
Spasmomen, a therapeutic agent based on Otilonium Bromide, is widely used in the treatment of Irritable Bowel Syndrome (IBS) and related gastrointestinal disorders. As IBS becomes increasingly prevalent, with symptoms ranging from abdominal pain to irregular bowel movements, clinicians and researchers are turning to evidence-based treatments that offer both efficacy and safety. Understanding the full therapeutic potential of compounds like Spasmomen requires deep visibility into molecular mechanisms, clinical trials, regulatory pathways, and real-world safety data. This is where tools like PatSnap Eureka AI Agent play a transformative role—empowering clinicians and pharmaceutical researchers to analyze therapeutic pathways and market dynamics of compounds like Otilonium Bromide, delivering insights across regulatory filings, clinical studies, and competitive IP landscapes.
What is Spasmomen?
Spasmomen is a proprietary brand name for Otilonium Bromide, a quaternary ammonium compound that functions as an intestinal antispasmodic. It is specifically designed to treat functional gastrointestinal disorders, primarily IBS, by reducing the motility and spasms of intestinal smooth muscles. It is important to note that Spasmoctyl and Otilo are alternative brand names containing the same active compound—Otilonium Bromide. While formulations and dosages may vary slightly by region, all are indicated for similar therapeutic use.
Spasmomen is well-regarded among gastroenterologists due to its localized action in the gut, minimal systemic absorption, and favorable safety profile, making it especially suitable for long-term symptom management in IBS patients.
Key Characteristics Snapshot
- Active Ingredient: Otilonium Bromide
- Drug Class: Quaternary ammonium antimuscarinic agent
- Target: Gastrointestinal smooth muscle
- Indications: Functional gastrointestinal disorders, especially IBS
- Advantages: Localized activity in the gut, minimal systemic absorption, favorable safety profile
Forms and Formulations
Spasmomen is available in oral formulations, typically in 40 mg or 80 mg tablet forms. The drug is often administered in divided doses throughout the day and is sometimes formulated with modified-release coatings to ensure sustained action.
| Formulation | Typical Strength | Route | Notes |
|---|---|---|---|
| Spasmomen Tablets | 40 mg / 80 mg | Oral | Often taken before meals |
| Spasmoctyl Capsules | 40 mg | Oral | Same active compound |
| Otilo Tablets | 40 mg | Oral | Alternate brand name |
Mechanism of Action
Its active ingredient, otilonium bromide, is a synthetic anticholinergic agent. The key mechanisms of action are as follows:
Anticholinergic Effects: As an anticholinergic, otilonium bromide inhibits the action of acetylcholine, a neurotransmitter, by blocking muscarinic receptors. This leads to a reduction in smooth muscle contractility and decreased secretions, which can help alleviate spasms and associated symptoms like pain and cramping.
Calcium Channel Blockade: Otilonium bromide has been shown to block L-type calcium channels, which are involved in the contraction of smooth muscles. By inhibiting these channels, the drug reduces the influx of calcium ions into the cells, leading to muscle relaxation. This mechanism is particularly relevant in the gastrointestinal tract, where smooth muscle contractions are regulated by calcium signaling.
Interaction with Enteric Neurons: The ability of otilonium bromide to block L-type Ca2+ channels may also extend to enteric neurons, which are part of the nervous system that controls gastrointestinal function. This interaction could further contribute to the drug’s spasmolytic effects by modulating neuronal activity in the gut.
In summary, Spasmomen’s mechanism of action involves both anticholinergic effects and calcium channel blockade, leading to smooth muscle relaxation and relief of spasms.
Clinical Uses
Spasmomen is primarily prescribed for the management of functional gastrointestinal disorders, with its most notable application being the treatment of Irritable Bowel Syndrome (IBS). Due to its targeted antispasmodic activity and favorable safety profile, Spasmomen is also effective in a broader range of GI-related conditions.

Irritable Bowel Syndrome (IBS)
This is the principal indication for Spasmomen. IBS is characterized by recurrent abdominal pain, bloating, and altered bowel habits (diarrhea, constipation, or both). Spasmomen works by acting directly on intestinal smooth muscle, inhibiting calcium influx and reducing hypermotility and spasm without systemic side effects.
- Clinical Evidence:
A comparative study showed that Spasmomen has a total effective rate of 76.2% after two weeks of treatment, outperforming the older antispasmodic 654-2, which had an effective rate of only 56%. Patients treated with Spasmomen not only experienced a significant reduction in abdominal pain and bowel irregularity but also reported improvements in vegetative functions (such as sleep and appetite) and psychoemotional status. Moreover, when combined with anxiolytic therapy, Spasmomen led to greater symptom relief and improved emotional well-being, suggesting its potential as part of a multidimensional IBS treatment strategy.
Functional Abdominal Pain
Spasmomen is used in cases of chronic or recurrent abdominal pain not explained by structural abnormalities. It effectively relaxes gastrointestinal muscles, relieving pain episodes associated with functional GI disorders.
Colonic and Rectal Spasms
In patients experiencing spastic colonic activity, rectal urgency, or pain, Spasmomen helps reduce muscular contraction and improve bowel comfort and control.
Bloating and Intestinal Discomfort
Bloating and pressure in the lower abdomen are often linked to dysfunctional motility. Spasmomen helps normalize peristalsis and reduce trapped gas sensations, improving overall patient quality of life.
Comparison with Other IBS Medications
While multiple treatment options exist for managing IBS, they vary in mechanism, efficacy, tolerability, and target patient subtypes (e.g., IBS-C, IBS-D, IBS-M). PatSnap Eureka AI Agent helps explore how Spasmomen compares to other commonly used agents:
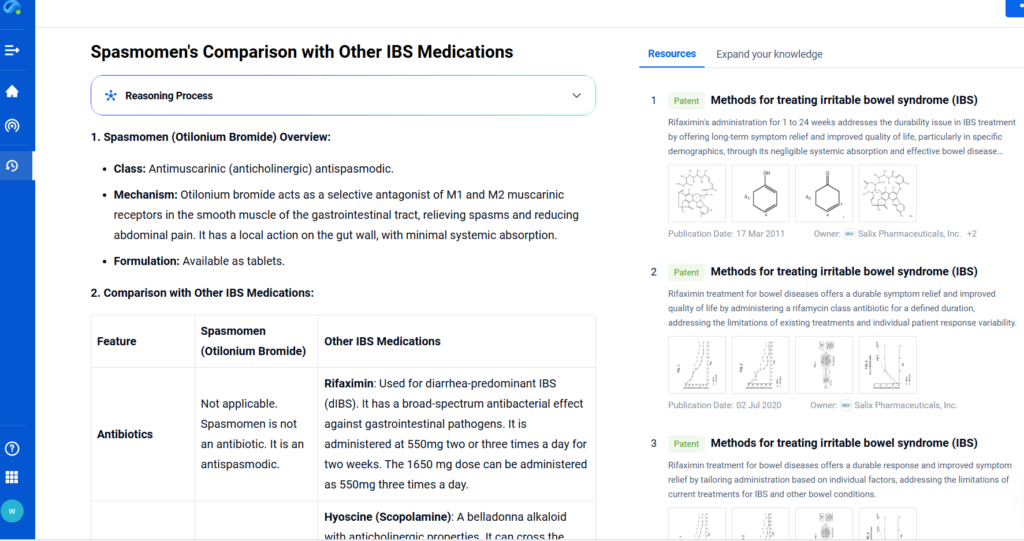
| Medication | Mechanism of Action | Primary IBS Subtype | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Spasmomen | Calcium channel blocker acting on GI smooth muscle | IBS-M / IBS-D | Localized gut action, low systemic side effects | Limited availability in some countries |
| Hyoscine Butylbromide (Buscopan) | Anticholinergic agent | IBS with spasms | Fast relief of cramping | Anticholinergic side effects (dry mouth, dizziness) |
| Mebeverine | Direct smooth muscle relaxant | IBS-A / IBS-M | Good tolerability, widely used in Europe | Less evidence in large-scale trials |
| Alosetron | 5-HT₃ receptor antagonist | IBS-D (women only) | Effective in severe diarrhea-predominant IBS | Restricted use due to ischemic colitis risk |
| Linaclotide | Guanylate cyclase-C agonist (pro-secretory) | IBS-C | Increases bowel movements, improves bloating | Diarrhea is a common side effect |
| Rifaximin | Non-absorbable antibiotic | IBS-D | Alters gut microbiota; short-term relief | Expensive; recurrence of symptoms common |
Using Eureka’s Competitive Intelligence module, researchers and product strategists can assess regional use trends, clinical trial outcomes, and safety profiles of these agents to optimize treatment positioning.
Key Takeaways:
- Spasmomen is particularly suited for patients seeking long-term symptom relief with minimal systemic exposure.
- Compared to newer agents like Linaclotide or Alosetron, Spasmomen offers a safer profile with broader applicability across IBS subtypes, especially in mixed or spasm-predominant cases.
- Unlike antibiotics like Rifaximin, Spasmomen does not disrupt gut microbiota, preserving digestive health in the long term.
Conclusion
s gastrointestinal disorders like IBS become increasingly recognized and diagnosed, the need for well-tolerated, effective treatment options is more urgent than ever. Spasmomen, through its active compound Otilonium Bromide, offers targeted relief by acting directly on the gut’s smooth muscles without significant systemic effects.
What sets Spasmomen apart is its local action, patient-friendly safety profile, and clinically validated efficacy across multiple IBS subtypes. For life science professionals tracking therapeutic innovations in this space, PatSnap Eureka enables real-time access to the latest trial results, regulatory approvals, and molecular insight—making it an essential companion for those navigating complex gastrointestinal drug development or clinical use decisions.
FAQs
Yes. All three are brand names for Otilonium Bromide, with regional naming variations.
While generally used for short-to-medium-term symptom relief, long-term use may be considered under medical supervision due to its low systemic impact.
Unlike drugs with systemic anticholinergic effects, Spasmomen acts locally in the gut, reducing side effects and improving patient compliance.
Spasmomen may help IBS – D – related diarrhea by relaxing gut muscles. Not for general diarrhea (e.g., infections). Consult a doctor.
For a deeper understanding of Spasmomen, try PatSnap Eureka AI Agent which can offer detailed intelligence on global trials, publications, and market landscapes for Otilonium Bromide and its analogs.

