Mask and flow generator system
a generator system and mask technology, applied in the field of mask and flow generator system, can solve the problems of destroying the quality of sleep of patients, putting extra strain on patients' hearts, significant health problems, etc., and achieve the effects of reducing treatment efficacy, reducing mask leakage, and improving treatment accuracy
- Summary
- Abstract
- Description
- Claims
- Application Information
AI Technical Summary
Benefits of technology
Problems solved by technology
Method used
Image
Examples
Embodiment Construction
4. System Design
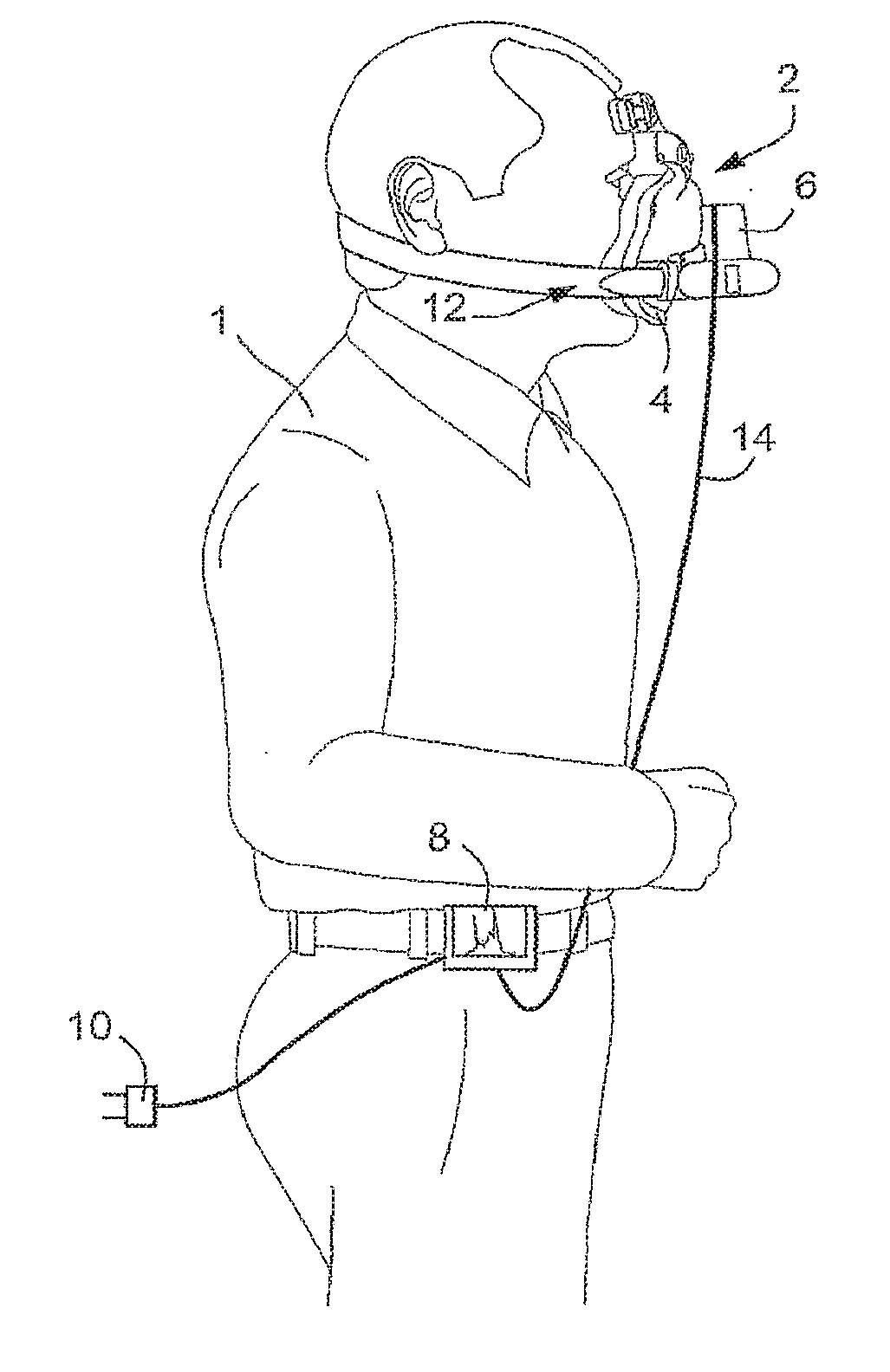
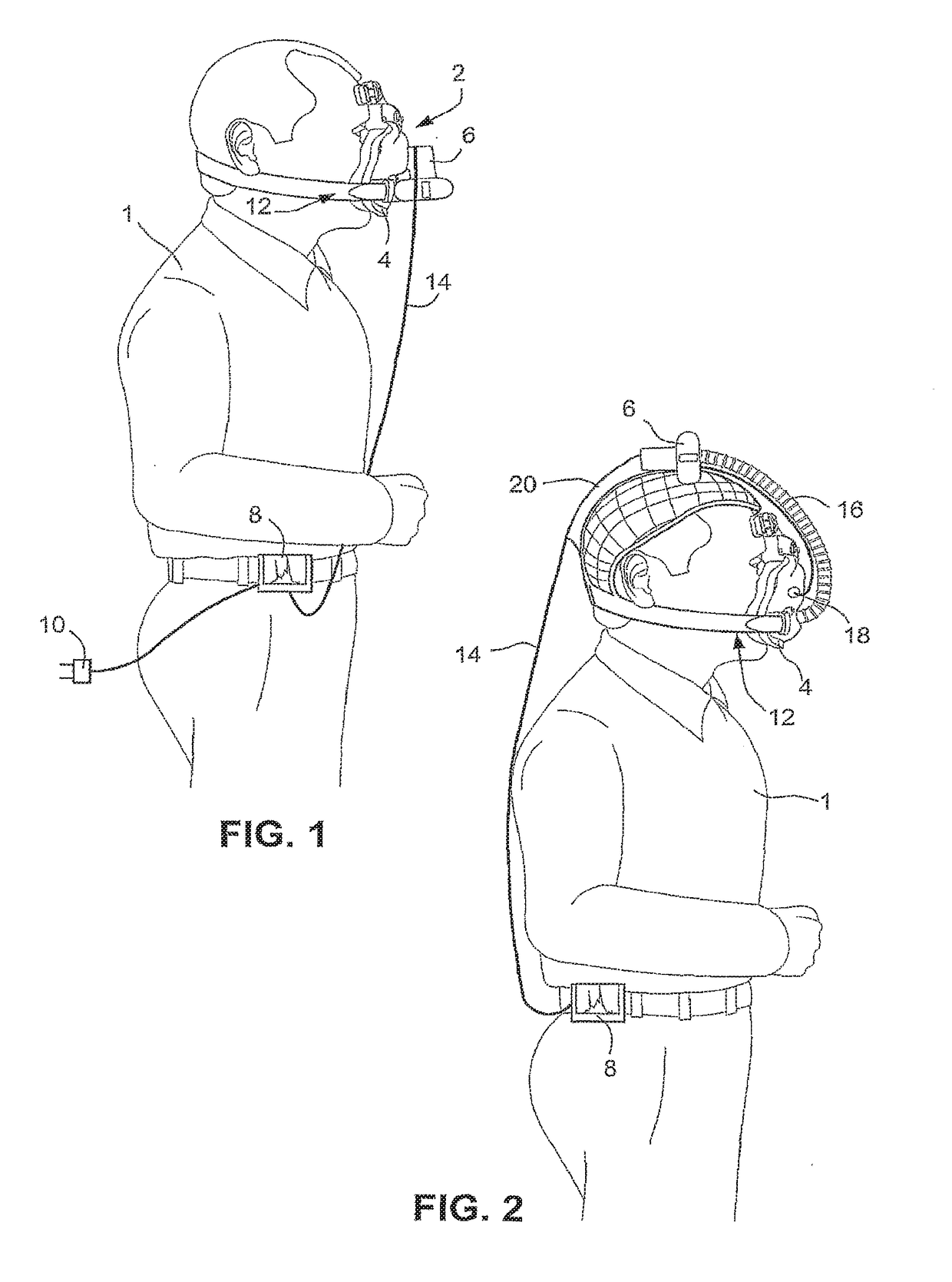
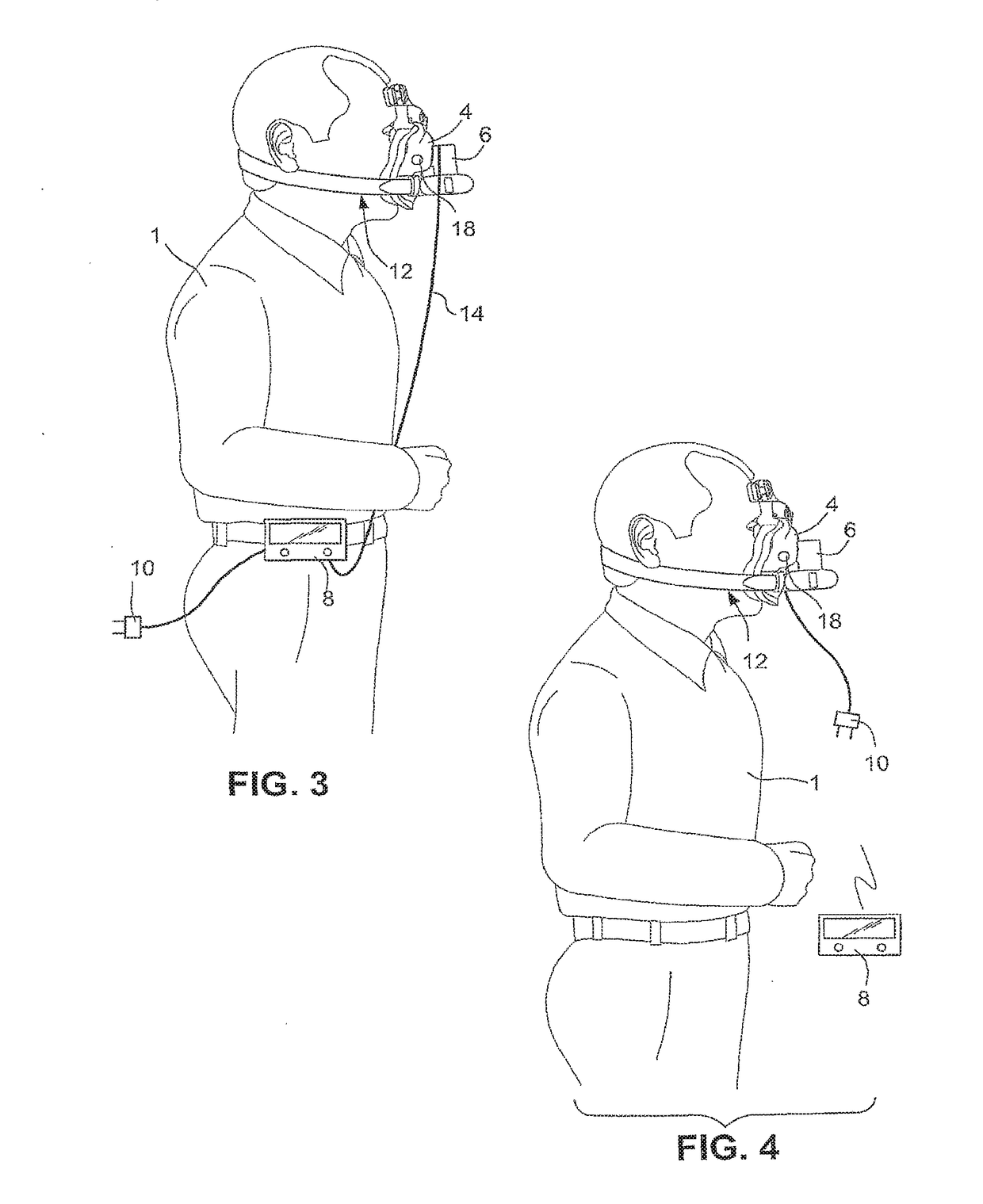
[0062]Referring to FIG. 1, a NIPPV system according to the present invention can generally be divided into two components. The first component is the user interface 8. The user interface 8 houses electrical components and allows the user 1 to control the system. The second component is the patient interface 2. The patient interface 2 is configured to house a flow generator 6, e.g., a pump, configured to generate a pressurised airflow in a mask 4 and deliver the pressurized flow into the user's airways. It should be appreciated that the mask 4 may be a nasal mask or a full face mask.
[0063]A power supply connector 10 may be provided to the user interface 8 to provide power to the user interface 8. The power supply connector 10 may also be configured to charge a rechargeable battery of the user interface 8.
[0064]The patient interface 2 may also include a headgear 12 configured to secure the mask 4 to the patient's face so that the mask 4 forms a substantially leak proof...
PUM
 Login to View More
Login to View More Abstract
Description
Claims
Application Information
 Login to View More
Login to View More - R&D
- Intellectual Property
- Life Sciences
- Materials
- Tech Scout
- Unparalleled Data Quality
- Higher Quality Content
- 60% Fewer Hallucinations
Browse by: Latest US Patents, China's latest patents, Technical Efficacy Thesaurus, Application Domain, Technology Topic, Popular Technical Reports.
© 2025 PatSnap. All rights reserved.Legal|Privacy policy|Modern Slavery Act Transparency Statement|Sitemap|About US| Contact US: help@patsnap.com