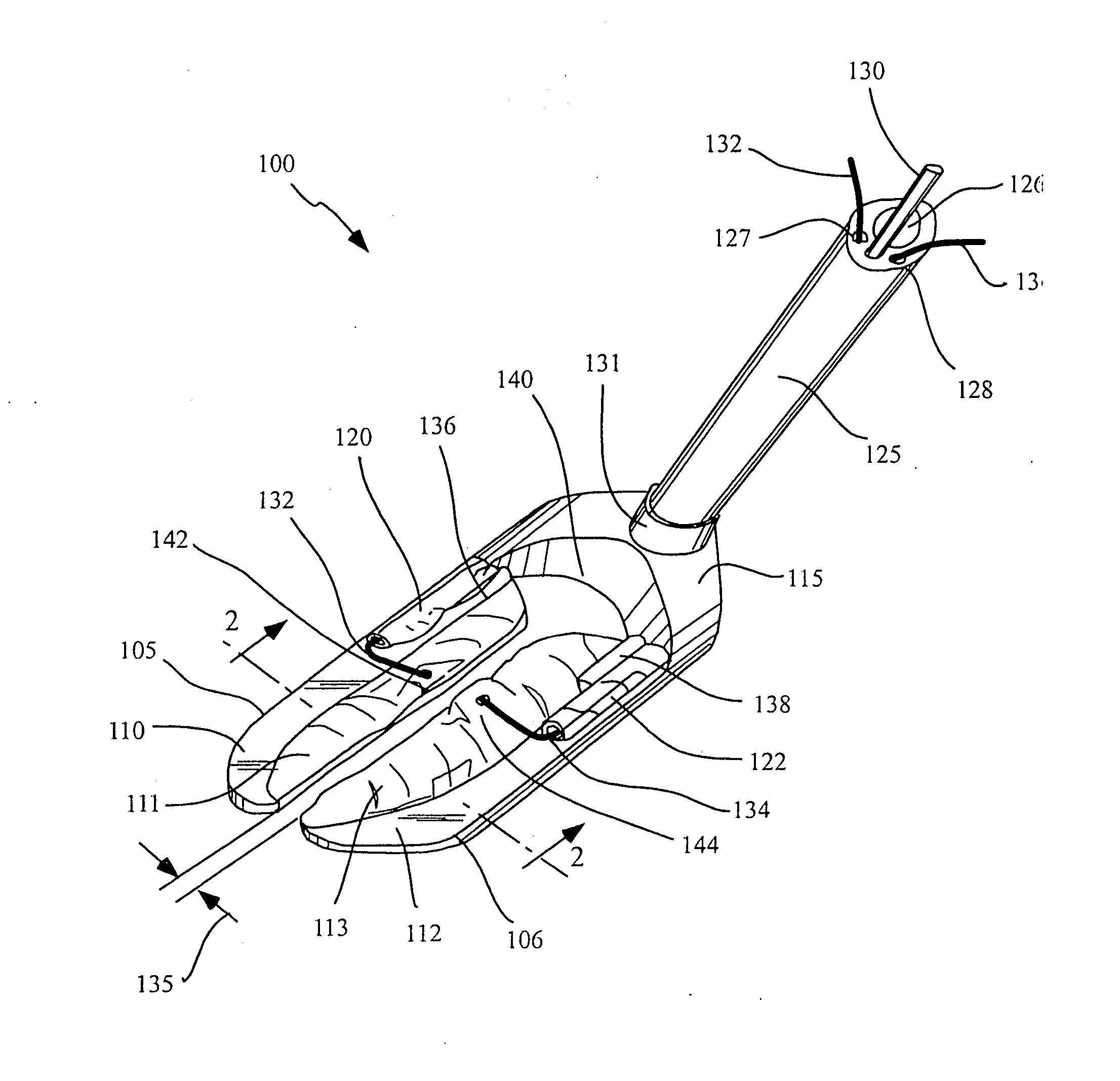
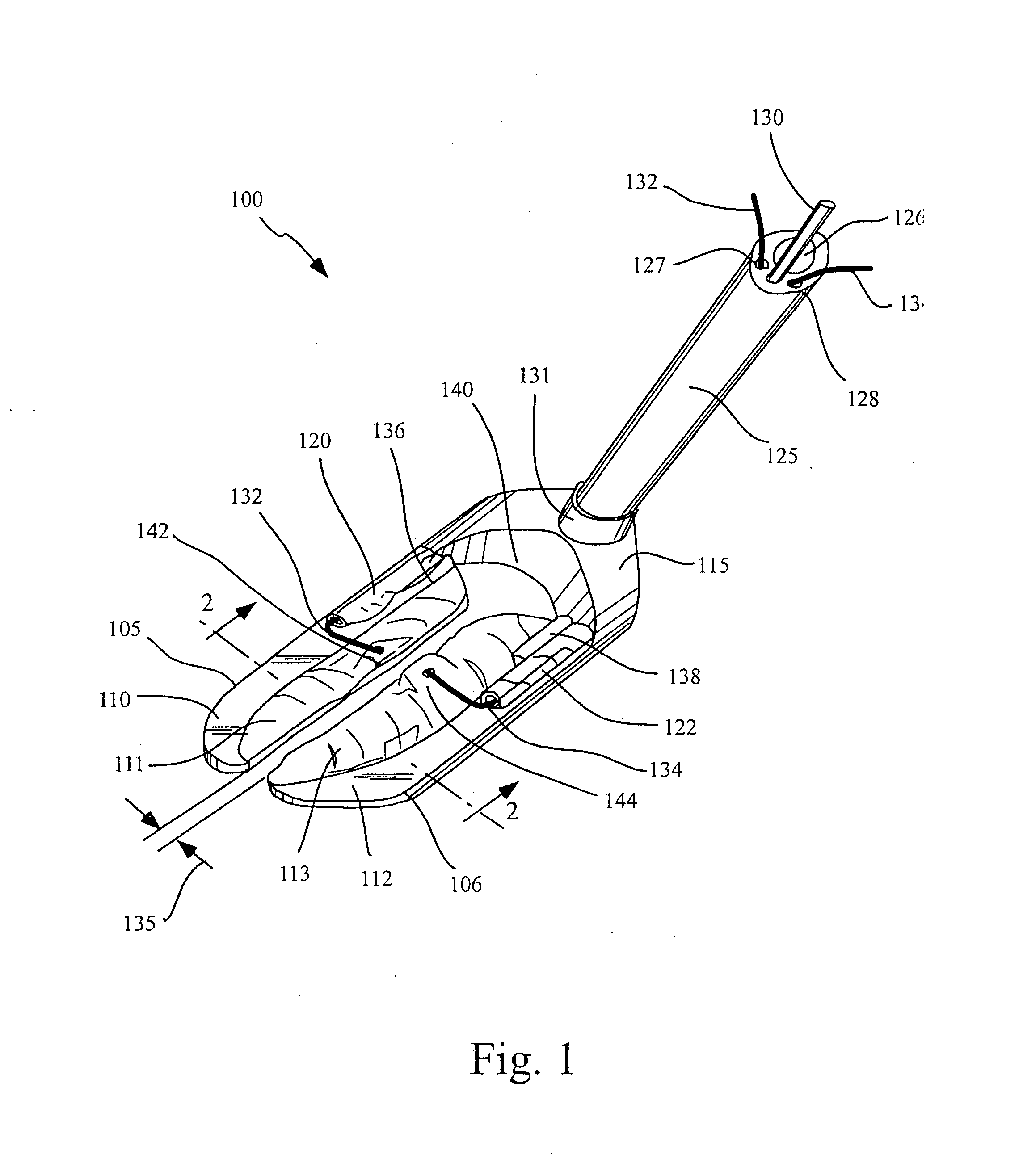
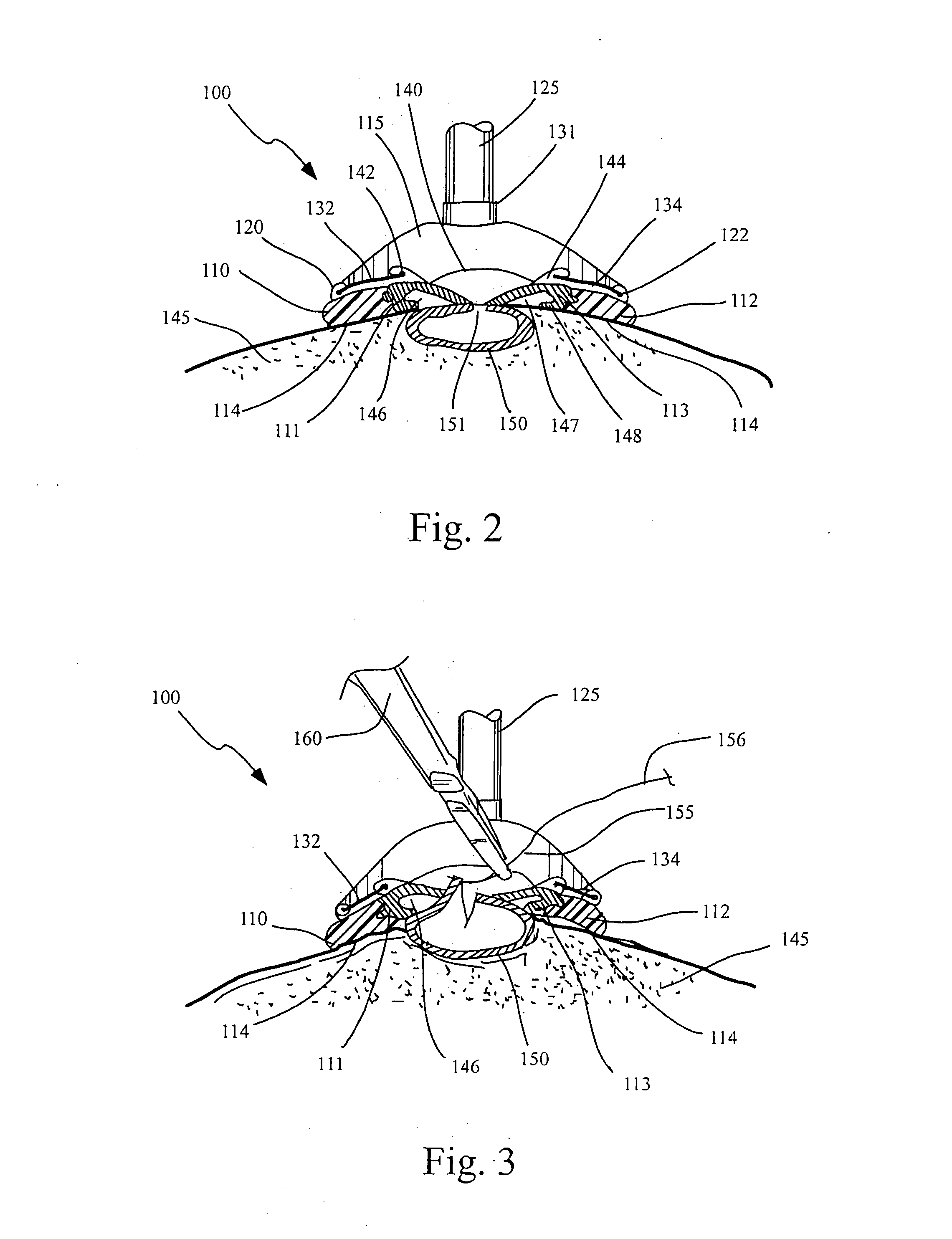
[0044] The present invention involves devices and methods for stabilizing tissue during a surgical operation. The devices described herein may be used in a wide variety of surgical applications that require a tissue structure to be stabilized or immobilized to provide a substantially stable and motionless surgical field on which a surgical procedure can be performed. By way of example only, the preferred embodiments described in detail below are directed to the stabilization of a portion of the heart to facilitate a surgical procedure on or within the heart, such as a coronary artery bypass graft (CABG) procedure.
[0045] Although the devices and methods of the present invention may be applied to conventional stopped-heart and beating heart procedures, they are preferably used to stabilize the beating heart during a CABG operation which has been specially developed to facilitate completion of an anastomosis, typically between a target coronary artery and a bypass graft or source arte...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com