While conventional corneal topography devices have achieved significant success, such devices suffer from a number of limitations, which, if overcome, could significantly enhance their accuracy and utility.
This imaginary extension could not be realized in a real system due to size and interference with the subject's head.
Therefore, such prior art devices are unable to measure the peripheral cornea.
For this strategy, however, the cylindrical or conical keratoscope target must be positioned very close to the eye, and thereby tends to impinge on the patient's brow and nose.
In addition to being potentially uncomfortable and potentially contributing to the spread of disease, the close approach of the keratoscope target makes the design very error-prone, as a slight error in alignment or focusing causes a large percentage change in the position of the keratoscope rings relative to the eye and, hence, a large error in the measurement of the cornea.
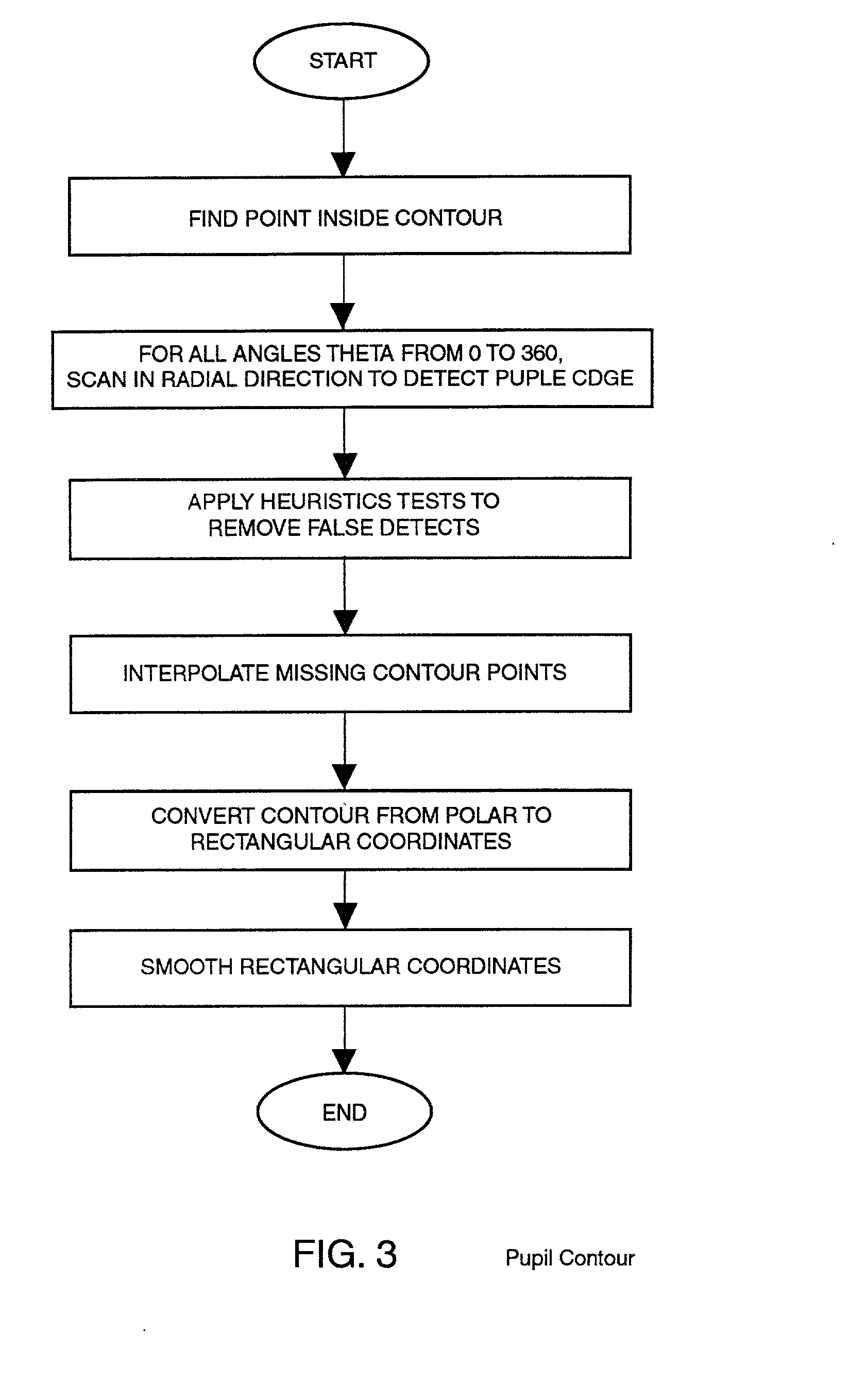
In addition, current systems tend to provide poor pupil detection and do not accurately measure non-rotationally symmetric corneas, such as those with astigmatism.
This is particularly difficult with conventional designs, however, as the intensity transition from the black pupil to a dark iris is minimal compared to the intensity transition from a bright keratoscope ring image to a dark interring spacing.
As a result, the pupil detection algorithms in current systems often fail or provide poor results.
It is well known that the innermost data of traditional corneal topography systems have relatively low accuracy, so it is likely that this new technique will have lower accuracy than that currently provided by the commercially available corneal topography systems.
Since the diffuse interaction of the light slit and the cornea can be ill-defined, the image processing will not be exact and so the measurements will contain some amount of error.
These techniques also suffer from the characteristic that a large number of images must be obtained and processed to estimate a large portion of the cornea.
The result is a large amount of data to process and store as well as the complexity of registration of the images due to movement of the eye during the acquisition period.
In contrast with man-made optical systems, human and animal eyes are optical systems in which the individual internal components of a given eye are not normally separately accessible for either direct measurement or adjustment, the output of the optical system is not directly accessible for analysis and the characteristics of individual components change over time with growth, aging and other factors.
Such determinations are subject to experimental errors and such events as accommodation of the eye to the substituted lens in a manner which gives the impression that a particular correction is desirable, when in fact that correction is not optimum.
Further, these measurement techniques determine corrections which improve overall vision, but are limited in normal practice to prism, cylindrical and spherical corrections which are low order corrections to the patient's actual, detailed vision errors which include higher order terms or characteristics which these measurement techniques cannot determine.
For the most part these prior art measurement systems are subjective and require the active participation of the patient for their success.
This requirement for active participation of the patient is a disadvantage in a number of circumstances such as in the diagnosis of small children who have difficulty in understanding what is being asked of them and prevents its use for infants who are incapable of indicating the effect of such lens substitutions.
The requirement for the active participation of the patient in the determination of the characteristics of the eye can have unfortunate effects.
Some anomalous conditions result in permanent disabilities because they are not detected during infancy because of the inability of infants to communicate with ophthalmologists.
For example, if one eye is in focus and the other is severely out of focus during the time the brain is developing its ability to interpret visual signals, then a permanent disability develops in which the out-of-focus eye is never able to contribute usefully to the brain's image recognition because of a lack of proper stimulation during the period in which the brain's image interpretation functions became established.
A person suffering from this condition can tell with the affected eye whether the lines in an image are sharp or fuzzy, but cannot assimilate the perceived information into an image.
Present subjective refraction measurement systems are incapable of determining the development of this condition in infants because they cannot accurately diagnose the visual acuity of the eye without the active participation of the patient.
However, each of these has had problems or deficiencies of its own.
One common deficiency is accommodation by the eye being measured.
Another common problem is determining and maintaining accurate alignment of the measurement system during the measurement cycle, since any misalignment can cause inaccurate results.
The resulting system is complex and is subject to errors due to patient movement.
Implementations of these lenslett array systems have been limited to research laboratories for several reasons.
In a clinical setting where exam time is important, finding which spectacle correction to use for each subject may be time prohibitive.
A more serious drawback is the problem of point "cross-over" shown in FIG. 17.
When this happens, the sign and / or magnitude of the partial derivatives of the wave front will contain a huge error.
Another issue is the choice of reference axis of the wave front aberration.
 Login to View More
Login to View More